Abstract
Study Design
Observational.
Objective
To provide normative values of lumbar flexion and extension for women of different age and racial groups.
Summary of Background Data
Spinal range of motion (ROM) is one of the AMA Guides criteria used to estimate level of impairment and subsequent compensation entitlement. Studies show that spinal ROM varies with age, gender, and possibly race/ethnicity, but adequate normative values for different age and racial/ethnic groups do not exist.
Methods
A cohort of free-living women was recruited for the Women's Injury Study at The Cooper Institute in Dallas. Originally, 917 women between the ages of 20 and 83 (M = 52 ± 13) underwent an orthopedic examination including lumbar spine flexion and extension measurement using an electronic inclinometer. Measurements were taken in the fully extended and flexed positions, respectively. This removes the influence of initial resting posture and is termed “extreme of motion” (EOM) as opposed to ROM. Age and racial groups were compared using a 2-way multivariate analysis of variance (MANOVA) followed with post hoc tests.
Results
Means (±SD) were calculated for racial (white, N = 619, African-American, N = 147) and age groups (young, 20–39 years, n = 126; middle, 40–59 years, n = 412; older, ≥60 years, n = 228). Lumbar extension for African-American women (60.1°) was significantly greater (P < 0.05) than for white women (52.6°), but flexion was not different (15.2° and 17.0°), respectively. Extension EOM for the young group (61.6°) was greater (P < 0.05) than the middle (56.6°) and older (50.8°) groups. Extension difference between the middle and older groups was significant. Flexion EOM for the young group (20.1°) was greater (P < 0.05) than the middle (15.2°) and older (12.8°) groups. The difference in flexion between the middle and older groups was not significant.
Conclusion
Normative values of lumbar extension are different for white and African-American women. Values for lumbar flexion and extension are different between age groups. Different criteria should be used to estimate impairment level in women of different racial and age groups.
Keywords: normative values, electronic inclinometer, range of motion, African-American
The measurement of lumbar spine range of motion (ROM) is important clinically for physicians and rehabilitation specialists who treat low back pain. Current clinical measurement techniques include the use of inclinometers, goniometers, and tape measures with each of the techniques having its own set of limitations. For information obtained from any of these measurement techniques to be useful, normative data for lumbar spine ROM using the specific measurement technique are needed. However, adequate documentation of normative data for the lumbar spine is lacking in the literature.
Most existing databases of normative data for lumbar spine ROM provide values obtained with measurement tools that are neither practical nor feasible for clinical use.1–4 The AMA Guides to the Evaluation of Permanent Impairment (AMA Guides) use spinal ROM measurements to estimate the level of impairment and subsequent compensation entitlement.5 The Guides specifically recommend the use of an inclinometer as the preferred device for measuring lumbar spine motion. However, normative values used by the Guides were not determined using an inclinometer3,6 and are based on a small sample size of 21 men and 20 women3 or a sample of mostly men (168 men and 4 women).6
Several investigators have demonstrated that mean values for lumbar spine ROM differ for gender2,3,7 and age.2–4,7 Despite this information, the baselines (the bottom of the impairment scale that reflects zero impairment) used to determine disability ratings do not take gender and age into account. Spieler et al,8 in a summary of criticisms of the fourth edition of the AMA Guides, argue that normative values used for baselines should include “known population variants” such as age, sex, and race.
In addition to the lack of established normative data, there have been measurement issues associated with documentation of lumbar spine mobility. The term “range of motion” implies that 2 numbers are needed to define a motion, with the first number indicating where the motion begins and the second number indicating where the motion ends. This is consistent with the neutral zero method of notation9 that is widely used throughout the world and is supported by the American Academy of Orthopedic Surgeons and the American Medical Association.5,10,11 Lumbar ROM is most often recorded as a single number that represents the end point. It is implied that the start position is zero but several researchers have identified this practice as being problematic.7,12 The double inclinometer measurement of lumbar flexion and extension advocated by the AMA Guides uses initial resting posture as the zero reference from which flexion and extension are measured.7 Initial resting posture varies among individuals with a mean value of 31.7° of lordosis for women and 24.3° for men when using the γ-tangent method originally described by Loebl.13 Other sources have reported similar values of resting lordotic posture and similar differences between men and women.14 The problem with the practice of using initial resting posture as the zero reference is that as a person flexes forward, the lordosis must first be reversed. Because this reversal of lordosis is added to the lumbar ROM measurement when using the double inclinometer technique, excessive lordosis will artificially inflate the flexion ROM value.12 For lumbar extension measurements, an excessive amount of lordosis artificially deflates the extension ROM measurement since the underlying vertebrae are already in a position of extension.15,16 Sullivan et al7 argue that the true measure of lumbar ROM in the sagittal plane should not be dependent on the amount of lumbar lordosis present.
The purpose of this study was to provide normative values of lumbar flexion and extension for a fairly large sample of women of different age and racial groups using inclinometric measurements that do not use lordosis as a zero reference point. Additionally, lumbar flexion and extension values were compared across age and racial groups and reliability for our inclinometer measurements was assessed.
Materials and Methods
Participants
Participants were a cohort of free-living women who were recruited for the Women's Injury Study (WIN) at The Cooper Institute in Dallas, TX. WIN is an ongoing (3-year) web-based surveillance study of physical activity habits and musculoskeletal injuries in women. To qualify for WIN, women had to be at least 20 years of age and have access to a computer with Internet capabilities. Women were excluded if they had a disease or condition that limited their mobility without the use of assistive devices or if the condition limited or interfered with their usual daily or recreational activities. Qualified women who voluntarily agreed to participate in WIN signed an informed consent in accordance with the Institute's review board and underwent a baseline orthopedic examination by a licensed physical therapist. This study presents data obtained from the baseline orthopedic examination.
Participants provided demographic information and a medical history during an orientation session for WIN. Nine hundred seventeen women between the ages of 20 and 83 (52 ± 13) underwent an orthopedic examination and completed an online symptom and injury history questionnaire at the time of the examination.
Measurement Procedures
Participants were asked to wear a sports bra, shorts, and no shoes so that all testing landmarks would be visible. Before the examination, the T12 and S1 vertebrae were marked with a pen. Height was measured using a stadiometer and weight was measured using a digital scale. Height and weight were used to calculate body mass index.
Additional clinical measurements were taken as part of the WIN orthopedic examination but only the procedures related to the measurement of lumbar spine extremes of motion are presented here. We use the term “extremes of motion” rather than “range of motion” to more accurately reflect our measurement procedures. To remove the influence of initial resting posture, lumbar spine flexion angle was determined by placing the inclinometer on the participant's fully flexed spine. This measurement is called flexion extreme of motion (EOM). For lumbar spine extension angle, the inclinometer was placed on the participant's fully extended spine and this measurement is called extension EOM. The use of EOM as opposed to ROM to quantify human motion has been advocated by Kondraske.17
EOM was assessed using the Human Performance Measurement (HPM) system (Human Performance Measurement, Inc., Arlington, TX). The HPM system is a computer-automated system used to assess a variety of sensorimotor functions or basic elements of performance (BEP). The BEP VIIa is the electronic inclinometer component of the HPM system used in this study to measure lumbar flexion and extension EOM (Figures 1, 2). The software, BEP for Windows (Human Performance Measurement, Inc., Arlington, TX), was used to run the BEP modules and record and collect data using a notebook computer.
Figure 1.
BEP-VIIa electronic inclinometer.
Figure 2.
Lumbar flexion measurement using the BEP-VIIa electronic inclinometer.
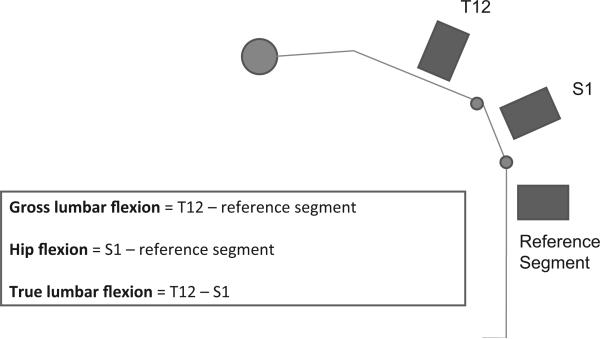
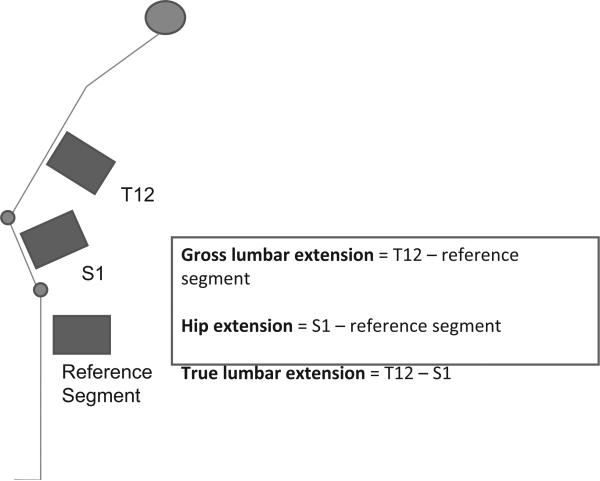
For measurement of lumbar flexion EOM, participants were asked to stand with their arms at their side and feet 8 cm apart. The tester first demonstrated the flexion motion to the participant and instructed her to bend forward as far as possible, keeping the knees straight, and to hold this position until told to return to the initial upright standing position. Participants were given 1 practice trial before performing the examination. The tester established a reference point for the lumbar flexion EOM measurement by aligning the electronic inclinometer along the participant's lateral thigh. Using the thigh as the reference allowed determination of the hip flexion contribution to the overall lumbar flexion EOM. Once the participant was in the fully flexed position, the tester clicked the inclinometer once along the lateral thigh, the S1 vertebrae, and the T12 vertebrae to complete measurement of lumbar flexion EOM. The flexion EOM measurement was performed 3 times and the mean of the 2 closest measurements was calculated. Lumbar extension EOM was measured in the same manner except the tester instructed the participant to lean back as far as possible, keeping the knees straight, and to hold this position until told to return to the upright position. Three different measurements for each EOM were recorded. Lumbar flexion EOM measurements included (1) total lumbar flexion, (2) hip flexion, and (3) true lumbar flexion. Lumbar extension EOM measurements included (1) total lumbar extension, (2) hip extension, and (3) true lumbar extension. See Figures 3 and 4 for the equations used to determine the EOM measurements.
Figure 3.
Demonstrates the placement of the inclinometer during lumbar flexion extreme of motion measurements and the equations used to calculate true lumbar, hip, and gross lumbar flexion.
Figure 4.
Demonstrates the placement of the inclinometer during lumbar extension extreme of motion measurements and the equations used to calculate true lumbar, hip, and gross lumbar extension.
To determine the reliability of the BEP-VII electronic inclinometer and our test procedures, 2 testers were used. Tester 1 was an experienced rehabilitation specialist with several years of experience in using the BEP-VII electronic inclinometer to measure lumbar flexion and extension EOM. Tester 2 was a novice who received training on use of the electronic inclinometer and the standardized test procedures solely for the purposes of assessing reliability of our test instrument and procedures. The novice received approximately 4 hours of training and practiced on 10 volunteers before the reliability testing. Each rater independently located and marked bony landmarks using removable adhesive stickers and tested 40 women between the ages of 21 and 75 (mean = 35.9 years ± 16.4) using the standardized testing procedures described above. Tester 1 measured each participant twice to determine intrarater reliability while tester 2 measured each participant once and these measurements were compared with those of tester 1 to determine interrater reliability. The average of 2 measures was used to compare measures between tests (intrarater) and between testers (interrater). All measurements were conducted on the same day with several minutes rest between each test.
Data Analysis
Descriptive statistics that included frequencies, means, and standard deviations were used to describe the demographic characteristics and lumbar EOM values of the participants. Independent t tests were performed to determine if differences in lumbar EOM between participants with or without current low back pain or injury were significant and should therefore be excluded for the purposes of determining normative lumbar spine values. A 3 × 2 MANOVA was conducted to compare differences in lumbar flexion EOM measurements (total lumbar flexion, hip flexion, true lumbar flexion) between age and racial groups. A second 3 × 2 MANOVA compared differences in lumbar extension measurements (total lumbar extension, hip extension, and true lumbar extension) between age and racial groups. Univariate ANOVAs were performed when the MANOVA was significant. Pairwise comparisons were conducted when main effects of age were found to be significant to determine where the differences were. A repeated measures ANOVA was used to calculate an ICC3,2 and ICC2,2 to determine intrarater and interrater reliability, respectively, for the lumbar EOM measurements. The alpha level was 0.05 for all statistical tests.
Results
Ten of the 917 participants had missing data so they were excluded from data analysis. Independent t tests showed significant differences in true lumbar flexion (P < 0.01) and true lumbar extension (P < 0.01) EOM between participants with and without current low back pain or injury. Therefore, participants who reported current low back pain or injury (n = 100) were excluded from data analysis leaving a total of 807 participants whose data were included in the normative data analysis. Normative data were only determined for the white (N = 619) and African-American (N = 147) groups due to the small sample sizes of the other ethnic groups combined (N = 41). A summary of demographic data for the remaining participants (N = 766) is presented in Table 1.
Table 1.
Demographic Data*
| Age Groups | Weight (kg) | Height (cm) | BMI (kg/m2) |
|---|---|---|---|
| White | |||
| 20–39 (n = 87) | 68.7 ± 14.5 | 165.2 ± 5.6 | 25.3 ± 5.7 |
| 40–59 (n = 330) | 72.8 ± 16.6 | 164.5 ± 6.4 | 26.9 ± 5.9 |
| 60+ (n = 202) | 70.8 ± 14.8 | 162.3 ± 5.8 | 26.9 ± 5.3 |
| African-American | |||
| 20–39 (n = 39) | 80.1 ± 18.2 | 164.3 ± 6.8 | 29.6 ± 6.1 |
| 40–59 (n = 82) | 83.1 ± 18.0 | 162.1 ± 6.4 | 31.6 ± 6.4 |
| 60+ (n = 26) | 84.8 ± 17.3 | 162.3 ± 5.1 | 31.7 ± 5.7 |
Values are means ± standard deviations.
Intrarater reliability for measures of true lumbar flexion and extension were found to be excellent (ICC3,2 = 0.97 and 0.94), respectively. A calculated ICC2,2 value of 0.90 also revealed excellent interrater reliability for measurements of true lumbar flexion. Interrater reliability for measures of true lumbar extension was less (ICC2,2 = 0.78) but still considered acceptable.
The lumbar EOM data were grouped into 20-year age intervals, and the mean and standard deviation (SD) were calculated for each of the 2 racial groups. The EOM measurements are summarized in Table 2. A 3 × 2 MANOVA of lumbar flexion dependent variables (gross lumbar flexion, hip flexion, true lumbar flexion) revealed that there was no significant age by race interaction (P = 0.37) and no main effects for race (P = 0.97). The main effects for age, however, were significant. Subsequent ANOVAs revealed that gross lumbar flexion (P < 0.01) and true lumbar flexion (P < 0.01) had significant main effects for age. Pairwise comparisons were performed to determine where the differences were between age groups for measures of gross lumbar and true lumbar flexion. The analysis showed significantly greater gross lumbar (P < 0.01) and true lumbar (P < 0.01) flexion in the 20 to 39 age group compared with the 40 to 59 and 60+ age groups (Table 3).
Table 2.
Lumbar Flexion and Extension Extreme of Motion*
| True Lumbar Flexion |
Hip Flexion |
Gross Lumbar Flexion |
||||
|---|---|---|---|---|---|---|
| Age Groups | White | African-American | White | African-American | White | African-American |
| 20–39 (n = 87)† (n = 39)‡ | 21.4 ± 10.4 | 19.1 ± 11.6 | 94.2 ± 14.5 | 95.7 ± 15.0 | 115.6 ± 14.9 | 114.8 ± 12.2 |
| 40–59 (n = 330)† (n = 82)‡ | 17.0 ± 9.6 | 13.6 ± 11.2 | 93.6 ± 16.9 | 90.9 ± 14.5 | 110.6 ± 19.4 | 104.5 ± 16.6 |
| 60+ (n = 202)† (n = 26)‡ | 12.9 ± 10.7 | 12.9 ± 9.0 | 89.6 ± 17.4 | 94.5 ± 11.9 | 102.4 ± 19.9 | 107.4 ± 11.8 |
| True Lumbar Extension | Hip Extension | Gross Lumbar Extension | ||||
|---|---|---|---|---|---|---|
| 20–39 (n = 87)† (n = 39)‡ | 56.7 ± 10.1 | 66.2 ± 16.3 | –10.0 ± 10.7 | –19.6 ± 10.2 | 46.7 ± 12.2 | 46.6 ± 12.4 |
| 40–59 (n = 330)† (n = 82)‡ | 53.6 ± 10.9 | 59.4 ± 13.3 | –9.4 ± 10.3 | –16.6 ± 11.4 | 44.2 ± 11.6 | 42.8 ± 12.1 |
| 60+ (n = 202)† (n = 26)‡ | 47.2 ± 12.3 | 54.5 ± 13.2 | –5.5 ± 10.1 | –18.6 ± 10.6 | 41.6 ± 13.2 | 35.8 ± 11.6 |
The negative hip extension values occur because when the lumbar spine was fully extended, the sacrum was in a flexed position. The resulting angle formed by the sacrum and vertical reference is then in an opposite direction than the measured extension movement and thus appears as a negative value.
Values are means ± standard deviations.
White women.
African American women.
Table 3.
Multivariate Analysis of Variance for Lumbar Flexion Extreme of Motion Variables
| Age Groups |
Statistics |
Multiple Comparisons |
||||||
|---|---|---|---|---|---|---|---|---|
| Lumbar Flexion EOM | 20–39 yr (Group 1) | 40–59 yr (Group 2) | 60+ yr (Group 3) | F | P | 1/2 | 1/3 | 2/3 |
| Gross flexion | 115.00 | 107.69 | 104.83 | 8.92 | <0.01 | * | * | |
| Hip flexion | 94.87 | 92.43 | 92.00 | 1.04 | 0.35 | |||
| True flexion | 20.13 | 15.25 | 12.83 | 14.58 | <0.01 | * | * | |
Indicates a significant difference between the means of the indicated pair of age groups.
A separate 3 × 2 MANOVA analysis of lumbar extension dependent variables (gross lumbar extension, hip extension, true lumbar extension) revealed that there was no significant age by race interaction (P = 0.25) but significant main effects of age (P < 0.01) and race (P < 0.01). ANOVAs revealed significant main effects of age for gross (P < 0.01) and true (P < 0.01) lumbar extension as well as significant main effects of race for gross lumbar (P = 0.05), hip (P < 0.01), and true lumbar (P < 0.01) extension (Tables 4, 5). Main effects of age were further explored by performing pairwise comparisons to determine differences between the age groups for measures of gross lumbar and true lumbar extension. Significant differences in gross lumbar extension were found between the middle (40–59) and older (60+) age groups and between the young (20–39) and older (60+) age groups (P < 0.01). For measures of true lumbar extension, significant differences were found between the young and the middle and older groups (P < 0.01) as well as between the middle and older groups (P < 0.01) (Table 5).
Table 4.
Multivariate Analysis of Variance for Lumbar Extension Extreme of Motion Variables
| Race |
Statistics |
|||
|---|---|---|---|---|
| Lumbar Extension EOM | White | African-American | F | P |
| Gross extension | 44.14 | 41.71 | 3.73 | 0.05* |
| Hip extension | –8.42 | –18.39 | 85.26 | <0.01* |
| True extension | 52.56 | 60.09 | 37.62 | <0.01* |
Indicates a significant difference between the means of the race groups.
Table 5.
Multivariate Analysis of Variance for Lumbar Extension Extreme of Motion Variables
| Age Groups |
Statistics |
Multiple Comparisons |
||||||
|---|---|---|---|---|---|---|---|---|
| Lumbar Extension EOM | 20-39 yr (Group 1) | 40–59 yr (Group 2) | 60+ yr (Group 3) | F | P | 1/2 | 1/3 | 2/3 |
| Gross extension | 46.69 | 43.44 | 38.64 | 10.93 | <0.01 | * | * | |
| Hip extension | –14.87 | –13.21 | –12.13 | 1.79 | 0.17 | |||
| True extension | 61.56 | 56.64 | 50.77 | 20.48 | <0.01 | * | * | * |
Indicates a significant difference between the means of the indicated pair of age groups.
Discussion
Although many studies have determined the effect of age and gender on lumbar motion,1–4,6,7 our study was the first to examine the effect of age and race on lumbar EOM measurements. We found that true lumbar flexion and extension EOM decreased as age increased in white and African-American women. Decreases between age groups in true lumbar flexion ranged from 2.4° to 7.3° while decreases in true lumbar extension ranged from 4.9° to 10.8°. The 2.4° decrease was between the middle and older age groups and was the only difference that was not statistically significant. All other decreases in true lumbar flexion and extension between age groups were statistically significant. These results support previous studies that also found reductions in lumbar spine mobility with increasing age.1–4,6,7 Our study also found that true lumbar extension EOM was an average of 7.5° greater in African-American women than in white women, but that true lumbar flexion was essentially the same with less than 2° difference between African-American and white women. There is no way to know why these differences in lumbar extension between racial groups occurred. Genetic influences as well as environmental and behavioral factors have been proposed as determinants of differences in spinal ROM between individuals but this has not been investigated in different racial groups. Interestingly, in a study of differences in lumbar ROM in adult male twin pairs, Battie et al found that lumbar flexion ROM variance was primarily determined by genetic influences (64% of variance), while lumbar extension was influenced to a greater extent by environmental and behavioral factors.18
It should be noted that our study used a measurement technique that was similar to Sullivan et al7 but different from most other studies of lumbar ROM. We measured the lumbar spine at the end of its available motion, thereby termed EOM rather than ROM. We also used a neutral reference segment parallel to the thigh rather than the initial resting lumbar posture. Use of the initial resting lumbar posture has been previously criticized for artificially inflating or deflating the measured lumbar motion depending on the amount of lumbar lordosis present at rest.12,15,16 The measurement technique that we used accounts for the differences in mean lumbar flexion and extension values when compared with values obtained using initial resting lumbar posture as the zero reference.1–4,6 Our lumbar EOM measurements are similar to those reported by Sullivan et al7 who measured lumbar flexion and extension using a technique similar to ours that did not use resting lumbar posture as the zero reference. However, Sullivan et al took measurements in the seated position for flexion and in the prone position for extension rather than the standing position that we used.
Using the thigh as a neutral reference also allowed us to determine how much hip motion contributed to the overall lumbar motions of flexion and extension. For example, when one bends forward from the standing position, the motion that is measured as gross lumbar flexion is a combination of motion that occurs at the hip (acetabulo-femoral joint) and motion that actually occurs in the lumbar spine (true lumbar flexion from T12/L1–L5/S1). The same is true in the opposite direction of extension (Figures 3 and 4). Because our statistical analyses did not show a significant age by race interaction for flexion or extension, we did not statistically compare the measured dependent variables for white women to African-American women in specific age groups (simple effects). However, we did observe some interesting differences between the 2 races. Lumbar motion in African-American and white women both decreased with age, but African-American women had less true lumbar flexion (0°–3.4°) and more true lumbar extension (6.1°–9.3°) across age groups than white women.
Conclusion
This study has created a database of normative values for lumbar EOM measurements for women of different race and age groups using inclinometric measurements that do not use lordosis as a zero reference point. As was shown in other studies, lumbar EOM declines as age increases. However, it was also demonstrated that African-American women have greater lumbar extension compared with white women. Further study on the relationship of this difference between races and low back pain is needed.
Key Points.
Normative values of lumbar extension are greater for African-American women than for white women.
Lumbar flexion and extension motion decrease significantly with age in white and African-American women.
Different criteria should be used when determining lumbar spine mobility impairment for different racial and age groups.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Award R01 AR052459.
References
- 1.Troke M, Moore AP, Maillardet FJ, et al. A new, comprehensive normative database of lumbar spine ranges of motion. Clin Rehabil. 2001;15:371–9. doi: 10.1191/026921501678310171. [DOI] [PubMed] [Google Scholar]
- 2.Van Herp G, Rowe P, Salter P, et al. Three-dimensional lumbar spinal kinematics: a study of range of movement in 100 healthy subjects aged 20 to 60+ years. Rheumatology (Oxford) 2000;39:1337–40. doi: 10.1093/rheumatology/39.12.1337. [DOI] [PubMed] [Google Scholar]
- 3.McGregor AH, McCarthy ID, Hughes SP. Motion characteristics of the lumbar spine in the normal population. Spine. 1995;20:2421–8. doi: 10.1097/00007632-199511001-00009. [DOI] [PubMed] [Google Scholar]
- 4.Dvorak J, Vajda EG, Grob D, et al. Normal motion of the lumbar spine as related to age and gender. Eur Spine J. 1995;4:18–23. doi: 10.1007/BF00298413. [DOI] [PubMed] [Google Scholar]
- 5.American Medical Association . Guides to the Evaluation of Permanent Impairment. 5th ed. American Medical Association; Chicago, IL: 2001. [Google Scholar]
- 6.Fitzgerald GK, Wynveen KJ, Rheault W, et al. Objective assessment with establishment of normal values for lumbar spinal range of motion. Phys Ther. 1983;63:1776–81. doi: 10.1093/ptj/63.11.1776. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan MS, Dickinson CE, Troup JD. The influence of age and gender on lumbar spine sagittal plane range of motion: a study of 1126 healthy subjects. Spine. 1994;19:682–6. doi: 10.1097/00007632-199403001-00007. [DOI] [PubMed] [Google Scholar]
- 8.Spieler EA, Barth PS, Burton JF, Jr, et al. Recommendations to guide revision of the guides to the evaluation of permanent impairment. American medical association. JAMA. 2000;283:519–23. doi: 10.1001/jama.283.4.519. [DOI] [PubMed] [Google Scholar]
- 9.Silver D. Measurement of the range of motion of joints. J Bone Joint Surg. 1923;21 [Google Scholar]
- 10.American Academy of Orthopaedic Surgeons . Joint Motion: Methods of Measuring and Recording. AAOS; Chicago, IL: 1965. [Google Scholar]
- 11.Greene WB, Heckman JD, editors. The Clinical Measurement of Joint Motion. American Academy of Orthopaedic Surgeons; Rosemont, IL: 1994. [Google Scholar]
- 12.Coates JE, McGregor AH, Beith ID, et al. The influence of initial resting posture on range of motion of the lumbar spine. Man Ther. 2001;6:139–44. doi: 10.1054/math.2001.0397. [DOI] [PubMed] [Google Scholar]
- 13.Norton FJ, Sahrmann SA, Van Dillen LR. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthop Sports Phys Ther. 2004;34:524–34. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- 14.Bergenudd H, Nilsson B, Uden A, et al. Bone mineral content, gender, body posture, and build in relation to back pain in middle age. Spine. 1989;14:577–9. doi: 10.1097/00007632-198906000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Loebl WY. Measurement of spinal posture and range of spinal movement. Ann Phys Med. 1967;9:103–10. doi: 10.1093/rheumatology/9.3.103. [DOI] [PubMed] [Google Scholar]
- 16.Twomey LT, Taylor JR. Sagittal movements of the human lumbar vertebral column: a quantitative study of the role of the posterior vertebral elements. Arch Phys Med Rehabil. 1983;64:322–5. [PubMed] [Google Scholar]
- 17.Kondraske GV. An elemental resource for the human-task interface. Int J Technol Assess Health Care. 1995;11:153–73. doi: 10.1017/s0266462300006802. [DOI] [PubMed] [Google Scholar]
- 18.Battie MC, Levalahti E, Videman T, et al. Heritability of lumbar flexibility and the role of disc degeneration and body weight. J Appl Physiol. 2008;104:379–85. doi: 10.1152/japplphysiol.01009.2007. [DOI] [PubMed] [Google Scholar]