Establishing entrance and exit block from pulmonary veins is an endpoint for pulmonary vein isolation (PVI) procedures (1). Reestablished pulmonary vein connection is a common cause of atrial fibrillation (AF) recurrence in patients who have previously undergone PVI. Here we provide images from a noninvasive cardiac electrophysiology imaging system (ECGI) performed during PVI.
The ECGI procedure has been described previously (2) (3). 250 carbon electrodes were applied to the patient’s torso before a pre-procedural contrast-enhanced CT scan, which provided torso-electrode positions and atrial geometry in the same reference frame. The electrodes were removed, then replaced on the day of the PVI procedure in the same configuration, and remained on the patient throughout the procedure. ECGI performed during the procedure noninvasively generated epicardial isochrone activation maps.
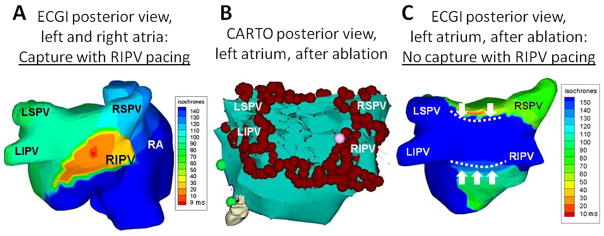
After circumferential ablation around the antrum of the right pulmonary veins, a lasso catheter in the right inferior pulmonary vein (RIPV) demonstrated entrance block. However, high-output pacing from within the RIPV captured the atrium, revealing incomplete exit block.
Panel A displays the real-time ECGI isochrone map during RIPV pacing, showing earliest activation in the superior-posterior antrum of the RIPV (red is earliest), with radial spread across the posterior LA. A 60-ms delay is seen from the pacing breakthrough (red) to posterior LA (green) activation, consistent with incomplete line of block created by the ablation.
The invasive electroanatomic map (Panel B) shows the final ablation lesion set and the additional ablation necessary for exit block from the RIPV (pink marker). This location on the invasive electroanatomic map corresponds closely to the exit site determined by ECGI in Panel A.
Panel C shows an ECGI isochrone map during high-output pacing from within the RIPV after the complete ablation. Pacing failed to capture the atrium, and the earliest LA activation in sinus rhythm was near Bachmann’s bundle (red). Posterior LA activation is limited superiorly and inferiorly with lines of block (white dotted lines) corresponding to the ablation lines on the LA roof and posterior wall seen in panel B. Three PV’s also demonstrate electrical isolation (blue). Although the RSPV in Panel C appears to have electrical connection in sinus rhythm, the appearance of activation is due to far-field signal from the posterior right atrium in close proximity. Invasive testing of the RSPV demonstrated entrance and exit block.
Rigorous prospective study is needed, but if real-time ECGI can accurately identify areas of incomplete PVI isolation, it may shorten procedure time and improve long-term success rates by pinpointing sites of incomplete linear ablation.
Figure 1.
Footnotes
Disclosures
Dr Rudy chairs the scientific advisory board of and holds equity in CardioInsight Technologies. CardioInsight Technologies does not support any research conducted by Dr Rudy, including that presented here.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Phillip S. Cuculich, Assistant Professor of Medicine, Division of Electrophysiology, Washington University School of Medicine, St. Louis, Missouri, 660 South Euclid Ave, Campus Box 8086, St. Louis, MO 63110, Phone: 314-454-7698 Fax: 314-454-8250 pcuculic@wustl.edu.
Yong Wang, Cardiac Bioelectricity Center, 260 Whitaker Hall, Campus Box 1097, One Brookings Dr. Saint Louis, Missouri, 63130-4899, Phone: (314) 935-8163 Fax: (314) 935-8168 wangyong@wustl.edu.
Bruce D. Lindsay, Section Head, Cardiac Electrophysiology and Pacing, Cardiovascular Medicine, Cleveland Clinic, Cleveland, Ohio, Phone: (216) 444-4293 Cleveland Clinic Main Campus, Mail Code F15, 9500 Euclid Avenue, Cleveland, OH 44195.
Ramya Vijayakumar, Cardiac Bioelectricity Center, 260 Whitaker Hall, Campus Box 1097, One Brookings Dr. Saint Louis, Missouri, 63130-4899, Phone: (314) 935-8163 Fax: (314) 935-8168 vramya@seas.wustl.edu.
Yoram Rudy, Cardiac Bioelectricity Center, 290 Whitaker Hall, Campus Box 1097, One Brookings Dr. Saint Louis, Missouri, 63130-4899, Phone: (314) 935-8160 Fax: (314) 935-8168 rudy@wustl.edu.
References
- 1.Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. Heart Rhythm. 2007;4:816–61. doi: 10.1016/j.hrthm.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Ramanathan C, Ghanem RN, Jia P, Ryu K, Rudy Y. Noninvasive electrocardiographic imaging for cardiac electrophysiology and arrhythmia. Nat Med. 2004;10:422–8. doi: 10.1038/nm1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramanathan C, Jia P, Ghanem R, Ryu K, Rudy Y. Activation and repolarization of the normal human heart under complete physiological conditions. Proc Natl Acad Sci U S A. 2006;103:6309–14.3. doi: 10.1073/pnas.0601533103. [DOI] [PMC free article] [PubMed] [Google Scholar]