Abstract
Context: Good health is the most important outcome of health care, and healthy life expectancy (HLE), an intuitive and meaningful summary measure combining the length and quality of life, has become a standard in the world for measuring population health.
Methods: This article critically reviews the literature and practices around the world for measuring and improving HLE and synthesizes that information as a basis for recommendations for the adoption and adaptation of HLE as an outcome measure in the United States.
Findings: This article makes the case for adoption of HLE as an outcome measure at the national, state, community, and health care system levels in the United States to compare the effectiveness of alternative practices, evaluate disparities, and guide resource allocation.
Conclusions: HLE is a clear, consistent, and important population health outcome measure that can enable informed judgments about value for investments in health care.
Keywords: Population surveillance, life expectancy, epidemiologic measurement, health promotion
Current efforts to improve health care in the United States, though necessarily concentrated on reducing costs and enhancing access because of the growing lack of affordability of health care, should also focus on health outcomes. The absence of an all-encompassing health outcome measure, however, limits our ability to make informed judgments about value for our health care investment. As Kindig, Asada, and Booske noted, “Without careful attention to the outcomes, attention to determinants and policies could proceed without reference to the ultimate goals and become ends instead of means to an end” (2008, p. 2081). The U.S. case is illustrative of this misalignment. In 2007 in the United States, 16.2 percent of GDP was spent on health care (Hartman et al. 2009), and in 2004, U.S. health spending per capita was 2.5 times greater than the median for the countries in the Organization for Economic Cooperation and Development (OECD) (Anderson, Frogner, and Reinhardt 2007). But according to the World Health Organization (WHO), in 2000 the United States ranked only twenty-eighth in the world in healthy life expectancy (Mathers et al. 2001). A greater focus on health outcome measures could help reallocate spending on health care to the broader social and environmental determinants of health, which, as McGinnis, Williams-Russo, and Knickman pointed out, are more influential determinants of population health than health care is (2002).
An important health policy concern in many countries is the extent to which the improvement of quality of life is keeping pace with the increase in life expectancy. More than ten years ago, the Institute of Medicine's Committee on Summary Measures of Population Health concluded that “mortality measures, although important, provide decision makers incomplete and insensitive information about overall population health. Summary measures of population health need to recognize the physical and psychological illnesses and disabilities that cause much individual suffering and limit social and economic advances within and across nations” (Field and Gold 1998, p. 2).
Healthy life expectancy (HLE) is a measure of population health that combines length and quality of life into a single measure. Our article makes the case for adopting HLE as an outcome measure in the United States at the national, state, community, and health care system levels to compare the effectiveness of alternative practices, evaluate disparities, and guide resource allocation. We define health care systems broadly to include those organizations responsible for financing and/or delivering health care to a defined population. Although hospitals and physicians’ groups without a defined population cannot measure HLE independently, they can contribute important mortality and health status information to its calculation. We critically review the literature and practices around the world for measuring and improving HLE and synthesize that information as a basis for recommendations for the adoption and adaptation of HLE as an outcome measure in the United States. HLE is a clear, consistent, and important population health outcome measure that can inform judgments about value for health care investment. HLE also can be an important outcome measure to guide and evaluate resource allocation and improvement initiatives for both health care systems and public health agencies. According to the World Health Organization (Murray, Salomon, and Mathers 2000), HLE's potential applications include comparing the health of one population with another, monitoring changes in the health of populations, and identifying and quantifying health inequalities within populations.
What Is Healthy Life Expectancy?
Healthy life expectancy (HLE) is the expected number of remaining years of life spent in good health from a particular age, typically birth or age sixty-five, assuming current rates of mortality and morbidity. According to the Réseau Espérance de Vie en Santé (REVES), the international network on health expectancies and the disablement process, healthy life expectancy, sometimes referred to as health expectancy, is a general term referring to “the entire class of indicators expressed in terms of life expectancy in a given state of health. Health expectancies are indicators of current health and mortality conditions” (REVES 2008b, p. 1). Health expectancies can be, and have been, created by adjusting life expectancy by a variety of different measures of health such as disease status, disability, and self-perceived health.
Health status indicators range from objective measures of physiologic, disease, and functional status (such as the ability to climb a flight of stairs) to subjective measures of self-perceived health. They also extend from single-question, global assessments of overall health status to assessments across multiple domains of health, including physical and mental health and functional status (Fryback et al. 2007). National surveys for population health surveillance frequently use single-question measures (such as overall self-perceived health or functional status), since these questions are short and easy to include in more general population surveys. Nonetheless, measures across multiple domains of health and function provide a more complete assessment of health for both individuals and populations.
Healthy life expectancy has a number of valuable measurement properties. Compared with mortality and morbidity rates, HLE is a more intuitive and meaningful measure of population health to which individuals can relate, as people care greatly about living a long and healthy life. In addition, age standardization is already embedded in the HLE measure, so populations with different age distributions can be compared directly without further adjustment.
HLE has two different and important interpretations. It is a valuable stand-alone measure of population health and also is expressed as a percentage of overall life expectancy (LE). The change in the ratio of HLE to LE over time is a measure of the compression or expansion of morbidity in a population, or the extent to which an increase in life expectancy is accompanied by an increase or decrease in the burden of ill health (Robine et al. 2003).
How Is Healthy Life Expectancy Calculated?
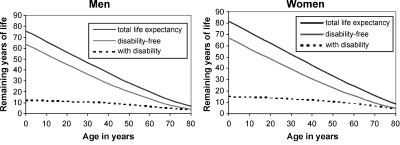
A common way to illustrate healthy life expectancy is shown in figure 1, taken from the European Health Expectancy Monitoring Unit (EHEMU) website (EHEMU 2007). In this example, the measure of HLE is the disability-free life expectancy (DFLE) for Belgian men and women in 2004. The graphs divide life expectancy into years spent with and without disability. For example, in 2004 Belgian women had a DFLE at birth of 66.6 years; thus, on average they spent 82 percent (66.6 years out of a total LE of 81.4 years) of their life free of disability.
Figure 1.
Life Expectancy and Disability-Free Life Expectancy for Belgian Males and Females, 2004
Source: European Health Expectancy Monitoring Unit. 2007. Interpreting Health Expectancies. Used with permission. Available at http://www.ehemu.eu/pdf/Interpreting_HE_guide_ver_6.pdf.
Several useful guides to calculating HLE (Clark et al. 2004; Jagger, Cox, and Le Roy 2006; Molla et al. 2003; Molla, Wagener, and Madans 2001; Murray and Evans 2003; REVES 2008a) have been published. The Sullivan method is, by far, the most commonly used. This method is a relatively straightforward approach that adjusts life expectancy data by the percentage of time spent in less than full health, typically based on cross-sectional survey data (Sullivan 1971). The Sullivan method makes inferences about longitudinal HLE from current cross-sectional or prevalence data, whereas directly measuring the incidence of HLE at various ages requires the longitudinal measurement of a cohort. This alternative technique is called the multistate method. Although it provides more accurate estimates, it is less often used because such longitudinal information requires collecting data on a cohort over time, which are more difficult and costly to obtain. In recent years, microsimulation techniques, combined with longitudinal data, have been used to enhance and make more realistic HLE projections.
How Is HLE Currently Used?
Healthy life expectancy is becoming a standard summary measure of population health at both the international and national levels. It is used for a variety of purposes, including highlighting health inequalities, targeting resources for health promotion, evaluating the impact of health policies, and planning for health, social, and fiscal policy (European Commission 2009). As we noted earlier, it also is used to assess the compression or expansion of population morbidity over time. The World Health Organization (WHO) measures HLE, labeled health-adjusted life expectancy, for 193 countries. These estimates are based on country life tables, analyses of 135 causes of disability for seventeen regions of the world, and sixty-nine health surveys in sixty countries. Disability scores are based in part on disability weights assigned to a large number of diseases and conditions. According to the WHO, in 2007 the range of life expectancy in good health was more than twofold, ranging from thirty-five years in Sierra Leone to seventy-six years in Japan (WHO 2009).
The European Union (EU) also monitors the HLE of its member countries, based on a standard set of questions from the Statistics on Income and Living Conditions Survey (EU-SILC) (European Commission 2009). In 2004, the EU selected HLE (labeled healthy life years) to be one of the European structural indicators to be monitored annually as a key economic outcome measure for social policies related to retirement age and spending for health and long-term care for its rapidly aging population (European Commission 2009). The European Commission (EC) sponsored a study by RAND Europe in 2006 to assess the uptake of the healthy life years (HLY) structural indicator in the EU and ministries in member states (Oortwijn et al. 2006). The EC concluded from this study that the HLY indicator is relevant to policies, impact assessment, and monitoring regarding labor force participation, pensions, health conditions, and lifestyles.
A large and growing number of countries now measure HLE at the national level. The United Kingdom currently uses HLE in a variety of policy applications, for example, to monitor the quality of life and social exclusion of the elderly, as an indicator of sustainable development, and in deliberations on changing the retirement age (Bajekal 2007; Breakwell and Bajekal 2005). Canada measures and reports HLE for the nation and its provinces based on the Health Utilities Index (HUI3), a measure of health status across multiple domains of health such as ambulation, pain, and cognition (Health Canada 2008). One aim of South Australia's Strategic Plan is increasing healthy life expectancy at birth by 5 percent for males and 3 percent for females between 2000 and 2014. This strategy has spawned a variety of community-level interventions targeting improvement in HLE, which have been evaluated and implemented based on an assessment of efficacy, acceptability, feasibility, and cost, stratified by socioeconomic status. Halfway through this period, HLE at birth had steadily increased by 1.9 percent for males and 1.3 percent for females (Banham et al. 2009). In the United States, the two goals of the federal government's Healthy People 2010 initiative are increasing the quality and years of healthy life and eliminating disparities (U.S. Department of Health and Human Services 2009a). HLE, by definition, is an appropriate measure for the first goal and also is an excellent measure for the disparities goal.
The positive relationship between socioeconomic status and HLE has been well documented (Kaplan et al. 2007). In Scotland, as well as in the rest of the United Kingdom, the population is divided into “deprivation” quintiles for many social service purposes, based on several socioeconomic measures (Carstairs and Morris 1991). In 2000, the life expectancy gap between the lowest and highest deprivation quintiles in Scotland was 4.6 years, but the HLE gap between the lowest and highest quintiles was almost three times wider. At age sixty-five, HLE was almost 40 percent higher in the least deprived quintile than in the most deprived quintile. Similar gaps in HLE were found across geographic areas (Clark et al. 2004).
Many of the measures and methods for calculating HLE are similar across countries, but important differences remain. In recent years, however, several organizations, including REVES, Eurostat, and the World Health Organization, have worked to develop comparable methods and measures of HLE for meaningful cross-country comparisons (Murray et al. 2002; REVES 2007; Robine et al. 2003; Robine and Jagger 2007). As a result, while many issues remain, there has been substantial progress in comparing HLE measures.
Although HLE is used less frequently at the subnational level, applications are growing rapidly and have been produced in many countries (Bebbington and Bajekal 2003; Clark et al. 2004; Manuel et al. 2000). In the United Kingdom, in addition to separate country reports, England, Wales, and Scotland also have conducted subnational studies (Bajekal 2005; Bajekal et al. 2002; Clark et al. 2004; Macdonald, Straughn, and Sutton 2006; Smith, Edgar, and Groom 2008). Bissett found that “by adapting the methods used in the national calculations, it is feasible to produce healthy life expectancy estimates for National Health Service regions and health authorities” (Bissett 2002, p. 21). Canada, as well, has conducted a variety of subnational studies of HLE using the Health Utilities Index. For example, Manuel and colleagues calculated HLE for Ontario's forty-two public health units between 1988 and 1992 (Manuel et al. 2000). Examples of subnational calculations of HLE in the United States include the state level—Utah (Utah Office of Public Health Assessment 2002), North Carolina (Buescher and Gizlice 2002), and Washington (Moriarty et al. 2003)—and the county level—Pierce County, Washington (Klementiev 2006). These studies collectively have demonstrated substantial differences in HLE across geographic, demographic, socioeconomic, and racial groups.
One of the few studies of HLE use at the health care provider group level investigated the feasibility of monitoring the health of elderly people with and without diabetes using a measure of “active life expectancy” with routinely collected primary care data in a general practice in England (Jagger et al. 2003). The study found that among the elderly, those with diabetes had a lower life expectancy and were active for a smaller percentage of their remaining life, compared with those without diabetes. It concluded that such methods could feasibly be used by the Strategic Health Authority, Primary Care Trust, and general practice levels to monitor health needs, highlight health inequalities, and evaluate intervention strategies. Although there are few examples of initiatives that measure improvement in HLE locally, England's East Lancashire Primary Care Trust has an ambitious, five-year campaign to increase life expectancy by Saving a Million Years of Life for its population of 380,000 people. The trust's preliminary estimate of life years saved during 2006/2007 is 300,000, based on mortality data from the Office for National Statistics, which represents an increase in life expectancy of nearly 0.8 years for the population, primarily through improvements in infant and cardiovascular disease mortality (Gibson and Iqbal 2009). The trust now is interested in assessing the extent to which the added life years are healthy life years.
Decomposition of HLE into the specific conditions that lead to mortality and morbidity illustrates the utility of the composite measure by providing important insights into how to improve overall HLE, including the impact on the compression or expansion of morbidity. Traditional studies of the impact and prevention of disease and disability tend to look separately at mortality and morbidity and thus ignore differences in the time spent in ill health. Interventions that add life years may have differential effects on the amount and percentage of time spent in ill health. Strategies delaying both death and functional loss may still increase the relative and absolute amount of time spent with functional loss (Nusselder and Peeters 2006). Various studies have shown that improving lifestyle and health behaviors, such as eating more nutritious food, not smoking, losing weight, and being more physically active, reduces morbidity more than mortality and thus decreases the amount of time spent with illness (Hubert et al. 2002; Nusselder et al. 2000). In addition, other studies have found that more disability-free years than total life years were gained for persons free of stroke, cognitive impairment, arthritis, and/or visual impairment, suggesting that reducing the prevalence of these conditions would result in compressing disability (Health Canada 2003; Jagger et al. 2007).
Decomposition studies also have been used to better understand differences in HLE across sociodemographic groups. Banham and colleagues studied the contributors to differences in HLE across deprivation quintiles in South Australia and found that cardiovascular disease contributed more than half a year to the shortfall in HLE in areas of most socioeconomic disadvantage (Banham et al. 2009). Nusselder and colleagues found, too, that disabling diseases such as arthritis, back complaints, and asthma/COPD contributed substantially to differences in HLE by education (Nusselder et al. 2005). Such studies provide important insights into potential policy and organizational initiatives to improve HLE and reduce disparities.
Adapting Healthy Life Expectancy Measurement for Health Care Systems and Communities
Challenges to the use of HLE for health care systems and communities include the lack of defined populations, the limited availability of mortality and health status data, small sample sizes, sensitivity of the HLE measure to improvement efforts, and migration of the population.
Lack of a Defined Population for U.S. Health Care Systems
The separation of health care delivery and financing in the United States makes it difficult to identify the population served by health care delivery systems outside managed care, and therefore we cannot independently calculate mortality and morbidity rates. In addition, hospitals are not a good source of health status data because their patients are sicker than the general population. But their discharge records can contribute valuable mortality data to a larger community collaboration that does serve a defined population. Physicians’ groups that do not serve a defined population do not have good information about mortality, but they can and often do gather health status information about their patients during office visits for routine exams or through outreach communications to their patients. This information also could be added to a larger collaboration serving a defined population. Even though health insurers do have a defined population, those that are not connected to health care delivery systems often have limited claims information about their enrollees. Because of the potential value of health status information for various purposes, however, including underwriting, insurers are increasingly finding ways to gather information about their enrollees’ health status.
Lack of a population denominator in U.S. health systems has become an important issue for U.S. health care reform. The Institute for Healthcare Improvement's Triple Aim initiative has called for health systems to focus on the simultaneous improvement of population health, per capita cost, and the individual experience of care (Berwick, Nolan, and Whittington 2008). In addition, Fisher and colleagues have called for creation of “accountable care organizations” with accountability for the care of a defined population, based on hospitals’ admitting practices by physicians (Fisher et al. 2007). Even without such reforms, the Dartmouth Atlas, which has been measuring geographic variation in health system performance across the United States for more than twenty years, has developed an innovative method for imputing a population denominator for more than three hundred hospital referral regions in the United States, based on regional patterns of utilization (Dartmouth Institute for Health Policy and Clinical Practice 2009). The Dartmouth Atlas then uses these population denominators to calculate population-based rates for costs, utilization, and quality, including mortality, in these hospital referral regions for the Medicare population. The mortality data available for these populations, coupled with the health status data provided by health care systems, could be used to calculate HLE for hospital referral regions or similar service populations defined by patterns of utilization. The United States has invested substantially over the past few years in developing the technology and systems to share such information across health care systems, through the development of regional health information organizations, sometimes referred to as health information exchanges (Healthcare Information and Management Systems Society 2009).
Limited Availability of Mortality and Health Status Data
Even integrated financing and delivery systems have difficulty reporting mortality rates, partly because of the difficulty of obtaining such data. Although mortality statistics are produced for the U.S. states and most of the counties through state vital statistics departments and the National Vital Statistics System of the National Center for Health Statistics (NCHS 2009), the populations served by health care systems usually do not map neatly to county boundaries. Mortality data are more readily available than commonly assumed, however, through the Social Security Administration (SSA) Death Master File, which contains more current information on all deaths reported to the SSA (National Technical Information Service 2009). Although this data source does not specify the cause of death, it can be used to supplement hospital discharge and vital statistics sources to provide a more complete assessment of deaths.
Also, as noted earlier, health care systems typically do not measure self-perceived health status. Various methodological, conceptual, practical, attitudinal, and informational barriers inhibit their more widespread use. These barriers include the time and cost of collecting and reviewing the data, as well as skepticism and uncertainty about their validity and utility compared with traditional clinical data (Nelson and Berwick 1989). Newer technologies, however, such as the Internet, automated telephone outreach, and personal health records, can make gathering health status data more convenient, quicker, and less costly. In addition, simple measures of self-perceived health status have been shown to be very good predictors of functional status, cost, and even mortality (DeSalvo et al. 2006; Idler and Kasl 1995; Southerland, Fisher, and Skinner 2009).
Small Sample Sizes
The inability to obtain adequate sample sizes is the most common reason given for the inability to calculate HLE for local areas. Variability in HLE estimates derives primarily from two sources: the normal variation of estimates of life expectancy from population mortality data and the variance attributable to sampling error of health status derived from survey data. Although mortality measurement is much more common than health status measurement, a small population size can be a greater problem for calculating life expectancy, since population mortality rates are low, especially in younger age groups. The smaller the population is, the more the mortality rate will vary from year to year. Even so, in many countries, life expectancy has become a standard subnational measure of health system performance. In England and Wales, the Office for National Statistics (ONS) has determined a minimum population size of five thousand for calculating life expectancy at the ward, or electoral district, level (Toson and Baker 2003). Experimental ward-level life expectancy estimates have been produced based on pooled deaths over five-year periods (ONS 2006). In the United States, counties are the smallest unit for which mortality data are routinely available. Ezzati and colleagues calculated life expectancy for U.S. counties with populations of at least ten thousand men and ten thousand women, pooled over five years, to create stable life expectancy estimates (Ezzati et al. 2008).
Although measuring health status is not as common as measuring life expectancy, a small population size is conceptually less problematic because health status information, unlike mortality data, is potentially available for everyone in the population. The practical difficulty is that health status data are typically collected for only small random samples of the population, resulting in large confidence intervals for the resulting estimates. But the sample sizes could be substantially increased through more widespread collection of this information in health care systems and greater collaboration among insurers, physicians’ groups, hospitals, and public health entities.
The tolerability of variation around estimates of HLE depends on the application. Statistically significant annual changes in HLE for small populations are difficult to detect. But with wide geographic variation in life expectancy, as demonstrated across local authorities in England and counties in the United States, differences across local areas in HLE should be both meaningful and important. The HLE calculator on the REVES website can be used to provide high-level estimates of the variability of HLE estimates based on the size of the population and the survey sample. For example, using baseline data for Belgian women in 2004, for a population of 100,000 with one thousand deaths and five thousand survey respondents, the 95 percent confidence interval around the estimate of HLE is approximately plus or minus one year. If health status information were collected for everyone in this hypothetical population of 100,000 people, the 95 percent confidence interval for HLE would be reduced to plus or minus one-half year (REVES 2008a).
Techniques for increasing the sample size include aggregation (by broader age groups, by gender, over time, or across geography) and gathering health status information from the health care systems in a community. Each technique has drawbacks. The broader the age group is, the less accurate the assumption of constant rates of ill health within the age group will be. Women have significantly longer HLE than men, so merging the two genders loses this important information. Merging multiple years of data is the most common way of increasing sample size, although this constrains comparisons over time. Geographic aggregation also is common and often necessary, but it masks variations within the geographic aggregation and is difficult to do across separate physicians’ groups and hospitals. The degree and type of data aggregation should be consistent with the purpose of the measurement, recognizing that in some cases, data aggregation may hide important differences between and within various subgroups and possibly limit the ability to drill down on important measures.
Even though using data from health care systems presents challenges in data comparability, they are a potentially valuable, and largely untapped, source of information about population health. Health risk assessments, or HRAs, are increasingly used for various purposes by insurers, employers, and providers. Most of the commercial HRAs include questions on self-perceived health that can be used in calculating HLE if such HRAs are available for a representative sample of a health care system. The Institute for Healthcare Improvement's Triple Aim initiative currently comprises more than seventy organizations from around the world, including integrated health systems, insurers, delivery systems, purchasers, public health systems, and community organizations (Berwick, Nolan, and Whittington 2008). Several of the participating organizations are exploring innovative approaches to gathering information on population health status. These approaches include a more widespread use of health risk assessment tools; a birthday greeting to members of a general practitioner panel by phone, postcard, or Internet that asks about current health status; documenting health status at all health care encounters; and an annual communitywide health status assessment day.
Sensitivity of the HLE Measure to Improvement Efforts
A related question about the utility of the HLE measure is the sensitivity of the measure to impacts of improvement efforts on changes in a population's mortality and morbidity. The REVES HLE calculator can also be used to provide a general idea about the sensitivity of the measure. Based on the same data for Belgian women in 2004, a 10 percent reduction in the number of deaths in the population, distributed evenly across age groups, would increase LE at birth by one year and HLE at birth by a little more than half a year. A 10 percent reduction in the percentage of the population in ill health, distributed evenly across age groups, would increase HLE at birth by 1.5 years (REVES 2008a).
Population Migration
Almost all estimates of HLE are constructed with cross-sectional data but are interpreted as expectations of future HLE for a cohort, assuming current rates of mortality and good health. For example, the underlying assumption is that a twenty-year-old will have the same mortality and morbidity when he or she reaches age eighty as current eighty-year-old residents in the area. While these assumptions can be reasonable for a static population, migration of the population can have a significant impact on this assumption, especially for small areas. For example, since Florida is a major retirement destination in the United States, the current mortality and morbidity of elderly Florida residents who come from other areas are not likely to be representative of a cohort of younger Florida residents. Therefore, migration might create a false impression about the relative healthfulness of local areas (Bebbington and Bajekal 2003). In areas with a large volume of migration, it might be necessary to track a stable cohort or to broaden the geographic area being analyzed.
Gaps
Despite the potential value of HLE measurement, the following important gaps remain:
The gap between the growing use and acceptance of HLE measurement at the national level and its limited use at the local level. To the extent that health care systems and communities do not measure HLE, there is a potential disconnect between what is important at the national level and what is managed at the local level.
The gap between what many health care systems articulate in their mission statements (population health outcomes) and what they actually measure and act upon (health care inputs, such as hospital days, procedures, and tests).
The gap between the outcome measures used in health services research and the outcome measures used in practice. Even though quality-adjusted life years (QALYs)—a specific application of the more general construct of healthy life years, the building blocks of HLE—are now the recommended standard outcome measures for comparative effectiveness research (Miller, Robinson, and Lawrence 2006), such measures are rarely used in practice.
The gap between the private health care financing and delivery system and the public health system. Public health systems do not take advantage of the potentially rich source of information about health available from the private health care system, instead often relying on small random samples. Likewise, private health care systems do not take full advantage of the rich sources of public health, environmental, and social information available to them, such as vital statistics, education, crime, pollution, income, and unemployment, which are important to the health of their patients and members. Such exchanges of information and coordination between the private health care delivery and public health systems would help improve communities’ health care and health.
Recommendations
The following recommendations should be considered to promote healthy life expectancy as an important outcome measure at the national, state, community, and health care system levels. Such considerations must necessarily address any privacy and data security issues with collecting and reporting such information.
Current national initiatives in the United States that are focused on health outcomes should adopt a consistent measure of HLE as the principal health outcome measure for the nation and states. Counties (or aggregations of small counties) should use consistent mortality and health status measures to construct HLE and report the data either as separate life expectancy and health status measures or in combination as HLE. Specifically, the health status data used to calculate HLE should be based on one or more questions from the four-item Healthy Days set (CDC HRQOL-4) used by the Centers for Disease Control and Prevention (CDC) in national surveys such as the Behavioral Risk Factor Surveillance System (BRFSS) (CDC 2005; National Center for Chronic Disease Prevention and Health Promotion 2009). These questions also should be considered for inclusion in the American Community Survey, a national survey of more than three million households designed to supplement the decennial census (U.S. Census Bureau 2009). The CDC's health status measurement set might be supplemented with measures of health status across multiple domains of health, especially mental health, as recommended by a recent CDC expert panel (CDC 2008). In addition, the United States should continue to participate in international efforts, such as the EU's Task Force on Health Expectancies (Robine and Jagger 2007), to harmonize HLE measures used in the United States with those used in other countries and thus facilitate international comparisons.
The following current national initiatives in the United States that are focused on health outcomes should consider HLE as a population health outcome measure:
Healthy People 2020 (U.S. Department of Health and Human Services 2009b).
The State of the USA (SUSA) recommended health indicators (Institute of Medicine 2009).
The National Priorities Partnership goal to improve the health of American communities according to a national index of health (National Priorities Partnership 2008).
The national county health rankings being developed by the University of Wisconsin Population Health Institute through a Robert Wood Johnson Foundation (RWJF) grant, Mobilizing Action Toward Community Health (Robert Wood Johnson Foundation 2009).
United Health Foundation, the American Public Health Association, and the Partnership for Prevention's America's Health Rankings (United Health Foundation, the American Public Health Association, and the Partnership for Prevention 2009).
Gallup-Healthways Well-Being Index (Gallup-Healthways 2009).
Health care systems in the United States should collect health status information for their patients or members at least on an annual basis. For comparability, self-perceived health measures should include the basic questions in the CDC HRQOL-4, and for a more complete picture of population health, health care systems should also consider using one of the standard health status assessment tools covering multiple domains of health, coupled with clinical or administrative data on disease status. Those systems without defined populations should investigate the feasibility of pooling their data regionally through the health information exchange technology infrastructure to create population denominators for the mortality data to calculate HLE for the regional health system. Systems with defined populations of sufficient size should investigate enhancing their mortality data with data from the Social Security Administration to calculate HLE for their populations.
Conclusion
Imagine a U.S. health system with the unifying goal of improving healthy life expectancy, measured consistently at the international, national, state, community, and health care system levels. Transformation to such a goal would gradually cause a shift in investment away from those health care interventions that do not contribute to HLE, including many high-intensity interventions near the end of life that patients do not necessarily value, to the broader social and environmental determinants of health that patients do value. It would also drive better integration among private and public health systems. The achievement of such a goal would help bring U.S. spending on health care more in line with that of other OECD countries and at the same time would improve the U.S. ranking on HLE in the world. Health care reform is ultimately about health.
Acknowledgments
The authors would like to acknowledge the expert editorial support of Jane Roessner, Institute for Healthcare Improvement.
References
- Anderson GF, Frogner BK, Reinhardt UE. Health Spending in OECD Countries in 2004: An Update. Health Affairs. 2007;26(5):1481–89. doi: 10.1377/hlthaff.26.5.1481. [DOI] [PubMed] [Google Scholar]
- Bajekal M. Healthy Life Expectancy by Area Deprivation: Magnitude and Trends in England, 1994–1999. Health Statistics Quarterly. 2005;25:18–27. [PubMed] [Google Scholar]
- Bajekal M. Health Expectancies: The UK Experience. 2007. REVES, May 15–17. Available at http://www.ehemu.eu/ppt/Bajekal_Health_Expectancies_UK.pps accessed May 20, 2009. [Google Scholar]
- Bajekal M, Purdon S, Woodgate-Jones G, Davies S. Healthy Life Expectancy at Health Authority Level: Comparing Estimates from the General Household Survey and the Health Survey for England. Health Statistics Quarterly. 2002;16:25–37. [Google Scholar]
- Banham D, Begg S, Nguyen A, Jury H, Woollacott T. Targeting Health Expectancy Gaps in South Australia. 2009. Paper presented at REVES Conference, Copenhagen, May 27–29. [Google Scholar]
- Bebbington A, Bajekal M. Sub-National Variations in Healthy Life Expectancy. In: Robine J-M, Jagger C, Mathers C, Crimmins E, Suzman R, editors. Determining Health Expectancies. Chichester: Wiley; 2003. pp. 127–47. [Google Scholar]
- Berwick DM, Nolan TW, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs. 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Bissett B. Healthy Life Expectancy in England at Subnational Level. Health Statistics Quarterly. 2002;14:21–29. [Google Scholar]
- Breakwell C, Bajekal M. Review of Sources and Methods to Monitor Healthy Life Expectancy. Health Statistics Quarterly. 2005;26:17–22. [PubMed] [Google Scholar]
- Buescher PA, Gizlice Z. North Carolina Public Health. 2002. Healthy Life Expectancy in North Carolina, 1996–2000. no. 129 (January). Available at http://www.schs.state.nc.us/SCHS/pdf/SCHS-129.pdf accessed May 20, 2009. [Google Scholar]
- Carstairs V, Morris R. Deprivation in Scotland. Aberdeen: Aberdeen University Press; 1991. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention Health-Related Quality-of-Life 14-Item Measure. 2005. Available at http://www.cdc.gov/hrqol/hrqol14_measure.htm accessed May 21, 2009. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Summary of the Health-Related Quality of Life (HRQOL) Surveillance Expert Panel. Atlanta: U.S. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Adult and Community Health; 2008. [Google Scholar]
- Clark D, McKeon A, Sutton M, Wood R. Healthy Life Expectancy in Scotland. 2004. National Health Service for Scotland: Information and Statistics Division, Common Services Agency. Available at http://www.scotpho.org.uk/nmsruntime/saveasdialog.asp?lID=3349&sID=4026 accessed May 20, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartmouth Institute for Health Policy and Clinical Practice. Dartmouth Atlas of Health Care. 2009. Available at http://www.dartmouthatlas.org/ accessed May 18, 2009. [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality Prediction with a Single General Self-Rated Health Question. A Meta-analysis. Journal of General Internal Medicine. 2006;21:267–75. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Commission. Healthy Life Years. 2009. Available at http://ec.europa.eu/health/ph_information/indicators/lifeyears_en.htm accessed May 20, 2009. [Google Scholar]
- European Health Expectancy Monitoring Unit (EHEMU) Interpreting Health Expectancies. 2007. Available at http://www.ehemu.eu/pdf/Interpreting_HE_guide_ver_6.pdf accessed May 20, 2009. [Google Scholar]
- Ezzati M, Friedman AB, Kulkarni SC, Murray CJ. The Reversal of Fortunes: Trends in County Mortality and Cross-County Mortality Disparities in the United States. PLoS Medicine. 2008;5(4):e66. doi: 10.1371/journal.pmed.0050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field MJ, Gold MR. Summarizing Population Health: Directions for the Development and Application of Population Metrics. Washington, DC: Committee on Summary Measures of Population Health, Institute of Medicine, National Academies Press; 1998. [PubMed] [Google Scholar]
- Fisher ES, Staiger DO, Bynum JPW, Gottlieb DJ. Creating Accountable Care Organizations: The Extended Hospital Medical Staff. Health Affairs. 2007;26(1):w44–w57. doi: 10.1377/hlthaff.26.1.w44. Available at http://content.healthaffairs.org/cgi/content/abstract/26/1/w44 accessed December 7, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryback D, Dunham N, Palta M, Hanmer J, Buechner J, Cherepanov D, Herrington SA, et al. U.S. Norms for Six Generic Health-Related Quality-of-Life Indexes from the National Health Measurement Study. Medical Care. 2007;45:1162–70. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallup-Healthways. Gallup-Healthways Well-Being Index. 2009. Available at http://www.well-beingindex.com/ accessed June 5, 2009. [Google Scholar]
- Gibson J, Iqbal A. Saving a Million Years of Life—Measuring Our Success. 2009. PowerPoint presentation, January 22. Available at http://www.eastlancspct.nhs.uk/about-us/smyl/ accessed June 14, 2009. [Google Scholar]
- Hartman M, Martin A, McDonnell P, Catlin A, the National Health Expenditure Accounts Team National Health Spending in 2007: Slower Drug Spending Contributes to Lowest Rate of Overall Growth since 1998. Health Affairs. 2009;28(1):246–61. doi: 10.1377/hlthaff.28.1.246. [DOI] [PubMed] [Google Scholar]
- Health Canada. Arthritis in Canada—An Ongoing Challenge. Ottawa: 2003. [Google Scholar]
- Health Canada. Healthy Canadians: A Federal Report on Comparable Health Indicators, 2008. 2008. Available at http://www.hc-sc.gc.ca/hcs-sss/pubs/system-regime/2008-fed-comp-indicat/index-eng.php accessed June 4, 2009. [Google Scholar]
- Healthcare Information and Management Systems Society (HIMSS) HIMSS Health Information Exchange (HIE) 2009. Available at http://www.himss.org/ASP/topics_rhio.asp accessed May 18, 2009. [Google Scholar]
- Hubert H, Bloch D, Oehlert J, Fries J. Lifestyle Habits and Compression of Morbidity. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2002;57A:M347–51. doi: 10.1093/gerona/57.6.m347. [DOI] [PubMed] [Google Scholar]
- Idler E, Kasl SV. Self-Ratings of Health: Do They Also Predict Change in Functional Ability? Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1995;50B(6):S344–53. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) State of the USA Health Indicators: Letter Report. Washington, DC: National Academies Press; 2009. Available at http://www.nap.edu/catalog.php?record_id=12534 accessed December 8, 2009. [PubMed] [Google Scholar]
- Jagger C, Cox B, Le Roy S. Health Expectancy Calculation by the Sullivan Method. 3rd ed. EHEMU Technical Report; 2006. Available at http://www.ehemu.eu/pdf/Sullivan_guide_final_jun2007.pdf accessed May 20, 2009. [Google Scholar]
- Jagger C, Goyder E, Clarke M, Brouard N, Arthur A. Active Life Expectancy in People with and without Diabetes. Journal of Public Health Medicine. 2003;25(1):42–46. doi: 10.1093/pubmed/fdg009. [DOI] [PubMed] [Google Scholar]
- Jagger C, Matthews R, Matthews F, Robinson T, Robine J-M, Brayne C, the Medical Research Council Cognitive Function and Ageing Study Investigators The Burden of Diseases on Disability-Free Life Expectancy in Later Life. Journal of Gerontology. 2007;62A(4):408–14. doi: 10.1093/gerona/62.4.408. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Orpana H, Feeny D, McFarland BH, Ross N. Prevalence and Factors Associated with Thriving in Older Adulthood: A 10-Year Population-Based Study. Journal of Gerontology. 2007;63A(10):1097–1104. doi: 10.1093/gerona/63.10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D, Asada Y, Booske B. A Population Health Framework for Setting National and State Health Goals. Journal of the American Medical Association. 2008;299(17):2081–83. doi: 10.1001/jama.299.17.2081. [DOI] [PubMed] [Google Scholar]
- Klementiev AA. An Alternative Measure of Years of Healthy Life. In: Estes RJ, editor. Advancing Quality of Life in a Turbulent World. New York: Springer; 2006. pp. 69–86. [Google Scholar]
- Macdonald A, Straughn J, Sutton M. Healthy Life Expectancy Measurement in Scotland. British Actuarial Journal. 2006;12(2):327–94. [Google Scholar]
- Manuel DG, Goel V, Williams JI, Corey P. Health-Adjusted Life Expectancy at the Local Level in Ontario. Chronic Diseases in Canada. 2000;21(2):73–80. [PubMed] [Google Scholar]
- Mathers CD, Murray CJL, Lopez AD, Salomon JA, Sadana R, Tandon A, Ustün BL, Chatterj S. Estimates of Healthy Life Expectancy for 191 Countries in the Year 2000: Methods and Results. 2001. Geneva: World Health Organization, Global Programme on Evidence for Health Policy Discussion Paper no. 38, November. Available at http://www.who.int/healthinfo/paper38.pdf accessed May 20, 2009. [Google Scholar]
- McGinnis JM, Williams-Russo P, Knickman JR. The Case for More Active Policy Attention to Health Promotion. Health Affairs. 2002;21(2):78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- Miller W, Robinson LA, Lawrence RS. Valuing Health for Regulatory Cost-Effectiveness Analysis. Washington, DC: National Academies Press; 2006. Available at http://www.nap.edu/catalog/11534.html accessed June 5, 2009. [Google Scholar]
- Molla MT, Madans JH, Wagener DK, Crimmins EM. Summary Measures of Population Health: Report of Findings on Methodologic and Data Issues. Hyattsville, MD: National Center for Health Statistics; 2003. Available at http://www.cdc.gov/nchs/data/misc/pophealth.pdf accessed December 8, 2009. [Google Scholar]
- Molla MT, Wagener DK, Madans JH. Healthy People 2010, Statistical Notes. Hyattsville, Maryland: National Center for Health Statistics; 2001. Summary Measures of Population Health: Methods for Calculating Healthy Life Expectancy. Number 21. Available at http://www.cdc.gov/nchs/data/statnt/statnt21.pdf accessed December 8, 2009. [DOI] [PubMed] [Google Scholar]
- Moriarty DG, Zack MM, Gizlice Z, Klementiev AA. The Use of Healthy Days Measures in Health Expectancy Estimates. Presentation at the International Network on Health Expectancy (REVES), Guadalajara, Mexico, May 5–7. 2003.
- Murray CJL, Evans DB. Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva: World Health Organization; 2003. [Google Scholar]
- Murray CJL, Salomon JA, Mathers C. A Critical Examination of Summary Measures of Population Health. Bulletin of the World Health Organization. 2000;78(8):981–94. [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Salomon A, Mathers C, Lopez A. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) Behavioral Risk Factor Surveillance System. 2009. Available at http://www.cdc.gov/BRFSS/ accessed May 21, 2009. [Google Scholar]
- National Center for Health Statistics (NCHS) Mortality Data from the National Vital Statistics System. 2009. Available at http://www.cdc.gov/nchs/nvss.htm accessed December 8, 2009. [Google Scholar]
- Nelson E, Berwick D. The Measurement of Health Status in Clinical Practice. Medical Care. 1989;27:S77–S90. doi: 10.1097/00005650-198903001-00007. [DOI] [PubMed] [Google Scholar]
- National Priorities Partnership. National Priorities and Goals: Aligning Our Efforts to Transform America's Healthcare. Washington, DC: National Quality Forum; 2008. Available at http://www.nationalprioritiespartnership.org/uploadedFiles/NPP/08-253-NQF%20ReportLo%5B6%5D.pdf accessed December 8, 2009. [Google Scholar]
- National Technical Information Service (NTIS) Social Security Administration's Death Master File. 2009. Available at http://www.ntis.gov/products/ssa-dmf.aspx accessed May 18, 2009. [Google Scholar]
- Nusselder WJ, Looman CW, Mackenbach JP, Huisman M, van Oyen PH, Deboosere P, Gadeyne S, Kunst AE. The Contribution of Specific Diseases to Educational Disparities in Disability-Free Life Expectancy. American Journal of Public Health. 2005;95(11):2035–41. doi: 10.2105/AJPH.2004.054700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusselder WJ, Looman CW, Marang-van de Mheen PJ, van de Mheen H, Mackenbach JP. Smoking and the Compression of Morbidity. Journal of Epidemiology and Community Health. 2000;54:566–74. doi: 10.1136/jech.54.8.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusselder WJ, Peeters A. Successful Aging: Measuring the Years Lived with Functional Loss. Journal of Epidemiology and Community Health. 2006;60:448–55. doi: 10.1136/jech.2005.041558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office for National Statistics (ONS) Life Expectancy at Birth for Wards in England and Wales, 1999–2003 (Experimental Statistics) 2006. Available at http://www.statistics.gov.uk/downloads/theme_health/Ward_LE_report.pdf accessed May 18, 2009. [Google Scholar]
- Oortwijn W, Mathijssen J, Lankhuizen M, Cave J. Evaluating the Uptake of the Healthy Life Years Indicator—Final Report. 2006. RAND Europe. Available at http://ec.europa.eu/health/ph_information/indicators/docs/RAND_HLY_en.pdf accessed June 5, 2009. [Google Scholar]
- REVES. About REVES. 2007. Available at http://reves.site.ined.fr/en/home/about_reves/ accessed May 18, 2009. [Google Scholar]
- REVES. The Sullivan Method. 2008a. calculations using online spreadsheet. Available at http://reves.site.ined.fr/en/resources/computation_online/sullivan/ accessed June 14, 2009. [Google Scholar]
- REVES. What Are Health Expectancies? 2008b. Available at http://reves.site.ined.fr/en/DFLE/definition/ accessed May 20, 2009. [Google Scholar]
- Robert Wood Johnson Foundation (RWJF) UW Population Health Institute Awarded $4.9 Million by the Robert Wood Johnson Foundation to Mobilize Community Health Improvement Nationwide. 2009. Available at http://www.rwjf.org/pr/product.jsp?id=38048 accessed May 23, 2009. [Google Scholar]
- Robine J-M, Jagger C. Strategic Plan of the Task Force on Health Expectancies, 2007–2010. 2007. EU's Task Force on Health Expectancies. Available at http://www.tf-he.eu/Strategic_Plan_Final.pdf accessed December 21, 2009. [Google Scholar]
- Robine J-M, Jagger C, Mathers C, Crimmins E, Suzman R. Determining Health Expectancies. Chichester: Wiley; 2003. [Google Scholar]
- Smith M, Edgar G, Groom G. Health Expectancies in the United Kingdom, 2004–2006. Office for National Statistics. Health Statistics Quarterly. 2008;40:77–80. [PubMed] [Google Scholar]
- Southerland JM, Fisher E, Skinner JS. Getting Past Denial—The High Cost of Health Care in the United States. New England Journal of Medicine. 2009;361(13):1227–30. doi: 10.1056/NEJMp0907172. [DOI] [PubMed] [Google Scholar]
- Sullivan DF. A Single Index of Mortality and Morbidity. HSMHA Health Reports. 1971;86(4):347–54. Available at http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1937122&blobtype=pdf accessed May 20, 2009. [PMC free article] [PubMed] [Google Scholar]
- Toson B, Baker A. National Statistics Methodological Series 33. 2003. Life Expectancy at Birth: Methodological Options for Small Populations. Available at http://www.statistics.gov.uk/statbase/Product.asp?vlnk=10626 December 8, 2009. [Google Scholar]
- United Health Foundation, the American Public Health Association, and the Partnership for Prevention. America's Health Rankings. 2009. Available at http://www.americashealthrankings.org/2009/report/AHR2009%20Final%20Report.pdf accessed December 21, 2009. [Google Scholar]
- U.S. Census Bureau. American Community Survey. 2009. Available at http://www.census.gov/acs/www/ accessed May 23, 2009. [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Healthy People 2010: Executive Summary. 2009a. Available at http://www.healthypeople.gov/data/midcourse/html/execsummary/Goal1.htm accessed May 20, 2009. [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Healthy People 2020: The Road Ahead. 2009b. Available at http://www.healthypeople.gov/HP2020/ accessed May 23, 2009. [Google Scholar]
- Utah Office of Public Health Assessment. Utah BRFSS Brief: Years of Healthy Life in Utah. 2002. Office of Public Health Assessment, Center for Health Data, July. Available at http://health.utah.gov/opha/publications/brfss/briefs/0207_Healthy_Life.pdf accessed May 20, 2009. [Google Scholar]
- World Health Organization (WHO) World Health Statistics 2009. 2009. Available at http://www.who.int/whosis/whostat/EN_WHS09_Full.pdf accessed May 31, 2009. [Google Scholar]