Abstract
Little is known regarding the potential risk posed by aerosolized prions. Chronic wasting disease (CWD) is transmitted horizontally, almost surely by mucosal exposure, and CWD prions are present in saliva and urine of infected animals. However, whether CWD may be transmissible by the aerosol or nasal route is not known. To address this question, FVB mice transgenetically expressing the normal cervid PrPC protein [Tg(cerPrP) mice] were exposed to CWD prions by either nose-only aerosol exposure or by drop-wise instillation into the nostrils. Mice were monitored for signs of disease for up to 755 days post-inoculation (p.i.) and by examination of tissues for lesions and PrPCWD after necropsy. In particular, nasal mucosa, vomeronasal organ, lungs, lymphoid tissue and the brain were assessed for PrPCWD by Western blotting and immunohistochemistry. Six of seven aerosol-exposed Tg(cerPrP) mice developed clinical signs of neurological dysfunction mandating euthanasia between 411 and 749 days p.i. In all these mice, CWD infection was confirmed by detection of spongiform lesions and PrPCWD in the brain. Two of nine intranasally inoculated Tg(cerPrP) mice also developed transmissible spongiform encephalopathy associated with PrPCWD between 417 and 755 days p.i. No evidence of PrPCWD was detected in CWD-inoculated Tg(cerPrP) mice examined at pre-terminal time points. These results demonstrate that CWD can be transmitted by aerosol (as well as nasal) exposure and suggest that exposure via the respiratory system merits consideration for prion disease transmission and biosafety.
INTRODUCTION
Chronic wasting disease (CWD) is an efficiently transmitted prion disease [transmissible spongiform encephalopathy (TSE)] affecting deer, elk and moose. Although discovered in Northern Colorado and Southern Wyoming, CWD has since been identified in 13 additional states, three Canadian providences and Korea (Dube et al., 2006; http://wildlifedisease.nbii.gov/documents/update%2094.pdf, 2009; Kim et al., 2005). CWD is unique as the only TSE that occurs in wild animal populations.
Available information indicates that CWD is transmitted by some horizontal means, most likely involving trans-mucosal entry (Miller & Williams, 2003; Sigurdson et al., 1999; Williams, 2005). CWD prions are known to be present in saliva and urine of infected cervids (Haley et al., 2009; Mathiason et al., 2006) and excreted prions can contaminate the environment and persist for years, given that clay components of soil bind prion proteins with high affinity (Johnson et al., 2006). Exposure of the nasal or other respiratory mucosa via aerosolization or direct contact to CWD prions is sufficient to initiate infection and disease remains unproven, yet plausible. Precedent for nasal transmission of prion disease can be found in studies of experimental scrapie in sheep and mice and transmissible mink encephalopathy (TME) in hamsters (Hamir et al., 2008; Kincaid & Bartz, 2007; Sbriccoli et al., 2008).
Olfactory sensory nerve endings in the olfactory epithelium (Buck & Axel, 1991) of animals such as cervids are highly developed to monitor the environment, e.g. to locate food, predators and prey, and detect the pheromones initiating reproductive behaviours (Dulac, 2000; Thorne & Amrein, 2003). Reproductive cues in particular are detected by the Flehmen response that draws the trapped particulates into the vomeronasal organ (VNO), a specialized neurosensory region in the anterior nasal mucosa (Doving & Trotier, 1998). The Flehmen response and social nuzzling both provide opportunities for CWD prions to enter the nasal passages.
To determine directly whether CWD is transmissible by the respiratory route, cervid PrP-expressing transgenic mice [Tg(CerPrP) mice] were exposed to CWD prions by aerosolization or intranasal (IN) instillation. We present evidence that exposure of the respiratory mucosa to CWD prions is sufficient to transmit the disease after long incubation periods.
RESULTS
Intracerebral (IC) exposure
All IC-inoculated mice exhibited clinical symptoms of CWD at 168±4 days post-inoculation (p.i.) and were euthanized. PrPCWD was detected in all positive controls by Western blot (WB) and immunohistochemistry (IHC), thus confirming the infectivity of the inoculum (data not shown).
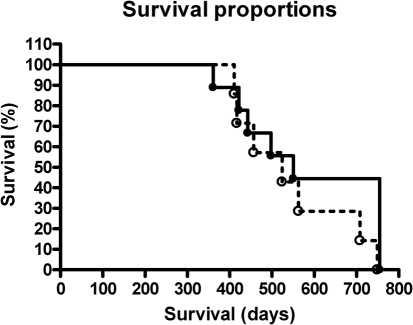
Aerosol exposure
In our first aerosol exposure of Tg(cerPrP) mice, four of six CWD and three of six sham-exposed mice died within 0–6 days p.i. The cause of death was not determined with certainty. After modification to the exposure protocol no similar fatalities occurred. Of a total of the seven mice exposed to CWD by aerosol, six developed TSE between 411 and 749 days p.i. None of the sham-inoculated mice developed evidence of prion infection through 749 days p.i. of observation. Neurological signs, survival times, weight loss and development of TSE lesions (primarily neuronal loss/vacuolation and gliosis) within the brain for the aerosol-exposed mice are summarized in Table 1 and Fig. 1(a).
Table 1.
Aerosol transmission of CWD in Tg(cerPrP) mice
+, Present; − not present.
| Animal no. | Neurological signs* | Survival (days p.i.) | Weight loss (% max. body wt) | PrPCWD WB | PrPCWD IHC | TSE lesions |
|---|---|---|---|---|---|---|
| Sham n=5 | − | 411–749 | 2 (average) | − | − | − |
| 384 | + | 411 | 31 | + | + | + |
| 746 | + | 417 | 32 | + | + | + |
| 739 | + | 457 | 35 | − | − | − |
| 732 | + | 524 | 27 | + | + | + |
| 734 | + | 563 | 31 | + | + | + |
| 738 | − | 708 | 11 | − | + | − |
| 380 | + | 749 | 12 | + | + | + |
*Animals were considered positive if they exhibited at least three of the following symptoms: ataxia, lethargy, tremors, weight loss, poor coat quality or rigid tail.
Fig. 1.
Kaplan–Meier survival plot of Tg(CerPrP) mice exposed to CWD by aerosol (○, black dotted line) versus IN instillation (•, black solid line).
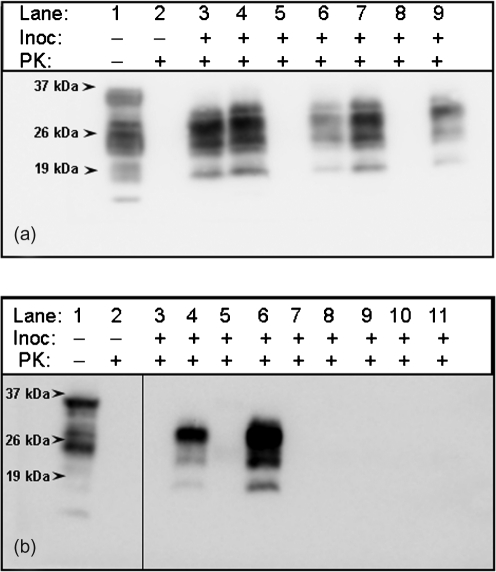
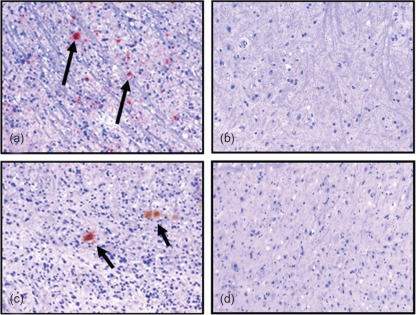
WB and IHC analysis of brains from the seven CWD-aerosol-exposed mice demonstrated PrPCWD in six of them (Figs 2a and 3a). All of the mice exposed by aerosol to CWD-negative control deer brain inoculum were negative for PrPCWD by WB (Fig. 2a, lanes 1 and 2) and IHC (Fig. 3b). IHC of the nasal passages, including the VNO, olfactory and respiratory epithelium, and nasal-associated lymphoid tissue (NALT), as well as the olfactory bulb of the brain and spleen, did not reveal PrPCWD (data not shown).
Fig. 2.
(a) PrPCWD (lanes 3, 4, 6, 7 and 9) in brains of Tg(CerPrP) mice exposed to aerosolized CWD prions demonstrated by WB. Aerosolized sham control (lanes 1 and 2) showing no PrPCWD. (b) PrPCWD (lanes 4 and 6) in brains of Tg(CerPrP) mice exposed to CWD prions intranasally demonstrated by WB. Intranasal sham control (lanes 1 and 2) showing no PrPCWD.
Fig. 3.
IHC from the obex region of the medulla from Tg(CerPrP) mice (×20 magnification). (a) PrPCWD (arrows) in a mouse exposed to CWD by aerosol versus (b) mouse exposed to sham inoculum. (c) Mouse exposed to CWD by IN route demonstrating PrPCWD aggregates (arrows) versus (d) mouse exposed intranasally to sham inoculum.
IN exposure
Nine of 12 Tg(cerPrP) mice exposed to CWD by IN inoculation survived past 250 days p.i. Two of these nine mice developed TSE at 422 and 498 days p.i., respectively. A summary of neurological signs, survival times, weight loss and development of TSE lesions (primarily neuronal loss/vacuolation and gliosis) is in Table 2 and Fig. 1(b). Both IN-inoculated mice that developed TSE had PrPCWD accumulation in the brain, as detected by WB (Fig. 2b, lanes 4 and 6) and IHC (Fig. 3c). None of the mice exposed intranasally to CWD-negative control deer brain inoculum displayed clinical signs of CWD. All were negative for PrPCWD by WB (Fig. 2b, lanes 1 and 2) and IHC (Fig. 3d). In none of the negative control or CWD-inoculated mice sacrificed at planned time points or dying spontaneously was evidence of PrPCWD or histopathologic lesions of TSE detected (data not shown). PrPCWD was also not detected in the nasal passages, olfactory bulb or spleen of any mice (data not shown).
Table 2.
IN transmission of CWD in Tg(cerPrP) mice
+, Present; − not present.
| Animal no. | Neurological signs* | Survival (days p.i.) | Weight loss (% max. body wt) | PrPCWD WB | PrPCWD IHC | TSE lesions |
|---|---|---|---|---|---|---|
| Sham n=9 | − | 361–755 | 5 (average) | − | − | − |
| 635 | + | 361 | 39 | − | − | − |
| 641 | + | 422 | 43 | + | + | + |
| 646 | + | 443 | 50 | − | − | − |
| 631 | + | 498 | 17 | + | + | + |
| 633 | − | 551 | +14 | − | − | − |
| 630 | − | 755 | 23 | − | − | − |
| 632 | − | 755 | 15 | − | − | − |
| 645 | − | 755 | 19 | − | − | − |
| 648 | − | 755 | 35 | − | − | − |
*Animals were considered positive if they exhibited at least three of the following symptoms: ataxia, lethargy, tremors, weight loss, poor coat quality or rigid tail.
Statistical analysis
Using the Fisher's exact test, the attack rates in Tg(CerPrP) mice exposed to CWD by aerosol versus nasal inoculation were demonstrated as being significantly different (Fisher's exact test, P-value=0.0406).
Dose estimations
To estimate the quantity of brain material delivered per mouse by aerosol exposure, we used lognormal distribution generator assumptions and calculations as described in Methods. Based on particle sizes ranging from 0.1 to 10 μm (log distribution) generated by the nebulizer, we estimated that 24 μg of solid brain material was deposited on the mucous membranes of each mouse. Applying the same algorithm to IN exposure produces an estimated value of 100 μg of brain material delivered per mouse.
DISCUSSION
In 1995, Shaw (1995) suggested that the occurrence of a shorter incubation period for Creutzfeldt–Jakob disease (CJD) in farmers could have come from ‘breathing the dust from feed containing prion’. The present studies were done to simulate the inhalation of airborne particles and the direct contamination of the nasal passages with CWD prions. The finding that CWD prions can be transmitted via inhalation (perhaps even more effectively than by nostril contact only), while unique for CWD infection, extends precedent for transmission of prions via the respiratory system. Sheep and hamsters inoculated with scrapie intranasally (Hamir et al., 2008; Sbriccoli et al., 2008) and hamsters inoculated with TME extranasally (Kincaid & Bartz, 2007) have been shown to develop TSE. Results in the latter study suggested that the nasal passages may even be more effective than the oral route in transmitting prion disease (Kincaid & Bartz, 2007).
In the present study, 86 % (six of seven) of Tg(cerPrP) mice exposed to CWD via aerosol developed CWD versus 22 % (two of nine) of IN-exposed mice (Fisher's exact test, P-value=0.0406). It may be argued that the early deaths of four mice in the initial CWD-aerosol exposure group could bias the statistical significance of the results. After modifications to the exposure procedure, early mortalities were eliminated. Moreover, two of two surviving mice in the initial exposure and four of five mice in the second exposure study developed TSE.
One possible explanation for the enhanced infectivity after aerosol exposure might be the disruption and dispersion of infectious PrPCWD aggregates during aerosolization to yield more small infectious particles or seeds (Silveira et al., 2005). These smaller aggregates might be more readily taken up by lymphoid or distal airway epithelial cells not typically accessible by either nasal contact or drop-wise instillation of prions.
Another potential explanation for enhanced infection after aerosolization could be that a larger prion dosage was delivered by aerosol versus nasal exposure. Based on a random distribution of infectivity in the aerosol material, the respiratory tidal volume of mice and the average anaesthetized respiratory rate for a 4 min period, we calculated that aerosol-exposed mice would receive approximately 1.2 % of the available inoculum, or a maximum of 24 μg of particulate inoculum deposited in the respiratory system. Mice inoculated intranasally received 10 μl of a 10 % brain homogenate or 100 μg of particulate inoculum – four times that delivered by aerosol. Given that only the nostril region (<5 mm) of each mouse was exposed during aerosolization, we estimate that even if up to an additional 15 μl of inoculum were to be ingested due to nasal region grooming, the total dosage would not surpass (and more likely would never attain) that delivered intranasally.
Clearly, inoculation by either the aerosol or nasal route would result in inoculum entering the alimentary tract via the nasopharynx. Thus, oral exposure and potential uptake cannot be avoided or excluded. However, oral inoculation of Tg(cerPrP) mice with 100 μg CWD particulate brain homogenate failed to transmit CWD infection or disease after >700 days of observation (D. M. Seelig, G. L. Mason, G. C. Telling & E. A. Hoover, unpublished results) (Table 3). Thus, it is unlikely that CWD transmission by the aerosol or nasal routes reflects infection via the alimentary tract.
Table 3.
Summary of CWD inoculation results in Tg(cerPrP) mice
| Route | Exposure dose | Attack rate* |
|---|---|---|
| Aerosol | 24 μg† | 6/7 (86 %) |
| IN | 100 μg‡ | 2/9 (22 %) |
| Oral | 100 μg§ | 0/10 (0 %) |
*No. affected/no. total (% positive).
†4 min aerosol of 5 % (w/v) homogenate.
‡10 μl of 10 % (w/v) homogenate.
§100 μl of 1 % (w/v) homogenate.
Mice are an excellent model for studying airborne and direct nasal contact transmissions because they are obligate nasal breathers (Klemens et al., 2005). Odorants and particles inhaled into the nasal passage are subject to a number of cell surfaces. Thus, multiple sites of CWD prion entry are plausible, including the NALT, the mucosal associated macrophages and/or dendritic cells, respiratory epithelium, olfactory epithelium and VNO. The NALT typically incorporates the retropharyngeal lymph nodes, palatine and lingual tonsil (Kuper et al., 1992) and is similar in structure and function to the gut-associated lymphoid tissue (GALT) in that it is responsible for antigen uptake and presentation by M cells, B cells and follicular dentritic cells (Heritage et al., 1997; Kuper et al., 1992). The GALT, especially the Peyer's patches, is considered to be the primary site of PrPSc uptake for BSE, variant CJD and scrapie (Beekes & McBride, 2000; Fox et al., 2006; Heggebo et al., 2002; Press et al., 2004; Spraker et al., 2002b; van Keulen et al., 2008).
Mice do not have tonsils or retropharyngeal lymph nodes per se, but rather a bi-symmetrical NALT structure that lines the floor of the nasal cavity (Heritage et al., 1997). Kincaid & Bartz (2007) found that hamsters inoculated via uptake of droplets of TME inoculum via the external nares had shorter incubation periods using a lower dose of infectious prions than those inoculated orally. Studies in deer inoculated orally or naturally exposed to CWD indicate that the primary structures that accumulate PrPCWD early in infection are the retropharyngeal lymph nodes and tonsils (Keane et al., 2008; Sigurdson et al., 1999; Spraker et al., 2004). Nevertheless, in the present study we were unable to demonstrate PrPCWD in the NALT of early, pre-terminal or terminal Tg(cerPrP) mice after aerosol or nasal exposure to CWD.
Another seemingly probably site for prion entry and infection is the olfactory mucosal epithelium, which contains odour receptors that provide a direct neural connection from the nasal cavity to the olfactory bulbs of the brain. Previous IHC studies of deer terminally infected with CWD have demonstrated PrPCWD depositions in the olfactory bulbs, which also show marked spongiform degenerative changes (Spraker et al., 1997, 2002b; Williams & Young, 1992, 1993). However, in deer, sequential PrPCWD accumulation in the brain appears to occur in a caudal (brainstem) to rostral (frontal cortex) fashion as the disease progresses (Spraker et al., 2002a). In the present study, PrPCWD was not detected in the olfactory bulbs of terminal CWD-infected Tg(cerPrP) mice, although aggregates were identified in the frontal cortex immediately dorsal to the olfactory bulbs in some mice. This was especially surprising since the olfactory bulb glomeruli are sites of substantial cervid PrPC expression in naïve Tg(cerPrP) mice.
Given that CWD prions have been demonstrated in saliva (Mathiason et al., 2006), urine (Haley et al., 2009; Kariv-Inbal et al., 2006) and soil (Johnson et al., 2006), it is possible that prion entry could involve the VNO – a region of the anterior ventral nasal passages specialized to detect non-volatile molecules such as pheromones by a process known as the Flehmen response (Thorne & Amrein, 2003; Kelliher et al., 2001; Meredith & O'Connell, 1979). Nevertheless, neither we nor DeJoia et al. (2006) were able to detect PrPRES in the VNO of terminal CWD-inoculated Tg(cerPrP) mice or TME-inoculated hamsters, respectively. Thus, while all of the above exposure studies failed to identify PrPCWD/RES in mucosal sites, it remains likely that early prion trafficking involves relatively few potential protease-sensitive oligomeric molecules, which may not be identifiable with the detection methods used.
Our inability to detect PrPCWD outside the central nervous system in the present studies was somewhat perplexing. This finding could reflect a more limited peripheral expression of PrPC expression in the Tg(cerPrP) mice versus deer, although other studies in our laboratory have demonstrated PrPC in many peripheral tissues of Tg(cerPrP) mice (D. M. Seelig, G. L. Mason, G. C. Telling & E. A. Hoover, unpublished results). Additionally, overfixation of our tissues could eliminate possible PrPCWD aggregates. An alternative explanation would be that TSE induced by nasal exposure to CWD prions in Tg(cerPrP) mice in mediated largely by non-lymphoreticular system pathways. Such a pathway is supported by the recent work of Bessen et al. (2009), demonstrating that IN inoculation of RML scrapie into immunodeficient transgenic mice transmits TSE without lymphoreticular system involvement.
In summary, the present study demonstrates the transmissibility of prions via aerosolization. Several aspects of respiratory transmission of CWD prions remain to be refined and no evidence of a peripheral or lymphoid phase of the infection was detected. The results suggest that prion exposure via the respiratory system merits consideration in prion transmission and biosafety.
METHODS
Tg(CerPrP) mice.
The cervid PrP-expressing transgenic mice and their susceptibility to CWD infection after IC inoculation have been described previously (Browning et al., 2004). All mice were cared for in accordance with the Colorado State University ACUC guidelines. Confirmation of the cervid PrPC gene insert was performed by WB and PCR. The Tg(cerPrP) mice were five to 12 weeks of age at inoculation. After inoculation, mice were examined for evidence of neurological abnormality every 2 days, and weighed weekly (starting at 3 months p.i.). Clinical criteria for assessing CWD symptoms included ataxia, lethargy, tail rigidity, poor coat quality and weight loss. Once the onset of clinical signs was observed, mice were isolated into individual cages to prevent cannibalism from cage mates. Mice were euthanized when distinct signs of neurological disease were evident. CWD- and sham-inoculated mice were housed in separate rooms to minimize the potential of cross contamination.
Inocula and inoculation routes.
The CWD inoculum consisted of brain homogenate from CWD-infected mule deer (D10), obtained through the courtesy of Dr Michael Miller, Colorado Division of Wildlife, USA. CWD-negative (sham) control brain homogenate was from a CWD-naïve white-tailed deer brain (UGA) obtained through the courtesy of Drs David Osborn, Carl Miller and Robert Warren at the University of Georgia Warnell School of Forestry, USA. Brain homogenates were prepared in 1× PBS to a final concentration of 10 % (w/v) for IN, 5 % (w/v) for aerosol and 1 % for IC and per os (PO) inoculations. All mice (except IC and PO) were administered 0.01 ml epinephrine intraperitoneally, immediately p.i. to stimulate the Flehmen response.
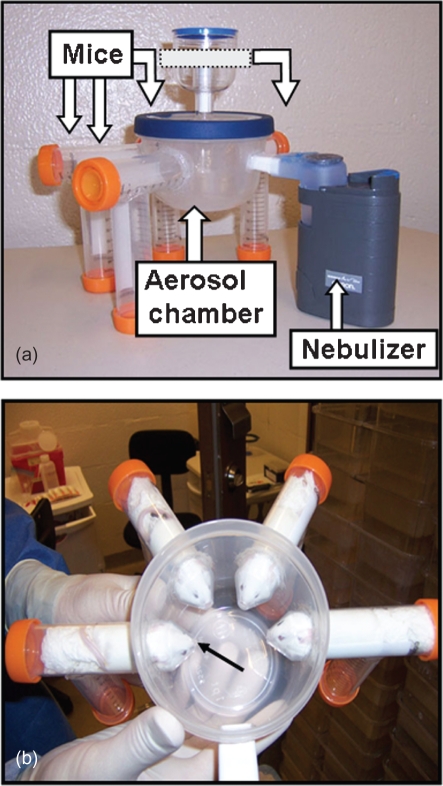
In two separate experiments, two cohorts of Tg(CerPrP) mice (n=6 CWD and n=6 sham) were inoculated by exposure to an aerosol of 5 % (w/v) CWD brain homogenate for 4 min in a custom designed chamber providing nose-only exposure. The mice were monitored until clinical symptoms were detected or until study termination at 749 days. Two additional cohorts of Tg(CerPrP) mice (n=24 CWD and n=24 sham) were inoculated with 10 μl (5 μl per nostril) of the 10 % weight to volume (w/v) extracts by direct pipette instillation into the nasal passages. A total of 12 mice in each cohort (n=4 per time point) were sacrificed at 7, 14 and 28 days p.i. and analysed for early PrPCWD detection. The remaining mice (12 per cohort) were monitored either until clinical symptoms became apparent or to study termination at 755 days. Per os inoculations into Tg(CerPrP) mice were administered in 2–50 μl doses of a 1 % extract given on two consecutive days. IC inoculations into Tg(CerPrP) mice of 30 μl of a 1 % extract from the same positive mule deer (D10) or naïve white-tailed deer (UGA) served as positive and negative controls.
Aerosolizing chamber.
Aerosolizing chambers commonly expose the entire animal to the agent being investigated. Our goal was to expose only the nose/nasal passages to CWD prions versus the entire animal. Thus, we (N. D. D./J. H. K.) fashioned an exposure chamber using a 473 ml, rubber-sealed lid container (Rubbermaid) into which 4–1′ diameter holes were drilled into the side walls. Four, 50 ml conical tubes (BD) with the tips removed were inserted and sealed into the holes. Each tube was supported by an additional tube that collectively functioned as legs. A 3/4′×1/2′ hole was also cut into the container to accommodate the mouth of the Omron Nebulizer (Ultranebs). The conical tubes and the nebulizer were sealed in place with silicone adhesive (GOOP). Finally, a 0.22 μm filter unit (Sterivex; Millipore) was attached and sealed to the lid of the container to serve as an air vent and trap aerosolized particles (Fig. 4a). After the mice and the inocula had been loaded into the apparatus (Fig. 4b), the entire chamber was placed in a secondary enclosure and exposure occurred in a separately vented room.
Fig. 4.
(a) Aerosolizing chamber with nebulizer chamber and four plastic enclosures to accommodate anaesthetized Tg(CerPrP) mice. (b) Top view of aerosol chamber with lid removed showing Tg(CerPrP) mice inserted in place to provide nose-only exposure to the chamber (arrow).
Statistical analysis.
Statistics (Fisher's exact test) were performed using the software package Graphpad Prism 4.
Delivered dose estimations.
To approximate the total solid mass of brain inoculum deposited onto the mucous membranes of each aerosol-exposed mouse, we used a lognormal distribution generator program created by Dr J. Volckens (Department of Environmental and Radiological Health Sciences, Colorado State University, USA), using modified equations (Hinds, 1999) for aerosolized particles. Using particle sizes generated by the nebulizer of 0.1–10 μm (log distribution), the estimated number of particles per each size generated and a designated mass for each particle size, the total mass for each particle size was calculated. The total mass was then multiplied by a deposition fraction (percentage of particles deposited in the respiratory tract based on size) and the fraction of total air inhaled by each mouse {1.2 %; [mouse respiration rate (163) multiplied by tidal volume (0.00015 L)]/air flow through the system (2 lpm)]} to give the total deposited particle mass. Using a 5 % brain homogenate, with brain material containing approximately 10 % solid material, we calculated the mass fraction of solids per particle to be 0.005 g (0.05×0.10). This fraction multiplied by the total deposited particle mass for each particle size produced the total mass of solid material deposited. The sums from each particle size deposited mass were then added to generate the total amount of solid inocula deposited into each mouse.
Similar algorithms were used to estimate the total amount of solid inoculum deposited into each intranasally inoculated mouse based on 10 μl of a 10 % brain homogenate.
Western blotting.
Harvested tissues were prepared at 10 % (w/v) in a 1× PBS/1 % Triton X-100 mixture. Glass beads (2.5 mm; Biospec) were added to each tube and samples subjected to one Fastprep (Biosalvant) cycle for 45 s at a speed setting of 5.5, followed by a 2 min cool down at −20 °C. Samples were then centrifuged for 5 min at 2000 r.p.m. (F241.5P Microfuge Fixed-Angle Polypropylene rotor) to remove tissue debris and supernatants stored at −20 °C until further use.
Samples were incubated with 50 mg Proteinase K (Invitrogen) μl−1 for 30 min at 37 °C, shaking at 1000 r.p.m. Samples were then combined with a Reducing Agent/Sample Buffer (Invitrogen) to a final concentration of 1× and run through NuPage 10 % Bistris gels (Invitrogen) for 2.5 h at 100 V. Proteins were then transferred to 0.22 μm PVDF membranes (Millipore) over 1.5 h at a setting of 110 V. Membranes were blocked in a casein/TBS (Thermo Scientific)+0.2 % Tween-20 mixture for 45 min, with shaking at room temperature. Monoclonal antibody BAR-224 (Spi-Bio) conjugated with HRP was used to detect the PrPCWD (1 : 20 000 dilution in casein/TBS+0.2 % Tween-20). Membranes were washed three times and developed with ECL Plus Western blotting Detection kit (GE). Blots were viewed and photographed with a Gel Doc system (LAS-3000; Fujifilms).
IHC.
Tissues were fixed in 10 % formalin for 5 days, transferred to 60 % ethanol (with the exception of the nasal passages), embedded in paraffin and sectioned at 5 μm for staining. Nasal tissues were placed in a 10 % tetra-sodium EDTA (Sigma) solution for 10 days, with a fresh solution change occurring on the fifth day. Slides were de-paraffined through a series of xylene/ethanol baths, treated in 89 % formic acid for 30 min, rinsed in running water for 5 min and then subjected to a 15 min antigen-retrieval process (Pickcell Laboratories). The Dako Autostainer was used for conventional IHC. Briefly, slides were blocked with 3 % H2O2 in methanol (30 min), blocked with TNB buffer (30 min), incubated with a 1 : 250 dilution of HRP-conjugated BAR-224 in TNB (45 min), developed with chromagen AEC (3-amino-9-ethylcarbazole; Dako) (10 min), and counterstained with haematoxylin (5 min) and bluing reagent (1 min). Both H&E and IHC sections were evaluated for the presence of TSE lesions, which were characterized by neuronal loss, spongiform change and gliosis.
Acknowledgments
This work was supported by NIH/NIAID contract NOI-AI-25491 (E. A. H., G. C. T.), NIH/NCRR grant T32-RR-07072 (D. M. S.), the Stephen G. and Susan E. Denkers Family Foundation (N. D. D.), USDA CSREES training grant 2005-38420-15813 (N. D. D.) and NIH RO1-NS-040334 (G. C. T.). Special thanks to Jeanette Hayes-Klug for her assistance in the design of the aerosol chamber and for care of the transgenic mice. We thank Candace Mathiason and Matthew Perrott for advice and assistance with several aspects of the work. We thank Dr John Volckens for his expertise in aerosolized particle distribution and computations.
References
- Beekes, M. & McBride, P. A. (2000). Early accumulation of pathological PrP in the enteric nervous system and gut-associated lymphoid tissue of hamsters orally infected with scrapie. Neurosci Lett 278, 181–184. [DOI] [PubMed] [Google Scholar]
- Bessen, R. A., Martinka, S., Kelly, J. & Gonzalez, D. (2009). Role of the lymphoreticular system in prion neuroinvasion from the oral and nasal mucosa. J Virol 83, 6435–6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning, S. R., Mason, G. L., Seward, T., Green, M., Eliason, G. A., Mathiason, C., Miller, M. W., Williams, E. S., Hoover, E. & Telling, G. C. (2004). Transmission of prions from mule deer and elk with chronic wasting disease to transgenic mice expressing cervid PrP. J Virol 78, 13345–13350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck, L. & Axel, R. (1991). A novel multigene family may encode odorant receptors: a molecular basis for odor recognition. Cell 65, 175–187. [DOI] [PubMed] [Google Scholar]
- DeJoia, C., Moreaux, B., O'Connell, K. & Bessen, R. A. (2006). Prion infection of oral and nasal mucosa. J Virol 80, 4546–4556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doving, K. B. & Trotier, D. (1998). Structure and function of the vomeronasal organ. J Exp Biol 201, 2913–2925. [DOI] [PubMed] [Google Scholar]
- Dube, C., Mehren, K. G., Barker, I. K., Peart, B. L. & Balachandran, A. (2006). Retrospective investigation of chronic wasting disease of cervids at the Toronto Zoo, 1973–2003. Can Vet J 47, 1185–1193. [PMC free article] [PubMed] [Google Scholar]
- Dulac, C. (2000). Sensory coding of pheromone signals in mammals. Curr Opin Neurobiol 10, 511–518. [DOI] [PubMed] [Google Scholar]
- Fox, K. A., Jewell, J. E., Williams, E. S. & Miller, M. W. (2006). Patterns of PrPCWD accumulation during the course of chronic wasting disease infection in orally inoculated mule deer (Odocoileus hemionus). J Gen Virol 87, 3451–3461. [DOI] [PubMed] [Google Scholar]
- Haley, N. J., Seelig, D. M., Zabel, M. D., Telling, G. C. & Hoover, E. A. (2009). Detection of CWD prions in urine and saliva of deer by transgenic mouse bioassay. PLoS One 4, e4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamir, A. N., Kunkle, R. A., Richt, J. A., Miller, J. M. & Greenlee, J. J. (2008). Experimental transmission of US scrapie agent by nasal, peritoneal, and conjunctival routes to genetically susceptible sheep. Vet Pathol 45, 7–11. [DOI] [PubMed] [Google Scholar]
- Heggebo, R., Press, C. M., Gunnes, G., Gonzalez, L. & Jeffrey, M. (2002). Distribution and accumulation of PrP in gut-associated and peripheral lymphoid tissue of scrapie-affected Suffolk sheep. J Gen Virol 83, 479–489. [DOI] [PubMed] [Google Scholar]
- Heritage, P. L., Underdown, B. J., Arsenault, A. L., Snider, D. P. & McDermott, M. R. (1997). Comparison of murine nasal-associated lymphoid tissue and Peyer's patches. Am J Respir Crit Care Med 156, 1256–1262. [DOI] [PubMed] [Google Scholar]
- Hinds, W. C. (1999). Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. New York: Wiley Interscience.
- Johnson, C. J., Phillips, K. E., Schramm, P. T., McKenzie, D., Aiken, J. M. & Pedersen, J. A. (2006). Prions adhere to soil minerals and remain infectious. PLoS Pathog 2, e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariv-Inbal, Z., Ben-Hur, T., Grigoriadis, N. C., Engelstein, R. & Gabizon, R. (2006). Urine from scrapie-infected hamsters comprises low levels of prion infectivity. Neurodegener Dis 3, 123–128. [DOI] [PubMed] [Google Scholar]
- Keane, D. P., Barr, D. J., Keller, J. E., Hall, S. M., Langenberg, J. A. & Bochsler, P. N. (2008). Comparison of retropharyngeal lymph node and obex region of the brainstem in detection of chronic wasting disease in white-tailed deer (Odocoileus virginianus). J Vet Diagn Invest 20, 58–60. [DOI] [PubMed] [Google Scholar]
- Kelliher, K. R., Baum, M. J. & Meredith, M. (2001). The ferret's vomeronasal organ and accessory olfactory bulb: effect of hormone manipulation in adult males and females. Anat Rec 263, 280–288. [DOI] [PubMed] [Google Scholar]
- Kim, T. Y., Shon, H. J., Joo, Y. S., Mun, U. K., Kang, K. S. & Lee, Y. S. (2005). Additional cases of chronic wasting disease in imported deer in Korea. J Vet Med Sci 67, 753–759. [DOI] [PubMed] [Google Scholar]
- Kincaid, A. E. & Bartz, J. C. (2007). The nasal cavity is a route for prion infection in hamsters. J Virol 81, 4482–4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemens, J. J., Kirtsreesakul, V., Luxameechanporn, T. & Naclerio, R. M. (2005). Acute bacterial rhinosinusitis causes hyperresponsiveness to histamine challenge in mice. Arch Otolaryngol Head Neck Surg 131, 905–910. [DOI] [PubMed] [Google Scholar]
- Kuper, C. F., Koornstra, P. J., Hameleers, D. M., Biewenga, J., Spit, B. J., Duijvestijn, A. M., van Breda Vriesman, P. J. & Sminia, T. (1992). The role of nasopharyngeal lymphoid tissue. Immunol Today 13, 219–224. [DOI] [PubMed] [Google Scholar]
- Mathiason, C. K., Powers, J. G., Dahmes, S. J., Osborn, D. A., Miller, K. V., Warren, R. J., Mason, G. L., Hays, S. A., Hayes-Klug, J. & other authors (2006). Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 314, 133–136. [DOI] [PubMed] [Google Scholar]
- Meredith, M. & O'Connell, R. J. (1979). Efferent control of stimulus access to the hamster vomeronasal organ. J Physiol 286, 301–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, M. W. & Williams, E. S. (2003). Prion disease: horizontal prion transmission in mule deer. Nature 425, 35–36. [DOI] [PubMed] [Google Scholar]
- Press, C. M., Heggebo, R. & Espenes, A. (2004). Involvement of gut-associated lymphoid tissue of ruminants in the spread of transmissible spongiform encephalopathies. Adv Drug Deliv Rev 56, 885–899. [DOI] [PubMed] [Google Scholar]
- Sbriccoli, M., Cardone, F., Valanzano, A., Lu, M., Graziano, S., De Pascalis, A., Ingrosso, L., Zanusso, G., Monaco, S., Bentivoglio, M. & Pocchiari, M. (2008). Neuroinvasion of the 263K scrapie strain after intranasal administration occurs through olfactory-unrelated pathways. Acta Neuropathologica 117, 175–184. [DOI] [PubMed] [Google Scholar]
- Shaw, I. C. (1995). BSE and farmworkers. Lancet 346, 1365. [DOI] [PubMed] [Google Scholar]
- Sigurdson, C. J., Williams, E. S., Miller, M. W., Spraker, T. R., O'Rourke, K. I. & Hoover, E. A. (1999). Oral transmission and early lymphoid tropism of chronic wasting disease PrPres in mule deer fawns (Odocoileus hemionus). J Gen Virol 80, 2757–2764. [DOI] [PubMed] [Google Scholar]
- Silveira, J. R., Raymond, G. J., Hughson, A. G., Race, R. E., Sim, V. L., Hayes, S. F. & Caughey, B. (2005). The most infectious prion protein particles. Nature 437, 257–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spraker, T. R., Miller, M. W., Williams, E. S., Getzy, D. M., Adrian, W. J., Schoonveld, G. G., Spowart, R. A., O'Rourke, K. I., Miller, J. M. & Merz, P. A. (1997). Spongiform encephalopathy in free-ranging mule deer (Odocoileus hemionus), white-tailed deer (Odocoileus virginianus) and Rocky Mountain elk (Cervus elaphus nelsoni) in northcentral Colorado. J Wildl Dis 33, 1–6. [DOI] [PubMed] [Google Scholar]
- Spraker, T. R., Zink, R. R., Cummings, B. A., Sigurdson, C. J., Miller, M. W. & O'Rourke, K. I. (2002a). Distribution of protease-resistant prion protein and spongiform encephalopathy in free-ranging mule deer (Odocoileus hemionus) with chronic wasting disease. Vet Pathol 39, 546–556. [DOI] [PubMed] [Google Scholar]
- Spraker, T. R., Zink, R. R., Cummings, B. A., Wild, M. A., Miller, M. W. & O'Rourke, K. I. (2002b). Comparison of histological lesions and immunohistochemical staining of proteinase-resistant prion protein in a naturally occurring spongiform encephalopathy of free-ranging mule deer (Odocoileus hemionus) with those of chronic wasting disease of captive mule deer. Vet Pathol 39, 110–119. [DOI] [PubMed] [Google Scholar]
- Spraker, T. R., Balachandran, A., Zhuang, D. & O'Rourke, K. I. (2004). Variable patterns of distribution of PrPCWD in the obex and cranial lymphoid tissues of Rocky Mountain elk (Cervus elaphus nelsoni) with subclinical chronic wasting disease. Vet Rec 155, 295–302. [DOI] [PubMed] [Google Scholar]
- Thorne, N. & Amrein, H. (2003). Vomeronasal organ: pheromone recognition with a twist. Curr Biol 13, R220–R222. [DOI] [PubMed] [Google Scholar]
- van Keulen, L. J., Bossers, A. & van Zijderveld, F. (2008). TSE pathogenesis in cattle and sheep. Vet Res 39, 24. [DOI] [PubMed] [Google Scholar]
- Williams, E. S. (2005). Chronic wasting disease. Vet Pathol 42, 530–549. [DOI] [PubMed] [Google Scholar]
- Williams, E. S. & Young, S. (1992). Spongiform encephalopathies in Cervidae. Rev Sci Tech 11, 551–567. [DOI] [PubMed] [Google Scholar]
- Williams, E. S. & Young, S. (1993). Neuropathology of chronic wasting disease of mule deer (Odocoileus hemionus) and elk (Cervus elaphus nelsoni). Vet Pathol 30, 36–45. [DOI] [PubMed] [Google Scholar]