Abstract
Objective
The use of donor sperm or ova becomes an option for some infertile couples. We sought to determine the views towards donor sperm and eggs of both men and women.
Design
Prospective cohort of infertile couples
Setting
Eight California reproductive endocrinology practices
Patients
Infertile couples (n=377) were recruited after initial infertility clinic visit.
Main Outcome Measures
From questionnaires administered at recruitment, ratings concerning the impact of the use of donor gametes were assessed. Differences between men and women in attitudes toward donor gametes were compared with ANOVA. Linear regression was used to identify independent predictors of attitudes towards gametes.
Results
Female's attitudes towards donor sperm were significantly more negative than their attitudes towards donor eggs (5.1±1.4 vs 4.7±1.6*). Similarly, male donor gamete attitude scores were higher for donor sperm compared to donor eggs (4.9±1.6 vs 4.1±1.6*). Both men and women agreed that the use of donor sperm was more likely to have negative effects on their relationship and negative societal ramifications. Female donor gamete attitude scores were predicted by marital status, race, and education while men's scores were independent of all measured factors.* p<0.0001
Conclusions
Both men and women view the use of donor sperm with more skepticism compared to the use of donor eggs suggesting a unique underlying perception regarding the use of male donor gametes.
Introduction
An estimated 12% of couples are unable to conceive after one year of unprotected intercourse and are considered infertile.(1) For some couples, the use of donor gametes becomes a necessary option for offspring. Donor sperm may be used when the male partner is unable to fertilize as with azoospermia or severe oligospermia which can occur in up to 10% of men.(2, 3) Similarly, the female may also be unable to conceive (e.g. diminished ovarian reserve) and require the assistance of donor eggs.(2)
When asked about the use of donor gametes, in a hypothetical sense, many individuals remain open to their use.(4) However, despite the risks of low chance for reproductive success or the possibility of spreading genetic defects, most couples prefer to use their own gametes rather than donors to avoid relinquishing genetic relatedness.(5-7) After conception, investigators have explored how couples continue to wrestle with the difficult decisions of whether to reveal the genetic origins to their offspring.(8, 9)
While the impact on the use of donor gametes after delivery has been explored, less is understood about the beliefs regarding the use of donor gametes prior to conception. As couples jointly decide upon appropriate technologies to utilize towards the goal of a pregnancy, each members' perceptions contributes. We sought to determine the views towards donor sperm and eggs of both men and women in infertile heterosexual couples.
Materials and Methods
Study Design and Subjects
After approval of the Institutional Review Board approval, couples were recruited into the study cohort from eight participating reproductive endocrinology clinics in the Bay Area after the female partner presented for an initial infertility appointment. The inclusion criteria for the study were defined as: currently trying to get pregnant with a male partner, English-speaking, no prior treatment with in vitro fertilization, no prior sterilization or hysterectomy, living in the greater Bay Area, and able to schedule an initial home visit interview within 6 weeks of the index clinic visit. Study participants completed questionnaires at the time of enrollment that contained medical and surgical histories, socioeconomic and demographic data, history of prior maternity or paternity, and an assessment of attitudes toward the use of donor eggs and donor sperm. Participants were also interviewed in person within 6 weeks of their initial appointment.
Item Development
Items were developed based prior literature by experts in the fields of psychometrics, clinical psychology, and reproductive medicine. A pilot test with a small number of individuals recruited in the same manner as the primary study subjects was performed, and problematic items were revised or discarded. Questions regarding the impact on the individual, the partner, the child, and the infertile couple's relationship were utilized.
Outcome Measures
Three sources were used to identify items to use in the attitude scales: 1) review of positive and negative consequences reported in the literature; 2) consequences suggested by experts in the fields of psychology, epidemiology, and reproductive medicine; and 3) pilot interviews with a small number of infertile individuals. The initial group of items was pilot tested on a separate group of individuals similar to those recruited in the main study and subsequently reduced after discarding problematic items. The final set of items reflected consequences across a range of domains, including consequences of donor gamete use for the individual, the partner, the marital relationship, and the child. Separate scales were created to assess attitudes towards donor sperm and towards donor eggs. These scales asked participants to judge the probability or likelihood that certain consequences would occur if they used donor gametes (e.g., “If you use donor sperm/egg, how likely do you think it is that you would experience emotional stress?”). Items were rated on 10-point scales, with end-points ranging from “definitely would not” to “definitely would” Scale reliability was good (Cronbach's alpha was 0.80, 0.75, 0.79, and 0.80 for female's donor egg scores, female's donor sperm scores, male's donor egg scores, and male's donor sperm scores, respectively). Scales were judged by a panel of experts in reproductive medicine, epidemiology, and psychology to have face and content validity as well.
Predictor Variables
The potentially confounding effects of male and female age, educational level, annual household income, religious affiliation, race, and duration of marriage were examined for average donor gamete attitude scores. Age (continuous), duration of marriage (None, ≤5 years, 6-9 years, ≥10 years), religious affiliation (yes/no), college graduate (yes/no), annual household income (≤$100,000, $100,000 - $199,000, and ≥ $200,000), and white race (yes/no) were determined by answers to questionnaires administered at enrollment.
The presence or absence of perceived male and female factor infertility was determined from the enrollment interview. During this interview, male and female members of the couple were asked if the doctor told them the reason for their “problems having a baby.” Four exposure categories were possible: female factor infertility (i.e. female factor infertility and no male factor), male factor in the absence of female factor infertility, concurrent male and female factor infertility, and unexplained infertility. Perception of infertility etiology rather than the eventual diagnosis was chosen for this classification given that the primary aim of this study was to assess baseline perceptions on the use of donor gametes.
Statistical Analysis
Descriptive statistics were used to characterize the study population. ANOVA was used to assess differences in donor gamete attitude scores and individual items across gender. Multivariable linear regression analysis was performed to assess the role of age, income, race, education, religion, and infertility diagnosis on the donor gamete attitude scores. To measure agreement within couples, a Pearson correlation coefficient was calculated for both donor ova and donor sperm. A significance level of 0.05 was used. STATA 10 (Statacorp, College Station, TX, USA) was used for all analyses.
Results
In all, 436 women were recruited into the study with 377 joining with their partner. Table 1 lists baseline demographics and diagnoses of the cohort with partnered and total women listed separately. Mean age was 35.7±4.8 years for women and 36.9±5.5 years for the men. Nine men (2.5%) were diagnoses with azoospermia and 158 (39.2%) with ovarian dysfunction.
Table 1.
Demographic, socioeconomic, and infertility characteristics of cohort.
| Female | Partnered Females | Male | ||
|---|---|---|---|---|
| Observations (%) | Observations (%) | Observations (%) | ||
| N | 436 | 377 | 377 | |
|
| ||||
| Age | ≤35 | 205 (47.3) | 181 (48.1) | 160 (42.4) |
| 36-39 | 130 (30.0) | 111 (29.5) | 110 (29.2) | |
| 40-44 | 85 (19.6) | 74 (19.7) | 71 (18.8) | |
| ≥45 | 13 (3.0) | 10 (2.7) | 36 (9.6) | |
|
| ||||
| Years Married | Not Married | 53 (12.2) | 42 (11.2) | 34 (9.3) |
| ≤5 | 235 (54.0) | 168 (44.7) | 177 (47.1) | |
| 6-9 | 97 (22.3) | 127 (33.8) | 124 (33.0) | |
| ≥10 | 50 (11.5) | 39 (10.4) | 41 (10.9) | |
|
| ||||
| Annual Household Income | ≤$100,000 | 139 (34.2) | 112 (31.9) | 113 (32.0) |
| $100,001-200,000 | 206 (50.6) | 185 (52.7) | 186 (52.7) | |
| ≥$200,001 | 62 (15.2) | 54 (15.4) | 54 (15.3) | |
|
| ||||
| Education | ≤Some College | 121 (28.3) | 101 (27.2) | 119 (31.8) |
| ≥College Degree | 307 (71.7) | 270 (72.7) | 255 (68.2) | |
|
| ||||
| Race | White | 303 (70.0) | 272 (72.3) | 283 (75.1) |
| Other | 130 (30.0) | 104 (27.7) | 94 (24.9) | |
|
| ||||
| Religion | None | 87 (20.1) | 74 (19.7) | 77 (20.4) |
| Catholic | 134 (31.0) | 121 (32.2) | 107 (28.4) | |
| Protestant | 61 (14.1) | 55 (14.6) | 54 (14.3) | |
| Other Christian | 58 (13.4) | 48 (12.8) | 59 (15.7) | |
| Jewish | 29 (6.7) | 25 (6.7) | 32 (8.5) | |
| Other | 64 (14.8) | 53 (14.1) | 48 (12.7) | |
|
| ||||
| Perceived Diagnosis | Female | 197 (45.8) | 168 (44.9) | 166 (46.6) |
| Male | 48 (11.2) | 44 (11.8) | 44 (12.4) | |
| Both | 50 (11.6) | 46 (12.3) | 56 (15.7) | |
| Unknown | 135 (31.4) | 116 (31.0) | 90 (25.3) | |
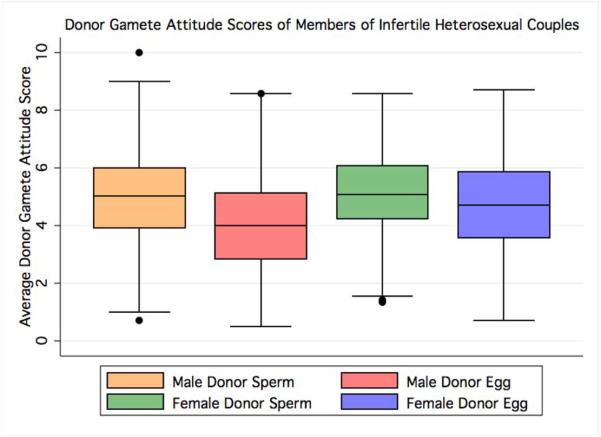
Among females, average donor gamete attitude scores were significantly higher (i.e. more negative attitude) for donor sperm compared to donor eggs (5.1±1.4 vs 4.7±1.6, p<0.00005). Similarly, male donor gamete attitude scores were higher for donor sperm compared to donor eggs (4.9±1.6 vs 4.1±1.6, p<0.00005). When examining attitudes toward donor eggs, women had higher donor gamete attitude scores (i.e. more negative attitude) than men (5.1±1.4 vs 4.1±1.6, p<0.00005). In contrast, women and men had similar average donor gamete attitude scores when queried about donor sperm (5.1±1.4 vs 4.9±1.6, p=0.15; Figure 1, Table 2). The Pearson correlation coefficient between each member of an infertile couple was 0.30 for donor ova attitude scores and 0.33 for donor sperm attitude scores.
Figure 1.
Boxplot showing average donor gamete attitude scores for all patients in cohort stratified by donor gamete and subject gender. Female donor gamete attitude scores were significantly higher for donor sperm compared to donor eggs (p<0.00005). Similarly, male donor gamete attitude scores were higher for donor sperm compared to donor eggs (p<0.00005). Women had higher donor gamete attitude scores than men (p<0.00005). Men and women had similar donor gamete attitude scores when queried about donor sperm (p=0.15).
Table 2.
Individual questions grouped by theme and composite donor gamete attitude scores for survey participants. Scores ranged from 0 (definitely would not) to 10 (definitely would). Paired t tests were utilized to compare scores between donor eggs and donor sperm within each gender for individual questions and average attitude scores (p values following questions for each sex). In addition, unpaired t tests compared composite donor gamete attitude scores for both donor eggs and donor sperm between men and women (p values at bottom of female egg and sperm columns). Cronbach's alpha is listed for each average donor gamete attitude score.
| Female | Male | |||||
|---|---|---|---|---|---|---|
| Would using donor egg/sperm... | Egg | Sperm | p value | Egg | Sperm | p value |
| make you feel you do not have control of your life | 7.5±2.9 | 6.9±3.1 | <0.00005 | 6.7±3.0 | 7.4±2.9 | <0.00005 |
| be emotionally stressful for you | 8.2±2.6 | 7.7±2.6 | 0.0001 | 6.1±3.1 | 7.1±3.0 | <0.00005 |
| mean you feel that you missed out on some of the joyful aspects of having a child | 5.0±3.9 | 5.5±3.7 | 0.1415 | 3.7±3.5 | 5.9±3.6 | <0.00005 |
| be emotionally stressful for your partner | 6.5±3.0 | 8.0±2.6 | <0.00005 | 7.2±2.9 | 6.7±2.8 | <0.00005 |
| make you feel that you and your partner did not create a child together | 5.1±3.3 | 6.5±3.2 | <0.00005 | 3.1±3.1 | 6.3±3.3 | <0.00005 |
| cause marital problems | 4.3±3.4 | 5.5±3.4 | <0.00005 | 3.6±3.1 | 4.4±3.4 | <0.00005 |
| mean having people make judgements about whether you would be a good parent | 1.8±2.9 | 5.6±2.8 | <0.00005 | 1.7±2.7 | 5.4±2.8 | <0.00005 |
| be wrong for moral or religious reasons | 2.4±3.4 | 3.0±3.6 | <0.00005 | 2.1±3.1 | 2.8±3.5 | <0.00005 |
| mean your child be physically unhealthy | 2.6±2.1 | 2.9±2.3 | 0.0019 | 2.7±2.2 | 3.2±2.2 | 0.0003 |
| lead to your child having significant | 2.5±2.5 | 2.6±2.6 | 0.4597 | 2.4±2.4 | 2.6±2.4 | 0.0193 |
| social/emotional problems mean that you would not know about your child's medical history | 2.9±3.0 | 3.4±3.1 | 0.0016 | 3.4±2.9 | 3.9±3.0 | 0.0011 |
| mean someone else having a claim to your child | 3.2±3.3 | 3.5±3.3 | 0.1789 | 2.2±2.8 | 3.1±3.1 | <0.00005 |
| mean you worry that the gamete donor would want to take your child from you | 4.9±3.5 | 3.8±3.6 | <0.00005 | 3.6±3.3 | 3.2±3.2 | 0.0012 |
| require spending a lot of money | 9.2±1.8 | 7.0±3.0 | <0.00005 | 8.3±2.4 | 6.9±2.8 | <0.00005 |
|
| ||||||
| Sum | 4.7±1.6 | 5.1±1.4 | <0.00005 | 4.1±1.6 | 4.9±1.6 | <0.00005 |
|
| ||||||
| Cronbach's alpha | 0.80 | 0.75 | 0.80 | 0.80 | ||
| <0.00005 | 0.1522 | |||||
In order to examine the differences seen between average donor gamete attitude scores, we looked at the individual questions asked (Table 2). Men and women felt that the use of donor sperm would be more likely to lead to marriage turmoil compared to donor eggs. Moreover, both men and women felt that using donor sperm would cause each to miss out on the joyful aspects of birth more than the use of donor eggs. In addition, both men and women felt the use of donor sperm would lessen the mutual feeling of creating a child and cause others to question their parenting skills more than the use of donor eggs. Men and women also suggested that the use donor sperm was more morally questionable compared to donor eggs (Table 2).
On multivariable analysis, being married significantly raised a woman's donor egg score compared to her single counterpart (ß: 0.88; CI 0.32, 1.43). Duration of marriage did not affect this association (data not shown). In addition, having a combined male and female infertility diagnosis raised a women's donor egg attitude score compared to a female infertility diagnosis alone (ß: 0.62; CI 0.06, 1.17). Marriage also raised a woman's donor sperm score (ß: 0.84; CI 0.34, 1.35), while white race (ß: -0.37; CI -0.72, -0.02) and a college degree (ß: -0.40; CI -0.77, -0.03) both lowered it. Religious beliefs did not predict donor gamete attitude scores in women. Neither azoospermia nor ovarian dysfunction predicted with male or female gamete attitude scores. Men's scores were independent of all measured variables (Table 3).
Table 3.
Multivariable linear regression analyses assessing effect of socioeconomic and infertility variables on donor gamete attitude scores. Adjusted regression coefficients are listed with 95% confidence intervals inside parentheses. Bolded coefficient denotes statistical significance (p<0.05). All coefficients reflect adjusts for all variables listed in table.
| Score | Variable | Women | Men | |
|---|---|---|---|---|
| Donor Egg Score | Married | Yes vs. No | 0.88 (0.32, 1.43) | 0.39 (-0.28, 1.06) |
| Age | -0.03 (-0.07, 0.01) | 0.00 (-0.04, 0.03) | ||
| Race | White vs. Other | -0.24 (-0.64, 0.16) | 0.03 (-0.41, 0.47) | |
| Education | ≤ Some College vs. ≥ College Degree | -0.25 (-0.65, 0.16) | 0.29 (-0.16, 0.73) | |
| Annual Household Income | ≤ $100,000 | Reference | Reference | |
| $100,001-200,000 | 0.15 (-0.27, 0.57) | 0.21 (-0.25, 0.68) | ||
| ≥ $200,001 | -0.04 (-0.61, 0.52) | 0.20 (-0.41, 0.82) | ||
| Religion | Yes vs. No | 0.00 (-0.45, 0.45) | 0.44 (-0.05, 0.92) | |
| Female Factor | Reference | Reference | ||
| Infertility Diagnosis | Male Factor | 0.18 (-0.42, 0.78) | 0.54 (-0.08, 1.16) | |
| Male & Female | 0.62 (0.06, 1.17) | 0.16 (-0.40, 0.72) | ||
| Unknown | 0.20 (-0.23, 0.62) | 0.01 (-0.47, 0.50) | ||
|
| ||||
| Donor Sperm Score | Married | Yes vs. No | 0.84 (0.34, 1.35) | 0.44 (-0.29, 1.16) |
| Age | 0.00 (-0.03, 0.04) | 0.00 (-0.04, 0.03) | ||
| Race | White vs. Other | -0.37 (-0.72, -0.02) | -0.15 (-0.62, 0.32) | |
| Education | ≤ Some College vs. ≥ College Degree | -0.40 (-0.77, -0.03) | 0.24 (-0.23, 0.71) | |
| Annual Household Income | ≤ $100,000 | Reference | Reference | |
| $100,001-200,000 | -0.16 (-0.54, 0.21) | -0.11 (-0.59, 0.38) | ||
| ≥ $200,001 | -0.29 (-0.81, 0.23) | -0.06 (-0.73, 0.61) | ||
| Religion | Yes vs. No | 0.09 (-0.30, 0.48) | 0.50 (-0.01, 1.00) | |
| Female Factor | Reference | Reference | ||
| Infertility Diagnosis | Male Factor | -0.02 (-0.56, 0.51) | 0.51 (-0.16, 1.19) | |
| Male & Female | 0.32 (-0.18, 0.82) | 0.25 (-0.34, 0.84) | ||
| Unknown | 0.06 (-0.32, 0.44) | 0.21 (-0.30, 0.72) | ||
Discussion
Our analysis found that both men and women from infertile couples have a more negative attitude toward the use of donor sperm than donor eggs. Fears of marital conflict, an incomplete gestational experience, and societal opinions of parenting ability were all worse for donor sperm compared to donor eggs.
The reason for increased reluctance toward the use of donor sperm compared to donor eggs for both men and women is uncertain. Some authors have postulated that in egg donation, both partners feel more involved compared to donor insemination.(4) Indeed, our data show that both men and women feel that using donor sperm would lessen the joyful aspects of childbirth more than the use of donor eggs. In addition, both members acknowledged that the use of donor sperm would cause others to question their parenting abilities significantly more than donor eggs. There was a pervasive negative connotation with the use of donor sperm that did not exist to the same degree for donor eggs. It may be that while many assume a mother would love a child regardless of genetic relatedness, a father does not generate similar feelings of selflessness.
Such attitudes are consistent with findings showing that egg donors are often regarded favorably while sperm donors have their own motivations questioned.(10, 11) Authors have surmised that in a patriarchal society where children inherit the father's name, maternal relatedness in less important.(4, 12,13)
Interestingly, both men and women acknowledged that the use of donor sperm would be more likely to lead to marital problems than donor eggs. Indeed, marital concerns are among the most important factors when couples consider the use of assisted reproductive technologies.(14) Given this fact, it is perhaps not surprising that unmarried women had lower gamete attitude scores than their married counterparts, regardless of duration of marriage.
While white race and education level did lessen donor gamete attitude scores in women, men's attitudes were independent of all examined socioeconomic and demographic factors. Rawson et al also showed a trend for women of higher education to have an improved attitude toward the use of donor insemination.(15) In contrast, Kazem et al showed that increasing education led to a decrease in the acceptability of using donor gametes for their own fertility needs for women in England.(4) This group postulated that a higher education made an individual more aware of genetic heritability and the desire to pass on their own genes. With conflicting results, both the trend and any explanation remain uncertain. In our analysis, white women showed decreased donor gamete attitude scores compared to women of other race/ethnicities implying a cultural component to donor gamete attitudes as well as a socioeconomic one.
Several limitations of our study warrant mention. Our recruitment was based on subject willingness to participate thus unmeasured biases may have accounted for some patients refusal to join. While we showed that few socioeconomic or demographic factors affected donor gamete attitude scores, it is possible that our sample size was inadequate to detect such differences. Indeed, our study and others have shown that patients who seek infertility services tend to be quite homogenous in regards to socioeconomic factors. The items utilized for this analysis focus on negative consequences of donor gametes rather than more positive aspects of family building which also play a role in the decision to proceed with donor ova or sperm. As this was a questionnaire was given at the initiation of the infertility evaluation, attitudes toward the use of donor gametes may change during the infertility evaluation as the need for their use becomes more imminent. In fact, Kazem et al showed that attitudes towards donor gametes differ between people who require infertility services and those who do not.(4)
In the United States, the use of donor eggs often requires consultation with a mental health professional, while no such requirements exist for the use of donor sperm.(2) However, the diagnosis of male infertility and the need for donor insemination is known to cause depression and marital problems.(16, 17) Some have instituted specialized seminars to discuss issues related to donor insemination in an effort to lessen the burden on the infertile couple.(18) Our data supports the notion that infertile couples' attitudes towards the use of donor sperm cause social anxiety and fear of relationship turmoil more so than the use of donor eggs. Just as couples must speak with medical and mental health professionals before using donor ova, perhaps similar safeguards should be instituted prior to donor insemination.
Acknowledgments
Support: P01 HD37074 from the National Institute for Child Health and Human Development (NICHD/NIH)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Capsule Both men and women believe the use of donor sperm would have more severe relationship and societal implications compared to donor eggs suggesting a unique underlying perception regarding the use of donor sperm.
References
- 1.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: Data from the 2002 National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat. 2005;23:1–174. [PubMed] [Google Scholar]
- 2.2006 Guidelines for Gamete and Embryo Donation. Fertility and sterility. 2006;86:S38–50. doi: 10.1016/j.fertnstert.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 3.van Zyl JA, Menkveld R. Oligozoospermia: recent prognosis and the outcome of 73 pregnancies in oligozoospermic couples. Andrologia. 2006;38:87–91. doi: 10.1111/j.1439-0272.2006.00720.x. [DOI] [PubMed] [Google Scholar]
- 4.Kazem R, Thompson LA, Hamilton MP, Templeton A. Current attitudes towards egg donation among men and women. Human reproduction (Oxford, England) 1995;10:1543–8. doi: 10.1093/humrep/10.6.1543. [DOI] [PubMed] [Google Scholar]
- 5.Giltay JC, Kastrop PM, Tuerlings JH, Kremer JA, Tiemessen CH, Gerssen-Schoorl KB, et al. Subfertile men with constitutive chromosome abnormalities do not necessarily refrain from intracytoplasmic sperm injection treatment: a follow-up study on 75 Dutch patients. Human reproduction (Oxford, England) 1999;14:318–20. doi: 10.1093/humrep/14.2.318. [DOI] [PubMed] [Google Scholar]
- 6.Nap AW, Van Golde RJ, Tuerlings JH, De Sutter P, Pieters MH, Giltay JC, et al. Reproductive decisions of men with microdeletions of the Y chromosome: the role of genetic counselling. Human reproduction (Oxford, England) 1999;14:2166–9. doi: 10.1093/humrep/14.8.2166. [DOI] [PubMed] [Google Scholar]
- 7.Stouffs K, Lissens W, Tournaye H, Van Steirteghem A, Liebaers I. The choice and outcome of the fertility treatment of 38 couples in whom the male partner has a Yq microdeletion. Human reproduction (Oxford, England) 2005;20:1887–96. doi: 10.1093/humrep/deh847. [DOI] [PubMed] [Google Scholar]
- 8.Golombok S, Lycett E, MacCallum F, Jadva V, Murray C, Rust J, et al. Parenting infants conceived by gamete donation. J Fam Psychol. 2004;18:443–52. doi: 10.1037/0893-3200.18.3.443. [DOI] [PubMed] [Google Scholar]
- 9.Mac Dougall K, Becker G, Scheib JE, Nachtigall RD. Strategies for disclosure: how parents approach telling their children that they were conceived with donor gametes. Fertility and sterility. 2007;87:524–33. doi: 10.1016/j.fertnstert.2006.07.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haimes E. Issues of gender in gamete donation. Social science & medicine (1982) 1993;36:85–93. doi: 10.1016/0277-9536(93)90308-q. [DOI] [PubMed] [Google Scholar]
- 11.Power M, Baber R, Abdalla H, Kirkland A, Leonard T, Studd JW. A comparison of the attitudes of volunteer donors and infertile patient donors on an ovum donation programme. Human reproduction (Oxford, England) 1990;5:352–5. doi: 10.1093/oxfordjournals.humrep.a137104. [DOI] [PubMed] [Google Scholar]
- 12.Lessor R, Reitz K, Balmaceda J, Asch R. A survey of public attitudes toward oocyte donation between sisters. Human reproduction (Oxford, England) 1990;5:889–92. doi: 10.1093/oxfordjournals.humrep.a137205. [DOI] [PubMed] [Google Scholar]
- 13.Pettee D, Weckstein LN. A survey of parental attitudes toward oocyte donation. Human reproduction (Oxford, England) 1993;8:1963–5. doi: 10.1093/oxfordjournals.humrep.a137968. [DOI] [PubMed] [Google Scholar]
- 14.Millstein SG, Katz P, Pasch L. Deciding about IVF: What's important to infertile couples? Fertility and sterility. 2002;78:S27–S. [Google Scholar]
- 15.Rawson G. Human artificial insemination by donor and the Australian community. Clinical reproduction and fertility. 1985;3:1–19. [PubMed] [Google Scholar]
- 16.Kerr J, Brown C, Balen AH. The experiences of couples who have had infertility treatment in the United Kingdom: results of a survey performed in 1997. Human reproduction (Oxford, England) 1999;14:934–8. doi: 10.1093/humrep/14.4.934. [DOI] [PubMed] [Google Scholar]
- 17.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004;63:126–30. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Daniels K, Thorn P, Westerbrooke R. Confidence in the use of donor insemination: an evaluation of the impact of participating in a group preparation programme. Human fertility (Cambridge, England) 2007;10:13–20. doi: 10.1080/14647270600973035. [DOI] [PubMed] [Google Scholar]