Abstract
OBJECTIVE
The family provides an important communication nexus for information and support exchange about family cancer history, and adoption of family-wide cancer risk reduction strategies. The goals of this study were to: 1) use the family systems theory to identify characteristics of this sample of families at increased risk of developing melanoma and 2) to relate familial characteristics to the frequency and style of familial risk communication.
METHODS
Participants were first-degree relatives (n=313) of melanoma patients, recruited into a family web-based intervention study. We used multivariable logistic regression models to analyze the association between family functioning and family communication.
RESULTS
Most participants were female (60%), with an average age of 51 years. Fifty percent of participants reported that they spoke to their relatives about melanoma risk and people were more likely to speak to their female family members. Familial adaptation, cohesion, coping, and health beliefs were strongly associated with an open style of risk communication within families. None were associated with a blocked style of risk communication. Only cohesion and adaptation were associated with the amount of risk communication that occurred within families.
CONCLUSIONS
Overall, individuals who came from families that were more highly cohesive, adaptable, and shared strong beliefs about melanoma risk were more likely to communicate openly about melanoma. The fact that this association was not consistent across blocked communication and communication frequency highlights the multifaceted nature of this process. Future research should focus on the interplay between different facets of communication.
INTRODUCTION
The family provides an important communication nexus for information exchange and support about family cancer history, and for the adoption of family-wide cancer risk reduction strategies. Individuals view and, interpret health information through the lens of their family and disseminate that information within the family as well [1-8]. Additionally, a diagnosis of cancer in one family members often has implications for other family members. Thus, when one individual gets diagnosed with melanoma, sharing this information can be crucial in leading to early screening or prevention activities to reduce morbidity and mortality. Since, under HIPPA regulations, medical professionals are constrained not to share health information directly with relatives[9], it is vital to understand the properties of families that may aid or hinder this information from reaching appropriate family members}. Previous intervention work with couples and parent-child dyads has shown that communication competencies can be learned and improved [10, 11]. This suggests that problems that may exist with family communication can be improved upon with intervention [12, 13].
What do we know about communicating cancer risk information within families?
Research on cancer risk communication within families has generally been centered around communication of genetic testing results in high risk families [14, 15]. While this literature provides a starting place to identify properties of family health communication, it is likely to have limited generalizability outside of the specific context of delivering a genetic test in high-risk families. Since we are looking at general cancer risk communication in families at moderate risk of developing melanoma, this literature may be less applicable.
Outside of high risk families in the genetic testing context, we know very little about how families communicate about cancer risk. Most, although not all [16] of these studies, have been conducted in families with a moderate risk of cancer and have reported low frequencies of communication within the family about cancer risk and risk factors [17-19]. A few qualitative studies also examined characteristics of risk communication within families [3, 4, 20, 21]. While these studies provide insight into the frequency and general patterns of familial communication, other familial characteristics such as coping, familial cohesion, health beliefs, and adaptation potentially associated with this communication are poorly understood.
Using a family systems perspective to study family communication
The family systems perspective provides a useful model for examining the association between familial characteristics and melanoma risk communication [22]. The family systems perspective has recently been proposed by Peterson and colleagues as a framework for conducting family-based research in hereditary risk and genetic testing [14]. The family systems perspective accounts for the reciprocal nature of family relationships, the broader social context in which families exist, and the multiple dimensions that comprise family functioning [14]. The model posits that families have certain characteristics generally within each of the following three dimensions: 1) organization and structure of family relationships, 2) health related cognitions and beliefs shared within families, and 3) family communication [23-26].
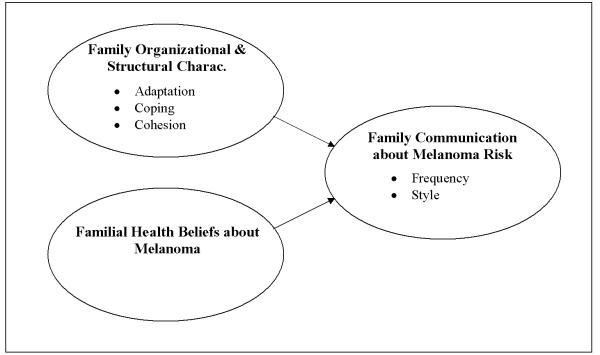
For this study, an expanded version of the Peterson’s version of the family systems model [14] was used to examine the relationship between familial organization and structures, health related beliefs, and communication (figure 1) in families at increased risk of developing melanoma. Following Peterson, we hypothesized that a family’s organizational and structural characteristics, especially adaptation, coping and cohesion, plus shared familial beliefs about melanoma would together predict the frequency and style of family communication about melanoma risk.
Figure 1.
Conceptual model for analyzing the relationship between family functioning and family communication about melanoma risk.
METHODS
Study Design
Data for this study come from the baseline data of participants in the SunTalk study, a randomized trial of a web-based intervention to measure and improve knowledge, awareness and communication about melanoma prevention within families at increased of developing melanoma. Families were randomized, as units, into the web-based intervention or to the control (delayed intervention) group. Family recruitment into the study began with a melanoma case. All family members were invited to participate in the intervention but three family members were randomized from each family and were recruited to participate in all evaluation activities. The members of the family unit that were randomized to participate in the evaluation activities were the case, one first-degree-relative of the case, and one adult member of the family who had a child under the age of 18 (this person did not have to be a first-degree-relative). For this paper, we analyzed only those first-degree relatives (FDRs) of melanoma.cases enrolled in the study who completed the baseline survey (n=313).
Recruitment/Randomization
Two sources were used to recruit cases and subsequently families into the SunTalk study: 1) the Northwest Cancer Genetics Network (NWCGN), the regional site of the Cancer Genetics Network and 2) The SEER registry (Cancer Surveillance System or CSS) at Fred Hutchinson Cancer Research Center. Melanoma cases diagnosed with a first primary melanoma between April 1st 1998 and October 1st 2001 from the NWCGN. The CSS is a population-based cancer registry, part of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. For both sources, cases were included who were living, had a diagnosis of non-ocular melanoma, and had an address and telephone number available in the registry.
If the case was eligible and interested, project staff then collected names and contact information for all possible first-degree-relatives (FDRs) and parents. One of the FDRs and one of the parents were then randomly selected to participate in the evaluation. Additional details about the recruitment process are described by Bowen and colleagues elsewhere [27]. Of the 1380 cases approached: 331 did not fulfill family eligibility criteria, 263 did not have valid family contact information, and 473 had at least one family member who declined. Overall, 313 families participated in the SunTalk study.
Measures
1) Outcome Variables
Two different components of family communication were examined: (i.e. frequency and style).
Frequency of communication was assessed using six items. Each item asked FDRs how much they spoke to each of six different family members (mother, father, sisters, brothers, children and grandchildren) about melanoma in the past year. Responses were measured using a 4-point Likert scale with the following categories: not at all, a little, somewhat, or a lot (or don’t currently have this family member). As previously described by Bowen and colleagues[19], an overall frequency of communication score was computed by summing responses within person and calculating an average. Communication frequency was dichotomized into two categories: less frequently (avg. score: 1–2) vs. more frequently (avg. score >2).
A novel 8-item measure of communication style was developed based on previous qualitative research conducted by Kenen and colleagues [21]. In their study of families with Hereditary Breast and Ovarian Cancer (HBOC), Kenen and colleagues identified several distinct styles that families employed when communicating genetic information, including open and supportive, directly and indirectly blocked, self-censored, and use of third parties [21]. Based on these categories, we generated an item-pool corresponding to these the three categories listed above and pilot tested these with a small group of individuals [28]. The final measure included items assessing open and supportive, directly and indirectly blocked, and self-censored communication styles. Each of the items asked FDRs to respond to a series of statements about their family. An example of an item is, “My family speaks openly about their worries about other family members developing melanoma.” FDRs were asked to use a four-point Likert scale to explain the amount to which they agreed or disagreed with the statement (strongly agree, somewhat agree, somewhat disagree, and strongly disagree).
We performed a principal components analysis on the item set [29]. If an item had a loading ≥ 0.30 for that component and ≤ 0.30 for all other components it was determined to load on that component. Two components were identified from the eight-item communication styles scale. The first component had an eigenvalue of 3.2 and the second had an eigenvalue of 1.7. Three questions comprised the first component.
We identified the first component as open communication style and the second as blocked communication style. Open communication style was defined by the perception that melanoma information could be freely shared within the family and that family members supported each other in discussing this information. Blocked communication style was defined by there being some type of barrier to information flow within the family, either direct refusal or lack of responsiveness to discussing melanoma.
The open communication style subscale explained 32% of the variance in the total scale and the blocked explained 30% of the variance. Both subscales showed high internal consistency reliability (α= 0.81 and 0.72 respectively). For open communication style, responses were dichotomized into those who had an average score> 3.5 (open) vs. those with a score ≤ 3.5 (moderately open- closed). For blocked communication style, responses were dichotomized into those who had an average score >1 (moderately blocked) vs. those who had an average score =1 (not blocked).
2) Independent Variables
Family Coping Type
Carver’s brief cope scale is a scale aimed at assessing an individual’s coping mechanisms [30]. The 28 item scale includes questions aimed at determining 14 different styles of coping. For the purposes of this study, the brief cope was modified to address a ‘familial coping style’ instead of an individual coping style. Thus all questions were asked in relation to how the family as a unit copes with stressful situations. For example, FDRs were asked to reply to their level of agreement with the following statement, “My family concentrates their efforts on doing something about the situation they are in (familial active coping).” Response categories ranged from one to four with one being ‘they usually do not do this at all’ to four being ‘they do this a lot’. We chose to focus on two styles (active coping and denial coping) due to the fact that they exhibited a satisfactory degree of internal consistency reliability in this population (α=0.66 and 0.57 respectively), in comparison to other subscales. An example Summary scores were calculated for each subscale and scores were dichotomized based on distributions. Summary scores were only calculated for individuals answering both subscale items [28].
Family Adaptation
The adaptation measure used here is a subscale within the ‘Family Adaptability and Cohesion Evaluation Scale’ version II (FACES II) measure developed by Olson and colleagues. This subscale has been used in variety of different populations and contexts to measure adaptation [11]. Adaptation refers to the amount of change in relationships and relationship rules within the family [11, 31]. It consists of 14 items and each item asked FDRs to respond to the degree to which he/she agrees with a statement about their family. Responses were assessed using a five-point Likert scale and response categories were assigned a numeric score from one through five with one being almost never and five being almost always. The alpha we calculated was reasonably high (α=0.73). If the individual answered at least 70% of the items, responses to unanswered items were imputed based on the mean value of the answered items (Approximately fifty people failed to answer at least one item and we imputed the value(s) for their missing item(s). Two individuals failed to answer >30% of items and thus we did not calculate a score for them). Updates to the original FACES II algorithm show that scores are purported to function in a linear manner (versus a curvilinear fashion) with lower scores indicating that families have low flexibility and higher scores indicating greater flexibility or adaptation [11, 31-33]. Due to the distribution of our data, summary scores were dichotomized into more flexible if the score was greater than 48 and less flexible if the score was between 14 and 48.
Family Cohesion
The cohesion measure is a subscale within FACES II. It consists of 16 items, with the same response structure used in the adaptation scale. An example of an item is, “Family members consult other family members on their decisions.” In previous research the items were shown to have a high degree of reliability (Cronbach’s α=0.87). We calculated a nearly identical Cronbach’s alpha in our population (α=0.88). If the individual answered at least 70% of the items, responses to unanswered items were imputed based on the mean value of the answered items (Approximately 14 individuals failed to answer at least one item and we imputed the value(s) for their missing item(s). Everone answered at least 75% of all items). As with the adaptation subscale, lower scores indicate a lower degree of family cohesion while higher scores indicate a greater degree of cohesion. Due to the distribution of our data, responses were dichotomized into two levels: more connectedness if their score was >62 and low connectedness if their score was between 16 and 62.
Familial Health Beliefs
In order to measure familial health beliefs, six items were developed to assess familial perceptions of melanoma severity, susceptibility, risk, and suntanning beliefs. An example of one question included in the survey is, “In my family, people generally believe that having melanoma is a serious threat to their health.” FDRs were asked to respond to the degree to which they agreed or disagreed with each statement. Responses were measured using a four-point Likert scale with categories one being strongly agree and four being strongly disagree.
As described above, a principle components analysis was conducted and two components were identified. The first had an eigenvalue of 2.2 and the second had an eigenvalue of 1.1. Three of the six questions comprised the first component and two of the six comprised the second component. As in the communication style scale, one item had approximately equal loadings on both components so we dropped this item. We identified the first component as ‘family norms around seriousness of melanoma’ and the second as ‘familial tanning norms’. The melanoma seriousness subscale accounted for 37% of the variance in the total scale and the tanning norms subscale explained 19% of the variance. Both subscales showed moderate internal consistency reliability (α= 0.52 and 0.50 respectively). Responses were dichotomized into low seriousness (2.01–4) vs. high seriousness (1–2).
3) Background Variables
Sociodemographic characteristics of the family were also measured. Sociodemographic variables included education, household income, geographic distance from case, gender, race, age, and marital status.
Analyses
Data analysis for this paper was performed using SPSS software, Version 15.0 of the SPSS System for Windows [34]. Multivariable logistic regression was used to analyze for possible associations between family functioning characteristics and three different family communication characteristics (open, blocked, and frequency), controlling for covariates. The first model examines the probability of having an open style of family communication, the second examines the probability of having a moderately blocked style of family communication, and the third examines the probability of having moderately frequent communication about melanoma. Separate regression models were examined for each of these three main outcomes.
All family functioning characteristics (i.e. independent variables) were analyzed using models that were adjusted for the following sociodemographic covariates: age, gender, geographic distance from case, education, and marital status.
RESULTS
Frequencies of family organization/structure and sociodemographic variables
Sociodemographic and family functioning characteristics are shown in Table 1. FDRs were between 19 and 91 years of age with an average age of 51. Overall, 8% of the sample did not provide income information. The majority of the sample was female (64%) with 56% reporting having at least a college degree. Most FDRs were married or partnered (72%) and 82% lived in a different city from the melanoma case in their family.
Table 1. Sociodemographic and family functioning characteristics of first-degree relatives of melanoma cases.
| Demographic Characteristics |
N | % | Family functioning variables | N | % |
|---|---|---|---|---|---|
| Total | 313 | Total | 313 | ||
| Age (yrs) | Active coping † | ||||
| Average age (SD) [range] |
51 (15.6) [19–91] |
------ | Often | 149 | 47.6 |
| Rarely | 160 | 51.1 | |||
| Gender | Denial coping † | ||||
| Female | 199 | 63.6 | Sometimes | 166 | 53.0 |
| Male | 114 | 36.4 | Never | 144 | 46.0 |
| Educational level | Adaptation/Flexibility† | ||||
| ≤High School degree | 35 | 11.2 | Mean summary score (SD) [range] |
50 (6.6) [31–64] |
------ |
| Some college | 102 | 32.6 | More | 192 | 61.3 |
| ≥College degree | 176 | 56.2 | Less | 119 | 38.0 |
| Race | Cohesion | ||||
| White | 299 | 95.5 | Mean summary score (SD) [range] |
62 (9.4) [25–80] |
------ |
| Non- White | 14 | 4.5 | High | 172 | 55.0 |
| Low | 141 | 45.0 | |||
| Marital status | Family seriousness norms† | ||||
| Not married | 88 | 28.1 | Serious | 261 | 83.4 |
| Married/partnered | 225 | 71.9 | Not serious | 43 | 13.7 |
|
| |||||
| Same City | Family tanning norms† | ||||
| Yes | 55 | 17.6 | Positive | 71 | 22.7 |
| No | 258 | 82.4 | Negative | 234 | 74.8 |
|
| |||||
| Income | |||||
| ≤ 50K | 96 | 30.7 | |||
| 51–70K | 55 | 17.6 | |||
| ≥ 70K | 137 | 43.8 | |||
| Missing | 25 | 8.0 | |||
Category contains less than 3% missing values. Percents may not sum to 100 due to missing values. Categories with more than 3% missing values (i.e. income) are noted in the table.
Approximately half of FDRs (48%) reported that their family often employs active coping strategies when faced with stressful events. Nearly half (46%) reported that their families rarely employ denial to cope with stressful events. Missing values represented less than 3% of the sample for each variable. Scores on the family adaptation ranged from 31 at the lower end (i.e. less flexible families) of the scale to 64 at the high end of the scale. The average score was around 50 and the majority of FDRs reported that their families were generally more flexible (61%). Approximately half (55%) reported high levels of family cohesion. Most participants reported that their families had strong beliefs about the seriousness of melanoma (83%). Family norms around tanning were generally negative, with 75% reporting that they did not support tanning.
Characteristics of family communication about melanoma
The frequencies for each of the different characteristics (i.e. frequency and style) of family communication about melanoma are shown in Table 2. Overall, 131 participants (42%) reported that their family had an open style of communication, meaning that family members were supportive and openly shared information. Most FDRs (71%) reported that their families did not have a blocked communication style and the remaining 28% reported that their families had a moderately blocked style of communication (meaning that there was a perceived or actual barrier to information sharing within the family).
Table 2. Family Communication Characteristics.
| Characteristics | N | % |
|---|---|---|
| Open style † | ||
| Open | 131 | 41.9 |
| Closed | 178 | 56.9 |
| Blocked style † | ||
| Blocked | 88 | 28.1 |
| Not blocked | 221 | 70.6 |
| Communication Frequency ‡ | ||
| Average frequency (SD) [range] |
2.2 (0.8) [1–4] |
------ |
| Frequently | 153 | 48.9 |
| Infrequently | 159 | 50.8 |
|
| ||
| Communication Frequency broken down by family member spoken with ‡ | ||
| Mother | ||
| Frequently | 91 | 49.7 |
| Infrequently | 92 | 50.3 |
| Father | ||
| Frequently | 52 | 34.4 |
| Infrequently | 99 | 65.6 |
| Sisters | ||
| Frequently | 95 | 40.6 |
| Infrequently | 139 | 59.4 |
| Brothers | ||
| Frequently | 74 | 33.9 |
| Infrequently | 144 | 66.1 |
| Children | ||
| Frequently | 106 | 44.4 |
| Infrequently | 133 | 55.6 |
| Grandchildren | ||
| Frequently | 15 | 13.2 |
| Infrequently | 99 | 86.8 |
4 missing values (1%).
1 missing value (<1%).
In terms of the amount or frequency with which communication occurred within families, 51% of FDRs reported that they communicated with family members less frequently or not at all about melanoma. Forty-nine percent reported more frequent communications about melanoma.
The amount (frequency) that the FDRs communicated about melanoma risk with each family member type is also shown in Table 2. Mothers were spoken with more frequently than any other family member. Of the 183 FDRs reporting they had a mother, 50% reported communicating moderately or frequently with their mother. 44% of FDRs with a child(ren) reported speaking to them moderately or frequently. 41% of sisters were spoken with frequently while 34% spoke with their brothers or fathers. Finally, few reported talking to their grandchildr(en) moderately or frequently about melanoma risk (13%).
Associations between family functioning and family communication variables
Multivariable logistic regression models are presented for each of the three communication variables in Table 3. Each model was adjusted for age, gender, education, geographic distance to case, and marital status. All family functioning variables assessed in the model were significantly associated with familial open communication style (table 3). Family coping styles were associated with an open style of family communication. For example, families who often engaged in active coping had 2.75 times the odds of having an open style of communication when compared to those who used this coping strategy less frequently (p <0.001). Families who never engaged in denial coping had 2.39 times the odds of having an open style than those who used this strategy more frequently (p <0.001). Similarly, family adaptation and cohesion both had a strong positive association with open communication style. Those who reported that their families were more flexible (i.e. high adaptation) had 3.22 times the odds of reporting a more open style than those reporting less familial adaptation (i.e. less flexibility) (p <0.001). Familial norms regarding tanning and familial norms around the seriousness of melanoma were also significantly associated with open communication styles. Those FDRs whose families felt that melanoma was more serious had 3.66 times the odds of reporting an open style of communication within their family than those who felt that melanoma was a less serious concern (p= 0.002). The familial tanning norm scale score was negatively associated with an open family communication style. For example, individuals reporting positive familial beliefs around tanning had 0.50 times the odds of openly communicating with their family than those who had negative beliefs (p= 0.02). None of the family functioning characteristics were significantly associated with a blocked style of family communication (Table 3).
Table 3. Odds ratios for family communication characteristics: comparing (1) Open to closed (2) Blocked to unblocked and (3) High vs. low frequency.†.
| (1) Open Communication Style |
(2) Blocked Communication Style |
(3) Communication Frequency | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Family Functioning Characteristics |
OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p |
| Active coping | |||||||||
| Rarely | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| Often | 2.75 | (1.69, 4.45) | <0.001 | 0.96 | (0.58, 1.60) | 0.96 | 2.04 | (1.27, 3.28) | 0.003 |
| Denial coping | |||||||||
| Sometimes | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| Never | 2.39 | (1.47, 3.86) | <0.001 | 0.77 | (0.46, 1.28) | 0.32 | 1.23 | (0.77, 1.97) | 0.38 |
| Adaptation | |||||||||
| Less | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| More | 3.22 | (1.91, 5.42) | <0.001 | 0.84 | (0.50, 1.43) | 0.53 | 1.87 | (1.15, 3.05) | 0.01 |
| Cohesion | |||||||||
| Low | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| High | 0.23 | (1.37, 3.62) | 0.001 | 1.17 | (0.69, 1.95) | 0.56 | 1.84 | (1.14, 2.97) | 0.01 |
| Seriousness norms | |||||||||
| Not serious | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| Serious | 3.66 | (1.60, 8.37) | 0.002 | 0.79 | (0.39, 1.59) | 0.50 | 1.46 | (0.73, 2.94) | 0.29 |
| Tanning norms | |||||||||
| Negative | 1.00 | --- | --- | 1.00 | --- | --- | 1.00 | --- | --- |
| Positive | 0.50 | (0.28, 0.91) | 0.02 | 1.15 | (0.63, 2.10) | 0.64 | 1.23 | (0.70, 2.16) | 0.47 |
Adjusted for: age, gender, education, geographic distance to case, gender, and marital status
An active family coping style, family adaptation, and cohesion were all positively associated with the frequency of communication about melanoma risk. For example, those families who often used active coping strategies had 2.04 times the odds of having frequent communication than those used these strategies less frequently (p= 0.003).
Similarly, the odds of having more frequent communication were 1.84 times higher (in families that were more cohesive than those that are less (p= 0.01). Similarly, the odds of having more frequent communication within the family about melanoma risk were 1.87 times higher in more flexible families (i.e. highly adaptive) when compared to less flexible ones (p= 0.01).
DISCUSSION
The main objective of this study was to use the family systems model to examine the relationship between family functioning characteristics and family communication. Because communication is multi-dimensional, we examined both communication style and communication frequency as our main outcome variables. The overall communication frequency with relatives were consistent though slightly higher than rates reported in another study of cancer risk communication in first-degree-relatives of breast cancer survivors [19]. Rates of communication in our study were lower than those found in studies of genetic test communication in high risk families [35, 36]. This is not surprising given the fact that genetic test disclosure provides a cue to communication while general cancer risk communication is likely to have different communication cues, barriers, and motivators.
Generally, communication occurred more frequently with mothers, sisters, and children and less frequently with fathers, brothers and grandchildren. These findings are consistent with those in the literature around breast cancer genetic risk and test disclosure [15, 19, 35, 37] {Demarco}. However, in diseases that don’t have a strong gender predominance such as hereditary non-polyposis colon cancer, dissemination of genetic test information was similar in men and women [15, 38]. It is unclear why female relatives were spoken with more frequently in the case of melanoma. It may be due to the fact that that our sample was largely composed of women (64%) and they may be more likely to communicate with their female family members than with male family members. It may also be that melanoma risk communication is a different communication event than disseminating a genetic test result. Further research is needed into the content of these discussions to determine if different types of information are discussed with different relatives.
There were several interesting findings with respect to the association between family characteristics and family communication. First, all family organizational variables (i.e. family coping, adaptation, and cohesion) and familial health beliefs were associated with an open style of communication. Those individuals reporting more active styles of coping and higher levels of adaptation and cohesion were more likely to have open communication about melanoma within their family. Denial coping styles and familial positive beliefs about suntanning were both negatively associated with an open style of family communication. It is possible that characteristics of families such as coping or familial health beliefs are amenable to intervention to improve communication outcomes. In addition to being more amenable to intervention, they may also illuminate pathways through which families communicate about health information. Future research is necessary to examine the most effective way to appropriately utilize these existing structures and belief systems to improve communication.
By illuminating the relationship between family characteristics and family communication styles, we also have defined a model for examining changes in family functioning following a hereditary disease diagnosis. Most of the literature around health communication within families posits that communication within families about health will result in improved health for families. However, there are a few studies that have shown that communication about genetic test results within the family can negatively alter families by increasing cancer related distress and anxiety [39, 40]. The insight gained from this study on how to operationalize the family systems framework illustrate how structures within families may affect how and whether risk information is disseminated. Findings also provids a catalyst for future research to identify structures, beliefs, and coping mechanisms within the family that could be affected by information dissemination. Future research could use this framework to identify properties within a family that may increase the negative impact of communicating about familial cancer risk. For example, in a less cohesive family, encouraging a proband to discuss their results within families may be more difficult or negatively impact familial relationships. Using the family systems framework may help in illuminating families in need of alternative methods for disseminating health information.
In contrast to the associations with open communication style and frequency, none of the family characteristics were associated with a blocked communication style. This raises three important points. First, it provides evidence that style of communication is a multi-faceted concept which is more complicated than simply thinking of a continuum with open and closed communication styles as the extreme. Second, it suggests that there may be situations in which a family might be characterized by more optimal functioning and still have communication factors that are perceived to be suboptimal (i.e. blocked). We can hypothesize that families with more blocked communication styles use different methods of interacting with each other (i.e. nonverbal communication, activities, using a single family member to communicate information with others) that still ensure that the family is highly functional. Third, there may be issues with the measure itself. For example, the mean for the blocked communication style scale was 1.21. Thus, most people were not reporting high levels of blocked communication in their family, perhaps because those with more highly blocked communication would not volunteer for a family intervention study. Future research into how people define blocked communication as well as future measurement development is necessary to test some of these hypotheses.
Study Limitations
Families are complex entities to examine, and there are several limitations inherent in any study of families and in this study in particular. First, this study is a cross-sectional design so we are unable to determine causality. Thus, whether or not family cohesion, coping, adaptation, or health norms are the cause or the effect of certain types of familial communication is unable to be determined with this type of design. Furthermore, these variables are quite interrelated, thus the only likely method of teasing apart these variables is to examine them in an experimental setting. The second limitation is with how communication style is operationalized. The purpose of the questions pertaining to communication style is to determine a general type of communication style in a family. These questions don’t account for different styles of communication between different individuals within the study. While this may be a limitation, the main purpose of this study is to examine family as a system or organization and not simply as a collection of individuals or dyadic relationships. Thus, this measurement schema is necessary to achieve our overall research aims. However, it may be difficult for people to provide a summary ‘communication style’ for their family. Since this is a novel measure of communication style, it would have been preferable to conduct cognitive interviewing with a pilot sample in order to determine the utility of these questions.
A third limitation is the fact that we were unable to control for the severity or extent of the FDR’s family history of melanoma. The severity or extent of a family’s experience with melanoma could affect the way in which they communicate. Families with multiple melanoma cases or who had experienced a death from melanoma may communicate very differently than those with only one family member affected. Future research is needed to determine how these factors may affect communication patterns within the family. Another limitation involves the fact that families that were recruited to the study may have higher levels of cohesion and communication than a more unselected sample of melanoma families, making it difficult to generalize these findings to the wider population. Additionally, this population had high levels of educational attainment and income and thus results may not generalize to families with lower socioeconomic status in general. One final limitation of the study is the fact
In summary, this study has illuminated two important points. First, it has illustrated the interplay between familial characteristics and family communication. Namely, that for open communication style and communication frequency there are several family-level variables that were associated with communication outcomes. Second, these findings highlight the fact that communication is a multi-faceted and complex concept. Simply measuring frequency or style may not capture the actual communication tendencies within a family. Examining only one of these facets may provide only a crude snapshot of the actual communication patterns occurring within families.
Acknowledgements
This work was supported by NCI Grant CA10743004 and Biobehavioral Cancer Prevention and Control Training Grant R25 CA092408 (JNH). Julie N Harris is a Robert Wood Johnson Foundation Health & Society Scholar at the University of California in San Francisco and Berkeley, CA. We would also like to thank all those families who participated in the SunTalk study.
Footnotes
IRB approval:
This study and all human subjects research in this study were approved by the Fred Hutchinson Cancer Research Center’s Institutional Review Board; Seattle, WA.
Conflict of Interest:
None of the authors of this manuscript have any conflicts of interest to report.
REFERENCES
- 1.DudokdeWit A, Tibben A, Frets P, Meijers-Heijboer E, Devilee P, Klijn J, Oosterwijk J, Niermeijer M. BRCA1 in the family: A case description of the psychological implications. American Journal of Human Genetics. 1997;61(1):120–128. doi: 10.1002/(sici)1096-8628(19970711)71:1<63::aid-ajmg12>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 2.Emery J, Kumar S, Smith H. Patient understanding of genetic principles and their expectations of genetic services within the NHS: A qualitative study. Community Genetics. 1998;1:78–83. doi: 10.1159/000016141. [DOI] [PubMed] [Google Scholar]
- 3.Koehly LM, Peterson SK, Watts BG, Kempf KK, Vernon SW, Gritz ER. A social network analysis of communication about hereditary nonpolyposis colorectal cancer genetic testing and family functioning. Cancer Epidemiol Biomarkers Prev. 2003;12(4):304–13. [PubMed] [Google Scholar]
- 4.Mellon S, Berry-Bobovski L, Gold R, Levin N, Tainsky M. Communication and Decision-Making about seeking inherited cancer risk information: findings from female survivor-relative focus groups. Psycho-oncology. 2006;15:193–208. doi: 10.1002/pon.935. [DOI] [PubMed] [Google Scholar]
- 5.DiLorenzo T, Schnur J, Montgomery G, Erblich J, Winkel G, Bovbjerg D. A model of disease-specific worry in heritable disease: the influence of family history, perceived risk, and worry about other illnesses. Journal of Behavioral Medicine. 2006;29(1):37–49. doi: 10.1007/s10865-005-9039-y. [DOI] [PubMed] [Google Scholar]
- 6.Erblich J, Bovjberg D, Valdimarsdottir H. Looking Forward and Back: Distress among women at familial risk for breast cancer. Annals of Behavioral Medicine. 2000;22(1):53–59. doi: 10.1007/BF02895167. [DOI] [PubMed] [Google Scholar]
- 7.Lerman C, Daly M, Sands C, Balshem A, Lustbader E, Heggan T, Goldstein L, James J, Engstrom P. Mammography adherence and psychological distress among women at risk for breast cancer. Journal of the National Cancer Institute. 1993;85:1074–1080. doi: 10.1093/jnci/85.13.1074. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y, Valdimarsdottir H, Bovbjerg D. Family histories of breast cancer, coping styles, and psychological adjustment. Journal of Behavioral Medicine. 2003;26(3):225–243. doi: 10.1023/a:1023460520645. [DOI] [PubMed] [Google Scholar]
- 9.Knoppers BM. Genetic information and the family: are we our brother’s keeper? Trends Biotechnol. 2002;20(2):85–6. doi: 10.1016/s0167-7799(01)01879-0. [DOI] [PubMed] [Google Scholar]
- 10.Stafford L. Communication Competencies and sociocultural priorities of middle childhood. In: Vangelista A, editor. Handbook of Family Communication. Lawrence Erlbaum Associates; Mahwah, NJ: 2004. pp. 311–332. [Google Scholar]
- 11.Olson D. Circumplex model of marital and family systems. Journal of Family Therapy. 2000;22:144–167. [Google Scholar]
- 12.Friedman LC, Webb JA, Everett TE. Psychosocial and Medical Predictors of Colorectal Cancer Screening Among Low-Income Medical Outpatients. Journal of Cancer Education. 2004;19(3):180–186. doi: 10.1207/s15430154jce1903_14. [DOI] [PubMed] [Google Scholar]
- 13.McCaul KD, Branstetter AD, Schroeder DM, Glasgow RE. What Is the Relationship Between Breast Cancer Risk and Mammography Screening? A Meta-Analytic Review. [Article] Health Psychology. 1996;15:423–429. doi: 10.1037//0278-6133.15.6.423. [DOI] [PubMed] [Google Scholar]
- 14.Peterson S. The Role of the Family in Genetic Testing: Theoretical Perspectives, Current Knowledge, and Future Directions. Health Education and Behavior. 2005;32:627–638. doi: 10.1177/1090198105278751. [DOI] [PubMed] [Google Scholar]
- 15.Wilson BJ, Forrest K, van Teijlingen ER, McKee L, Haites N, Matthews E, Simpson SA. Family Communication about Genetic Risk: The Little That Is Known. Community Genetics. 2004;7(1):15–24. doi: 10.1159/000080300. [DOI] [PubMed] [Google Scholar]
- 16.Hay J, Ostroff J, Martin A, Serle N, Soma S, Mujumdar U, Berwick M. Skin Cancer Risk Discussions in Melanoma-Affected Families. Journal of Cancer Education. 2005;20:240–246. doi: 10.1207/s15430154jce2004_13. [DOI] [PubMed] [Google Scholar]
- 17.Pho K, Geller A, Schroy P. Lack of communication about familial colorectal cancer risk associated with colorectal adenomas (United States) Cancer Causes and Control. 2000;11(6):543–546. doi: 10.1023/a:1008932417421. [DOI] [PubMed] [Google Scholar]
- 18.Schroy P, Lal S, Wilson S, Heeren T, Farraye F. Deficiencies in knowledge and familial risk communication among colorectal adenoma patients. Journal of Clinical Gastroenterology. 2005;39(4):298–302. doi: 10.1097/01.mcg.0000155129.31208.0d. [DOI] [PubMed] [Google Scholar]
- 19.Bowen D, Bourcier E, Press N, Lewis F, Burke W. Effects of individual and family functioning on interest in genetic testing. Community Genetics. 2004;7(1):25–32. doi: 10.1159/000080301. [DOI] [PubMed] [Google Scholar]
- 20.Hay J, Shuk E, Brady M, Berwick M, Ostroff J, Halpern A. Family Communication after Melanoma Diagnosis. Archives of Dermatology. 2008;144(4):553–554. doi: 10.1001/archderm.144.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kenen R, Arden-Jones A, Eeles R. We are talking but are they listening? Communicating patterns in families with a history of breast/ovarian cancer (HBOC) Psycho-oncology. 2004;13:335–345. doi: 10.1002/pon.745. [DOI] [PubMed] [Google Scholar]
- 22.Ross C, Mirowsky J, Goldsteen K. The impact of the family on health: A decade in review. Journal of Marriage and the Family. 1990;52:1059–1078. [Google Scholar]
- 23.van Oostrom I, Meijers-Heijboer H, Duivenvoorden H, Brocker-Vfriends A, Van Asperen C, sijmons R, Seyaneve C, Van Gool A, Klijn J, Tibben A. Comparison of individuals opting for BRCA1/2 or HNPCC genetic susceptibility testing with regard to coping, illness perceptions, illness experiences, family system characteristics and hereditary cancer distress. Patient Education and Counseling. 2007;65:58–68. doi: 10.1016/j.pec.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 24.van Oostrom IV, Meijers-Heijboer H, Duivenvoorden HJ, Brocker-Vriends AH, van Asperen CJ, Sijmons RH, Seynaeve C, Van Gool AR, Klijn JG, Riedijk SR, van Dooren S, Tibben A. A prospective study of the impact of genetic susceptibility testing for BRCA1/2 or HNPCC on family relationships. Psychooncology. 2006 doi: 10.1002/pon.1062. [DOI] [PubMed] [Google Scholar]
- 25.Sobel S, Cowan D. Impact of genetic testing for Huntington disease and the family system. American Journal of Medical Genetics. 2000;90(1):49–59. doi: 10.1002/(sici)1096-8628(20000103)90:1<49::aid-ajmg10>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 26.Sinicrope P, Vernon S, Diamond P, Patterson C, Kelder S, Rabe K, Peterson G. Development and preliminary validation of the cancer family impact scale for colorectal cancer. Genetic Testing. 2009;12(1):161–170. doi: 10.1089/gte.2007.0077. [DOI] [PubMed] [Google Scholar]
- 27.Bowen D, Hay J, Mayer J, Kuniyuki A, Meischke H, Harris JN, Asgari M, Shovellor J, Press N, Burke W. Recruiting melanoma families into a cancer prevention research project. Cancer Epidemiology Biomarkers and Prevention. under review. [Google Scholar]
- 28.DeVellis RF. Scale Development: Theory and Applications. SAGE Publications; Newbury Park, CA: 1991. Guidelines in Scale Development; pp. 51–90. [Google Scholar]
- 29.Dunteman GH. Principal Components Analysis. In: S.P. Inc., editor. Quantitative Applications in the Social Sciences. Sage Publications; Newbury Park, CA: 1989. [Google Scholar]
- 30.Carver CS. You want to measure coping but your protocol’s too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4:91–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 31.Olson DH, Tiesel JW. FACES II update: linear scoring and interpretation. In: Olson, McCubbin HI, Barnes H, Larsen A, Muxen M, Wilson M, editors. Family Inventories: Inventories Used in A National Survey of Families Across the Family Life Cycle. 2nd Revised Edition ed. University of Minnesota; St. Paul, MN: 1992. pp. 12–20. D.H. 1992. [Google Scholar]; Olson D, et al., editors. Family Inventories: Inventories used in a national survey of families across the life cycle. University of Minneosta; St. Paul, MN: 1992. FACES II update: linear scoring and interpretation; pp. 12–20. [Google Scholar]
- 32.Olson D. Empirical approaches to family assessment. Journal of Family Therapy. 1999 [Google Scholar]
- 33.Olson D. Three dimensional (3-D) Circumplex Model & revised scoring of FACES. Family Process. 1991;30:74–79. doi: 10.1111/j.1545-5300.1991.00074.x. [DOI] [PubMed] [Google Scholar]
- 34.Inc S. SPSS for Windows, Rel. 15.0.1. Chicago: 2006. [Google Scholar]
- 35.Hughes C, Lerman C, Schwartz M, Peshkin B, Wenzel L, Narod S, Corio C, Tercyak K, Hanna D, Isaacs C. All in the Family: Evaluation of the Process and Content of sisters’ communication about BRCA1 and BRCA2 genetic test results. American Journal of Medical Genetics. 2002;107:143–150. doi: 10.1002/ajmg.10110. [DOI] [PubMed] [Google Scholar]
- 36.Wagner Costalas J, Itzen M, Malick J, Babb J, Bove B, Godwin A, Daly M. Communication of BRCA1 and BRCA2 results to at-risk relatives: a cancer risk assessment program’s experience. American Journal of Medical Genetics C Seminars in Medical Genetics. 2003;119C(1):11–18. doi: 10.1002/ajmg.c.10003. [DOI] [PubMed] [Google Scholar]
- 37.DeMarco TA, McKinnon WC. Life after BRCA1/2 testing: family communication and support issues. Breast Disease. 2007;27:127–136. doi: 10.3233/bd-2007-27108. 27 2006. [DOI] [PubMed] [Google Scholar]
- 38.Peterson SK, Watts BG, Koehly LM, Vernon SW, Baile WF, Kohlmann WK, Gritz ER. How families communicate about HNPCC genetic testing: findings from a qualitative study. Am J Med Genet C Semin Med Genet. 2003;119(1):78–86. doi: 10.1002/ajmg.c.10010. [DOI] [PubMed] [Google Scholar]
- 39.van Oostrom I, Meijers-Heijboer H, Duivenvoorden HJ, Brocker-Vriends AH, van Asperen CJ, Sijmons RH, Seynaeve C, Van Gool AR, Klijn JG, Tibben A. Prognostic factors for hereditary cancer distress six months after BRCA1/2 or HNPCC genetic susceptibility testing. Eur J Cancer. 2007;43(1):71–7. doi: 10.1016/j.ejca.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 40.van Oostrom I, Meijers-Heijboer H, Duivenvoorden HJ, Brocker-Vriends AH, van Asperen CJ, Sijmons RH, Seynaeve C, van Gool AR, Klijn JG, Tibben A. Family system characteristics and psychological adjustment to cancer susceptibility genetic testing: a prospective study. Clin Genet. 2007;71(1):35–42. doi: 10.1111/j.1399-0004.2007.00731.x. [DOI] [PubMed] [Google Scholar]