Abstract
Alcohol consumption causes injury in a dose-response manner. The most common mode of sustaining an alcohol-attributable injury is from a single occasion of acute alcohol consumption, but much of the injury literature employs usual consumption habits to assess risk instead. An analysis of the acute dose-response relationship between alcohol and injury is warranted to generate single occasion- and dose-specific relative risks. A systematic literature review and meta-analysis was conducted to fill this gap. Linear and best-fit first-order model were used to model the data. Usual tests of heterogeneity and publication bias were run. Separate meta-analyses were run for motor vehicle and non motor vehicle injuries, as well as case-control and case-crossover studies. The risk of injury increases non-linearly with increasing alcohol consumption. For motor vehicle accidents, the odds ratio increases by 1.24 (95% CI: 1.18–1.31) per 10-gram in pure alcohol increase to 52.0 (95% CI: 34.50 – 78.28) at 120 grams. For non-motor vehicle injury, the OR increases by 1.30 (95% CI: 1.26–1.34) to an OR of 24.2 at 140 grams (95% CI: 16.2 – 36.2). Case-crossover studies of non-MVA injury result in overall higher risks than case-control studies and the per-drink increase in odds of injury was highest for intentional injury, at 1.38 (95% CI: 1.22 – 1.55). Efforts to reduce drinking both on an individual level and a population level are important. No level of consumption is safe when driving and less than 2 drinks per occasion should be encouraged to reduce the risk of injury.
Keywords: alcohol, injury, epidemiology, risk, meta-analysis
1. Introduction
There is little doubt that alcohol consumption causes injury (Rehm et al. 2003). Although the risk of alcohol-attributable injury from motor vehicle accidents (MVA) is the most visible connection in the research literature and popular media, a large body of work has shown that alcohol consumption is broadly associated with the risk of both intentional and unintentional injury in cross-sectional (Watt et al., 2005; Vingilis et al., 2007; Goodman et al., 1991; Malmivaara et al., 1993; Ivers et al., 2006), case-crossover (Borges et al., 2006; Vinson et al., 2003), and case-control analyses (Peck et al., 2008; Smith et al., 2001). The most common mode of sustaining an alcohol-attributable injury is from a single occasion of acute alcohol consumption, most commonly leading to intoxication and/or drunkenness and thus impairment. Recent work has shown that engaging in such occasions of acute consumption repeatedly results in high cumulative risks of injury over the life course (Taylor et al., 2008; Rehm et al., 2008). In previous work, measures of association have tended to show linear, dose-response relationships with risk compared to zero alcohol consumption (Borges et al., 2006; Kuendig et al., 2008; Li et al., 2001; Stockwell et al., 2002). What’s more, these general relationships have persisted throughout the last 40–50 years of research (Borkenstein et al., 1964; Anda et al., 1988), across countries and cultural boundaries (Cherpitel et al., 2006; Lin et al., 2003; Fabbri et al., 2001; Kasantikul et al., 2005) and without major distinctions by age or gender (Corrao et al., 1999), although absolute values of risk tend to be higher for young males involved in fatal motor-vehicle crashes (Zador et al., 2000). Overall, the disease burden attributable to alcohol consumption is high, particularly with respect to premature death and disability (Rehm et al., 2009)
There are two particular problem areas in the literature of alcohol and injury. The first is varying and/or unusable exposure measurements and the second is the inclusion of lab-based studies to generate risk estimates. In the first case, injury risks have tended to be based on two drinking models – usual consumption patterns or acute exposure. Information on usual consumption patterns does not capture the influence of alcohol on a particular episode of injury. It does not give information on whether alcohol was even consumed nor at what level prior to a specific injury event. For acute exposure measures, even though we can be certain the alcohol consumption occurred prior to the injury, many studies only report a dichotomous (YES/NO) measure of alcohol consumption. This precludes the construction of dose-response curves that have been informative in other areas of alcohol epidemiology, even though we are certain that risk increases with number of drinks consumed. Tightly controlled lab-based studies do exist and provide dose-response risk curves, but this is also problematic since tightly controlled situations may not represent real world scenarios. Thus, case-control and case-crossover in emergency room settings represent the best available evidence for measuring the real association between acute alcohol consumption and injury outcomes. The only previous meta-analysis for injury and alcohol consumption is Corrao et al. (1999), but this study suffered from the same problem in exposure definition by only presenting risk estimates as a function of usual consumption (Corrao et al., 1999).
This systematic review and meta-analysis thus aims to fill two gaps in this research at once– (1) to calculate a dose-response curve between alcohol and injury (2) by using only high-quality, real world epidemiological studies. Specifically, it will systematically seek out and locate those articles that present risk estimates of injury by specific alcohol consumption categories during the 6 hours immediately preceding the injury or report the blood alcohol level at the time of presentation/reporting of the injury. This will enable this analysis to pool acute alcohol dose-response data to capture an overall estimate of drinking during the period immediately before the outcome, and thus try to capture the true, real-world risk more accurately.
2. Methods
This study was completed in three main phases: the systematic review, data abstraction, and the meta-analysis.
2.1. Case Definition
The definition of injury was relatively broad in the sense that no strict adherence to ICD codes or strict diagnostic criteria was followed, since some studies only used qualitative descriptions of injury (e.g. “hit”, “cut”, “fall” etc.) and others used the more traditional ICD-9 or ICD-10-based definitions. Most studies were either emergency room studies (e.g. Borges et al. 2006) in which the patient presented with an injury, was admitted and recruited, or were MVA studies based on accident data, (e.g. (Krüger and Vollrath 2004)).
2.2. Systematic Review
A systematic review of the literature published between 1 January, 1980 and 21 November, 2008 was completed. Databases queried were Medline, EMBASE, CINAHL, PubMED, CABS (BIDS), WHOKIST, SIGLE, ETOH, Alcohol in Moderation (Alcohol Industry Database), and Web of Science using a pre-defined key word algorithm. Initially, the search used the bare minimum in search criteria in order to cast the widest net (and therefore the most conservative strategy) to identify articles. It combined the search terms “alcohol” AND “case control” OR “case crossover” AND “risk” AND “injury” OR specific outcomes: “motor vehicle accidents”, “poisonings”, “falls”, “suicide”, “homicide”, “drowning”, and was restricted to full articles (excluded reviews, editorials, and letters) of human studies only. This resulted in 323 articles, from which 182 were selected for closer inspection. For this analysis, only case-control or case-crossover articles were selected since these represent the best available evidence on alcohol-injury. Abstracts were selected from the total pool of identified citations and were excluded from further investigation if at least one of the following criteria were met:
No indication of any information pertaining to an association between alcohol and injury morbidity/mortality
The study was NOT a case-control or case-crossover
Inappropriate exposure data: No dose-response information presented (e.g., “yes” versus “no” alcohol consumption was unacceptable in this case)
The article did not have an appropriate endpoint measure (e.g. improper case definition)
Acute consumption was not presented e.g., average weekly consumption was used
In the event no abstract was available or existed, the full journal article was obtained and the abstract was reviewed and assessed for exclusion based on the same criteria. For non-English articles, a native speaker of the language in which the article was written completed the translation. For those abstracts selected for further investigation, the full article was obtained and judged based on the same five criteria. Only those articles NOT meeting any of the five exclusion criteria were selected for data abstraction. Full reference lists of selected articles and reviews were hand-searched to identify any studies that may have been missed in the systematic search.
2.3. Data abstraction
Information about the level of alcohol exposures in each study, the number of cases at each exposure level, the total population at risk at each exposure level, the adjusted estimates of relative risk (RR), and the corresponding upper and lower 95% confidence intervals of the adjusted RR were all recorded. When ranges of alcohol were given, the midpoint was taken. In cases where no upper bound for the highest category existed, 50% of the length of the previous category range was added to the low bound and this measure was used. In some cases, risks for increasing blood alcohol concentrations (BAC) were reported instead of consumption in grams of pure ethanol prior to the event. In these cases, BAC was converted to grams of consumption by using a modified Widmark formula (Brick 2006). The following formula was used, solving for the number of beverages consumed and then converting to grams of pure alcohol (taken from: http://www.cs.duke.edu/courses/fall05/cps001/labs/lab4.html, accessed November 24th, 2008):
Where:
0.01882816 = concentration of alcohol in blood (g/L)
concentration = alcohol by volume of the specific beverage type. For this analysis we assumed 40% (spirits), 12.5% (wine), 5% (beer).
weight_kg = weight in kilograms. For this analysis, average weights of men and women in different countries were based on published data and were country specific.
gender fraction = percentage of water in the human body: this was assumed to be 58% for men and 49% for women.
liver clearance rate = the rate at which liver metabolized alcohol per hour. This was assumed to be 0.017 per hour. All drinking was assumed to have taken place in the three hours prior to the BAC level being taken, corresponding to how many of the injury studies had measured alcohol consumption.
To convert the number of drinks to grams, we assumed different standard drink sizes for different countries in which the individual studies took place (US: 14g; Australia/New Zealand: 10g; Europe: 12g).
If the study did not include a measure of association but enough information existed for the reviewer to calculate an odds ratio (OR) or RR, this was done. If the study only reported combined (male + female) measures, the one measure was applied to both males and female datasets.
2.4. Meta-analysis
Step 1
Quantifying the heterogeneity of risk estimates across all studies was important given the diversity of study methods, effect sizes, and controlled variables (Thompson 1994). Heterogeneity was quantitatively assessed among studies by using both the Q statistic and the I2 statistic (Higgins and Thompson 2002). To assess publication bias, two independent tests were used - Begg’s and Egger’s regression asymmetry test for publication (Begg and Mazumdar 1994; Egger et al., 1997). This was done to investigate whether the existing literature was reflective of all studies, including negative or null associations, as well as those reporting positive associations and high risk estimates. If the studies were found to be highly heterogeneous and a large amount of between-study variation existed, it would be important to account for this variation by using a random effects model. If the opposite were true, a fixed effects model was justified (Field 2001; Field 2003). All analysis was completed using STATA software version 10.1 (Stata Corporation, College Station, TX).
Step 2
The meta-analysis step was the curve-generating step, using linear and first-order fractional polynomial regression of the inverse-variance weighted data to estimate a best fitting curve to the data according to Royston (Royston 2000). The first order fractional polynomials take the general form shown in Equation 1:
| (Equation 1) |
Where x is the alcohol exposure level (in grams per day, P1 is the polynomial power and β1 is the corresponding coefficient. No intercept term exists since all models have a start point of Log RR = 0 (RR = 1 at zero consumption). For first-order models, P1 takes values from −2 to +3. For model fitting, models were tested systematically from least to most complicated (linear, first order, second order) using the GLST command in STATA. Best-fit curves or lines were assessed using standard goodness-of-fit statistics, with an emphasis on decreased deviance (gain) compared to the quadratic model. Comparisons of curves to determine the best fit were made using a Chi-square distribution, as recommended by Royston and Altman (Royston and Altman 1994), using the linear (P = 1) as the referent for all first-order polynomials.
In addition to abstracting the number of cases, controls, sex, measures of association, and 95% confidence intervals, dummy variables for each study were created to differentiate between studies of general injury or motor-vehicle accidents (0 or 1, respectively), and case-crossover or case-control design (0 or 1, respectively).
3. Results
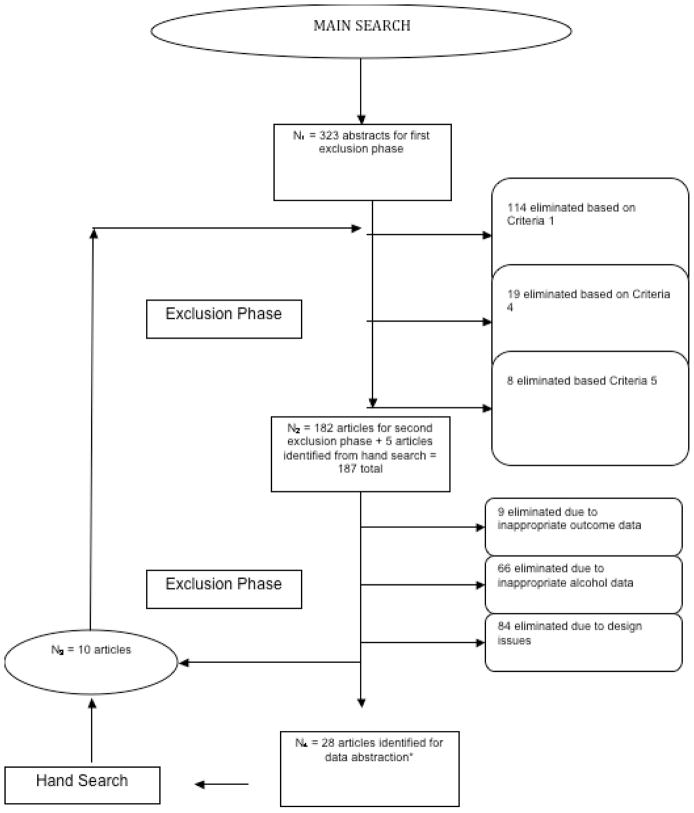
Figure 1 illustrates the search and article selection process, with numbers of articles retrieved and discarded at the abstract selection and the article selection phases.
Figure 1.
Results of the systematic review of the relationship between alcohol and injury.
3.1. Systematic Review
The systematic review identified 28 articles assessing the relationship between acute alcohol and injury. 9 of the articles presented multiple separate analyses and thus it was possible to present data from the same article on different groups. Overall, 39 datasets from the 28 articles were included in this meta-analysis (see Table 1). The search identified 14 datasets (8 articles) of MVA only (all case-control studies) and 25 datasets of other types of injury (23 articles). A total of 6 studies used a case-crossover design and all studies except for 3 investigated only injury morbidity as an outcome. Most studies reported combined estimates for males and females, so it was not possible for this study to separate gender effects either.
Table 1.
Description of studies selected for meta-analysis, with selected characteristics.
| Author | Year | Study Type | Data Type | Endpoint | N Cases | Covariates included* | Country |
|---|---|---|---|---|---|---|---|
| Haworth | case-control | Roadside testing | Both | 214 | 1, 2, 3, 4 | Australia | |
| (Honkanen et al., 1983) | 1983 | case-control | Emergency room | Morbidity | 278 | 1, 2, 3, 5, 6, 7, 8, 9, 10, 11 | Finland |
| (Olkkonen & Honkanen 1990) | 1990 | case-control | Emergency room | Morbidity | 140 | 3, 9, 12, 13 | Finland |
| (Borges et al., 1994) | 1994 | case-control | Emergency room | Morbidity | 274 | 1, 2, 3, 4, 5, 14, 15 | Mexico |
| (Hurst et al., 1994) | 1994 | case-control | Roadside testing | Morbidity | 4878 | -- | USA |
| (Vinson et al., 1995) | 1995 | case-crossover | Emergency room | Morbidity | 350 | 10, 14, 15, 17, 18 | USA |
| (Borges & Rosovsky 1996) | 1996 | case-control | Emergency room | Morbidity | 40 | 1, 2, 5, 6, 10, 14, 15 | Mexico |
| (Borges et al., 1998) | 1998 | case-control | Emergency room | Morbidity | 445 | 1, 2, 5, 6, 14, 15 | Mexico |
| (Cherpitel et al., 1999) | 1999 | case-control | Emergency room | Morbidity | 725 | 1, 2, 6, 14, 15, 18, 19, 28, 33 | Canada |
| (Li et al., 2001) | 2001 | case-control | Emergency room | Morbidity | 124 | 1, 2, 19 | USA |
| (Smith et al., 2001) | 2001 | case-control | Death record review/population controls | Mortality | 221 | 1, 2, 3, 4, 5, 19, 20, 21 | USA |
| (Stockwell et al., 2002) | 2002 | case-control | Population-based | Morbidity | 797 | 1, 2, 4, 6, 10, 14, 15, 19, 22, 23 | Australia |
| (Keall et al., 2004) | 2004 | case-control | Roadside testing | Mortality | 85 | 1, 2, 3, 24 | New Zealand |
| (Mura et al., 2003) | 2003 | case-control | Emergency room | Morbidity | 900 | -- | France |
| (Vinson et al., 2003a) | 2003 | case-control | Emergency room/population controls | Morbidity | 102 | 1, 6, 4, 14, 25 | Australia |
| (Connor et al., 2004) | 2004 | case-control | Emergency room | Morbidity | 571 | 1, 2, 3, 14, 26, 27 | New Zealand |
| (Krüger & Vollrath 2004) | 2004 | case-control | Roadside testing | Morbidity | 1451 | 1, 2, 3, 5, 24 | Germany |
| (Watt et al., 2004) | 2004 | case-control | Emergency room | Morbidity | 488 | 10, 15, 22, 24, 25, 28, 29, 30 | Australia |
| (Borges et al., 2004) | 2004 | case-crossover | Emergency room | Morbidity | 705 | 1, 2, 6, 22, 28, 31, 32 | Mexico |
| (Cherpitel et al., 2004) | 2004 | case-crossover | Emergency room | Morbidity | 218 | 2 | Poland |
| (Spurling & Vinson 2005) | 2005 | both | Emergency room/population controls | Morbidity | 2517 | 1, 2, 16, 32 | USA |
| (Borges et al., 2006) | 2006 | case-crossover | Emergency room | Morbidity | 4290 | -- | Argentina, Belarus, Brazil, Canada, China, Czech Republic, India, Mexico, Mozambique, New Zealand, South Africa, Sweden |
| (Borges et al., 2008b) | 2008b | case-crossover | Emergency room | Morbidity | 188 | -- | Argentina, Mexico, Brazil |
| (Borges et al., 2008a) | 2008a | case-crossover | Emergency room | Morbidity | 530 | 1, 2 | Argentina, Mexico, Brazil |
| (Kool et al., 2008) | 2008 | case-control | Hospital/Death record review | Morbidity | 335 | 1, 2, 15, 19, 22 | New Zealand |
| (Kuendig et al., 2008) | 2008 | case-control | Emergency room | Morbidity | 3682 | 1, 2, 28 | Switzerland |
| (Peck et al., 2008) | 2008 | case-control | Roadside testing | Morbidity | 3791 | 1, 2 | USA |
| (Gmel et al., 2008) | 2009 | case-crossover | Emergency room | Morbidity | 486 | 2 | Switzerland |
NOTE: 1: Age 2: Sex 3: Hour of day 4: Location 5: Day of week 6: Marital status 7: Road Conditions 8: Socioeconomic Status 9: Health condition 10: Drug use 11: Shoe type 12: Impaired vision 13: Hour of day 14: Education 15: Employment 16: Place of residence 17: Body weight 18: Weather conditions 19: Race 20: Driver/passenger 21: Vehicle type 22: Income 23: Drinking pattern 24: # of passengers/accompanying people 25: Health insurance coverage 26: Seatbelt use 27: Tiredness/fatigue 28: Usual alcohol use 29: Risk-taking behaviour 30: Risk perception 31: Cause/weapon used 32: Alcohol abuse 33: Previous ER visit
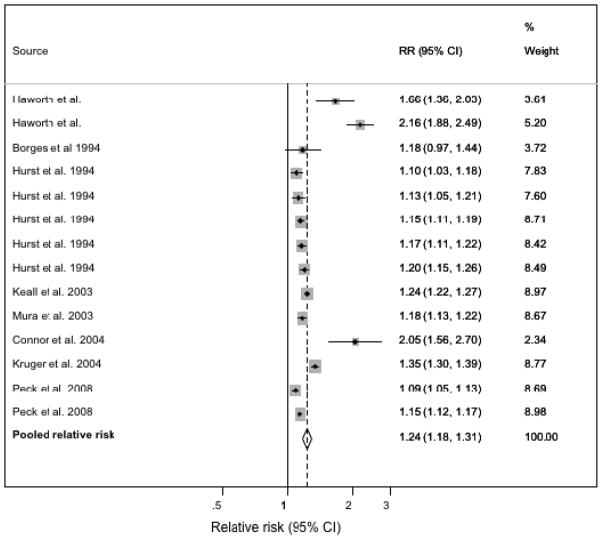
Figure 2 shows the results of the heterogeneity assessment for non-motor vehicle accidents, which indicated significant heterogeneity between these studies (Q-statistic = 136.74, df = 67 I2 = 51, p < 0.0001). The meta-analysis was run as a random effects model in order to account for this variability. Publication bias was detected by the Begg’s (p =0.023) and Egger’s (p = 0.004) tests, with scarcity seen at the bottom right of the funnel plot (not shown). The forest plot shows the relative contributions of each study to the pooled estimate, which shows the odds of a non-MVA injury increase by 1.30 (95% CI: 1.26–1.34) for every 10-gram increase in alcohol consumption.
Figure 2.
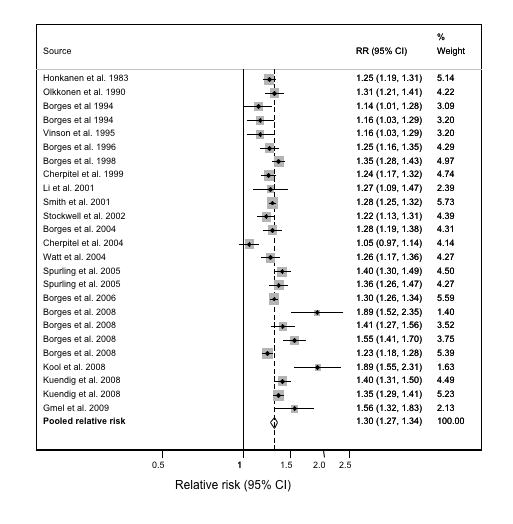
Forest plot for studies of non-motor vehicle accidents only and estimated relative risks associated with a 10 g/day increase in alcohol consumption: Estimates were derived from a random effects linear model.
Among non-motor vehicle accident studies, comparisons between case-control and case-crossover studies were made. This analysis (not shown) indicated that case-control studies presented lower overall risks than case-crossover studies (p = 0.02), reinforcing the substantial heterogeneity seen in this group of studies.
The results of the heterogeneity assessment studies reporting motor vehicle accidents are shown in Figure 3. A large degree of variation between study estimators was seen for this group of injuries as well (Q-statistic = 485.11 df = 43, I2 = 91, p < 0.0001), indicating that a random effects model would be appropriate for curve-fitting steps. No publication bias was detected by either the Begg’s test (p= 0.732) or the Egger’s test (p=0.494). The forest plot in Figure 3 shows the odds of an MVA injury increase by 1.24 (95% CI: 1.18–1.31) for every 10-gram increase in alcohol consumption.
Figure 3.
Forest plot for studies of motor vehicle accidents only and estimated relative risks associated with a 10 g/day increase in alcohol consumption: Estimates were derived from a random effects linear model.
3.2. Meta-analysis
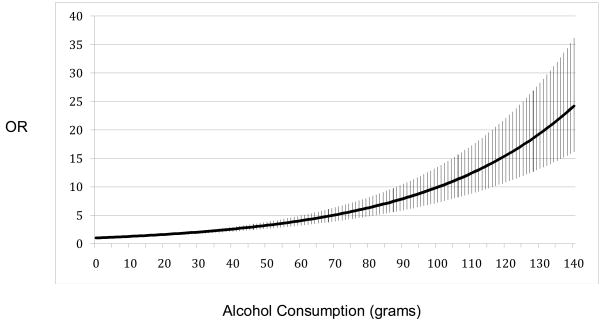
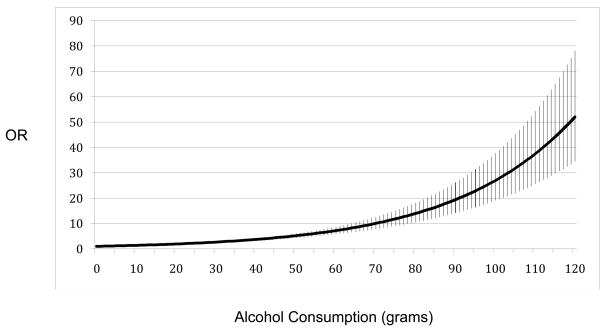
The results of the meta-analysis (Figures 4 and 5) showed a strong dose-response relationship of alcohol consumption and both MVA and non-MVA injury. Initially, the linear model for both MVA and non-MVA curves was fit to the pooled data, and then a first-order best-fit curve was attempted to try and improve the fit of the line to the data. For both MVA and non-MVA, the best-fit line was not the linear model but was P1 = 2 (squared) and P1 = 0.5 (square root), respectively.
Figure 4.
Dose-response curve for the amount of alcohol consumed 3 hours prior and the odds of non-motor vehicle accident injury.
Figure 5.
Dose-response curve for the amount of alcohol consumed 3 hours prior and the odds of motor vehicle accident injury.
At 140 grams of pure alcohol consumption prior to injury, a maximum odds ratio of 24.2 (95% CI: 16.2 – 36.2) for non-MVA injury was calculated. The curve for MVA went up much quicker, with an odds of about 52.0 (95% CI: 34.50 – 78.28) at 120 grams of alcohol consumed in the three hours prior. Even at generally accepted moderate doses (24 grams per day, or 2 standard drinks), the odds ratios for non-MVA and MVA injuries were 1.79 (1.59 – 2.00) and 2.20 (2.03 – 2.09), respectively.
A second analysis was run that separated out different injury types, with the stipulation that each injury-specific meta-analysis must have had at least 3 datasets included. This resulted in 4 distinct injury groups: violence (including one study on suicide), falls, MVA, and other unintentional injury. Identical meta-analyses were run on each of these injury subtypes and are shown in Table 2. Deviations from the non-MVA group were seen with falls, for which the data fit best to a linear line. The two unintentional injury categories (falls and other unintentional) had statistically similar pooled odds ratios, indicated by overlapping of confidence intervals. Intentional injury had the highest odds ratio point estimate of all injury categories and was significantly larger than the odds ratio of MVA, but not significantly different from the ratios for either falls or other unintentional injury. Separation of studies of falls and intentional injury from the non-MVA category resulted in a small decrease in heterogeneity of the other unintentional injury category, but the difference was non-significant (not shown).
Table 2.
Selected results of separate meta-analyses for specific injury types
| Injury Type | No. of studies * | Number of datasets | Best fit line | Increase in odds per 10-gram increase in consumption |
|---|---|---|---|---|
| Intentional Injury | 5 | 5 | non-linear | 1.38 (95% CI: 1.22 – 1.55) |
| Falls | 5 | 5 | linear | 1.25 (95% CI 1.14 – 1.36) |
| MVA | 8 | 14 | non-linear | 1.24 (95% CI: 1.18 – 1.31) |
| Other unintentional | 13 | 15 | non-linear | 1.32 (95% CI: 1.27 – 1.36) |
Note: 9 studies presented data on more than one injury category
4. Discussion
This is the first meta-analysis to quantify the overall relationship between episodic alcohol consumption and the risk of acute injury. It confirmed that the risk of injury rises monotonically with increasing alcohol consumption, consistent with previous individual studies. Comparison to the only other meta-analysis investigating alcohol and injury (Corrao et al., 1999) is difficult since that analysis used average daily consumption as the exposure measure and not acute drinking. The present study is the first meta-analysis to separate motor vehicle from non-motor vehicle crashes and also the first to separate case-control from case-crossover studies. Non-linear, positive relationships between alcohol consumption and the risk of injury were found for both MVA and non-MVA injuries, with non-MVA injuries having a greater proportional per-drink increase in risk, although confidence intervals overlapped slightly. As well, the risk profile for intentional injury was found to be higher than other types of injury when analysis by injury type was done, confirming previous, single studies (Cherpitel et al., 2005; Borges et al., 2004).
There are a number of limitations that provide context to the risk estimates provided in this article. Some of these are inherent to meta-analyses generally and some are specific to the alcohol-injury field. Of the former, the first is the value of pooled risk estimates when the heterogeneity between individual study risks is high (as in this analysis). Some have argued that if heterogeneity is found to be significant, the merit of the pooled estimate is lowered. However, tests of heterogeneity are generally underpowered and it is more important, and may be of more use, to identify the sources of heterogeneity through more thoughtful consideration rather than by the statistic alone (Thompson 1994; Ionnadis 2008).
In this and all meta-analyses, differences between single studies in additional independent variables, sample size, and statistical technique were apparent despite efforts to separate out injury types as much as possible. When this was done, the heterogeneity dropped significantly for each type of non-MVA crash, reinforcing the differences in risk estimates and methods between them and the need for this kind of separation in future. As well, including observation level data on confounding factors was not possible given the aggregate nature of the data and data-sharing policy. Among individual studies, experimental design differed mainly with variations between case-control and case-crossover designs. There are a number of differences in these study types that can affect heterogeneity, the most important of which is obviously the control group and the biases that result from this difference. In a case-crossover study, between-person confounding is well controlled compared to case-control studies, but recall biases still exist (Borges et al., 2006; Gmel and Daeppen 2007). Since the respondent is his own control, the differences in cases and controls do not lie between people, but rather within people, specifically, the time between case and control periods. The control period is farther away (e.g. the week previous) from the case interview and therefore self-reported alcohol consumption is more likely to be estimated or misreported by the respondent when interviewed at the case period (current time). It is important, as well, that investigations of single-occasion drinking and injury risk may be particularly susceptible to this type of recall bias - previous research has reported that 7-day recall bias is higher in sporadic drinkers than regular drinkers, the majority of whom are young men (Gmel et al., 2008), a group in which injury constitutes the highest alcohol-attributable mortality (Rehm et al., 2006). Analysis of this 7-day recall bias compared to 1 day prior found that respondents underestimated their consumption by almost 1 standard drink, meaning the injury risk estimates may be inflated in case-crossover studies using 7-day recall methods (Gmel and Daeppen 2007).
A second important source of uncertainty in this analysis may be a result of differences in how alcohol consumption is measured. Some studies used a breathalyzer or other blood-alcohol measures while others use self-reported drinking in the time preceding the injury. This creates the problem of determining the actual level of alcohol in the blood at the time of injury. The Widmark formulas used to estimate numbers of standard drinks from BAC measures require estimations of weight, time spent drinking, and liver clearance rates, all of which may combine to cause considerable uncertainty in consumption estimates and thus the OR/RR. The literature estimates the uncertainty (standard deviation) of Widmark methods between 1.2 and 2.1 drinks per 10 standard drinks (coefficient of variation: 12.3% to 21.2%; (Gullberg 2007). In addition, the correlation between objective and subjective measures is limited, showing a high degree of uncertainty in the measurement of exposure (e.g., (Sommers et al., 2000)). Many of the studies presented here used data from emergency room studies, which may not reflect all alcohol-attributable injuries, nor the general population. However, the relative risks for alcohol-attributable death are considerably higher than for morbidity (Rehm et al., 2004), so this study can be seen as a conservative estimate in this regard.
Lastly, previous work has shown that the relationship between alcohol and injury may be confounded by usual drinking patterns, risk-taking behaviour and substance use (Watt et al., 2004). Many of the studies included in this meta-analysis did not control for these factors, or only controlled just one or two of them. This means the overall pooled estimate may be biased with respect to these confounders. On the other side of this argument, though, is that explicitly controlling for some of these types of confounders may lead to biased risk estimates due to the fact that alcohol and risk-taking behaviour, for example, are on the causal path from alcohol consumption and injury. Decisions to engage in activities that are likely to lead to an injury are positively influenced to a large degree by the consumption of alcohol, so over-controlling by including these confounders would result in incorrect RR as well (Deery and Love 1996; Bazargan-Hejazi et al., 2007; Greenfield and Rogers 1999).
Future work in this field, particularly in the areas of what variables to control for and why, is necessary. Over-controlling for variables that are on the causal pathway biases risk estimates towards a null finding, which is dangerous in terms of public health policy and risk communication. Additionally, research in this field must strive to adopt standard exposure assessment tools. This is one of the most challenging aspects of this field, considering that study participants may provide unreliable information themselves either from fear of legal implications or social factors, and may not be examined for alcohol use until a significant amount of time has passed from the time of initial injury. Efforts to improve in these areas will result in making different studies more comparable and result in more reliable relative risks.
With consistent risk estimates comes responsibility to reduce well-established harms, and the alcohol-injury association is no different. Strategies to reduce binge drinking and injury should be high on the public agenda, and there are a number of policy measures that have prove to be effective in this area. These include policies that affect price, such as increased taxation, setting limits on alcohol retail outlet density and operating hours, raising the legal age of purchase of alcohol, and random, roadside breath testing of drivers (Babor et al., 2003).
5. Conclusion
The risk of injury increases non-linearly with increasing alcohol consumption, so efforts to reduce drinking both on an individual level and a population level are important. No level of consumption is safe and even for 2 standard drinks, the odds of injury are almost double for most types of injury. Obviously abstinence is related to the lowest risk, but policy measures such as taxation, raising legal drinking ages, and efforts to reduce acute alcohol consumption and associated injury, are to be encouraged and implemented given the high risks associated with acute alcohol consumption.
Contributor Information
B. Taylor, Center for Addiction and Mental Health, Toronto, Ontario Canada
H.M Irving, Center for Addiction and Mental Health, Toronto, Ontario Canada.
F. Kanteres, Center for Addiction and Mental Health, Toronto, Ontario Canada
R. Room, Turning Point Alcohol and Drug Centre, Victoria, Australia
G. Borges, National Institute of Psychiatry, Mexico, City
C.J. Cherpitel, Alcohol Research Group, Emeryvill, CA
J. Bond, Alcohol Research Group, Emeryvill, CA
T. Greenfield, Alcohol Research Group, Emeryvill, CA
J. Rehm, Center for Addiction and Mental Health, Toronto, Ontario Canada
Reference List
- Anda RF, Williamson DF, Remington PL. Alcohol and fatal injuries among US adults. Findings from the NHANES I Epidemiologic Follow-up Study. JAMA. 1988;260:2529–2532. [PubMed] [Google Scholar]
- Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube J, Gruenewald P, Hill L, Holder H, Homel R, Österberg E, Rehm J, Room R, Rossow I. Alcohol: No ordinary commodity. Research and public policy. Oxford University Press; Oxford and London: 2003. [Google Scholar]
- Bazargan-Hejazi S, Gaines T, Duan N, Cherpitel C. Correlates of injury among ED visits: effects of alcohol, risk perception, impulsivity, and sensation-seeking behaviours. Am J Drug Alcohol Abuse. 2007;33:101–108. doi: 10.1080/00952990601087455. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- Borges G, Cherpitel C, Macdonald S, Giesbrecht NA, Stockwell T, Wilcox HC. A case-crossover study of acute alcohol use and suicide attempt. J Stud Alcohol. 2004;65:708–714. doi: 10.15288/jsa.2004.65.708. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel C, Orozco R, Bond J, Ye Y, Macdonald S. Multicenter study of acute alcohol use and non-fatal injuries: Data from the WHO Collaborative Study on Alcohol and Injuries. Bull World Health Organ. 2006;84:453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkenstein R, Crowther R, Shumate R, Ziel W, Zylman R. The role of the drinking driver in traffic accidents. Department of Police Administration, Indiana University; Bloomington, Indiana: 1964. [Google Scholar]
- Brick J. Standardization of alcohol calculations in research. Alcohol Clin Exp Res. 2006;30:1276–1287. doi: 10.1111/j.1530-0277.2006.00155.x. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bond J, Ye Y, Borges G, Room R, Poznyak V, Hao W. Multi-level analysis of causal attribution of injury to alcohol and modifying effects: Data from two international emergency room projects. Drug Alcohol Depend. 2006;82:258–268. doi: 10.1016/j.drugalcdep.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Moskalewicz J, Switkiewicz G. Risk of injury: a case-crossover analysis of injured emergency service patients in Poland. Alcohol Clin Exp Res. 2005;29:2181–2187. doi: 10.1097/01.alc.0000191771.44999.a1. [DOI] [PubMed] [Google Scholar]
- Corrao G, Bagnardi V, Zambon A, Arico S. Exploring the dose-response relationship between alcohol consumption and the risk of several alcohol-related conditions: a meta-analysis. Addiction. 1999;94:1551–1573. doi: 10.1046/j.1360-0443.1999.9410155111.x. [DOI] [PubMed] [Google Scholar]
- Deery H, Love A. The effect of a moderate dose of alcohol on the traffic hazard perception profile of young drink-drivers. Addiction. 1996;91:815–827. doi: 10.1046/j.1360-0443.1996.9168158.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabbri A, Marchesini G, Morselli-Labate AM, Rossi F, Cicognani A, Dente M, Iervese T, Ruggeri S, Mengozzi U, Vandelli A. Blood alcohol concentration and management of road trauma patients in the emergency department. J Trauma. 2001;50:521–528. doi: 10.1097/00005373-200103000-00018. [DOI] [PubMed] [Google Scholar]
- Field AP. The problems in using fixed-effects models of meta-analysis on real-world data. Understanding Statistics. 2003;2:77–96. [Google Scholar]
- Field AP. Meta-analysis of correlation coefficients: A Monte Carlo comparison of fixed-and random-effects methods. Psychol Methods. 2001;6:161–180. doi: 10.1037/1082-989x.6.2.161. [DOI] [PubMed] [Google Scholar]
- Gmel G, Daeppen JB. Recall bias for 7-day recall measurement of alcohol consumption among emergency room patients. J Stud Alcohol Drugs. 2007;68:303–310. doi: 10.15288/jsad.2007.68.303. [DOI] [PubMed] [Google Scholar]
- Gmel G, Gaume J, Faouzi M, Kulling JP, Daeppen JB. Who drinks most of the total alcohol in young men -risky single occasion drinking as normative behaviour. Alcohol Alcohol. 2008;43:692–697. doi: 10.1093/alcalc/agn070. [DOI] [PubMed] [Google Scholar]
- Goodman RA, Istre GR, Jordan FB, Herndon JL, Kelaghan J. Alcohol and fatal injuries in Oklahoma. J Stud Alcohol. 1991;52:156–161. doi: 10.15288/jsa.1991.52.156. [DOI] [PubMed] [Google Scholar]
- Greenfield T, Rogers J. Alcoholic beverage choice, risk perception and self-reported drunk driving: effects of measurement on risk analysis. Addiction. 1999;94:1735–1743. doi: 10.1046/j.1360-0443.1999.9411173510.x. [DOI] [PubMed] [Google Scholar]
- Gullberg RG. Estimating the uncertainty associated with Widmark’s equation commonly applied in forensic toxicology. Forensic Sci Int. 2007;172:33–39. doi: 10.1016/j.forsciint.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Ionnadis JP. Interpretation of tests of heterogeneity and bias in meta-analysis. J Eval Clin Pract. 2008;14:951–957. doi: 10.1111/j.1365-2753.2008.00986.x. [DOI] [PubMed] [Google Scholar]
- Ivers RQ, Blows SJ, Stevenson MR, Norton RN, Williamson A, Eisenbruch M, Woodward M, Lam L, Palamara P, Wang J. A cohort study of 20,822 young drivers: the DRIVE study methods and population. Injury Prevention. 2006;12:385–389. doi: 10.1136/ip.2006.011825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasantikul V, Ouellet JV, Smith T, Sirathranont J, Panichabhongse V. The role of alcohol in Thailand motorcycle crashes. Accid Anal Prev. 2005;37:357–366. doi: 10.1016/j.aap.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Krüger HP, Vollrath M. The alcohol-related crash risk in Germany: procedure, methods and results. Accid Anal Prev. 2004;36:125–133. doi: 10.1016/s0001-4575(02)00134-3. [DOI] [PubMed] [Google Scholar]
- Kuendig H, Hasselberg M, Laflamme L, Daeppen JB, Gmel G. Alcohol and nonlethal injuries: a Swiss emergency department study on the risk relationship between acute alcohol consumption and type of injury. J Trauma. 2008;65:203–211. doi: 10.1097/TA.0b013e318068fc64. [DOI] [PubMed] [Google Scholar]
- Li G, Baker SP, Smialek JE. Use of alcohol as a risk factor for bicycling injury. JAMA. 2001;285:893–896. doi: 10.1001/jama.285.7.893. [DOI] [PubMed] [Google Scholar]
- Lin MR, Chang SH, Pai L, Keyl PM. A longitudinal study of risk factors for motorcycle crashes among junior college students in Taiwan. Accid Anal Prev. 2003;35:243–252. doi: 10.1016/s0001-4575(02)00002-7. [DOI] [PubMed] [Google Scholar]
- Malmivaara A, Heliovaara M, Knekt P, Reunanen A, Aromaa A. Risk factors for injurious falls leading to hospitalization or death in cohort of 19,500 adults. Am J Epidemiol. 1993;138:384–394. doi: 10.1093/oxfordjournals.aje.a116871. [DOI] [PubMed] [Google Scholar]
- Peck RC, Gebers MA, Voas RB, Romano E. The relationship between blood alcohol concentration (BAC) and crash risk. J Safety Res. 2008;39:311–319. doi: 10.1016/j.jsr.2008.02.030. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable toalcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos CT, Frick U, Jernigan D. Alcohol Use. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Vol. 1. WHO; Geneva: 2004. pp. 959–1109. [Google Scholar]
- Rehm J, Room R, Taylor B. Method for moderation: measuring lifetime risk of alcohol-attributable mortality as a basis for drinking guidelines. Int J Methods Psychiatr Res. 2008;17:141–151. doi: 10.1002/mpr.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Taylor B, Room R. Global burden of disease from alcohol, illicit drugs and tobacco. Drug Alcohol Rev. 2006;25:503–513. doi: 10.1080/09595230600944453. [DOI] [PubMed] [Google Scholar]
- Royston P. A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med. 2000;19:1831–1847. doi: 10.1002/1097-0258(20000730)19:14<1831::aid-sim502>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modeling. Applied Statistics. 1994;43:429–467. [Google Scholar]
- Smith GS, Keyl PM, Hadley JA, Bartley CL, Foss RD, Tolbert WG, McKnight J. Drinking and recreational boating fatalities: a population-based case-control study. JAMA. 2001;286:2974–2980. [PubMed] [Google Scholar]
- Sommers MS, Dyehouse JM, Howe SR, Lemmink J, Volz T, Manharth M. Validity of self-reported alcohol consumption in nondependent drinkers with unintentional injuries. Alcohol Clin Exp Res. 2000;24:1406–1413. [PubMed] [Google Scholar]
- Stockwell T, McLeod R, Stevens M, Philips M, Webb M, Jelinek G. Alcohol consumption, setting, gender and activity as predictors of injury: a population-based case-control study. J Stud Alcohol. 2002;63:372–379. doi: 10.15288/jsa.2002.63.372. [DOI] [PubMed] [Google Scholar]
- Taylor B, Rehm J, Room R, Patra J, Bondy S. Determination of lifetime injury mortality risk in Canada in 2002 by drinking amount per occasion and number of occasions. Am J Epidemiol. 2008;168:1119–1125. doi: 10.1093/aje/kwn215. [DOI] [PubMed] [Google Scholar]
- Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. BMJ. 1994;309:1351–1355. doi: 10.1136/bmj.309.6965.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vingilis E, McLeod AI, Stoduto G, Seeley J, Mann RE. Impact of extended drinking hours in Ontario on motor-vehicle collision and non-motor-vehicle collision injuries. J Stud Alcohol Drugs. 2007;68:905–911. doi: 10.15288/jsad.2007.68.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinson DC, Maclure M, Reidinger C, Smith GS. A population-based case-crossover and case-control study of alcohol and the risk of injury. J Stud Alcohol. 2003;64:358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- Watt K, Purdie D, Roche AM, McClure RJ. Risk of injury from acute alcohol consumption and the influenceof confounders. Addiction. 2004;99:1262–1273. doi: 10.1111/j.1360-0443.2004.00823.x. [DOI] [PubMed] [Google Scholar]
- Watt K, Purdie DM, Roche AM, McClure RJ. The relationship between acute alcohol consumption and consequent injury type. Alcohol Alcohol. 2005;40:263–268. doi: 10.1093/alcalc/agh164. [DOI] [PubMed] [Google Scholar]
- Zador PL, Krawchuk SA, Voas RB. Alcohol related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. J Stud Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]