Abstract
We report here a case study of a rare neurological patient with bilateral brain damage encompassing a substantial portion of the so-called “limbic system.” The patient, Roger, has been studied in our laboratory for over 14 years and the current article presents his complete neuroanatomical and neuropsychological profiles. The brain damage occurred in 1980 following an episode of herpes simplex encephalitis. The amount of destroyed neural tissue is extensive and includes bilateral damage to core limbic and paralimbic regions, including the hippocampus, amygdala, parahippocampal gyrus, temporal poles, orbitofrontal cortex, basal forebrain, anterior cingulate cortex, and insular cortex. The right hemisphere is more extensively affected than the left, although the lesions are largely bilateral. Despite the magnitude of his brain damage, Roger has a normal IQ, average to above average attention, working memory, and executive functioning skills, and very good speech and language abilities. In fact, his only obvious presenting deficits are a dense global amnesia and a severe anosmia and ageusia. Roger's case presents a rare opportunity to advance our understanding of the critical functions underlying the human limbic system, and the neuropsychological and neuroanatomical data presented here provide a critical foundation for such investigations.
Introduction
Historically, the so-called “limbic system” construct was conceived on purely anatomical grounds. In 1664, the preeminent physician and anatomist, Thomas Willis, observed that a cortical border appeared to encircle the brainstem and termed this the cerebri limbus (in Latin limbus means “border” or “edge”) (Willis, 1664). Over 200 years later, Broca introduced the term, “le grand lobe limbique” to describe the same cortical regions forming the inner border of the cerebral hemispheres and speculated that these regions played a primary role in olfaction (Broca, 1878). The dawn of an emotion-related limbic system commenced in 1937 when Papez incorporated aspects of Broca's great cortical limbic lobe into the subcortically-mediated emotion theories of Cannon and Bard in order to construct his prescient emotional circuitry: “It is proposed that the hypothalamus, the anterior thalamic nuclei, the gyrus cinguli, the hippocampus, and their interconnections constitute a harmonious mechanism which may elaborate the functions of central emotion, as well as participate in emotional expression.” (Papez, 1937). Fifteen years later, MacLean formally introduced the term “limbic system” to describe an expanded version of the Papez circuit which he characterized as “a visceral brain that interprets and gives expression to its incoming information in terms of feeling, being incapable perhaps of getting at the meaning of things at the level of symbolic language.” (Maclean, 1952). The high-reaching and tantalizing theories of Papez and MacLean inspired a whole movement toward understanding the emotional limbic system; a movement which continues to this very day. At the very onset of this movement, only a few years after MacLean's original proposal, emerged the famous case of patient HM (Scoville, 1954). From this case it became readily apparent that bilateral removal of the human medial temporal lobes (including the hippocampus) primarily disrupts memory rather than emotion or feeling (Scoville & Milner, 1957). Future studies would confirm this finding and expand upon it by showing that damage to other limbic areas (such as the basal forebrain, thalamus, or mammillary bodies) also primarily disrupted memory, not emotion (for reviews see Tranel, Damasio, & Damasio, 2000; Zola-Morgan & Squire, 1993). Thus, the extant evidence suggests that the functional role of the limbic system aligns more closely with memory than it does with emotion.
There is currently no consensus in the field concerning the exact definition of what neural structures constitute the limbic system (Kotter & Meyer, 1992; LeDoux, 2000). As aptly stated by Ledoux, “after half a century of debate and discussion, there are still no agreed upon criteria that can be used to decide which areas of the brain belong to the limbic system.” (LeDoux, 2000, p. 158). Rather than argue for or against the inclusion of a particular brain region, we will define the limbic system as a set of highly interconnected brain regions situated within the medial portion of the brain. This liberal definition encompasses all the cortical regions located along the medial fringe of the cortical mantle (Broca, 1878), as well as other adjacent cortical and subcortical structures that have been added to the limbic system over the years by several prominent investigators (Heimer & Van Hoesen, 2006; Maclean, 1952; Mesulam & Mufson, 1982; Papez, 1937; Yakovlev, 1972). These regions include (in no particular order): the orbitofrontal cortex, insular cortex, anterior and posterior cingulate cortices, temporopolar cortex, parahippocampal gyrus, hippocampal formation, amygdala, basal forebrain, anterior thalamic nuclei, and hypothalamus.
We want to emphasize from the outset that we are using the term “limbic system” in a heuristic spirit, not because it has any particular anatomical or behavioral precision. In fact, due to the functional and anatomical elusiveness of the limbic system, some researchers have implored the scientific community to abandon the concept (e.g. Brodal, 1981; Kotter & Meyer, 1992; LeDoux, 2000). Others, however, continue to embrace the limbic system concept (e.g., see special issue edited by Mokler & Morgane, 2006). It is not our intention to adjudicate this issue. Rather, we would like to use the “limbic system” concept heuristically in the current report because it provides a provocative and appropriate platform for reporting a unique case in which virtually all of the key structures that we have defined as comprising the limbic system have been bilaterally damaged.
Bilateral limbic system destruction can be caused by herpes simplex virus type 1 encephalitis (HSE) (Shaw & Alvord, 1997). The severe inflammation following HSE triggers a process of necrosis that leads to the “total disintegration of the affected tissue” (Hierons, Janota, & Corsellis, 1978). Other forms of limbic encephalitis share a similar clinical presentation with HSE, but at the cellular level the neuronal damage is much sparser than the widespread hemorrhagic necrosis typical of HSE (Corsellis, Goldberg, & Norton, 1968; Tuzun & Dalmau, 2007). Only about two people per million are infected with HSE (Hjalmarsson, Blomqvist, & Skoldenberg, 2007) and over 70% of those infected will die without proper antiviral treatment (Skoldenberg et al., 1984; Whitley et al., 1986). The route of HSE's entry into the central nervous system is not clearly understood. The dominant view is that the virus lays dormant in the ganglion of the trigeminal nerve, becomes reactivated by some unknown mechanism, and then progressively infects the brain through transneuronal spread (Barnett, Jacobsen, Evans, Cassell, & Perlman, 1994). Another possible route is viral entry via the olfactory nerve following a direct infection. Once the herpes virus penetrates the central nervous system, it appears to have a striking affinity for attacking neurons located within the limbic system (Damasio & Van Hoesen, 1985). The border between damaged and non-damaged cortices is remarkably sharp, often times appearing to respect cytoarchitectonic boundaries (Damasio & Van Hoesen, 1985; Damasio, 2000; Hierons et al., 1978; Kapur et al., 1994). HSE's propensity to destroy limbic tissue while leaving much of the adjacent tissue intact is still unknown. Nevertheless, such well-demarcated bilateral lesions make HSE one of the best probes for examining limbic-related brain-behavior relationships in humans (Damasio, 2000; Kapur et al., 1994).
The current case report features an extremely rare encephalitic patient named Roger. Nearly 30 years ago – prior to critical improvements in antiviral medication – Roger had a life-threatening bout with HSE. He managed to survive the encephalitic attack, but his brain was left permanently scarred with extensive damage encompassing the bulk of his limbic system, bilaterally. The present study is dedicated to presenting Roger's complete neuroanatomical and neuropsychological profiles. Great care is also taken to discuss his current medical status in order to assess any confounding variables that can potentially alter the interpretation of other results. We offer this case in the spirit of contributing to the neuropsychological literature of detailed case studies, and also as a foundation for future empirical investigations exploring the functional correlates of the “limbic system.”
Case Overview
Roger is a 56-year-old man, fully right-handed (+100), with 16 years of education. All of his first-degree relatives are also fully right-handed. The original report of Roger's case was briefly described in a book chapter (Tranel et al., 2000). The following report represents an extensive addition to the details contained within the initial case description. In previous studies, Roger was usually identified as “RH-1951.” In this article, by written consent and preference of both the patient and his family, the name “Roger” was specifically chosen as the subject identifier and this name will continue to be used in future studies.
Life for Roger began in 1952 with no health complications and no delays in achieving developmental milestones. Based on his parents' report, Roger lived a normal childhood, attained average grades throughout school, had a good social network of friends, and enjoyed playing sports, especially baseball and football. During his early teenage years, Roger developed insulin-dependent diabetes mellitus (Type 1 diabetes). He learned to adjust his lifestyle around his diabetes and his family reports that he has always effectively monitored his glucose levels, self-administered insulin, and maintained a strict diet. Following high school, Roger attended college and earned a BA in business administration. Uncertain of what career path to pursue, Roger spent his time enjoying outdoor activities. He was an avid skier and spent the winters helping with the day to day operations at a local ski resort. During the summers, Roger worked at Yellowstone National Park and spent much of his free time hiking and enjoying the tranquility of his surroundings. During this time period, Roger's family describes him as being a “friendly, easy-going guy” who was “quiet, reserved, and usually kept to himself.” While at Yellowstone, Roger met a woman who motivated him to pursue a career capable of supporting a family. He enrolled in a manager training program and became an assistant manager for a large department store. A few months later, at the age of 28, Roger developed a high fever, nausea, and an intense headache. The emergency room physician sent him home with a diagnosis of influenza. When Roger failed to show up to work later in the week, his coworkers became worried and went to his apartment where they found him lying unconscious. He was rushed to the hospital where he was diagnosed with herpes simplex virus type 1 encephalitis and administered the antiviral agent vidarabine (ara-A). Roger's prognosis looked bleak and his family was told there was a strong likelihood he would not survive. After a nine day coma, Roger's condition stabilized and he slowly emerged from the coma, completely disoriented. A few weeks later he was discharged from the hospital with normal vision and hearing, sufficient strength and motor coordination, and a severe amnesia, anosmia, and ageusia.
Since the encephalitic attack in 1980, Roger has literally lived another lifetime. However, for Roger, not much has changed over the past 28 years. He has virtually no episodic memories for any events which have transpired over the past three decades. For example, he has no recollection of 9/11 and when shown pictures of the planes crashing into the World Trade Center he often responds with bewilderment, speculating that Russia must be attacking America. At times, Roger confabulates, although his confabulations are generally non-bizarre and are usually provoked by memory-related questioning. He has no idea how many years have passed since the encephalitis, and when asked, his answers range from a few years to a few decades. His insight into his own condition is markedly impoverished. For example, Roger exhibits a complete anosognosia for his anosmia and ageusia. On occasion, only when directly asked, Roger might admit to having some problems with his memory. However, these problems are always downplayed and do not seem to disturb or upset him even though their severity has entirely precluded him from living an independent life and obtaining any sort of gainful employment. It could be said that he “doesn't remember that he doesn't remember.”
Up until 2003, Roger lived under the close supervision of his parents. Due to his parents' aging, he has moved into an assisted-care facility specialized for patients with brain injury. One element of Roger's behavior that must be closely supervised is his voracious appetite. Without monitoring, Roger will eat to the point of purging, showing no signs of satiation or fullness, and no memory for how much food has already been consumed. Interestingly, his appetite is still discriminative, as he will fastidiously avoid foods with high sugar content such as non-diet soft drinks and candy. Roger also has a compulsive tendency to collect objects of questionable value (e.g., matchbooks, pens, shiny metal objects, cottonballs, napkins, etc.) and hold onto them for no reason or particular purpose (Anderson, Damasio, & Damasio, 2005 – subject AP1). During his free time, Roger frequently plays solitaire or listens to his extensive collection of 1960's rock n' roll vinyl albums (he has an impressive ability to hear a song from this time period and produce the name of the song, the name of the artist, as well as the name of the B-side song). He is also an excellent bowler and participates in a competitive weekly bowling league.
Roger appears remarkably unconcerned by his condition. He hardly ever complains, and in general, shows little worry for anything in life. Both of his parents and his sister fervently claim that “Roger is always happy,” an observation that is consistent with our own impression. Moreover, based on his family's report, Roger is paradoxically happier now than he was before his brain damage. This profound personality and affect change has also altered his social behavior. His premorbid disposition of being somewhat reserved and introverted has shifted to being outgoing and extraverted. In everyday life, Roger will often approach complete strangers, with no hesitation, and with no regard for social signals and contextual cues indicating otherwise. Consistent with these observations, Roger was found to rate pictures of complete strangers as significantly more trustworthy and approachable than healthy comparison participants (Adolphs et al., 1998 – subject RH). During all social encounters, Roger has a strong proclivity towards jocularity and routinely recites jokes that are haphazardly handwritten in a notebook he keeps in his pocket. A quote found in this notebook has become Roger's life motto: “A good time to laugh is anytime you can.” Roger is also a master of puns and has an uncanny ability to produce rich commentary about trivial aspects of his immediate environment. Indeed, a clinical psychologist who saw Roger in 1988 noted in his report that “Roger plays creatively and artistically with the nuances of language as if language was his toy.” In many ways, Roger's loquacious speech and jocoseness is a form of vocal disinhibition, where his inner thoughts often appear to be freely spoken without a filter and without reflection.
Roger's condition is stable. Since his referral to our laboratory in 1994, we have tested him on numerous occasions. Over the course of the past 14 years, we have not observed any changes in his personality or affect. Indeed, if it were not for his receding hairline, one would wonder whether Roger was aging at all. Roger's complacent and easy-going nature makes him a very pleasant and straightforward patient to test. He happily complies with all testing procedures, always puts forth his best effort, stays alert and attentive, and has excellent cognitive stamina.
Neuropsychological Profile
Over the course of numerous visits to our laboratory, Roger has completed an extensive battery of neuropsychological tests and the results are presented in Tables 1–7. One of the most striking findings is the substantial degree of preserved functioning across many different cognitive domains (with the exception of memory). Below, the results for each domain will be discussed in greater detail.
Table 1.
Intellect and Academic Achievement
| Test | Score | %ile | Year Administered | Interpretation |
|---|---|---|---|---|
| Full-Scale IQ - WAIS-III | 106 | 66 | 1999 | average |
| Full-Scale IQ - WAIS-R | 107 | 68 | 1994 | average |
| Full-Scale IQ - WAIS | 115 | 84 | 1981 | high average |
| National Adult Reading Test - Revised | 108 | 70 | 1994 | average |
| Performance IQ - WAIS-III | 106 | 66 | 1999 | average |
| Performance IQ - WAIS-R | 99 | 47 | 1994 | average |
| Performance IQ - WAIS | 119 | 90 | 1981 | high average |
| Processing Speed Index - WAIS-III | 86 | 18 | 1999 | low average |
| Verbal Comprehension Index - WAIS-III | 107 | 68 | 1999 | average |
| Verbal IQ - WAIS-III | 105 | 63 | 1999 | average |
| Verbal IQ - WAIS-R | 113 | 81 | 1994 | high average |
| Verbal IQ - WAIS | 112 | 79 | 1981 | high average |
| Wechsler Test of Adult Reading | 112 | 79 | 2007 | high average |
| WRAT3 - Arithmetic | 106 | 66 | 1999 | average |
| WRAT3 - Reading | 105 | 63 | 1999 | average |
| WRAT3 - Spelling | 106 | 66 | 1999 | average |
| WRAT4 - Math Computation | 112 | 79 | 2007 | high average |
| WRAT4 - Reading Composite | 107 | 68 | 2007 | average |
| WRAT4 - Sentence Comprehension | 113 | 81 | 2007 | high average |
| WRAT4 - Spelling | 100 | 50 | 2007 | average |
| WRAT4 - Word Reading | 101 | 53 | 2007 | average |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Table 7.
Mood, Personality, and Psychiatric Assessment
| Test | Score | Interpretation |
|---|---|---|
| Beck Anxiety Inventory | 1 (raw score) | not anxious |
| Beck Depression Inventory-IA (BDI-IA) | 5 (raw score) | not depressed |
| Beck Depression Inventory-II (BDI-II) | 5 (raw score) | not depressed |
| MMPI-2 | (t-scores) L(70)-F(55)-K(66) Hs(57)-D(57)-Hy(50) Pd(50)-Mf(44)-Pa(42) Pt(57)-Sc(55)-Ma(43) Si(55) |
normal |
| PANAS - General Negative Affect | 10 (raw score) | low |
| PANAS - General Positive Affect | 28 (raw score) | normal |
| Spielberger State Anxiety Inventory | 33 (raw score) | normal |
| Spielberger Trait Anxiety Inventory | 36 (raw score) | normal |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Intellect and Academic Achievement (Table 1)
Roger has an above average intelligence that has remained remarkably stable over the years; the data show no hint of decline over more than two decades of testing. For example, in 1981 (one year after his brain damage), a neuropsychological report stated that his full-scale IQ was 115 on the original Wechsler Adult Intelligence Scale (WAIS). In 1994, he obtained a full-scale IQ of 107 on the WAIS-R, entirely consistent with the expected 8-point difference between the WAIS and WAIS-R observed in the normative data. More recently, we tested him on the WAIS-III and his full-scale IQ was 106. The enduring stability of Roger's intelligence is also evident in his verbal and performance IQ scores, both of which are consistently above average. Roger does show a slight weakness on tests involving processing speed demands (a common finding in most brain-injured populations). His academic achievement in math, reading, and spelling – as measured by the Wide Range Achievement Test (WRAT) – is also in the average to above average range and has remained stable over the years.
Working Memory, Attention, and Executive Function (Table 2)
Table 2.
Working Memory, Attention, and Executive Function
| Test | Score | %ile | Interpretation |
|---|---|---|---|
| Booklet Category Test | 44 errors (t-score = 40) | 16 | low average |
| Controlled Oral Word Association Test (Form A) | 40 words | 63 | average |
| Digit Span - WAIS-III | SS=9 (max F=6, B=6) | 39 | average |
| Letter-Number Sequencing - WAIS-III | SS=9 (max=6) | 39 | average |
| Matrix Reasoning - WAIS-III | SS=13 | 86 | high average |
| Mental Control - WMS-III | SS=9 | 39 | average |
| Spatial Span | SS=13 (max F=6, B=7) | 86 | high average |
| Stroop - Color Score | 42 (t-score) | 21 | low average |
| Stroop - Color Word Score | 51 (t-score) | 55 | average |
| Stroop - Interference Score | 58 (t-score) | 79 | high average |
| Stroop - Word Score | 40 (t-score) | 16 | low average |
| Tower of Hanoi | 120 moves (all 4 trials) | defective | |
| Tower of London | Excess moves = 9 (12% above optimal strategy) Average time per trial = 18 sec |
normal | |
| Trail-making Test (Part A) | 27 seconds (t-score = 47) | 39 | average |
| Trail-making Test (Part B) | 53 seconds (t-score = 51) | 55 | average |
| Wisconsin Card Sorting Test | 46 (t-score) # correct = 68, # errors = 23, # perseverative errors = 17, # categories completed = 6 |
34 | average |
| WMS-III -Working Memory Index | 108 | 70 | average |
| WMS-R - Attention/Concentration Index | 108 | 70 | average |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Roger manifests mostly intact functioning in the domains of working memory, attention, and executive functioning. Moreover, on repeated assessment over the course of 13 years, his scores have remained completely stable. His working memory skills are consistently in the average to above average range. His maximum digit span is 6 (both forward and backward) and his maximum spatial (tapping) span is 6 forward, and surprisingly, 7 backward. Roger's scores on tests measuring attention, including more complex forms of selective and divided attention, are normal and fall squarely within expectations for someone of his age and education. His Trails performances (both A and B) are in the average range, as is his Letter-Number Sequencing. On the Color-Word Stroop, he has an interference T-score of 58 which suggests he can effectively inhibit the prepotent response and overcome the interference. Similarly, on the Wisconsin Card Sorting Test, Roger shows good cognitive flexibility and is able to rapidly and accurately shift his responses when there is a change in the rules. Roger's performances on the Tower tests are more variable. On the Tower of Hanoi, he shows no learning across trials and performs poorly within trials. Recent evidence, however, suggests that declarative memory plays a vital role in learning the recursive strategy for solving the Tower of Hanoi (Xu & Corkin, 2001). Thus, Roger's poor performance on the Tower of Hanoi does not necessarily indicate poor planning skills, and in fact, his basic planning skills appear to be relatively intact as evidenced by his normal performance on the Tower of London (a task with minimal declarative memory demands). Roger shows good verbal fluency skills as evidenced by his performance on the Controlled Oral Word Association Test (COWAT). His abstract reasoning ranges from low average (based on the Booklet Category Test) to high average (based on the matrix reasoning subtest of the WAIS-III). Overall, across a series of standardized neuropsychological tests, his working memory, attention, and executive functioning skills appear largely intact, stable, and well within the normal range.
Speech and Language (Table 3)
Table 3.
Speech and Language
| Test | Score | %ile | Interpretation |
|---|---|---|---|
| Benton Writing Assessment | normal | ||
| Boston Diagnostic Aphasia Exam - Reading Sentences and Paragraphs | 9 (raw score) | normal | |
| Boston Naming Test | 49 (raw score) | defective | |
| Controlled Oral Word Association Test (Form A) | 40 words | 63 | average |
| Naming - Animals | 94% | normal | |
| Naming - Fruits and Vegetables | 83% | defective | |
| Naming - Iowa Famous Faces Test | 94% | normal | |
| Naming - Iowa Famous Landmarks Test | 95% | normal | |
| Naming - Musical Instruments | 87% | normal | |
| Naming - Tools | 86% | defective | |
| Naming - Utensils | 96% | normal | |
| Naming - Vehicles | 100% | normal | |
| National Adult Reading Test - Revised | 108 | 70 | average |
| Recognition - Animals | 77% | defective | |
| Recognition - Fruits and Vegetables | 88% | normal | |
| Recognition - Iowa Famous Faces Test | 41% | defective | |
| Recognition - Iowa Famous Landmarks Test | 59% | borderline impaired | |
| Recognition - Musical Instruments | 94% | normal | |
| Recognition - Tools | 98% | normal | |
| Recognition - Utensils | 100% | normal | |
| Recognition - Vehicles | 100% | normal | |
| Token Test (Multilingual Aphasia Exam) | 44 (raw score) | normal | |
| Vocabulary - WAIS-III | SS=10 | 50 | average |
| Wechsler Test of Adult Reading | 112 | 79 | high average |
| WRAT4 - Reading Composite | 107 | 68 | average |
| WRAT4 - Sentence Comprehension | 113 | 81 | high average |
| WRAT4 - Spelling | 100 | 50 | average |
| WRAT4 - Word Reading | 101 | 53 | average |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Roger seamlessly produces fully intelligible speech that is fluent, nonparaphasic, and well articulated. The paralinguistic aspects of his communication, including gestures and prosody, are also intact, endowing Roger with a veritable ever-present “twinkle in the eye.” His scores on tests measuring reading, writing, and spelling are entirely normal. He shows no evidence of aphasia when tested on selected subtests of the Multilingual Aphasia Examination and the Boston Diagnostic Aphasia Examination. In everyday conversation, Roger demonstrates good verbal fluency skills along with an ample vocabulary, consistent with his normal performances on the COWAT and the WAIS-III Vocabulary Test. Roger has excellent oral comprehension as indicated by his ability to closely follow all test instructions and by his ceiling performance on the Token Test. He also has good written comprehension as evidenced by his above average performance on the Sentence Comprehension portion of the WRAT4. Roger's performance on the Boston Naming Test was mildly defective, suggesting some difficulties with naming common objects. Likewise, when shown color photographs of various objects across a range of categories, Roger had mild defects in naming tools, fruits, and vegetables. He also had significant trouble recognizing pictures of living entities, including animals and pictures of famous faces. However, in instances where Roger recognized the animal or person, he was also able to produce the appropriate name. Similar naming and recognition deficits, especially for living entities, have also been found in other HSE patients (Barbarotto, Capitani, & Laiacona, 1996; Gainotti, 2000; Tranel, Feinstein, & Manzel, 2008; Warrington & Shallice, 1984). Roger's sense of familiarity for faces is also defective. For example, Roger rated only about half of the faces on the Iowa Famous Faces test as being “familiar.” Likewise, in everyday life, Roger has great difficulty distinguishing familiar people from strangers, often times approaching complete strangers as if they are people whom he knows.
Visual Functioning (Table 4)
Table 4.
Visual Functioning
| Test | Score | %ile | Interpretation |
|---|---|---|---|
| Benton Facial Recognition Test | 44 (raw score) | 41 | average |
| Block Design - WAIS-R | SS=17 | 99 | very superior |
| Drawing to dictation - Clock | normal | ||
| Drawing to dictation - House | normal | ||
| Grooved Pegboard (left hand) | 73 sec (t-score = 46) | 34 | average |
| Grooved Pegboard (right hand) | 75 sec (t-score = 35) | 7 | borderline impaired |
| Hooper Visual Organization Test | 57 (t-score) | average | |
| Judgment of Line Orientation | 30 (raw score) | normal | |
| Perceptual-Organization Index - WAIS-III | 116 | 86 | high average |
| REY-O Complex Figure Test - Copy | 32 (raw score) | normal |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Roger has entirely normal visuospatial, visuoperceptual, and visuoconstructional abilities. He scored in the high average range on the Perceptual-Organization Index of the WAIS-III and his performance on the Judgment of Line Orientation test was perfect. Roger also performed well on the Hooper Visual Organization Test which requires one to mentally rearrange pieces of an object. On the Benton Facial Recognition Test, Roger was able to make fine-grained discriminations between unfamiliar faces. On the Grooved Pegboard test, Roger was slightly slower with his right hand compared to his left hand, although, only by 2 seconds. He had no difficulty copying a complex figure or drawing a clock or a house. Likewise, his performance on the Block Design test was in the very superior range (99th percentile), suggesting excellent visuoconstructional abilities.
Retrograde Memory (Table 5)
Table 5.
Retrograde Memory
| Test | Score | Interpretation |
|---|---|---|
| Boston Famous Faces Test - 1950's | 25% | |
| Boston Famous Faces Test - 1960's | 63% | |
| Boston Famous Faces Test - 1970's | 38% | |
| Boston Remote Memory Test - Recall 1950's | 38% | defective |
| Boston Remote Memory Test - Recall 1960's | 88% | normal |
| Boston Remote Memory Test - Recall 1970's | 50% | defective |
| Boston Remote Memory Test - Recognition 1950's | 25% | defective |
| Boston Remote Memory Test - Recognition 1960's | 75% | normal |
| Boston Remote Memory Test - Recognition 1970's | 50% | defective |
| Information - WAIS-R | SS=12 | high average |
| Iowa Autobiographical Memory Questionnaire – Early childhood and adolescence (0–18 years old) | 97% | normal |
| Iowa Autobiographical Memory Questionnaire – Young adulthood (18–39 years old) | 68% | defective |
| Iowa Famous Faces Test - 1950's | 47% | |
| Iowa Famous Faces Test - 1960's | 58% | |
| Iowa Famous Faces Test - 1970's | 31% | |
| Squire's Remote Memory Test for Public Events - Recall 1950's |
22% | defective |
| Squire's Remote Memory Test for Public Events - Recall 1960's |
25% | defective |
| Squire's Remote Memory Test for Public Events - Recall 1970's |
11% | defective |
| Squire's Remote Memory Test for Public Events - Recognition 1950's |
44% | defective |
| Squire's Remote Memory Test for Public Events - Recognition 1960's |
54% | defective |
| Squire's Remote Memory Test for Public Events - Recognition 1970's |
48% | defective |
| Verfaellie's Remote Memory for Words - Recall 1950's and prior |
94% | normal |
| Verfaellie's Remote Memory for Words - Recall 1960's |
90% | normal |
| Verfaellie's Remote Memory for Words - Recall 1970's |
73% | borderline impaired |
| Verfaellie's Remote Memory for Words - Recognition 1950's and prior |
96% | normal |
| Verfaellie's Remote Memory for Words - Recognition 1960's |
96% | normal |
| Verfaellie's Remote Memory for Words - Recognition 1970's |
79% | defective |
| Vocabulary - WAIS-III | SS=10 | average |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
Roger was administered a large battery of retrograde memory tests. The critical point of reference is October of 1980 when Roger was 28 and had his encephalitis. His autobiographical memory was examined using the Iowa Autobiographical Memory Questionnaire, an interview based questionnaire that validates all answers with family members (Tranel & Jones, 2006). His memory for autobiographical events occurring during early childhood and adolescence (up to 18 years old) was within the normal range. However, in a study specifically probing emotional autobiographical memory (Buchanan, Tranel, & Adolphs, 2005 – subject 1951), Roger demonstrated a robust positivity bias for memories occurring up through young adulthood; he readily recalled highly pleasant memories, whereas his recall of highly unpleasant memories was markedly reduced. Beginning in the early 1970's, Roger showed evidence of significant memory loss. For example, Roger could not remember any details of his sister's wedding (which occurred in 1975) despite the fact that it was a large wedding in which he played a prominent role. This finding of severely impoverished memory during the 1970's (when Roger was in his twenties) was corroborated by a series of standardized memory tasks. In Squire's Remote Memory Test for Public Events, Roger showed essentially no recall of significant public events occurring in the 1970's, whereas his recall of events in the 1960's was somewhat better. Likewise, on the Boston Remote Memory Test (which also assesses knowledge for important public events), Roger showed extremely impoverished recall and recognition for events in the 1970's, but largely intact recall and recognition for events in the 1960's. In two different tests examining recall and recognition for famous faces, Roger showed a nearly two-fold improvement when shown pictures of 1960's famous faces compared with 1970's famous faces. His memory for public events and famous faces from the 1950's was also found to be deficient when compared with the 1960's, a finding that might be partially explained by the fact that Roger was quite young during this time period. Another factor potentially contributing to the modest retrograde memory impairments found during early-life periods is the observation that Roger led somewhat of a nomadic lifestyle prior to his brain damage, suggesting that he may not have been particularly interested in public figures and events. Roger's remote semantic memory is largely intact as evidenced by his performance on the Vocabulary and Information subtests of the WAIS-III. Likewise, his recall and recognition of words introduced into the English lexicon prior to 1970 is completely normal, whereas his recall and recognition of words introduced after 1970 is markedly impoverished (Verfaellie, Reiss, & Roth, 1995). Based on the results across this wide range of tests, a clear pattern emerges; Roger has a temporally graded retrograde amnesia (for both episodic and semantic information) that is most apparent during the 10 years preceding the onset of his brain damage. Memories for events occurring before 1970 are less impaired than more recent memories, although his low scores on certain tests (e.g., Squire's Remote Memory Test for Public Events) suggest mild to moderate retrograde memory impairments that extend throughout his lifetime. Clearly, however, his retrograde memory for events occurring after the early-1970's is virtually non-existent.
Anterograde Memory (Table 6)
Table 6.
Anterograde Memory
| Test | Score | %ile | Interpretation |
|---|---|---|---|
| Benton Visual Retention Test (Form C) | 6 correct, 5 errors | defective | |
| Logical Memory (Prose Delayed Recall) - WMS-III |
SS=2 (raw score=1) | extremely impaired | |
| Logical Memory (Prose Immediate Recall) - WMS-III |
SS=5 (raw score=23) | borderline impaired | |
| Mirror Tracing (Triangle) - # errors | Trials 1–5: 11, 9, 7, 4, 2 30 min delay (trials 6 and 7): 2, 3 5 hour delay (trials 8 and 9): 3, 3 |
normal | |
| Mirror Tracing (Triangle) - Time to complete (seconds) | Trials 1–5: 44, 34, 23, 16, 18 30 min delay (trials 6 and 7): 18, 17 5 hour delay (trials 8 and 9): 15, 18 |
normal | |
| REY Auditory Verbal Learning Test (Form 1) | Trials 1–5: 5-7-9-5-9 30 min recall: 1 30 min recognition: 17/30 |
borderline immediate recall defective delayed recall defective delayed recognition |
|
| REY-O Complex Figure Test - 30 min recall | 4 (raw score) | defective | |
| Verbal Paired Associates (Delayed Recall) - WMS-III |
SS=5 (raw score=0) | extremely impaired | |
| Verbal Paired Associates (Immediate Recall) - WMS-III |
SS=6 (raw score=4) | borderline impaired | |
| Warrington Recognition Memory Test - Faces | 34 (raw score) | defective | |
| Warrington Recognition Memory Test - Words | 33 (raw score) | defective | |
| WMS-III - Auditory Delayed | 61 | <1st | extremely impaired |
| WMS-III - Auditory Immediate | 74 | 4 | borderline impaired |
| WMS-III - Auditory Recognition Delayed | 65 | 1 | extremely impaired |
| WMS-III - General Memory | 57 | <1st | extremely impaired |
| WMS-III - Immediate Memory | 55 | <1st | extremely impaired |
| WMS-III - Visual Delayed | 65 | 1 | extremely impaired |
| WMS-III - Visual Immediate | 49 | <1st | extremely impaired |
| WMS-R - Delayed Recall Index | 53 | <1st | extremely impaired |
| WMS-R - General Memory Index | 75 | 5 | borderline impaired |
| WMS-R - Verbal Memory Index | 77 | 6 | borderline impaired |
| WMS-R - Visual Memory Index | 78 | 7 | borderline impaired |
Note: For all tables, scores are reported as standard scores, unless otherwise noted. Scores followed by a “%” indicate percent correct. SS=scaled score. When available, all scores were corrected for age, education, and gender. Interpretations are based on standard neuropsychological convention. For scores which have not been normalized, an interpretation of “normal” refers to scores within 2 standard deviations of the mean and an interpretation of “defective” refers to scores greater than 2 standard deviations below the mean.
As previously mentioned, Roger's brain damage has produced a profound anterograde amnesia for both verbal and non-verbal declarative information. On the Wechsler Memory Scale-III, he obtained a General Memory Index score of 57 which is severely impaired. This creates a nearly 50-point discrepancy between his Full Scale IQ and his General Memory Index (IQ minus MQ = 49). This considerable disparity is of the same magnitude as other gold-standard amnesia cases in the literature such as patient H.M. who has a 46-point difference (Schmolck, Kensinger, Corkin, & Squire, 2002). Another significant discrepancy arises when comparing Roger's visual immediate memory (index score=49) to his auditory immediate memory (index score=74). Considering that the visual immediate memory tasks are predominantly non-verbal and the auditory immediate memory tasks are predominantly verbal, we suspect that the asymmetry in his visual versus auditory immediate memory is directly related to his asymmetry in brain damage (right hemisphere > left hemisphere). Moreover, we have found that this asymmetry extends into the retrograde direction such that Roger can provide accurate verbal descriptions of geographical places that he knows well (e.g., Yellowstone National Park and Bridger Bowl Ski Area), but cannot generate accurate drawings or other non-verbal depictions of these places (Tranel et al., 2000). It's important to note that in regard to his anterograde memory defect, the verbal/non-verbal asymmetry tends to disappear following a short delay (i.e., a delay of more than a few minutes), due to the fact that memory for both types of material is severely impaired. For example, his performance on the Warrington Recognition Memory Test was equally defective for both faces and for words. On the most recent administration of the Rey Auditory-Verbal Learning Test, Roger was able to recall 9 out of 15 words after the fifth presentation. However, he could only recall 1 word following a 30-minute delay and had essentially chance recognition performance (17/30). Similarly, following a 30-minute delay on the Complex Figure Test, Roger was unable to recall the figure. When further cued, Roger confabulated and proceeded to draw a rectangular plot of land where cows were grazing around a pool (a configuration which by sheer luck earned him a score of 4 out of 36 possible points).
Roger was also tested on a number of non-declarative memory tasks. He showed completely normal procedural learning on the mirror tracing task that was retained at both a 30-minute delay and a 5-hour delay. The intact learning on the mirror tracing task took place despite the fact that Roger could not explicitly remember having done the task before. When tested on additional procedural memory tasks that model real-world activities (e.g., weaving or driving), Roger showed intact learning that in some instances was retained for over a 2-month delay (Cavaco, Anderson, Allen, Castro-Caldas, & Damasio, 2004 – subject 3; Anderson et al., 2007 – subject AP1). Roger also demonstrated an ability to learn new habits – albeit, rather bizarre habits – in that following his brain damage he started exhibiting a compulsive tendency to collect rather valueless objects (Anderson et al., 2005 – subject 6). Another non-declarative memory process that was formally tested in Roger was fear conditioning (Bechara et al., 1995 – subject RH-1951). Presumably due to his bilateral amygdala damage, Roger was unable to form an emotional association between the unconditioned stimulus and the conditioned stimulus. Taken together, these findings add to the corpus of data supporting the existence of multiple memory systems in the brain (Squire, 1992).
Emotion, Mood, Personality, and Psychiatric Assessment (Table 7)
In terms of basic emotion recognition, Roger shows a specific impairment in recognizing anger from pictures of facial expressions (Adolphs et al., 1999 – subject RH; Adolphs & Tranel, 2003 – subject RH). Somewhat surprisingly, Roger does not demonstrate significant impairments in recognizing other emotions in facial expressions, such as fear or disgust, despite the fact that he has both amygdala and insula damage. In terms of emotion expression, most conversations with Roger involve animated speech that is replete with prosody, gesture, and often times, laughing. He readily displays signs of positive emotion including happiness, amusement, interest, and excitement. As previously noted, Roger's positive mood has remained essentially unchanged over the nearly three decades that have passed since his brain injury. Roger's parents, whom he lived with for over 24 years post-encephalitis, claim that they have never witnessed a change in Roger's mood that lasted for more than a few minutes. On occasion, Roger will display short bouts of anger, usually in situations where he feels his independence is being hindered (e.g., when a caregiver won't let him eat an apple because his blood sugar level is elevated). However, the anger dissipates often as rapidly as it was triggered. In general, Roger appears to experience little, if any, negative emotion. On the trait version of the Positive and Negative Affect Schedule (PANAS), Roger's self-report of experiencing negative affect was at the lowest possible level, whereas, his positive affect level was in the normal range. His scores on the Beck Depression Inventory (filled out on two different occasions separated by over a decade in time) indicate no evidence of any depression. Similarly, his scores on the Beck Anxiety Inventory and the Spielberger State-Trait Anxiety Inventory indicate no evidence of any anxiety. On the Minnesota Multiphasic Personality Inventory-2 (MMPI-2), Roger showed no significant elevations on any of the clinical scales and had a completely normal profile. Likewise, on a standardized clinical interview (MINI International Neuropsychiatric Interview) assessing for the presence of DSM-IV-TR Axis I diagnoses, Roger did not endorse any symptoms indicative of psychiatric illness. It should be noted that many of these self-report instruments contain a retrospective component (e.g., how have you felt over the past two weeks), which brings into question their validity when used in patients with severe amnesia. Future investigations with Roger will attempt to collect real-time emotion and mood measurements across a large time span in order to more validly assess his affective experience. Irrespective of this issue, Roger's overall lack of distress in everyday life is a striking feature of his presentation that stands in stark contrast to the extreme severity of his amnesic condition. Interestingly, other famous amnesic cases also seem to exhibit very little distress or concern for their condition (Tate, 2002). Taken together, these data confirm that Roger has no psychiatric problems and no evidence of any form of psychopathology.
Medical Profile
In 2007, while being tested at Iowa, Roger received a complete medical workup and neurological examination. In this section we discuss Roger's current medical status in order to assess any confounding variables that could potentially alter the interpretation of his experimental data.
Roger is 5 feet, 6 inches tall and weighs 183 pounds. Based on his BMI of 29.5, he is overweight but not obese. He does not currently smoke or drink alcohol, and has completely refrained from smoking and drinking ever since his encephalitic attack. In the days following his encephalitis, Roger had a few seizures for which he was prescribed a prophylactic anticonvulsant that was discontinued after six months; he has had no further seizures. He has a history of hypercholesterolemia, hypothyroidism, and hypertension. However, all of these conditions are well controlled by his current medication regimen which includes Simvastatin, Levothyroxine, and Enalapril. In a blood test conducted at Iowa in 2007, Roger's lipid levels and thyroid hormone levels were all within the normal range. His vital signs and 12-lead electrocardiogram were also within the normal range (body temperature = 97°F, heart rate = 82 beats per minute, and blood pressure = 114/63).
As noted earlier, Roger's brain damage has abolished his sense of smell and taste. He is completely anosmic and performed at chance-level on a standardized smell identification test. He is also densely ageusic and is unable to distinguish between water, salt, and sugar on forced choice. Beyond smell and taste, Roger's other senses appear to be grossly intact. His hearing is normal and his vision is slightly myopic. His visual fields are full to confrontation and his color vision is intact as confirmed by normal performance on the Ishihara Test for Color Blindness. He has normal discriminative touch, bilaterally, but moderate difficulty with stereognosis and graphesthesia in his left hand. He has no Romberg sign and normal proprioception. His motor strength, coordination, and gait are normal as well.
Diabetes
As previously mentioned, Roger has had Type 1 diabetes for over four decades. Despite his dense amnesia, Roger remains very aware that he has diabetes. He continues to self-monitor his blood glucose levels and self-administer insulin injections three times per day (short acting Novolog and long acting Lantus). His diabetes has been carefully managed by the same physician for many years. Roger's past medical records indicate that he has maintained satisfactory control over his blood glucose levels. Over a two-week time period during which Roger was testing at Iowa, his blood glucose was measured 68 different times (both before and after meals) and had a combined average level of 156 mg/dl (his preprandial average was 130 mg/dl). While slightly on the higher end of the spectrum, these average levels are still within the recommended target range for adults with diabetes (American Diabetes Association, 2008). On individual measurements his blood sugar level did demonstrate periodic fluctuations. Despite these occasional fluctuations, his hemoglobin A1c level during this same time period was 7.3%, indicating adequate blood glucose control (his average hemoglobin A1c level during the past three years is 7.8%)1.
A thorough search through Roger's medical record indicates that classic signs of diabetic neuropathy are absent. Monofilament testing on four different occasions during the past three years has revealed normal sensation, bilaterally, with no evidence of diabetic foot ulcerations. The neurological exam in 2007 confirmed that he has no signs of retinopathy or neuropathy. Light touch was normal in both the hands and the feet. He could also feel deflection of single hairs on the dorsa of the toes. He exhibited preserved ankle jerk reflexes and intact distal leg sensation. Based on this clinical profile, the neurologist concluded that there was no evidence of diabetic neuropathy.
In order to further rule out any possibility of peripheral neuropathy, quantitative sensory testing was conducted using the gold-standard Semmes-Weinstein monofilament examination (Perkins, Olaleye, Zinman, & Bril, 2001; Perkins & Bril, 2002). The testing was performed in a blinded manner with stepwise increases in monofilament strength and interspersed sham stimulations. Multiple sites were tested, bilaterally, including the medial and lateral eminence of the palm, the dorsum of the hand, the volar wrist, the dorsum of the forearm, and the plantar surface of the lateral midfoot. Correct responses required the positive identification of a stimulus following application of the filament and the appropriate localization of the site of stimulation. At all sites, Roger had completely normal touch sensation using a calibrated 10-gram monofilament (the filament most commonly used to diagnosis peripheral neuropathy) (Perkins & Bril, 2002). In fact, at all sites, Roger's pressure thresholds were found to be well below 10 grams. For example, his threshold at the volar wrist was .05 grams for the right side and .4 grams for the left side. Likewise, his threshold at the plantar surface of the lateral midfoot was .4 grams for the right side and 2 grams for the left side. Taken together, numerous independent sources of evidence – including clinical, biochemical, and experimental indices of diabetic neuropathy – all indicate that Roger does not have any signs of significant sensory neuropathy.
Neuroanatomical Profile
Three T1-weighted MRI scans were acquired on a 3.0-Tesla Siemens Trio MRI scanner (MPRAGE, AC-PC aligned coronal acquisition, TR = 2530 ms, TE = 3 ms, TI=800 ms, Flip angle = 10 degrees, FOV = 256 × 256 mm2, Slice thickness = 1 mm). The images were bias field corrected and registered together with a rigid body transformation and a sinc interpolation (AIR 3.08). The three scans were then averaged together in order to reduce motion artifacts, increase the signal-to-noise ratio, and enhance the contrast-to-noise ratio between gray and white matter.
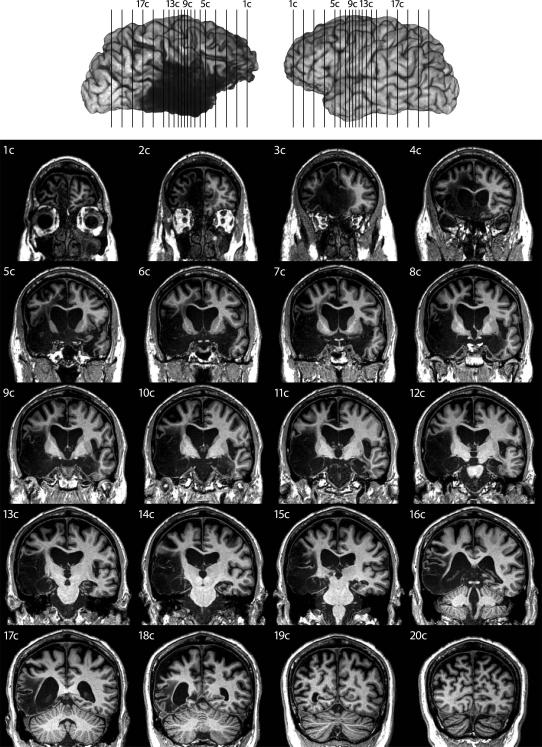
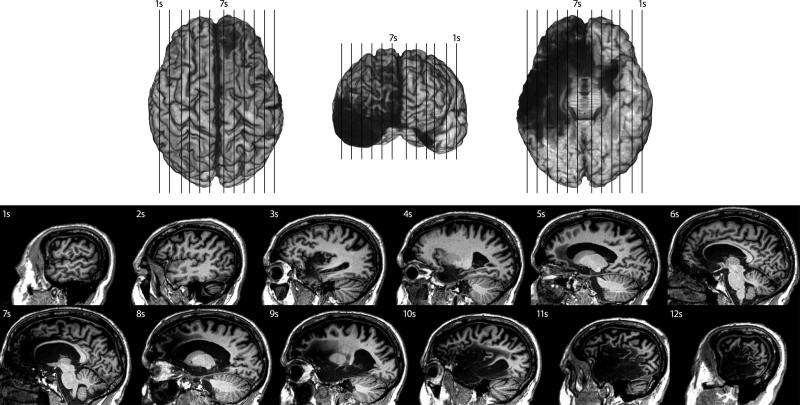
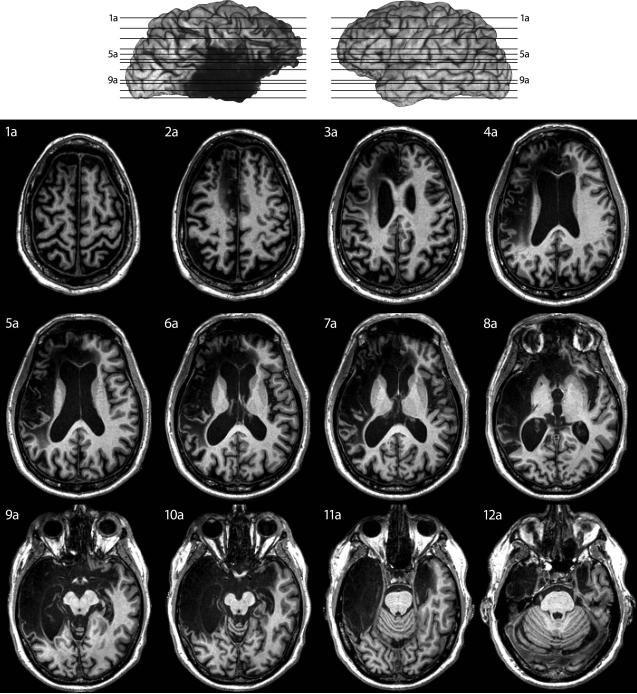
Roger's averaged MRI dataset is presented to the reader in three dimensions (Figure 1 = coronal slices, Figure 2 = sagittal slices, and Figure 3 = axial slices). Slices were specifically chosen in order to present a comprehensive picture of Roger's entire brain that captures the intricacies of his brain damage. A neuroanatomist (M. Cassell) thoroughly examined Roger's MRI and derived the following description of his lesion in collaboration with the other authors.
Figure 1.
Coronal slices of Roger's brain.
Note: All MRI images use standard radiological convention (left side=right hemisphere & right side=left hemisphere)
Figure 2.
Sagittal slices of Roger's brain.
Note: All MRI images use standard radiological convention (left side=right hemisphere & right side=left hemisphere)
Figure 3.
Axial slices of Roger's brain.
Note: All MRI images use standard radiological convention (left side=right hemisphere & right side=left hemisphere)
General appearance of the brain
The rostrocaudal length (frontal pole to occipital pole) of Roger's brain is ~17–18 cm. His ventricles are considerably larger in the right hemisphere compared to the left hemisphere. Sharply demarcated lesions are present bilaterally, with much greater damage found in the right hemisphere than the left hemisphere. Damage in the right hemisphere encompasses virtually the entire limbic system and temporal lobe (both gray and white matter), as well as significant cortical atrophy throughout much of the prefrontal cortex. The damage in the left hemisphere is largely confined to gray matter within the limbic system, without any prominent signs of atrophy on the cortical surface.
Damage to core limbic and paralimbic structures
As stated in the introduction, this case study defines the limbic system as a set of highly interconnected brain regions situated within the medial portion of the brain. These regions include (in no particular order): the orbitofrontal cortex, insular cortex, anterior and posterior cingulate cortices, temporopolar cortex, parahippocampal gyrus, hippocampal formation, amygdala, basal forebrain, anterior thalamic nuclei, and hypothalamus. Roger's damage in each of these regions is enumerated below. Brodmann Areas (BA) are occasionally used to describe certain aspects of the lesion. When appropriate, specific slices in Figures 1–3 are highlighted so that the reader can view exemplar images of damaged or spared tissue.
Orbitofrontal Cortex
The medial orbital cortex and gyrus rectus are severely damaged, bilaterally. In the right cerebral hemisphere, the entire orbital surface of the cortex (medial and lateral) is affected from the frontal pole to the anterior perforated substance. In the left hemisphere, the damage is more circumscribed and limited to posterior and medial portions of the cortex, sparing the lateral orbital gyrus and the most anterior portion of the medial orbital cortex (slice 8a).
Insular Cortex
On the right side, the entire insula is destroyed (slice 10s). The circular sulcus does not demarcate the edge of the damage which continues into the frontal, parietal and temporal opercula. The external capsule marks the deep limit of the lesion; both the extreme capsule and the claustrum appear to have been affected and can not be discerned (slice 6a). As on the right, virtually the entire left insula is damaged with the exception of what appears to be two islands of spared tissue located in dorsal regions of the anterior and posterior limits of the insula (slices 3s and 4s). In contrast to the right hemisphere, the left insula damage is clearly demarcated by the circular sulcus and does not extend into the opercula or the claustrum (slice 7a).
Anterior Cingulate
In the right hemisphere, the lesioned area includes the entire anterior cingulate region (BA24, 25, 32, and 33) spanning the subgenual area to the mid-point of the body of the corpus callosum (slice 7s). Quite remarkably, the caudal limit of the lesion appears to be located at the border between the anterior (BA24) and posterior (BA23) sectors of the cingulate gyrus (A. R. Damasio & Van Hoesen, 1985; McCormick et al., 2006; Vogt, Nimchinsky, Vogt, & Hof, 1995). In the left hemisphere, the lesioned area is restricted largely to BA24, 25, and 33. The left-sided damage includes the entire subgenual area up through the caudal limit of BA33. A large portion of BA32 in the left hemisphere – bordering on the cingulate sulcus and rostral to the genu of the corpus callosum – is also damaged. However, the more dorsal and posterior aspects of BA32 appear to be spared on the left (slice 6s).
Posterior Cingulate
In the right hemisphere, the posterior cingulate region and underlying white matter appear somewhat atrophied. The cortex over the isthmus (including the retrosplenial cortex) was shrunken and the underlying white matter was severely affected (slices 7s or 17c). The lesioned area in the isthmus was continuous with the damage in the right parahippocampal gyrus. The left posterior cingulate region appeared normal.
Temporopolar Cortex
The entire right temporal pole is destroyed. Right-sided damage includes the piriform cortex, the cortex of the limen insulae that links parahippocampal areas (BA35 and 36) with the insula, as well as BA38, BA20 and 21. Damage to the left temporal pole is confined to the medial polar cortex (BA20 and 21) and limen insulae while sparing the lateral polar cortex (BA38) and most of the adjacent white matter (slice 11a). The extent of damage to the left limen appears to include the piriform cortex and the cortex connecting the parahippocampal gyrus and insula, as on the right side.
Parahippocampal Gyrus
The parahippocampal gyrus includes the entorhinal cortex (BA28 and 34), the perirhinal cortex (BA35), and the parahippocampal region (BA36). It extends from near the temporal pole to the isthmus and is bounded by the hippocampal fissure medially and the collateral sulcus laterally. The entorhinal cortex is located more anteriorly, whereas the parahippocampal region is located more posteriorly and contains two distinct regions, usually referred to as TH and TF. Along the medial edge of the collateral sulcus is the perirhinal cortex.
In the right hemisphere, the entire right parahippocampal gyrus, including the subjacent white matter, is destroyed (slice 10s). In the left hemisphere, the entorhinal and anterior two-thirds of the perirhinal cortex appear damaged while the posterior parahippocampal gyrus (areas TH and TF) appears to be spared (slice 4s). The lesion in the parahippocampal gyrus extends to the fundus of the collateral sulcus but the remaining cortex within the sulcus is unaffected. This suggests that BA28 and 35 (i.e., the entorhinal and perirhinal cortices) were involved but not BA36 (i.e., parahippocampal region).
Hippocampal Formation
In the right hemisphere, the entire hippocampal formation (hippocampus proper or Ammon's horn, dentate gyrus, and subicular complex) appeared destroyed. Complete loss of morphological features was evident from the anteroventral pes hippocampi to the caudal tail of the hippocampus where it flattens out to continue onto the dorsal surface of the corpus callosum. No trace of the hippocampus proper, dentate gyrus, subiculum or fimbria could be identified (slice 9s).
In the left hemisphere, the anterior portion of the hippocampal formation (including the pes hippocampi) was entirely destroyed. The posterior portion contained some features of the dentate gyrus, hippocampus and fimbria that could be discerned up to the splenium. In total, about 1–2 cm of the posterior left hippocampus may have been spared (slice 4s). Based on volumetric data obtained from an older scan and reported in a previous study (Buchanan et al., 2005 – subject 1951), it is estimated that ≈20% of Roger's left hippocampus is spared. This spared segment includes the gyrus of Andreas Retzius, the fasciola cinerea and the gyrus fasciolaris, as well as continuations of the subiculum, dentate gyrus and hippocampus onto the underside of the splenium.
Amygdala
The amygdala is composed of three major regions: (1) a corticomedial region lying on the surface of the semilunar gyrus rostral to the uncus and containing boundary or transition areas with the piriform, entorhinal cortex, and hippocampus, (2) a large basal component consisting mostly of the large lateral and basal nuclei, and (3) the striatal-like extended amygdala composed of the central nucleus, the dorsal part of the substantia innominata and the bed nucleus of the stria terminalis situated in the medial basal forebrain.
The entire amygdala, including the contained white matter, appears lesioned in both hemispheres (slice 9c). The area of damage extends up to the ventral boundary of the putamen and continues anteromedially through the substantia innominata up to the medial forebrain. On this basis, it would appear that all three components of the amygdala have been completely destroyed bilaterally.
Basal Forebrain
The basal forebrain is a term that encompasses a portion of the telencephalon located anterior and lateral to the hypothalamus. Structures generally included within the basal forebrain are the forebrain cholinergic cell groups (medial septum, vertical and horizontal limbs of the diagonal band of Broca, and the basal nucleus of Meynert), the septal nuclei, the substantia innominata and the limbic striatum (including the fundus striati, olfactory tubercle, ventral pallidum, and nucleus accumbens).
The whole of the superficial and medial portions of the basal forebrain appears destroyed bilaterally (slice 6c). The lesioned area is continuous on both sides with the damage to the dorsomedial amygdalae and includes the anterior perforated substance, the olfactory tubercle, the medial and lateral olfactory striae, the septal nuclei, and the region containing the diagonal band of Broca and the basal nucleus of Meynert. At the level of the anterior commissure, which was indistinct, the medial limit of the lesioned area was the hypothalamic preoptic region which was unaffected. In contrast, the ventral pallidum and nucleus accumbens appeared largely spared, although smaller than normal, possibly indicative of atrophy. The accumbens nuclei appeared symmetrical, whereas the head of the caudate and putamen are smaller on the right side, as compared to the left. Thus, with the exception of the limbic striatum, the entire basal forebrain is destroyed.
Thalamus
The most conspicuous feature of thalamic structural changes is restricted to limbic-related nuclei in the right hemisphere (slice 12c). The right thalamus is noticeably smaller; the thalamic tubercle over the anterior thalamic nuclei is indistinct suggesting atrophy of these nuclei, the pulvinar is shrunken and the mediodorsal thalamic nucleus is greatly reduced in size. The midline thalamic nuclei were clearly atrophied but showed no evidence of necrosis. As a contrast, there appeared to be no damage or atrophy to the other thalamic nuclei; the lateral and medial geniculate bodies were bilaterally symmetrical and the ventral posterior complex appeared normal.
Hypothalamus
There was no evidence of necrosis in the hypothalamus and the only notable feature was the enlargement of the third ventricle (slice 10c). The right mammillary body was conspicuously smaller than the left mammillary body. The pituitary stalk was aligned with the midline and there appeared to be no obvious changes in the pituitary itself. In the epithalamus, the pineal appeared normal and the posterior commissure and stria medullares thalami were clearly identifiable. The habenula appeared moderately smaller on the right and there was a small region of hypodensity just beneath the habenular trigone.
Damage to other brain regions
Primary and Secondary Sensory Cortices
Roger's primary olfactory cortex (piriform) is completely destroyed, bilaterally. His primary gustatory cortex (anterior insula and frontal operculum) is also completely destroyed on the right side, but only partially damaged on the left side. In the right hemisphere, the damage completely encompasses the primary auditory cortex (Heschl's gyrus) and the vestibular cortex (parietal operculum and posterior insula). The right hemisphere damage also severely impacts the second somatosensory cortex, especially the underlying white matter. All other primary and secondary sensory cortices – including vision (bilaterally), auditory (left hemisphere only), vestibular (left hemisphere only), motor (bilaterally), and somatosensory (bilaterally except the right S2) – appear to be spared.
Frontal Lobe
In the right hemisphere, Roger's orbitofrontal and anterior cingulate damage extends outward to include the remainder of the medial surface all the way through the frontal pole (BA9, 10, 11, 12, and 32) (slice 3c). The lesion continues into the inferior frontal gyrus including the pars orbitalis, pars opercularis, as well as some minor damage to the pars triangularis (BA44, 45 and 47). Laterally, there is extreme thinning of the cortex over the middle and superior frontal gyri, including dorsolateral parts of BA6 and 8. Only the caudal part of the middle frontal gyrus, the adjacent part of the lateral superior frontal gyrus, and the upper two-thirds of the precentral gyrus appear to be spared. Medially, the damage extends throughout most of the gray and white matter in the superior frontal gyrus (including the supplementary motor area), although the paracentral lobule appears intact (slice 7s). In the left hemisphere, his frontal damage is largely confined to the ventromedial prefrontal cortex, while sparing the remainder of his frontal lobe, including the entire dorsolateral and frontopolar sectors.
Temporal Lobe
The lesion encompassed the entire right temporal lobe, from the temporal pole to the conventionally delineated boundaries with the occipital and parietal lobes. All surfaces were affected and no clear distinction between gray and white matter could be made. Rostro-medially, the damage is continuous with the lesion in the orbital and insular cortices via the limen insulae. Caudo-medially, the lesion in the parahippocampal gyrus ends at the commencement of the calcarine sulcus with some minor damage to the rostral parts of the lingual and fusiform gyri. This latter damage possibly reflects the caudal limit of the lesion to temporal areas BA36 and 20 rather than actual involvement of occipital regions. The left temporal lobe presented a much more restricted distribution of damage that is mainly confined to the limbic areas previously described.
Other Regions
In the right hemisphere, the temporal and insular damage extends into the parietal operculum and the supramarginal gyrus, particularly in the white matter. There is thinning over both the supramarginal and angular gyri on the right but the main damage is to the underlying white matter for the entire inferior parietal lobule (slice 17c). There may also be some minor damage to the anterior tip of the right inferior lateral occipital cortex (BA19). Beyond these areas of damage, the parietal and occipital lobes appear to be completely normal in appearance.
In the brainstem, the right pons is smaller than the left (slice 10a) and there is a reduction in the size of the cerebral peduncle. In the midbrain, the medial portion of the right crus cerebri is reduced (slice 9a), consistent with a loss of frontopontine fibers. The cerebellum appears normal in both hemispheres.
White matter damage
Cerebral white matter is severely affected, particularly on the right. The right fornix, especially as it proceeds along the junction with the septum pellucidum, is greatly reduced in size and can not be followed through to the right hypothalamus. Both mammillothalamic tracts can be discerned but the anterior commissure appears shrunken and less distinct. The posterior commissure appears intact. The optic chiasm is symmetrical and the infundibulum is aligned with the midline despite considerable enlargement of the third ventricle.
Beneath the gray matter of the right frontal lobe, the corona radiata and forceps minor are completely damaged. The anterior limb of the internal capsule, other than being noticeably thinner, appears to be intact. The right inferior and superior longitudinal fasciculi are severely damaged, and the right inferior frontal-occipital fasciculus is affected and the density changes can be followed almost all the way to the occipital pole. The cingulum is affected on both sides. The left cingulum damage closely follows the anterior cingulate damage, whereas, the right cingulum damage continues beneath the posterior cingulate cortex into the isthmus. The body of the corpus callosum is considerably shrunken and all that remains of the genu is a thin strip of white matter. The uncinate fasciculus on both sides is severely damaged.
Discussion
This case report presents the complete neuropsychological and neuroanatomical profiles of Roger, an extremely rare neurological patient who sustained bilateral limbic system destruction following a severe bout with herpes simplex virus type 1 encephalitis. Perhaps the single most unique aspect of this case is the sheer magnitude of Roger's brain damage. Simply looking at the MRI images or reading through the lesion description may leave one wondering how Roger is capable of functioning. Quite remarkably, not only is Roger capable of functioning, but he functions surprisingly well. Most people who meet Roger for the first time have no idea that anything is wrong. They see a normal looking middle-aged man who walks, talks, listens, and acts no differently than the average person. They might be slightly taken aback by his overly friendly behavior, or perhaps, they might be confused as to why a stranger just walked up to them and started telling jokes. They would not, however, be inclined to think that Roger is missing a substantial portion of his brain; a stark reminder that the territories of Roger's brain which are damaged, including the limbic system, are not critical for a broad range of basic life functions and behaviors.
Roger's brain and behavior have undergone a tremendous transformation in order to compensate for the massive damage inflicted by the encephalitis. The precise time course of this transformation remains a mystery. Nevertheless, given Roger's widespread frontal, temporal, and limbic damage, one might expect to find a myriad of deficits. Yet, remarkably, Roger's attention, working memory, executive functioning, speech, language, and overall intellectual functioning fall largely within the range of what one would expect for an average, healthy, non-brain-damaged middle-aged adult. Unfortunately, we will never be able to know for sure what specific impairments Roger may have manifested during the weeks and months immediately following his brain damage. The earliest data we have on record are from an IQ test administered to Roger within the first year of his brain injury. Even during this early time period, he demonstrated an above-average performance. Thus, it is unclear whether Roger's brain damage initially caused particular impairments that have since recovered, or alternatively, whether the damaged regions were never actually necessary for performing the wide range of intact behaviors evident in Roger's neuropsychological profile. In either case, compensatory mechanisms were unable to mend the devastating blow to Roger's declarative memory system. The damage has caused a temporally-graded retrograde amnesia that is most severe during the ten years preceding the encephalitic attack. Moreover, the severity of Roger's anterograde amnesia is on the same scale as other famous amnesic cases, such as patient HM (Schmolck et al., 2002), patient SS (O'Connor, Cermak, & Seidman, 1995), patient RFR (McCarthy, Kopelman, & Warrington, 2005), patient EP (Stefanacci, Buffalo, Schmolck, & Squire, 2000), Boswell (A. R. Damasio, Eslinger, Damasio, Van Hoesen, & Cornell, 1985), and Clive Wearing (Wilson, Baddeley, & Kapur, 1995).
What makes Roger's case so unique is not so much the severity of his amnesia, but rather, the severity of his brain damage. Bilaterally, Roger is missing most of his limbic system, including the orbitofrontal cortex, insular cortex, temporopolar cortex, anterior cingulate, parahippocampal gyrus, hippocampal formation, amygdala, and basal forebrain. The lesions, especially in the left hemisphere, are often sharply demarcated and appear to preferentially target the gray matter of the limbic system. The damage in the right hemisphere extends beyond the boundaries of the limbic system and includes much of the temporal lobe, prefrontal cortex, operculum, and white matter underlying the inferior parietal lobe and secondary somatosensory cortex. Additionally, the damage has severely affected many of the brain's major white matter tracts, creating a massive neural disconnection, especially in the right hemisphere. The MRI scans of Roger that have been acquired over the past 14 years appear to be highly consistent, showing virtually no change in his lesions across scans. This does not preclude the possibility that subtle changes have occurred over the years, especially degeneration of white matter pathways that might be detectable using diffusion tensor imaging. However, with the available MRI datasets, Roger's lesions appear to be stable and will likely remain this way for the remainder of his life.
While describing Roger's lesions, great effort was spent trying to distinguish regions which were clearly damaged from regions that appear to be spared. The regions of Roger's limbic system that appear to be spared include most of the hypothalamus, limbic striatum, and posterior cingulate (although, the right posterior cingulate seems to be partially damaged). The left thalamus and left posterior parahippocampal gyrus also appear to be spared, along with a small portion of the left posterior hippocampus. Clearly, however, the vast majority of Roger's limbic system is completely destroyed. It is important to note that MRI lacks the spatial resolution needed to definitively determine which brain regions are intact and free from HSE-related damage. Moreover, the inflammatory processes of HSE often extend beyond the site of overt lesion (Nicoll, Love, & Kinrade, 1993). For these reasons, post-mortem examination of Roger's brain will be critical for assessing neuronal damage not detectable using current neuroimaging methods.
The extreme rarity of Roger's lesion deserves further emphasis. Over the 30 years we have been conducting brain lesion research, we have come across only one other HSE patient (Boswell) with bilateral limbic system destruction of similar magnitude (A. R. Damasio et al., 1985; Tranel et al., 2000). Both Roger and Boswell have a very similar pattern of brain damage, especially with regard to the limbic system. There are, however, some notable differences. Roger has more extensive damage to his dorsal anterior cingulate, bilaterally. Roger also has much greater damage to non-limbic frontal and temporal regions in the right hemisphere. On the other hand, in the left hemisphere, Boswell has more extensive damage to the lateral orbitofrontal cortex and lateral temporal pole. Boswell's more extensive damage to his nonmesial left temporal lobe could very well have contributed to his more severe retrograde memory deficits for both episodic and semantic knowledge. Boswell also has complete destruction of his left hippocampus and parahippocampal gyrus, whereas the posterior portion of these regions appears to be partially spared in Roger. We suspect that Roger's relatively longer retention of verbal material (on the order of several minutes), as compared to Boswell's extremely short retention of such material (on the order of seconds), might be related to the spared tissue in the posterior portion of Roger's left medial temporal lobe. Finally, in posterior regions of the right hemisphere, there is a dorsal-ventral split, with Roger's damage extending dorsally into the parietal lobe and Boswell's damage extending ventrally into the occipital lobe. This extra damage to Boswell's occipital lobe may be related to his more profound impairments in the realm of visual recognition. Beyond Roger and Boswell, there exist only two other reported HSE cases (Friedman & Allen, 1969; Gascon & Gilles, 1973) who have extensive bilateral limbic damage beyond the medial temporal lobes that included the insular cortices, orbitofrontal cortices, basal forebrain structures, and the anterior cingulate. Interestingly, in all four of these cases, damage in the right hemisphere was much more extensive than in the left hemisphere. Also, of the four cases, Roger is the only one who is still living. Other HSE cases with extensive bilateral limbic damage exist (e.g., Hierons et al., 1978; Kapur et al., 1994), but have not been reported in great detail. Moreover, none of the more well-known HSE cases (such as Clive Wearing (Wilson, Kopelman, & Kapur, 2008), patient SS (O'Connor et al., 1995), patient RFR (McCarthy, Kopelman, & Warrington, 2005), and patient EP (Bayley, Gold, Hopkins, & Squire, 2005)) have bilateral frontal damage that includes both the anterior cingulate and the orbitofrontal cortices. In fact, almost all HSE patients with damage as extensive as Roger's do not end up surviving the encephalitic attack. Thus, based on the extant literature, Roger appears to be the only living HSE patient with bilateral limbic system destruction who is accessible to the scientific community.
In some ways, Roger may indeed be the last of his kind. Most current cases of HSE are left with relatively circumscribed unilateral lesions (e.g., Tranel et al., 2000). Much of this reduced brain damage can be attributed to the introduction of acyclovir, a potent antiviral medication (King, 1988). Unfortunately for Roger, acyclovir's efficacy was not discovered until the mid-1980's, a few years after the onset of his encephalitic attack (Kennedy, 1988; Skoldenberg et al., 1984; Whitley et al., 1986). Following acyclovir's introduction, the mortality and morbidity associated with HSE, as well as the extent of residual brain damage, were dramatically reduced (Kennedy, 1988; Rantalaiho, Farkkila, Vaheri, & Koskiniemi, 2001; Skoldenberg et al., 1984; Tyler, 2004; Whitley et al., 1986). In addition, during the early 1990's, an efficient method for quickly detecting HSE using polymerase chain reaction (PCR) was established (Al-Shekhlee, Kocharian, & Suarez, 2006; Lakeman & Whitley, 1995). Ever since these significant advances in the detection and treatment of HSE, cases of bilateral limbic system destruction have become vanishingly rare, leaving Roger as one of the last representatives of a soon-to-be extinct lesion population.
Acknowledgments
We are greatly indebted to Roger and his family for their unwavering support and continued commitment to brain research. We would also like to thank Ned N. Tranel, Melissa Duff, Ken Manzel, Kathy Jones, Ruth Henson, Nick Jones, Jocelyn Cole, Tim Salomons, Laura Frey Law, Jennifer Lee, Carol Vance, India Morrison, Satish Rao, and the many other collaborators who played an integral part in testing Roger. Supported by NINDS P01 NS19632, NIDA R01 DA022549, NSF Graduate Research Fellowship, and the Kiwanis Foundation.
Footnotes
Hemoglobin A1c, a measure of glycosylated hemoglobin, gives an accurate estimate of blood glucose levels during the previous three to four months. Hemoglobin A1c values of around 7% or lower in type 1 diabetics are indicative of good glucose control and have been associated with a lower occurrence of peripheral neuropathy (The Diabetes Control and Complications Trial Research Group, 1993).
References
- Adolphs R, Tranel D. Amygdala damage impairs emotion recognition from scenes only when they contain facial expressions. Neuropsychologia. 2003;41(10):1281–1289. doi: 10.1016/s0028-3932(03)00064-2. [DOI] [PubMed] [Google Scholar]
- Adolphs R, Tranel D, Hamann S, Young AW, Calder AJ, Phelps EA, et al. Recognition of facial emotion in nine individuals with bilateral amygdala damage. Neuropsychologia. 1999;37(10):1111–1117. doi: 10.1016/s0028-3932(99)00039-1. [DOI] [PubMed] [Google Scholar]
- Adolphs R, Tranel D, Damasio AR. The human amygdala in social judgment. Nature. 1998;393(6684):470–474. doi: 10.1038/30982. [DOI] [PubMed] [Google Scholar]
- Al-Shekhlee A, Kocharian N, Suarez JJ. Re-evaluating the diagnostic methods in herpes simplex encephalitis. Herpes. 2006;13(1):17–19. [PubMed] [Google Scholar]
- American Diabetes Association Standards of medical care in diabetes - 2008. Diabetes Care. 2008;31(Supplement 1):S12–S54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- Anderson SW, Damasio H, Damasio AR. A neural basis for collecting behaviour in humans. Brain. 2005;128(1):201–212. doi: 10.1093/brain/awh329. [DOI] [PubMed] [Google Scholar]
- Anderson SW, Rizzo M, Skaar N, Stierman L, Cavaco S, Dawson J, et al. Amnesia and driving. Journal of Clinical and Experimental Neuropsychology. 2007;29(1):1–12. doi: 10.1080/13803390590954182. [DOI] [PubMed] [Google Scholar]
- Barbarotto R, Capitani E, Laiacona M. Naming deficit in herpes simplex encephalitis. Acta Neurologica Scandinavica. 1996;93(4):272–280. doi: 10.1111/j.1600-0404.1996.tb00520.x. [DOI] [PubMed] [Google Scholar]
- Barnett EM, Jacobsen G, Evans G, Cassell M, Perlman S. Herpes simplex encephalitis in the temporal cortex and limbic system after trigeminal nerve inoculation. The Journal of Infectious Diseases. 1994;169(4):782–786. doi: 10.1093/infdis/169.4.782. [DOI] [PubMed] [Google Scholar]
- Bayley PJ, Gold JJ, Hopkins RO, Squire LR. The neuroanatomy of remote memory. Neuron. 2005;46(5):799–810. doi: 10.1016/j.neuron.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A, Tranel D, Damasio H, Adolphs R, Rockland C, Damasio AR. Double dissociation of conditioning and declarative knowledge relative to the amygdala and hippocampus in humans. Science. 1995;269(5227):1115–1118. doi: 10.1126/science.7652558. [DOI] [PubMed] [Google Scholar]
- Broca P. Anatomie comparée des circonvolutions cérébrales. le grand lobe limbique et la scissure limbique dans la série des mammiferes. Rev Anthropol. 1878;1:385–498. [Google Scholar]
- Brodal A. Neurological anatomy in relation to clinical medicine. Oxford University Press; New York: 1981. [Google Scholar]
- Buchanan TW, Tranel D, Adolphs R. Emotional autobiographical memories in amnesic patients with medial temporal lobe damage. Journal of Neuroscience. 2005;25(12):3151–3160. doi: 10.1523/JNEUROSCI.4735-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavaco S, Anderson SW, Allen JS, Castro-Caldas A, Damasio H. The scope of preserved procedural memory in amnesia. Brain. 2004;127(8):1853. doi: 10.1093/brain/awh208. [DOI] [PubMed] [Google Scholar]
- Corsellis JA, Goldberg GJ, Norton AR. “Limbic encephalitis” and its association with carcinoma. Brain. 1968;91(3):481–496. doi: 10.1093/brain/91.3.481. [DOI] [PubMed] [Google Scholar]
- Damasio AR, Eslinger PJ, Damasio H, Van Hoesen GW, Cornell S. Multimodal amnesic syndrome following bilateral temporal and basal forebrain damage. Archives of Neurology. 1985;42(3):252–259. doi: 10.1001/archneur.1985.04060030070012. [DOI] [PubMed] [Google Scholar]
- Damasio AR, Van Hoesen GW. The limbic system and the localisation of herpes simplex encephalitis. Journal of Neurology, Neurosurgery, and Psychiatry. 1985;48(4):297–301. doi: 10.1136/jnnp.48.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damasio H. The lesion method in cognitive neuroscience. Handbook of Neuropsychology. 2000;1:77–102. [Google Scholar]
- Friedman HM, Allen N. Chronic effects of complete limbic lobe destruction in man. Neurology. 1969;19(7):679–690. doi: 10.1212/wnl.19.7.679. [DOI] [PubMed] [Google Scholar]
- Gainotti G. What the locus of brain lesion tells us about the nature of the cognitive defect underlying category-specific disorders: A review. Cortex. 2000;36(4):539–559. doi: 10.1016/s0010-9452(08)70537-9. [DOI] [PubMed] [Google Scholar]
- Gascon GG, Gilles F. Limbic dementia. Journal of Neurology, Neurosurgery, and Psychiatry. 1973;36(3):421–430. doi: 10.1136/jnnp.36.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heimer L, Van Hoesen GW. The limbic lobe and its output channels: Implications for emotional functions and adaptive behavior. Neuroscience and Biobehavioral Reviews. 2006;30(2):126–147. doi: 10.1016/j.neubiorev.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hierons R, Janota I, Corsellis JA. The late effects of necrotizing encephalitis of the temporal lobes and limbic areas: A clinico-pathological study of 10 cases. Psychological Medicine. 1978;8(1):21–42. doi: 10.1017/s0033291700006607. [DOI] [PubMed] [Google Scholar]
- Hjalmarsson A, Blomqvist P, Skoldenberg B. Herpes simplex encephalitis in sweden, 1990–2001: Incidence, morbidity, and mortality. Clin Infect Dis. 2007;45(7):875–880. doi: 10.1086/521262. [DOI] [PubMed] [Google Scholar]
- Kapur N, Barker S, Burrows EH, Ellison D, Brice J, Illis LS, et al. Herpes simplex encephalitis: Long term magnetic resonance imaging and neuropsychological profile. Journal of Neurology, Neurosurgery & Psychiatry. 1994;57(11):1334–1342. doi: 10.1136/jnnp.57.11.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy PG. A retrospective analysis of forty-six cases of herpes simplex encephalitis seen in glasgow between 1962 and 1985. Quarterly Journal of Medicine, New Series. 1988;68(255):533–540. [PubMed] [Google Scholar]
- King DH. History, pharmacokinetics, and pharmacology of acyclovir. Journal of the American Academy of Dermatology. 1988;18(1 Pt 2):176–179. doi: 10.1016/s0190-9622(88)70022-5. [DOI] [PubMed] [Google Scholar]
- Kotter R, Meyer N. The limbic system: A review of its empirical foundation. Behavioural Brain Research. 1992;52(2):105–127. doi: 10.1016/s0166-4328(05)80221-9. [DOI] [PubMed] [Google Scholar]
- Lakeman FD, Whitley RJ. Diagnosis of herpes simplex encephalitis: Application of polymerase chain reaction to cerebrospinal fluid from brain-biopsied patients and correlation with disease. National institute of allergy and infectious diseases collaborative antiviral study group. The Journal of Infectious Diseases. 1995;171(4):857–863. doi: 10.1093/infdis/171.4.857. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. Emotion circuits in the brain. Annual Review of Neuroscience. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- Maclean PD. Some psychiatric implications of physiological studies on frontotemporal portion of limbic system (visceral brain) Electroencephalography and Clinical Neurophysiology. 1952;4(4):407–418. doi: 10.1016/0013-4694(52)90073-4. [DOI] [PubMed] [Google Scholar]
- McCarthy RA, Kopelman MD, Warrington EK. Remembering and forgetting of semantic knowledge in amnesia: a 16 year follow-up investigation of RFR. Neuropsychologia. 2005;43:356–372. doi: 10.1016/j.neuropsychologia.2004.06.024. [DOI] [PubMed] [Google Scholar]
- McCormick LM, Ziebell S, Nopoulos P, Cassell M, Andreasen NC, Brumm M. Anterior cingulate cortex: An MRI-based parcellation method. NeuroImage. 2006;32(3):1167–1175. doi: 10.1016/j.neuroimage.2006.04.227. [DOI] [PubMed] [Google Scholar]
- Mesulam MM, Mufson EJ. Insula of the old world monkey. I. architectonics in the insulo-orbito-temporal component of the paralimbic brain. The Journal of Comparative Neurology. 1982;212(1):1–22. doi: 10.1002/cne.902120102. [DOI] [PubMed] [Google Scholar]
- Mokler DJ, Morgane PJ. Special issue: The limbic brain: Structure and function. Neuroscience & Biobehavioral Reviews. 2006;30(2):119–272. doi: 10.1016/j.neubiorev.2005.04.020. [DOI] [PubMed] [Google Scholar]
- Nicoll JA, Love S, Kinrade E. Distribution of herpes simplex virus DNA in the brains of human long-term survivors of encephalitis. Neuroscience Letters. 1993;157(2):215–218. doi: 10.1016/0304-3940(93)90740-c. [DOI] [PubMed] [Google Scholar]
- O'Connor MG, Cermak LS, Seidman LJ. Social and emotional characteristics of a profoundly amnesic postencephalitic patient. In: Campbell R, Conway M, editors. Broken memories: Case studies in memory impairment. Blackwell Publishers; Oxford: 1995. pp. 45–53. [Google Scholar]
- Papez JW. A proposed mechanism of emotion. Arch Neurol Psychiatry. 1937;38(725):43. [Google Scholar]
- Perkins BA, Bril V. Diagnosis and management of diabetic neuropathy. Current Diabetes Reports. 2002;2(6):495–500. doi: 10.1007/s11892-002-0119-x. [DOI] [PubMed] [Google Scholar]
- Perkins BA, Olaleye D, Zinman B, Bril V. Simple screening tests for peripheral neuropathy in the diabetes clinic. Diabetes Care. 2001;24(2):250–256. doi: 10.2337/diacare.24.2.250. [DOI] [PubMed] [Google Scholar]
- Rantalaiho T, Farkkila M, Vaheri A, Koskiniemi M. Acute encephalitis from 1967 to 1991. Journal of the Neurological Sciences. 2001;184(2):169–177. doi: 10.1016/s0022-510x(01)00441-5. [DOI] [PubMed] [Google Scholar]
- Schmolck H, Kensinger EA, Corkin S, Squire LR. Semantic knowledge in patient HM and other patients with bilateral medial and lateral temporal lobe lesions. Hippocampus. 2002;12:520–533. doi: 10.1002/hipo.10039. [DOI] [PubMed] [Google Scholar]
- Scoville WB. The limbic lobe in man. Journal of Neurosurgery. 1954;11(1):64–66. doi: 10.3171/jns.1954.11.1.0064. [DOI] [PubMed] [Google Scholar]
- Scoville WB, Milner B. Loss of recent memory after bilateral hippocampal lesions. Journal of Neurology, Neurosurgery, and Psychiatry. 1957;20:11–21. doi: 10.1136/jnnp.20.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw CM, Alvord EC., Jr. Neuropathology of the limbic system. Neuroimaging Clinics of North America. 1997;7(1):101–142. [PubMed] [Google Scholar]
- Skoldenberg B, Forsgren M, Alestig K, Bergstrom T, Burman L, Dahlqvist E, et al. Acyclovir versus vidarabine in herpes simplex encephalitis: Randomised multicentre study in consecutive swedish patients. Lancet. 1984;(2):707–711. doi: 10.1016/s0140-6736(84)92623-0. [DOI] [PubMed] [Google Scholar]
- Squire LR. Memory and the hippocampus: A synthesis from findings with rats, monkeys, and humans. Psychological Review. 1992;99(2):195–231. doi: 10.1037/0033-295x.99.2.195. [DOI] [PubMed] [Google Scholar]
- Stefanacci L, Buffalo EA, Schmolck H, Squire LR. Profound amnesia after damage to the medial temporal lobe: A neuroanatomical and neuropsychological profile of patient E.P. Journal of Neuroscience. 2000;20(18):7024–7036. doi: 10.1523/JNEUROSCI.20-18-07024.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate RL. Emotional and social consequences of memory disorders. In: Baddeley AD, Kopelman MD, Wilson BA, editors. The handbook of memory disorders. 2nd ed. John Wiley & Sons Ltd; West Sussex, England: 2002. pp. 785–808. [Google Scholar]
- The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes and the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England Journal of Medicine. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- Tranel D, Damasio H, Damasio AR. Amnesia caused by herpes simplex encephalitis, infarctions in basal forebrain, and anoxia/ischemia. In: Boller F, Grafman J, editors. Handbook of neuropsycholgy. 2nd Edition Vol. 2. Elsevier; 2000. pp. 85–110. [Google Scholar]
- Tranel D, Feinstein JS, Manzel K. Further lesion evidence for the neural basis of conceptual knowledge for persons and other concrete entities. Journal of Neuropsychology. 2008;2:301–320. doi: 10.1348/174866407x227033. [DOI] [PubMed] [Google Scholar]
- Tranel D, Jones R. Knowing what and knowing when. Journal of Clinical and Experimental Neuropsychology. 2006;28(1):43–66. doi: 10.1080/13803390490919344. [DOI] [PubMed] [Google Scholar]
- Tuzun E, Dalmau J. Limbic encephalitis and variants: classification, diagnosis and treatment. The Neurologist. 2007;13(5):261–271. doi: 10.1097/NRL.0b013e31813e34a5. [DOI] [PubMed] [Google Scholar]
- Tyler KL. Update on herpes simplex encephalitis. Reviews in Neurological Diseases. 2004;1(4):169–178. [PubMed] [Google Scholar]
- Verfaellie M, Reiss L, Roth HL. Knowledge of new english vocabulary in amnesia: An examination of premorbidly acquired semantic memory. Journal of the International Neuropsychological Society. 1995;1(5):443–453. doi: 10.1017/s1355617700000540. [DOI] [PubMed] [Google Scholar]
- Vogt BA, Nimchinsky EA, Vogt LJ, Hof PR. Human cingulate cortex: Surface features, flat maps, and cytoarchitecture. The Journal of Comparative Neurology. 1995;359(3):490–506. doi: 10.1002/cne.903590310. [DOI] [PubMed] [Google Scholar]
- Warrington EK, Shallice T. Category specific semantic impairments. Brain. 1984;107:829–854. doi: 10.1093/brain/107.3.829. [DOI] [PubMed] [Google Scholar]
- Whitley RJ, Alford CA, Hirsch MS, Schooley RT, Luby JP, Aoki FY, et al. Vidarabine versus acyclovir therapy in herpes simplex encephalitis. New England Journal of Medicine. 1986;314(3):144–149. doi: 10.1056/NEJM198601163140303. [DOI] [PubMed] [Google Scholar]
- Willis T. Cerebri anatomie. Martzer and Alleftry; London: 1664. [Google Scholar]
- Wilson BA, Baddeley AD, Kapur N. Dense amnesia in a professional musician following herpes simplex virus encephalitis. Journal of Clinical and Experimental Neuropsychology. 1995;17(5):668–681. doi: 10.1080/01688639508405157. [DOI] [PubMed] [Google Scholar]
- Wilson BA, Kopelman M, Kapur N. Prominent and persistent loss of past awareness in amnesia: Delusion, impaired consciousness or coping strategy? Neuropsychological Rehabilitation. 2008;18(5&6):527–540. doi: 10.1080/09602010802141889. [DOI] [PubMed] [Google Scholar]
- Xu Y, Corkin S. HM revisits the tower of hanoi puzzle. Neuropsychology. 2001;15(1):69–79. doi: 10.1037//0894-4105.15.1.69. [DOI] [PubMed] [Google Scholar]
- Yakovlev PI. A proposed definition of the limbic system. In: Hockman CH, editor. Limbic system mechanisms and autonomic function. Thomas; Springfield, IL: 1972. pp. 241–283. [Google Scholar]
- Zola-Morgan S, Squire LR. Neuroanatomy of memory. Annual Reviews in Neuroscience. 1993;16(1):547–563. doi: 10.1146/annurev.ne.16.030193.002555. [DOI] [PubMed] [Google Scholar]