Abstract
Background
Assessment of peak oxygen uptake (VO2) is recommended in the evaluation of patients with borderline pulmonary function as VO2 is the strongest independent predictor of postoperative pulmonary complications. However, the measurement of VO2 requires expensive equipment not available in many medical facilities. The shuttle walking test (SWT) has been proposed to be used as a screening tool prior to performing a cardiopulmonary exercise test. Although an association exists between SWT distance and VO2, only one small study directly measured VO2 during the SWT.
Objectives
The aim of this study was to further validate the VO2-SWT association by directly measuring VO2 during SWT in a larger cohort of patients with stable chronic obstructive pulmonary disease (COPD).
Methods
Fifty stable COPD patients with mild/severe disease were studied. Each patient performed an SWT while wearing a validated portable metabolic monitor.
Results
Mean VO2 (ml/kg/min) measured after each finalized minute of the SWT was (95% confidence interval): 6 (5–7), 9 (8–10), 11 (10–12), 13 (11–14), 15 (14–16), 18 (16–20) and 21 (18–26) for minutes 1–7, respectively. Patients that completed the British Thoracic Society-recommended 25 shuttles (5 min or 250 m) in the SWT had a mean VO2 of 15 (14–16). The positive predictive value for walking 25 shuttles (predicting a VO2 of ≥15ml/kg/min) was 90% and the negative predictive value was 90%.
Conclusions
Our findings validate the association between VO2 and SWT distance and facilitate the interpretation of the test in general practice, particularly when deciding the candidacy of a patient for surgical resection.
Key Words: Activities of daily living, Chronic obstructive pulmonary disease, Emphysema, Exercise test, Lung cancer resection, Shuttle walking test
Introduction
Exercise capacity expressed as peak oxygen uptake (VO2) has been reported to be the variable most predictive of postoperative pulmonary complications following lung cancer resection in patients with chronic obstructive pulmonary disease (COPD) [1,2,3,4]. However, the measurement of peak VO2 requires expensive equipment not available in many centers. Therefore, a simple screening test was needed to better define the patients with an exercise capacity associated with a higher risk for postoperative pulmonary complications (defined as VO2 <15 ml/kg/min), requiring a maximal cardiopulmonary test with VO2 measure. Attending to that need, the British Thoracic Society (BTS) recommended the shuttle walking test (SWT) [5] as a screening method to be used before doing a formal cardiopulmonary exercise test in the evaluation of patients suggested for lung resection [5]. The SWT is a maximal, progressive paced test validated externally, which is widely used in Europe but less so in America [6,7,8]. The BTS algorithm proposes 25 shuttles (5 min or 250 m) as the distance associated with a VO2 of 15 ml/kg/min (exercise capacity related with an average operative risk of surgical complications). Although an association exists between SWT distance and VO2[9,10,11,12], only one small study (10 patients) directly measured VO2 during the SWT [7], and to date no study reported the range of VO2 associated with each minute walked during the test, which could be of clinical importance for test interpretation.
In addition, we aimed to validate the VO2-SWT association by directly measuring VO2 during the SWT in a larger group of stable COPD patients and to provide a range of VO2 associated with each minute walked during the test.
Patients and Methods
This study was approved by the Institutional Review Board and all patients signed an informed consent. Stable patients attending a COPD clinic for a regular scheduled visit were invited to participate. Exclusion criteria were: the presence of acute respiratory symptoms, the use of antibiotics or oral prednisone in the previous 2 weeks or physical impediment to walk.
Shuttle Walking Test
The 10-meter course was established in the corridor of the clinic and the speed of walking was dictated by a timed signalplayed on a compact disc player. Within the first 2 min, thesubjects were advised to increase or decrease their speed ifrequired, but no further encouragement was given. The test endedif the subject was unable to continue (due to breathlessnessor any other reason) or was unable to maintain the required pace, as previously published [6]. The test was performed 30 min after bronchodilators (2 metered-dose inhaler actuations of albuterol plus ipratropium delivered through a spacer).
Although a practice walk is the ideal situation, it proved to be tooexhausting for some subjects and not suitable for this study done in a clinical practice setting. The protocol included that if subjectsfailed to understand the test appropriately in the first 2 min, it was stopped and restarted after a 20-min rest period.
Portable Metabolic Monitoring
The patients were connected to a validated MedGraphics VO2000 portable metabolic testing system (MedGraphics, St. Paul, Minn., USA) via a MedGraphics proprietary neoprene mask. Heart rate was assessed using a Polar heart rate monitor (Polar, Port Washington, N.Y., USA). This system utilizes a MedGraphics proprietary pneumotachometer as volume transducer, a galvanic fuel cell O2 analyzer and an infrared CO2 analyzer. Data were transmitted between each breath interval and stored in breath rate packets of 6 breaths. The system ‘warm-up’ was completed prior to each walk test as recommended by the manufacturer to permit self-calibration. Data collected during the walk tests included VO2, carbon dioxide production (VCO2), heart rate, respiratory rate and tidal volume. The VO2000 weighs 740 g and was worn with a harness during the tests. ‘Real-time’ data acquisition was done through a telemetric MedGraphics system.
Statistical Analysis
All data are expressed as means ± SD or with 95% confidence interval, as indicated. Pearson correlation was used to determine the association between the continuous variables.
The variables distance walked and VO2 were converted into binary variables to perform risk analysis using the cutoff proposed in the BTS guideline: distance walked ≥25 shuttles (250 m) versus lower, and VO2 ≥15 ml/kg/min versus lower. Fisher's exact test and the χ2 test were used for the analysis of discrete variables, and risk analysis (odds ratios) was performed from the 2 × 2 tables.
To determine the association between VO2 >15 ml/kg/min and other baseline variables, we used univariate logistic regression analyses. If a variable had a p value <0.1 in univariate analyses, we included it in the multiple logistic regression model to predict the odds of having a VO2 >15 ml/kg/min.
Receiver-operating characteristic (ROC) analysis was used to determine the true-positive rate (sensitivity) and the false-positive rate (1 – specificity) for different cutoff values of the SWT for identifying high-risk patients (VO2 >15 ml/kg/min).
SPSS (version 13; SPSS, Chicago, Ill., USA) [13] was employed for the above analyses.
Results
Subject Characteristics
We studied 50 patients (24 males) with mild/severe COPD according to the guidelines of the Global Initiative for Chronic Obstructive Lung Disease [14]: age (mean + SD) 60 + 12 years, body mass index 28 + 6, forced expiratory volume in the first second (FEV1) 60.5 + 23.1% of predicted and forced vital capacity (FVC) 77.7 + 17.9% of predicted. Dyspnea, measured by the Medical Research Council (MRC) dyspnea score (range 1–5), was 2.8 + 1.0.
Shuttle Walking Test
All patients followed the guidelines of the test without difficulty, and there was no need to repeat any walk. None of the patients reported the weight of the equipment as a significant factor to affect their walking capacity. The physiologic parameters obtained during the SWT are summarized in table 1.
Table 1.
SWT parameters measured by the metabolic monitor (VO2000)
| Maximal heart rate, % of predicted | 69 (65-72) |
| Borg scale (peak) | |
| Dyspnea | 4.4 (3.8-5.1) |
| Fatigue | 4.1 (3.4-4.7) |
| VO2 (peak) | |
| ml/kg/min | 17.4 (15.4-19.2) |
| % of predicted | 80 (69-90) |
| VCO2 (peak), liters/min | 1.1 (1.0-1.3) |
| VE/VCO2max | 34.92 (32.5-37.2) |
| VE/MVVmax | 0.61 (0.55-0.67) |
| Respiratory quotient (max.) | 0.83 (0.8-0.89) |
| Shuttle distance walked, m | 317 (276-359) |
Results are expressed as means (95% confidence intervals). VE/MVV = minute ventilation/maximal voluntary ventilation; max. = maximal.
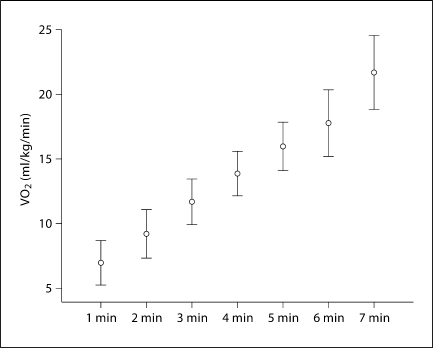
VO2 increased linearly with every level of the SWT (fig. 1). Table 2 lists the mean VO2 (95% confidence interval) measured at the end of every SWT level (1 min each).
Fig. 1.
Mean VO2 associated with each level of the SWT. 95% confidence intervals are also included.
Table 2.
VO2 attained with a completed SWT level (means and 95% confidence intervals)
| SWT levels (each level lasts 1 min) | Distance m | VO2 ml/kg/min |
|---|---|---|
| Level 1 | 30 | 6.28 (5.5-7.0) |
| Level 2 | 70 | 9.08 (8.1-10.0) |
| Level 3 | 120 | 11.1 (10.1-12.2) |
| Level 4 | 180 | 12.9 (11.4-14.1) |
| Level 5 | 250 | 14.8 (13.5-16.1) |
| Level 6 | 330 | 17.7 (15.8-19.6) |
| Level 7 | 420 | 21.4 (18.3-24.5) |
The analysis of the binary outcomes VO2 >15 ml/kg/min and 25 shuttles showed a very significant association, as expected. The agreement analysis was very high (κ = 0.77). Interestingly, the positive predictive value for walking 25 shuttles (predicting a VO2 ≥15 ml/kg/min) was 90% and the negative predictive value was 90%. The odds (95% confidence interval) of having a VO2 ≥15 ml/kg/min when a patient can walk 25 shuttles was 50 (8–300).
The distance walked during SWT correlated significantly with the following parameters: MRC dyspnea score (p < 0.0001), age (p = 0.001), FEV1 (% of predicted: p < 0.009), peak VO2 (ml/kg/min: p < 0.0001; % of predicted: p < 0.035) and VCO2max (p < 0.0001).
Logistic regression analysis, predicting a binary variable of VO2 ≥15 ml/kg/min or not, indicated that walking 25 shuttles was the best independent predictor in the model (90% of the total explained variance) followed by gender (10% of the total explained variance) when adjusting for other meaningful covariates such as body mass index, FEV1 (% of predicted), dyspnea (MRC score) and age. The explanation of the variance by this model was very high (Nagelkerke R2 = 0.87).
ROC analysis (SWT distance vs. VO2 >15 ml/kg/min; binary outcome) is detailed in table 3. The area under the curve for this analysis was 0.89. The cutoff of 250 m (5 min) of the SWT has a sensitivity of 94% and a false-positive rate of 23% (specificity: 77%) for detecting VO2 >15 ml/kg/min. According to our analysis, the false-positive rate can decrease to 17, 11 and 0% if the patient walks 27 (270 m), 32 (320 m) and 38 shuttles (380 m), respectively.
Table 3.
ROC analysis
| VO2 >15 ml/kg/min | Valid cases | |
|---|---|---|
| Positive | 33 | |
| Negative | 17 |
| Positive if ≥ | True-positive rate (sensitivity) | False-positive rate (1 - specificity) |
|---|---|---|
| 59.00 ma | 1.000 | 1.000 |
| 85.00 ma | 1.000 | 0.941 |
| 125.00 ma | 1.000 | 0.882 |
| 142.00 ma | 1.000 | 0.765 |
| 147.00 ma | 0.970 | 0.765 |
| 155.00 ma | 0.970 | 0.647 |
| 165.00 ma | 0.939 | 0.529 |
| 185.00 ma | 0.939 | 0.412 |
| 205.00 ma | 0.939 | 0.353 |
| 215.00 ma | 0.939 | 0.294 |
| 235.00 ma | 0.939 | 0.235 |
| 255.00 ma | 0.848 | 0.235 |
| 265.00 ma | 0.848 | 0.176 |
| 275.00 ma | 0.758 | 0.176 |
| 290.00 ma | 0.697 | 0.176 |
| 315.00 ma | 0.697 | 0.118 |
| 335.00 ma | 0.667 | 0.118 |
| 350.00 ma | 0.636 | 0.118 |
| 365.00 ma | 0.576 | 0.118 |
| 380.00 ma | 0.485 | 0.000 |
Area under the curve = 0.891. The positive actual state is 1.00 for VO2 >15 ml/kg/min.
Test result variable: shuttles.
Discussion
This study validates the linear association between VO2 and the distance walked, and provides ranges of VO2 associated with the completed levels of the SWT. The study results support the proposed 25 shuttles as a screening method for a defined level of exercise capacity associated with a VO2 of 15 ml/kg/min and also show the shortcomings of such a cutoff.
Our work also provides clinically useful estimates for daily practice: the positive and negative predictive values of walking the proposed 25 shuttles associated with the desired VO2.
The SWT, in our experience, has shown to be simple to perform in the clinic setting and is feasible to routinely evaluate exercise capacity in COPD. To our knowledge, this is the largest series of patients in whom VO2 was measured during the performance of the SWT, being one of the strengths of this study. We believe our results have external validity as we recruited a convenient sample of patients attending a COPD clinic.
We extend previous reports on the association of distance walked during SWT by providing the specific energy cost of every level (minute walked) of the SWT (fig. 1, table 2) and by determining the high positive and negative predictive values of the 25 shuttles to determine the desired exercise capacity. ROC analysis showed insightful results since it reveals the shortcomings of the 250 m proposed by the BTS. Our results are a helpful addition to the clinical patient information to decide ordering a cardiopulmonary exercise test (by knowing the false-positive rates of the distance walked by the patient that associates with a VO2 <15 ml/kg/min). Walking 2, 7 and 13 more shuttles than the 25 proposed by the BTS decreases the false-positive rates of the test to 17, 11 and 0%, respectively. Our result on the 0% false-positive rate of walking 380 m coincides with previous results [12].
The results of the logistic regression model provide further important information: 25 shuttles was the strongest predictor of VO2 ≥15/ml/kg/min, accounting for most of the explained variance while controlling for very meaningful covariates: dyspnea (MRC score), age, gender, body mass index and FEV1 (% of predicted).
We found that the prediction of a VO2 of 15 ml/kg/min (associated with an average operative risk) is further improved by adjusting for gender, indicating that gender is a factor to consider when interpreting results of exercise tests in absolute values of VO2 (in ml/kg/min), as women characteristically have lower absolute exercise capacity. A previous report suggested the use of percent of the predicted exercise capacity, in part driven by the different exercise capacity related to gender [3].
We believe that our estimates of shuttle distance and VO2 for each level of the test are not affected by the use of the equipment, being in contrast to a previous report employing heavier equipment (4.1 kg) that made the patients walk shorter distances when wearing the monitor compared to controls without it [15]. We used a lightweight monitor (0.7 kg) that at least subjectively did not affect the walking ability of the subjects.
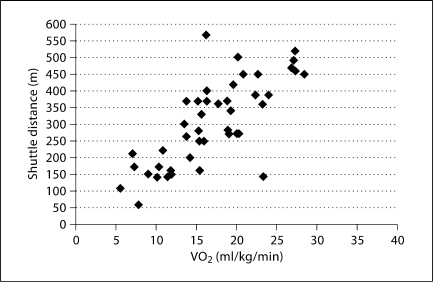
This study has limitations: first, we acknowledge that adding a practice walk could have improved the distance walked, but it is not feasible in a clinical setting and previous reports do not recommend a practice walk in clinical practice [16,17,18]. Second, as in any model validation, a separate validation cohort is desirable since it may provide slightly different estimates. Third, in our group of COPD patients, the prevalence of VO2 <15 ml/kg/min was 30%, i.e., 15 patients falling below the cutoff values for the average operative risk (fig. 2); we recognized that a larger series may provide a more accurate range of VO2 estimates for every SWT level. Finally, in this work, oxygen consumption is measured during walking and is possibly overestimated compared to the one the same patients could have reached with the bike, as it is known that walking requires higher oxygen consumption than cycling. This fact should be taken into account when using these results for operability selection.
Fig. 2.
Peak VO2 versus SWT distance: raw data.
In summary, we believe that these results are important. They are informative of the SWT value as a screening tool, as recommended by the BTS, and will help clinicians and surgeons with the interpretation of SWT results. Our work supports the association between SWT and VO2, and confirms the feasibility of this test in clinical practice.
Acknowledgement
Dr. Benzo is supported by grant #1K23CA106544 from the National Institutes of Health.
References
- 1.Bolliger CT, Jordan P, Solèr M, Stulz P, Grädel E, Skarvan K, Elsasser S, Gonon M, Wyser C, Tamm M, et al. Exercise capacity as a predictor of postoperative complications in lung resection candidates. Am J Respir Crit Care Med. 1995;151:1472–1480. doi: 10.1164/ajrccm.151.5.7735602. [DOI] [PubMed] [Google Scholar]
- 2.Wyser C, Stulz P, Solèr M, Tamm M, Müller-Brand J, Habicht J, Perruchoud AP, Bolliger CT. Prospective evaluation of an algorithm for the functional assessment of lung resection candidates. Am J Respir Crit Care Med. 1999;159:1450–1456. doi: 10.1164/ajrccm.159.5.9809107. [DOI] [PubMed] [Google Scholar]
- 3.Win T, Jackson A, Sharples L, Groves AM, Wells FC, Ritchie AJ, Laroche CM. Cardiopulmonary exercise tests and lung cancer surgical outcome. Chest. 2005;127:1159–1165. doi: 10.1378/chest.127.4.1159. [DOI] [PubMed] [Google Scholar]
- 4.Bolliger CT, Guckel C, Engel H, Stohr S, Wyser CP, Schoetzau A, Habicht J, Solèr M, Tamm M, Perruchoud AP. Prediction of functional reserves after lung resection: comparison between quantitative computed tomography, scintigraphy, and anatomy. Respiration. 2002;69:482–489. doi: 10.1159/000066474. [DOI] [PubMed] [Google Scholar]
- 5.BTS guidelines Guidelines on the selection of patients with lung cancer for surgery. Thorax. 2001;56:89–108. doi: 10.1136/thorax.56.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh SJ, Morgan MD, Scott S, Walters D, Hardman AE. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax. 1992;47:1019–1024. doi: 10.1136/thx.47.12.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh SJ, Morgan MD, Hardman AE, Rowe C, Bardsley PA. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J. 1994;7:2016–2020. [PubMed] [Google Scholar]
- 8.Chetta A, Olivieri D. The clinical relevance of exercise capacity assessment in respiratory diseases: introduction. Respiration. 2009;77:2. doi: 10.1159/000178797. [DOI] [PubMed] [Google Scholar]
- 9.Booth S, Adams L. The shuttle walking test: a reproducible method for evaluating the impact of shortness of breath on functional capacity in patients with advanced cancer. Thorax. 2001;56:146–150. doi: 10.1136/thorax.56.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morales FJ, Martínez A, Méndez M, Agarrado A, Ortega F, Fernández-Guerra J, Montemayor T, Burgos J. A shuttle walk test for assessment of functional capacity in chronic heart failure. Am Heart J. 1999;138:291–298. doi: 10.1016/s0002-8703(99)70114-6. [DOI] [PubMed] [Google Scholar]
- 11.Morales FJ, Montemayor T, Martinez A. Shuttle versus six-minute walk test in the prediction of outcome in chronic heart failure. Int J Cardiol. 2000;76:101–105. doi: 10.1016/s0167-5273(00)00393-4. [DOI] [PubMed] [Google Scholar]
- 12.Win T, Jackson A, Groves AM, Sharples LD, Charman SC, Laroche CM. Comparison of shuttle walk with measured peak oxygen consumption in patients with operable lung cancer. Thorax. 2006;61:57–60. doi: 10.1136/thx.2005.043547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J. 2004;23:698–702. doi: 10.1183/09031936.04.00121404. [DOI] [PubMed] [Google Scholar]
- 14.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 15.Singh SJ, Jones PW, Evans R, Morgan MD. Minimum clinically important improvement for the incremental shuttle walking test. Thorax. 2008;63:775–777. doi: 10.1136/thx.2007.081208. [DOI] [PubMed] [Google Scholar]
- 16.Sciurba F, Criner GJ, Lee SM, Mohsenifar Z, Shade D, Slivka W, Wise RA. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med. 2003;167:1522–1527. doi: 10.1164/rccm.200203-166OC. [DOI] [PubMed] [Google Scholar]
- 17.Elías Hernández MT, Fernández Guerra J, Toral Marín J, Ortega Ruiz F, Sánchez Riera H, Montemayor Rubio T. Reproducibility of a shuttle walking test in patients with chronic obstructive pulmonary disease (in Spanish) Arch Bronconeumol. 1997;33:64–68. [PubMed] [Google Scholar]
- 18.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]