Abstract
Intramyocardial hematoma is known to be associated with myocardial infarction, chest trauma, coronary artery bypass operation, and complication of percutaneous coronary intervention (PCI). We describe here a rare case of 50-year-old man with a huge right ventricular (RV) wall hematoma which was newly developed two hours after PCI. The patient was treated conservatively with a successful outcome. We discuss plausible mechanisms for the development of RV wall hematoma and treatment options for the case.
Keywords: Hematoma, Complication, Right ventricle, Percutaneous coronary intervention
Introduction
Intramyocardial hematoma is a rare disease, usually associated with myocardial infarction, chest trauma, coronary artery bypass operation, and complication of percutaneous coronary intervention (PCI) or can occur spontaneously.1-7) We report a rare case of giant right ventricular (RV) wall hematoma which was newly developed two hours after PCI.
Case
A 50-year-old man was transferred to our emergency room (ER) due to new onset chest pain, dyspnea, and RV wall mass, which were newly developed two hours after PCI at a local hospital. He visited the local hospital because of accelerating chest pain of three weeks duration. His initial electrocardiogram (ECG) was normal sinus rhythm without ST segment changes, and routine hematologic and biochemical tests produced normal results. His coronary angiographic findings before PCI revealed no significant luminal narrowing in the left anterior descending (LAD), and left circumflex coronary arteries, but total occlusion of the distal posterior descending artery (PDA) with poor collateral flow (grade 2) from distal LAD and 60% focal stenosis of posterolateral (PL) branch were observed. Sirolimus-eluting stent (Cypher, 2.75/28 mm, Cordis, Miami Lakes, FL, USA) was deployed without predilatation at the PL branch, and angioplasty with a 2.0/20 mm Maverick balloon (Boston Scientific, Natick, MA, USA) was performed at the proximal PDA. Final angiogram revealed acceptable results at PDA and PL branch without any abnormal findings (Fig. 1A). The patient tolerated the procedure well without any chest pain.
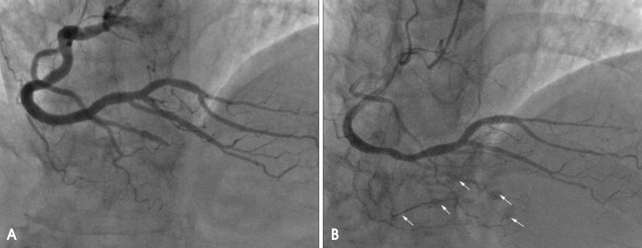
Fig. 1.
Final angiogram after stenting shows acceptable results at posterior descending artery and posterolateral branch of right coronary artery (A). Emergent coronary angiogram reveals a large amount of frank streaming of contrast material (arrows) in RV wall (B). RV: right ventricular.
Two hours after the procedure, he suddenly complained of severe chest pain. Emergent coronary angiogram revealed patent stent at the PL branch, but a large amount of frank streaming of contrast material in the RV wall, which was fed from the acute marginal branch of right coronary artery, was noted (Fig. 1B). Two dimensional echocardiography demonstrated a large 4×6 cm sized hematoma in the RV free wall without communication to the RV cavity and a small amount of pericardial effusion (Fig. 2). One day after the procedure, the patient was then transferred to our hospital for further evaluation.
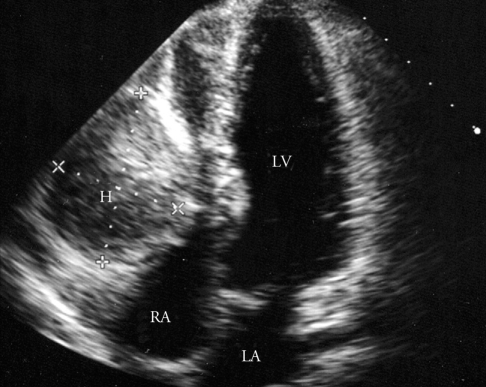
Fig. 2.
Transthoracic echocardiogram from apical 4-chamber view shows a large right ventricular wall mass that almost completely obliterates right ventricular chamber. A small pericardial effusion is also present. H: hematoma, LA: left atrium, LV: left ventricle, RA: right atrium.
Physical examinationat our ER revealed blood pressure of 120/70 mmHg, pulse rate of 80 bpm, and respiratory rate of 22/min. A 12-lead ECG showed normal sinus rhythm, left axis deviation, and Q waves with ST segment elevation in leads II, III, and aVF. The chest radiograph was unremarkable. CK-MB and troponin I levels were 130 ng/mL and 28.6 ng/mL, respectively.
Although the RV wall hematoma was so large enough to rupture, treatment option was decided based on his stable vital sign and tolerable chest pain. The patient was managed with standard anti-anginal therapy including intravenous nitroglycerin and morphine sulfate. Repeated echocardiogram revealed no interval changes in the size of hematoma. However, follow-up angiogram in our hospital showed the RV hematoma drained into RV cavity, suggesting the possibility of a fistula formation between the hematoma and RV cavity (Fig. 3). The patient's subsequent hospital course was uncomplicated. A final echocardiogram at eight weeks after PCI showed a complete resolution of the hematoma (Fig. 4). The patient is currently doing well.
Fig. 3.
Follow-up coronary angiogram shows a direct communication between hematoma and right ventricular cavity through fistula (arrow).
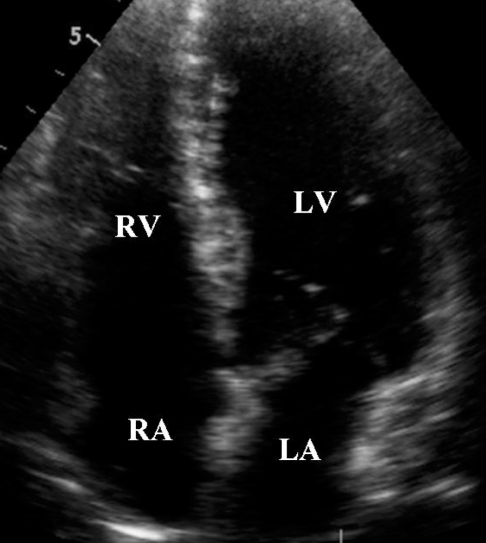
Fig. 4.
A final echocardiogram at eight weeks after percutaneous coronary intervention shows a complete resolution of the hematoma. LA: left atrium, LV: left ventricle, RA: right atrium, RV: right ventricle.
Discussion
Intramyocardial hematoma is a very rare condition that can occur following myocardial infarction, coronary artery bypass operation, chest trauma, catheter ablation and perforation of coronary artery during PCI.1-5) However, it can occur spontaneously.6),7) Although procedure-related intramyocardial hematoma is primarily associated with guidewire- or balloon-induced coronary perforation,1-4) there is no definite evidence of procedure-related RV hematoma in our case. In addition, it is interesting to observe the complete resolution of RV hematoma by spontaneous fistula formation between the hematoma and RV cavity.
Development of intramyocardial hematoma mostly composed of a rupture of intramyocardial vessel into the media and subadventitial region by a blunt trauma or vessel injury, which leads to an acute increase of coronary capillary perfusion pressure by recanalization causing intramyocardial bleeding when capillary permeability is altered by prolonged ischemia or necrosis.5) The exact cause of hematoma in our case remains unexplained. Procedure-related intramural hematoma shows a various clinical outcomes. Lin et al.1) reported a case of septum hematoma due to a complication of retrograde wiring in chronic total occlusion, which resolved spontaneously. Kawase et al.2) described a case of shock due to localized hematoma after coronary artery perforation during PCI in a patient with a remote history of CABG. Steinwender et al.3) reported a case of RV hematoma manifested with pseudo-pericardial tamponade after perforation of right coronary artery. The best therapeutic option for intramyocardial hematoma depends on its clinical situation. Surgical intervention is recommended when the patient has the sign of cardiac tamponade or compression of cardiac chamber due to hematoma.3),4) Otherwise, close observations are needed with monitoring of hemodynamic status and serial echocardiographic examination of the hematoma size.
Acknowledgements
This work was supported for two years by Pusan National University Research Grant.
References
- 1.Lin TH, Wu DK, Su HM, Chu CS, Voon WC, Lai WT, Sheu SH. Septum hematoma: a complication of retrograde wiring in chronic total occlusion. Int J Cardiol. 2006;113:e64–e66. doi: 10.1016/j.ijcard.2006.04.032. [DOI] [PubMed] [Google Scholar]
- 2.Kawase Y, Hayase M, Ito S, Ojio S, Tahara H, Ehara M, Kondo H, Ito Y, Suzuki Y, Ishihara Y, Suzuki T. Compression of right ventricular out-flow due to localized hematoma after coronary perforation during PCI. Catheter Cardiovasc Interv. 2003;58:202–206. doi: 10.1002/ccd.10443. [DOI] [PubMed] [Google Scholar]
- 3.Steinwender C, Hofmann R, Leisch F. Pseudo-pericardial tamponade after perforation of the right coronary artery. Heart. 2004;90:e36. doi: 10.1136/hrt.2004.035378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahman N, Sharif H, Jafary FH. Intramyocardial hematoma after coronary perforation during percutaneous coronary intervention--anticipated and treated. J Invasive Cardiol. 2008;20:e224–e228. [PubMed] [Google Scholar]
- 5.Drobinski G, Montalescot G, Nivet M. Intra-myocardial haemorrhage following recanalisation of a venous coronary arterial bypass by balloon angioplasty. Int J Cardiol. 1991;31:256–258. doi: 10.1016/0167-5273(91)90228-h. [DOI] [PubMed] [Google Scholar]
- 6.Cheng HW, Hung KC, Lin FC, Wu D. Spontaneous intramyocardial hematoma mimicking a cardiac tumor of the right ventricle. J Am Soc Echocardiogr. 2004;17:394–396. doi: 10.1016/j.echo.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Oh DH, Doh JH, Lee SH, Kwon SU, Namgung J, Lee SY, Kim CY, Chang WI, Chang SH, Lee WR. A case of spontaneous left atrial intramural hematoma causing vaso-occlusive cardiogenic shock. J Cardiovascular Ultrasound. 2006;14:112–115. [Google Scholar]