Abstract
We report the case of a female patient with severe acute necrotizing pancreatitis associated with hypercalcemia as first manifestation of primary hyperparathyroidism caused by a benign parathyroid adenoma. Initially the acute pancreatitis was treated conservatively. The patient subsequently underwent surgical resection of the parathyroid adenoma and surgical clearance of a large infected pancreatic pseudocyst. Although the association of parathyroid adenoma-induced hypercalcemia and acute pancreatitis is a known medical entity, it is very uncommon. The pathophysiology of hypercalcemia-induced acute pancreatitis is therefore not well known, although some mechanisms have been proposed. It is important to treat the provoking factor. Therefore, the cause of hypercalcemia should be identified early. Surgical resection of the parathyroid adenoma is the ultimate therapy.
Keywords: Acute necrotizing pancreatitis, Hypercalcemia, Primary hyperparathyroidism, Parathyroid adenoma
INTRODUCTION
Acute necrotizing pancreatitis is a severe condition with a high mortality rate[1]. In the Western world, alcohol and biliary stones are the main causes of acute pancreatitis[2,3]. As shown by the Ranson[4] grading of acute nonalcoholic pancreatitis, severe pancreatitis is associated with a decrease in serum calcium levels. However, the relationship between increased serum calcium levels and acute pancreatitis may be a diagnostic clue to primary hyperparathyroidism (PHPT)[5]. Acute pancreatitis caused by hypercalcemia due to PHPT is a very rare condition[6]. We present a case report of a young female patient with hypercalcemia-induced acute necrotizing pancreatitis as first manifestation of a benign parathyroid adenoma.
CASE REPORT
A 42-year-old female presented at the emergency room with a sudden attack of severe epigastric pain and vomiting. Years ago she had undergone surgery for a benign ovarian cyst and a right nephrectomy for ureterolithiasis-induced hydronephrosis. Her medical history also mentioned three episodes of deep vein thrombosis in the lower limb.
She was a non-smoker and consumed alcohol only sporadically. There was no recent use of alcohol. She did not take medication and did not travel abroad. Family history mentioned a brother infected with hepatitis B virus.
Clinical examination revealed a severely ill patient, a silent abdomen which was distended with painful percussion and palpation of the epigastrium.
Blood analysis showed signs of inflammation with an elevated C-reactive protein (CRP) of 6.77 mg/dL (< 0.5 mg/dL) and leukocytosis of 30.8 × 10E9/L (4.3-10 × 10E9/L) with elevated neutrophils of 28.1 × 10E9/L (2.0-7.0 × 10E9/L). Pancreatic enzymes were elevated, serum amylase was 1033 U/L (24-72 U/L) and serum lipase was 7189 U/L (13-300 U/L). There was a slight impairment of renal function as shown by an increase in serum creatinine 1.23 mg/dL (0.6-1.1 mg/dL). Both liver transaminases and canalicular liver tests were normal. In contrast to what was expected in a case of severe pancreatitis, serum calcium was increased to 11.7 mg/dL (8.5-10.2 mg/dL), the albumin-modified serum calcium concentration was 11.9 mg/dL. IgG4 was normal as were triglycerides.
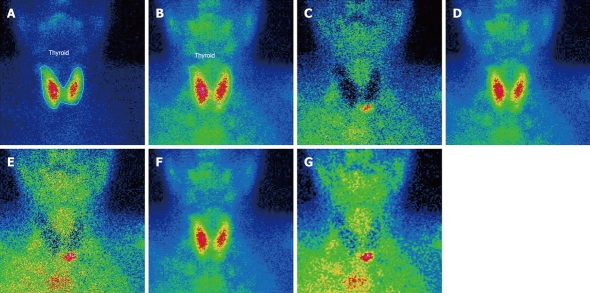
Based on the clinical picture and blood analysis she was diagnosed with acute pancreatitis. Abdominal ultrasound was carried out and showed no evidence of cholelithiasis or dilated bile ducts. Abdominal computed tomography (CT) scan confirmed the diagnosis of exudative pancreatitis (Figure 1A). The patient was admitted to the ward and was treated conservatively with intravenous fluids and analgesia. Because of slow improvement of paralytic ileus, enteral feeding was started through a nasojejunal tube. The patient improved gradually during the following weeks. At day 20 after admission, abdominal CT scan was repeated and showed the development of pancreatic pseudocysts and necrosis of the pancreas with few remnants of normal pancreatic tissue (Figure 1B).
Figure 1.
Abdominal computed tomography scan at the level of the pancreas. A: On the day of admission showing acute exudative pancreatitis. Note the history of a right nephrectomy; B: On day 20 showing the development of pancreatic pseudocysts and few remnants of normal pancreatic tissue.
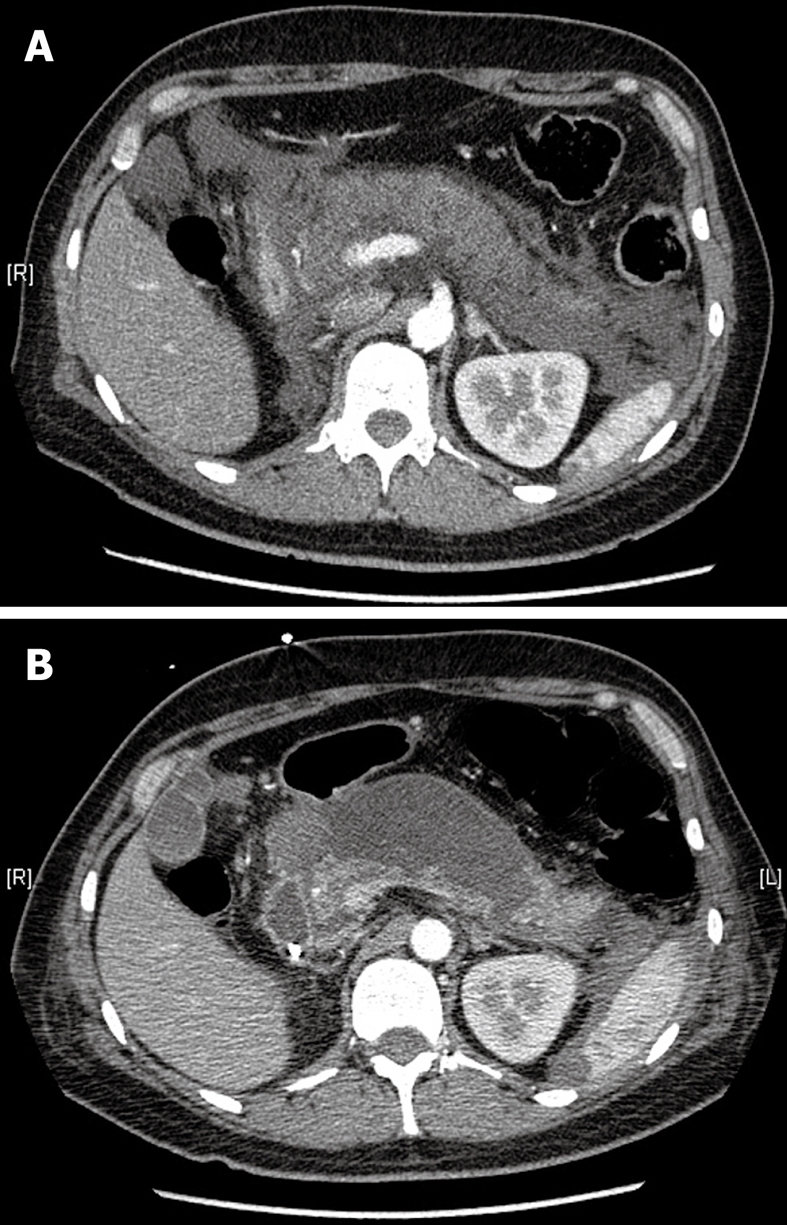
After exclusion of alcohol-induced and biliary pancreatitis as well as auto-immune pancreatitis, elevated serum calcium levels remained another potential etiology of acute pancreatitis. On reviewing her medical records, normal serum calcium levels at the time of previous surgical interventions was noted. Serum levels of intact parathyroid hormone (iPTH) were determined and showed an increase up to 82 pg/mL (13-54 pg/mL). This result confirmed hypercalcemia caused by hyperparathyroidism. Ultrasound of the parathyroid glands showed no abnormalities. A 99mTc-Sestamibi scintigraphy was then carried out which was consistent with a lower left side parathyroid adenoma (Figure 2).
Figure 2.
99mTc-Sestamibi scintigraphy showing a lower left side parathyroid adenoma. A: Thyroid SKM: SK ELUAAT, -Tc-99mANT; B: Parathyroid SKM: SK MIBI, -Tc-99mH1; C: Normalized subtracted f = 1; D: Registered parathyroid; E: Normalized subtracted f = 1.25; F: Normalized parathyroid f = 1.25; G: Smoothed subtracted f = 1.25.
The patient underwent surgical resection of this tumor, and histological examination confirmed the diagnosis of benign parathyroid adenoma. In the postoperative period, serum levels of iPTH and calcium decreased and the patient required calcium supplements. Following clinical resolution, the patient was discharged from hospital.
A few weeks later she was re-admitted to the emergency room due to abdominal pain and fever. Blood analysis showed elevated CRP of 15.18 mg/dL (< 0.5 mg/dL), serum amylase and serum lipase were normal. Serum calcium was slightly decreased: 8.3 mg/dL (8.5-10.2 mg/dL). Infection of the previously diagnosed pancreatic pseudocysts was suspected. Abdominal magnetic resonance imaging (MRI) and endoscopic ultrasonography showed debris in the large pseudocyst (Figure 3). Initially she was treated with broad spectrum antibiotics, however, she suffered recurrent episodes of fever and abdominal pain. Abdominal CT scan revealed rupture of the largest pancreatic pseudocyst. Surgical cystogastrostomy and necrosectomy of the pancreatic corpus was performed. She recovered well and the patient remained free of symptoms without signs of exocrine or endocrine pancreas insufficiency.
Figure 3.
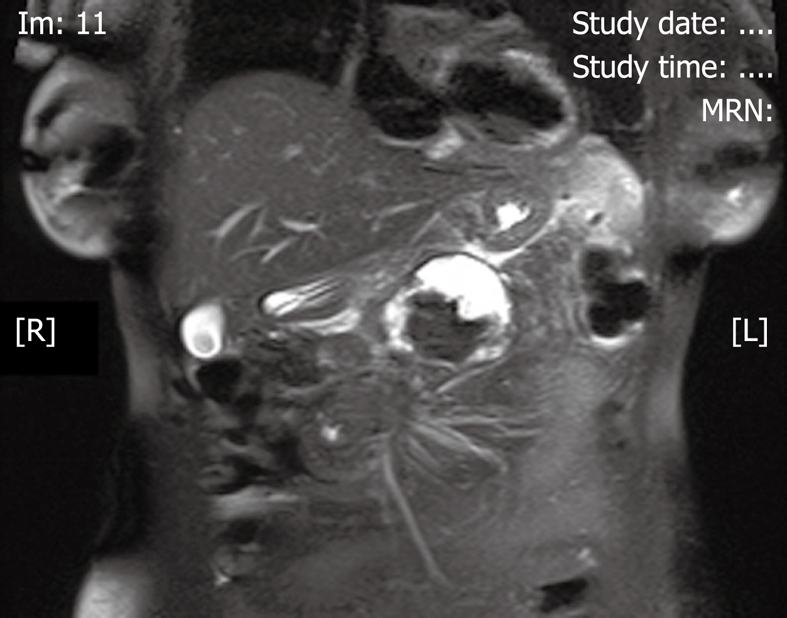
Abdominal magnetic resonance imaging at the level of the pancreas showing debris in the pancreatic pseudocyst.
DISCUSSION
Acute pancreatitis caused by PHPT-induced hypercalcemia is a rare condition. It was first described in 1957 by Cope et al[5]. Since then, the relationship between PHPT and pancreatitis has been questioned, but nowadays PHPT has been acknowledged as an accepted etiology of pancreatitis[1,7,8]. The prevalence of acute pancreatitis in patients with PHPT is estimated between 1.5% and 7%[6]. Some studies have associated hyperparathyroidism with pancreatitis, however, the prevalence of acute pancreatitis in patients with PHPT seems no different from that in the general population[9,10]. Therefore, there appears to be no direct causal relationship between PHPT and acute pancreatitis based on epidemiological data. However, it has been shown that hypercalcemia of any cause can lead to acute pancreatitis[11]. When this combination occurs, pancreatitis is likely to be severe and the degree of hypercalcemia may play an important role in this association[12,13]. Three pathophysiological mechanisms are suggested. The deposition of calcium in the pancreatic duct may cause pancreatic duct obstruction[14]. Hypercalcemia may also lead to activation of trypsinogen within the pancreatic parenchyma causing autodigestion of the pancreas[15]. Finally, genetic variants in SPINK 1 (serine protease inhibitor Kazal type 1) and CFTR (cystic fibrosis transmembrane conductance regulator) genes in combination with hypercalcemia increase the risk of developing acute pancreatitis in patients with PHPT[16].
Usually, acute pancreatitis is associated with a decrease in serum calcium levels. Based on the Ranson[4] grading, low serum calcium levels have prognostic importance. Therefore, it is uncommon to detect hypercalcemia in a patient presenting with severe acute pancreatitis. This unusual condition should always alert physicians to the presence of hyperparathyroidism or malignancy[17,18]. In order to complete the diagnosis, parathyroid hormone levels should be determined and imaging of the parathyroid glands is important. It is also important to take into account the possibility of an ectopic localization of a parathyroid adenoma as a cause of acute pancreatitis[19,20]. In the present case, diagnosis of the parathyroid tumor was made by 99mTc-Sestamibi scintigraphy. Surgical resection and histological examination of the tumor is the ultimate therapy and parathyroidectomy may prevent the recurrence of pancreatitis[7,12]. Subsequent rapid hypocalcemia may develop requiring calcium supplementation. Good cooperation between gastroenterologists, endocrinologists and surgeons is important in treating this rare phenomenon of acute necrotizing pancreatitis caused by PHPT-induced hypercalcemia.
Footnotes
Peer reviewer: Takashi Kobayashi, MD, PhD, Department of Surgery, Showa General Hospital, 2-450 Tenjincho, Kodaira, Tokyo 187-8510, Japan
S- Editor Tian L L- Editor Webster JR E- Editor Lin YP
References
- 1.Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 2.Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168:649–656. doi: 10.1001/archinte.168.6.649. [DOI] [PubMed] [Google Scholar]
- 3.Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 4.Ranson JH. Etiological and prognostic factors in human acute pancreatitis: a review. Am J Gastroenterol. 1982;77:633–638. [PubMed] [Google Scholar]
- 5.Cope O, Culver PJ, Mixter CG Jr, Nardi GL. Pancreatitis, a diagnostic clue to hyperparathyroidism. Ann Surg. 1957;145:857–863. doi: 10.1097/00000658-195706000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egea Valenzuela J, Belchí Segura E, Sánchez Torres A, Carballo Alvarez F. Acute pancreatitis associated with hypercalcemia. A report of two cases. Rev Esp Enferm Dig. 2009;101:65–69. doi: 10.4321/s1130-01082009000100009. [DOI] [PubMed] [Google Scholar]
- 7.Carnaille B, Oudar C, Pattou F, Combemale F, Rocha J, Proye C. Pancreatitis and primary hyperparathyroidism: forty cases. Aust N Z J Surg. 1998;68:117–119. doi: 10.1111/j.1445-2197.1998.tb04719.x. [DOI] [PubMed] [Google Scholar]
- 8.Koppelberg T, Bartsch D, Printz H, Hasse C, Rothmund M. [Pancreatitis in primary hyperparathyroidism (pHPT) is a complication of advanced pHPT] Dtsch Med Wochenschr. 1994;119:719–724. doi: 10.1055/s-2008-1058752. [DOI] [PubMed] [Google Scholar]
- 9.Khoo TK, Vege SS, Abu-Lebdeh HS, Ryu E, Nadeem S, Wermers RA. Acute pancreatitis in primary hyperparathyroidism: a population-based study. J Clin Endocrinol Metab. 2009;94:2115–2118. doi: 10.1210/jc.2008-1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bess MA, Edis AJ, van Heerden JA. Hyperparathyroidism and pancreatitis. Chance or a causal association? JAMA. 1980;243:246–247. [PubMed] [Google Scholar]
- 11.Brandwein SL, Sigman KM. Case report: milk-alkali syndrome and pancreatitis. Am J Med Sci. 1994;308:173–176. doi: 10.1097/00000441-199409000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Prinz RA, Aranha GV. The association of primary hyperparathyroidism and pancreatitis. Am Surg. 1985;51:325–329. [PubMed] [Google Scholar]
- 13.Curto C, Caillard C, Desurmont T, Sebag F, Brunaud L, Kraimps JL, Hamy A, Mathonnet M, Bresler L, Henry JF, et al. [Acute pancreatitis and primary hyperparathyroidism: a multicentric study by the Francophone Association of Endocrine Surgeons] J Chir (Paris) 2009;146:270–274. doi: 10.1016/j.jchir.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Ward JB, Petersen OH, Jenkins SA, Sutton R. Is an elevated concentration of acinar cytosolic free ionised calcium the trigger for acute pancreatitis? Lancet. 1995;346:1016–1019. doi: 10.1016/s0140-6736(95)91695-4. [DOI] [PubMed] [Google Scholar]
- 15.Mithöfer K, Fernández-del Castillo C, Frick TW, Lewandrowski KB, Rattner DW, Warshaw AL. Acute hypercalcemia causes acute pancreatitis and ectopic trypsinogen activation in the rat. Gastroenterology. 1995;109:239–246. doi: 10.1016/0016-5085(95)90290-2. [DOI] [PubMed] [Google Scholar]
- 16.Felderbauer P, Karakas E, Fendrich V, Bulut K, Horn T, Lebert R, Holland-Letz T, Schmitz F, Bartsch D, Schmidt WE. Pancreatitis risk in primary hyperparathyroidism: relation to mutations in the SPINK1 trypsin inhibitor (N34S) and the cystic fibrosis gene. Am J Gastroenterol. 2008;103:368–374. doi: 10.1111/j.1572-0241.2007.01695.x. [DOI] [PubMed] [Google Scholar]
- 17.Braun C, Duffau P, Mahon FX, Rosier E, Leguay T, Etienne G, Michaud M. [Acute pancreatitis due to hypercalcemia revealing adult T-cell leukemia] Rev Med Interne. 2007;28:116–119. doi: 10.1016/j.revmed.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Kanno K, Hikichi T, Saito K, Watanabe K, Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A, et al. A case of esophageal small cell carcinoma associated with hypercalcemia causing severe acute pancreatitis. Fukushima J Med Sci. 2007;53:51–60. doi: 10.5387/fms.53.51. [DOI] [PubMed] [Google Scholar]
- 19.Imachi H, Murao K, Kontani K, Yokomise H, Miyai Y, Yamamoto Y, Kushida Y, Haba R, Ishida T. Ectopic mediastinal parathyroid adenoma: a cause of acute pancreatitis. Endocrine. 2009;36:194–197. doi: 10.1007/s12020-009-9223-x. [DOI] [PubMed] [Google Scholar]
- 20.Foroulis CN, Rousogiannis S, Lioupis C, Koutarelos D, Kassi G, Lioupis A. Ectopic paraesophageal mediastinal parathyroid adenoma, a rare cause of acute pancreatitis. World J Surg Oncol. 2004;2:41. doi: 10.1186/1477-7819-2-41. [DOI] [PMC free article] [PubMed] [Google Scholar]