Abstract
Background and aims
It was reported that high coffee consumption was related to decreased diabetes risk. The aim of this study is to examine the association between coffee consumption and the incidence of type 2 diabetes in persons with normal glucose tolerance in a population with a high incidence and prevalence of diabetes.
Methods and results
In a prospective cohort study, information about daily coffee consumption was collected at the baseline examination (1989-1992) in a population-based sample of American Indian men and women 45-74 years of age. Participants with normal glucose tolerance (N=1141) at the baseline examination were followed for an average of 7.6 years. The incidence of diabetes was compared across the categories of daily coffee consumption. The hazard ratios of diabetes related to coffee consumption were calculated using Cox proportional hazards models, adjusted for potential confounders.
Levels of coffee consumption were positively related to levels of current smoking and inversely related to body mass index, waist circumference, female gender, and hypertension. Compared to those who did not drink coffee, participants who drank 12 or more cups of coffee daily had 67% less risk of developing diabetes during the follow-up (hazard ratio: 0.33, 95% confidence interval: 0.13, 0.81).
Conclusion
In this population, a high level of coffee consumption was associated with a reduced risk of deterioration of glucose metabolism over an average 7.6 years of follow-up. More work is needed to understand whether there is a plausible biological mechanism for this observation.
Keywords: coffee, Diabetes Mellitus, type 2, Indians, North American
Introduction
Diabetes is a huge burden for the US health care system [1], affecting about 23.6 million people or 7.8% of the population in United States. Estimated diabetes costs in the United States in 2007 were $174 billion. The association between coffee consumption and risk of some chronic diseases including cardiovascular disease and cancer has been reported[2,3]. Several recent studies reported that coffee consumption is inversely related to the risk of type 2 diabetes [4-12]. Different components in coffee such as antioxidants, phenol chlorogenic acid, magnesium, and caffeine have been proposed to be involved in the process of developing type 2 diabetes[13]. More than 50% of Americans drink coffee, and the average per capita intake is about 2 cups per day [5]. Therefore, a protective effect of coffee could have widespread impact on the population health. Previous studies about coffee consumption and type 2 diabetes were conducted in different populations across European and US. However, data are sparse in populations with a high incidence of diabetes or in individuals with documented normal glucose tolerance.
This report presents analyses from the Strong Heart Study, a population based study of American Indians who are known to have high prevalence (range from 40% to 70% among three study centers) and incidence of diabetes (20% developed incident diabetes in a 4-year period) [14,15]. The aim of the study was to determine whether there is an association between coffee consumption and type 2 diabetes in this population.
Methods
Study population and the assessment of diabetes
The Strong Heart Study is a cohort study of cardiovascular disease in 13 American Indian tribes/communities in southwestern Oklahoma, central Arizona, and North and South Dakota. Participants (n = 4,549) aged 45 to 74 years underwent a baseline examination from 1989 to 1992. The design, survey methods, and laboratory techniques were described previously [16-18]. The analysis group for this study was participants with normal glucose tolerance at the baseline examination (1989-92), defined as fasting plasma glucose < 6.1 mmol/l (110mg/dl) and 2-h plasma post-glucose load < 7.8 mmol/l (140mg/dl) and those not on any oral hypoglycemic drugs or insulin. There were a total of 1141 men and women with normal glucose tolerance at the baseline examination who made up the “at risk” cohort for this analysis. Cases of incident diabetes were identified at the second (August 1993 – October 1995) and the third follow-up examinations (January 1998 – August 1999). Participants were followed for an average of 7.6 years by the end of the third follow-up examination. Diabetes was defined according to the 1998 Provisional World Health Organization Report [19] as use of an oral hypoglycemic agent or insulin, or fasting glucose ≥ 7.0 mmol/l (126mg/dl) or post-challenge glucose ≥11.1 mmol/l (200mg/dl) (75–g oral glucose tolerance test). Indian Health Service Institutional Review Boards, Institutional Review Boards of the participating institutions, and the participating tribes approved the study. Informed consent was obtained from all participants.
Measurements of coffee consumption
At the baseline examination of the Strong Heart Study, a personal interview was conducted with each participant, which included a question related to coffee consumption. The question was, “How many cups/glasses of caffeinated beverages (i.e., hot or iced coffee, tea, cocoa or chocolate milk) do you drink per day?” Although the question included beverages other than coffee, the information from the 24-h dietary recall at the second follow-up examination indicated that the proportion of participants who consumed tea, cocoa, or chocolate milk is very low in this population (2.5 % (83/3354)). Thus, the results of this question reflect primarily consumption of coffee (97.5%).
Assessments of medical history, anthropometry, and lifestyle
During the Strong Heart Study, personal interview information was collected on demographic factors, medical history, medication use, and personal health habits (physical activity, smoking, and alcohol consumption). Information on leisure-time and occupation-related physical activities was collected using a physical activity questionnaire that has been validated in Pima Indians and in other populations. An estimate of the individual's self-reported physical activity level was averaged over the past year and expressed as hours per week[20]. Past smoking was defined as smoking at least 100 cigarettes in entire lifetime, smoking cigarettes regularly in the past, and not smoking currently. Current smoking was defined as smoking at least 100 cigarettes in entire lifetime, smoking cigarettes regularly, and smoking currently. Past alcohol user was defined as consuming at least 12 drinks of any kind of alcoholic beverage in entire lifetime and the last drink at least 1 year ago. Current alcohol user was defined as consuming at least 12 drinks of any kind of alcoholic beverage in entire lifetime and drinking currently. A physical examination was conducted in the morning, which included collecting fasting blood samples for laboratory tests and a 75-g oral glucose tolerance test. Glucose was measured by enzymatic methods using a Hitachi chemistry analyzer (Boehringer Mannheim Diagnostics, Indianapolis, IN)[21]. Anthropometric measurements were performed with participants in light clothing and without shoes and included weight, height, and waist and hip circumferences. Sitting blood pressure (first and fifth Korotkoff sounds) was measured three times consecutively after five minutes rest using a standard mercury sphygmomanometer (WA Baum Co) [22]. The average of the second and third systolic and diastolic blood pressure measurements was used in the analysis. The information about medication use was ascertained by interview and confirmed by review of the medications brought to the examination or by medical record review.
Statistical methods
Means and percentages of baseline characteristics were calculated by categories of coffee consumption (0, 1-2, 3-4, 5-7, 8-11, ≥ 12 cups/glasses per day) collected at the baseline examination. Baseline characteristics included age, body mass index, waist circumference, occupational and leisure time physical activity, fasting glucose, gender, smoking, alcohol use, hypertension (yes/no), and parental history of diabetes (yes/no). The cut-points of coffee consumption categories were initially defined by quartiles. Then, those who did not consume any coffee were separated as the reference group (roughly 10%). Those who drank 12 cups/glasses per day or more comprised 8.1% of the participants and became another group. General linear models were used to test the trend of continuous variables such as age, BMI, waist circumference, fasting glucose, and occupational and leisure time physical activity according to categories of coffee consumption. Mantel-Haenszel Chi-square test was used to test the trends of categorical variables such as proportions of smokers, alcohol users, hypertensives, females, and those with a parental history of diabetes according to the categories of coffee consumption. A two-tailed p <0.05 was considered to be statistically significant.
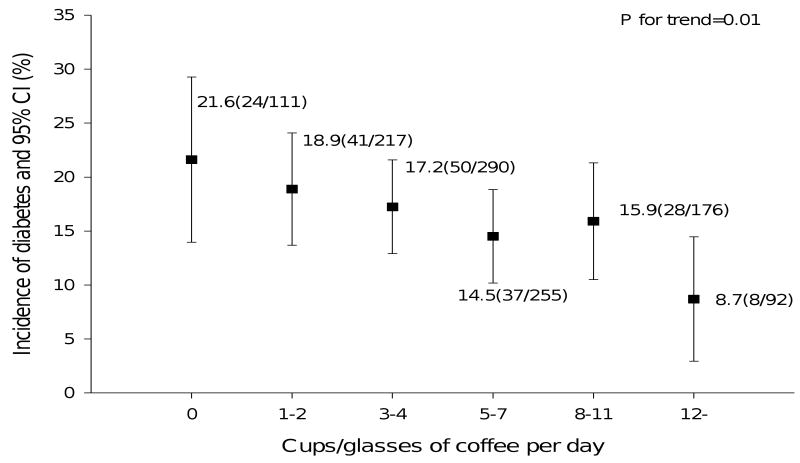
Cumulative incidence of diabetes was calculated and presented in a graph by the six categories of daily coffee consumption. Cumulative incidence was calculated by dividing the number of newly diagnosed diabetic participants by the third exam by the total number of participants at risk at baseline exam. Mantel-Haenszel Chi-square test was used to test the trends of incidence by the six categories of daily coffee consumption.
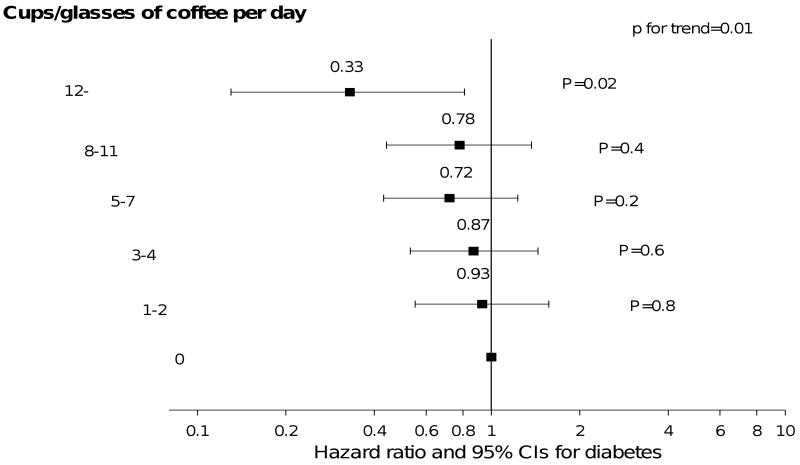
Cox proportional hazard models were used for multivariable analyses. The date of incident diabetes was estimated as the mid-point between the exam with the negative results and the exam with positive results. For example, for a participant who was diabetes-free at baseline examination and who became diabetic at the second examination, the time to diabetes is estimated as the midpoint of the interval between the two examinations. The covariates in the model included age, gender, smoking, alcohol use, parental history of diabetes, physical activity, and body mass index. All analyses were performed using SAS (Version 9.1, 2002, SAS Institute Inc, Cary, NC). Coffee consumption was also put in the model as continuous variable to examine linear associations between coffee consumption and risk of type 2 diabetes.
Results
As shown in Table 1, 111 participants reported no current consumption of coffee at the baseline examination. Ninety-two participants reported drinking more than 12 cups of coffee daily. The average coffee consumption at baseline was four cups, with the first and third quartile as two and six cups, respectively. There was a significant, consistent increase in the proportion of current smokers as the category of coffee consumption increased. Coffee intake was inversely related to body mass index, waist circumference, being female, past smoking, and hypertension. There was no significant association in this univariate analysis between categories of coffee consumption and age, physical activity, fasting glucose, or alcohol use.
Table 1.
Baseline characteristics by coffee drinking habits in normal glucose tolerance participants: The Strong Heart Study
| Characteristics | Coffee drinking status (cups/glasses per day) | P for trend | |||||
|---|---|---|---|---|---|---|---|
| 0 (n=111, 9.7%) | 1-2 (n=217, 19%) | 3-4 (n=290,25.4 %) | 5-7 (n=255, 22.3%) | 8-11 (n=176, 15.4%) | 12- (n =92, 8.1%) | ||
| Age, yrs (Mean, SD) | 53.8 (8.1) | 55.1(8.0) | 55.9(8.1) | 55.1(7.6) | 54.1(7.4) | 52.6(6.5) | 0.1 |
| BMI, kg/m2 (Mean, SD) | 29.3 (5.0) | 28.9(5.5) | 28.6(5.3) | 28.0(5.2) | 28.5(5.6) | 27.2(5.6) | 0.004 |
| Waist circumference, cm (Mean, SD) | 99.7 (12.6) | 99.8(14.0) | 99.5(13.1) | 97.2(12.4) | 99.0(13.9) | 94.2(13.8) | 0.002 |
| Physical activity, hrs/week (Median, Q1,Q3) | 18.9(4.6,37.6) | 16.4(3.7,31.8) | 14.1(2.6, 33.3) | 18.8(5.7,36.5) | 17.2(6.2,33.4) | 18.1(4.6,37.5) | 0.3 |
| Fasting glucose, mg/dl (Median, Q1,Q3) | 99(93,104) | 98(91,103) | 98(92,103) | 96(92,102) | 99(93, 104) | 96(92, 102) | 0.2 |
| Gender (% female) | 63.1 | 59.9 | 51.4 | 47.8 | 47.2 | 48.9 | 0.0008 |
| Smoking (%) | |||||||
| Past | 27.9 | 33.2 | 33.1 | 25.1 | 26.7 | 17.4 | 0.01 |
| Current | 30.6 | 24.9 | 40.0 | 53.7 | 60.8 | 77.2 | 0.0001 |
| Alcohol use (%) | |||||||
| Past | 36.0 | 38.9 | 38.3 | 37.0 | 43.2 | 40.2 | 0.4 |
| Current | 45.1 | 45.8 | 48.6 | 49.6 | 52.3 | 50.0 | 0.2 |
| Hypertension (%) | 37.8 | 27.4 | 31.1 | 19.8 | 21.7 | 12.1 | 0.0001 |
| Parental history of diabetes | 36.9 | 30.9 | 35.2 | 32.6 | 43.2 | 42.4 | 0.05 |
The crude cumulative incidence and 95% confidence intervals (CI) for diabetes (figure 1) decreased with increasing coffee consumption. For coffee consumption categories 0, 1-2, 3-4, 5-7, 8-11, and 12- cups/glasses per day, the corresponding numbers are 21.6% (14%, 29.2%), 18.9% (13.7%, 24.1%), 17.2% (12.9%, 21.6%), 14.5% (10.2%, 18.8%), 15.9% (10.5%, 21.3%), and 8.7% (2.9%, 14.5%) respectively (p for trend = 0.01). At the highest level of coffee consumption (≥ 12 cups/glasses per day), the hazard ratio for diabetes was 0.33 (95% CI: 0.13, 0.81); no other level of consumption was significantly related to diabetes risk (Figure 2). The hazard ratios and 95% CI for categories as 1-2, 3-4, 5-7, and 8-11 (cups/glasses per day) are 0.93 (0.55, 1.57), 0.87 (0.53, 1.44), 0.72 (0.43, 1.23), and 0.78 (0.44, 1.37) respectively. The follow-up person-years for each coffee consumption category are as follows (from the lowest to the highest level): 714, 1374, 1873, 1676, 1144, and 623. When coffee consumption entered the model as a continuous variable, the result was consistent with the model including coffee consumption as categorical variables (p=0.01, hazard ratio and 95% confidence interval as 0.95 (0.91, 0.99)). We did the same analyses in participants with impaired fasting glucose and impaired glucose tolerance. In these participants, the association between coffee consumption and diabetes incidence was minimal.
Figure 1.
Crude incidence of diabetes by daily coffee consumption categories
Figure 2.
Hazard ratios (and 95% CIs) for incident diabetes by daily coffee consumption categories adjusted for age, gender, smoking, alcohol use, family history of diabetes, physical activity, body mass index.
Discussion
In the current study, coffee consumption at baseline of 12 or more cups of coffee per day was independently associated with a significant 67% reduction in incidence of diabetes over the following 7.6 years compared to those who were not drinking coffee.
We found an association between high coffee consumption and decreased diabetes risk in a population with high prevalence and incidence of type 2 diabetes. Although such an association was not found in Pima Indians[23], differences in the categories of coffee consumption (the highest category was 3 cups of coffee or more per day), adjusted lifestyle risk factor (the report from Pima Indian only adjusted for age, sex, and BMI), geographic location of the tribe, and tribal customs related to coffee drinking may contribute to the difference of the study results. By only including the people with normal glucose tolerance, a bias from coffee consumption behavior changes caused by diagnosis of preclinical diabetes has been avoided [5,13]. Our study adds to the existing literature concerning the association between coffee consumption and the risk of type 2 diabetes[4-8,11,12,24].
Although our study was not designed to assess by which biological mechanisms coffee was involved in reducing diabetes risk, there are several possible mechanisms. First, coffee contains compounds that are antioxidants[25,26], which may be related to the risk of diabetes because the oxidative stress may be a pathogenic mechanism linking insulin resistance with dysfunction of both beta cells and endothelium [27]. Second, phenol chlorogenic acid and its degradation products (quinides) in coffee contribute to inhibition of glucose absorption in the intestine [28,29], reducing hepatic glucose output through inhibition of glucose-6-phosphatase[30]. Third, caffeine may also contribute to the inverse association between coffee and diabetes through increasing of basal energy expenditure[31], stimulating fat oxidation and mobilization of glycogen in muscle [32], and weight loss[33]. Caffeine has also been related to acute decrease of insulin sensitivity [34], although prolonged use of caffeine may result in tolerance for such acute effect [35,36]. Finally, other components in coffee such as magnesium have been associated with a lower risk for type 2 diabetes [37,38]. We did not collect other dietary information at the baseline exam. When Exam 2 dietary data were analyzed to explore relations of dietary intake according to coffee consumption of baseline exam, we found that participants who drank 12 or more cups of coffee per day had the highest magnesium intake among all groups. Energy intake, polyunsaturated-to-saturated fat intake ratio, and fiber intake were not significantly different among coffee groups. Further studies on the biological mechanisms relating consumption are needed. Several characteristics of coffee drinkers, such as BMI, physical activity, and smoking are known to be associated with diabetes incidence; these, however, were included as covariates in all analyses.
The strength of this study is the longitudinal design, the systematic diagnosis of diabetes by using blood glucose values measured following a glucose-tolerance test instead of self-reported diabetes, and the availability of information on a wide range of potential confounders.
The limitations of this study include the lack of availability of dietary data on the participants. Given that an independent, inverse association of diabetes risk and coffee consumption was observed only for the highest consumption category (≥ 12 cups/glasses per day), it may be that high coffee consumption is a marker for other factors such as energy intake, meal patterns, and food choices not measured here that are related to diabetes risk. This study was conducted in a single ethnic group; although this population has been shown to be representative of many populations in the US with high levels of obesity and diabetes, analyses in other populations must be done. In addition, analyses were limited to individuals with normal glucose tolerance.
In summary, the consumption of 12 or more cups of coffee per day was associated with a significant, 67% reduction in the incidence of diabetes compared to those who did not drink coffee. Further studies are needed to determine whether this association is causal or a result of unmeasured confounders. The potential effects of high level of coffee consumption on risk of type 2 diabetes may be important but should be considered in light of putative health effects of coffee, such as potential detrimental effects on blood pressure and sleep quality [39,40].
Acknowledgments
This study was supported by cooperative agreement grants U01-HL41642, U01-HL41652, UL01-HL41654, U01-HL65520, and U01-HL65521 from the National Heart, Lung, and Blood Institute, Bethesda, MD. The authors acknowledge the assistance and cooperation of the Ak-Chin Tohono O'Odham (Papago)/Pima, Apache, Caddo, Cheyenne River Sioux, Comanche, Delaware, Spirit Lake Sioux, Fort Sill Apache, Gila River Pima Maricopa, Kiowa, Oglala Sioux, Salt River Pima/Maricopa and Wichita Indian communities. It would have been impossible to conduct this study without their support. The authors also want to thank the Indian Health Service hospitals and clinics at each center, the directors of the Strong Heart Study clinics, the field coordinators, and their staffs. In addition, we thank Holly A. Anderson for editing the manuscript. The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Sources of support for research: This study was supported by cooperative agreement grants U01-HL41642, U01-HL41652, UL01-HL41654, U01-HL65520, and U01-HL65521 from the National Heart, Lung, and Blood Institute, Bethesda, MD, USA.
Footnotes
Disclaimer: The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC. National Diabetes Fact Sheet. 2007 In. [Google Scholar]
- 2.van Dam RM. Coffee consumption and risk of type 2 diabetes, cardiovascular diseases, and cancer. Appl Physiol Nutr Metab. 2008;33:1269–1283. doi: 10.1139/H08-120. [DOI] [PubMed] [Google Scholar]
- 3.Sofi F, Conti AA, Gori AM, Eliana Luisi ML, Casini A, Abbate R, Gensini GF. Coffee consumption and risk of coronary heart disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2007;17:209–223. doi: 10.1016/j.numecd.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Tuomilehto J, Hu G, Bidel S, Lindstrom J, Jousilahti P. Coffee consumption and risk of type 2 diabetes mellitus among middle-aged Finnish men and women. JAMA. 2004;291:1213–1219. doi: 10.1001/jama.291.10.1213. [DOI] [PubMed] [Google Scholar]
- 5.Salazar-Martinez E, Willett WC, Ascherio A, Manson JE, Leitzmann MF, Stampfer MJ, Hu FB. Coffee consumption and risk for type 2 diabetes mellitus. Annals of Internal Medicine. 2004;140:1–8. doi: 10.7326/0003-4819-140-1-200401060-00005. [see comment][summary for patients in Ann Intern Med. 2004 Jan 6; 140(1):I17; PMID: 14706993]. [DOI] [PubMed] [Google Scholar]
- 6.van Dam RM, Feskens EJ. Coffee consumption and risk of type 2 diabetes mellitus. Lancet. 2002;360:1477–1478. doi: 10.1016/S0140-6736(02)11436-X. [see comment] [DOI] [PubMed] [Google Scholar]
- 7.Rosengren A, Dotevall A, Wilhelmsen L, Thelle D, Johansson S. Coffee and incidence of diabetes in Swedish women: a prospective 18-year follow-up study. Journal of Internal Medicine. 2004;255:89–95. doi: 10.1046/j.1365-2796.2003.01260.x. [DOI] [PubMed] [Google Scholar]
- 8.van Dam RM, Willett WC, Manson JE, Hu FB. Coffee, caffeine, and risk of type 2 diabetes: a prospective cohort study in younger and middle-aged U.S. women. Diabetes Care. 2006;29:398–403. doi: 10.2337/diacare.29.02.06.dc05-1512. [DOI] [PubMed] [Google Scholar]
- 9.Carlsson S, Hammar N, Grill V, Kaprio J. Coffee consumption and risk of type 2 diabetes in Finnish twins. International Journal of Epidemiology. 2004;33:616–617. doi: 10.1093/ije/dyh185. [DOI] [PubMed] [Google Scholar]
- 10.Smith B, Wingard DL, Smith TC, Kritz-Silverstein D, Barrett-Connor E. Does coffee consumption reduce the risk of type 2 diabetes in individuals with impaired glucose? Diabetes Care. 2006;29:2385–2390. doi: 10.2337/dc06-1084. [DOI] [PubMed] [Google Scholar]
- 11.Pereira MA, Parker ED, Folsom AR. Coffee consumption and risk of type 2 diabetes mellitus: an 11-year prospective study of 28 812 postmenopausal women. Arch Intern Med. 2006;166:1311–1316. doi: 10.1001/archinte.166.12.1311. [DOI] [PubMed] [Google Scholar]
- 12.Paynter NP, Yeh HC, Voutilainen S, Schmidt MI, Heiss G, Folsom AR, Brancati FL, Kao WH. Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the atherosclerosis risk in communities study. Am J Epidemiol. 2006;164:1075–1084. doi: 10.1093/aje/kwj323. [DOI] [PubMed] [Google Scholar]
- 13.van Dam RM, Hu FB. Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA. 2005;294:97–104. doi: 10.1001/jama.294.1.97. [DOI] [PubMed] [Google Scholar]
- 14.Lee ET, Welty TK, Cowan LD, Wang W, Rhoades DA, Devereux R, Go O, Fabsitz R, Howard BV. Incidence of diabetes in American Indians of three geographic areas: the Strong Heart Study. Diabetes Care. 2002;25:49–54. doi: 10.2337/diacare.25.1.49. [DOI] [PubMed] [Google Scholar]
- 15.Lee ET, Howard BV, Savage PJ, Cowan LD, Fabsitz RR, Oopik AJ, Yeh J, Go O, Robbins DC, Welty TK. Diabetes and impaired glucose tolerance in three American Indian populations aged 45-74 years. The Strong Heart Study Diabetes Care. 1995;18:599–610. doi: 10.2337/diacare.18.5.599. [DOI] [PubMed] [Google Scholar]
- 16.Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, Cucchiara AJ, Savage PJ, Howard BV. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. American Journal of Epidemiology. 1990;132:1141–1155. doi: 10.1093/oxfordjournals.aje.a115757. [DOI] [PubMed] [Google Scholar]
- 17.Howard BV, Welty TK, Fabsitz RR, Cowan LD, Oopik AJ, Le NA, Yeh J, Savage PJ, Lee ET. Risk factors for coronary heart disease in diabetic and nondiabetic Native Americans. The Strong Heart Study. Diabetes. 1992;41(Suppl 2):4–11. doi: 10.2337/diab.41.2.s4. [DOI] [PubMed] [Google Scholar]
- 18.Cowan LD, Go OT, Howard BV, Devereux RB, Pettitt DJ, Fabsitz RR, Lee ET, Welty TK. Parity, postmenopausal estrogen use, and cardiovascular disease risk factors in American Indian women: the Strong Heart Study. Journal of Women's Health. 1997;6:441–449. doi: 10.1089/jwh.1997.6.441. [DOI] [PubMed] [Google Scholar]
- 19.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Medicine. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [see comment] [DOI] [PubMed] [Google Scholar]
- 20.Kriska AM, Sandler RB, Cauley JA, LaPorte RE, Hom DL, Pambianco G. The assessment of historical physical activity and its relation to adult bone parameters. Am J Epidemiol. 1988;127:1053–1063. doi: 10.1093/oxfordjournals.aje.a114881. [DOI] [PubMed] [Google Scholar]
- 21.Cowan LD, Go OT, Howard BV, Devereux RB, Pettitt DJ, Fabsitz RR, Lee ET, Welty TK. Parity, postmenopausal estrogen use, and cardiovascular disease risk factors in American Indian women: the Strong Heart Study. J Womens Health. 1997;6:441–449. doi: 10.1089/jwh.1997.6.441. [DOI] [PubMed] [Google Scholar]
- 22.Howard BV, Lee ET, Yeh JL, Go O, Fabsitz RR, Devereux RB, Welty TK. Hypertension in adult American Indians. The Strong Heart Study. Hypertension. 1996;28:256–264. doi: 10.1161/01.hyp.28.2.256. [DOI] [PubMed] [Google Scholar]
- 23.Saremi A, Tulloch-Reid M, Knowler WC. Coffee consumption and the incidence of type 2 diabetes. Diabetes Care. 2003;26:2211–2212. doi: 10.2337/diacare.26.7.2211. [DOI] [PubMed] [Google Scholar]
- 24.van Dam RM. Coffee and type 2 diabetes: from beans to beta-cells. Nutr Metab Cardiovasc Dis. 2006;16:69–77. doi: 10.1016/j.numecd.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Svilaas A, Sakhi AK, Andersen LF, Svilaas T, Strom EC, Jacobs DR, Jr, Ose L, Blomhoff R. Intakes of antioxidants in coffee, wine, and vegetables are correlated with plasma carotenoids in humans. J Nutr. 2004;134:562–567. doi: 10.1093/jn/134.3.562. [DOI] [PubMed] [Google Scholar]
- 26.Pulido R, Hernandez-Garcia M, Saura-Calixto F. Contribution of beverages to the intake of lipophilic and hydrophilic antioxidants in the Spanish diet. Eur J Clin Nutr. 2003;57:1275–1282. doi: 10.1038/sj.ejcn.1601685. [DOI] [PubMed] [Google Scholar]
- 27.Ceriello A, Motz E. Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol. 2004;24:816–823. doi: 10.1161/01.ATV.0000122852.22604.78. [DOI] [PubMed] [Google Scholar]
- 28.Clifford M. Chlorogenic acids and other cinnamates - nature, occurrence, dietary burden, absorption and metabolism. Journal of the Science of Food and Agriculture. 2000;80:1033–1043. [Google Scholar]
- 29.Johnston KL, Clifford MN, Morgan LM. Coffee acutely modifies gastrointestinal hormone secretion and glucose tolerance in humans: glycemic effects of chlorogenic acid and caffeine. Am J Clin Nutr. 2003;78:728–733. doi: 10.1093/ajcn/78.4.728. [DOI] [PubMed] [Google Scholar]
- 30.Arion WJ, Canfield WK, Ramos FC, Schindler PW, Burger HJ, Hemmerle H, Schubert G, Below P, Herling AW. Chlorogenic acid and hydroxynitrobenzaldehyde: new inhibitors of hepatic glucose 6-phosphatase. Arch Biochem Biophys. 1997;339:315–322. doi: 10.1006/abbi.1996.9874. [DOI] [PubMed] [Google Scholar]
- 31.Astrup A, Toubro S. Thermogenic, metabolic, and cardiovascular responses to ephedrine and caffeine in man. Int J Obes Relat Metab Disord. 1993;17(Suppl 1):S41–43. [PubMed] [Google Scholar]
- 32.Spriet LL, MacLean DA, Dyck DJ, Hultman E, Cederblad G, Graham TE. Caffeine ingestion and muscle metabolism during prolonged exercise in humans. Am J Physiol. 1992;262:E891–898. doi: 10.1152/ajpendo.1992.262.6.E891. [DOI] [PubMed] [Google Scholar]
- 33.Greenberg JA, Axen KV, Schnoll R, Boozer CN. Coffee, tea and diabetes: the role of weight loss and caffeine. International Journal of Obesity. 2005;29:1121–1129. doi: 10.1038/sj.ijo.0802999. [DOI] [PubMed] [Google Scholar]
- 34.Keijzers GB, De Galan BE, Tack CJ, Smits P. Caffeine can decrease insulin sensitivity in humans. Diabetes Care. 2002;25:364–369. doi: 10.2337/diacare.25.2.364. [DOI] [PubMed] [Google Scholar]
- 35.Robertson D, Wade D, Workman R, Woosley RL, Oates JA. Tolerance to the humoral and hemodynamic effects of caffeine in man. J Clin Invest. 1981;67:1111–1117. doi: 10.1172/JCI110124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoshioka K, Kogure A, Yoshida T, Yoshikawa T. Coffee consumption and risk of type 2 diabetes mellitus. Lancet. 2003;361:703. doi: 10.1016/S0140-6736(03)12585-8. [DOI] [PubMed] [Google Scholar]
- 37.Salmeron J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC. Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA. 1997;277:472–477. doi: 10.1001/jama.1997.03540300040031. [DOI] [PubMed] [Google Scholar]
- 38.Meyer KA, Kushi LH, Jacobs DR, Jr, Slavin J, Sellers TA, Folsom AR. Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr. 2000;71:921–930. doi: 10.1093/ajcn/71.4.921. [DOI] [PubMed] [Google Scholar]
- 39.James JE. Critical review of dietary caffeine and blood pressure: a relationship that should be taken more seriously. Psychosom Med. 2004;66:63–71. doi: 10.1097/10.psy.0000107884.78247.f9. [DOI] [PubMed] [Google Scholar]
- 40.Sin CW, Ho JS, Chung JW. Systematic review on the effectiveness of caffeine abstinence on the quality of sleep. J Clin Nurs. 2009;18:13–21. doi: 10.1111/j.1365-2702.2008.02375.x. [DOI] [PubMed] [Google Scholar]