Abstract
Face field evaluation provides insights into the presence and location of the preferred retinal locus, as validated by comparisons with findings from microperimetry. This technique requires no special equipment and can be used in a clinic or at a person’s home by clinicians and low vision rehabilitation specialists.
Central scotomas from macular diseases, such as age-related macular degeneration (AMD), that necessitate the use of the eccentric retina have a major impact on reading, the recognition of faces, and the performance of other activities of daily living that require fine vision. Since the fovea is specialized for fine resolution and excellent visual acuity in a way that the peripheral retina is not, a person with a central scotoma must use magnification or large-print text. Likewise, with the loss of central vision, there is a drop in contrast sensitivity, and improved contrast and lighting are often required. However, the third important component in restoring optimal vision to a person with a central scotoma has not been as easy to quantify or address—the impact of having a blind spot in the central field of vision. If a person places what he or she wants to see at the location of the (now blind) fovea and within the scotomatous area, he or she will not be able to see it. If a person cannot establish a way to use the peripheral retina as a “pseudo-fovea” (Guez, Gargasson, Rigaudiere, & O’Regan, 1993; White & Bedell, 1990)—that is, to direct the object of interest to the eccentric preferred retinal locus (PRL) for fixation—the person will waste time and effort scanning, moving his or her head in all different directions, and having letters and words appear and disappear as they enter and emerge from the scotoma.
Some persons with central scotomas are able to adopt a regular and reliable fixation pattern; they look to the side or above the object of interest in a consistent way and thereby move the central scotoma out of the way. They may or may not be consciously aware of what they do, but they do it consistently. Other persons cannot seem to place the object of interest on the seeing retina regularly and, according to anecdotal evidence, have their visual acuity measured at levels that are far worse than one would expect from the observed retinal lesions. Most persons seem to fall in the middle; they have a PRL, but it is not strongly established. They may, for example, keep missing the first letters on the line in the acuity chart, implying that they are moving the scotoma to the left to read, but they do not compensate for this situation and may not do it consistently.
With the development of fundus perimeters (more commonly called microperimeters), such as the Rodenstock scanning laser ophthalmoscope (SLO) and the Nidek MP-1, the clinician can see the actual site of the PRL on the retina, evaluate how stable it is, and measure the size and location of the scotoma relative to the location of the PRL (Fletcher & Schuchard, 1997; Rohrschneider et al., 1995; Timberlake et al., 1986). Studies that have used microperimeters in geographic atrophy (GA) from AMD have shown that with the acquisition of a PRL over time, measured visual acuity can actually improve despite progressive enlargement of the atrophy (Sunness, Applegate, & Gonzalez-Baron, 2000). These microperimeters are the gold standard for characterizing the PRL and fixation pattern relative to the central scotoma and give the clinician or low vision provider an awareness of the PRL that can be strengthened through verbal coaching and specific exercises. However, microperimeters are not widely available; the Rodenstock SLO is no longer being manufactured, and the MP-1 costs about $48,000, so that most low vision providers do not have access to them.
Therefore, simpler inexpensive ways to assess fixation are desirable, particularly ways that can be used both in a clinic and at a person’s home, where low vision instruction may be taking place. It has long been recognized that, presumably because of perceptual completion (or “filling in”), more than 40% of persons with definite scotomas in their central visual field cannot detect them on an Amsler grid (Fine et al., 1986; Schuchard, 1993). In addition, despite an effort to be clear in the instructions to persons who use the grid, clinicians often do not know whether these persons are centering their fixation (using the corners of the grid, for example) at the fovea or whether they are using an eccentric PRL to fixate the center spot (Schuchard & Raasch, 1992). Even if a person reports an abnormality, it is difficult to interpret its location clearly. Conventional visual field testing that does not correct for eye movements cannot accurately measure the location of the PRL or the size of the scotoma (Sunness, Schuchard et al., 1995).
In examinations of persons with low vision, it is clear that they are aware of the blurring of facial features that is associated with their scotomas. It is easy and quick to do a “face field”—to map out where the blurred areas of the face are relative to fixation. As is described later, the face field is a much simpler and more familiar task than is using clock hours and numbers for looking for PRLs (Watson, 1999). To validate the face field technique, a retrospective study was performed of persons with central scotomas who, during a single visit, underwent first face fields and then SLO or MP-1 analysis.
Methods
TESTING PROCEDURE
As part of their low vision evaluations, I performed face fields on each patient in the study, as described next. All the patients with macular disease who had undergone both face fields and microperimetry and had scotomas in the central visual field were included in the analysis.
All the patients underwent low vision evaluations, in which their best-corrected visual acuity was measured and their near vision was assessed with a letter card and then the MNRead charts. During the acuity and reading testing, any behavior that was indicative of interference associated with a scotoma was recorded, including missing the first or last letters of a word or line, having difficulty determining where a new line began, and having difficulty reading words out of proportion to the letter acuity. Face fields were then administered, as described in Box 1. After the remainder of the examination was completed, an SLO or MP-1 evaluation was performed. I recorded in words the results of the face fields, along with any particular behavior that was indicative of a scotoma that I noted while the patient read the visual acuity chart or text. Imaging and fixation assessment was then performed with the SLO (acquired at the Greater Baltimore Medical Center, GBMC, in early 2005) or the Nidek MP-1 (acquired in early 2006). A list of all the SLO and MP-1 evaluations performed until September 2006 was obtained from the respective dedicated computers. All persons with macular disease who had undergone both face fields and microperimetry and had scotomas in the central visual field were included in the analysis.
Procedure for performing face fields
The examiner sits about 60 centimeters from the patient, with the examiner and patient at the same eye level.
The patient occludes one eye.
The examiner instructs the patient as follows: “Look at my nose so you can see it as clearly as possible.” (The examiner waits for a few seconds until the patient has done so and then continues.)
“While you are looking at my nose, I want you to tell me if there is part of my face that is missing or blurry or distorted.”
The patient describes what he or she sees. The examiner then records the patient’s description. For example, “the eyes are blurry, ” “the eye to the patient’s right is blurry, ” “the face to the patient’s left is blurry,” “the patient can see my nose, but my eyes and mouth are gone,” or “my whole face is blurred.”
The fellow eye is then tested.
This retrospective study protocol was approved by the GBMC institutional review board. The study adhered to the tenets of the Declaration of Helsinki.
MICROPERIMETRY AND IMAGING AND STATISTICAL METHODS
Using the fixation module of the SLO, I watched as the patient fixated the fixation cross, saved an image showing the location of the cross on the retina, and recorded my impression of the fixation behavior relative to the lesion and the fovea in a drawing or with words or both. Time limitations and the availability of the room precluded my routinely performing actual macular perimetry. Testing with the MP-1 provided a map of the stability and location of the fixation, as well as a map of the location and size of the dense scotoma.
JMP expert data analysis software (Cary, North Carolina) was used for most of the statistics presented in this article. The 95% confidence intervals were computed as described in Altman (1991). Phi coefficients were calculated using Vassar Stats (<http://faculty.vassar.edu/lowry/odds2x2.html?>).
Results
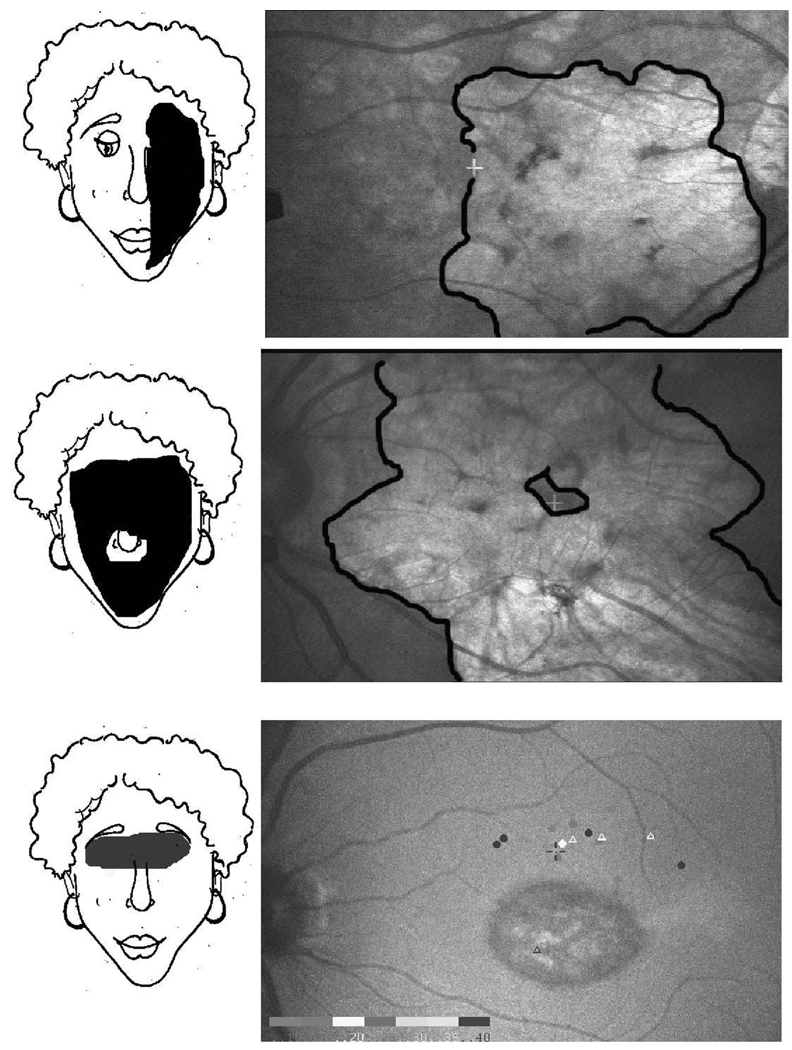
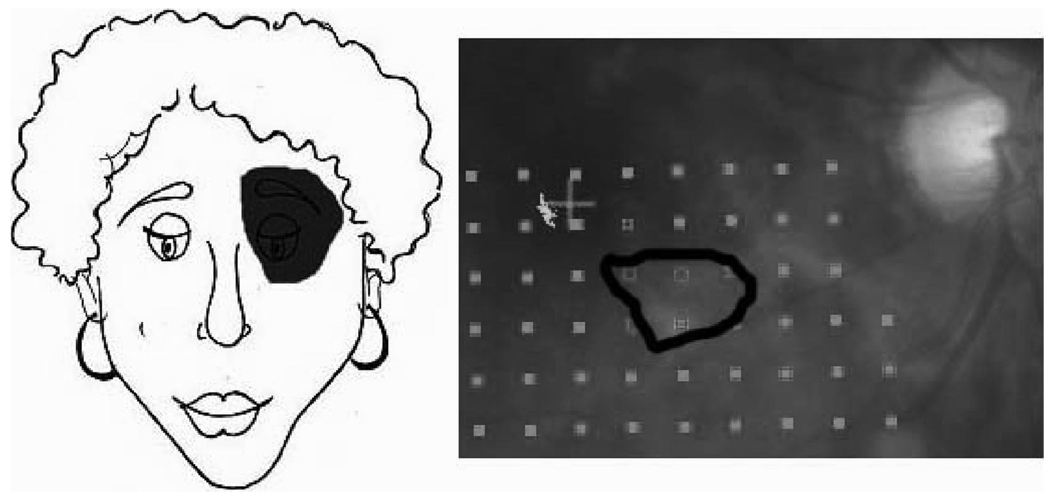
Two hundred fifty-three eyes of 147 persons with macular disease and scotomas in the central visual field had undergone both face fields and microperimetry. Microperimetry, referred to here as “SLO analysis,” was performed on 122 patients using SLO and on 25 using MP-1. Of the 147 persons, 101 had AMD (about equally divided between geographic atrophy and choroidal neovascularization), 23 had Stargardt’s disease, and 23 had other macular diseases. Figure 1 presents examples of face field findings and corresponding SLO images. A small scotoma, determined by MP-1 perimetry and detected on face fields, is shown in Figure 2.
Figure 1.
Examples of face field findings. On the left are schematics of the face field findings, and on the right are SLO images showing fixation (white cross in top and middle, dark cross above atrophy in bottom). Fundus images are the same right and left as the visual field space. Superior and inferior are inverted relative to the visual field space. Top: Geographic atrophy from age-related macular degeneration. Visual acuity 20/160. The person looked to the right to see my nose. My face to her right was blurred. Middle: Geographic atrophy from age-related macular degeneration. Visual acuity 20/50. The person only saw a tiny part of my nose and nostrils; the rest was blurred. Bottom: Stargardt’s disease. Visual acuity 20/160. My eyes were missing.
Figure 2.
Detection of smaller scotomas. Radiation retinopathy. Visual acuity was 20/20. MP-1 imaging shows a dense scotoma (outlined in black), corresponding to a cotton wool spot, below and to the right of the fixation (red cross). In the visual field space, this corresponds to a scotoma up and to the right. The person reported that my eye to her right was missing.
AGREEMENT BETWEEN FACE FIELDS AND SLO ANALYSIS FOR EYES WITHOUT CENTRAL FIXATION
SLO analysis and face fields were performed for 188 eyes without central fixation. Of these 188, 149 (79%) had a PRL on SLO testing (called PRL), and 125 (66%) had evidence of an eccentric fixation locus on face field testing, called ffPL (face field preferred locus); that is, they reported a localized area of blurring or loss of detail with respect to their fixation on the nose.
A PRL and an ffPL were both present in 114 eyes. Table 1 shows the agreement between the face field findings and the SLO findings for these eyes. Seventy five (66%) had agreement of the ffPL with the PRL. The last column to the right in Table 1 shows the proportion of eyes overall with each pattern of fixation on SLO testing. A positive finding on face fields significantly increased the likelihood of that pattern being present in SLO testing. For example, 50% of all eyes fixated with the scotoma superior when measured in the SLO. In contrast, 78% of the eyes with face field findings that are positive for a scotoma superior had that pattern of fixation on SLO analysis (Table 1, top row).
Table 1.
Percentage correct for face fields, using the SLO as the gold standard, eyes without central fixation.
| Face field pattern | % agreement for eyes with an eccentric PRL on SLO testing |
Probability of this SLO pattern for all eyes with an eccentric PRL |
|---|---|---|
| Face field PRL | ||
| Scotoma superior (n = 59) | 78 (68–88) | 50 (42–58%) |
| Scotoma to right (n = 26) | 62 (43–81) | 30 (23–37%) |
| Scotoma to left (n = 19) | 47 (25–69) | 13 (8–18%) |
| Scotoma inferior (n = 10) | 40 (10–70) | 8 (4–12%) |
| Total % correct (n = 114) | 66 (57–75) | |
| % of eyes with SLO pattern of no fixation, unstable fixation, or fixation surrounded by scotoma |
Probability of this SLO pattern for all eyes without central fixation |
|
| Diffuse blurring on face field (n = 48) |
52 (38–66) | 21 (15–27) |
Note: The first column gives the percentage of eyes with each face field pattern that had the same pattern on SLO testing, including only eyes that had a defined fixation pattern on SLO testing. The second column gives the prevalence of each SLO pattern. Knowledge of the face field significantly improved estimation of the SLO PRL. The bottom row of the chart gives the percentage of eyes with diffuse blurring on the face field test that had an SLO pattern that would be compatible with this finding (that is, no fixation, unstable fixation, or eccentric fixation surrounded by a scotoma).
Sixty-three eyes without central fixation did not show an ffPL, and for 14 eyes, the face was reported as normal, including both eyes of 6 persons and 1 eye of 2 persons whose fellow eye had face field findings of diffuse blurring. For 48 eyes, diffuse blurring on face field testing was reported; 25 (52%) of these 48 eyes had SLO findings of no PRL (including putting the fixation cross in the atrophy where it was not seen, being able to bring the fixation cross out of the atrophy at times but not maintaining it on the seeing retina, or eccentric fixation surrounded by the scotoma). The remaining eye without an ffPL had a ring pattern on the face fields.
AGREEMENT BETWEEN FACE FIELDS AND SLO ANALYSIS FOR EYES WITH CENTRAL FIXATION
Sixty-five eyes with central fixation and scotomas within the central field were included (see Table 2). Forty-eight eyes (74%) had face field findings that were compatible with the SLO findings (see the footnotes to Table 2). For 13 (20%) of the 65 eyes with central fixation and scotomas within the central field, the face was reported as normal. This figure is significantly higher than the 7% report of a normal face for eyes with no central fixation (χ2 p = .008, phi = +0.18).
Table 2.
Agreement between SLO and face fields, eyes with central fixation.
| SLO finding | Face field finding correcta |
Face field finding incorrect |
Normal face |
Total |
|---|---|---|---|---|
| Macular ring scotoma | 24b | 0 | 4 | 28 (43%) |
| Horseshoe surrounding fixation | 8 | 1 | 4 | 13 (20%) |
| Scotoma to one side of the fixation | 16 | 3 | 5 | 24 (37%) |
| Total | 48 (74%) | 4 (6%) | 13 (20%) |
Correct face field findings for a macular ring scotoma included seeing a ring scotoma (10 eyes), a partial ring scotoma (7 eyes), or diffuse blurriness of the face (7 eyes) on face fields. Correct face field findings for a horseshoe scotoma included seeing a ring scotoma (1 eye), a scotoma to the closed side of the horseshoe (5 eyes), or diffuse blurriness of the face (2 eyes).
One eye with a macular ring scotoma on both the SLO and the face field analysis also had a second eccentric, PRL with the scotoma superior in both evaluations. This was the only patient with two fixation loci observed in this study.
READING BEHAVIOR AND PRLS
For 73 eyes, a reading behavior suggestive of a particular fixation pattern was noted when reading the visual acuity card or the MNRead card or both. The reading behavior was the same as the PRL in 44 eyes (60%) and was the same as the ffPL in 43 eyes (59%). (It was the same as both the PRL and the ffPL in 34 eyes.)
FIXATION PATTERNS AND DIAGNOSIS
There was a difference in fixation pattern as a function of the diagnosis for eyes with no central fixation. The patients with Stargardt’s disease had a significantly larger percentage of eyes fixating with the scotoma above fixation (76%) than did those with GA (19%; phi = −0.60) or choroidal neovascularization (CNV) (35%; phi = −0.43). When there was still a central fixation, those with GA and CNV may have had a macular ring scotoma, a horseshoe scotoma, or a scotoma to one side of fixation. Unlike GA and CNV, when the center is still spared in Stargardt’s disease, the retina seems to be affected symmetrically in a ring around the fovea. No patient with Stargardt’s disease and central fixation had a horseshoe scotoma or a scotoma to only one side of fixation.
Discussion
IMPORTANT FINDINGS AND IMPLICATIONS OF THE STUDY
The PRL and ffPL findings agreed for 66% of the eyes for which both were assessed. Face fields may be used at a person’s home, require no equipment, and are an excellent illustration to the person of the “boulder” blocking his or her vision and preventing the person from reading effectively and recognizing faces.
When the better eye has central fixation, it is less likely for the fellow eye with no central fixation to develop a PRL than it is when both eyes have no central fixation. The person with central fixation in one eye is constrained to putting the fixation cross on the scotomatous retina in the fellow eye under binocular conditions. In the fellow eye, there may be more potential vision than is measured. An earlier study of persons with bilateral GA who were followed for three or more years found that 17% of the worse-seeing eyes improved in ETDRS visual acuity by 2 or more lines over the three-year follow-up (Sunness et al., 2000). None of the better-seeing eyes improved. On SLO analysis, the worse eyes often could not move the fixation cross out of the scotoma initially, but by three years, the patient’s use of the peripheral seeing retina could be demonstrated.
Eight patients without central fixation in either eye reported that the face appeared normal; 6 had normal face fields for both eyes, and 2 had normal face fields in one eye and diffuse blurring for the fellow eye. This finding suggests that the perception of a localized defect on face fields may be related more to the individual than to the type of scotoma that is present. The 14 eyes with a report of a normal face field represent 7% of the 188 eyes without central fixation. The 65 eyes with central fixation but with scotomas in the central field had a significantly greater frequency of normal face fields, with 13 (20%) reporting the face field as being normal (χ2, p = .008, phi = +0.18). By comparison, the Amsler grid has a much higher rate (40% or more) of not detecting a scotoma on Amsler grid testing in persons with known scotomas from macular degeneration and its treatment (Fine et al., 1986; Schuchard, 1993).
More than half the patients with a report of diffuse blurring on face fields had no PRL on SLO testing, so diffuse blurring was an accurate representation of their fixation pattern. Those with central scotomas and low vision seem to be aware of the difference in perception between blurring as a result of a scotoma (perhaps from “filling in”) and blurring because the eccentric retina is being used and more magnification is needed.
The findings of this study confirmed the predilection for fixation with the scotoma above fixation or to the right of fixation (see Table 1, first column), in agreement with past reports (Fletcher & Schuchard, 1997; Guez et al., 1993; Sunness, Applegate, Haselwood, & Rubin, 1996). Although for persons without macular disease with simulated scotomas, the field to the right contains critical information for reading (Fine & Rubin, 1999; Rayner, Well, & Pollatsek, 1980), the more common fixation pattern is clearly with the scotoma to the right, rather than to the left. A teleological purpose may be to anchor the person to where the line or the word begins. However, most studies to date have not shown a definite association of reading speed with placement of the scotoma (Crossland, Culham, Kabanarou, & Rubin, 2005; Fletcher, Schuchard, & Watson, 1999; Sunness & Applegate, 2005).
RELATIONSHIP BETWEEN EYES ON SLO TESTING AND ON FACE FIELD TESTING
SLO testing is necessarily performed on one eye at a time. Under conditions of binocular viewing, since the eye movements of both eyes are yoked together, the position of objects of interest must fall on the corresponding retinal positions in the two eyes. When I looked at how often the SLO pattern in the two eyes was similar, I found that of the 53 patients without central fixation in either eye who had a PRL on SLO testing in both eyes, 36 (68%) had the same fixation pattern for both eyes. For face fields, one might expect more consistency between the eyes, since persons may be more likely to report a particular finding for the second eye tested when it is similar to the first eye. In addition, face fields are more of a real-life test and may more strongly reflect the way the eyes typically work. For the 76 patients without central fixation in each eye, 55 (72%) had an ffPL in the better-seeing eye. Forty-six of these 55 persons had an ffPL in the worse-seeing eye as well, with 40 (87% of the 46) having the same ffPL pattern in both eyes. The remaining 9 patients with an ffPL in the better-seeing eye had diffuse blurring in the worse-seeing eye. There is significantly greater agreement between the two eyes of each patient in the ffPLs than in the PRLs (87% versus 68%; χ2, p = .02, phi = −0.22).
Twelve patients had central fixation in the eye with better visual acuity and no central fixation in the eye with worse visual acuity. In these eyes, the foveating eye would set the viewing pattern for both eyes, so that one might expect that the fellow eyes would be less likely to be using a PRL. In fact, 8 of these 12 patients (67%) did not have a PRL in the worse eye on SLO testing. This is a significantly higher rate than the 17 out of 76 patients (22%) with no PRL in the eye with the worse visual acuity when there was no central fixation in either eye (χ2, p = .003, phi = +0.34).
LIMITATIONS OF THE STUDY
The time available for doing SLO evaluations was limited because the evaluations were performed in a shared space. Ideally, microperimetric scotoma mapping should be performed to delineate the borders of the scotoma and to quantify the stability of fixation. However, I previously showed that in geographic atrophy from AMD, the dense scotoma corresponds to the area of atrophy. For cases of GA or a discrete scar, observing the fixation pattern and capturing an image showing fixation was often adequate to define the PRL location (Sunness, 2008; Sunness, Schuchard et al., 1995). In cases in which the location of the scotoma was unclear, macular perimetry was performed. Certainly, a formal research study should include a formal fixation analysis (Fujii et al., 2002) and microperimetry, but this evaluation was not generally performed in this retrospective study of clinical data.
Because of the limited way that fixation was analyzed in the SLO, I thought that the most robust correlation would be to identify the main direction of the scotoma relative to fixation, as reported in the note in the medical chart. The main direction was identified roughly by the 90 degrees surrounding the cardinal direction, but practically it was defined by how the scotoma was described in the report. This technique led to an underestimate of the agreement between the face fields and the SLO analysis; for example, if the face fields reported a blind spot above primarily but also to the right and the SLO analysis was reported as showing a blind spot to the right, these reports would be judged as not being in agreement.
A basic question remains as to whether microperimetry is truly the gold standard for fixation behavior. Since microperimetry is performed monocularly, there is a question of whether it represents the actual fixation behavior when a person is binocular and is in a real-world environment. Also, the particular visual task may change how a person fixates and may even induce the selection of several PRLs, each for a different task (Crossland, Culham, & Rubin, 2004; Duret, Issenhuth, & Safran, 1999; Lei & Schuchard, 1997; Sunness, Bressler, & Maguire, 1995). Some of the differences between the results for microperimetry and those for face field may be related to such discrepancies.
Finally, this retrospective study could not address how much the presence of a PRL contributes to persons’ visual function. The observation of persons with central scotomas trying to read and do other tasks illustrates to the low vision provider the importance of awareness of a scotoma and a PRL, but little hard data are available to confirm this observation. A previous study (Sunness et al., 2000) found that 17% of the worse eyes of persons with bilateral GA experienced an improvement of 2 or more lines of ETDRS visual acuity over the course of 3 years, and this finding correlated with these persons acquiring a PRL in the worse eye. Thus, persons may have more potential vision in their worse eye than they realize, and rehabilitation efforts focused on the worse eye are indicated when the better eye is no longer able to perform adequately. There have been conflicting findings on whether the particular fixation pattern that is adopted affects reading speed (Crossland et al., 2005; Fletcher et al., 1999; Sunness & Applegate, 2005; Watson, Schuchard, De l’Aune, & Watkins, 2006). To document the importance of a PRL, a study would have to measure the size of the scotoma, visual acuity, reading rate, and the magnification required to read a given text size and look at the correlation of function with the presence, fixation stability, and pattern of a PRL. This study also could not answer whether more precise information on the direction and degree of eccentricity of the PRL would be of greater benefit to a person than this more general estimation of fixation.
Acknowledgments
The research on which this article was based was supported, in part, by Grant R03 EY14148 from the National Institutes of Health and by the John Mitchell, Jr. Trust. Portions of the article were presented at the 2006 annual meeting of the American Academy of Ophthalmology and the 2007 annual meeting of the Association for Research in Vision and Ophthalmology. The author thanks Brenda Margolis for her help in schematizing the face field procedure.
References
- Altman DG. Practical statistics for medical research. London: Chapman & Hall; 1991. [Google Scholar]
- Crossland MD, Culham LE, Kabanarou SA, Rubin GS. Preferred retinal locus development in patients with macular disease. Ophthalmology. 2005;112:1579–1585. doi: 10.1016/j.ophtha.2005.03.027. [DOI] [PubMed] [Google Scholar]
- Crossland MD, Culham LE, Rubin GS. Fixation stability and reading speed in patients with newly developed macular disease. Ophthalmic and Physiological Optics. 2004;24:327–333. doi: 10.1111/j.1475-1313.2004.00213.x. [DOI] [PubMed] [Google Scholar]
- Duret F, Issenhuth M, Safran AB. Combined use of several preferred retinal loci in patients with macular disorders when reading single words. Vision Research. 1999;39:873–879. doi: 10.1016/s0042-6989(98)00179-5. [DOI] [PubMed] [Google Scholar]
- Fine AM, Elman MJ, Ebert JE, Prestia PA, Starr JS, Fine SL. Earliest symptoms caused by neovascular membranes in the macula. Archives of Ophthalmology. 1986;104:513–514. doi: 10.1001/archopht.1986.01050160069013. [DOI] [PubMed] [Google Scholar]
- Fine EM, Rubin GS. Reading with simulated scotomas: Attending to the right is better than attending to the left. Vision Research. 1999;39:1039–1048. doi: 10.1016/s0042-6989(98)00208-9. [DOI] [PubMed] [Google Scholar]
- Fletcher DC, Schuchard RA. Preferred retinal loci. Relationship to macular scotomas in a low-vision population. Ophthalmology. 1997;104:632–638. doi: 10.1016/s0161-6420(97)30260-7. [DOI] [PubMed] [Google Scholar]
- Fletcher DC, Schuchard RA, Watson G. Relative locations of macular scotomas near the PRL: Effect on low vision reading. Journal of Rehabilitation Research and Development. 1999;36:356–364. [PubMed] [Google Scholar]
- Fujii GY, deJuan EJ, Sunness J, Humayun MS, Pieramici DJ, Chang TS. Patient selection for macular translocation surgery using the scanning laser ophthalmoscope. Ophthalmology. 2002;109:1737–1744. doi: 10.1016/s0161-6420(02)01120-x. [DOI] [PubMed] [Google Scholar]
- Guez J-E, Gargasson J-FL, Rigaudiere F, O’Regan JK. Is there a systematic location for the pseudo-fovea in patients with central scotoma? Vision Research. 1993;9:1271–1279. doi: 10.1016/0042-6989(93)90213-g. [DOI] [PubMed] [Google Scholar]
- Lei H, Schuchard RA. Using two preferred retinal loci for different lighting conditions in patients with central scotomas. Investigative Ophthalmology and Visual Science. 1997;38:1812–1818. [PubMed] [Google Scholar]
- Rayner K, Well AD, Pollatsek A. Asymmetry of the effective visual field in reading. Perception and Psychophysics. 1980;27:537–544. doi: 10.3758/bf03198682. [DOI] [PubMed] [Google Scholar]
- Rohrschneider K, Fendrich T, Becker M, Krastel H, Kruse FE, Volcker HE. Static fundus perimetry using the scanning laser ophthalmoscope with an automated threshold strategy. Graefe’s Archive for Clinical and Experimental Ophthalmology. 1995;233:743–749. doi: 10.1007/BF00184084. [DOI] [PubMed] [Google Scholar]
- Schuchard RA. Validity and interpretation of Amsler grid reports. Archives of Ophthalmology. 1993;111:776–780. doi: 10.1001/archopht.1993.01090060064024. [DOI] [PubMed] [Google Scholar]
- Schuchard RA, Raasch TW. Retinal locus for fixation: Pericentral fixation targets. Clinical Vision Science. 1992;7:511–520. [Google Scholar]
- Sunness JS. What you see is not always what you get in atrophic macular disease. Retinal Cases & Brief Reports. 2008;2:205–208. doi: 10.1097/ICB.0b013e31806011e6. [DOI] [PubMed] [Google Scholar]
- Sunness JS, Applegate CA. Long-term follow-up of fixation patterns in eyes with central scotomas from geographic atrophy associated with age-related macular degeneration. American Journal of Ophthalmology. 2005;140:1085–1093. doi: 10.1016/j.ajo.2005.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunness JS, Applegate CA, Gonzalez-Baron J. Improvement of visual acuity over time in patients with bilateral geographic atrophy from agerelated macular degeneration. Retina. 2000;20:162–169. [PubMed] [Google Scholar]
- Sunness JS, Applegate CA, Haselwood D, Rubin GS. Fixation patterns and reading rates in eyes with central scotomas from advanced atrophic age-related macular degeneration and Stargardt’s’s disease. Ophthalmology. 1996;103:1458–1466. doi: 10.1016/s0161-6420(96)30483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunness JS, Bressler NM, Maguire MG. Scanning laser ophthalmoscope analysis of the pattern of visual loss in age-related geographic atrophy of the macula. American Journal of Ophthalmology. 1995;119:143–151. doi: 10.1016/s0002-9394(14)73866-8. [DOI] [PubMed] [Google Scholar]
- Sunness JS, Schuchard R, Shen N, Rubin G, Dagnelie G, Haselwood D. Landmark-driven fundus perimetry using the scanning laser ophthalmoscope (SLO) Investigative Ophthalmology and Visual Science. 1995;36:1863–1874. [PMC free article] [PubMed] [Google Scholar]
- Timberlake GT, Mainster MA, Peli E, Augliere RA, Essock EA, Arend LE. Reading with a macular scotoma: I. Retinal location of scotoma and fixation area. Investigative Ophthalmology and Visual Science. 1986;27:1137–1147. [PubMed] [Google Scholar]
- Watson GR. Using low vision effectively. In: Fletcher DC, editor. Low vision rehabilitation: Caring for the whole person. San Francisco: American Academy of Ophthalmology; 1999. pp. 64–66. [Google Scholar]
- Watson GR, Schuchard RA, De l’Aune WR, Watkins E. Effects of preferred retinal locus placement on text navigation and development of advantageous trained retinal locus. Journal of Rehabilitation Research and Development. 2006;43:761–770. doi: 10.1682/jrrd.2005.07.0120. [DOI] [PubMed] [Google Scholar]
- White JM, Bedell HE. The oculomotor reference in humans with bilateral macular disease. Investigative Ophthalmology and Visual Science. 1990;31:1149–1161. [PubMed] [Google Scholar]