Abstract
Background:
Retransplantation is the only form of treatment for patients with irreversible graft failure. The aim of this study was to analyse a single centre's experience of the indications for and outcomes of retransplantation.
Methods:
A total of 196 patients who underwent liver retransplantation using 225 grafts, between January 1982 and July 2007, were included in the study. The following parameters were analysed: patient demographics; primary diagnosis; distribution of retransplantation over different time periods; indications for retransplantation; time interval to retransplantation, and overall patient and graft survival.
Results:
Of the 2437 primary orthotopic liver transplantations, 196 patients (8%) required a first regraft, 23 patients (1%) a second regraft and six patients (0.25%) a third regraft. Autoimmune hepatitis was the most common primary diagnosis for which retransplantation was required (12.7% of primary transplantations). The retransplantation rate declined from 12% at the beginning of our programme to 7.6% at the end of the study period. The most common indication for retransplantation was hepatic artery thrombosis (31.6%). Nearly two-thirds of the retransplantations were performed within 6 months of the primary transplantation. The 1-, 3-, 5- and 10-year patient survival rates following first retransplantation were 66%, 61%, 57% and 47%, respectively. Five-year survival after second retransplantation was 40%. None of the patients have yet survived 3 years after a third regraft. Donor age of ≤55 years and a MELD (Model for End-stage Liver Disease) score of ≤23 were associated with better outcome following retransplantation.
Conclusions:
First retransplantation was associated with good longterm survival. There was no survival benefit following second and third retransplantations. A MELD score of ≤23 and donor age of ≤55 years correlated with better outcome following retransplantation.
Keywords: liver retransplantation
Introduction
Orthotopic liver transplantation is currently the life-saving therapeutic modality for patients with end-stage liver failure, with 5- and 10-year survival rates of over 70% and 65%, respectively.1 However, a significant proportion of patients (10.0–19.4%) suffer graft loss following primary liver transplantation.1–4 Retransplantation is the only viable treatment option for patients with irreversible graft failure. The incidence of retransplantation varies between 5% and 22% worldwide.5–7
Retransplantation presents a clinical dilemma because it is associated not only with ethical and economic issues, but also with a significantly poorer outcome compared with that following primary transplantation.8–11 Every liver allocated for retransplantation in one patient results in a missed opportunity for primary transplantation in another. This assumes greater significance in the context of increasing donor organ shortage.
However, as the number of transplantations performed every year using marginal grafts and grafts from non-heart-beating donors is rising, the incidence of graft loss is likely to increase proportionately, thereby increasing the need for retransplantation in the future. Although several studies on retransplantation have been published in the literature, most reports are based on small sample sizes.6,12–14 Moreover, only limited data are available on multiple retransplants and retransplantation experiences from the UK.11 As our institution is one of the largest transplant centres in the UK, we reviewed our experience to identify the indications for retransplantation and evaluate its outcomes.
Materials and methods
This is a retrospective study performed over a 25-year period from January 1982 to July 2007. All adult patients who underwent primary cadaveric orthotopic liver transplantation during the study period at the University Hospitals of Birmingham National Health Service (NHS) Foundation Trust (UHB) were analysed to identify those who had subsequent retransplantation. All consecutive patients who had first, second and third retransplants were included in the study. The data were collected from the prospectively maintained dedicated liver unit database at UHB.
Surgical technique
A standard subcostal approach was used. During the initial part of the programme, all patients underwent caval replacement with end-to-end suprahepatic and infrahepatic caval anastomosis. Temporary veno–venous bypass was introduced in 1987. In recent years we have increasingly used the piggyback technique with side-to-side cavo–cavoplasty between the donor and recipient retro-hepatic inferior vena cava without bypass. In these cases, a temporary end-to-side porto–caval shunt was performed except in patients with significantly spontaneous shunts. Following completion of caval and portal anastomoses, the graft was flushed with 1 l of 5% dextrose to prevent reperfusion injury, although a blood flush was used by one surgeon. The hepatic artery was reconstructed using an end-to-end anastomosis or a jump artery graft to the aorta or its major branches. Biliary reconstruction involved either a choledocho-choledochostomy or a Roux-en-Y choledocho-jejunostomy.
Immunosuppression
A standard triple therapy with prednisolone, azathioprine and tacrolimus has been used since 2000. Prior to this period, immunosuppression was based on cyclosporin. Tacrolimus trough level was maintained around 10 ng/ml. Mycophenolate mofetil (MMF) was used instead of azathioprine in the presence of tacrolimus toxicity in order to reduce the dose of tacrolimus. In the presence of MMF, trough tacrolimus level was maintained around 5 ng/ml.
Data analysis
We analysed a number of variables pertaining to the retransplanted patients, including: demographic data; primary diagnosis; time period of retransplantation; indications for retransplantation; time interval between primary transplantation and retransplantation; preoperative MELD (Model for End-stage Liver Disease) score; cold ischaemia time, and donor age. The overall 30-day, 90-day, 1-, 3-, 5- and 10-year graft and patient survival rates were calculated and compared among patients who received first, second and third retransplantations. Different parameters predicting survival following retransplantation were also analysed.
In order to study the effect of increasing experience in transplantation and improvements in perioperative care and immunosuppression, the study period was divided into four eras: 1982–1988, 1989–1994, 1995–2001 and 2002–2007. Similarly, procedures were classified as early and late retransplantations according to the time interval between primary transplantation and retransplantation. Early retransplantations included regrafts performed within 7 days of primary transplantation. Patients were classified as belonging to one of two groups according to whether their MELD score was ≤23 or >23 as 23 was the median MELD score in the study group. They were also divided into groups according to length of cold ischaemia time (≤12 hours and >12 hours) and donor age (≤55 years and >55 years).
Statistical analysis
Survival data are displayed in the form of Kaplan–Meier curves. A log-rank test was used to compare survivals. Multivariate logistic regression analysis was also performed, in which a P-value of <0.05 was considered statistically significant. spss for Windows Version 15 (SPSS, Inc., Chicago, IL, USA) was used for data analysis.
Results
A total of 2437 primary cadaveric orthotopic liver transplantations were performed during the study period. Of these patients, 196 underwent retransplantation, requiring 225 liver grafts (9.2%). Out of the 196 patients who underwent a first regraft, 23 patients subsequently underwent a second regraft (0.9%). Six of the 23 patients who underwent a third liver graft (second regraft) subsequently required a fourth graft (0.25%). The mean age at the time of first regraft was 43 years (range 16–68 years).
The primary diagnoses of end-stage liver failure in the 196 retransplanted patients were autoimmune hepatitis (12.7% of primary transplantations), fulminant hepatic failure (10.7%), primary sclerosing cholangitis (10.1%), primary biliary cirrhosis (8.5%), hepatitis C cirrhosis (7.0%), alcoholic liver disease (5.1%) and others (5.5%). Other aetiologies include cryptogenic cirrhosis, tumours of the liver, alpha-1 antitrypsin deficiency and polycystic liver disease (Table 1).
Table 1.
Primary aetiology of end-stage liver disease in retransplanted patients
| Primary diagnosis | Primary transplantation, n | First retransplantation, n (%) |
|---|---|---|
| Primary biliary cirrhosis | 634 | 54 (8.5) |
| Primary sclerosing cholangitis | 267 | 27 (10.1) |
| Fulminant hepatic failure | 327 | 35 (10.7) |
| Autoimmune hepatitis | 150 | 19 (12.7) |
| Alcoholic liver disease | 255 | 13 (5.1) |
| Hepatitis C cirrhosis | 272 | 19 (7.0) |
| Others | 532 | 29 (5.5) |
| Total | 2437 | 196 |
When the incidence of retransplantation was analysed in the four different time periods, we found that despite a steady increase in the number of primary transplantations, the number of retransplantations had remained relatively unchanged. During 1982–1988, 23 first retransplantations were performed compared with 191 primary transplantations (12.0%); in 1989–1994, 54 first regrafts were performed in a primary transplant group of 635 patients (8.5%). In the 1995–2001 period, 61 regrafts were undertaken in 846 primary transplant patients (7.2%); during 2002–2007, 58 retransplants were carried out in 765 primary transplant patients (7.6%). This implies a steady decline in the retransplantation rate from 12.0% at the beginning to 7.6% at the end of the study period. However, some retransplants were performed in a later era to the era of first transplant, so these proportions may not reflect the true retransplant rate of those transplanted in each era.
Analysis of the indications for retransplantation revealed that hepatic artery thrombosis (HAT) was the most common indication for first, second and third regrafts (31.6%, 34.8% and 33.3%, respectively) followed by chronic rejection (22.4% of first regrafts) and recurrent disease (13.2% of first regrafts). Acute rejection and primary non-function (PNF) as the cause of primary graft failure requiring retransplantation were relatively uncommon, accounting for only 2.5% and 10.7%, respectively (Table 2).
Table 2.
Indications for retransplantation
| Indications | First retransplantation, n (%) | Second retransplantation, n (%) | Third retransplantation, n (%) |
|---|---|---|---|
| Acute rejection | 4 (2.0) | 0 | 0 |
| Chronic rejection | 44 (22.4) | 6 (26.1) | 1 (16.7) |
| Graft infarction | 26 (13.2) | 3 (13.0) | 0 |
| Hepatic artery thrombosis | 61 (31.1) | 8 (34.8) | 2 (33.3) |
| Primary non-function | 21 (10.7) | 0 | 1 (16.7) |
| Recurrent disease | 26 (13.2) | 4 (17.4) | 2 (33.3) |
| Others | 14 (7.1) | 2 (8.7) | 0 |
| Total | 196 | 23 | 6 |
The median time interval between primary transplantation and first retransplantation was 69 days (range 1–7870 days. Early retransplantation was performed in 36 patients (18.4%), the most common indication being HAT (30.6%). Nearly two-thirds of the regrafted patients underwent the procedure within 6 months of their primary transplantation. Most of the late retransplantations were performed within 5 years of primary transplantation and only 10.7% of patients required retransplantation after 5 years (Table 3). Again, HAT was the predominant indication for late retransplantation, accounting for 31.3% of cases.
Table 3.
Time interval between primary transplantation and first retransplantation
| Time interval | First retransplantation, n (%) |
|---|---|
| 0–7 days | 36 (18.4) |
| 8–30 days | 38 (19.4) |
| 1–6 months | 51 (26.0) |
| 6 months–1 year | 8 (4.1) |
| 1–3 years | 33 (16.8) |
| 3–5 years | 9 (4.6) |
| 5–10 years | 11 (5.6) |
| >10 years | 10 (5.1) |
The median preoperative MELD score of the retransplanted patients was 22.3 (range 6–40). The median donor age was 36 years (range 9–72 years). The median cold ischaemia time was 597 min (range 131–1151 min).
Survival and prognostic factors
Overall graft and patient survival rates following first retransplantation are shown in Fig. 1. Figure 2 compares the cumulative survival curves following first, second and third retransplantations. In essence, 1-, 3-, 5- and 10-year patient survival rates following first retransplantation were 66%, 61%, 57% and 47%, respectively. After second retransplantation, patient survival figures fell to 45% at 1 year, 40% at 3 years, 40% at 5 years and 25% at 10 years. Following a third regraft, 24% of patients survived up to 1 year and none of the patients survived up to 3 years.
Figure 1.
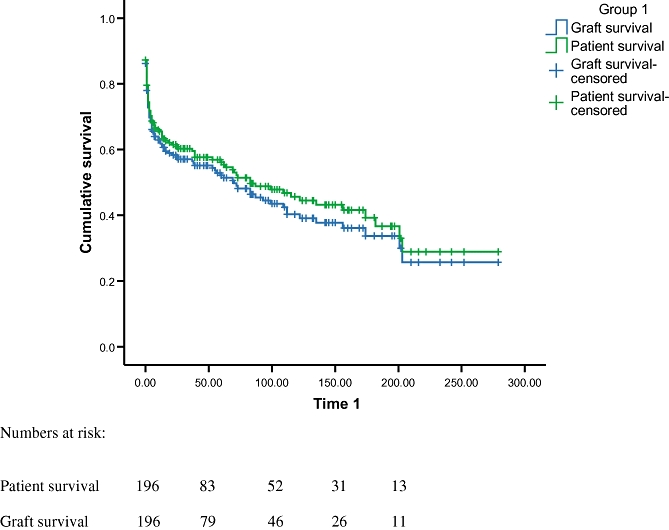
Survival curves showing patient and graft survival rates after first retransplantation
Figure 2.
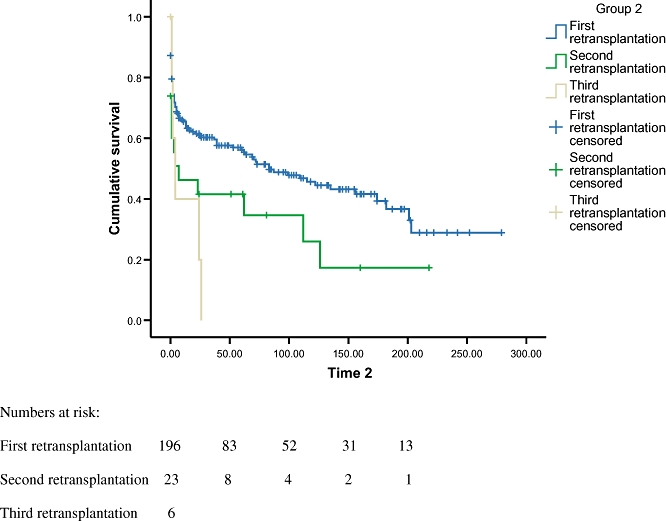
Cumulative survival curves comparing outcomes after first, second and third retransplantations
Univariate analysis was performed initially to identify factors predicting survival (Table 4A). There was a statistically significant difference in survival in different eras of operation. Patients who underwent retransplantation during 2002–2007 had better survival than those who underwent earlier procedures (P= 0.006) (Fig. 3). Early retransplantation was associated with worse outcome compared with late retransplantation (P= 0.015) (Fig. 4). Patients who had retransplantation for PNF and graft infarction had poorer survival in comparison with patients with other indications (P= 0.028). Other factors, including primary diagnosis (P= 0.507), MELD score (P= 0.919), cold ischaemia time (P= 0.406) and donor age (P= 0.428), were not found to be statistically significant. However, on stepwise logistic regression analysis, MELD score (P= 0.029) and donor age (P= 0.036) reached statistical significance, but all the other factors mentioned above did not (Table 4B, C).
Table 4.
(A) Univariate analysis of variables predicting outcome following retransplantation. (B) Multivariate analysis of the variables predicting outcome following retransplantation. (C) Stepwise logistic regression analysis of variables predicting outcome following retransplantation
| Variable | Odds ratio | 95% CI | P-value |
|---|---|---|---|
| (A) | |||
| Period of retransplantation | |||
| 1982–1988 | – | – | – |
| 1989–1994 | 3.24 | 1.59–6.58 | 0.001 |
| 1995–2001 | 1.96 | 1.04–3.69 | 0.036 |
| 2002–2007 | 1.68 | 0.89–3.18 | 0.108 |
| Early vs. late retransplantation | |||
| 0–7 days | – | – | – |
| 8–30 days | 1.93 | 1.19–3.14 | 0.008 |
| >30 days | 1.00 | 0.59–1.69 | 0.998 |
| Indications for retransplantation | |||
| Acute rejection | – | – | – |
| Hepatic artery thrombosis | 1.41 | 0.31–6.31 | 0.653 |
| Primary non-function | 0.73 | 0.26–2.12 | 0.570 |
| Graft infarction | 1.53 | 0.49–4.70 | 0.459 |
| Recurrent disease | 1.84 | 0.62–5.45 | 0.271 |
| Chronic rejection | 1.09 | 0.36–3.30 | 0.885 |
| Biliary complications | 0.71 | 0.24–2.09 | 0.538 |
| Others | 0.72 | 0.16–3.24 | 0.672 |
| Primary diagnosis | |||
| Alcoholic cirrhosis | – | – | – |
| Autoimmune hepatitis | 1.56 | 0.66–3.69 | 0.309 |
| Acute liver failure | 1.39 | 0.65–2.97 | 0.397 |
| Hepatitis C cirrhosis | 0.67 | 0.31–1.43 | 0.300 |
| Primary biliary cirrhosis | 1.24 | 0.54–2.84 | 0.606 |
| Primary sclerosing cholangitis | 1.05 | 0.57–1.96 | 0.868 |
| Others | 1.02 | 0.49–2.09 | 0.951 |
| Preoperative MELD score | |||
| ≤23 | – | – | – |
| >23 | 0.98 | 0.63–1.51 | 0.921 |
| Cold ischaemia time | |||
| >12 hours | – | – | – |
| ≤12 hours | 0.84 | 0.55–1.28 | 0.419 |
| Donor age | |||
| >55 years | – | – | – |
| ≤55 years | 0.72 | 0.31–1.66 | 0.445 |
| (B) | |||
| Period of retransplantation | |||
| 1982–1988 | – | – | – |
| 1989–1994 | 5.93 | 2.47–14.19 | 0.000 |
| 1995–2001 | 3.21 | 1.52–6.80 | 0.002 |
| 2002–2007 | 2.43 | 1.21–4.87 | 0.012 |
| Early vs. late retransplantation | |||
| 0–7 days | – | – | – |
| 8–30 days | 0.92 | 0.35–2.41 | 0.881 |
| >30 days | 0.50 | 0.23–1.07 | 0.075 |
| Indications for retransplantation | |||
| Acute rejection | – | – | – |
| Hepatic artery thrombosis | 1.50 | 0.26–8.65 | 0.645 |
| Primary non-function | 0.57 | 0.18–1.81 | 0.343 |
| Graft infarction | 0.94 | 0.20–4.32 | 0.937 |
| Recurrent disease | 1.52 | 0.41–5.63 | 0.530 |
| Chronic rejection | 0.85 | 0.26–2.75 | 0.787 |
| Biliary complications | 0.33 | 0.10–1.08 | 0.068 |
| Others | 0.28 | 0.05–1.44 | 0.130 |
| Primary diagnosis | |||
| Alcoholic cirrhosis | – | – | – |
| Autoimmune hepatitis | 1.72 | 0.69–4.30 | 0.239 |
| Acute liver failure | 1.40 | 0.59–3.29 | 0.440 |
| Hepatitis C cirrhosis | 0.45 | 0.20–1.04 | 0.063 |
| Primary biliary cirrhosis | 1.26 | 0.51–3.10 | 0.606 |
| Primary sclerosing cholangitis | 0.81 | 0.42–1.59 | 0.557 |
| Others | 0.84 | 0.39–1.82 | 0.670 |
| Preoperative MELD score | |||
| ≤23 | – | – | – |
| >23 | 0.93 | 0.54–1.62 | 0.821 |
| Cold ischaemia time | |||
| >12 hours | – | – | – |
| ≤12 hours | 0.61 | 0.38–0.98 | 0.042 |
| Donor age | |||
| >55 years | – | – | – |
| ≤55 years | 1.13 | 0.47–2.74 | 0.775 |
| (C) | |||
| Preoperative MELD score ≤23 | 1.03 | 1.00–1.06 | 0.029 |
| Donor age ≤55 years | 1.02 | 1.00–1.04 | 0.036 |
95% CI, 95% confidence interval; MELD, Model for End-stage Liver Disease
Figure 3.
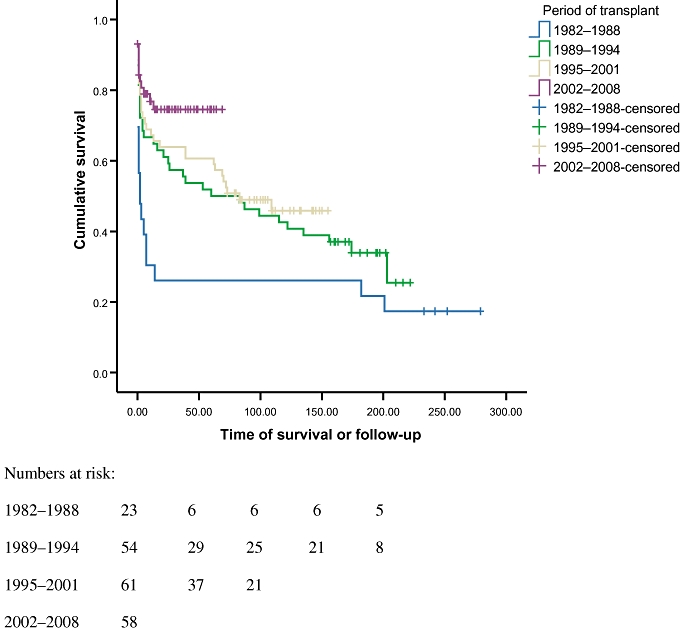
Cumulative survival curves comparing the four different eras of retransplantation
Figure 4.
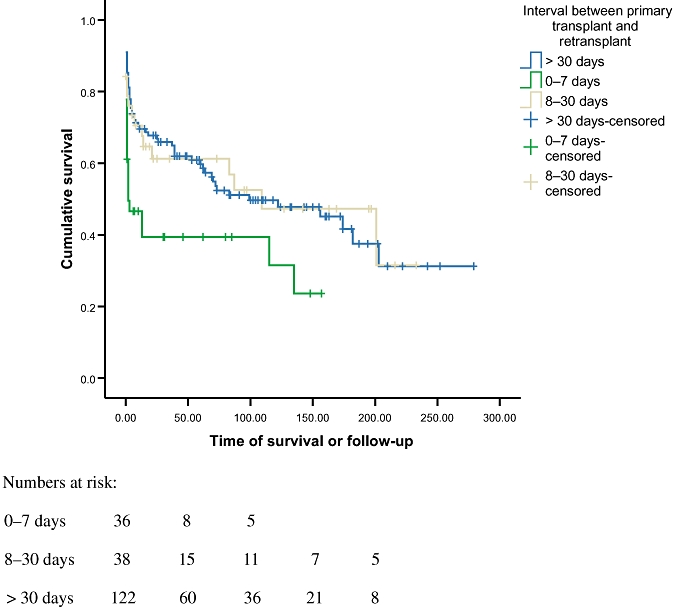
Cumulative survival curves comparing time intervals between primary transplantation and retransplantation
Discussion
This study confirms that liver retransplantation is an effective treatment modality for patients with primary graft failure and offers good longterm survival.
The incidence of retransplantation in our study was 9.2%. This is comparable with the figures quoted in the literature, which vary between 5% and 22%.5–7,14–15 At our centre, the retransplantation rate fell from 12.0% at the beginning of our study period to 7.6% at the end of it, despite a steady increase in both the number of primary transplantations and the use of marginal grafts. This reflects improvements in intraoperative monitoring, surgical technique, organ preservation, postoperative care and effective immunosuppressive therapy.
The most common indication for retransplantation in this study was HAT, accounting for around one-third of all patients undergoing first, second or third retransplantations. Published data show that HAT accounted for 11.5–36.0% of all retransplant cases in adults.1–4,16,17 Although technical reasons commonly account for HAT, it is also known to be associated with older donors and marginal donors.18,19 The higher rate of HAT requiring retransplantation in our study possibly reflects our policy to retransplant all HAT patients as we feel that any other interventional procedure may delay the decision for retransplantation and worsen the patient's prognosis. We did not find any association between the use of arterial conduit and the development of HAT. Nishida et al. found that protocol Doppler ultrasonography of the liver graft detects early HAT and that urgent revascularization based on this could significantly reduce the incidence of graft loss requiring retransplantation in the paediatric population.20
The proportion of regrafts performed for PNF was lower in our study (10.7% of patients) compared with the published data. The incidence of PNF varies from 10.0% to 32.3% worldwide.1–4,16,17 Jain et al. demonstrated that PNF was the most common indication for retransplantation, accounting for 32.3% of cases.2 The lower incidence of PNF in our centre may be attributable to strict graft selection, harvesting and graft preservation protocols.
The overall 1-, 3-, 5- and 10-year survival rates following first retransplantation were 66%, 61%, 57% and 47%, respectively. These are comparable with rates cited in the literature.8,15,21 These survival figures are lower than equivalent rates after primary transplantation. Despite its inferior results compared with primary grafting, hepatic retransplantation cannot be abandoned because it is the only treatment option for patients with a failing liver graft. Hence a rationalized approach is needed to balance the fulfilling of responsibilities to patients requiring retransplantation and to patients awaiting a primary liver graft. This might be achieved by identifying a subgroup of patients who are likely to have a poor outcome following retransplantation. In the present study, 1-year patient survival was 45% after second retransplantations and 24% after third retransplantations. Based on these outcomes, if the general rule requiring a 50% survival rate at 5 years were adhered to, no patients should undergo second or third retransplantations. Similar findings have been reported from Pittsburg and Los Angeles.11,22
Analysis of the prognostic factors using the logistic regression model revealed preoperative MELD score and donor age as independent risk factors predicting outcome following regrafts. Several authors have attempted to devise risk scores and predict survival after retransplantation.1,11,19,21,23–25 A number of factors have been found to significantly affect outcome after retransplantation. These include donor variables (age and gender), recipient variables (bilirubin, creatinine, recipient age, preoperative mechanical ventilation and choice of immunosuppression),11,22 MELD score,25,26 timing of retransplantation,6,9,27 use of intraoperative blood products10 and indications for retransplantation.8
The timing of retransplantation has been shown to play a significant role in both patient and graft survival.8,27 Chen et al. demonstrated that patients in whom the interval to retransplantation was 8–30 days displayed lower survival rates compared with those who underwent later retransplantations.6 They reasoned that this might be a consequence of postoperative sepsis and more severely compromised clinical status because of the delay in retransplantation, thereby leading to higher post-transplant mortality. In the current study, early retransplantation within 7 days of primary grafting was found to be a predictor of poorer outcome on univariate analysis. However, this did not reach statistical significance on multivariate regression analysis. The higher incidence of mortality following early retransplantation may be explained by the fact that the initial period after transplantation represents that of the most intense immunosuppression. This is supported by another study which found that the most common cause of death in this group of patients was sepsis.11 Moreover, patients who need early retransplantation are by definition suffering from acute liver failure, whereas those who require late retransplantation usually have chronic liver failure, which accounts for the higher mortality in the former group.
The indication for retransplantation has not been confirmed as a predictor of prognosis in most studies.10,11,15 Facciuto et al. showed that patients who underwent retransplantation for recurrent hepatitis C had poorer 90-day survival than those who underwent retransplantation for other indications, although this difference was not statistically significant.10 We found that patients with PNF and graft infarction had a significantly poorer outcome on univariate analysis. However, this did not reach significance on multivariate analysis. This is possibly because this group of patients would have been clinically septic and immunocompromised prior to second grafting.
The MELD scale was implemented in 2002 to evaluate the severity of disease in patients with end-stage liver disease and to stratify patients for prioritization for transplantation. It has been shown to be a good predictor of pre-transplant mortality, although it is a poor indicator of the outcome of the transplantation itself.26 Contrary to this, Rosen et al. found MELD scores to be predictive of survival following retransplantation when they stratified disease severity using MELD cut-off scores of <22, 22–31 and ≥32.25 This was confirmed in our study, in which a MELD cut-off score of 23 was used.
This study demonstrated that a MELD score of ≤23 and donor age of ≤55 years correlated with a better outcome following retransplantation. We conclude from our data that first retransplantation is associated with good longterm graft and patient survival. However, candidates for second and third retransplantations should be scrutinized carefully and the procedure considered only in a selected group of low-risk patients. Second and third retransplantations should not be performed routinely in all patients with failing second grafts because there is no demonstrable longterm survival benefit.
Conflicts of interest
None declared.
References
- 1.Azoulay D, Linhares MM, Huguet E, Delvart V, Castaing D, Adam R, et al. Decision for retransplantation of liver: an experience and cost-based analysis. Ann Surg. 2002;236:713–721. doi: 10.1097/01.SLA.0000036264.66247.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K, et al. Longterm survival after liver transplantation in 4000 consecutive patients at a single centre. Ann Surg. 2000;232:490–500. doi: 10.1097/00000658-200010000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bramhall SR, Minford E, Gunson B, Buckels JA. Liver transplantation in the UK. World J Gastroenterol. 2001;7:602–611. doi: 10.3748/wjg.v7.i5.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jimenez M, Turrion VS, Alvira LG, Lucena JL, Ardaiz J. Indications and results of retransplantation after a series of 406 consecutive liver transplantations. Transplant Proc. 2002;34:262–263. doi: 10.1016/s0041-1345(01)02753-1. [DOI] [PubMed] [Google Scholar]
- 5.Pfitzmann R, Benscheidt B, Langrehr JM, Schumacher G, Neuhaus R, Neuhaus P. Trends and experiences in liver retransplantation over 15 years. Liver Transpl. 2007;13:248–257. doi: 10.1002/lt.20904. [DOI] [PubMed] [Google Scholar]
- 6.Chen GH, Fu BS, Cai CJ, Lu MQ, Yang Y, Yi SH, et al. A single-centre experience of retransplantation for liver transplant recipients with a failing graft. Transplant Proc. 2008;40:1485–1487. doi: 10.1016/j.transproceed.2008.01.076. [DOI] [PubMed] [Google Scholar]
- 7.Kashyap R, Jain A, Reyes J, Demetris AJ, Elmagd KA, Dodson SF, et al. Causes of retransplantation after primary liver transplantation in 4000 consecutive patients: 2–19 years follow-up. Transplant Proc. 2001;33:1486–1487. doi: 10.1016/s0041-1345(00)02563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Postma R, Haagsma EB, Peeters PM, Van den Berg AP, Slooff MJ. Retransplantation of liver in adults: outcome and predictive factors for survival. Transplant Int. 2004;17:234–240. doi: 10.1007/s00147-004-0708-5. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman MA, Ghobrial RM. When shouldn't we retransplant? Liver Transpl. 2005;11(Suppl. 2):14–20. doi: 10.1002/lt.20599. [DOI] [PubMed] [Google Scholar]
- 10.Facciuto M, Heidt D, Guarrera J, Bodian CA, Miller CM, Emre S, et al. Retransplantation for late liver graft failure: predictors of mortality. Liver Transpl. 2000;6:174–179. doi: 10.1002/lt.500060222. [DOI] [PubMed] [Google Scholar]
- 11.Markmann JF, Markowitz JS, Yersiz H, Morrisey M, Farmer DG, Farmer DA, et al. Longterm survival after retransplantation of the liver. Ann Surg. 1997;226:408–420. doi: 10.1097/00000658-199710000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang ZF, Liu C. Liver retransplantation: indications and outcomes. Hepatobiliary Pancreat Dis Int. 2004;3:175–178. [PubMed] [Google Scholar]
- 13.Magee JC, Barr ML, Basadonna GP, Johnson MR, Mahadevan S, McBride MA, et al. Repeat organ transplantation in the United States, 1996–2005. Am J Transplant. 2007;7:1424–1433. doi: 10.1111/j.1600-6143.2007.01786.x. [DOI] [PubMed] [Google Scholar]
- 14.Adani GL, Baccarani U, Risaliti A, Sainz-Barriga M, Lorenzin D, Costa G, et al. A single-centre experience of late retransplantation of the liver. Transplant Proc. 2005:2599–2600. doi: 10.1016/j.transproceed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 15.Lang H, Sotiropoulos GC, Beckebaum S, Fouzas I, Molmenti EP, Omar OS, et al. Incidence of liver retransplantation and its effect on patient survival. Transplant Proc. 2008;40:3201–3203. doi: 10.1016/j.transproceed.2008.09.039. [DOI] [PubMed] [Google Scholar]
- 16.Deshpande RR, Rela M, Girlanda R, Bowles MJ, Muiesan P, Dhawan A, et al. Longterm outcome of liver retransplantation in children. Transplantation. 2002;74:1124–1130. doi: 10.1097/00007890-200210270-00012. [DOI] [PubMed] [Google Scholar]
- 17.Jain A, Mazariegos G, Kashyap R, Kosmach-Park B, Starzl TE, Fung JJ, et al. Paediatric liver transplantation in 808 consecutive children: 20 years experience from a single centre. Transplant Proc. 2002;34:1955–1957. doi: 10.1016/s0041-1345(02)03136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adam R, McMaster P, O'Grady JG, Castaing D, Klempnauer JL, Jamieson N, et al. Evolution of Liver Transplantation in Europe: Report of the European Liver Transplant Registry. Liver Transplant. 2003;9:1231–1243. doi: 10.1016/j.lts.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 19.Biggins SW, Beldecos A, Rabkin JM, et al. Retransplantation for hepatic allograft failure: prognostic modelling and ethical considerations. Liver Transpl. 2002;8:313–322. doi: 10.1053/jlts.2002.31746. [DOI] [PubMed] [Google Scholar]
- 20.Nishida S, Kato T, Levi D, Naveen M, Thierry B, Vianna R, et al. Effect of protocol Doppler ultrasonography and urgent revascularization on early hepatic artery thrombosis after paediatric liver transplantation. Arch Surg. 2002;137:1279–1283. doi: 10.1001/archsurg.137.11.1279. [DOI] [PubMed] [Google Scholar]
- 21.Yao FY, Saab S, Bass NM, Hirose R, Ly D, Terrault N, et al. Prediction of survival after liver retransplantation for late graft failure based on preoperative prognostic scores. Hepatology. 2004;39:230–238. doi: 10.1002/hep.20005. [DOI] [PubMed] [Google Scholar]
- 22.Doyle H, Morelli F, McMichael J, Doria C, Aldrighetti L, Starzl TE, et al. Hepatic retransplantation: an analysis of risk factors associated with outcome. Transplantation. 1996;61:1499–1505. doi: 10.1097/00007890-199605270-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghobrial RM, Gornbein J, Steadman R, Danino N, Markmann JF, Holt C, et al. Pre-transplant model to predict post-transplant survival in liver transplant patients. Ann Surg. 2002;236:315–323. doi: 10.1097/00000658-200209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bilbao I, Armadans L, Lazaro JL, Hidalgo E, Castells L, Margarit C. Predictive factors for early mortality following liver transplantation. Clin Transplant. 2003;17:401–411. doi: 10.1034/j.1399-0012.2003.00068.x. [DOI] [PubMed] [Google Scholar]
- 25.Rosen HR, Prieto M, Taltavull TC, Cuervas Mons V, Guckelberger O, Muiesan P, et al. Validation and refinement of survival models for liver retransplantation. Hepatology. 2003;38:460–469. doi: 10.1053/jhep.2003.50328. [DOI] [PubMed] [Google Scholar]
- 26.Edwards E, Harper A. Does MELD work for relisted candidates? Liver Transpl. 2004;10(Suppl):10–16. doi: 10.1002/lt.20271. [DOI] [PubMed] [Google Scholar]
- 27.Busuttil RW, Farmer DG, Yersiz H, Hiatt JR, McDiarmid SV, Goldstein LI, et al. Analysis of longterm outcomes of 3200 liver transplantations over two decades: a single-centre experience. Ann Surg. 2005;241:905–916. doi: 10.1097/01.sla.0000164077.77912.98. [DOI] [PMC free article] [PubMed] [Google Scholar]


