Abstract
Objectives
Depression is known to be a major problem in cancer patients, and evidence is emerging about the importance of anxiety. Because the disorders are highly comorbid, we examined the relationship of anxiety and depression with health-related quality of life (HRQL) in cancer patients.
Methods
Sample included 405 adult oncology patients participating in a randomized controlled trial of telecare management for pain and depression. This secondary cross-sectional analysis of baseline data examined independent and additive effects of anxiety and depression on HRQL, disability, and somatic symptom severity.
Results
In 397 patients who screened positive for either pain or depression or both, 135 had comorbid anxiety and depression, 174 had depression but not anxiety, and 88 had neither. Differences existed across all non-physical HRQL domains and were more pronounced incrementally across the 3 groups in the expected direction. In GLM modeling, anxiety and depression were each associated with all domains when modeled separately (p < 0.0001). When modeled together, anxiety and depression had independent and additive effects on the mental health domains of HRQL and on somatic symptom burden. In other domains (vitality, perceived disability, overall quality of life, and general health perceptions), only depression had an effect.
Conclusion
Anxiety and depression have strong and independent associations with mental health domains and somatic symptom burden in cancer patients. However, depression has a more pervasive association with multiple other domains of HRQL. Paying attention to both anxiety and depression may be particularly important when addressing mental health needs and somatic symptom distress.
Keywords: Cancer, oncology, anxiety, depression, symptoms, health-related quality of life
Anxiety and depression are troubling and disabling symptoms in patients with cancer. Significant psychological distress is common across all stages of this life-threatening disease, with anxiety and depression representing its most typical manifestation (1). Anxiety disorders are the most common mental health problem in the U.S. with a 1-year general population prevalence rate of 16.4% (2). It is found in 10% to 30% of people with cancer. The most commonly diagnosed anxiety disorders in cancer patients are generalized anxiety disorder (GAD), specific phobias, panic disorder with or without agoraphobia, adjustment disorder with anxious mood, and posttraumatic stress disorder (3, 4). Depression occurs in about 10% to 25% of cancer patients, a rate estimated to be at least four times greater than in the general population (5, 6) but similar to rates of depressive states in patients similarly ill with other medical diagnoses (7). These important psychological symptoms have historically been under-diagnosed and undertreated in cancer care but are gaining more attention recently as researchers seek ways to improve quality of life during treatment and survivorship.
Of these two symptoms, depression has received the most attention from cancer researchers and its adverse effects on functional status and quality of life are well established. The importance of diagnosing and treating depression has been recognized not only to enhance quality of life but because it may adversely affect compliance with treatment, length of time in the hospital, and ability for self-care (8). Although less is known about anxiety, some suggest that its disabling effects may be as troubling as that of depression (3). With prevalence equal to or exceeding that of depression and a potential for adversely affecting functional status, anxiety is an important symptom to target in cancer research.
Anxiety and depression are highly comorbid, both in cancer and non-cancer samples, and distinguishability of the two disorders has long been the subject of investigation with mixed and inconclusive results (9). Various conceptualizations of the relationship between the two symptoms have been advanced over time. Anxiety and depression have recently been viewed by various researchers as being related in one of several ways—as different points on the same continuum, as alternative manifestations of a common underlying diathesis, as heterogeneous syndromes that are associated because of shared subtypes, as separate phenomena that may develop into the other over time, or as distinct phenomena. The current diagnostic system supports the last view listed—a categorical conceptualization; however, dimensional views have gained momentum on the strength of recent evidence. Although some investigators have gone so far as to question whether anxiety and depression are actually distinct phenomena, a comprehensive review of the literature led researchers to conclude that despite significant overlap, the two constructs are indeed distinguishable (2, 9, 10). Greater clarity about the nature of anxiety and depression in cancer patients would enhance our ability to recognize and treat it effectively.
We were interested in examining the relationship of anxiety and depression with health-related quality of life (HRQL) in cancer patients. Of particular interest was the degree to which anxiety may be associated with HRQL independent of depression—and vice versa. We hypothesized that depression severity has a clear association with multiple domains of HRQL (H1) and that anxiety severity examined separately also has a similarly clear association (H2). We further expected to find that depression severity and anxiety severity have moderate independent associations with multiple domains of HRQL (H3); and that these independent associations are only mildly attenuated by adjusting for covariates (H4). We also conducted exploratory analyses of the associations of anxiety and depression on several domains of functional status.
Methods
Study Design and Sample
Baseline data from the Indiana Cancer Pain and Depression (INCPAD) study was analyzed. INCPAD is a randomized controlled trial that tested telecare management delivered by a nurse-psychiatrist team in a statewide network of urban and rural community-based cancer clinics. The intervention was based upon the Three-Component Model—a collaboration between the oncology practice, a centralized nurse care manager, and a supervising pain-psychiatrist (11, 12). A telemedicine approach was utilized with automated home-based symptom monitoring of pain and depressive symptomatology coupled with telephonic nurse care management over 12 months. Recruitment began in February 2006 and ended in August 2008. The study was approved by the Institutional Review Boards of Indiana University and Community Hospitals of Indianapolis. The study has been described in more detail elsewhere (13).
The INCPAD sample consisted of 405 adult oncology patients who screened positive for pain (24%) or depression (32%) or both (44%). Participants were recruited from 15 oncology clinics affiliated with the Community Cancer Care (CCC) network. Clinic staff members asked patients to complete a 4-item depression and pain questionnaire, which is a combination of 2-item screeners which are both well-validated for assessing depression and pain severity. The PHQ-2 depression scale (14) was drawn from the 9-item Patient Health Questionnaire (PHQ-9) and the pain screener is the SF-36 bodily pain scale (15). Patients who screened positive for pain, depression, or both and expressed willingness were contacted by telephone for an eligibility interview. Informed consent was audiotaped, with follow-up by mail.
To be eligible for the INCPAD study, cancer patients had to meet criteria for either pain or clinical depression. Depression had to be of at least moderate severity, which is defined as a PHQ-9 score of 10 or greater with endorsement of depressed mood and/or anhedonia. In past research, over 90% of patients meeting these criteria had major depression and/or dysthymia, and the depression of the remaining patients was clinically significant with substantial functional impairment(16, 17). Participants were eligible to be enrolled for their pain if it was cancer-related, of at least moderate severity—defined by a score of 5 or greater on the Brief Pain Inventory (18)—and persistent after use of at least 2 different analgesics.
Study Outcomes and Measures
The current secondary cross-sectional analysis of baseline data examined the independent and additive effects of anxiety and depression on cancer patients' HRQL, disability, and related outcomes. Independent variables were anxiety severity and depression severity. The primary dependent variables were multiple domains of HRQL; secondary dependent variables included disability and somatic symptom severity.
Independent Variables
Anxiety was measured by the 7-item Patient Health Questionnaire Generalized Anxiety Disorder Scale (GAD-7), which has been shown to have excellent internal consistency (Cronbach's alpha of 0.92) and test-retest reliability (ICC = 0.83) in a sample of 965 patients from 15 primary care sites. Criterion, construct, factorial, and procedural validity are also established (19). Though initially developed for generalized anxiety disorder, the GAD-7 also has good operating characteristics as a screener for panic, social anxiety, and posttraumatic stress disorder (20). Responses are chosen from a 4-point Likert-type scale including “not at all,” “several days,” “more than half the days,” and “nearly every day.” The scale is scored by summing the points across all items, with scores ranging from 0 to 27. Cut-points of 5, 10, and 15 represent mild, moderate, and severe levels of anxiety. A score of 10 has been empirically established as a reasonable cut-point for identifying an anxiety case (19) and was used in the current analysis.
Depression severity was measured with the Depression Subscale (SCL-20) of the Hopkins Symptom Checklist (SCL-90). The SCL-20 is a well-validated modified subscale of the SCL-90 that was chosen for its demonstrated sensitivity in detecting differences in depression severity between treatment groups in previous trials (16). The 20 items ask respondents to rate how much distress was experienced over the past 4 weeks because of various symptoms such as “feeling lonely or blue,” “feeling no interest in things,” “trouble falling asleep,” and “thinking, speaking, and moving at a slower pace.” Five response choices range from “not at all” to “extremely.” The diagnostic utility of the SCL-90-R has been demonstrated in numerous studies (21).
Dependent Variables
HRQL was measured across multiple domains with the Medical Outcomes Study Short Form (SF). Subscales from the SF-36 were used to assess Vitality and Mental Health. The SF-36 was developed to measure HRQL in samples of any age, disorder, or treatment group, and includes subscales in 8 domains (22). Its psychometric properties are well established (15, 22, 23). Other SF-derived independent variables besides the 2 subscales were the Mental Component Summary (MCS-12) and the Physical Component Summary (PCS-12) derived from items from the briefer SF-12 scale, and a single-item General Health score—also from the SF-12. The component summary scales were developed as a comprehensive measure of mental or physical health status and each includes 6 items. General health was measured with the item “In general, would you say your health is [excellent, very good, good, fair, or poor]?” This item has been shown to predict long-term health outcomes (24). All SF scores range from 0 (maximal impairment) to 100 (no impairment). Items use a mix of Likert-type scales ranging from 3 to 6 points.
An additional single-item measure also assessed overall quality of life (25). The item asked patients to rate their quality of life during the past month including physical and mental well-being on a scale of 0 to 10. “If you feel your life is perfect—you are completely well—then choose level 10. If you feel your situation is about as bad as dying, then choose level 0.”
Disability was measured in two ways—with the 3-item Sheehan Disability Scale (26), and by assessing the number of days spent in bed or with reductions in usual activities in the previous 4 weeks. Somatic symptom severity was assessed with a combined scale made up of 14 items from the PHQ-15 (27) and 10 items from the M.D. Anderson Symptom Inventory (28).
Covariate
Age, comorbid diseases (i.e., presence of a disorder from one of eight disease groups such as arthritis or heart disease), gender, race, and a composite index of socioeconomic disadvantage were analyzed as potential covariates. The socioeconomic disadvantage index includes self-reported levels of education, employment, and income.
Analysis
For categorical analysis, participant data were initially allocated by clinical status into four groups—no depression or anxiety (reference group), anxiety only, depression only, and comorbid anxiety and depression. To determine group status, a cutoff score of ≥ 10 was used for both the GAD-7 for anxiety and the PHQ-9 for depression. It should be noted that, because only participants who were assessed as having pain or depression were enrolled in the INCPAD study, all in the reference group had cancer-related pain of at least moderate severity, whereas those in the other 2 groups may or may not have had pain. Means and standard deviations were calculated by group for each continuous variable and analysis of variance (ANOVA) was used to test for differences among groups.
To test our hypotheses, generalized linear regression (GLM) modeling was conducted for each dependent variable—first separately with anxiety alone or depression alone as independent variables, then with both anxiety and depression entered into the model, and third, with anxiety and depression in the model along with the covariates of age, sex, race, medical comorbidity, and the socioeconomic index. For total disability days, Poisson regression modeling was substituted for GLM. All hypothesis testing was conducted at the 0.05 significance level (2-tailed).
Results
Sample Characteristics
Roughly, about a third of the total INCPAD sample had minimal to no anxiety (37%), a third had mild anxiety (28%), and a third had moderate to severe anxiety (35%). Depression was more heavily represented in the sample—assessed in 309 participants (78%)—which was expected given that depression, along with pain, was the focus of the INCPAD study and a factor in the inclusion criteria. Of the 309 participants with depression, 135 had comorbid anxiety.
Because only patients with depression and/or pain were enrolled in INCPAD, a disproportionate number of participants had depression relative to a typical oncology practice and, consequently, few patients (n =8) had anxiety without depression. Thus, the latter group was excluded from the analysis, leaving a sample of 397 adult cancer patients. Overall, 271 (68%) were women, and 315 (79%) were white. About half (49%) were married. The sample included people of various education levels, with 86 (22%) lacking a high school diploma, 159 (40%) being high school graduates, and the remainder having at least some college. Only 20% were employed, with 44% reporting they were unable to work. Most of the remaining participants (29%) were retired. Nearly half (48%) reported having just enough income to make ends meet; 24% reported being financially “comfortable,” and 27% reported not having enough to make ends meet.
Characteristics by Clinically Defined Groups
Table 1 summarizes the baseline characteristics by anxiety and/or depression subgroup. Participants with comorbid depression and anxiety were younger (p < 0.0001), less likely to be married (p = 0.01), and reported more comorbid medical diseases (p = 0.01) than the other groups. People in the groups with depression or comorbid depression and anxiety also were less likely to be employed, more often reported being unable to work, and were less likely to self-report being financially comfortable (all at p < 0.0001). There were no differences between groups by gender or race. Group differences existed across all but one of the HRQL domains (Table 2). As expected, differences in the Physical Component Summary (PCS-12) were nonsignificant, suggesting that the groups had been successfully allocated according to psychological rather than physical differences. In those variables with group differences, symptoms were shown to be significantly more severe or problems more pronounced in an incremental fashion across the three groups. That is, the depression-only group reported doing less well than the group with neither depression nor anxiety, and the comorbid depression-anxiety group did less well than those with depression only. All pairwise comparisons except one (SF General Health) remained significant (p < 0.05) even after Tukey's adjustment for multiple comparisons. Taken as a whole, these findings suggest that depression has an adverse association with cancer patients' quality of life, and that comorbid anxiety is an additive influence.
Table 1. Demographic characteristics by Anxiety and Depression Status*.
| Baseline Characteristics | No Depression or Anxiety | Depression only | Depression and Anxiety |
|---|---|---|---|
| n=88 | n=174 | n=135 | |
| Age | 60.53 (9.53) | 60.31 (11.40) | 55.89 (10.13) |
| Women | 62 (70%) | 115 (66%) | 94 (70%) |
| White | 65 (74%) | 143 (82%) | 107 (79%) |
| Married | 47 (53%) | 96 (55%) | 52 (39%) |
| BPI Pain Severity | 4.93 (2.00) | 3.53 (2.48) | 4.80 (2.16) |
| Comorbid Diseases (#, 0-8) | 1.81 (1.45) | 1.96 (1.51) | 2.39 (1.76) |
| Education | |||
| • < High school | 20 (25%) | 31 (18%) | 33 (24%) |
| • High school graduate | 30 (34%) | 74 (43%) | 55 (41%) |
| • Some college | 23 (26%) | 44 (25%) | 35 (26%) |
| • College graduate | 13 (15%) | 25 (14%) | 12 (9%) |
| Employment status | |||
| • Employed | 30 (34%) | 26 (15%) | 22 (16%) |
| • Unable to work | 25 (29%) | 67 (39%) | 82(61%) |
| • Retired | 27 (31%) | 66 (38%) | 21 (16%) |
| • Other | 5 (6%) | 15 (9%) | 10 (7%) |
| Income | |||
| • Comfortable | 28 (32%) | 51 (29%) | 18 (13%) |
| • Just enough to make ends meet | 48 (55%) | 79 (46%) | 63 (47%) |
| • Not enough to make ends meet | 11 (13%) | 43 (25%) | 54 (40%) |
Anxiety-only group had only 8 participants and was dropped from the analysis. Of note, all participants in the No Depression or Anxiety group met study criteria for clinically significant pain and therefore should not be considered asymptomatic for comparison purposes.
Table 2. Baseline Functional Status and Quality of Life by Anxiety and Depression Status*.
| No Depression or Anxiety | Depression only | Depression and Anxiety | P value * | |
|---|---|---|---|---|
| n=88 | n=174 | n=135 | ||
| Independent Variables (range) | ||||
| SCL-20 depression (0-4) | 0.76 (0.49) | 1.34 (0.52) | 2.03 (0.56) | 0.000 |
| GAD anxiety (0-21) | 2.83 (2.66) | 4.84 (2.78) | 14.71 (3.28) | 0.000 |
| Dependent Variables (range) | ||||
| SF General Health (0-100) | 37.41 (29.53) | 28.51 (29.32) | 22.07 (25.71) | 0.004 |
| SF Vitality (0-100) | 42.97 (20.16) | 26.62 (17.40) | 20.97 (15.51) | 0.000 |
| SF Mental Health (0-100) | 76.65 (15.23) | 58.51 (16.64) | 39.44 (18.19) | 0.000 |
| SF 12 Mental-MCS (0-100) | 51.49 (9.38) | 40.88 (10.49) | 33.03 (11.06) | 0.000 |
| Sheehan Disability (0-10) | 3.54 (2.75) | 5.49 (2.68) | 6.60 (2.44) | 0.000 |
| Overall Quality of Life (0-10) | 7.20 (2.16) | 5.47 (1.97) | 4.81 (2.25) | 0.000 |
| Physical symptom total (0-44) | 14.40 (6.57) | 17.34 (5.23) | 21.96 (6.21) | 0.000 |
| Total 4-wk disability days (0-28) | 11.36 (10.14) | 17.31 (10.33) | 19.50 (8.90) | 0.000 |
All pairwise comparisons with Tukey adjustment were significant (p < 0.05) except SF General Health, in which no difference was found between the Depression-Anxiety group and the Depression-Only group.
Independent and Additive Effects
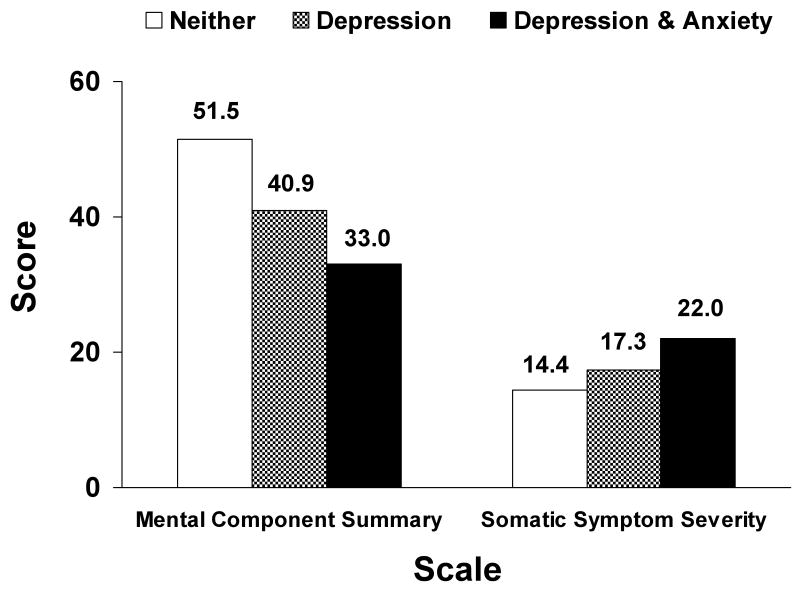
In testing our hypotheses through GLM modeling, anxiety was found to be significantly associated with every dependent variable tested when entered into the model separately, and the same was true for depression (p < 0.0001 in all but 1 case; see Table 3). These findings supported H1 and H2. When anxiety and depression were entered into the same model together for each dependent variable, however, the results were mixed. Depression's association held across every dependent variable (p < 0.0001), but anxiety's association remained significant only for the SF Mental Health subscale (p < 0.0001), the MCS-12 (p = 0.005), and somatic symptom severity (p < 0.0001). The independent and additive effects of depression and anxiety are illustrated in the Figure. Thus, H3 was not supported; after accounting for depression, anxiety had an independent association in some domains of HRQL but not others. Similar results were found when both anxiety and depression were entered into models together along with covariates—age, sex, race, medical comorbidity, and socioeconomic disadvantage index. In the covariate models, depression was associated with every dependent variable. After accounting for depression, however, anxiety was only associated with SF Mental Health (p < 0.0001), the MCS-12 (p = 0.004), and somatic symptom severity (p = 0.007). H4 is, therefore, partially supported. In those domains in which anxiety had an association independent of depression, that association was only mildly attenuated by the covariates and the association was still found to be statistically significant.
Table 3. Association of Depression and Anxiety with Functional Status and Health-Related Quality of Life in Multivariable Models.
| Functional Status and Health-Related Quality of Life Domains † | Strength of Association of Depression (SCL-20) and Anxiety (GAD-7) Severity with Functional Status and Health-Related Quality of Life * | |||||
|---|---|---|---|---|---|---|
| Separately | Combined | Adjusted Combined | ||||
| t | p | t | p | t | p | |
| SF Mental Health | ||||||
| • Depression | - 24.15 | < .0001 | - 13.34 | < .0001 | - 13.29 | < .0001 |
| • Anxiety | - 19.03 | < .0001 | - 6.98 | < .0001 | - 6.95 | < .0001 |
| SF MCS | ||||||
| • Depression | - 20.96 | < .0001 | - 13.12 | < .0001 | -12.92 | < .0001 |
| • Anxiety | - 14.04 | < .0001 | -2.80 | .005 | - 2.94 | .004 |
| Somatic symptoms | ||||||
| • Depression | 14.97 | < .0001 | 8.69 | < .0001 | 8.30 | < .0001 |
| • Anxiety | 11.67 | < .0001 | 2.98 | < .0001 | 2.72 | .007 |
| SF Vitality | ||||||
| • Depression | - 14.01 | < .0001 | - 11.11 | < .0001 | - 11.53 | < .0001 |
| • Anxiety | - 7.64 | < .0001 | 1.55 | .12 | 1.09 | .28 |
| SF Gen Health Percept. | ||||||
| • Depression | - 5.44 | < .0001 | - 3.99 | < .0001 | - 3.63 | .0003 |
| • Anxiety | - 3.62 | .0003 | 0.17 | .86 | 0.60 | .55 |
| Sheehan Disability Index | ||||||
| • Depression | 12.47 | < .0001 | 8.67 | < .0001 | 8.64 | < .0001 |
| •Anxiety | 8.21 | < .0001 | 0.30 | .76 | - 0.03 | .98 |
| Overall quality of life | ||||||
| • Depression | - 10.06 | < .0001 | - 6.90 | < .0001 | - 6.92 | < .0001 |
| • Anxiety | - 6.92 | < .0001 | - 0.39 | .70 | - 0.49 | .63 |
Association of each functional status domain with depression alone and anxiety alone in separate models, with depression and anxiety together in combined model, and with depression and anxiety adjusted for covariates of age, sex, race, medical comorbidity, and socioeconomic disadvantage index
Figure.
Incremental adverse effect of depression and anxiety on Mental Component Summary score (scored on 0 to 100 scale, with 0 representing worst and 100 best mental health) and somatic symptom severity (scored on 0 to 44 scale, with 0 representing no somatic symptom burden and 44 the worst burden).
Poisson regression modeling tested the association between depression/anxiety and the number of self-reported disability days in the past four weeks. Results were similar to those found in the GLM models. In the Poisson models, depression and anxiety were each significantly related to disability days when entered separately (Wald χ2 = 419.5, and 222.4 respectively, p < 0.0001). When entered together into the model, however, depression was significantly associated with disability days (χ2= 199.9, p < 0.0001) and anxiety was not (χ2= 0.43, p = .51). Adjusting for covariates did not change the findings (depression χ2= 172.6, p < 0.0001; anxiety χ2= 0.22, p = -.64).
Discussion
These findings indicate that depression and anxiety are each associated with multiple domains of health-related quality of life in cancer patients. Group comparisons suggested that participants with no depression or anxiety had better HRQL than did those with depression only, and that those with comorbid depression-anxiety reported worse HRQL than did the depression-only group. Moreover, the participants in the depression and anxiety groups also self-reported incrementally more disability on both an overall measure (Sheehan Disability Index) and a measure of the number of disability days. In interpreting these findings, it is important to note that the 88 patients in the reference group with no depression or anxiety did meet criteria for pain, making it an atypical comparison group. However, since pain itself causes pervasive disability across multiple domains of HRQL and functional status (29), it is likely that even greater differences would be found if we had compared a depressed group and a group with depression and anxiety to a group of cancer patients with no pain as well as no anxiety or depression. Thus, our findings of the relationship between depression/anxiety and HRQL may be conservative given the nature of our reference group.
GLM regression modeling further supported significant linear associations of depression severity and anxiety severity on HRQL and disability, all in the expected direction. Associations were significant for each symptom across all domains when modeled separately. The findings are more equivocal, however, about the degree to which anxiety's relationship to these outcomes exists independent of depression. When the two variables were entered into the models together, depression showed a significant association across all domains, but anxiety associations were not found to be significant in a majority of the domains after depression had been accounted for.
Of the three domains in which significant independent associations of anxiety were found, two were mental health constructs—SF Mental Health and the SF Mental Component Summary. It is not surprising that anxiety would show an association independent of depression in these domains, which are intended to represent psychological symptoms. Somatic symptom severity was the other variable in which anxiety showed an association over and above that of depression. This finding is consistent with previous evidence in noncancer medical populations of the strong associations among anxiety, depression, and somatization – the “SAD triad” (30, 31). The current finding does contradict, however, a recent finding that neither anxiety nor depressed mood was associated with physical symptoms in a sample of hospitalized advanced cancer patients (1). The explanation for the incongruent findings may be difference in measurement and/or differences in the cancer patient sample, since the current data is derived from a more representative sample of patients with different types and stages of cancer .
Our results suggest that depression has more pervasive effects than anxiety on non-mental domains of quality of life in cancer patients. Anxiety had an effect distinguishable from depression on mental health and functioning as well as somatic symptom severity. Perhaps these findings could be considered consistent with the tripartite model of anxiety and depression (10). This theory holds that anxiety and depression represent two affective syndromes with some components in common and some that are unique. According to the tripartite model, anxiety and depression share a general distress factor. An additional structural component that is specific to anxiety, however, is physiological hyper-arousal, whereas a component over and above general distress that distinguishes depression is anhedonia. It could be that accounting for depression in our GLM analyses represented a partialing out of the general distress that is common to both anxiety and depression. Factors specific to anxiety, then, might explain why the comorbid anxiety-depression group fared worse than the depression-only group on most domains in our group comparisons. It might also explain the independent association of anxiety over and above depression on the mental health domains in this study. In the context of the tripartite model, our findings may merely suggest that in cancer patients, the general distress component is proportionally more influential than the unique factors of anxiety and depression on domains of HRQL. INCPAD was by design oversampled for depression, which may have contributed to the more pervasive findings for depression. An important next step would be to conduct similar analyses in a sample with a relatively even proportion of patients with anxiety, and including an anxiety-only group in the comparisons.
A limitation to this study is its cross-sectional design, which precludes any interpretations about causality or directionality. While it is tempting to conclude that anxiety and depression have negative effects on HRQL, it is also possible that lower HRQL contributes to severity of anxiety and depression or that a cancer diagnosis or other cause has simultaneous effects on HRQL as well as depression and anxiety. Moreover, it is possible that the lower self-reported HRQL might be related to the tendency of a depressed person to make more negative appraisals of HRQL. Other important limitations have already been alluded to—the oversampling of depression relative to anxiety and the fact that the reference group is a clinical sample with pain symptoms.
In summary, depression and anxiety are independently associated with mental health domains and somatic symptom severity in a heterogeneous sample of cancer patients who screened positive for depression or pain or both. In other important domains of HRQL and disability (vitality, general health, overall quality of life, and disability), anxiety and depression had significant associations when analyzed separately; however, when entered into a general linear model together, anxiety did not show an independent association after depression had been accounted for. The overall findings of this study are consistent with a large body of literature that suggests that, although the overlap of the two symptoms is pronounced, anxiety is distinguishable from depression in some—although not all—contexts (9, 10). It also highlights the importance of recognizing and treating depression and anxiety in oncology practice, not only for the suffering caused by the disorders themselves but also for their adverse effects on multiple domains of HRQL.
Acknowledgments
This manuscript was supported by a grant from the National Cancer Institute to Dr. Kroenke (R01 CA-115369) and a grant from the National Cancer Institute (R25 CA-117865-01A11)
Footnotes
Financial Disclosures: Dr. Kroenke has received previous research support from Eli Lilly and honoraria from Eli Lilly, Forest Pharmaceutical, and Pfizer, Inc.
References
- 1.Teunissen SCCM, de Graeff A, Voest EE. Are anxiety and depressed mood related to physical symptom burden? A study in hospitalized advanced cancer patients. Palliative Medicine. 2007;21:341–346. doi: 10.1177/0269216307079067. [DOI] [PubMed] [Google Scholar]
- 2.Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd. Guilford Press; New York: 2002. p. 704. [Google Scholar]
- 3.Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJG, Goodwin RD, Kubzansky L, et al. Anxiety disorders and comorbid medical illness. General Hospital Psychiatry. 2008 May-Jun;30(3):208–225. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Stark D, Kiely M, Smith A, Velikova G, House A, Selby P. Anxiety disorders in cancer patients: Their nature, associations, and relation to quality of life. Journal of Clinical Oncology. 2002 July 15;20(14):3137–3148. doi: 10.1200/JCO.2002.08.549. [DOI] [PubMed] [Google Scholar]
- 5.Carr D, Goudas L, Lawrence D, Pirl W, Lau J, DeVine D, et al. Management of cancer symptoms: Pain, depression, and fatigue. Evidence Report: Technology Assessment (Summary) 2002 July;61:1–5. doi: 10.1037/e439612005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pirl WF. Evidence report on the occurrence, assessment, and treatment of depression in cancer patients. Journal of the National Cancer Institute Monographs. 2004;32:32–39. doi: 10.1093/jncimonographs/lgh026. [DOI] [PubMed] [Google Scholar]
- 7.Spiegel D, Giese-Davis J. Depression and cancer: Mechanisms and disease progression. Biological Psychiatry. 2003;54:269–282. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- 8.McDaniel JS, Musselman DL, Porter MR, Reed DA, Nemeroff CB. Depression in patients with cancer. Archives of General Psychiatry. 1995 February;52:89–99. doi: 10.1001/archpsyc.1995.03950140007002. [DOI] [PubMed] [Google Scholar]
- 9.Brown TA, Barlow DH. Classification of anxiety and mood disorders. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd. Guilford Press; New York: 2002. pp. 292–327. [Google Scholar]
- 10.Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100(3):316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 11.Dietrich AJ, Oxman TE, Williams JW, Jr, Schulberg HC, Bruce ML, Lee PW, et al. Reengineering systems for the treatment of depressionin primary care: Cluster randomised controlled trial. BMJ. 2004;329:602–605. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oxman Te, Dietrich AJ, Williams JW, Jr, Kroenke K. A three-component model for reengineering systems for the treatment of depression in primary care. Psychosomatics. 2002;43:441–450. doi: 10.1176/appi.psy.43.6.441. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Theobald D, Norton K, Sanders R, Schlundt S, McCalley S, et al. The Indiana Cancer Pain and Depression (INCPAD) Trial: Design of a telecare management intervention for cancer-related symptoms and baseline characteristics of study participants. General Hospital Psychiatry. 2009;31:240–253. doi: 10.1016/j.genhosppsych.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Kosinski M, Keller SD. SF-35 Physical and Mental Health Summary Scales: A user's manual. The Health Institute, New England Medical Center; Boston: 1994. [Google Scholar]
- 16.Kroenke K, West SL, Swindle R, Gilsenan A, Eckert GJ, Dolor R, et al. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: A randomized trial. JAMA. 2001;286:2947–2955. doi: 10.1001/jama.286.23.2947. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cleeland CS. Pain assessment in cancer. CRC Press; Boca Raton, FL: 1991. [Google Scholar]
- 19.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007 Mar 6;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 21.Derogatis LR. SCL-90-R, Brief Symptom Inventory, and matching clinical rating scales. In: Maruish M, editor. Psychological testing, treatment planning, and outcome assessment. Erlbaum; New York: 1994. [Google Scholar]
- 22.Ware JE, Gandek B, IQOLA Project Group The SF-36 Health Survey: Development and use in mental health research and the IQOLA Project. International Journal of Mental Health. 1994;23(2):49–73. [Google Scholar]
- 23.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. The Health Institute, New England Medical Center; Boston: 1993. [Google Scholar]
- 24.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- 25.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler EM, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting. JAMA. 2002 December 11;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 26.Sheehan DV, Harnett-Sheehan K, Raj Ba. The measurement of disability. International Clinical Psychopharmacology. 1996;11(Supplement 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K. Physical symptom disorder: A simpler dianostic category for somatization-spectrum conditions. Journal of Psychosomatic Research. 2006;60:335–339. doi: 10.1016/j.jpsychores.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 28.Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, et al. Assessing symptom distress in cancer patients - The M D Anderson Symptom Inventory. 2000:1634–1646. doi: 10.1002/1097-0142(20001001)89:7<1634::aid-cncr29>3.0.co;2-v. 2000. [DOI] [PubMed] [Google Scholar]
- 29.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Archives of Internal Medicine. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 30.Lowe B, Spitzer RL, Williams JBW, Mussell M, Schellberg D, Kroenke K. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. General Hospital Psychiatry. 2008 May-Jun;30(3):191–199. doi: 10.1016/j.genhosppsych.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K. The interface between physical and psychological symptoms. Primary Care Companion Journal of Clinical Psychiatry. 2003;5 7:11–18. [Google Scholar]