Abstract
Social network structure and norms are linked to HIV risk behavior. However little is known about the gradient of norm of HIV risk that exists among social networks. We examined the association between injection risk network structure and HIV risk norms among 818 injection drug users (IDUs). IDUs were categorized into four distinct groups based on their risk behaviors with their drug networks: no network members with whom they shared cookers or needles, only cooker-sharing member, one needle-sharing member, and multiple needle-sharing members. The riskiest group, networks of multiple needle sharers, was more likely to endorse both risky needle-sharing and sex norms. Networks of only cooker sharers were less likely to endorse high-risk norms, as compared to the networks with no sharing. There were also differences based on gender. Future HIV prevention interventions for IDUs should target both injection and sex risk norms, particularly among IDUs in the multiple needle-sharing networks.
Keywords: Social norms, Social network, Needle sharing, HIV risk, Injection drug use, Gender
Introduction
There is a growing consensus on the need for HIV prevention efforts to focus on structural factors that perpetuate risk and impede harm reduction. There is a long-standing recognition of the role that social networks have in the transmission of HIV and other infectious diseases (Friedman and Aral 2001; Rhodes et al. 2005). Social network structure and social norms, a function of networks, are linked to HIV risk behavior (Bailey et al. 2007; Davey-Rothwell and Latkin 2007; De et al. 2007; Latkin et al. 2003a; Miller and Neaigus 2001; Neaigus 1998; Neaigus et al. 2001; Shaw et al. 2007). Network structure refers to the size and interconnections, and function refers to the resources and types of support. Networks may differ in their level of risk based on both structure and function.
Social norms have a strong influence on numerous health behaviors. Descriptive norms refer to an individual’s interpretation of what behaviors are practiced among a given social group, while injunctive norms refer to individual’s perception of how others may respond to their behavior (Cialdini et al. 1990). Once norms are established within a group, these tend to be reinforced by group members (Bettenhausen and Murnighan 1985; Zucker 1977). Moreover, promoting new norms may influence individuals to change their own behavior so that it is congruent with the perceived norm.
There is ample research on the strong and persistent association between norms and HIV-related risk behaviors. Davey-Rothwell and colleagues found that injunctive norm predict needle-sharing behavior 6 months later (Davey-Rothwell et al. 2009). Peer norms for syringe sharing have also been associated with receptive needle sharing among young adult IDUs (Bailey et al. 2007). Peer norms for safer drug use has also been associated with less frequent lending of needles among HIV-positive individuals (Metsch et al. 2007). Several other studies have also found an association between norms and unprotected sex (van Empelen et al. 2001) and exchanging sex for money and drugs (Davey-Rothwell and Latkin 2008).
In studying social norms, it is important to determine the group which individuals observe and refer to (Newcomb 1950). As suggested by Reifman et al. (2006), not all peer network members have an equal influence on health behaviors. In their study, only the drinking patterns of “drinking buddies” prospectively predicted level of drinking (Reifman et al. 2006). Similarly, certain network members of IDUs may influence the development and maintenance of social norms related to HIV-risk behaviors more than other network members. Previous studies among drug users have noted that drug partners have more influence on an individual’s drug-using pattern than family or friends (Latkin et al. 1995). Although one study noted that having more network members who used crack increased the risk for engaging in sex exchange (Latkin et al. 2003b), no study to date has examined how type of social network HIV risk structures may be associated with sex and injection risk norms.
In this paper, we examined the association between injection risk network structure and two HIV risk behaviors: unprotected sex and needle-sharing behaviors. Specifically, we examined the following questions: Is there a meaningful gradation of HIV risk behavior in networks; do high-risk drug networks endorse risky drug norms, and do high-risk drug networks endorse risky sexual norms? To address this question, we divided participants into groups based on social network structure defined by their risk behaviors with their drug-using network members.
We hypothesized that IDUs who engage in riskier injection behavior with their network members would also endorse both high-risk injection norms and high-risk sex norms, as compared to IDUs who reported being in less riskier networks. We further sought to explore gender differences in these associations, based on published studies of norms and HIV risk among injection drug users (Davey-Rothwell and Latkin 2007; Mizuno et al. 2000).
Methods
Data Source
The data for this study were collected at baseline from the participants in the STEP into Action study (STEP), a social network-based HIV prevention intervention of IDUs and their social network members from Baltimore, Maryland. Participants were recruited using community outreach methods in neighborhoods with high concentrations of drug use and drug sales. Two types of participants were enrolled in the STEP study: Index and Network participants. The Index participants were eligible for the study if they: (1) were 18 years and older; (2) resided in Baltimore; (3) had not participated in other HIV or network studies in the past year; (4) engaged in frequent cocaine or heroin injection in the past 3 months; and (5) were willing to talk to network members about HIV prevention. Index participants were further provided an opportunity to recruit their social network members to be a part of the study. Network members were eligible for this study if they met the following criteria: (1) 18 years or older; (2) Baltimore resident; and one of the following risk behaviors: (3a) self-reported use of heroin or cocaine in the past 6 months; (3b) used drugs with index participant; (3c) shared injection paraphernalia with index participant; or (3d) was a sex partner of index participant.
Participants completed face-to-face interviews that included both interviewer-administered sections and Audio Computer-Assisted Self-Interview (ACASI) sections for items pertaining to sex and drug behaviors. After completing the interview, participants were compensated with $35.
Measurement
Social Network Variables
The social network structure data were collected using the Personal Network Inventory, a modified version of the Arizona Social Support Inventory (Barrera and Gottlieb 1981). This inventory has been shown to have good concurrent and predictive validity and internal consistency (Latkin et al. 1996). The first section of this inventory is designed to generate names of people in the entire social network. This name generating section entailed respondents listing the names (first and last initials) of individuals based on different questions about people who provided support and with whom they socialized etc. The following network questions were used to specifically delineate participants’ drug networks, “Now, I am going to ask you about another group of people, those who you do drugs with. (“Do drugs with” was defined as being in the same room when using drugs). These individuals may be close friends or casual acquaintances. Who are the people that you do drugs with? These might be people you have listed before or they could be new names. (This question pertains to all drugs, not just injection drugs, but does not include alcohol or marijuana.) Is there anyone else you can think of?”
Probes included the following questions: “When you use drugs with [NAME], who else is usually there? Who do you consider your running buddy? Who did you do drugs with last month? How about 3 months ago, who were you doing drugs with then? Think about the place where you copped last week and the people who you were with. Who are the people that you regularly buy or use drugs with? Think about the all the different places where you used last week. These might be friends’ places, abandoned houses, your place, or galleries. Was there anyone there who you do drugs with on a regular basis? Sometimes people that you list are not available, they may be sick, locked up or just not around. So can you think of anyone else that you did drugs with in the last couple of months?”
At the end of the name-generating section, participants were asked to list the type and frequency of drugs used among their network members. A drug network member was defined by asking, “who on this list has used drugs, like heroin, cocaine, or crack, in the past 6 months?”
For each network member listed, respondents were asked if they had shared a needle with that network member in the past 6 months. The number of network members with whom the respondent shared needles was summed to obtain the total number of needle-sharing network members. This distribution was highly right skewed and ranged from 0 to 12. A similar question was asked for sharing cookers. The number of network members with whom the respondent shared cookers ranged from 0 to 12 members and was highly right skewed as well.
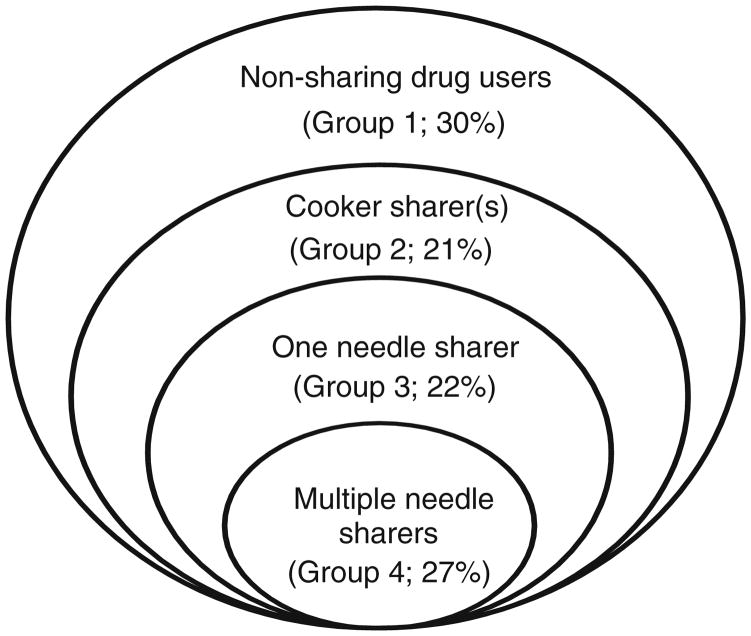
The main independent variable of interest was structure of the injection risk network. Structure was categorized into four mutually exclusive groups based on the number of needle- and cooker-sharing network members. Each category (i.e., Group) in this variable represents an increasing level of risk. Group 1: Lowest risk—drug network includes drug-using network member who do not share cookers or needles; Group 2—network includes at least one network member who shares cookers: Group 3—network includes only one network member who shares needles; or Group 4: highest level of risk—network includes two or more network members who share needles. We differentiated IDUs who share needles with one member from those who share with multiple members, because individuals who share exclusively with one person may qualitatively differ from those who share with more than one individual. Selective sharing for needles has been noted in previous studies (Valente and Vlahov 2001), and many individuals, especially women, report sharing only with one person who are often their sex partners (Evans et al. 2003; Sherman et al. 2001). Sharing cookers tends to be more common than sharing syringes. It is often linked to injectors buying drugs together. Although it is possible to distinguish between individuals who share cookers with one other person and those who share with two or more persons, we only made this distinction for needle sharing. The differences in injection risk between sharing cookers with one or multiple network members may not be as pronounced as IDUs who share needles with one or more network members, especially since cooker sharing is considered less risky than needle sharing. Figure 1 presents the distribution of these four injection risk network structures within the sample; the risk for HIV infection increases as an individual moves into the center of the circle.
Fig. 1.
Distribution of injection risk network structure, STEP study (n = 818)
Two additional social network characteristics were collected via the network inventory: (1) total network size was calculated by summing the number of individuals named by the respondent (up to twenty network members possible); and (2) density was defined as the proportion of individuals listed who were friends with each other. Density is a structural component of social networks that indicates degree of interconnectedness among social ties (Wasserman and Faust 1994).
Norms Variables
The outcomes of this study were descriptive and injunctive norms regarding sex and injection behavior (Table 1). The item on injunctive sex risk norm asked, “How many of your friends would disapprove if you were to have sex or turn a trick to get money or drugs?” This response had a bimodal distribution (Table 1). The respondents were classified as supporting low risk norm if they reported that about half (50%), most (about 75%), or all (about 100%) of their friends would disapprove of turning tricks, and high-risk norms if none or a few of their friends (about 25%) would disapprove.
Table 1.
Distribution of sex and injection risk norms among IDUs with drug-using networks, STEP study (n = 818)
| Responses | Sex exchange norms |
Needle sharing norms |
|||
|---|---|---|---|---|---|
| Friends would disapprove if you were to have sex or turn a trick to get money or drugsa | Number of friends have sex or turn tricks to get money or drugsb | Number of drug buddies share needles with other peoplec | Responses | My drug buddies would give me a hard time if I shared a needle with a strangerd | |
| None | 211 (26) | 241 (30) | 217 (27) | Strongly disagree | 28 (3) |
| A few (about 25%) | 174 (21) | 391 (48) | 447 (55) | Disagree | 136 (17) |
| About half (50%) | 48 (6) | 87 (11) | 78 (10) | Neither agree or disagree | 49 (6) |
| Most (about 75%) | 101 (12) | 67 (8) | 52 (6) | Agree | 391 (48) |
| All (about 100%) | 282 (35) | 25 (3) | 16 (2) | Strongly agree | 214 (26) |
2 missing,
7 missing,
8 missing,
3 missing
The injunctive norm on needle-sharing behavior asked, “Drug buddies would give me a hard time if I shared needles with other people.” The available response categories were “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” and “strongly agree.” The distribution was bimodal, with neither agree nor disagree having the least number of respondents (Table 1). The respondents were classified as supporting high injunctive injection risk norm if they indicated strongly agree and agree and low risk norm if they responded agree nor disagree, disagree, or strongly agree.
The descriptive norms for sex and injection risk were “How many of your friends have sex or turn tricks to get money or drugs?” and “How many of your drug buddies share needles with other people?” respectively. The available responses were none, a few (about 25%), about half (50%), most (about 75%) or all (about 100%). The distributions were right skewed for both items (Table 1). The responses to each question were dichotomized as high-risk norm if individuals responded that over a half of their friends engaged in this behavior, and low risk if they responded “none” or a “few.”
Additional Variables
Sociodemographic characteristics examined in this study were gender, race/ethnicity (African-American vs. others), age (median split for 44 years and above), relationship status (married or in a committed relationship vs. others), education (have high school diploma or GED), self-reported HIV status, unemployment, incarceration, and homelessness in the past 6 months. Respondents were also asked if they have snorted, sniffed or smoked heroin, crack or cocaine in the past 6 months.
Data Analyses
The present study was restricted to individuals who self-reported injecting drugs in the past 6 months (IDUs). Baseline data (n = 1,024) were collected from March 2004 to March 2006. Of these individuals, 842 reported injecting drugs in the past 6 months; 24 IDUs who did not report having drug-using networks were excluded from the analysis. The final sample was 818 IDUs, which consisted of 584 indexes (71%) and 234 (29%) of their risk network members. A few individuals were excluded from the multivariate models due to missing data on the norms or drug use variable, which is presented in Tables 1 and 2.
Table 2.
Sample characteristics of IDUs with drug-using networks, STEP study (n = 818)
| Characteristics | Injection risk network structure |
Test statistica | |||
|---|---|---|---|---|---|
| Non-sharing drug users (Group 1) | Cooker sharer(s) (Group 2) | One needle sharer (Group 3) | Multiple needle sharers (Group 4) | ||
| (n = 243) | (n = 175) | (n = 179) | (n = 221) | ||
| Gender: male | 152 (63) | 125 (71) | 107 (60) | 134 (61) | 6.67 |
| Race: African-American | 206 (85) | 151 (86) | 140 (78) | 155 (70) | 21.30** |
| Age: 43 or younger | 121 (50) | 64 (37) | 103 (58) | 123 (56) | 19.51** |
| Married or in a committed relationship | 65 (27) | 47 (27) | 69 (39) | 56 (25) | 10.36* |
| High school diploma or GED | 144 (59) | 100 (57) | 105 (59) | 127 (57) | 0.26 |
| Unemployed in past 6 months | 219 (90) | 161 (92) | 163 (91) | 205 (93) | 1.13 |
| Imprisoned in past 6 months | 49 (20) | 54 (31) | 57 (32) | 78 (35) | 14.42* |
| Homeless in past 6 months | 70 (29) | 58 (33) | 71 (40) | 106 (48) | 19.97* |
| HIV positive (self-report) | 25 (10) | 36 (21) | 32 (19) | 33 (16) | 10.65** |
| Snorted or sniffed heroin in past 6 monthsb | 135 (56) | 62 (35) | 79 (44) | 98 (44) | 17.23** |
| Snorted or sniffed cocaine in past 6 monthsc | 74 (31) | 34 (19) | 30 (17) | 59 (27) | 13.61** |
| Smoked crack in past 6 months | 152 (63) | 93 (53) | 131 (73) | 158 (71) | 20.87** |
| Attended shooting gallery in past 6 months | 68 (28) | 50 (29) | 62 (35) | 108 (49) | 27.04** |
| Total network size [mean (SD)]e | 8.6 (4.1) | 8.3 (3.5) | 8.0 (3.8) | 9.8 (4.0) | 9.03** |
| Density [mean(SD)]d,e | 0.5 (0.3) | 0.5 (0.3) | 0.5 (0.3) | 0.5 (0.3) | 0.16 |
| No. of active drug users [mean (SD)]e | 4.1 (2.8) | 4.4 (2.5) | 4.2 (2.6) | 5.7 (2.7) | 16.99** |
3 degrees of freedom for all test statistics,
1 missing,
3 missing,
4 missing,
ANOVA F-tests, all other used Chi-squared test statistics
P < 0.05;
P < 0.01
First, Chi-square tests and ANOVAs were conducted to examine the unadjusted relationships between the four groups of networks and individual and social network characteristics. Generalized Estimating Equations (GEE) modeling was used to examine the relationship between norms and network structure, since network analysis may violate the independent observations assumptions required for conventional logistic regressions (Zeger and Liang 1986). GEE bivariate logistic regressions were conducted to model the unadjusted association between each of the four norms and sociodemographic characteristics. GEE multivariate logistic regression was then conducted to examine the association between each norm and injection risk network structure after adjusting for potential confounders. All covariates were entered in the model. The model was made more parsimonious by retaining covariates significant at the P < 0.05 in the exploratory analyses and those variables that have been associated with norms in previously published literature. The inferences from the more parsimonious model remained similar as those for the full model.
Four different models are presented, each describing the association between the four groups of injection risk networks and a specific norm variable. Model A examined the association with friend’s disapproval of engaging in sex exchange (injunctive norm). Model B focused on the number of friends who engage in sex exchange (descriptive norm). Models C and D examined the association with needle-sharing norms, specifically whether drug buddies would give the respondent a hard time if the respondent share needles (Model C) (injunctive norm) and number of drug buddies who share needles (Model D) (descriptive norm). Each of the four models was also stratified by gender to examine if this relationship varied by gender. Although no differences was found for Model A and C, gender differences were observed for Model B and D and are presented in Table 4.
Table 4.
Gender differences in the adjusted association between HIV risk norms and type of network members among IDUs, STEP study
| Characteristics | Model B: number of friends have sex or turn tricks to get money or drugsa |
Model D: number of drug buddies share needles with other peoplea |
||||||
|---|---|---|---|---|---|---|---|---|
| Male (n = 514) |
Female (n = 294) |
Male (n = 513) |
Female (n = 294) |
|||||
| AORb | 95%CI | AORb | 95%CI | AORb | 95%CI | AORb | 95%CI | |
| Injection risk network composition (Ref: Group 1: non-sharing drug users) | ||||||||
| Group 4: multiple needle sharers | 3.2** | 1.6–6.4 | 0.8 | 0.4–1.6 | 2.2* | 1.2–4.1 | 1.6 | 0.7–3.4 |
| Group 3: one needle sharer | 2.1 | 1.0–4.3 | 0.4* | 0.2–0.9 | 1.1 | 0.5–2.3 | 0.8 | 0.3–1.8 |
| Group 2: cooker sharer(s) | 0.9 | 0.4–2.4 | 0.4* | 0.1–0.9 | 0.3* | 0.1–0.9 | 0.5 | 0.2–1.5 |
| African-American | 0.4** | 0.2–0.7 | 0.4* | 0.2–0.8 | ||||
| Age (Ref: 43 or younger) | 0.5* | 0.3–0.9 | 0.8 | 0.4–1.4 | 1.1 | 0.7–1.9 | 0.6 | 0.3–1.1 |
| Married or in a committed relationship | 0.7 | 0.4–1.5 | 0.6* | 0.3–1.0 | ||||
| HS Diploma or GED | ||||||||
| HIV status (self-report) | ||||||||
| Homeless in past 6 months | 1.4 | 0.8–2.3 | 2.9** | 1.7–4.9 | 1.1 | 0.6–2.0 | 1.1 | 0.6–2.2 |
| Unemployed in the past 6 months | 0.5 | 0.2–1.1 | 0.6 | 0.2–1.8 | ||||
| Prison in the past 6 months | ||||||||
| Attended shooting gallery in the past 6 months | 1.6 | 1.0–2.8 | 3.5** | 2.0–6.4 | 2.1** | 1.2–3.6 | 2.6** | 1.4–4.8 |
| Smoked crack in the past 6 months | 1.8* | 1.0–3.2 | 2.1* | 1.0–4.5 | 1.9* | 1.1–3.4 | 0.9 | 0.4–1.8 |
| Snorted or sniffed heroin in past 6 months | 1.0 | 0.6–1.7 | 1.0 | 0.6–1.7 | ||||
| Snorted/smoked cocaine in the past 6 months | ||||||||
Responses dichotomized as all/most/half versus little/none
AOR refers to odds ratio adjusted for other covariates in the model
P < 0.05;
P < 0.01
Results
The 818 IDUs were distributed across the four groups of injection risk networks as followed: Group 1—30% (n = 243) had drug-using network members with whom they did not share needles or cookers; Group 2—21% (n = 175) had cooker-sharing network members but no needles-sharing members; Group 3—22% (n = 179) had only one network member with whom they shared needles; and Group 4—27% (n = 221) had more than one needle-sharing network members (Figure 1). The vast majority of IDUs who reported sharing needles with network members also reported cooker sharing; only thirteen IDUs reported sharing needles alone. Nine of these IDUs were classified as Group 3, and four were classified as Group 4. Table 2 further describes the sample characteristics of IDUs across these network typologies. Significant differences were noted for almost all characteristics examined, except for gender, education, unemployment, and network density. A greater proportion of IDUs in a riskier injection network group had attended a shooting gallery in the past 6 months. About 49% of IDUs in Group 4 attended a shooting gallery, whereas 28% of IDUs in Group 1 attended a shooting gallery (Chi-square: 27.04; P < 0.01). IDUs in Group 4 also had larger total network size (F-test: 9.03; P < 0.01) and greater number of drug users in their networks (F-test: 16.99; P < 0.01), as compared to IDUs in the network structures with lower injection risk (Group 1–3). A high proportion of IDUs in Group 3 were married or in a committed relationship, as compared to other groups (Chi-squared test: 10.36; P < 0.05).
Table 3 presents the unadjusted and adjusted associations between the four network groups and each of the four norms (two sex risk norms and two needle-sharing norms). Only Group 4 was related to both risky sex and needle sharing norms. Even after adjusting for other covariates, IDUs in this group were 30% less likely to perceive that their friends would disapprove of them exchange sex, as compared to IDUs in Group 1 [Model A: AOR (95%CI): 0.7 (0.5–1.0)]. Additionally, IDUs in Group 4 were approximately twice as likely to report that many of their drug buddies share needles with other people, as compared to IDUs in Group 1 [Model D: AOR (95%CI): 1.9 (1.2–3.1)].
Table 3.
Unadjusted and adjusted association between HIV risk norms and type of network members among IDUs, STEP study
| Characteristics | Model A: friends would disapprove if you were to have sex or turn a trick to get money or drugsa (n = 813) |
Model B: number of friends have sex or turn tricks to get money or drugsa (n = 808) |
Model C: drug buddies will give me a hard time if I share needles with other peopleb (n = 815) |
Model D: number of drug buddies share needles with other peoplea (n = 807) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusted |
Unadjusted |
Adjusted |
Unadjusted |
Adjusted |
Unadjusted |
Adjusted |
|||||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Injection risk network structure (Ref: Group 1: non-sharing drug users) | ||||||||||||||||
| Group 4: multiple needle sharers | 0.6** | 0.4–0.9 | 0.7* | 0.5–1.0 | 2.0** | 1.3–3.1 | 1.6 | 1.0–2.5 | 0.5 ** | 0.4–0.8 | 0.7 | 0.5–1.0 | 2.7 ** | 1.7–4.2 | 1.9** | 1.2–3.1 |
| Group 3: one needle sharer | 0.8 | 0.5–1.2 | 0.9 | 0.6–1.3 | 1.1 | 0.7–1.7 | 1.0 | 0.6–1.6 | 1.0 | 0.6–1.6 | 1.2 | 0.7–1.9 | 1.1 | 0.7–1.9 | 1.0 | 0.5–1.7 |
| Group 2: cooker sharer(s) | 0.8 | 0.5–1.2 | 0.8 | 0.5–1.1 | 0.5* | 0.3–0.9 | 0.6 | 0.3–1.1 | 1.7* | 1.0–2.8 | 1.8 * | 1.1–3.0 | 0.4* | 0.2–0.9 | 0.4* | 0.2–0.9 |
| Gender (Ref: male) | 0.8 | 0.6–1.0 | 0.8 | 0.6–1.0 | 3.4** | 2.4–4.8 | 4.0 ** | 2.6–6.1 | 1.1 | 0.8–1.6 | 1.1 | 0.8–1.5 | 1.5* | 1.0–2.1 | 1.6 * | 1.0–2.4 |
| African-American | 1.0 | 0.7–1.4 | 0.7 | 0.5–1.0 | 1.8 ** | 1.2–2.6 | 1.7* | 1.1–2.5 | 0.3** | 0.2–0.5 | 0.4 ** | 0.3–0.6 | ||||
| Age (Ref: 43 or younger) | 1.1 | 0.8–1.4 | 0.5** | 0.3–0.7 | 0.6 * | 0.4–0.9 | 1.2 | 0.9–1.6 | 0.6** | 0.4–0.9 | 0.8 | 0.6–1.2 | ||||
| Married or in a committed relationship | 1.1 | 0.8–1.5 | 0.8 | 0.5–1.1 | 0.6 * | 0.4–1.0 | 1.1 | 0.8–1.6 | 1.2 | 0.8–1.8 | ||||||
| High school diploma or GED | 0.9 | 0.7–1.2 | 0.8 | 0.6–1.2 | 1.2 | 0.9–1.6 | 1.0 | 0.7–1.4 | ||||||||
| HIV status (self-report) | 0.9 | 0.6–1.3 | 1.0 | 0.6–1.6 | 0.7 | 0.4–1.0 | 0.5** | 0.3–0.8 | 1.2 | 0.7–1.9 | ||||||
| Homeless in the past 6 months | 0.8* | 0.6–1.0 | 0.8 | 0.6–1.1 | 2.1** | 1.5–2.9 | 1.9 ** | 1.3–2.7 | 0.5 ** | 0.4–0.7 | 0.7* | 0.5–0.9 | 1.7** | 1.2–2.5 | 1.1 | 0.7–1.7 |
| Unemployed in the past 6 months | 0.8 | 0.5–1.3 | 0.9 | 0.5–1.8 | 0.5 * | 0.2–0.9 | 0.5 | 0.3–1.0 | 1.2 | 0.6–2.3 | ||||||
| Prison in the past 6 months | 0.8 | 0.6–1.1 | 1.3 | 0.9–1.9 | 0.7 * | 0.5–1.0 | 0.8 | 0.6–1.2 | 1.4 | 1.0–2.1 | ||||||
| Attended shooting gallery in the past 6 months | 0.8 | 0.6–1.0 | 0.8 | 0.6–1.1 | 2.3** | 1.6–3.2 | 2.2 ** | 1.5–3.3 | 0.6** | 0.4–0.8 | 0.8 | 0.5–1.1 | 2.6** | 1.8–3.8 | 2.3** | 1.5–3.5 |
| Smoked crack in the past 6 months | 0.8 | 0.6–1.1 | 0.8 | 0.6–1.1 | 2.6** | 1.8–3.9 | 1.9** | 1.2–3.0 | 0.7 * | 0.5–0.9 | 0.8 | 0.5–1.2 | 1.7** | 1.1–2.5 | 1.4 | 0.9–2.2 |
| Snorted or sniffed heroin in past 6 months | 0.9 | 0.7–1.2 | 1.6* | 1.1–2.1 | 1.0 | 0.7–1.5 | 0.8 | 0.6–1.1 | 1.2 | 0.9–1.7 | ||||||
| Snorted/smoked cocaine in the past 6 months | 0.9 | 0.7–1.2 | 1.2 | 0.8–1.7 | 0.6 * | 0.4–0.9 | 0.7* | 0.5–1.0 | 1.4 | 0.9–2.1 | ||||||
Responses dichotomized as all/most/half versus little/none
Responses dichotomized as strongly agree/agree versus neither/disagree/strongly disagree
P < 0.05;
P < 0.01
In contrast, Group 3 was either weakly or not significantly associated with any of these norms. Group 2 was inversely associated with injection risk norms. After adjusting for other covariates, IDUs in Group 2 were 1.8 times more likely to perceive that their drug buddies would give them a hard time if the they shared needles with other people, as compared to IDUs in Group 1 [Model C; AOR (95%CI): 1.8 (1.1–3.0)]. In addition, IDUs in Group 2 were less likely to perceive that many of their drug buddies share needles with other people, as compared to IDUs in Group 1 [Model D: AOR (95%CI): 0.4 (0.2–0.9)].
For Models B and D, the relationship between network groups and HIV risk norms also varied by gender (Table 4). Males in Group 4 were over three times more likely to perceive that many of their friends exchanged sex, as compared to males in Group 1 [AOR (95%CI): 3.2 (1.6–6.4)]. On the other hand, females in Group 2 or 3 were less likely to perceive that their friends exchange sex, as compared to females in Group 1 [AOR (95% CI): 0.4 (0.1–0.9) and 0.4 (0.2–0.9), respectively]. The gender-stratified model in Model D showed that the norm on needle sharing was only relevant to male IDUs. Specifically, males IDUs in Group 4 perceived that many of their drug buddies share needles with others, as compared to male IDUs in Group 1 [AOR (95%CI): 2.2 (1.2–4.1)]. In addition, males in Group 2 were 70% less likely to perceive that many of their drug buddies share needles with others, as compared to males in Group 1 [AOR (95%CI): 0.3 (0.1–0.9)].
Discussion
Consistent with previous studies (Bailey et al. 2007; Davey-Rothwell and Latkin 2007), we report a strong association between injection risk behavior and needle-sharing norms among a sample of current IDUs in Baltimore, Maryland. Our study further showed that IDUs have a gradient of risk based on their personal network structure. IDUs across these networks were heterogeneous in their endorsement of needle-sharing norms. Furthermore, Group 4, the highest risk group, was associated with risky sex norms. The relationships between the injection risk network structure and risky sex and needle-sharing norms also varied by gender.
Among the four network groups, Group 4 (multiple needle-sharing networks) was the only group that was associated with both risky needle-sharing and sex norms. The finding suggests that IDUs in this particular network structure have greater HIV risk compared to those in other network configurations. IDUs in Group 3 (networks of one needle sharer) were no more likely to report sex or injection risk norms, as compared to the IDUs in the lowest risk group (Group 1). We found one exception in the gender-stratified multivariate model. In this model, females in Group 3 were actually less likely to perceive that most of their friends exchanged sex. Our finding is consistent with previous studies that suggested qualitative differences between IDUs who practice exclusive sharing with a specific network member from other IDUs (Unger et al. 2006). It is important to note that although Group 3 was not strongly associated with sex and injection risk norms in our study, individuals in this network are not necessarily without risk for HIV infection. Those who share needles with close ties may not necessarily engage in safe injection practices such as cleaning the needles (Barnard 1993). IDUs who practice exclusive sharing may not feel comfortable cleaning needles or perceive less risk when sharing drugs with people they feel emotionally close (Unger et al. 2006). Engaging in safe injection practice within such close ties may also imply distrust in their relationships (Barnard 1993; Unger et al. 2006). Additionally, ties among risk network members of IDUs may be unstable (Valente and Vlahov 2001); the dynamics of social networks has been associated with HIV-risk behavior (Costenbader et al. 2006; Hoffmann et al. 1997). Even those who engage in exclusive sharing may be at increased risk if these relationships are constantly changing.
IDUs in the cooker-sharing networks (Group 2) perceived sex and injection risk norms differently from IDUs in the multiple needle-sharing networks (Group 4). Whereas multiple needle-sharing networks were linked to social influences that encourage HIV risk behaviors, cooker-sharing networks were associated with social norms that discouraged individuals from engaging in these risky behaviors (e.g. my drug buddies would give a hard time if I share needles with other people). Since cooker sharing is often considered less risky than needles sharing, it is interesting that there was an inverse relationship between needle-sharing norms and cooker-sharing networks. The finding suggests that some IDUs are organizing their drug networks to avoid needle sharing.
Certain injection risk network characteristics were also associated with risky sex norms. This linkage suggests the need for preventive interventions among IDUs that target both sex and injection risk norms. There were more frequent associations found between network typologies and needle-sharing norms than with the sex risk norms. This was expected for several reasons. First, we defined HIV risk network grouping based on sharing cookers or needles with their network members, which are specific behaviors more relevant to needle-sharing norms. Second, the reference group for needle-sharing norms was drug buddies, whereas the sex risk norms referred to friends, which may or may not include drug buddies. “Drug buddies” refer to a specific group of social networks, in which needle sharing behavior may be enacted more frequently. Finally, sex behaviors tend to be private behaviors, whereas injection behaviors are often practiced in semi-public settings. Descriptive needle-sharing norms may be more accurate since others may view this behavior, and thus they may be more influential on the actual behavior (Hawkins et al. 1999).
The associations between network structure and risky sex and needle-sharing norms also differed between females and male IDUs. Gender differences in the relationship between injection risk behavior and needle-sharing norms have been noted in a previous study (Davey-Rothwell and Latkin 2007). In the present study, multiple needle-sharing networks were strongly associated with risky sex norms for males. In contrast, networks of one needle sharer or only cooker sharers were protective against risky sex norms among females. Previous studies have noted that women were more likely to have overlapping sex and needle-sharing partners (Evans et al. 2003; Miller and Neaigus 2001; Sherman et al. 2001), whereas males were more likely to share with their drug partners as well. As such, many women in the one needle-sharing network structure may be in a committed relationship and surrounded by individuals who are less likely to exchange sex.
There are several limitations to this study. This study was based on a voluntary sample of IDUs who self-selected into the study. It was also a cross-sectional study based on self-reports. Although this study does not consider needle and cooker-sharing behaviors outside the context of one’s social network, studies have found that often these sharing episodes occur within close ties, i.e., within individuals in one’s social network (Sherman et al. 2001). It is possible that individuals have more frequent interactions with their networks than non-network ties and are more likely to remember these episodes of sharing. As the network inventory in the current study focused on network members known for at least 1 month, the analyses did not examine sharing with strangers and using syringes from common containers and other sources of contaminated syringes (Page et al. 1990). However, focusing on understanding the social dynamics associated with sharing within network members is a useful approach for development of interventions that target their social network. A final limitation of the study was that although we examined both injunctive and descriptive norms, we were not able to contrast the influence of injunctive and descriptive norms for two reasons. First, both norms were moderately correlated (Spearman’s correlation coefficients of −0.24 and −0.26 for risky sex and needle-sharing norms, respectively with P < 0.01 for both). Second, the injunctive norm items did not focus on the exact same behaviors as the descriptive norms.
Despite these limitations, the study offers evidence that social norms of both sex and injection risks are relevant to IDUs in certain risk network structures, specifically to those in the multiple needle-sharing or cooker-sharing networks. These results have several public health implications. They suggest that there are high-risk networks that endorse high-risk norms and hence may perpetuate these norms. These networks are important targets for interventions. These networks, however, may be resistant to the larger normative influence of risk reduction and require greater intervention focus. We do not know how these personal networks fit into larger sociometric networks (i.e. social ties that exist among members of a connected group). Understanding their relationship to sociometric network structure is important for both blood-borne disease transmission and developing appropriate community-based interventions. The findings also suggest that networks are an important venue for understanding social norms and potentially developing interventions to change network norms.
Acknowledgments
This work was funded by the National Institute on Drug Abuse (grant# 1RO1 DA016555 and 1F31 DA026318).
Contributor Information
C. A. Latkin, Email: clatkin@jhsph.edu.
S. J. Kuramoto, Email: skuramot@jhsph.edu.
References
- Bailey SL, Ouellet LJ, Mackesy-Amiti ME, Golub ET, Hagan H, Hudson SM, et al. Perceived risk, peer influences, and injection partner type predict receptive syringe sharing among young adult injection drug users in five U.S. cities. Drug and Alcohol Dependence. 2007;91(S1):S18–S29. doi: 10.1016/j.drugalcdep.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Barnard MA. Needle sharing in context: Patterns of sharing among men and women injectors and HIV risks. Addiction (Abingdon, England) 1993;88:805–812. doi: 10.1111/j.1360-0443.1993.tb02094.x. [DOI] [PubMed] [Google Scholar]
- Barrera M, Gottlieb BH. Social support in the adjustment of pregnant adolescents: Assessment issues. In: Gottlieb BH, editor. Social networks and social support. Baverly Hills, CA: Sage; 1981. pp. 61–96. [Google Scholar]
- Bettenhausen K, Murnighan JK. The emergence of norms in competitive decision-making groups. Administrative Science Quarterly. 1985;30(3):350–372. doi: 10.2307/2392667. [DOI] [Google Scholar]
- Cialdini RB, Reno RR, Kallgreen CA. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology. 1990;58:1015–1026. doi: 10.1037/0022-3514.58.6.1015. [DOI] [Google Scholar]
- Costenbader EC, Astone NM, Latkin CA. The dynamics of injection drug users’ personal networks and HIV risk behaviors. Addiction (Abingdon, England) 2006;101(7):1003–1013. doi: 10.1111/j.1360-0443.2006.01431.x. [DOI] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latkin CA. Gender differences in social network influence among injection drug users: Perceived norms and needle sharing. Journal of Urban Health. 2007;84:691–703. doi: 10.1007/s11524-007-9215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latkin CA. An examination of perceived norms and exchanging sex for money or drugs among women injectors in Baltimore, MD, USA. International Journal of STD & AIDS. 2008;19(1):47–50. doi: 10.1258/Ijsa.2007.007123. [DOI] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latkin CA, Tobin KE. Longitudinal analysis of the relationship between perceived norms and sharing injection paraphernalia. AIDS and Behavior. 2009 doi: 10.1007/s10461-008-9520-z. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De P, Cox J, Boivin J-F, Platt RW, Jolly AM. The importance of social networks in their association to drug equipment sharing among injection drug users: A review. Addiction (Abingdon, England) 2007;102:1730–1739. doi: 10.1111/j.1360-0443.2007.01936.x. [DOI] [PubMed] [Google Scholar]
- Evans JL, Hahn JA, Page-Shafer K, Lum PJ, Stein ES, Davidson PJ, et al. Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study) Journal of Urban Health. 2003;80(1):137–146. doi: 10.1093/jurban/jtg137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman S, Aral S. Social networks, risk-potential networks, health, and disease. Journal of Urban Health. 2001;78:411–418. doi: 10.1093/jurban/78.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins WE, Latkin C, Mandel W, Oziemkowska M. Do actions speak louder than words? Perceived peer influences on needle-sharing and cleaning in a sample of injection drug users. AIDS Education and Prevention. 1999;11(2):122–131. [PubMed] [Google Scholar]
- Hoffmann JP, Su SS, Pach A. Changes in network characteristics and HIV risk behavior among injection drug users. Drug and Alcohol Dependence. 1997;46(1–2):41–51. doi: 10.1016/S0376-8716(97)00038-0.. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Forman VL, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science & Medicine. 2003a;56(3):465–476. doi: 10.1016/S0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Hua W, Forman VL. The relationship between social network characteristics and exchanging sex for drugs or money among drug users in Baltimore, MD, USA. International Journal of STD & AIDS. 2003b;14(11):770–775. doi: 10.1258/09564620360719831. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Mandell W, Oziemkowska M, Celentano D, Vlahov D, Ensminger M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug and Alcohol Dependence. 1995;38(1):1–9. doi: 10.1016/0376-8716(94)01082-V. [DOI] [PubMed] [Google Scholar]
- Latkin C, Mandell W, Vlahov D, Oziemkowska M, Celentano D. People and places: Behavioral settings and personal network characteristics as correlates of needle sharing. Journal of Acquired Immune Deficiency Syndrome. 1996;13(3):273–280. doi: 10.1097/00042560-199611010-00010. [DOI] [PubMed] [Google Scholar]
- Metsch LR, Pereyra M, Purcell DW, Latkin CA, Malow R, Gomez CA. Correlates of lending needles/syringes among HIV-seropositive injection drug users. Journal of Acquired Immune Deficiency Syndrome. 2007;46(2):S72–S79. doi: 10.1097/QAI.0b013e3181576818.. [DOI] [PubMed] [Google Scholar]
- Miller M, Neaigus A. Networks, resources and risk among women who use drugs. Social Science & Medicine. 2001;52(6):967–978. doi: 10.1016/S0277-9536(00)00199-4. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Kennedy M, Seals B, Myllyluoma J. Predictors of teens’ attitudes toward condoms: Gender differences in the effects of norms. Journal of Applied Social Psychology. 2000;30:1381–1395. doi: 10.1111/j.1559-1816.2000.tb02526.x. [DOI] [Google Scholar]
- Neaigus A. The network approach and interventions to prevent HIV among injection drug users. Public Health Reports. 1998;113(supp1):140–150. [PMC free article] [PubMed] [Google Scholar]
- Neaigus A, Friedman SR, Kottiri BJ, Des Jarlais DC. HIV risk networks and HIV transmission among injecting drug users. Evaluation and Program Planning. 2001;24(2):221–226. doi: 10.1016/S0149-7189(01)00012-X. [DOI] [Google Scholar]
- Newcomb TM. Social psychology. The Dryden Press, Inc; New York: 1950. [Google Scholar]
- Page JB, Smith PC, Kane N. Shooting galleries, their proprietors, and implications for prevention of AIDS. Drugs and Society. 1990;5:69–85. doi: 10.1300/J023v05n01_06. [DOI] [Google Scholar]
- Reifman A, Watson WK, McCourt A. Social networks and college drinking: Probing processes of social influence and selection. Personality and Social Psychology Bulletin. 2006;32(6):820–832. doi: 10.1177/0146167206286219. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Shaw SY, Shah L, Jolly AM, Wylie JL. Determinants of injection drug user (IDU) syringe sharing: The relationship between availability of syringes and risk network member characteristics in Winnipeg, Canada. Addiction (Abingdon, England) 2007;102(10):1626–1635. doi: 10.1111/j.1360-0443.2007.01940.x. [DOI] [PubMed] [Google Scholar]
- Sherman SG, Latkin CA, Gielen AC. Social factors related to syringe sharing among injecting partners: A focus on gender. Substance Use & Misuse. 2001;36(14):2113–2136. doi: 10.1081/JA-100108439. [DOI] [PubMed] [Google Scholar]
- Unger JB, Kipke MD, De Rosa CJ, Hyde J, Ritt-Olson A, Montgomery S. Needle-sharing among young IV drug users and their social network members: The influence of the injection partner’s characteristics on HIV risk behavior. Addictive Behaviors. 2006;31(9):1607–1618. doi: 10.1016/j.addbeh.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Valente TW, Vlahov D. Selective risk taking among needle exchange participants: Implications for supplemental interventions. American Journal of Public Health. 2001;91(3):406–411. doi: 10.2105/AJPH.91.3.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Empelen P, Schaalma HP, Kok G, Jansen MWJ. Predicting condom use with casual and steady sex partners among drug users. Health Education Research. 2001;16(3):293–305. doi: 10.1093/her/16.3.293. [DOI] [PubMed] [Google Scholar]
- Wasserman S, Faust K. Social network analysis: Methods and applications. Cambridge University Press; Cambridge: 1994. [Google Scholar]
- Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- Zucker LG. The role of institutionalization in cultural persistence. American Sociological Review. 1977;42(5):726–743. doi: 10.2307/2094862. [DOI] [Google Scholar]