Abstract
Objective:
Inhalants are a serious public health concern and a dangerous form of substance use. An important unresolved issue in the inhalant literature concerns the validity of inhalant-use diagnoses and the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, distinction between inhalant abuse and inhalant dependence. To address these limitations and provide the foundation for helping build stronger diagnostic and assessment tools related to inhalant problems, this study examined the dimensionality of the criteria set and the abuse—dependence distinction using item response theory (IRT) analysis.
Method:
This study used data from a survey of the population of Missouri Division of Youth Services' residents of the residential treatment system. The current study focused on adolescents and young adults who reported a lifetime history of inhalant use (N = 279).
Results:
The results from the IRT analysis showed no consistent hierarchical ordering of abuse and dependence criteria, providing strong evidence against the abuse—dependence distinction. The abuse criterion of legal problems associated with use represented the item with the highest level of inhalant severity. The dependence criterion that was related to giving up important social, occupational, or recreational activities provided the most accurate discrimination between individuals at different levels of severity.
Conclusions:
Inhalant-use disorders are best represented using a dimensional versus a categorical approach. IRT analysis provides guidance for selecting criteria that can be useful for brief assessments of inhalant-use problems.
For many years, inhalants have been a serious public health concern and among the most dangerous forms of substance use (Dinwiddie, 1994, 1998). Inhalants are associated with harmful outcomes that rival or exceed those characteristic of other substances (Esmail et al., 1992; Hormes et al., 1986). They disproportionately afflict vulnerable subpopulations, including the poor, select minority groups, the mentally ill, and persons involved with the juvenile and criminal justice systems (Mackesy-Amiti and Fendrich, 1999; McBride et al., 1991). Inhalants can lead to “sudden sniffing death” and serious accidents (El-Menyar et al., 2005; Pfeiffer et al., 2006).
Recent survey evidence shows widespread use in the adolescent population—approximately 16.1% of eighth graders reported inhalant use, a rate that is slightly higher than the rate of marijuana use among this group (15.7%; Johnston et al., 2007). Other survey results show that more than half a million youths ages 12-17 years reported past-year inhalant use (Wu et al., 2004). Recent research also shows significant abuse liability associated with inhalants, with nearly 20% of adults who used inhalants meeting lifetime criteria for inhalant abuse or dependence (Wu and Howard, 2007).
Despite the prevalence and public significance of inhalant use, inhalants are among the least studied of the major psychoactive substances (Balster, 1987; Balster, 1998; Hartman, 1998; Young et al., 1999). The general absence of knowledge is reflected in the minimal description of inhalant-use disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 2000), vis-à-vis prevalence; course; subtypes; comorbid medical and mental health conditions; and specific age, gender, and sociodemographic features.
With the growth in epidemiologic studies of inhalants, questions have been raised about the reliability and validity of DSM-IV criteria for inhalant-use disorders (Ridenour et al., 2007). An important unresolved issue concerns the validity of the DSM-IV distinction between inhalant-abuse and inhalant-dependence disorders. This issue is recognized in DSM-IV (American Psychiatric Association, 2000), where generic substance-use disorder criteria are used in the inhalant-use disorder criteria set but may not be appropriate. Specifically, one generic substance-dependence criterion assesses whether “a great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects” (p. 197). However, it is unlikely that inhalant users spend a great deal of time trying to access inhalants, given their ubiquity in the physical environment.
In a study of adolescent and young-adult inhalant users, Ridenour et al. (2007) found low reliabilities of diagnoses but better reliabilities for symptom counts and abuse diagnoses, irrespective of whether an individual qualified for dependence. Based on their findings, they emphasized the importance of future research examining alternative configurations of diagnostic criteria for inhalant-use disorders. This underscores the need for analyses of the latent structure of inhalant-use disorders, with careful attention to how each criterion performs relative to what it is supposed to indicate.
At present, we are aware of only one study that examined the latent structure of DSM-IV disorders. Specifically, Howard and Perron (2009) subjected DSM-IV inhalant-use disorder criteria to identify subgroups of inhalant users. Three groups were identified: (a) nonsymptomatic users, (b) symptomatic users, and (c) highly symptomatic users. These classes exhibited a graded relationship of severity that would be expected with a distinction between abuse and dependence. However, these empirically derived groups showed only modest correspondence with classifications made using DSM-IV diagnostic criteria and guidelines.
There have been recent studies of the latent structure of the DSM-IV diagnostic criteria for other substance-use disorders, such as alcohol-, cannabis-, and cocaine-use disorders (Blanco et al., 2007; Compton et al., 2009; Flaherty, 2008; Gillespie et al., 2007; Langenbucher et al., 2004; Martin et al., 2006; Muthén, 2006; Saha et al., 2006, 2007). These studies are important because they help address the validity of diagnoses and disorders, which provides the necessary conditions for developing effective assessment and treatments. The results of Howard and Perron (2009) and the long-standing controversy regarding the abuse-dependence distinction (Hasin and Paykin, 1999; Lopez et al., 2007) suggest the need for empirical investigation of inhalant-use disorders, particularly viewing the disorder on a single continuum of severity.
The purpose of this study was to examine the construct validity of inhalant-use disorders using item response theory (IRT), with focused attention to the abuse-dependence distinction. IRT refers to a set of generalized linear models and related statistical procedures that relate a person's observed survey responses to an unmeasured underlying or latent trait (Hays, 2000). By using IRT, we sought to identify where on the continuum of severity each inhalant-related criterion is located (i.e., item severity) and the extent to which the items distinguished individuals based on severity (i.e., item discrimination). This study is an important advancement in understanding the validity of DSM-IV inhalant-use disorders and represents the first IRT analysis of the inhalant-use disorder criteria set.
Method
Sampling frame and recruitment approach
Findings from the present study come from a survey of the population of Missouri Division of Youth Services' (MDYS) residents of the residential treatment system. MDYS is the legal guardian of residents committed to its care by the state's 45 juvenile courts. The 723 adolescents who completed the interview constituted 97.7 % of MDYS residents at the time interviews were conducted and 55.0 % of youths committed to MDYS care in the prior year. Thus, the survey was a virtual census of MDYS residents at the time the study was undertaken, and it produced a large, representative sample of MDYS annual residents.
Participation in the study was voluntary. All youths received an age-appropriate explanation of their privacy rights and a copy of the Washington University brochure “Your Privacy Matters,” as well as a copy of their signed informed-assent agreement. Before participating in the study, all youths were asked to read an informed-assent agreement, raise any questions they had about the study, and then sign the assent form if they felt that their questions had been answered satisfactorily and if they had decided to participate. The informed-assent form provided youths with detailed information about the study and assured them that they were not required to participate, that they could end participation in the interview at any time, and that their legal status would not be affected by their decision to participate or not participate in the study. The informed-assent form also provided potential participants with the name and telephone number of a nonstudy and non-university-affiliated advocate whom they could call for more information about the study. As legal guardian of the youths, MDYS provided formal permission for youths to participate in the study. MDYS agreed that youths could use the telephone during business hours to call the advocate, should they desire to do so, and youths were informed of this agreement. The informed-assent form was based on a template developed by the Washington University Institutional Review Board and was specifically designed for use with pediatric populations.
This study was approved by the MDYS Institutional Review Board, Washington University Human Studies Committee Institutional Review Board (with prisoner representative and otherwise operating in accordance with governing regulations for research on prisoners and youths), and the federal Office of Human Research Protection (as required for research on prisoners) and was granted a Certificate of Confidentiality by the National Institute on Drug Abuse. All interviewers completed an intensive 8-hour training session, and an interview editor was on site at each facility as adolescents were interviewed to minimize interviewer omissions and errors. Interviews were conducted in rooms with private areas. Participants received $10.00 for their participation.
MDYS youths are representative of delinquent youths in state-mandated care nationally with regard to age, gender, and number of state youths in residential care per 100,000 adolescents. In 2000, 15.3 % of MDYS residents were committed for minor “status” offenses (e.g., truancy), 32.4% were committed for misdemeanors, 40.2 % were committed for less serious felonies, and 12.1 % were committed for more serious felonies.
Measures
Structured, face-to-face interviews of adolescents were conducted using two assessments, the Volatile Solvent Screening Inventory and the Comprehensive Solvent Assessment Interview (Howard et al., 2008). All participants completed the Volatile Solvent Screening Inventory, which assesses demographic characteristics, medical history, lifetime and past-year use of 55 volatile solvent inhalants, other drug use and substance-related problems, current psychiatric symptoms, suicidality, trauma history, antisocial traits, and criminal activity. A description of the Volatile Solvent Screening Inventory, its psychometrics, and a copy of the instrument itself are available in Howard et al. (2008). Consistent with DSM-IV diagnostic guidelines, nitrite vasodilator and nitrous oxide use were not considered inhalant use for the purposes of this investigation.
Youths who reported lifetime use of one or more volatile solvents included in the Volatile Solvent Screening Inventory also completed the Comprehensive Solvent Assessment Interview (Howard et al., 2008). Items from the Diagnostic Interview Schedule (Version IV) were included to assess for the presence of DSM-IV inhalant-abuse and inhalant-dependence disorders. The Diagnostic Interview Schedule generally evidences good reliability for the assessment of substance-use disorders (Atkan et al., 1997; Howard et al., 2008) but we are unaware of any studies that examine the psychometrics of the Diagnostic Interview Schedule items specifically related to inhalants. Psychometric properties are unavailable on the Volatile Solvent Screening Inventory and the Comprehensive Solvent Assessment Interview. However, prior research with this study sample also revealed graded associations between the level of inhalant involvement (i.e., lifetime use without a disorder, lifetime abuse without dependence, and lifetime abuse with or without dependence) and other psychiatric and substance-use conditions (Freedenthal et al., 2007; Howard and Perron, 2009; Howard et al., 2008; Perron and Howard, 2009).
Data analysis
Most applications of IRT assume unidimensionality and local independence. Unidimensionality refers to only one construct being measured by the scale items, and local independence means that items are uncorrelated with each other when the latent trait has been controlled for (Hays et al., 2000). According to Hays et al. (2000), if the assumption of unidimensionality holds, then only a single trait is influencing item responses, and local independence is obtained. Similar to prior studies employing IRT, this study tested a unidimensional (i.e., single-factor) model using confirmatory factor analysis. Given that the items used are dichotomous, weighted least squares estimation methods were used because the assumptions for maximum likelihood estimation could not be met.
The IRT model estimated in this study is a two-parameter model, which includes severity and discrimination parameters (Saha et al., 2006). The severity parameter, also commonly referred to as the difficulty parameter in other studies using IRT, describes how the criterion is associated with the latent trait, based on the point on the latent continuum where there is a 50% chance of the criterion being endorsed. Item severity coefficients are in the metric of a standard distribution with a mean of zero. The discrimination parameter represents the extent to which the criterion can discriminate people who are higher on the continuum versus those who are lower (Saha et al., 2006). The constants for both item severity and discrimination parameters were set at 1.0 (Embretson and Reise, 2000).
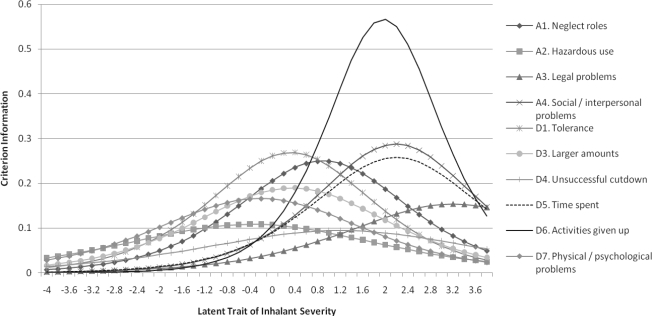
To facilitate interpretation of the values, two different types of curves were constructed: criterion response curves and criterion information curves. Criterion response curves are a visual representation of the severity and discrimination parameters. Criteria associated with higher levels of severity are found further to the right on the X axis. The slope of the criterion response curve indicates the criterion's ability to discriminate individuals along the latent continuum, with steeper curves representing greater ability to discriminate. Criterion information curves were constructed to summarize the amount of information value for each criterion using severity and discrimination parameters (Saha et al., 2006). Curves with the highest peak represent the criterion that conveys the most information about the severity and discrimination of the criterion relative to the underlying continuum examined.
Results
Sample characteristics
Regarding the sample of inhalant users in this study, approximately 75% (n = 209) were White, and 84% (n = 233) were male. The mean age was 15.6 years (SD = 1.12). Thirty-nine percent (n = 107) reported that their family received public assistance. We examined differences between inhalant users and inhalant nonusers using chi-square and t tests. No differences were observed with respect to age, gender, and family receipt of public assistance. However, inhalant use was associated with urbanicity, χ2(1) = 53.72, p < .001, with a greater proportion of inhalant users living in small towns/ urban areas. Inhalant use also was more common among White subjects versus non-White subjects, χ2(1) = 131.83, p < .001.
More than one third (38.6 %; n = 279) of the sample reported lifetime inhalant use. The current study focused on these youths. Among inhalant users, 62 (22.2%) met criteria for lifetime inhalant abuse; 79 (28.3%) met criteria for inhalant dependence; and 138 (49.5%) did not meet criteria for inhalant abuse or dependence. Fifty-two subjects (18.6%) were classified as “diagnostic orphans”—that is, meeting one or two criteria for dependence but not meeting diagnostic criteria for either inhalant abuse or dependence.
Prevalence of symptoms
Table 1 presents findings describing the prevalence of each DSM-IV inhalant-abuse and inhalant-dependence criterion among inhalant users. The most prevalent criterion was recurrent inhalant use in situations in which it is physically hazardous. This abuse criterion was reported by more than half of the adolescent inhalant users (54.5%). The most prevalent dependence criterion was continued use despite knowledge of physical or psychological problems, which was reported by 53.0% of the sample. Recurrent substance-related legal problems had the lowest rate of endorsement (15.1%) of all the criteria. It should be noted that the prevalence for each symptom by diagnosis is reported in Howard and Perron (2009).
Table 1.
Symptom prevalence, factor analysis and item response theory parameter results of DSM-IV inhalant abuse and dependence criteria
| Diagnostic criteria | Symptom prevalence n (%) | CFA factor loadings | Discrimination | Severity |
| Abuse criteria | ||||
| A1. Failure to fulfill major role obligations | 105 (37.6) | .80 | 1.28 | 0.41 |
| A2. Use in which it is physically hazardous | 152 (54.5) | .69 | 0.84 | −0.17 |
| A3. Recurrent substance-related legal problems | 42 (15.1) | .67 | 1.00 | 1.47 |
| A4. Continued use despite having persistent social or interpersonal problems | 59 (21.1) | .82 | 1.37 | 1.00 |
| Dependence criteriaa | ||||
| D1. Tolerance | 127 (45.5) | .81 | 1.33 | 0.15 |
| D3. Inhalant taken in larger amounts | 127 (45.5) | .75 | 1.12 | 0.16 |
| D4. Persistent desire or unsuccessful efforts to cut down | 102 (36.6) | .63 | 0.79 | 0.55 |
| D5. Great deal of time spent to obtain, use, or recover from inhalant effects | 60 (21.5) | .78 | 1.30 | 1.00 |
| D6. Important social, occupational, or recreational activities given up | 60 (21.5) | .87 | 1.93 | 0.90 |
| D7. Continued use despite knowledge of physical or psychological problems | 148 (53.0) | .72 | 1.04 | −0.10 |
Notes: Overall N = 279; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; CFA = confirmatory factor analysis.
Withdrawal (criterion D2) is not part of the DSM-IV inhalant-dependence criteria set.
Dimensionality
Factor analyses were used to test the assumption of unidimensionality of inhalant symptoms. Confirmatory factor analysis provided evidence for a one-factor solution. Goodness of fit indices were within their expected range (comparative fit index = .97, Tucker-Lewis index = .98, root mean square error of approximation = .07). Factor loadings for each criterion also are presented in Table 1. All factor loadings were close to or exceeded the generally accepted threshold of .70, with the exception of the dependence criterion related to persistent desire or unsuccessful efforts to cut down (D4; .63).
Item response theory model parameters
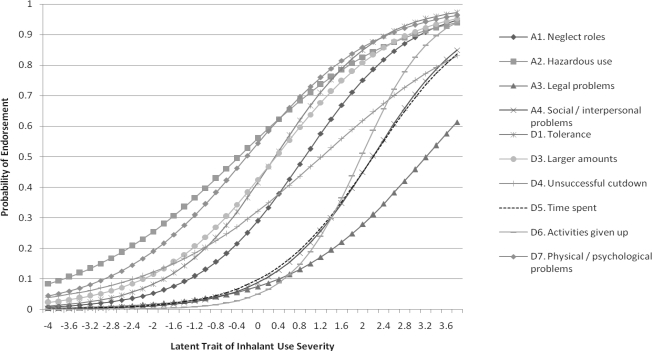
Criterion response curves for the 10 inhalant criteria of abuse and dependence are presented in Figure 1. The symptoms showed a range of discrimination and severity values but did not suggest a clear distinction between the DSM-IV inhalant-abuse and inhalant-dependence disorders. Specifically, the symptoms were mixed in severity without any clear pattern identifying less and more severe clusters of symptoms.
Figure 1.
Criterion response curves for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), inhalant-abuse and inhalant-dependence criteria. Note: Withdrawal (Criterion D2) is not part of the DSM-IV inhalant-dependence criteria set.
Table 1 presents IRT model parameters for inhalant-abuse and inhalant-dependence criteria. The severity parameter represents the point on the latent continuum where there is a 50% chance of respondents endorsing the criterion. Items from the abuse criteria set exhibited the highest and lowest severity parameters. The highest severity estimate was recurrent substance-related legal problems (A3; 1.47); the lowest was use in physically hazardous situations (A2; -0.17). The dependence criterion of spending a great deal of time obtaining, using, or recovering from effects (D5) exhibited the highest severity estimate among all the dependence criteria (1.00).
The discrimination parameter indicates how well a criterion discriminates subjects above the threshold from subjects below the threshold. Discrimination values ranged from 0.84 to 1.93. The dependence criterion regarding giving up important activities (D6) had the highest level of discrimination (1.93), which was substantially higher than the criterion with the second highest value (1.37)—continued use despite persistent social or interpersonal problems (A4). The dependence criterion regarding a persistent desire or unsuccessful efforts to cut down (D4) had the lowest level of discrimination (0.79). This item also exhibited the highest degree of measurement error based on confirmatory factor analysis results.
Criterion information functions were computed and graphically depicted in Figure 2. These curves convey how well each criterion is estimated across the entire inhalant underlying continuum (Baker, 2001). As shown in Figure 2, the dependence criterion regarding giving up activities (D6) measured more precisely than any other criterion, evidenced by the high peaked curve. No other criterion conveyed a similar level of precision. Criteria with the lowest levels of precision were use in hazardous situations (A2) and unsuccessful efforts in cutting down (D4).
Figure 2.
Criterion information curves for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), inhalant-abuse and inhalant-dependence criteria. Note: Withdrawal (Criterion D2) is not part of the DSM-IV inhalant-dependence criteria set.
Discussion
To our knowledge, this is the first study that examined criteria for inhalant-use disorders using a dimensional approach. A confirmatory factor analysis provided support for a unidimensional model, which is consistent with literature favoring a dimensional versus a categorical approach to measuring substance-use disorders (Lopez et al., 2007). Combined with the IRT analysis, study findings provide support for a single, unitary construct of inhalant severity as opposed to discrete abuse and dependence syndromes.
The most compelling support for reconsidering the abuse and dependence distinction for inhalant-use disorders relates to the ordering of the criteria on the severity continuum. More specifically, legal problems (A3) was at the highest end of the severity continuum. This should have preceded the dependence criteria if there was a valid distinction between abuse and dependence. However, the severity of this item may have been inflated because of the use of an incarcerated sample—that is, respondents may not have viewed inhalants as being associated with illegal behaviors relative to other substances such as cannabis or cocaine. This is particularly the case, given that inhalants are readily available and easy to obtain. Two dependence criteria, use in larger amounts (D3) and tolerance (D1), preceded social/interpersonal problems (A4) on the severity scale. The criterion response curve for social/interpersonal problems (A4) was nearly identical to the criterion response curve for time spent recovering from inhalants (D5). Thus, the overall pattern of ordering on the severity continuum does not suggest a hierarchical distinction between abuse and dependence.
Based on the criterion information curve, activities given up was the criterion that conveyed the most information about inhalant-use severity. Not surprisingly, it also had the highest reliability estimate in the confirmatory factor analysis. Therefore, this item might be usefully employed in brief assessments of inhalant-related problems. After this item, four other items were relatively high in the information they conveyed. They included two abuse criteria, social and interpersonal problems (A4) and roles neglected (A1); and two dependence criteria, tolerance (D1) and time spent recovering from inhalants (D5). These indicators, too, would be candidate items for inclusion in brief assessments.
No real comparison studies exist, because this is the first IRT analysis of inhalant-use disorder criteria. However, interesting parallels with IRT analyses of other substances can be made. For example, in an IRT analysis of cannabis-use disorder criteria with a community sample, Compton et al. (2009) also found differential ordering of the abuse and dependence criteria. Similar to the current study, Compton et al. (2009) also found the abuse criterion of legal problems to be at the highest end of the severity continuum and the abuse criterion of hazardous use to be at the lowest end. Saha et al. (2006) also found a mixed ordering of abuse and dependence criteria, but criteria for highest severity were activities given up (dependence criterion) and neglecting roles (abuse criterion). Gillespie et al. (2007) conducted a comprehensive investigation of DSM-IV criteria for abuse and dependence separately for cannabis, cocaine, hallucinogens, stimulants, and opioids. This study, too, found that each class of substances is best represented with a single underlying dimension of severity as opposed to having an abuse and dependence distinction. Moreover, this set of IRT analyses also revealed different patterns of ordering with respect to the severity for the different abuse and dependence criteria.
Study limitations
Although this study has numerous strengths, most notably the large sample of inhalant users and the use of structured interview techniques, it is important that the study findings are interpreted in the context of limitations. Limitations of this study include the self-report nature of the data. The seminal study of Brown et al. (1992) shows that self-reports are reliable and valid for cocaine, alcohol, and marijuana, but the extent to which these results generalize to inhalants remains limited. As described elsewhere, biochemical assays are currently largely unavailable or infeasible for inhalant-use assessment, and the reliability of the Diagnostic Interview Schedule assessment of DSM-IV inhalant-use disorder diagnostic criteria is uncertain (Howard and Perron, 2009). Although the reliability and validity of inhalant-related self-reports are limited in general, some important features of this study build confidence in these areas. For example, in this study subjects were queried on 55 volatile solvent inhalants rather than relying on a single item as done in other psychiatric epidemiologic surveys. The inhalant-related research is underdeveloped compared with that for other types of substances, and further research on the reliability and validity of self-reports of inhalant use is needed.
Another limitation is that this study cannot place inhalant-use disorders in the context of other DSM-IV substance-use disorders or non-substance-related psychiatric disorders, because these conditions were not assessed via structured psychiatric interview in this inhalant-focused study. Additionally, it is important to note that inhalants are the only class of substances that is defined by the method of administration and not the composition of the substance (Balster et al., 2009). It is possible that different inhalants and combinations of inhalants used could be related to differential risks for each substance-use disorder criterion.
Finally, the generalizability of these findings is potentially limited. Specifically, this study included adolescents who were incarcerated in the MDYS and thus do not generalize to the general population of adolescents or adults. Also, in accordance with the DSM-IV, we did not include nitrites as an inhalant; therefore, it is unclear whether these findings generalize to that type of substance.
Future directions
Advancing research on the assessment and diagnosis of inhalants will require investigations of the abuse liability and consequences of the most common types of inhalants, while controlling for the use of other substances and psychiatric conditions. In addition, future research needs to take into consideration the role of inhalant withdrawal as an indicator of inhalant-use severity. It is currently not part of the DSM-IV criteria set for inhalant dependence, although Perron and colleagues (Perron et al., 2009) reviewed evidence contradicting the removal of withdrawal. Although empirical efforts on classifying substance-use disorders from a dimensional point of view continue to grow in strength, additional work—both theoretical and empirical—is needed on how the dimensional system could be effectively applied within the current system of care for the troublesome use of substances.
Footnotes
This research was supported by National Institute on Drug Abuse grants DA027832 awarded to Brian E. Perron and DA021405 and DA15929 awarded to Matthew O. Howard. The National Institute on Drug Abuse had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
References
- Aktan GB, Calkins RF, Ribisl KM, Kroliczak A, Kasim FM. Test-retest reliability of psychoactive substance abuse and dependence diagnoses in telephone interviews using a modified Diagnostic Interview Schedule-Substance Abuse Module. American Journal of Drug and Alcohol Abuse. 1997;23:229–248. doi: 10.3109/00952999709040944. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000. [Google Scholar]
- Baker F. The basics of item response theory. College Park, MD: ERIC Clearinghouse on Assessment and Evaluation, University of Maryland; 2001. [Google Scholar]
- Balster RL. Abuse potential evaluation of inhalants. Drug and Alcohol Dependence. 1987;19:7–15. doi: 10.1016/0376-8716(87)90082-2. [DOI] [PubMed] [Google Scholar]
- Balster RL. Neural basis of inhalant abuse. Drug and Alcohol Dependence. 1998;51:207–214. doi: 10.1016/s0376-8716(98)00078-7. [DOI] [PubMed] [Google Scholar]
- Balster RL, Cruz SL, Howard MO, Dell CA, Cottler LB. Classification of abused inhalants. Addiction. 2009;104:878–882. doi: 10.1111/j.1360-0443.2008.02494.x. [DOI] [PubMed] [Google Scholar]
- Blanco C, Harford TC, Nunes E, Grant B, Hasin D. The latent structure of marijuana and cocaine use disorders: Results from the National Longitudinal Alcohol Epidemiologic Survey (NLAES) Drug and Alcohol Dependence. 2007;91:91–96. doi: 10.1016/j.drugalcdep.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, Kranzler HR, Del Boca FK. Self-reports by alcohol and drug abuse inpatients: Factors affecting reliability and validity. British Journal of Addiction. 1992;87:1013–1024. doi: 10.1111/j.1360-0443.1992.tb03118.x. [DOI] [PubMed] [Google Scholar]
- Compton WM, Saha TD, Conway KP, Grant BF. The role of cannabis use within a dimensional approach to cannabis use disorders. Drug and Alcohol Dependence. 2009;100:221–227. doi: 10.1016/j.drugalcdep.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie SH. Abuse of inhalants: A review. Addiction. 1994;89:925–939. doi: 10.1111/j.1360-0443.1994.tb03348.x. [DOI] [PubMed] [Google Scholar]
- Dinwiddie SH. Psychological and psychiatric consequences of inhalants. In: Tarter RE, Ammerman RT, Ott PJ, editors. Handbook of substance abuse: Neurobehavioral pharmacology. New York: Plenum; 1998. pp. 269–279. [Google Scholar]
- El-Menyar AA, El-Tawil M, Al Suwaidi J. A teenager with angiographically normal epicardial coronary arteries and acute myocardial infarction after butane inhalation. European Journal of Emergency Medicine. 2005;12:137–141. doi: 10.1097/00063110-200506000-00009. [DOI] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item response theory for psychologists. Mahwah, NJ: Lawrence Erlbaum; 2000. [Google Scholar]
- Esmail A, Anderson HR, Ramsey JD, Taylor J, Pottier A. Controlling deaths from volatile substance abuse in under 18s: The effects of legislation. BMJ. 1992;305:692. doi: 10.1136/bmj.305.6855.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherty BP. Testing the degree of cross-sectional and longitudinal dependence between two discrete dynamic processes. Developmental Psychology. 2008;44:468–480. doi: 10.1037/0012-1649.44.2.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedenthal S, Vaughn MG, Jensen JM, Howard MO. Inhalant use and suicidality among incarcerated youth. Drug and Alcohol Dependence. 2007;90:81–88. doi: 10.1016/j.drugalcdep.2007.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie NA, Neale MC, Prescott CA, Aggen SH, Kendler KS. Factor and item-response analysis DSM-IV criteria for abuse of and dependence on cannabis, cocaine, hallucinogens, sedatives, stimulants and opioids. Addiction. 2007;102:920–930. doi: 10.1111/j.1360-0443.2007.01804.x. [DOI] [PubMed] [Google Scholar]
- Hartman DE. Behavioral pharmacology of inhalants. In: Tarter RE, Ammerman RT, Ott PJ, editors. Handbook of substance abuse: Neurobehavioral pharmacology. New York: Plenum; 1998. pp. 263–268. [Google Scholar]
- Hasin D, Paykin A. Alcohol dependence and abuse diagnoses: Concurrent validity in a nationally representative sample. Alcoholism: Clinical and Experimental Research. 1999;23:144–150. [PubMed] [Google Scholar]
- Hays RD, Morales LS, Reise SP. Item response theory and health outcomes measurement in the 21st century. Medical Care. 2000;38(9 Suppl):1128–1142. doi: 10.1097/00005650-200009002-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hormes JT, Filley CM, Rosenberg NL. Neurologic sequelae of chronic solvent vapor abuse. Neurology. 1986;36:698–702. doi: 10.1212/wnl.36.5.698. [DOI] [PubMed] [Google Scholar]
- Howard M, Perron BE. A survey of inhalant use disorders among delinquent youth: Prevalence, clinical features, and latent structure of DSM-IV diagnostic criteria. BMC Psychiatry. 2009;9:8. doi: 10.1186/1471-244X-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard MO, Balster RL, Cottler LB, Wu L-T, Vaughn MG. Inhalant use among incarcerated adolescents in the United States: Prevalence, characteristics, and correlates of use. Drug and Alcohol Dependence. 2008;93:197–209. doi: 10.1016/j.drugalcdep.2007.08.023. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2006. Volume I: Secondary school students. (NIH Publication No. 07-6205) Bethesda, MD: National Institute on Drug Abuse; 2007. [Google Scholar]
- Langenbucher JW, Labouvie E, Martin CS, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Lopez MF, Compton WM, Grant BF, Breiling JP. Dimensional approaches in diagnostic classification: A critical appraisal. International Journal of Methods in Psychiatric Research. 2007;16(Suppl. No. 1):S6–S7. doi: 10.1002/mpr.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Fendrich M. Inhalant use and delinquent behavior among adolescents: A comparison of inhalant users and other drug users. Addiction. 1999;94:555–564. doi: 10.1046/j.1360-0443.1999.94455510.x. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: Implications for DSM-V. Journal of Abnormal Psychology. 2006;115:807–814. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- McBride AA, Joe GW, Simpson DD. Prediction of long-term alcohol use, drug use, and criminality among inhalant users. Hispanic Journal of Behavioral Sciences. 1991;13:315–323. [Google Scholar]
- Muthén B. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006;101(Suppl. No. 1):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- Perron BE, Howard MO. Adolescent inhalant use, abuse and dependence. Addiction. 2009;104:1185–1192. doi: 10.1111/j.1360-0443.2009.02557.x. [DOI] [PubMed] [Google Scholar]
- Perron BE, Howard MO, Vaughn MG, Jarman CN. Inhalant withdrawal as a clinically significant feature of inhalant dependence disorder. Medical Hypotheses. 2009;73:935–937. doi: 10.1016/j.mehy.2009.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer H, Al Khaddam M, Brinkmann B, Kohler H, Beike J. Sudden death after isobutane sniffing: A report of two forensic cases. International Journal of Legal Medicine. 2006;120:168–173. doi: 10.1007/s00414-005-0062-x. [DOI] [PubMed] [Google Scholar]
- Ridenour TA, Bray BC, Cottler LB. Reliability of use, abuse, and dependence of four types of inhalants in adolescents and young adults. Drug and Alcohol Dependence. 2007;91:40–49. doi: 10.1016/j.drugalcdep.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and Alcohol Dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, Howard MO. Psychiatric disorders in inhalant users: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;88:146–155. doi: 10.1016/j.drugalcdep.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, Pilowsky DJ, Schlenger WE. Inhalant abuse and dependence among adolescents in the United States. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1206–1214. doi: 10.1097/01.chi.0000134491.42807.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SJ, Longstaffe S, Tenenbein M. Inhalant abuse and the abuse of other drugs. American Journal of Drug and Alcohol Abuse. 1999;25:371–375. doi: 10.1081/ada-100101866. [DOI] [PubMed] [Google Scholar]