Abstract
Objective
Vaginal bleeding is a risk factor for preterm PROM (PPROM). A disorder of decidual hemostasis has been implicated in the genesis of PROM. Indeed, excessive thrombin generation has been demonstrated in PPROM both before and at the time of diagnosis. Decidua is a potent source of tissue factor (TF), the most powerful natural pro-coagulant. A decidual hemostatic disorder may link vaginal bleeding, PPROM, and placental abruption. This study was conducted to determine the behavior of maternal TF and its natural inhibitor, the tissue factor pathway inhibitor (TFPI) in PPROM.
Methods
This cross-sectional study included women with PPROM (n=123) and women with normal pregnancies (n=86). Plasma concentrations of TF and TFPI were measured by a sensitive immunoassay. Non-parametric statistics were used for analysis.
Results
1) The median maternal plasma TF concentration was significantly higher in patients with PPROM than in women with normal pregnancies (median: 369.5 pg/ml; range: 3.27-2551 pg/ml vs. median: 291.5 pg/ml; range: 6.3-2662.2 pg/ml, respectively; p=0.001,); 2) the median maternal TFPI plasma concentration was significantly lower in patients with PPROM than in women with a normal pregnancies (median: 58.7 ng/ml; range: 26.3-116 ng/ml vs. median: 66.1 ng/ml; range: 14.3-86.5 ng/ml, respectively; p=0.019); 3) there was no correlation between the plasma concentration of TF and TFPI and the gestational age at sample collection; and 4) among patients with PPROM there was no association between the presence of intra-amniotic infection or inflammation and median plasma concentrations of TF and TFPI.
Conclusions
1) Patients with PPROM have a higher median plasma concentration of TF and a lower median plasma concentration of TFPI than women with normal pregnancies. 2) These findings suggest that PPROM is associated with specific changes in the hemostatic/coagulation system.
Keywords: coagulation, inflammation, pregnancy, preterm delivery, thrombin, prelabor rupture of membranes, thrombosis, prematurity
INTRODUCTION
Preterm prelabor rupture of membranes (PROM) is associated with placental vascular lesions including a failure of physiologic transformation of the spiral arteries [1], atherosis, and decidual vasculopathy (i.e. fibrinoid necrosis and thrombosis of decidual vessels) [1,2]. Moreover, women with preterm PROM have a higher median maternal plasma concentration of thrombin-antithrombin (TAT) complexes than women with normal pregnancies [3,4]. Thus, the activation of the coagulation cascade that results in an increased thrombin generation may be one of the mechanisms of disease leading to preterm PROM.
The activation of the coagulation system in the placental and maternal compartment of patients with preterm PROM can result from the following underlying mechanisms of disease: 1) decidual hemorrhage that leads to a retro-placental clot formation [5]; 2) intra-amniotic infection which can induce decidual bleeding and sub-clinical abruption [6], as well as increased intra-amniotic TAT complexes [7]; and 3) an increased maternal systemic inflammatory response [8] that may activate the extrinsic pathway of coagulation due to the expression and release of tissue factor (TF) by activated monocytes [9]. These mechanisms result in an increased thrombin generation, which has been associated with the following: 1) stimulation of decidual cell secretion of matrix metalloproteinases (MMP) (i.e. MMP-1 [10] and MMP-3 [11]) that can degrade the extracellular matrix of the chorioamniotic membranes; and 2) myometrial activation and uterine contractions generation that may lead to preterm labor with or without rupture of membranes and a subsequent preterm delivery [12-14].
While thrombin is generated as a consequence of activation of the coagulation cascade, TF, the most powerful natural pro-coagulant, is abundant in the uterine decidua in the normal state [15,16]. Tissue factor is part of an efficient hemostatic mechanism in the uterine wall, which is activated in the course of normal pregnancy during implantation [17] and after delivery [18]. However, this hemostatic mechanism may also be activated due to pathological decidual bleeding in pregnancies complicated by placental abruption [5,19] and intra-amniotic infection [6].
The main physiological inhibitor of the TF pathway is tissue factor pathway inhibitor (TFPI), which is a glycoprotein comprise of three Kunitz domain[20] that are specific inhibitors of trypsin-like proteinases[21]. The mean maternal plasma concentration of total TFPI (TFPI-1 and TFPI-2) have been reported to increase during pregnancy until 20 weeks of gestation, to remain relatively constant until term [22] and to decrease during labor [23]. There are two types of TFPI: 1) TFPI-1 is the more prevalent form in the non-pregnant state in the maternal circulation and can also be found in the fetal blood, platelets, endothelial cells and other organs [24,25]; and 2) TFPI-2- the major form of TFPI in the placenta [26-31], is also known as Placental Protein 5 (PP5) [32,33]. During pregnancy, the maternal plasma concentration of TFPI-2 increases gradually, reaches a plateau at 36 weeks and subsides after delivery [33-38].
Pregnancy complications are associated with changes in the maternal plasma and placental concentration of TF and TFPI. Maternal plasma concentrations of TF and free TFPI are higher in women with preeclampsia than in patients with a normal pregnancy [39-41]. Placental TF concentrations and mRNA expression are higher in patients with severe preeclampsia than in those with a normal pregnancy [42]. In contrast, placentas of patients with gestational vascular complications (preeclampsia, eclampsia, fetal growth restriction, placental abruption, and fetal demise) have lower placental concentrations of total TFPI and mRNA expression than in those of patients with a normal pregnancy [43].
The increased thrombin generation in the maternal plasma of patients with preterm PROM [3,4] reflects the activation of the coagulation cascade; however, it is not clear whether this activation is associated with changes in TF and TFPI plasma concentrations as well. Thus, the objective of this study is to determine the changes in the maternal plasma concentrations of TF and its natural inhibitor TFPI in women with preterm PROM.
METHODS
Study design
This cross-sectional study included patients in the following groups: 1) patients with preterm PROM (n=123), and 2) women with normal pregnancies (n=86). Patients with multiple pregnancies or fetuses with congenital and/or chromosomal anomalies were excluded.
Samples and data were retrieved from the bank of biological samples and clinical databases. Many of these samples have been previously used to study the biology of inflammation, hemostasis, angiogenesis regulation, and growth factor concentrations in non-pregnant women, normal pregnant women and those with pregnancy complications. All women provided a written informed consent prior to the collection of maternal blood. The Institutional Review Boards of both Wayne State University and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD/NIH/DHHS) approved the collection and utilization of the samples for research purposes.
Definitions
Women were considered to have a normal pregnancy if they did not have obstetrical, medical, or surgical complication of pregnancy, and delivered a term neonate of appropriate birth weight for gestational age without complications. Preterm PROM was diagnosed by a sterile speculum examination demonstrating pooling of amniotic fluid in the vagina (with nitrazine and ferning tests when necessary) occurring <37 weeks of gestation in the absence of labor.
Amniotic fluid collection was performed by trans-abdominal amniocentesis under ultrasonographic guidance in order to determine the microbiologic state of the amniotic cavity in a subset of patients at the discretion of the treating physician. Amniotic fluid was transported to the laboratory in a capped plastic syringe and cultured for aerobic, anaerobic bacteria, as well as for genital Mycoplasmas. White blood cell (WBC) count, glucose concentration, and Gram stain for microorganisms were performed in amniotic fluid shortly after collection. Intra-amniotic infection was defined by the presence of amniotic fluid cultures that were positive for microorganisms and inflammation by an amniotic fluid WBC count ≥ 100 cells/ml. The results of the amniotic fluid analyses were used for clinical management. Small for gestational age (SGA) neonate was defined as birthweight below the 10th percentile [44].
Placental histopathologic examinations
Placental tissue samples were taken by systematic random sampling, and subsequently fixed in 10% neutral buffered formalin overnight, and embedded in paraffin. Five mm-thick paraffin sections were stained with haematoxylin and eosin, and examined using bright-field light microscopy. Histopathologic examinations were performed by three pathologists who were blinded to the clinical information. The placental histologic lesions were classified according to a diagnostic schema proposed by Redline et al [45].
Blood samples collection
All blood samples were collected with a vacutainer into 0.109M trisodium citrate anticoagulant solution (BD; San Jose, CA, USA). The samples were centrifuged at 1300g for 10 minutes at 4°C and stored at −70°C until assayed.
Human tissue factor (TF) immunoassays
Maternal plasma TF concentrations were determined by sensitive and specific immunoassays obtained from American Diagnostica (Greenwich, CT, USA) which recognizes TF-apo, TF and TF-FVII complexes. The assay was conducted according to the manufacturer’s recommendations. The calculated coefficient of variation (CV) in our laboratory was 5.3%, and the sensitivity is 10 pg/ml.
Human tissue factor pathway inhibitor (TFPI) immunoassay
The concentrations of TFPI in maternal plasma were determined by sensitive and specific immunoassays obtained from American Diagnostica (Greenwich, CT, USA). The TFPI ELISA employs a murine anti-TFPI monoclonal as the capture antibody. This capturing antibody is directed against the Kunitz-1 domain of the TFPI molecule; therefore, it detects both TFPI-1 and TFPI-2 and measures the total TFPI plasma concentrations. The assay was conducted according to the manufacturer’s recommendations. The calculated CV in our laboratory was 6.6%, and the sensitivity is approximately 10 ng/ml. The correlation between TFPI antigen concentrations and functional activity is approximately r2 = 0.785.
Statistical analysis
Plasma concentrations of TF and TFPI were not normally distributed. Thus, a Mann–Whitney U test was used for comparisons of continuous variables, and a Chi-square test was used to compare categorical variables. The Spearman’s rho test was used to detect a correlation between the maternal plasma TF and TFPI concentrations and the gestational age at blood collection in women with normal pregnancies. A p-value <0.05 was considered statistically significant. The statistical package employed was SPSS version 12 (SPSS Inc., Chicago, IL, USA).
RESULTS
Demographic characteristics and changes in maternal plasma TF and TFPI concentrations during normal pregnancy
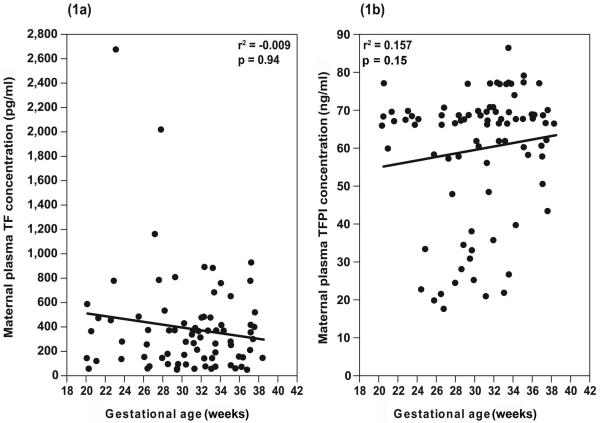
Table I displays the demographic and clinical characteristics of the study groups. Patients with preterm PROM had a lower median gestational age at blood sample collection and at delivery, as well as a lower median neonatal birth weight in comparison to the control group. There was no significant correlation between the maternal plasma TF and TFPI concentrations and the gestational age at blood sample collection in patients with normal pregnancy (TF: r= −0.009, p=0.94; TFPI: r= 0.157, p=0.15) (Figure 1).
Table I.
Demographic and clinical characteristics of the study population
| Normal pregnancy (n= 86) |
Preterm PROM (n= 123) |
P value | |
|---|---|---|---|
| Maternal age (years) | 24 (21-27) | 24 (10.25-31) | 0.09 |
| Gravidity€ | |||
| 1 | 18 (21.4%) | 18 (14.6%) | |
| 2-5 | 53 (63.1%) | 78 (63.4%) | 0.3 |
| ≥6 | 13 (15.5%) | 27 (22%) | |
| Parity§ | |||
| 1 | 46 (54.1%) | 59 (48.8%) | |
| 2-5 | 38 (44.7%) | 53 (43.8%) | 0.1 |
| ≥6 | 1 (1.2%) | 9 (7.4%) | |
| Ethnic origin £ | |||
| African-American | 67 (80.7%) | 105 (85.4%) | |
| Caucasian | 11 (13.3%) | 16 (13.0%) | |
| Hispanic | 2 (2.4%) | 1 (0.8%) | 0.119 |
| Asian | 3 (3.6%) | 1 (0.8%) | |
| Gestational age at blood collection (weeks) |
31.1 (27.4-35) | 30.1 (26-32.5) | 0.024 |
| Gestational age at delivery (weeks) |
39.6 (38.4-40.7) | 31.6 (27.2-33.1) | <0.0001 |
| Induction of labor | 16 (22.9%) | 49 (42.6%) | 0.006 |
| Cesarean delivery* | 24 (33.8%) | 34 (27.9%) | 0.5 |
| Neonatal birthweight | 3342.5 (3050-3700) | 1580 (957-2040) | <0.0001 |
Data are presented as median (interquartile range) or numbers (%)
Normal pregnancy (n= 84)
Normal pregnancy (n= 85)
Normal pregnancy (n=68)
Normal pregnancy (n=71); Preterm PROM ( n=122)
PROM – prelabor rupture of membranes
Figure 1.
The correlations between maternal plasma tissue factor (TF)(1a) and tissue factor pathway inhibitor (TFPI) (1b) concentrations and gestational age at blood collection.
Changes in maternal plasma TF and TFPI concentrations among patients with preterm PROM and their association with intra-amniotic infection/inflammation
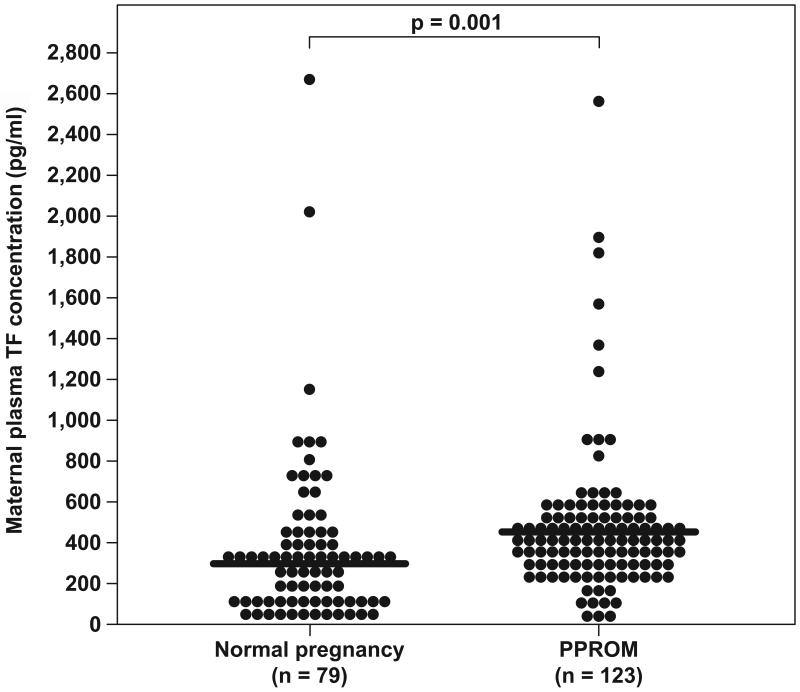
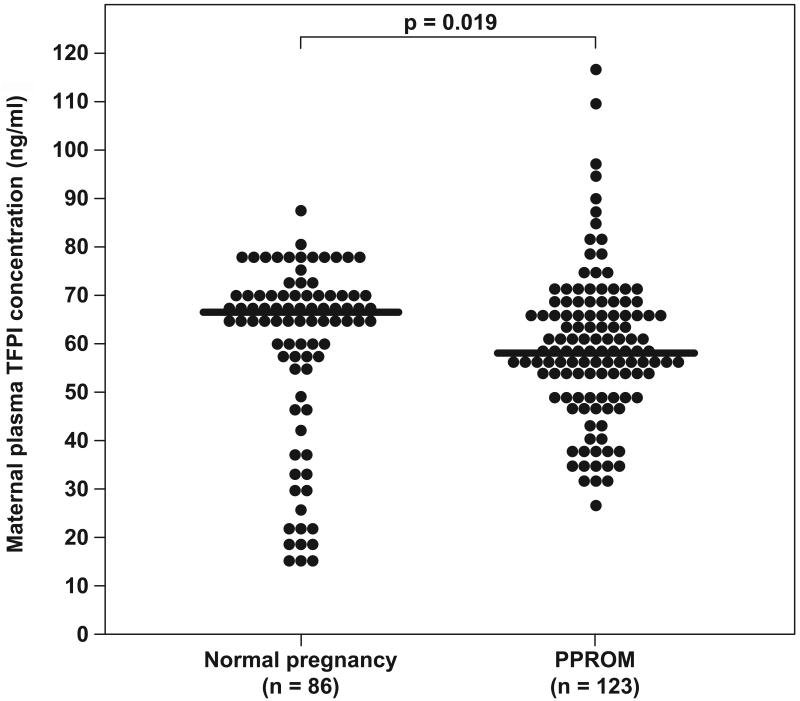
Of the 86 patients in the normal pregnancy group 91.9% (79/86) had detectable immunoreactive TF in the plasma. Maternal plasma TF concentrations were significantly higher in women with preterm PROM than those with a normal pregnancy (median: 369.5 pg/ml; range: 3.3-2551 pg/ml vs. median: 291.5 pg/ml; range: 6.3-2662.2 pg/ml, respectively; p=0.001) (Figure 2). In contrast, maternal plasma TFPI concentrations were significantly lower in women with preterm PROM than those with a normal pregnancy (median: 58.7 ng/ml; range: 26.3-116 ng/ml vs. median: 66.1 ng/ml; range: 14.3-86.5 ng/ml, respectively; p=0.019) (Figure 3). Patients with preterm PROM had a significantly lower median maternal plasma TFPI/TF ratio than those with normal pregnancies (median: 142.8; range: 21.8-16422 vs. median: 221.5; range: 25.4-3355.3l, respectively; p<0.0001).
Figure 2.
Comparison of maternal plasma tissue factor (TF) concentrations between women with normal pregnancy (n=79) and patients with preterm PROM (n=123). Tissue factor plasma concentrations were significantly higher in patients with preterm PROM than in women with a normal pregnancy (median: 369.5 pg/ml; range: 3.27-2551 pg/ml vs. median: 291.5 pg/ml; range: 6.3-2662.2 pg/ml, respectively; p=0.001).
Figure 3.
Comparison of maternal plasma tissue factor pathway inhibitor (TFPI) concentrations between women with normal pregnancy (n=86) and patients with preterm PROM (n=123). TFPI plasma concentrations were significantly lower in patients with preterm PROM than in women with a normal pregnancy (median: 58.7 ng/ml; range: 26.3-116 ng/ml vs. median: 66.1 ng/ml; range: 14.3-86.5 ng/ml, respectively; p=0.019).
Sixty-eight patients in the preterm PROM group underwent amniocentesis, of which 54.4% (37/68) had intra-amniotic infection/inflammation. Isolated intra-amniotic inflammation was diagnosed in 16.2% (11/68) of the cases. Positive amniotic fluid cultures for microorganisms were detected in 38.2% (26/68) of patients with preterm PROM (the frequency of the specific microorganisms is presented in Table II).
Table II.
Microorganisms isolated from the amniotic cavity in patients with preterm PROM who underwent trans-abdominal amniocentesis
| Microorganism | n(%) |
|---|---|
| Ureaplasma urealyticum | 6 (23.07%) |
| Mycoplasma hominis | 2 (7.6%) |
| Niesseria gonorrhea | 2 (7.6%) |
| Streptococcus agalactiae | 2 (7.6%) |
| Mixed flora | 10(38.5%) |
| Others | 4 (15.4%) |
Table III displays the changes in the median maternal plasma TF and TFPI concentrations according to the presence or absence of intra-amniotic infection and/or inflammation. The patients in both subsets of the preterm PROM group (with and without intra-amniotic infection/inflammation) had a significantly higher median maternal plasma TF concentration than women with normal pregnancies. There were no significant differences in the median maternal plasma TF and TFPI concentrations between preterm PROM patients with and without intra-amniotic infection and/or inflammation. (Table IV).
Table III.
Maternal plasma concentrations of Tissue factor and Tissue factor pathway inhibitor in patients with preterm PROM with and without intra-amniotic infection and/or inflammation in comparison to women with normal pregnancy
| Preterm PROM without IAI (n=31) |
Preterm PROM with IAI (n=37) |
p value | Normal pregnancy (n=86) |
p value‡ | |
|---|---|---|---|---|---|
| Tissue factor (pg/mL)† |
423.5* (3.3-899.4) |
369.4* (105.3-2551.0) |
0.9 | 291.5 (6.3-2662.2) |
0.026 |
| Tissue factor pathway inhibitor (ng/mL) |
58.7 (31.2-116.0) |
59.7 (37.8-83.6) |
0.3 | 66.1 (14.3-86.5) |
0.23 |
Data presented as median (minimum, maximum)
IAI: intra-amniotic infection/inflammation
PROM: prelabor rupture of membranes
p<0.05 in comparison to normal pregnancy group
normal pregnancy (n= 79)
Kruskal Wallis test
Table IV.
Placental lesions in patients with preterm PROM
| Placental histologic findings | Preterm PROM n= 101 |
|---|---|
| Findings consistent with amniotic fluid infection | |
| Chorioamnionitis, maternal response | 59 (58.4%) |
| Chorioamnionitis, fetal response | 49(48.5%) |
| Findings consistent with maternal underperfusion | |
| Remote villous infarcts | 1 (0.9%) |
| Recent villous infarcts | - |
| Increased syncytial knots | 5(4.95) |
| Villous agglutination | - |
| Increased intervillous fibrin | 1(0.9%) |
| Decreased placental weight | - |
| Distal villous hypoplasia | 3(2.97%) |
| Persistent muscularization of basal plate arteries | 6(5.9%) |
| Mural hypertrophy of decidual arterioles | 1(0.9%) |
| Acute atherosis of basal plate arteries/decidual arterioles | - |
| Findings consistent with fetal vascular thrombo-occlusive disease | |
| Early villous stromal-vascular karyorrhexis | - |
| Exclusively small foci | 1 (0.9%) |
| Variable size foci | - |
| Fetal thrombotic vasculopathy | 1 (0.9%) |
| Thrombi, large fetal vessels | - |
| Intimal fibrin cushions, large fetal vessels | - |
| Fibromuscullar sclerosis, Intermediate size fetal vessels | - |
| Chronic villitis with obliterative fetal vasculopathy | 4 (3.96%) |
PROM – prelabor rupture of membranes
Changes in maternal plasma TF and TFPI concentrations among patients with preterm PROM according to their placental lesions and the occurrence of vaginal bleeding during pregnancy
Placental histology was available in 82.11% (101/123) of patients with preterm PROM. Of those, 58.4% (59/101) had histologic chorioamnionitis of maternal response, and 48.5% (49/101) had histologic chorioamnionitis of fetal response (i.e. umbilical phlebitis, necrotizing funisitis). Persistent muscularization of the basal plate arteries was the most frequent vascular placental lesion (Table IV). The placental histologic findings were not associated with significant changes in the median maternal plasma concentrations of TF and TFPI.
Vaginal bleeding during pregnancy was documented in 21 preterm PROM patients. The median maternal plasma TFPI concentration was significantly lower in preterm PROM patients without vaginal bleeding than in women with normal pregnancies; conversely, no difference was observed in the median maternal plasma TFPI concentration between patients with preterm PROM and vaginal bleeding and those with normal pregnancies (Table V). In addition, no significant differences were found in the median maternal plasma TF and TFPI concentrations in preterm PROM patients with and without vaginal bleeding during pregnancy [TF: median 412.6 pg/ml, range (256-2551) vs. median 369.5 pg/ml, range (3.3-1879.4), p=0.5, respectively; and TFPI: median 56.8 ng/ml, range (31.4-74.2) vs. median 58.7 pg/ml, range (26.3-116), p=0.6, respectively] (Table V).
Table V.
Maternal plasma concentrations of Tissue factor and Tissue factor pathway inhibitor in patients with preterm PROM with and without vaginal bleeding during pregnancy in comparison to women with normal pregnancy
| Preterm PROM without vaginal bleeding (n=100) |
Preterm PROM with vaginal bleeding (n=21) |
p value | Normal pregnancy (n=86) |
p value‡ | |
|---|---|---|---|---|---|
| Tissue factor (pg/mL)† |
369.5* (3.3-1879.4) |
412.6* (256-2551) |
0.5 | 291.5 (6.3-2662.2) |
0.003 |
| Tissue factor pathway inhibitor (ng/mL) |
58.7* (26.3-116) |
56.8 (31.4-74.2) |
0.6 | 66.1 (14.3-86.5) |
0.049 |
Data presented as median (range)
IAI: intra-amniotic infection/inflammation
PROM: prelabor rupture of membranes
p<0.05 in comparison to normal pregnancy
normal pregnancy- (n= 79)
Kruskal Wallis test
COMMENTS
Principal findings of the study
1) Women with preterm PROM have significantly higher median plasma TF concentrations than those with normal pregnancies; 2) the median plasma TFPI concentration was significantly lower in patients with preterm PROM than those with normal pregnancies; 3) there were no significant differences in maternal plasma TF or TFPI concentrations in patients with preterm PROM with or without intra-amniotic infection/inflammation; and 4) no significant correlation was observed between maternal plasma TF or TFPI concentrations and gestational age at time of blood collection.
What are the changes in TF during pregnancy?
Tissue factor is essential for the maintenance of pregnancy and about 90% of TF null mice embryo die at embryonic day 10.5 [46-49] due to abnormalities in yolk sack vasculature [46]. In humans, a substantial increase in decidual and myometrial TF expression and concentrations was reported during the luteal phase of the menstrual cycle [15,16,50,51], as well as during early and late stages of pregnancy [15,16,50-52]. Similarly, high TF concentrations have been detected in the fetal membranes (mainly the amnion) and amniotic fluid [23,53-55]. In contrast, the maternal plasma TF concentrations do not change significantly during normal pregnancy in comparison to non-pregnant women [56,57], though women in labor at term have significantly higher maternal plasma TF concentrations than non-pregnant women [23]. Of interest, TF expression on monocytes is decreased throughout pregnancy, but returns to the normal state by the third day post-partum [58,59].
Why does TF increase in patients with preterm PROM?
Our observation that women with preterm PROM have a significantly higher median maternal plasma concentration of TF is novel. Possible sources for the elevated TF in the maternal plasma could be from decidual activation that is prominent among patients with preterm PROM, and from monocyte activation that is associated with the moderate systemic maternal inflammatory state reported in these patients [8]. Both may lead to increased activation of coagulation cascade and higher thrombin generation that can propagate the rupture of membrane through MMP activation[10,11,60]
Tissue factor and activation of coagulation cascade
The higher median maternal plasma concentration of TAT complexes [3,4] along with the higher rate of placental aggregated vascular lesions (atherosis, fibrinoid necrosis of decidual vessels, decidual vessels thrombosis and fetal thrombotic vasculopathy) [1,2,61] observed in patients with preterm PROM support the suggested increased activation of the coagulation cascade and thrombin generation in these patients.
It has been proposed that a high expression of TF by the decidua and myometrium during normal pregnancy is needed for tight hemostatic control that may prevent decidual bleeding during blastocyst implantation and trophoblast invasion at the early stages of pregnancy, as well as to sustain an adequate uterine hemostasis during the postpartum period[17,18]. Indeed, an increased decidual expression of TF (mRNA and protein) is reported already during the luteal phase of the menstrual cycle and later during pregnancy [62]. Moreover, preterm PROM is associated with an increased activation of the decidual component of the common pathway of parturition[63]. Thus, in pregnancies complicated by abnormal placentation or intrauterine infection, decidual bleeding may lead to a higher expression of TF and activation of the coagulation cascade, resulting in increased thrombin generation. The latter has uterotonic properties that may generate uterine contractions that could initiate labor[12-14]. Moreover, thrombin can mediate the activation of MMP-1 [11], MMP-3 [10], and MMP-9 [60] that can digest components of the extracellular matrix, weaken the choriamniotic membranes and predispose to preterm PROM.
Tissue factor and increased maternal intravascular inflammatory response
The mechanisms described above are localized to the maternal-fetal interface. The lack of association between median maternal plasma TF concentrations and the presence of intra-amniotic infection/inflammation or vaginal bleeding in patients with preterm PROM suggest that the systemic maternal inflammatory response during preterm PROM[8] may contribute the increase median maternal plasma TF concentration in these patients regardless to the presence of infection or inflammation in the amniotic cavity or the occurrence of vaginal bleeding.
The interaction between the coagulation cascade and inflammation is well established [64-66]. Patients with chronic and acute inflammation or infection (i.e. chronic and acute pancreatitis [67,68] non-crescentic glumerolonephritis [69], and meningococcal sepsis [70]) have higher plasma TF concentrations than healthy controls. During preterm PROM, there is a moderate maternal systemic inflammation that results in monocyte and granulocyte activation [8]. Activated monocytes express TF on their membrane [71-75] and shed micro-particles containing TF into the plasma [71]. In addition, the lack of association between intra-amniotic infection/inflammation, as well as the placental histologic findings and median maternal plasma concentrations of TF and TFPI, suggest that the procoagulant changes observed in patients with preterm PROM may be due to a systemic rather than a local (i.e. placental, intrauterine) inflammatory process.
The procoagulant activity of immunoreactive TF in the maternal plasma (blood born TF) is a topic of debate [71,72,76-79]. In a recent in-vitro study, blood-born TF had very little or no procoagulant activity [71]. Moreover, whole blood and plasma clot formation, after inhibition of the contact factor (factor XIIa), was obtained only by adding exogenous, active TF. Of note, only six fentomol of exogenous TF were sufficient for clot formation [71]. On the other hand, it has been proposed that blood-born TF does not initiate the coagulation cascade but rather propagates clot formation by attaching to activated platelets and further enhancing the coagulation process [76-79]. This might be the reason why the administration of anti-TF antibodies has an anti-thrombotic effect without causing severe bleeding; since these antibodies inhibit blood-born TF at concentrations below those needed for inhibiting its hemostatic effect [80]. Moreover, positive immunostaining of arterial thrombosis and atherosclerotic plaques for TF suggests that blood-born TF may participate in the propagation of atherosclerotic plaques and the generation of arterial thrombosis [80,81]. Further, higher concentrations of blood-born TF were predictive of cardiovascular mortality of patients with acute coronary syndrome [82,83]. Therefore, the higher blood-born TF concentration in patients with preterm PROM, compared to those with normal pregnancies, may result from the association between moderate maternal inflammation and an increased activation of the coagulation cascade, whether or not intra-amniotic infection or inflammation occurs.
What is tissue factor pathway inhibitor?
The main physiological inhibitor of the TF pathway of coagulation is tissue factor pathway inhibitor (TFPI). Two types of TFPI have been described: TFPI-1 and TFPI-2. TFPI-1 directly inhibits factor Xa through the Kunitz-2 domain [84], while the inhibition of the FVIIa/TF complex is performed by the Kunitz-1 domain in a factor Xa-dependent manner [20,85,86]. TFPI-1 is found in the maternal circulation, fetal blood, platelets, endothelial cells and other organs [24,25], and it is the major form of TFPI in the plasma of non-pregnant individuals [87,88].
TFPI-2, first isolated from human placenta as Placental Protein 5 (PP5) [32,33], is the major form of TFPI in the placenta [26-31], and it is expressed by the syncytiotrophoblast [35,36]. In the non-pregnant state, TFPI-2 is present mainly in the extracellular matrix and its plasma concentrations are very low [33-35]. Recombinant TFPI-2 inhibits trypsin and factor VIIa activity (in a dose dependant manner). High concentrations of TFPI-2 are needed for a weak inhibition of factor Xa [89]. Moreover, TFPI-2 does not affect thrombin activity [89]. The administration of heparin reduces the dose of TFPI-2 needed for factor VIIa inhibition, but it does not increase the inhibitory activity of TFPI-2 on factor Xa [89]. In addition to its anticoagulant activity, TFPI-2 has a localized inhibitory activity on serine protease (i.e. trypsin, plasmin, plasma kalikrein) [28,89-93], as well as the turnover of pro-MMP1 and pro-MMP3 to their active forms [94].
Heparin and low molecular weight heparins increase production and secretion of TFPI by the endothelial cells [95-100], leading to an increase in the plasma concentrations of both types of TFPI [95,97-112]. Heparin binds factor Xa and TFPI simultaneously, bringing them into proximity that enhances factor Xa inhibition by TFPI [20,85,113,114].
What are the changes in tissue factor pathway inhibitor during pregnancy?
During normal pregnancy, the maternal plasma concentration of TFPI-2 increases along gestation reaching a plateau at 36 weeks [33-37] and subsiding after delivery [38]. Twin pregnancies have higher median maternal plasma concentration of TFPI-2 than singleton pregnancies, but the rate of the increase in TFPI-2 during gestation is lower in twins than in singletons [37]. However, the mean maternal plasma concentrations of total TFPI have been reported to increase during the first half of pregnancy until 20 weeks of gestation and then remain relatively constant until term [22]. Conflicting data exists concerning the changes in maternal plasma concentrations during labor. While some authors described an increase in TFPI plasma concentrations in early stages of labor [87], others reported a decrease in the TFPI plasma concentrations during labor [23].
Decreased median TFPI plasma concentrations and low TFPI/TF ratio in patients with preterm PROM: an additional mechanism for increased thrombin generation?
The procoagulable state reported in preterm PROM may be, in part, due to reduced natural anticoagulant concentrations and not only derived from the higher concentrations of procoagulant proteases (i.e. thrombin). This is supported by the novel finding of this study, that patients with preterm PROM have a lower median total maternal plasma TFPI concentration than women with normal pregnancies. Similar association between low plasma concentrations of TFPI and procoagulant state have been reported in non-pregnant and pregnant women.
In non-pregnant patients
1) low TFPI concentrations are considered an independent risk factor for deep vein thrombosis[115]; 2) among patients undergoing IVF treatments, those who developed the procoagulable state of ovarian hyper-stimulation syndrome, have lower TFPI plasma concentrations than those who did not[116]; and 3) non-pregnant women with a history of recurrent pregnancy loss [117] and a higher rate of thrombophilic mutation, have lower plasma TFPI concentrations than non-pregnant healthy women.
During pregnancy
1) pregnant women with vascular complications of pregnancy (preeclampsia, eclampsia, placental abruption, fetal growth restriction, and fetal demise) have lower placental extract total TFPI concentrations and TFPI mRNA expression than those of women with normal pregnancies [43]; and 2) a different report demonstrated a lower placental immunoreactivity of TFPI-2 in patients with preeclampsia but not in patients with fetal growth restriction [118]. Collectively, our results suggest that lower concentrations of total TFPI may contribute to the maternal procoagulant state observed in patients with preterm PROM.
The finding of a significantly lower TFPI/TF ratio in patients with preterm PROM than in women with normal pregnancy is novel and represents the procoagulant state in the maternal plasma of patients with preterm PROM. Immunoreactive TFPI is 500 to 1000 times more abundant in the maternal plasma than TF [119]. Changes in this ratio have been observed in patients with disseminated intravascular coagulation (DIC) [119] and thrombotic thrombocytopenic purpura (TTP) [79]. Moreover, patients with DIC who had a poor outcome also had a higher TF/TFPI ratio [119], while patients with TTP had a significant increase in TFPI/TF ratio after treatment; the authors had proposed that this reflects an improvement in the hypercoagulable state associated with TTP [79]. Therefore, the ratio of TFPI/TF can serve as an additional marker for increase activation of coagulation cascade.
In conclusion, preterm PROM is associated with increased median maternal plasma TF and decreased TFPI concentrations. This may result from the moderate systemic inflammatory state associated with preterm PROM but also from activation of the coagulation cascade as reflected by the low TFPI/TF ratio. Moreover, we suggest that measurement of the ratio between TF and its inhibitor (TFPI) may be of benefit in the assessment of hypercoagulable states during pregnancy.
Acknowledgment
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
Reference List
- 1.Kim YM, Chaiworapongsa T, Gomez R, Bujold E, Yoon BH, Rotmensch S, Thaler HT, Romero R. Failure of physiologic transformation of the spiral arteries in the placental bed in preterm premature rupture of membranes. Am J Obstet Gynecol. 2002;187:1137–1142. doi: 10.1067/mob.2002.127720. [DOI] [PubMed] [Google Scholar]
- 2.Arias F, Victoria A, Cho K, Kraus F. Placental histology and clinical characteristics of patients with preterm premature rupture of membranes. Obstet.Gynecol. 1997;89:265–271. doi: 10.1016/S0029-7844(96)00451-6. [DOI] [PubMed] [Google Scholar]
- 3.Chaiworapongsa T, Espinoza J, Yoshimatsu J, Kim YM, Bujold E, Edwin S, Yoon BH, Romero R. Activation of coagulation system in preterm labor and preterm premature rupture of membranes. J.Matern.Fetal Neonatal Med. 2002;11:368–373. doi: 10.1080/jmf.11.6.368.373. [DOI] [PubMed] [Google Scholar]
- 4.Rosen T, Kuczynski E, O’Neill LM, Funai EF, Lockwood CJ. Plasma levels of thrombin-antithrombin complexes predict preterm premature rupture of the fetal membranes. J.Matern.Fetal Med. 2001;10:297–300. doi: 10.1080/714904361. [DOI] [PubMed] [Google Scholar]
- 5.Lockwood CJ, Toti P, Arcuri F, Paidas M, Buchwalder L, Krikun G, Schatz F. Mechanisms of abruption-induced premature rupture of the fetal membranes: thrombin-enhanced interleukin-8 expression in term decidua. Am J Pathol. 2005;167:1443–1449. doi: 10.1016/S0002-9440(10)61230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gomez R, Romero R, Nien JK, Medina L, Carstens M, Kim YM, Chaiworapongsa T, Espinoza J, Gonzalez R. Idiopathic vaginal bleeding during pregnancy as the only clinical manifestation of intrauterine infection. J Matern.Fetal Neonatal Med. 2005;18:31–37. doi: 10.1080/14767050500217863. [DOI] [PubMed] [Google Scholar]
- 7.Gomez R, Athayde N, Pacora P, Mazor M, Yoon BH, Romero R. Increased Thrombin in Intrauterine Inflammation. Am.J.Obstet.Gynecol. 1998;178:S62. [Google Scholar]
- 8.Gervasi MT, Chaiworapongsa T, Naccasha N, Pacora P, Berman S, Maymon E, Kim JC, Kim YM, Yoshimatsu J, Espinoza J, et al. Maternal intravascular inflammation in preterm premature rupture of membranes. J Matern.Fetal Neonatal Med. 2002;11:171–175. doi: 10.1080/jmf.11.3.171.175. [DOI] [PubMed] [Google Scholar]
- 9.Osterud B, Bjorklid E. Sources of tissue factor. Semin.Thromb.Hemost. 2006;32:11–23. doi: 10.1055/s-2006-933336. [DOI] [PubMed] [Google Scholar]
- 10.Mackenzie AP, Schatz F, Krikun G, Funai EF, Kadner S, Lockwood CJ. Mechanisms of abruption-induced premature rupture of the fetal membranes: Thrombin enhanced decidual matrix metalloproteinase-3 (stromelysin-1) expression. Am J Obstet Gynecol. 2004;191:1996–2001. doi: 10.1016/j.ajog.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Rosen T, Schatz F, Kuczynski E, Lam H, Koo AB, Lockwood CJ. Thrombin-enhanced matrix metalloproteinase-1 expression: a mechanism linking placental abruption with premature rupture of the membranes. J.Matern.Fetal Neonatal Med. 2002;11:11–17. doi: 10.1080/jmf.11.1.11.17. [DOI] [PubMed] [Google Scholar]
- 12.Elovitz MA, Ascher-Landsberg J, Saunders T, Phillippe M. The mechanisms underlying the stimulatory effects of thrombin on myometrial smooth muscle. Am.J.Obstet.Gynecol. 2000;183:674–681. doi: 10.1067/mob.2000.106751. [DOI] [PubMed] [Google Scholar]
- 13.Elovitz MA, Saunders T, Ascher-Landsberg J, Phillippe M. Effects of thrombin on myometrial contractions in vitro and in vivo. Am.J.Obstet.Gynecol. 2000;183:799–804. doi: 10.1067/mob.2000.108897. [DOI] [PubMed] [Google Scholar]
- 14.Elovitz MA, Baron J, Phillippe M. The role of thrombin in preterm parturition. Am.J.Obstet.Gynecol. 2001;185:1059–1063. doi: 10.1067/mob.2001.117638. [DOI] [PubMed] [Google Scholar]
- 15.Lockwood CJ, Krikun G, Schatz F. The decidua regulates hemostasis in human endometrium. Semin.Reprod.Endocrinol. 1999;17:45–51. doi: 10.1055/s-2007-1016211. [DOI] [PubMed] [Google Scholar]
- 16.Lockwood CJ, Krikun G, Schatz F. Decidual cell-expressed tissue factor maintains hemostasis in human endometrium. Ann.N.Y.Acad.Sci. 2001;943:77–88. doi: 10.1111/j.1749-6632.2001.tb03793.x. 77-88. [DOI] [PubMed] [Google Scholar]
- 17.Lockwood CJ, Schatz F. A biological model for the regulation of peri-implantational hemostasis and menstruation. J Soc.Gynecol Investig. 1996;3:159–165. [PubMed] [Google Scholar]
- 18.Hahn L. On fibrinolysis and coagulation during parturition and menstruation. Acta Obstet Gynecol Scand.Suppl. 1974;28:7–40. [PubMed] [Google Scholar]
- 19.Major CA, de VM, Lewis DF, Morgan MA. Preterm premature rupture of membranes and abruptio placentae: is there an association between these pregnancy complications? Am.J.Obstet.Gynecol. 1995;172:672–676. doi: 10.1016/0002-9378(95)90591-x. [DOI] [PubMed] [Google Scholar]
- 20.Broze GJ, Jr., Warren LA, Novotny WF, Higuchi DA, Girard JJ, Miletich JP. The lipoprotein-associated coagulation inhibitor that inhibits the factor VII-tissue factor complex also inhibits factor Xa: insight into its possible mechanism of action. Blood. 1988;71:335–343. [PubMed] [Google Scholar]
- 21.Laskowski M, Jr., Kato I. Protein inhibitors of proteinases. Ann Rev Biochem. 1980;49:593–626. doi: 10.1146/annurev.bi.49.070180.003113. [DOI] [PubMed] [Google Scholar]
- 22.Sarig G, Blumenfeld Z, Leiba R, Lanir N, Brenner B. Modulation of systemic hemostatic parameters by enoxaparin during gestation in women with thrombophilia and pregnancy loss. Thromb.Haemost. 2005;94:980–985. doi: 10.1160/TH05-03-0212. [DOI] [PubMed] [Google Scholar]
- 23.Uszynski M, Zekanowska E, Uszynski W, Kuczynski J. Tissue factor (TF) and tissue factor pathway inhibitor (TFPI) in amniotic fluid and blood plasma: implications for the mechanism of amniotic fluid embolism. Eur.J.Obstet.Gynecol.Reprod.Biol. 2001;95:163–166. doi: 10.1016/s0301-2115(00)00448-6. [DOI] [PubMed] [Google Scholar]
- 24.Tay SP, Cheong SK, Boo NY. Circulating tissue factor, tissue factor pathway inhibitor and D-dimer in umbilical cord blood of normal term neonates and adult plasma. Blood Coagul.Fibrinolysis. 2003;14:125–129. doi: 10.1097/00001721-200302000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Edstrom CS, Calhoun DA, Christensen RD. Expression of tissue factor pathway inhibitor in human fetal and placental tissues. Early Hum.Dev. 2000;59:77–84. doi: 10.1016/s0378-3782(00)00084-0. [DOI] [PubMed] [Google Scholar]
- 26.Hube F, Reverdiau P, Iochmann S, Trassard S, Thibault G, Gruel Y. Demonstration of a tissue factor pathway inhibitor 2 messenger RNA synthesis by pure villous cytotrophoblast cells isolated from term human placentas. Biol Reprod. 2003;68:1888–1894. doi: 10.1095/biolreprod.102.011858. [DOI] [PubMed] [Google Scholar]
- 27.Iino M, Foster DC, Kisiel W. Quantification and characterization of human endothelial cell-derived tissue factor pathway inhibitor-2. Arterioscler.Thromb.Vasc.Biol. 1998;18:40–46. doi: 10.1161/01.atv.18.1.40. [DOI] [PubMed] [Google Scholar]
- 28.Sprecher CA, Kisiel W, Mathewes S, Foster DC. Molecular cloning, expression, and partial characterization of a second human tissue-factor-pathway inhibitor. Proc.Natl.Acad.Sci.U.S.A. 1994;91:3353–3357. doi: 10.1073/pnas.91.8.3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Udagawa K, Miyagi Y, Hirahara F, Miyagi E, Nagashima Y, Minaguchi H, Misugi K, Yasumitsu H, Miyazaki K. Specific expression of PP5/TFPI2 mRNA by syncytiotrophoblasts in human placenta as revealed by in situ hybridization. Placenta. 1998;19:217–223. doi: 10.1016/s0143-4004(98)90011-x. [DOI] [PubMed] [Google Scholar]
- 30.Udagawa K, Yasumitsu H, Esaki M, Sawada H, Nagashima Y, Aoki I, Jin M, Miyagi E, Nakazawa T, Hirahara F, et al. Subcellular localization of PP5/TFPI-2 in human placenta: a possible role of PP5/TFPI-2 as an anti-coagulant on the surface of syncytiotrophoblasts. Placenta. 2002;23:145–153. doi: 10.1053/plac.2001.0774. [DOI] [PubMed] [Google Scholar]
- 31.Kamei S, Kazama Y, Kuijper JL, Foster DC, Kisiel W. Genomic structure and promoter activity of the human tissue factor pathway inhibitor-2 gene. Biochim.Biophys.Acta. 2001;1517:430–435. doi: 10.1016/s0167-4781(00)00298-0. [DOI] [PubMed] [Google Scholar]
- 32.Kisiel W, Sprecher CA, Foster DC. Evidence that a second human tissue factor pathway inhibitor (TFPI-2) and human placental protein 5 are equivalent. Blood. 1994;84:4384–4385. [PubMed] [Google Scholar]
- 33.Butzow R, Virtanen I, Seppala M, Narvanen O, Stenman UH, Ristimaki A, Bohn H. Monoclonal antibodies reacting with placental protein 5: use in radioimmunoassay, Western blot analysis, and immunohistochemistry. J Lab Clin.Med. 1988;111:249–256. [PubMed] [Google Scholar]
- 34.Chand HS, Foster DC, Kisiel W. Structure, function and biology of tissue factor pathway inhibitor-2. Thromb.Haemost. 2005;94:1122–1130. doi: 10.1160/TH05-07-0509. [DOI] [PubMed] [Google Scholar]
- 35.Seppala M, Wahlstrom T, Bohn H. Circulating levels and tissue localization of placental protein five (PP5) in pregnancy and trophoblastic disease: absence of PP5 expression in the malignant trophoblast. Int.J Cancer. 1979;24:6–10. doi: 10.1002/ijc.2910240103. [DOI] [PubMed] [Google Scholar]
- 36.Than GN, Bohn H, Szabo DG. Advances in pregnancy- related protein research. CRC Press; Boca Raton, FL: 1993. pp. 1–333. [Google Scholar]
- 37.Obiekwe BC, Chard T. Placental protein 5: circulating levels in twin pregnancy and some observations on the analysis of biochemical data from multiple pregnancy. Eur.J Obstet Gynecol Reprod.Biol. 1981;12:135–141. doi: 10.1016/0028-2243(81)90068-x. [DOI] [PubMed] [Google Scholar]
- 38.Obiekwe BC, Sooby J, Salem HT, Chard T. Placental protein 5: disappearance from the circulation after delivery. Eur.J Obstet Gynecol Reprod.Biol. 1982;13:1–5. doi: 10.1016/0028-2243(82)90031-4. [DOI] [PubMed] [Google Scholar]
- 39.Abdel Gader AM, Al-Mishari AA, Awadalla SA, Buyuomi NM, Khashoggi T, Al-Hakeem M. Total and free tissue factor pathway inhibitor in pregnancy hypertension. Int.J.Gynaecol.Obstet. 2006;95:248–253. doi: 10.1016/j.ijgo.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 40.Bellart J, Gilabert R, Angles A, Piera V, Miralles RM, Monasterio J, Cabero L. Tissue factor levels and high ratio of fibrinopeptide A:D-dimer as a measure of endothelial procoagulant disorder in pre-eclampsia. Br.J.Obstet.Gynaecol. 1999;106:594–597. doi: 10.1111/j.1471-0528.1999.tb08330.x. [DOI] [PubMed] [Google Scholar]
- 41.Schjetlein R, Abdelnoor M, Haugen G, Husby H, Sandset PM, Wisloff F. Hemostatic variables as independent predictors for fetal growth retardation in preeclampsia. Acta Obstet Gynecol Scand. 1999;78:191–197. [PubMed] [Google Scholar]
- 42.Di Paolo S, Volpe P, Grandaliano G, Stallone G, Schena A, Greco P, Resta L, Selvaggi L, Cincione R, Schena FP, et al. Increased placental expression of tissue factor is associated with abnormal uterine and umbilical Doppler waveforms in severe preeclampsia with fetal growth restriction. J Nephrol. 2003;16:650–657. [PubMed] [Google Scholar]
- 43.Aharon A, Lanir N, Drugan A, Brenner B. Placental TFPI is decreased in gestational vascular complications and can be restored by maternal enoxaparin treatment. J Thromb.Haemost. 2005;3:2355–2357. doi: 10.1111/j.1538-7836.2005.01564.x. [DOI] [PubMed] [Google Scholar]
- 44.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet.Gynecol. 1996;87:163–168. doi: 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- 45.Redline RW, Heller D, Keating S, Kingdom J. Placental diagnostic criteria and clinical correlation--a workshop report. Placenta. 2005;26(Suppl A):S114–S117. doi: 10.1016/j.placenta.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 46.Carmeliet P, Mackman N, Moons L, Luther T, Gressens P, Van V I, Demunck H, Kasper M, Breier G, Evrard P, et al. Role of tissue factor in embryonic blood vessel development. Nature. 1996;383:73–75. doi: 10.1038/383073a0. [DOI] [PubMed] [Google Scholar]
- 47.Erlich J, Parry GC, Fearns C, Muller M, Carmeliet P, Luther T, Mackman N. Tissue factor is required for uterine hemostasis and maintenance of the placental labyrinth during gestation. Proc.Natl.Acad.Sci.U.S.A. 1999;96:8138–8143. doi: 10.1073/pnas.96.14.8138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Toomey JR, Kratzer KE, Lasky NM, Stanton JJ, Broze GJ., Jr. Targeted disruption of the murine tissue factor gene results in embryonic lethality. Blood. 1996;88:1583–1587. [PubMed] [Google Scholar]
- 49.Bugge TH, Xiao Q, Kombrinck KW, Flick MJ, Holmback K, Danton MJ, Colbert MC, Witte DP, Fujikawa K, Davie EW, et al. Fatal embryonic bleeding events in mice lacking tissue factor, the cell-associated initiator of blood coagulation. Proc.Natl.Acad.Sci U.S.A. 1996;93:6258–6263. doi: 10.1073/pnas.93.13.6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lockwood CJ, Krikun G, Papp C, Toth-Pal E, Markiewicz L, Wang EY, Kerenyi T, Zhou X, Hausknecht V, Papp Z, et al. The role of progestationally regulated stromal cell tissue factor and type-1 plasminogen activator inhibitor (PAI-1) in endometrial hemostasis and menstruation. Ann.N.Y.Acad.Sci. 1994;734:57–79. doi: 10.1111/j.1749-6632.1994.tb21736.x. [DOI] [PubMed] [Google Scholar]
- 51.Lockwood CJ, Krikun G, Rahman M, Caze R, Buchwalder L, Schatz F. The role of decidualization in regulating endometrial hemostasis during the menstrual cycle, gestation, and in pathological states. Semin.Thromb.Hemost. 2007;33:111–117. doi: 10.1055/s-2006-958469. [DOI] [PubMed] [Google Scholar]
- 52.Kuczynski J, Uszynski W, Zekanowska E, Soszka T, Uszynski M. Tissue factor (TF) and tissue factor pathway inhibitor (TFPI) in the placenta and myometrium. Eur.J.Obstet.Gynecol.Reprod.Biol. 2002;105:15–19. doi: 10.1016/s0301-2115(02)00113-6. [DOI] [PubMed] [Google Scholar]
- 53.Creter D. Amnioplastin: new reagent for coagulation tests. Lancet. 1977;2:251. doi: 10.1016/s0140-6736(77)92871-9. [DOI] [PubMed] [Google Scholar]
- 54.Omsjo IH, Oian P, Maltau JM, Osterud B. Thromboplastin activity in amniotic fluid. Gynecol.Obstet.Invest. 1985;19:1–5. doi: 10.1159/000299000. [DOI] [PubMed] [Google Scholar]
- 55.Lockwood CJ, Bach R, Guha A, Zhou XD, Miller WA, Nemerson Y. Amniotic fluid contains tissue factor, a potent initiator of coagulation. Am.J.Obstet.Gynecol. 1991;165:1335–1341. doi: 10.1016/0002-9378(91)90363-v. [DOI] [PubMed] [Google Scholar]
- 56.Holmes VA, Wallace JM. Haemostasis in normal pregnancy: a balancing act? Biochem.Soc.Trans. 2005;33:428–432. doi: 10.1042/BST0330428. [DOI] [PubMed] [Google Scholar]
- 57.Bellart J, Gilabert R, Miralles RM, Monasterio J, Cabero L. Endothelial cell markers and fibrinopeptide A to D-dimer ratio as a measure of coagulation and fibrinolysis balance in normal pregnancy. Gynecol.Obstet.Invest. 1998;46:17–21. doi: 10.1159/000009989. [DOI] [PubMed] [Google Scholar]
- 58.Oian P, Omsjo I, Maltau JM, Osterud B. Increased sensitivity to thromboplastin synthesis in blood monocytes from pre-eclamptic patients. Br.J.Obstet.Gynaecol. 1985;92:511–517. doi: 10.1111/j.1471-0528.1985.tb01357.x. [DOI] [PubMed] [Google Scholar]
- 59.Holmes VA, Wallace JM, Gilmore WS, McFaul P, Alexander HD. Tissue factor expression on monocyte subpopulations during normal pregnancy. Thromb.Haemost. 2002;87:953–958. [PubMed] [Google Scholar]
- 60.Stephenson CD, Lockwood CJ, Ma Y, Guller S. Thrombin-dependent regulation of matrix metalloproteinase (MMP)-9 levels in human fetal membranes. J.Matern.Fetal Neonatal Med. 2005;18:17–22. doi: 10.1080/14767050500123632. [DOI] [PubMed] [Google Scholar]
- 61.Arias F, Rodriquez L, Rayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am.J.Obstet.Gynecol. 1993;168:585–591. doi: 10.1016/0002-9378(93)90499-9. [DOI] [PubMed] [Google Scholar]
- 62.Schatz F, Krikun G, Caze R, Rahman M, Lockwood CJ. Progestin-regulated expression of tissue factor in decidual cells: implications in endometrial hemostasis, menstruation and angiogenesis. Steroids. 2003;68:849–860. doi: 10.1016/s0039-128x(03)00139-9. [DOI] [PubMed] [Google Scholar]
- 63.Romero R, Goncalves LF, Chaiworapongsa T, Kusanovic JP, Espinoza J. Mechanisms of preterm labor and preterm premature rupture of the membranes. In: Kurjak A, Chervenak F, editors. Textbook of Perinatal Medicine. 2nd Edition Taylor and Francis; 2006. pp. 1379–1393. [Google Scholar]
- 64.Esmon CT. The interactions between inflammation and coagulation. Br.J.Haematol. 2005;131:417–430. doi: 10.1111/j.1365-2141.2005.05753.x. [DOI] [PubMed] [Google Scholar]
- 65.Levi M, van der Poll T. Two-way interactions between inflammation and coagulation. Trends Cardiovasc.Med. 2005;15:254–259. doi: 10.1016/j.tcm.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 66.Levi M, van der Poll T, ten Cate H. Tissue factor in infection and severe inflammation. Semin.Thromb.Hemost. 2006;32:33–39. doi: 10.1055/s-2006-933338. [DOI] [PubMed] [Google Scholar]
- 67.Haas SL, Jesnowski R, Steiner M, Hummel F, Ringel J, Burstein C, Nizze H, Liebe S, Lohr JM. Expression of tissue factor in pancreatic adenocarcinoma is associated with activation of coagulation. World J.Gastroenterol. 2006;12:4843–4849. doi: 10.3748/wjg.v12.i30.4843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sawa H, Ueda T, Takeyama Y, Yasuda T, Matsumura N, Nakajima T, Ajiki T, Fujino Y, Suzuki Y, Kuroda Y. Elevation of plasma tissue factor levels in patients with severe acute pancreatitis. J.Gastroenterol. 2006;41:575–581. doi: 10.1007/s00535-006-1806-1. [DOI] [PubMed] [Google Scholar]
- 69.Naumnik B, Borawski J, Chyczewski L, Pawlak K, Mysliwiec M. Tissue factor and its inhibitor in human non-crescentic glomerulonephritis--immunostaining vs plasma and urinary levels. Nephrol.Dial.Transplant. 2006;21:3450–3457. doi: 10.1093/ndt/gfl365. [DOI] [PubMed] [Google Scholar]
- 70.Roldan V, Marin F, Blann A. Soluble E-selectin, interleukin-6 and tissue factor in two cases of meningococcal septicaemia. Blood Coagul.Fibrinolysis. 2004;15:179–182. doi: 10.1097/00001721-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 71.Butenas S, Bouchard BA, Brummel-Ziedins KE, Parhami-Seren B, Mann KG. Tissue factor activity in whole blood. Blood. 2005;105:2764–2770. doi: 10.1182/blood-2004-09-3567. [DOI] [PubMed] [Google Scholar]
- 72.Osterud B. Cellular interactions in tissue factor expression by blood monocytes. Blood Coagul.Fibrinolysis. 1995;6(Suppl 1):S20–S25. [PubMed] [Google Scholar]
- 73.Rivers RP, Hathaway WE, Weston WL. The endotoxin-induced coagulant activity of human monocytes. Br.J.Haematol. 1975;30:311–316. doi: 10.1111/j.1365-2141.1975.tb00547.x. [DOI] [PubMed] [Google Scholar]
- 74.Bach RR, Moldow CF. Mechanism of tissue factor activation on HL-60 cells. Blood. 1997;89:3270–3276. [PubMed] [Google Scholar]
- 75.Egorina EM, Sovershaev MA, Bjorkoy G, Gruber FX, Olsen JO, Parhami-Seren B, Mann KG, Osterud B. Intracellular and surface distribution of monocyte tissue factor: application to intersubject variability. Arterioscler.Thromb.Vasc.Biol. 2005;25:1493–1498. doi: 10.1161/01.ATV.0000168413.29874.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Balasubramanian V, Grabowski E, Bini A, Nemerson Y. Platelets, circulating tissue factor, and fibrin colocalize in ex vivo thrombi: real-time fluorescence images of thrombus formation and propagation under defined flow conditions. Blood. 2002;100:2787–2792. doi: 10.1182/blood-2002-03-0902. [DOI] [PubMed] [Google Scholar]
- 77.Chou J, Mackman N, Merrill-Skoloff G, Pedersen B, Furie BC, Furie B. Hematopoietic cell-derived microparticle tissue factor contributes to fibrin formation during thrombus propagation. Blood. 2004;104:3190–3197. doi: 10.1182/blood-2004-03-0935. [DOI] [PubMed] [Google Scholar]
- 78.Balasubramanian V, Vele O, Nemerson Y. Local shear conditions and platelet aggregates regulate the incorporation and activity of circulating tissue factor in ex-vivo thrombi. Thromb.Haemost. 2002;88:822–826. [PubMed] [Google Scholar]
- 79.Kobayashi M, Wada H, Wakita Y, Shimura M, Nakase T, Hiyoyama K, Nagaya S, Minami N, Nakano T, Shiku H. Decreased plasma tissue factor pathway inhibitor levels in patients with thrombotic thrombocytopenic purpura. Thromb.Haemost. 1995;73:10–14. [PubMed] [Google Scholar]
- 80.Rauch U, Nemerson Y. Circulating tissue factor and thrombosis. Curr.Opin.Hematol. 2000;7:273–277. doi: 10.1097/00062752-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 81.Westmuckett AD, Lupu C, Goulding DA, Das S, Kakkar VV, Lupu F. In situ analysis of tissue factor-dependent thrombin generation in human atherosclerotic vessels. Thromb.Haemost. 2000;84:904–911. [PubMed] [Google Scholar]
- 82.Campo G, Valgimigli M, Ferraresi P, Malagutti P, Baroni M, Arcozzi C, Gemmati D, Percoco G, Parrinello G, Ferrari R, et al. Tissue factor and coagulation factor VII levels during acute myocardial infarction: association with genotype and adverse events. Arterioscler.Thromb.Vasc.Biol. 2006;26:2800–2806. doi: 10.1161/01.ATV.0000247249.82030.94. [DOI] [PubMed] [Google Scholar]
- 83.Morange PE, Blankenberg S, Alessi MC, Bickel C, Rupprecht HJ, Schnabel R, Lubos E, Munzel T, Peetz D, Nicaud V, et al. Prognostic value of plasma tissue factor and tissue factor pathway inhibitor for cardiovascular death in patients with coronary artery disease: the AtheroGene study. J Thromb.Haemost. 2007;5:475–482. doi: 10.1111/j.1538-7836.2007.02372.x. [DOI] [PubMed] [Google Scholar]
- 84.Girard TJ, Warren LA, Novotny WF, Likert KM, Brown SG, Miletich JP, Broze GJ., Jr. Functional significance of the Kunitz-type inhibitory domains of lipoprotein-associated coagulation inhibitor. Nature. 1989;338:518–520. doi: 10.1038/338518a0. [DOI] [PubMed] [Google Scholar]
- 85.Broze GJ, Jr., Girard TJ, Novotny WF. Regulation of coagulation by a multivalent Kunitz-type inhibitor. Biochemistry. 1990;29:7539–7546. doi: 10.1021/bi00485a001. [DOI] [PubMed] [Google Scholar]
- 86.Kaiser B, Hoppensteadt DA, Jeske W, Wun TC, Fareed J. Inhibitory effects of TFPI on thrombin and factor Xa generation in vitro--modulatory action of glycosaminoglycans. Thromb.Res. 1994;75:609–616. doi: 10.1016/0049-3848(94)90173-2. [DOI] [PubMed] [Google Scholar]
- 87.Novotny WF, Brown SG, Miletich JP, Rader DJ, Broze GJ., Jr. Plasma antigen levels of the lipoprotein-associated coagulation inhibitor in patient samples. Blood. 1991;78:387–393. [PubMed] [Google Scholar]
- 88.Butzow R, Alfthan H, Stenman UH, Suikkari AM, Bohn H, Seppala M. Immunofluorometric demonstration and quantification of placental protein 5 in the absence of pregnancy. Clin.Chem. 1988;34:1591–1593. [PubMed] [Google Scholar]
- 89.Petersen LC, Sprecher CA, Foster DC, Blumberg H, Hamamoto T, Kisiel W. Inhibitory properties of a novel human Kunitz-type protease inhibitor homologous to tissue factor pathway inhibitor. Biochemistry. 1996;35:266–272. doi: 10.1021/bi951501d. [DOI] [PubMed] [Google Scholar]
- 90.Rao CN, Peavey CL, Liu YY, Lapiere JC, Woodley DT. Partial characterization of matrix-associated serine protease inhibitors from human skin cells. J Invest Dermatol. 1995;104:379–383. doi: 10.1111/1523-1747.ep12665851. [DOI] [PubMed] [Google Scholar]
- 91.Rao CN, Liu YY, Peavey CL, Woodley DT. Novel extracellular matrix-associated serine proteinase inhibitors from human skin fibroblasts. Arch.Biochem.Biophys. 1995;317:311–314. doi: 10.1006/abbi.1995.1168. [DOI] [PubMed] [Google Scholar]
- 92.Rao CN, Gomez DE, Woodley DT, Thorgeirsson UP. Partial characterization of novel serine proteinase inhibitors from human umbilical vein endothelial cells. Arch.Biochem.Biophys. 1995;319:55–62. doi: 10.1006/abbi.1995.1266. [DOI] [PubMed] [Google Scholar]
- 93.Rao CN, Reddy P, Liu Y, O’Toole E, Reeder D, Foster DC, Kisiel W, Woodley DT. Extracellular matrix-associated serine protease inhibitors (Mr 33,000, 31,000, and 27,000) are single-gene products with differential glycosylation: cDNA cloning of the 33-kDa inhibitor reveals its identity to tissue factor pathway inhibitor-2. Arch.Biochem.Biophys. 1996;335:82–92. doi: 10.1006/abbi.1996.0484. [DOI] [PubMed] [Google Scholar]
- 94.Rao CN, Mohanam S, Puppala A, Rao JS. Regulation of ProMMP-1 and ProMMP-3 activation by tissue factor pathway inhibitor-2/matrix-associated serine protease inhibitor. Biochem.Biophys.Res.Commun. 1999;255:94–98. doi: 10.1006/bbrc.1999.0153. [DOI] [PubMed] [Google Scholar]
- 95.Li Y, Rodriquez M, Spencer FA, Becker RC. Comparative effects of unfractionated heparin and low molecular weight heparin on vascular endothelial cell tissue factor pathway inhibitor release: a model for assessing intrinsic thromboresistance. J Thromb.Thrombolysis. 2002;14:123–129. doi: 10.1023/a:1023280811804. [DOI] [PubMed] [Google Scholar]
- 96.Hansen JB, Svensson B, Olsen R, Ezban M, Osterud B, Paulssen RH. Heparin induces synthesis and secretion of tissue factor pathway inhibitor from endothelial cells in vitro. Thromb.Haemost. 2000;83:937–943. [PubMed] [Google Scholar]
- 97.Menabawey M, Silman R, Rice A, Chard T. Dramatic increase of placental protein 5 levels following injection of small doses of heparin. Br.J Obstet Gynaecol. 1985;92:207–210. doi: 10.1111/j.1471-0528.1985.tb01083.x. [DOI] [PubMed] [Google Scholar]
- 98.Meisser A, Bischof P, Bohn H. Placental protein 5 (PP5) inhibits thrombin-induced coagulation of fibrinogen. Arch.Gynecol. 1985;236:197–201. doi: 10.1007/BF02133936. [DOI] [PubMed] [Google Scholar]
- 99.Nisbet AD, Brenner RD, Horne CH, Bohn H. Placental protein 5 (PP5) in pregnancy and malignant disease: the influence of heparin binding. Clin.Chim.Acta. 1982;119:21–29. doi: 10.1016/0009-8981(82)90401-6. [DOI] [PubMed] [Google Scholar]
- 100.Jones GR, Davey MW, Sinosich M, Grudzinskas JG. Specific interaction between placental protein 5 and heparin. Clin.Chim.Acta. 1981;110:65–70. doi: 10.1016/0009-8981(81)90301-6. [DOI] [PubMed] [Google Scholar]
- 101.Jeske W, Fareed J. Pharmacodynamic considerations in the selection of dosage of tinzaparin for various indications: experimental studies in primates. Semin.Thromb.Hemost. 2004;30(Suppl 1):41–47. doi: 10.1055/s-2004-823002. [DOI] [PubMed] [Google Scholar]
- 102.Kemme MJ, Burggraaf J, Schoemaker RC, Kluft C, Cohen AF. Quantification of heparin-induced TFPI release: a maximum release at low heparin dose. Br.J Clin.Pharmacol. 2002;54:627–634. doi: 10.1046/j.1365-2125.2002.t01-1-01705.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kaiser B, Hoppensteadt DA, Fareed J. Tissue factor pathway inhibitor: an update of potential implications in the treatment of cardiovascular disorders. Expert.Opin.Investig.Drugs. 2001;10:1925–1935. doi: 10.1517/13543784.10.11.1925. [DOI] [PubMed] [Google Scholar]
- 104.Sandset PM, Bendz B, Hansen JB. Physiological function of tissue factor pathway inhibitor and interaction with heparins. Haemostasis. 2000;30(Suppl 2):48–56. doi: 10.1159/000054163. [DOI] [PubMed] [Google Scholar]
- 105.Kaiser B, Glusa E, Hoppensteadt DA, Breddin HK, Amiral J, Fareed J. A supersulfated low-molecular-weight heparin (IK-SSH) increases plasma levels of free and total tissue factor pathway inhibitor after intravenous and subcutaneous administration in humans. Blood Coagul.Fibrinolysis. 1998;9:517–523. doi: 10.1097/00001721-199809000-00009. [DOI] [PubMed] [Google Scholar]
- 106.Hansen JB, Sandset PM, Huseby KR, Huseby NE, Bendz B, Ostergaard P, Nordoy A. Differential effect of unfractionated heparin and low molecular weight heparin on intravascular tissue factor pathway inhibitor: evidence for a difference in antithrombotic action. Br.J Haematol. 1998;101:638–646. doi: 10.1046/j.1365-2141.1998.00770.x. [DOI] [PubMed] [Google Scholar]
- 107.Jeske W, Hoppensteadt D, Klauser R, Kammereit A, Eckenberger P, Haas S, Wyld P, Fareed J. Effect of repeated Aprosulate and Enoxaparin administration on tissue factor pathway inhibitor antigen levels. Blood Coagul.Fibrinolysis. 1995;6:119–124. doi: 10.1097/00001721-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 108.Jesty J, Wun TC, Lorenz A. Kinetics of the inhibition of factor Xa and the tissue factor-factor VIIa complex by the tissue factor pathway inhibitor in the presence and absence of heparin. Biochemistry. 1994;33:12686–12694. doi: 10.1021/bi00208a020. [DOI] [PubMed] [Google Scholar]
- 109.Huang ZF, Wun TC, Broze GJ., Jr. Kinetics of factor Xa inhibition by tissue factor pathway inhibitor. J Biol.Chem. 1993;268:26950–26955. [PubMed] [Google Scholar]
- 110.Ostergaard P, Nordfang O, Petersen LC, Valentin S, Kristensen H. Is tissue factor pathway inhibitor involved in the antithrombotic effect of heparins? Biochemical considerations. Haemostasis. 1993;23(Suppl 1):107–111. doi: 10.1159/000216919. [DOI] [PubMed] [Google Scholar]
- 111.Wun TC. Lipoprotein-associated coagulation inhibitor (LACI) is a cofactor for heparin: synergistic anticoagulant action between LACI and sulfated polysaccharides. Blood. 1992;79:430–438. [PubMed] [Google Scholar]
- 112.Lindahl AK, Abildgaard U, Larsen ML, Aamodt LM, Nordfang O, Beck TC. Extrinsic pathway inhibitor (EPI) and the post-heparin anticoagulant effect in tissue thromboplastin induced coagulation. Thromb.Res.Suppl. 1991;14:39–48. doi: 10.1016/0049-3848(91)90402-i. 39-48. [DOI] [PubMed] [Google Scholar]
- 113.Wesselschmidt R, Likert K, Huang Z, MacPhail L, Broze GJ., Jr. Structural requirements for tissue factor pathway inhibitor interactions with factor Xa and heparin. Blood Coagul.Fibrinolysis. 1993;4:661–669. [PubMed] [Google Scholar]
- 114.Broze GJ., Jr. Tissue factor pathway inhibitor and the revised theory of coagulation. Annu.Rev.Med. 1995;46:103–12. doi: 10.1146/annurev.med.46.1.103. 103-112. [DOI] [PubMed] [Google Scholar]
- 115.Dahm A, Van H, Bendz B, Rosendaal F, Bertina RM, Sandset PM. Low levels of tissue factor pathway inhibitor (TFPI) increase the risk of venous thrombosis. Blood. 2003;101:4387–4392. doi: 10.1182/blood-2002-10-3188. V. [DOI] [PubMed] [Google Scholar]
- 116.Rogolino A, Coccia ME, Fedi S, Gori AM, Cellai AP, Scarselli GF, Prisco D, Abbate R. Hypercoagulability, high tissue factor and low tissue factor pathway inhibitor levels in severe ovarian hyperstimulation syndrome: possible association with clinical outcome. Blood Coagul.Fibrinolysis. 2003;14:277–282. doi: 10.1097/01.mbc.0000061296.28953.d0. [DOI] [PubMed] [Google Scholar]
- 117.Gardiner C, Cohen H, Austin SK, Machin SJ, Mackie IJ. Pregnancy loss, tissue factor pathway inhibitor deficiency and resistance to activated protein C. J.Thromb.Haemost. 2006;4:2724–2726. doi: 10.1111/j.1538-7836.2006.02197.x. [DOI] [PubMed] [Google Scholar]
- 118.Ogawa M, Yanoma S, Nagashima Y, Okamoto N, Ishikawa H, Haruki A, Miyagi E, Takahashi T, Hirahara F, Miyagi Y. Paradoxical discrepancy between the serum level and the placental intensity of PP5/TFPI-2 in preeclampsia and/or intrauterine growth restriction: possible interaction and correlation with glypican-3 hold the key. Placenta. 2007;28:224–232. doi: 10.1016/j.placenta.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 119.Shimura M, Wada H, Wakita Y, Nakase T, Hiyoyama K, Nagaya S, Mori Y, Shiku H. Plasma tissue factor and tissue factor pathway inhibitor levels in patients with disseminated intravascular coagulation. Am J Hematol. 1997;55:169–174. doi: 10.1002/(sici)1096-8652(199707)55:4<169::aid-ajh1>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]