Abstract
Background
The Centers for Disease Control and Prevention (CDC) recently published recommendations for routine, voluntary human immunodeficiency virus (HIV) testing of adults in all healthcare settings, including the emergency department (ED).
Study Objective
The objective of this study was to examine the willingness of ED providers to offer HIV testing, as well as their perceived barriers to implementation of these guidelines.
Methods
Prior to the establishment of a routine HIV testing program in the ED, a 21-item survey was used to assess ED providers’ knowledge, attitudes, and perceived challenges to HIV testing. Six months after program initiation, the identical survey was re-administered to determine if HIV testing program experience altered providers’ perceptions.
Results
There were 108 (74%) of 146 providers who completed both the pre- and post-implementation surveys. While the majority of emergency providers at six months were supportive of an ED-based HIV testing program (59/108 [55%]), only 38% (41/108) were willing to offer the HIV test most or all of the time. At six months, the most frequently cited barriers to offering a test were: inadequate time (67/108 [62%]), inadequate resources (65/108 [60%]), and concerns regarding provision of follow-up care (64/108 [59%]).
Conclusions
After the implementation of a large scale HIV testing program in an ED, the majority of emergency providers were supportive of routine HIV testing. Nevertheless, six months after program initiation, providers were still reluctant to offer the test because of persistent barriers. Further studies are needed to identify feasible implementation strategies that minimize barriers toward routine HIV testing in the ED.
Keywords: HIV/AIDS, Testing, Emergency Department, Emergency Providers
INTRODUCTION
In 2006, the Centers for Disease Control and Prevention (CDC) published recommendations for routine, voluntary human immunodeficiency virus (HIV) testing of persons 13–64 years of age in all healthcare settings, including the emergency department (ED) (1). In settings like the ED, the rapid pace of patient flow, coupled with substantial disease severity, may lead providers to focus preferentially on acute patient care over HIV screening. The successful implementation of any HIV testing program in the ED setting depends upon the willingness and commitment of ED providers to adopt such a program.
In April 2007, the American College of Emergency Physicians (ACEP) responded to the new Center for Disease Control and Prevention (CDC) guidelines with a policy statement suggesting criteria under which EDs would embrace HIV testing. The criteria include requirements that ED-based HIV testing be feasible, practical, and based on local needs. The requirements also require that testing have adequate funding and not interfere with the acute care mission of Emergency Medicine (2). The implementation of an HIV testing program requires the provision of ED resources in addition to those required to meet the acute care mission. A more detailed understanding of emergency provider knowledge, attitudes, perceptions, and barriers towards HIV testing is needed for successful implementation of such a program.
The NAME (NAME) Trial is a National Institutes of Health (NIH)-funded study examining alternative strategies for implementing routine HIV testing in the ED at the HOSPITAL, Boston, Massachusetts. Before and after trial initiation, ED providers were surveyed to examine their attitudes and perceived barriers to HIV testing. The objective was to identify these barriers and then to see if they changed over time. The data collected may help inform further HIV testing programs so that these barriers can be addressed early and long-term, thereby facilitating program success.
MATERIALS AND METHODS
Study Design
The NAME trial is a randomized, prospective clinical trial designed to evaluate alternative approaches to routine HIV testing in the ED. For this study, a survey was distributed to ED healthcare providers before (T0, December 2006) and 6 months after (T1, July 2007) clinical trial initiation. To be eligible for survey inclusion in this analysis, providers had to be full-time ED staff at both time points.
The analysis was focused on ED providers’ knowledge and attitudes towards routine HIV testing, perceived barriers to HIV testing, and independent correlates with supporting routine ED-based HIV testing programs. This study was approved by the institutional Human Subjects Committee, and verbal informed consent was obtained from providers.
Setting
The HOSPITAL ED is a major level-one trauma center with over 56,000 patient visits per year. The ED serves as a tertiary referral center with an estimated HIV seroprevalence of approximately 1% and with a dedicated, on-site HIV outpatient clinic. Prior to the NAME Trial, there were no routine HIV testing efforts in the ED or in the hospital at large.
Selection of Participants
The subjects in this study were ED providers, comprised of Emergency Service Assistants (ESAs, or nursing assistants), Nurses, Physician Assistants (PAs), Residents, and Attending Physicians. Prior to beginning enrollment in the NAME Trial, the ED providers were offered opportunities for formal education and training that covered the standards and goals of the ED-based routine HIV testing program and NAME study protocols; these sessions also addressed anticipated provider concerns regarding HIV testing. The education and training sessions were mandatory for the Emergency Service Assistants and Attending Physicians. The Residents and Physician Assistants participated in a one-hour grand rounds lecture and had the option of attending other education and training sessions. Nurses were offered Continuing Educational Units (CEUs) for their attendance at the sessions. The first education and training session was videotaped and offered online to all providers who could not attend one of the two live sessions.
Providers were informed of their roles and responsibilities with regard to patients enrolled in the NAME Trial. To minimize undue burden on any single provider, testing, consent, and follow-up responsibilities were distributed among the staff. Emergency Service Assistants offered the HIV test, obtained written informed consent, conducted an Oraquick ® ADVANCE ™ Rapid HIV 1/2 Antibody Test (Orasure Technologies, Inc., Bethlehem, PA), and assisted with linkage to care. Residents or PAs delivered the negative test results. For patients with a reactive (preliminary positive) test, the Attending Physicians delivered the positive test results to the patients and at that time obtained consent for confirmatory testing. Upon consent, Nurses then performed venipuncture for laboratory testing.
Methods of Measurement
A 21-item paper survey was distributed to eligible ED providers at baseline, or T0, before trial initiation and mandatory training sessions, and at T1, six months after trial initiation. The surveys were anonymous, but linked between the two time points by an identification number. In the absence of a previously-validated ED provider survey on HIV testing, we developed one based on the literature about providers’ perceived barriers toward HIV testing in the emergency department. The survey covered the following domains: 1) demographics (professional title, gender, race or ethnicity); 2) HIV knowledge; 3) support of HIV testing; and 4) perceived barriers to HIV testing.
HIV Knowledge
Provider HIV knowledge was assessed by asking providers to estimate the HIV prevalence by percentage (%) in the HOSPITAL patient population, in the Boston, Massachusetts population, and in the United States (US) general population. Their answers were selected from three categories: <0.5%, 0.5–5%, and >5%. The percentage of providers who answered correctly (i.e., 0.5–5%) is reported for each category. Providers were also asked to estimate the cost of a rapid HIV test, given the choices of $1, $15, $50, $100, and $500. The percentage of providers who answered correctly (i.e., $15) is reported.
Support of HIV Testing
Provider attitudes toward HIV testing were assessed by querying respondents on whether or not they favored routine testing in general, or routine testing specifically in the ED. Their willingness to offer a test was also assessed. Providers were asked to select who they thought should be offered an HIV test from the following options: injection drug users, men who have sex with men, all pregnant women, all sexually active men and women, all patients in hospitals with any level of HIV prevalence, or all US citizens. Their answers were dichotomized into favoring routine testing (all US citizens) or risk-based targeted testing (injection drug users). Using a 5-item Likert scale (strongly agree to strongly disagree), providers were asked if a routine HIV testing program in the ED setting is a good idea. The responses “strongly agree” and “agree” were used as indicators supporting a testing program in the ED. ED providers’ willingness to offer the test was assessed by asking them if they would offer an HIV test to someone in the ED if results were available within 20 minutes. This question could be answered “rarely,” “occasionally,” “most of the time,” or “all of the time.” A provider who chose “most of the time” or “all of the time” was considered willing to test.
Perceived Barriers to HIV Testing
Providers’ perceived barriers to offering HIV tests were assessed by eliciting their reasons for not offering an HIV test in the ED setting by choosing one of the following: it is not a currently recommended guideline; HIV disease prevalence is too low; it is too expensive; there are inadequate resources; there is not enough time; it is not part of provider responsibilities; there are concerns with follow-up; it is uncomfortable delivering the test results; or there is a lack of understanding of the legal implications of HIV testing.
Primary Data Analysis
Analyses were performed using SAS (Statistical Analysis System) Version 9 (SAS Institute, Cary, NC) and were limited to the 108 providers who responded to surveys at both T0 and T1. Preliminary univariate chi-square analysis (categorical variables) and non-parametric Wilcoxon tests (continuous variables) were used to examine the barriers most likely to affect attitudes towards routine HIV testing in the ED. Repeated measures logistic regression models using Generalizing Estimating Equations (GEE) were run to detect associations favoring testing. Multivariate analysis controlled for provider characteristics that might influence favoring testing, including gender, age, role, and HIV knowledge. We also analyzed the differences when providers were categorized as physicians or physician assistants (Attending Physicians, Residents, and PAs) versus staff (ESAs and Nurses).
RESULTS
Characteristics of Study Subjects
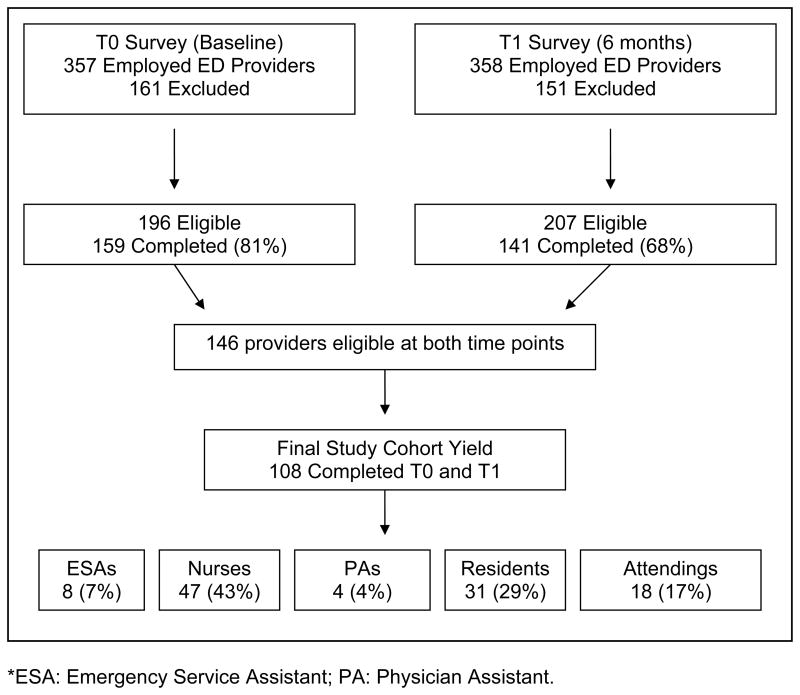
At T0 (baseline), 357 emergency providers were employed in the HOSPITAL ED, and 161 were excluded based on their part-time or per-diem status. Among the 196 eligible full-time ED providers, 159 (81%) completed the survey prior to NAME Trial initiation (Figure 1). At T1 (6 months), 358 emergency providers were employed and 151 were excluded for the same reasons. Among the 207 eligible providers, 141 (68%) completed the survey 6 months after program initiation. The intersection of respondents between T0 and T1 yielded a final study cohort of 108/146 (74% of all eligible providers). Among the 108 providers in the final study cohort, 8 (7%) were ESAs, 47 (43%) were Nurses, 4 (4%) were PAs, 31 (29%) were Residents, and 18 (17%) were Attending Physicians (Figure 1). Among the 108 responders, the mean (±SD) age was 37.6 ± 9.8 years; 46 (43%) were male, and 88 (81%) were Caucasian (Table 1). Within provider type, the response rate was 80% (8/10) for ESAs, 76% (47/62) for Nurses, 100% (4/4) for PAs, 63% (31/49) for Residents, and 86% (18/21) for Attending Physicians.
Figure 1.
Enrollment and eligibility of study cohort at T0 (baseline) and T1 (6 months). *ED: Emergency Department, ESA: Emergency Service Assistant (i.e. Nursing Assistant), PA: Physician Assistant.
Table 1.
Demographic Characteristics of ED Providers in the Final Cohort (N=108)*
| ESA (N=8) | Nurse (N=47) | PA/Resident (N=35) | Attending (N=18) | Overall (N=108) | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Age (Years) | |||||
| Mean (±SD) | 24.1 (3.1) | 44.7 (8.0) | 29.9 (2.6) | 40.5 (7.7) | 37.6 (9.8) |
| Male | 3 (37) | 15 (32) | 14 (40) | 14 (78) | 46 (43) |
| Race | |||||
| 7 (87) | 44 (94) | 22 (63) | 15 (83) | 88 (81) | |
| Caucasian | 1 (13) | 3 (6) | 13 (37) | 3 (17) | 20 (19) |
| Non-White | |||||
SD: Standard Deviation ESA: Emergency Service Assistant; PA: Physician Assistant
HIV Knowledge and Attitudes about Testing
Table 2 summarizes the survey results at T0 and T1 on providers’ knowledge about HIV infection and their attitudes toward HIV testing. The table stratifies results by provider category and time point. Overall, the majority of providers estimated the correct HIV prevalence of 0.5–5% at HOSPITAL (T0= 77%, T1= 77%), in Boston (T0= 66%, T1= 73%), and in the US (T0= 64%, T1= 64%). The majority of ESAs, Residents, and Attending Physicians were consistent in their answers for each area (HOSPITAL, Boston, and US) and at both time points. However, the nurses tended to overestimate the prevalence of HIV infection in Boston, leading to a lower percentage of correct prevalence estimates (T0= 34%, T1= 45%) as well as in the US (T0= 47%, T1= 29%). Six months after study initiation, more than half of all providers (53%, N=55) knew the correct cost of a rapid HIV test.
Table 2.
HIV Knowledge and Testing Attitudes*
| ESA (N=8) | Nurse (N=47) | PA/Resident (N=35) | Attending (N=18) | Overall (N=108) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Knowledge: HIV Prevalence (0.5–5%) | ||||||||||
| At HOSPITAL | 7 (87) | 7 (87) | 26 (60) | 26 (67) | 31 (89) | 31 (89) | 15 (88) | 13 (72) | 79 (77) | 77 (77) |
| in Boston | 5 (71) | 7 (87) | 12 (34) | 17 (45) | 29 (88) | 32 (91) | 15 (83) | 16 (89) | 61 (66) | 72 (73) |
| in US | 5 (71) | 7 (87) | 15 (47) | 11 (29) | 25 (76) | 30 (86) | 12 (71) | 15 (83) | 57 (64) | 63 (64) |
| Rapid Test Cost ($15) | 5 (62) | 6 (75) | 16 (36) | 22 (51) | 11 (31) | 17 (49) | 11 (65) | 10 (59) | 43 (41) | 55 (53) |
| Attitudes: Favor Routine Testing (Yes) | ||||||||||
| in General | 8 (100) | 8 (100) | 36 (77) | 38 (81) | 32 (91) | 31 (89) | 17 (94) | 17 (94) | 93 (86) | 94 (87) |
| in the ED | 7 (87) | 6 (75) | 22 (47) | 22 (47) | 23 (66) | 21 (60) | 9 (50) | 10 (56) | 61 (56) | 59 (55) |
| Willingness to Offer Test (Most/All of Time) | 6 (75) | 6 (75) | 20 (42) | 20 (42) | 10 (29) | 11 (31) | 4 (22) | 4 (22) | 40 (37) | 41 (38) |
ESA: Emergency Service Assistant; PA: Physician Assistant
Overall, providers were in favor of general routine, targeted testing at both time points (T0= 86%, T1= 87%), and 55% of emergency providers favored or strongly favored ED-based routine HIV testing at six months. The frequency of responses in favor of routine testing was largely unchanged at the two time points. Despite support for routine HIV testing and ED-based routine testing, only 38% (at T1) of providers overall indicated their willingness to offer an HIV test themselves. Support for routine ED-based testing was similar at the two time points among the physician/PA group (physician/PA, T0=32/53, 60%; T1=31/53, 58%) as well as the staff group (staff, T0=29/55, 53%; T1=28/53, 51%). However, at both time points the physician/PA group was significantly less willing to offer an HIV test than the staff group (physician/PA group, T0=14/53, 26% and T1=15/53, 28% vs. staff group at both T0 and T1=26/55, 47%, p<0.05).
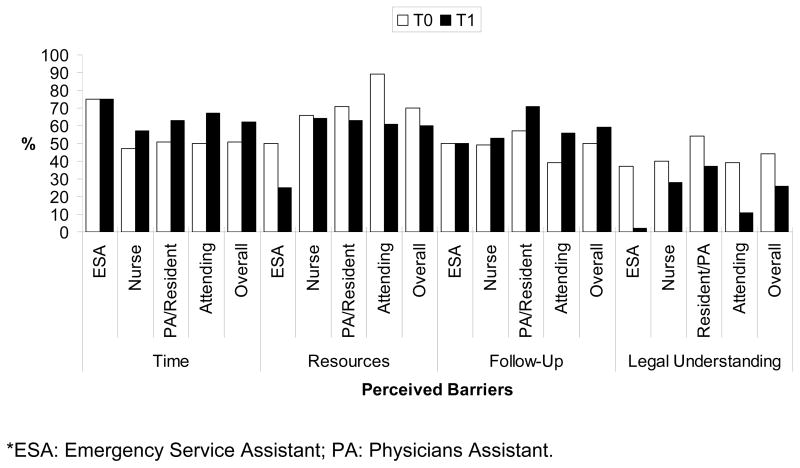
Reported Barriers to HIV Testing
The reported frequency of barriers to HIV testing, stratified by provider role and time point, is provided in Figure 2. The most frequently cited barriers to ED-based HIV testing by all providers at baseline were: inadequate resources, 76/108 (70%); time constraints, 55/108 (51%); and concerns regarding provision of follow-up care, 54/108 (50%). After the first six months of the program, the barriers reported were similar: inadequate resources, 65/108 (60%); time constraints, 67/108 (62%); and concerns regarding provision of follow-up care 64/108 (59%). Despite the success of the testing program, two barriers were reported more frequently at T1 compared to T0: inadequate time (T0= 51%, T1= 62%) and concern regarding provision of follow-up (T0= 50%, T1= 59%). In contrast, there was a decrease in the frequency of reported concerns regarding inadequate resources (T0=70%, T1=60%) and lack of legal understanding (T0= 44%, T1= 26%, p<0.05). When results were compared between physician/PA and staff groups, the perceived barrier data were reported at similar frequencies.
Figure 2.
Major barriers to HIV testing perceived by ED providers at T0 (baseline) and T1 (6 months). *ESA: Emergency Service Assistant, PA: Physician Assistant.
Independent Correlates Favoring HIV Testing
Results of the multivariate analysis of independent correlates favoring HIV testing in the ED are summarized in Table 3. Female providers were more likely than males to favor ED-based routine HIV testing (OR 2.5, 95% CI: 1.2 – 5.1). There was no significant correlation between the provider role (physician/PA vs. staff group) and favoring routine ED-based HIV testing. Providers who felt they had adequate time were 2.9 times (OR 2.9, 95% CI: 1.5 – 5.3) more likely to support routine ED-based testing than those who did not. Providers with a clear legal understanding of the HIV testing process had 2.9 times increased support over those who did not (OR 2.9, 95% CI: 1.5 – 5.5).
Table 3.
Independent Correlates with Favoring HIV Testing in the ED*
| Predictor | Adjusted Odds Ratio (95% C.I.) | p-value |
|---|---|---|
| Gender | 0.02 | |
| Female | 2.5 (1.2,5.1) | |
| Male | 1.0 | |
| Age (years) | 0.38 | |
| 20–29 | 0.95 (0.28, 3.2) | |
| 30–39 | 0.51 (0.15, 1.7) | |
| 40–49 | 0.45 (0.15, 1.4) | |
| ≥50 | 1.0 | |
| Provider Role | 0.24 | |
| Physicians/PAs | 1.7 (0.68, 4.3) | |
| Staff (RNs and ESAs) | 1.0 | |
| Estimate of HIV prevalence | 0.69 | |
| Incorrect | 1.2 (0.45, 3.3) | |
| Correct | 1.0 | |
| Survey Time Point | 0.32 | |
| T0 (baseline) | 1.3 (0.77, 2.2) | |
| T1 (at 6 months) | 1.0 | |
| Provider felt did not have adequate time | 0.001 | |
| Agree | 2.9 (1.5, 5.3) | |
| Disagree | 1.0 | |
| Provider felt had legal understanding | 0.002 | |
| Agree | 2.9 (1.5, 5.5) | |
| Disagree | 1.0 | |
DISCUSSION
This study reports results from a survey of providers in an urban emergency department before and after the implementation of an HIV testing program. The results suggest that emergency providers generally favor the implementation of a large scale HIV testing program in accordance with the CDC recommendations, but due to several major barriers, they are still generally unwilling to offer the test (1). While some of the perceived barriers to testing were improved over time, other barriers were reported at an increased frequency. Elimination of these barriers will likely facilitate greater support for testing. These findings have important implications for those designing and implementing ED-based HIV testing programs, especially for programs relying on emergency department personnel to carry them out.
ED healthcare provider support has been previously shown for the implementation of certain preventive programs, including health promotion, domestic violence, and alcohol screening, in the ED setting. Like HIV testing, these programs were considered successful despite some commonly faced programmatic barriers (3–12). Frequently reported barriers in other prevention studies parallel some of the concerns noted by the ED providers participating in this study, including time constraints, personal discomfort, privacy issues, need for resources and protocols, legal concerns, lack of knowledge, and lack of space (4, 5, 7–12). Equipped with prior experience from these prevention-intervention studies, ED-based editorials regarding routine HIV testing in the ED have voiced appropriate concerns. Although Emergency Medicine professional societies like the American College of Emergency Physicians and Society for Academic Emergency Medicine are generally supportive of public health initiatives, the message is clear that there is a need to proceed with caution as these programs begin to emerge (13–16). Despite provider concerns, in recent years numerous EDs in the US have successfully implemented some form of HIV screening (14, 17–20).
HIV screening programs are important since several studies have shown that patients who frequently seek care in EDs may not have access to a primary medical provider (3, 13, 14). Among the most powerful reasons to implement the CDC guidelines in the ED setting is to identify HIV-infected patients who present to the healthcare system only through the ED. One study in South Carolina noted that 41% of patients given a new diagnosis of HIV infection might have been identified sooner had routine ED-based testing been in place (21).
ED-based testing may be difficult to implement because of provider-perceived barriers. This study found that, for all providers, the most frequently cited barriers to an ED-based HIV testing persisted after six months experience with a testing program. These concerns were perceived even in the context of a funded clinical trial in which resources were available, pathways for linkage to care were provided, long-term education and training sessions were offered, and stringent protocols were implemented after approval from the institution’s Human Subjects Committee. The education and training received by ED providers through the program is one possible explanation for their generally positive attitude, especially as it relates to the legal implications of HIV testing in Massachusetts. These training sessions may have addressed a knowledge deficit about HIV that subsequently led to changes in their earlier attitudes. The fact that these barriers exist across all personnel suggests that the manifestations of an ED-based testing program are palpable by all healthcare providers.
Results of this study demonstrate that an HIV testing program, like other preventive programs, cannot be easily layered onto current ED practices. A commonly reported barrier, concern for follow-up, is one of critical importance that deserves special mention. Patients newly identified as HIV-infected require not only linkage to medical care but also support from social work during the critical period of transition. The impact of a routine HIV testing program will be realized only if patients who are identified with HIV infection reach appropriate and comprehensive HIV outpatient services in a timely fashion (22, 23).
Among all of the factors examined in this study, gender and provider-perceived barriers were identified as the most influential independent correlates of support for HIV testing in the ED. Age, provider role, knowledge about HIV, and time of survey did not correlate with support for HIV testing. Addressing these barriers long-term with the providers through education and training sessions, newsletters, and an informational website may help testing programs become successful.
Limitations
The results of this study should be interpreted in the context of its limitations. First, ED provider samples assembled for this study may be biased in that those who were willing to complete the survey may have been more likely to be supportive of an HIV testing program than those who declined. Thus, results of this study may under-represent the true level of skepticism. Although the response rate was high, analyses stratified by provider type generally were based on modest sample sizes. The analysis was performed using cross-sectional data from a survey instrument that has not been validated. Further, despite reporting an improvement in knowledge about HIV among providers, it was not an initial intent of the study to directly measure the effects of the educational and training efforts of the program on providers. Also, while this study was distributed at baseline and at 6 months after program implementation began, it cannot address how perceptions might have changed with even more testing experience (e.g., for 1 year). Further studies will need to longitudinally follow the impact of an HIV testing program on providers’ perceptions.
CONCLUSION
ED healthcare providers are generally supportive of the recent CDC guidelines recommending routine HIV testing in the ED setting (1). Results of this study emphasize the importance of understanding provider barriers to HIV testing, as these perceived barriers highly correlate with providers’ support of testing programs. These results have significant implications for EDs trying to implement routine testing efforts, and suggest the need to collect data specific to individual institutions, since barriers may be different in different locations.
Acknowledgments
Grants: This research was funded by the National Institute of Mental Health (R01 MH0735445, R01 MH65869) and the Doris Duke Charitable Foundation (Clinical Scientist Development Award to Rochelle P. Walensky, MD, MPH) ClinicalTrials.Gov: #NCT00502944
Footnotes
Prior Presentation(s):
- Arbelaez C, Losina E, Wright E, et al., National Society for Academic Emergency Medicine, Washington D.C., USA, June, 2008
- Arbelaez C, Losina E, Wright E, et al., New England Society for Academic Emergency Medicine Regional Meeting, Shrewsbury, MA, April, 2008
- Arbelaez C, Losina E, Wright E, et al., American College of Emergency Physicians Research Forum, Seattle, WA., October, 2007
Trial Number: Clinical Trials.Gov NCT00502944
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Branson BM, Handsfield HH, Lampe MA, et al. MMWR. RR-14. Vol. 55. 2006. Sep 22, Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings; p. 1.p. 17. [PubMed] [Google Scholar]
- 2.American College of Emergency Physicians. HIV testing and screening in the emergency department. Ann Emerg Med. 2007 Aug;50(2):209. doi: 10.1016/j.annemergmed.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 3.Scott BC. Emergency departments: An important component of public health. J Natl Med Assoc. 1995 Mar;87(3):181–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Larkin GL, Hyman KB, Mathias SR, et al. Routine screening for intimate partner violence in the emergency department: Importance of patient and provider factors. Ann Emerg Med. 1999 Jun;33(6):669–75. doi: 10.1016/s0196-0644(99)70196-4. [DOI] [PubMed] [Google Scholar]
- 5.Ellis JM. Barriers to effective screening for domestic violence by registered nurses in the emergency department. Crit Care Nurs Q. 1999 May;22(1):27–41. doi: 10.1097/00002727-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Williams JM, Chinnis AC, Gutman D. Health promotion practices of emergency physicians. Am J Emerg Med. 2000 Jan;18(1):17–21. doi: 10.1016/s0735-6757(00)90041-x. [DOI] [PubMed] [Google Scholar]
- 7.Davis RE, Harsh KE. Confronting barriers to routine screening for domestic violence. J Prof Nurs. 2001 Nov-Dec;17(6):313–20. doi: 10.1053/jpnu.2001.28181. [DOI] [PubMed] [Google Scholar]
- 8.Hungerford DW, Williams JM, Furbee PM, et al. Feasibility of screening and intervention for alcohol problems among young adults in the ED. Am J Emerg Med. 2003 Jan;21(1):14–22. doi: 10.1053/ajem.2003.50004. [DOI] [PubMed] [Google Scholar]
- 9.Nordqvist C, Johansson K, Lindqvist K, et al. Attitude changes among emergency department triage staff after conducting routine alcohol screening. Addict Behav. 2006 Feb;31(2):191–202. doi: 10.1016/j.addbeh.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 10.Yonaka L, Yoder MK, Darrow JB, et al. Barriers to screening for domestic violence in the emergency department. J Contin Educ Nurs. 2007 Jan-Feb;38(1):37–45. doi: 10.3928/00220124-20070101-08. [DOI] [PubMed] [Google Scholar]
- 11.McCann TV, Clark E, McConnachie S, et al. Deliberate self-harm: Emergency department nurses’ attitudes, triage and care intentions. J Clin Nurs. 2007 Sep;16(9):1704–11. doi: 10.1111/j.1365-2702.2006.01555.x. [DOI] [PubMed] [Google Scholar]
- 12.Furniss K, McCaffrey M, Parnell V, et al. Nurses and barriers to screening for intimate partner violence. MCN Am J Matern Child Nurs. 2007 Jul-Aug;32(4):238–43. doi: 10.1097/01.NMC.0000281964.45905.89. [DOI] [PubMed] [Google Scholar]
- 13.Borg KT. To test or not to test? HIV, emergency departments, and the new Centers for Disease Control and Prevention guidelines. Ann Emerg Med. 2007 May;49(5):573–4. doi: 10.1016/j.annemergmed.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Rothman RE, Lyons MS, Haukoos JS. Uncovering HIV infection in the emergency department: A broader perspective. Acad Emerg Med. 2007 Jul;14(7):653–7. doi: 10.1197/j.aem.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Peckler B. Emergency Department HIV testing: Sounds good, but...? Acad Emerg Med. 2003 Dec;10(12):1415, 6. doi: 10.1111/j.1553-2712.2003.tb00023.x. author reply 1416–7. [DOI] [PubMed] [Google Scholar]
- 16.Irvin CB, Flagel BT, Fox JM. The emergency department is not the ideal place for routine HIV testing. Ann Emerg Med. 2007 May;49(5):722. doi: 10.1016/j.annemergmed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Brown J, Shesser R, Simon G. Establishing an ED HIV screening program: Lessons from the front lines. Acad Emerg Med. 2007 Jul;14(7):658–61. doi: 10.1197/j.aem.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 18.Brown J, Shesser R, Simon G, et al. Routine HIV screening in the emergency department using the new US Centers for Disease Control and Prevention guidelines: Results from a high-prevalence area. J Acquir Immune Defic Syndr. 2007 Dec 1;46(4):395–401. doi: 10.1097/qai.0b013e3181582d82. [DOI] [PubMed] [Google Scholar]
- 19.Lyss SB, Branson BM, Kroc KA, et al. Detecting unsuspected HIV infection with a rapid whole-blood HIV test in an urban emergency department. J Acquir Immune Defic Syndr. 2007 Apr 1;44(4):435–42. doi: 10.1097/QAI.0b013e31802f83d0. [DOI] [PubMed] [Google Scholar]
- 20.Mehta SD, Hall J, Lyss SB, et al. Adult and pediatric emergency department sexually transmitted disease and HIV screening: Programmatic overview and outcomes. Acad Emerg Med. 2007 Mar;14(3):250–8. doi: 10.1197/j.aem.2006.10.106. [DOI] [PubMed] [Google Scholar]
- 21.CDC. Missed opportunities for earlier diagnosis of HIV infection—South Carolina, 1997–2005. MMWR. 2006 December 1;55(47):1269–72. [PubMed] [Google Scholar]
- 22.Paltiel AD, Walensky RP, Schackman BR, et al. Expanded HIV screening in the United States: Effect on clinical outcomes, HIV transmission, and costs. Ann Intern Med. 2006 Dec 5;145(11):797–806. doi: 10.7326/0003-4819-145-11-200612050-00004. [DOI] [PubMed] [Google Scholar]
- 23.Walensky RP, Weinstein MC, Smith HE, et al. Optimal allocation of testing dollars: The example of HIV counseling, testing, and referral. Med Decis Making. 2005 May-Jun;25(3):321–9. doi: 10.1177/0272989X05276955. [DOI] [PubMed] [Google Scholar]