Abstract
OBJECTIVE
Paracrine signaling via γ-aminobutyric acid (GABA) and GABAA receptors (GABAARs) has been documented in rodent islets. Here we have studied the importance of GABAergic signaling in human pancreatic islets.
RESEARCH DESIGN AND METHODS
Expression of GABAARs in islet cells was investigated by quantitative PCR, immunohistochemistry, and patch-clamp experiments. Hormone release was measured from intact islets. GABA release was monitored by whole-cell patch-clamp measurements after adenoviral expression of α1β1 GABAAR subunits. The subcellular localization of GABA was explored by electron microscopy. The effects of GABA on electrical activity were determined by perforated patch whole-cell recordings.
RESULTS
PCR analysis detected relatively high levels of the mRNAs encoding GABAAR α2, β3, γ2, and π subunits in human islets. Patch-clamp experiments revealed expression of GABAAR Cl− channels in 52% of β-cells (current density 9 pA/pF), 91% of δ-cells (current density 148 pA/pF), and 6% of α-cells (current density 2 pA/pF). Expression of GABAAR subunits in islet cells was confirmed by immunohistochemistry. β-Cells secreted GABA both by glucose-dependent exocytosis of insulin-containing granules and by a glucose-independent mechanism. The GABAAR antagonist SR95531 inhibited insulin secretion elicited by 6 mmol/l glucose. Application of GABA depolarized β-cells and stimulated action potential firing in β-cells exposed to glucose.
CONCLUSIONS
Signaling via GABA and GABAAR constitutes an autocrine positive feedback loop in human β-cells. The presence of GABAAR in non–β-cells suggests that GABA may also be involved in the regulation of somatostatin and glucagon secretion.
Pancreatic islets of Langerhans are endocrine micro-organs with a central role in plasma glucose homeostasis. Islets consist of three main endocrine cell types: insulin-producing β-cells, glucagon-secreting α-cells, and somatostatin-releasing δ-cells. Insulin release from β-cells is directly controlled by the blood glucose level and modulated by circulating hormones and the autonomous nervous system. In addition, hormone release from β-cells, as well as from the other islet cell types, is regulated by autocrine and paracrine interactions.
The local signaling roles of the major islet hormones have been extensively studied and are well established (1). Islet cells also contain and release a variety of additional factors with putative local signaling functions, including ions (Zn2+, Ca2+) and neurotransmitters (GABA, glutamate, ATP) (2–5). We and others have presented evidence that GABA released from β-cells inhibits glucagon secretion in rodent islets by activating GABAA receptors (GABAAR) in α-cells (6–8).
The architecture of human islets, with non–β-cells distributed throughout the islet, rather than confined to the islet periphery as in rodents, facilitates paracrine signaling (9,10). Human β-cells contain high concentrations of GABA (11,12), and expression of GABAAR subunits in human islets has been detected by RT-PCR (8,13). We have now studied the possible involvement of GABA/GABAAR-mediated signaling in the regulation of hormone release from human islets. Our results suggest that GABA plays a more diverse role in human islets than suggested by previous work in rodent islets (5–7).
RESEARCH DESIGN AND METHODS
Islet preparation and cell culture.
Human pancreases were obtained with ethical approval and clinical consent from nondiabetic donors. Islets were isolated in the Diabetes Research and Wellness Foundation Human Islet Isolation Facility by collagenase digestion (Serva, Heidelberg, Germany), essentially as reported previously (14,15). For hormone release measurements, the islets were cultured overnight in Connaught Medical Research Laboratories (CMRL) medium containing 5 mmol/l glucose. The electrophysiological experiments were performed on single cells or cell clusters obtained by dissociation of islets in Ca2+-free buffer (16). The resulting cell suspension was then plated onto plastic Petri dishes and cultured in RPMI-1640 containing 10 mmol/l glucose and 2 mmol/l l-glutamine. For biophysical detection of GABA release (Figs. 3–5), cells were infected with recombinant adenoviruses encoding the GABAAR α1 and β1 subunits 24–48 h before the experiments (17).
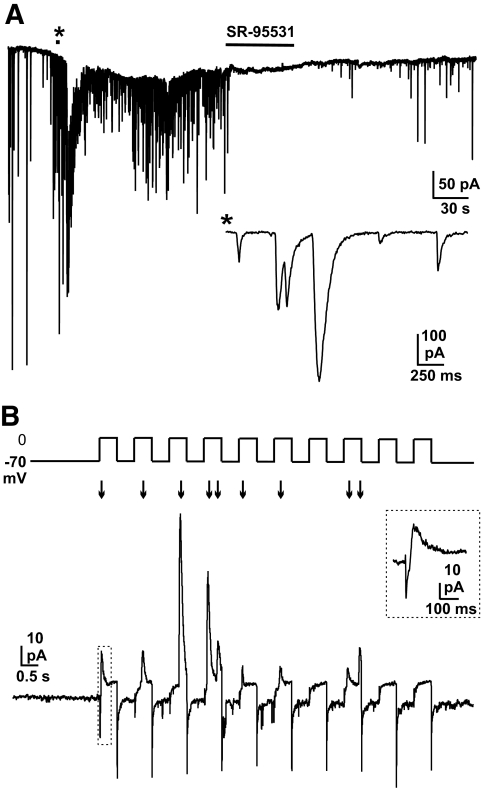
FIG. 3.
Quantal release of GABA from human β-cells. A: A β-cell overexpressing α1/β1 GABAAR was held at −70 mV and infused with intracellular solution containing 2 μmol/l free Ca2+ (at 5 mmol/l extracellular glucose). SR-95531 (10 μmol/l) was applied as indicated by the bar. The inset shows a part of the trace (indicated by *) on an expanded time scale. B: A train of 10 500-ms voltage-clamp depolarizations from −70 to 0 mV was applied to a cell overexpressing α1/β1 GABAAR (with intracellular solution containing 50 μmol/l EGTA). GABA-induced transient currents are indicated by arrows. The inset shows a part of the trace (marked by the dotted rectangle) on an expanded time base. Note that the direction of transient currents is outward at 0 mV. The initial downward component represents the opening of the voltage-gated Na+ and Ca2+ currents triggered by the depolarization. The activation of the GABAAR accounts for the outward current. The recording shown is representative of seven experiments.
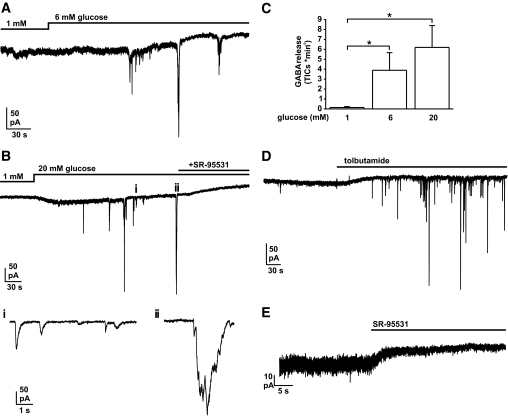
FIG. 4.
Glucose- and tolbutamide-induced GABA release from human β-cells. Experiments were performed in small clusters of islet cells overexpressing α1/β1 GABAAR. The patch-clamped cell was held at −70 mV and infused with pipette solution containing 10 mmol/l EGTA. A: The glucose concentration in the bath was increased from 1 to 6 mmol/l as indicated. B (upper): The extracellular glucose concentration was increased from 1 to 20 mmol/l. SR-95531 (10 μmol/l) was included as indicated. B (lower): Sections of top trace (as indicated by letters i and ii) shown on an expanded time base. C: Summary of observed frequencies of GABA release (TICs/min) at the indicated glucose concentrations (*P < 0.05). The measurements were made at steady state (1–5 min after addition of glucose). D: Tolbutamide (100 μmol/l) was applied as indicated (extracellular glucose concentration 4 mmol/l). E: SR-95531 (10 μmol/l) was applied as indicated at 1 mmol/l extracellular glucose.
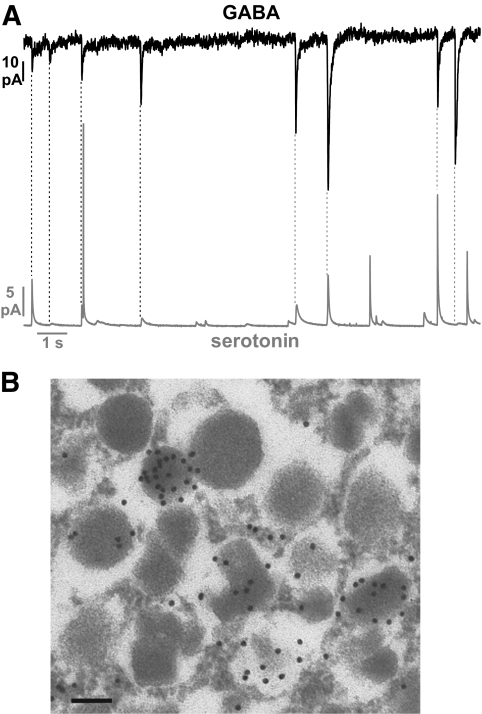
FIG. 5.
Storage and secretion of GABA by insulin-containing LDCVs in human β-cells. A: GABA release was detected by patch-clamping in an identified β-cell overexpressing α1/β1 GABAAR (upper trace). The cell was held at −70 mV and infused with intracellular solution containing 2 μmol/l free Ca2+. Serotonin release was measured simultaneously in the same cell by carbon fiber amperometry (lower trace). The dashed lines indicate simultaneous occurrence of GABA-induced TICs and amperometric currents. B: Immunogold labeling of GABA in a human β-cell. Scale bar: 250 nm.
Electrophysiology.
Patch pipettes were pulled from borosilicate glass and heat-polished (tip resistance 4–8 MΩ). Petri dishes were mounted onto an Axiovert 10 microscope (Zeiss, Jena, Germany) positioned on a vibration isolation table with a Faraday cage (TMC, Peabody, MA). Experiments were performed in the standard or perforated-patch whole-cell configuration using an EPC9 amplifier and Pulse software (HEKA, Lambrecht, Germany). All electrophysiological measurements were conducted at 32–33°C and cells were continuously superfused with extracellular medium. For rapid application of GABA (Figs. 1 and 7), a Nanoliter 2000 Oocyte Injector (WPI, Stevenage, U.K.) was used.
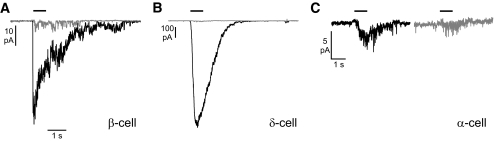
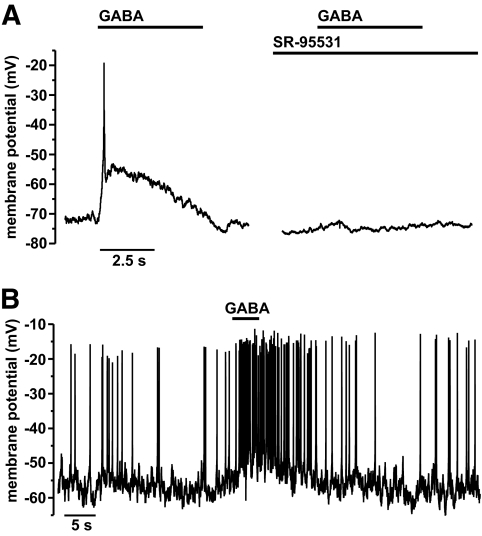
FIG. 1.
Functional detection of endogenous GABAAR Cl− channels in human islet cells. A: Patch-clamp recording of currents evoked by puffer application of GABA (1 mmol/l, as indicated by the bars) to an identified β-cell in the absence (black trace) and presence (gray trace) of 50 μmol/l SR-95531 in the same cell. The cell was held at −70 mV throughout the experiment. B: As in A, showing a δ-cell (note the difference in scale bars). C: As in A, showing an α-cell. The cell had been incubated in the presence of 0.5 μmol/l insulin for 1 h before the experiment.
FIG. 7.
Effects of GABA on the membrane potential of human β-cells. Membrane potential was recorded in noninfected cells in the perforated-patch configuration, using the Cl−-impermeable antibiotic gramicidin as the perforating agent. Recordings were made at 6 mmol/l extracellular glucose. A: Application of GABA (100 μmol/l, indicated by bars) to a β-cell in the absence (left) or presence (right) of 50 μmol/l SR-95531. B: Application of 10 μmol/l GABA (bar) to an electrically active β-cell.
The extracellular solution for measuring glucose- or tolbutamide-induced GABA release (Fig. 4) and membrane potential (Fig. 7) contained (in mmol/l) 138 NaCl, 5.6 KCl, 2.6 CaCl2, 1.2 MgCl2, 5 HEPES (pH 7.4, NaOH), and glucose at the indicated concentration. For detecting expression of endogenous GABA-activated currents (Fig. 1) and GABA-release elicited by Ca2+ infusion or voltage-clamp depolarizations in infected cells (Figs. 3 and 5), TEACl (20 mmol/l) was added and NaCl correspondingly reduced. In Fig. 1, the intracellular solution was composed of (in mmol/l) 120 CsCl, 1 MgCl2, 10 EGTA, 1 CaCl2, 10 HEPES, and 3 MgATP (pH 7.2, CsOH). In Fig. 4, CsCl was replaced equimolarly with KCl. The Ca2+ infusion experiments (Figs. 3A and 5A) were performed with pipette solution consisting of (in mmol/l) 110 CsCl, 10 KCl, 10 NaCl, 1 MgCl2, 3 MgATP, 0.1 cAMP, 5 HEPES, 9 CaCl2, and 10 EGTA (pH 7.15 with CsOH; free Ca2+ ∼2 μmol/l). Depolarization-evoked GABA release was recorded with intracellular medium containing (in mmol/l) 125 Cs-glutamate, 10 CsCl, 10 NaCl, 1 MgCl2, 5 HEPES, 50 μmol/l EGTA, 3 MgATP, and 0.1 cAMP (pH 7.15 with CsOH). The membrane potential measurements were performed with a pipette solution composed of (in mmol/l) 76 K2SO4, 10 KCl, 10 NaCl, 1 MgCl2, 5 HEPES, and 10–50 μg/ml gramicidin (pH adjusted to 7.35 with CsOH, osmolarity adjusted to ∼300 mOsm with sucrose). Biocytin (0.5 mg/ml) was sometimes added to the pipette solution to facilitate subsequent immunocytochemical identification.
Amperometry.
Cells were preloaded with serotonin by addition of 0.5 mmol/l 5-hydroxytryptophan and 0.5 mmol/l serotonin to the culture medium >6 h before the experiment. Serotonin release was detected using a carbon fiber electrode (ProCFE, Dagan Corporation, Minneapolis, MN) connected to the second head-stage of the EPC9/3 amplifier. The electrode was held at 650 mV and positioned ∼1 μm from the cell. Exocytosis was stimulated by infusion of cells with solution containing 2 μmol/l free Ca2+ via the patch electrode (see above), and whole-cell GABA-activated currents were measured in parallel from the same cell.
Immunocytochemistry.
De-paraffinized human pancreatic tissue sections (4 μm) were heated to 95°C in 10 mmol/l Tris + 1 mmol/l EDTA (pH 6) for 40 min, followed by incubation at 4°C for 10 min in the same buffer. Sections were then incubated with antibodies directed against GABAAR subunits α1–6 (1:50, H-300; Santa Cruz Biotechnology, Santa Cruz, CA), β2/3 (1:100, MAB341, Millipore, Hampshire, U.K.) or γ2 (1:100, LS-C14, Life span, Seattle, WA) dissolved in REAL antibody diluent (Dako, Cambridge, U.K.) at 4°C overnight. Endogenous peroxidases were blocked using methanol containing 1% H2O2 (15 min). A peroxidase-conjugated secondary antibody (Dako) was added for 30 min, followed by Alexa 488–labeled tyramide (Invitrogen) for 20 min. Co-staining for insulin, glucagon, somatostatin, or pancreatic polypeptide and visualization of fluorescence were performed as previously described (18).
Identification of the cell type after patch-clamp experiments was performed by immunodetection of insulin, glucagon, and somatostatin as described previously (19,20) (see the online appendix available at http://diabetes.diabetesjournals.org/cgi/content/full/db09-0797/DC1).
Hormone secretion measurements.
Batches of 10–20 islets (in triplicates) were preincubated in 1 ml Krebs-Ringer buffer containing 2 mg/ml BSA and supplemented with 1 mmol/l glucose for 1 h followed by a 1-h test incubation in 1 ml Krebs-Ringer buffer supplemented as indicated. The hormone content of the supernatant was measured by radioimmunoassay (insulin, glucagon: Millipore, Watford, U.K.; somatostatin: Euro-Diagnostica, Malmö, Sweden).
Quantitative RT-PCR.
Gene expression profiling of GABAAR subunits was performed by RT-qPCR on human islet total RNA as described previously (19) (see the online appendix).
Electron microscopy.
Isolated human islets were fixed in 2.5% glutaraldehyde in phosphate buffer, postfixed in 1% OsO4, dehydrated, and embedded in Spurr's resin. Ultrathin sections cut onto nickel grids were immunolabeled for GABA using a rabbit polyclonal antibody (1:1,000 dilution, Sigma) and protein A gold particles (15 nm, Biocell, Cardiff, U.K.). Sections were viewed with a Joel 1010 microscope (accelerating voltage 80 kV).
Data analysis.
All data are expressed as means ± SEM. Statistical significances were calculated using Student's t test. GABA-induced transient inward currents (TICs) and amperometric events were analyzed using MiniAnalysis software (Synaptosoft, Decatur, GA).
RESULTS
Expression of endogenous GABAAR Cl− channels in human islets.
Functional expression of endogenous GABAAR Cl− channels in human islet cells was investigated in patch-clamp experiments. Figure 1A shows a representative recording in which puffer application of GABA to a β-cell triggered a rapidly activating and desensitizing inward current that was sensitive to the GABAAR antagonist SR-95531. GABA-activated currents were found in 26 of 50 β-cells (52%), and the current amplitude in receptor-positive cells averaged 64 ± 20 pA (current density 9.4 ± 2.1 pA/pF). The GABA-evoked current was decreased by 78 ± 2% in the presence of SR-95531 (from 32 ± 5 to 7 ± 2 pA, P < 0.01, n = 8). GABA application also elicited inward currents in 31 out of 34 δ-cells (91%), but the responses were typically much larger than in β-cells (Fig. 1B). On average, the GABA-evoked currents had an amplitude of 668 ± 188 pA (148 ± 42 pA/pF, n = 31), which was reduced by 75 ± 6% (from 570 ± 330 to 33 ± 8 pA, P < 0.01, n = 10) in the presence of SR-95531. By contrast, GABA application triggered inward currents in only 3 out of 48 α-cells (6%; Fig. 1C), with the current amplitude in these cells averaging 7 ± 3 pA (current density 2 pA/pF). Insulin has been reported to translocate GABAAR to the cell surface in α-cells (8). In α-cells that had been preincubated with insulin (0.5 μmol/l for 1 h in the culture medium), application of GABA in the continued presence of insulin (0.1 μmol/l) elicited inward currents in 3 out of 19 cells tested (16%), but the current amplitude was not increased and averaged 4.3 ± 0.6 pA/pF in these three cells. As shown in Fig. 1C, SR95531 reduced the GABA-activated current in α-cells by 70% (n = 2). Of the 64 cells analyzed in which GABA evoked a measurable current, only one cell did not contain insulin, glucagon, or somatostatin, and this cell was not positive for pancreatic polypeptide (not shown).
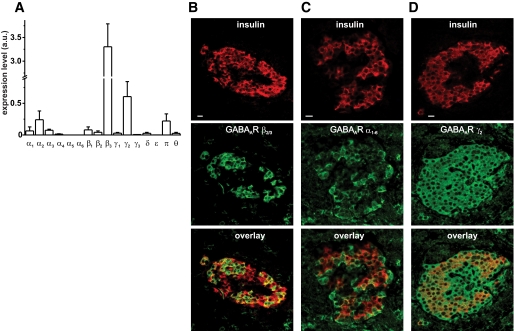
Expression of GABAAR subunits in human islets was investigated by quantitative RT-PCR. Among the α- and β-subunits, α2 and β3 predominated. Fairly high levels of the γ2 and π were also observed. In addition, low levels of α1, α3, α4, β1, β2, γ1, and θ were detected (Fig. 2A).
FIG. 2.
Expression of GABAAR subunits in human islets. A: Expression profiling of GABAAR subunits in islets by quantitative RT-PCR (n = 3 preparations from three donors). B–D: Co-labeling of pancreatic tissue sections with anti-insulin and anti-GABAAR β2/3 (B), anti-GABAAR α1–6 (C), or anti-GABAAR γ2 (D). Insulin is shown in red and GABAAR subunits in green; co-localization results in yellow labeling (scale bars = 10 μm). a.u., arbitrary units.
Expression of GABAAR subunits in human islets was confirmed by immunohistochemistry. An antibody against the β2/3 subunit labeled ∼50% of the β-cells in pancreatic tissue sections (Fig. 2B); no staining of α-cells, δ-cells, or PP-cells was observed (supplementary Fig. 1, available in the online appendix). An α1–6–specific antibody stained 22% of the β-cells (Fig. 2C), 94% of the δ-cells, and 14% of the α-cells (supplementary Fig. 1). Finally, an antibody directed against the γ2 subunit labeled β-cells (Fig. 2D) as well as α- and δ-cells (supplementary Fig. 1). No specific labeling of human pancreatic sections was observed with an antibody against β1 subunits (not shown).
GABA release from human β-cells.
To determine if GABA is released from human β-cells, a patch-clamp–based assay was used (17). Briefly, GABAARs were overexpressed in isolated β-cells using adenoviral vectors encoding the GABAAR α1 and β1 subunits, respectively. GABA released upon fusion of GABA-containing secretory vesicles activates these receptors in the same cell, giving rise to transient inward currents (TICs). Figure 3A shows a recording from a cell held at −70 mV, in which exocytosis was stimulated by inclusion of 2 μmol/l free Ca2+ in the intracellular solution. The trace displays numerous TICs that were sensitive to the GABAAR blockers SR-95531 (10 μmol/l; n = 4) and bicuculline (100 μmol/l; n = 2; not shown), demonstrating that they reflect activation of GABAAR. The TICs had an average rise time (10–90%) of 14 ± 1 ms and a half-width of 40 ± 2 ms (n = 274 events from four cells). These values are comparable to those reported in rat β-cells (17).
Quantal release of GABA could be elicited by voltage-clamp depolarizations from −70 to 0 mV (Fig. 3B). Depolarization-evoked transient currents were outward because the experiments were conducted at low [Cl−]i (22 mmol/l). Thus, the Cl− equilibrium potential (ECl) is approximately −50 mV, resulting in a net inward driving force at 0 mV for Cl− ions.
GABA release was also observed in δ-cells stimulated by Ca2+ infusion or voltage-clamp depolarizations (supplementary Fig. 2A). As δ-cells express high levels of endogenous GABAAR, GABA-induced TICs were sometimes (three cells) seen even in noninfected cells (supplementary Fig. 2B).
Glucose-induced GABA release.
Figure 3B demonstrated that GABA is released from β-cells in response to depolarization-induced Ca2+ influx via voltage-gated Ca2+ channels. We went on to investigate whether glucose, via membrane depolarization, can evoke GABA release. These experiments were performed on clusters of islet cells overexpressing α1/β1 GABAAR. The membrane potential of the patch-clamped cell was held at −70 mV and its cytoplasm infused with a buffer containing 10 mmol/l EGTA. These steps prevent exocytosis in the patch-clamped cell, and it will therefore serve as a sensor (“sniffer-cell”) for GABA released from neighboring cells within the cluster. TICs evoked by GABA release were rarely observed at 1 mmol/l extracellular glucose, but increasing the glucose concentration to 6 or 20 mmol/l increased the frequency of TICs after a delay of 1–2 min (Fig. 4A–C). The glucose-induced TICs were sensitive to SR-95531 (Fig. 4B), confirming that they reflect GABA release and activation of GABAAR. When they occurred, the TICs tended to occur in bursts (Fig. 4B, ii).
GABA release was likewise stimulated by addition of the ATP-sensitive K+ (KATP) channel blocker tolbutamide (100 μmol/l) to the extracellular solution (Fig. 4D; n = 4) and inhibited by the KATP channel opener diazoxide (n = 4, supplementary Fig. 3). The change in holding current in Fig. 4D probably reflects closure of KATP channels that remain active in the patch-clamped cells despite the presence of 3 mmol/l ATP in the intracellular solution. By contrast, glucose stimulation did not consistently affect the holding current.
In cell clusters overexpressing α1/β1 GABAAR, addition of SR-95531 reduced both the holding current and current noise even at low (1 mmol/l) extracellular glucose, in the absence of observable TICs (Fig. 4E). In a series of seven experiments, SR-95531 decreased the holding current from −47 ± 15 to −36 ± 15 pA (P < 0.05) and the current variance from 9.8 ± 2.7 × 10−24 A2 to 4.1 ± 1.8 × 10−24 A2 (P < 0.05). From the excess noise (sensitive to SR-95531), we estimate the size of the unitary event as ∼0.5 pA, corresponding to a single-channel conductance of 7 pS. This is in reasonable agreement with the 10–15 pS reported for recombinant α1β1 GABAAR Cl− channels (21).
Subcellular localization of GABA in human β-cells.
GABA and GAD65 have been reported to be associated with synaptic-like microvesicles in rodent β-cells (22). However, we have recently presented evidence for release of GABA from insulin-containing large dense-core vesicles (LDCV) in rat β-cells (23). To determine whether vesicular GABA secretion from human β-cells reflects exocytosis of insulin-containing granules, we combined the patch-clamp–based assay for GABA release with amperometric detection of serotonin, assumed to accumulate in LDCVs (24–27). As shown in Fig. 5A, the transient currents induced by vesicular release of GABA (top) and serotonin (bottom) occurred simultaneously in most cases. In this experiment, 90 out of 165 GABAergic TICs were accompanied by a simultaneous amperometric spike. In a series of four experiments, co-release of serotonin was detected for 44 ± 9% of the GABA-release events. This suggests that GABA and serotonin are released by exocytosis of the same vesicles; the correlation is <100% because amperometry only detects exocytotic events occurring in the vicinity of the carbon fiber (usually <50%), whereas GABA release is detectable over the entire cell surface (23). Close inspection of the records indicated that GABA may also be released during the “pedestals” that precede full fusion and during kiss-and-run exocytosis (supplementary Fig. 4).
Not all amperometric events were accompanied by simultaneous release of GABA (Fig. 5A). Indeed, only 13 ± 3% (n = 4) of the amperometric events were associated with GABA-evoked TICs, suggesting that GABA is only present in a subpopulation of insulin granules. This was verified by immunogold electron microscopy using a GABA-specific antibody. Some insulin granules were strongly labeled with gold particles, whereas other granules were not stained at all (Fig. 5B). This finding is in agreement with previous results from rat β-cells (23). Immunogold electron micrographs confirmed that non–β-cells (including δ-cells) contain GABA at levels 50–70% of those detected in β-cells (supplementary Fig. 5).
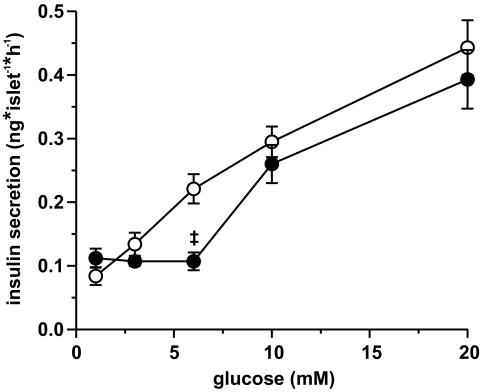
Effect of GABAAR blockade on insulin secretion.
In intact human islets, glucose at a concentration as low as 3 mmol/l stimulated insulin secretion above that seen at 1 mmol/l glucose. At higher glucose concentrations, there was a concentration-dependent further stimulation of insulin release (Fig. 6). The GABAAR antagonist SR-95531 had no effect on basal insulin release but inhibited insulin release at 6 mmol/l glucose. No (statistically) significant inhibition of insulin secretion was observed at 3, 10, or 20 mmol/l glucose.
FIG. 6.
Effect of GABAAR blockade on insulin secretion from isolated human islets. Insulin secretion was measured at 1, 3, 6, 10, or 20 mmol/l extracellular glucose in the absence (○) or presence (●) of SR-95531 (10 μmol/l) as indicated (n = 9–12 from four donors; ‡P < 0.001 for the effect of SR-95531). Under control conditions insulin release at all glucose concentrations was significantly different from the previous lower glucose concentration (not indicated). The results at 1, 6, and 20 mmol/l glucose were repeated with islets from seven different donors with the same results.
Somatostatin secretion was stimulated by elevation of the glucose concentration to ≥3 mmol/l (supplementary Fig. 6A). Glucagon secretion was suppressed when the glucose level in the medium was raised from 1 to ≥3 mmol/l (supplementary Fig. 6B). Inhibition was maximal at 6 mmol/l glucose and gradually reduced at higher concentrations (28). SR95531 had complex and glucose-dependent effects on glucagon and somatostatin secretion.
Effect of endogenous GABAAR activation on islet cell membrane potential.
The effect of activation of endogenous GABAARs on the membrane potential of islet cells was studied in noninfected cells using the perforated-patch whole-cell configuration. To maintain normal [Cl−]i, the Cl−-impermeable antibiotic gramicidin was used as the perforating agent (29). Figure 7A shows a β-cell exposed to 6 mmol/l glucose that was not electrically active. We point out that insulin secretion at 6 mmol/l is only ∼40% of that evoked by 20 mmol/l glucose. The finding that some β-cells are not electrically active at the lower glucose concentration indicates that the concentration-dependent stimulation of insulin secretion involves recruitment of β-cells that were previously not active. Application of GABA depolarized the cell to approximately −55 mV. This effect was blocked by the GABAAR antagonist SR-95531. On average, puffer application of GABA depolarized β-cells from −64 ± 7 to −43 ± 4 mV (n = 4). Assuming that the membrane potential in the presence of GABA approximates ECl, [Cl−]i can be estimated to be 32 ± 5 mmol/l (ECl = −60 · log[Cl−]o/[Cl−]i). GABA, when applied at the high concentration used in Fig. 7A (100 μmol/l), typically triggered single action potentials. This we attribute to the large Cl− conductance, which effectively clamps the membrane potential to ECl and thus prevents regenerative electrical activity. When a lower GABA concentration (10 μmol/l) was applied to a β-cell that was electrically active at 6 mmol/l glucose (Fig. 7B), a smaller membrane depolarization accompanied by increased action potential firing was observed. In a series of five experiments, 10 μmol/l GABA increased β-cell action potential frequency approximately fivefold, from 0.6 ± 0.2 to 2.9 ± 0.4 Hz (P < 0.05).
Puffer application of GABA also depolarized the membrane potential of δ-cells (supplementary Fig. 7). In a series of four experiments, the δ-cell membrane potential averaged −28 ± 5 mV after application of 100 μmol/l GABA, corresponding to a [Cl−]i of 54 ± 9 mmol/l. The membrane potential of α-cells was not affected by GABA, reflecting the low GABAAR density in these cells (not shown).
DISCUSSION
Human pancreatic islets contain concentrations of GABA similar to those found in the brain (30), but the physiological function of pancreatic islet GABA in humans remains poorly defined. Here we have investigated the role of GABA and GABAAR Cl− channels in paracrine and autocrine signaling in human pancreatic islets.
Blocking GABAARs inhibited insulin secretion from human islets induced by 6 mmol/l glucose, i.e., close to the concentration at half-maximal stimulation (EC50) for glucose-stimulated insulin secretion (31). These findings imply that GABA, by activating GABAAR, stimulates β-cell secretion. This may seem paradoxical, since GABA is best known as an “inhibitory neurotransmitter.” GABAARs are ligand-gated Cl− channels, and opening of these channels shifts the cell's membrane potential toward ECl. The effect of GABA will accordingly depend on the membrane potential of the cell and [Cl−]i. Our measurements of ECl indicate that [Cl−]i in human β-cells is ∼32 mmol/l. This value is in close agreement with that measured in mouse β-cells using a Cl−-sensitive fluorescent indicator (34 mmol/l [32]). Assuming a plasma Cl− concentration of 110 mmol/l, ECl in β-cells is greater than −40 mV and thereby positive to the threshold for action potential firing in human β-cells (−55 mV [19]). For comparison, [Cl−]i in neurons is <10 mmol/l, resulting in an ECl more negative than −60 mV (33), whereas it will produce depolarization in β-cells exposed to nonstimulatory glucose concentrations. A stimulatory role for Cl− conductances in β-cells is also supported by the observation that a reduction of [Cl−]i below physiological levels suppresses glucose-induced electrical activity in mouse β-cells (34). A positive GABAergic feedback loop may account for bursts of TICs observed during glucose stimulation (Fig. 4B, ii): the release of one GABA-containing vesicle will depolarize the β-cell and this in turn (via stimulation of electrical activity) triggers the release of further vesicles. Desensitization of GABAARs eventually terminates the burst.
GABAAR inhibition reduced insulin secretion at 6 but not 10 and 20 mmol/l glucose. This is similar to results obtained in INS-1 cells where GABA stimulates insulin secretion at 2.8 mmol/l glucose but is inhibitory at 28 mmol/l glucose (35). These divergent effects of GABA can be explained if increasing glucose concentrations lead to a progressive depolarization of the β-cell membrane potential (36,37). At high glucose levels, when the membrane potential approaches ECl, opening of Cl− channels may have no further depolarizing effect and even reduce excitability (by clamping the membrane potential to ECl).
It has previously been demonstrated that glucose regulates GABAergic signaling in islets by increasing GABAAR subunit expression (6) and via insulin-induced trafficking of GABAARs to the cell surface (8). Here we provide the important additional observation that glucose stimulates vesicular release of GABA from β-cells (Fig. 4C). GABA was co-released with the LDCV marker serotonin, and electron microscopy demonstrated accumulation of GABA in a subpopulation of insulin granules. This is in agreement with similar observations in rat β-cells (23). The findings suggest that vesicular GABA release in human β-cells is principally due to exocytosis of insulin-containing LDCVs, although a contribution of synaptic-like microvesicle exocytosis cannot be excluded (22).
Rat β-cells release 25% of their GABA content per hour independently of the glucose concentration (38). This cannot be explained by release of GABA solely by exocytosis of LDCVs. Indeed, in cell clusters overexpressing GABAAR, SR-95531 blocked a component of the holding current at 1 mmol/l glucose, indicating extracellular accumulation of GABA in the absence of detectable vesicular GABA release (23). Here we demonstrate that this also occurs in human β-cells. These data suggest that in addition to the glucose-dependent vesicular route of GABA release, a tonic glucose-independent background release mechanism exists in β-cells. Analysis of the excess noise (blockable by SR-95531) suggests that background release of GABA is only sufficient to activate individual channels. This indicates that background release of GABA is of a nonvesicular nature, the details of which remain to be elucidated but may involve GABA transporters operating in reverse or other nonvesicular routes (39).
Patch-clamp experiments revealed that human δ-cells express high levels of GABAAR and that activation of these receptors—similar to what was observed in β-cells—depolarizes δ-cell membrane potential. In line with an excitatory effect of GABAAR activation, blocking GABAAR reduced somatostatin secretion at 3 and 20 mmol/l but not at 10 mmol/l glucose. In agreement with the study of Xu et al. (8), the GABAAR antagonist SR95531 also modulated glucagon secretion from human islets. The fact that so few isolated α-cells exhibited GABA-activated currents may suggest that the effects on glucagon secretion are principally mediated by paracrine effects. It should be noted, however, that 14% of the α-cells in intact islets contained detectable α1–6 subunit immunoreactivity. This is similar to the 16% obtained by electrophysiological analysis of α-cells preincubated in the presence of insulin and only slightly lower than the 22% observed in β-cells. Thus, it is possible that the expression of GABAARs in isolated α-cells is artifactually low because of the loss of intra-islet insulin signaling. In control experiments, we did not find any evidence that SR-95531 interferes nonspecifically with voltage-gated channels and electrical activity in islet cells. More work is needed to explain the effects of SR-95531 on glucagon and somatostatin secretion.
In summary, our data suggest that signaling via GABA and GABAAR stimulates insulin secretion by a positive autocrine feedback loop in human β-cells. Many important pharmacological agents target GABAAR, and it is possible that they, given the presence of GABAAR in β-cells, also affect insulin secretion from pancreatic islets. Indeed, treatment of epileptic patients with the anticonvulsant valproic acid (which blocks the degradation of GABA) has been reported to result in increased postprandial insulin levels (40).
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Medical Research Council (MRC), the Wellcome Trust, the European Union (Biosim [LSHB-CT-2004-005137] and Eurodia [SHM-CT-2006-518153]), and the Department of Health (NIHR Biomedical Research Centre's funding scheme).
No potential conflicts of interest relevant to this article were reported.
M.Br. researched data and wrote the manuscript; R.R., M.Be., A.C., and N.W. researched data; and P.R.J. and P.R. contributed to discussion and reviewed/edited the manuscript.
We thank Dr. S. Hughes, Dr. D. Gray, and Dr. S. Cross for isolation of human islets and D. Wiggins for assistance with hormone release measurements.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Samols E, Bonner-Weir S, Weir GC: Intra-islet insulin-glucagon-somatostatin relationships. Clin Endocrinol Metab 1986;15:33–58 [DOI] [PubMed] [Google Scholar]
- 2.Grapengiesser E, Salehi A, Qader SS, Hellman B: Glucose induces glucagon release pulses antisynchronous with insulin and sensitive to purinoceptor inhibition. Endocrinology 2006;147:3472–3477 [DOI] [PubMed] [Google Scholar]
- 3.Hayashi M, Yamada H, Uehara S, Morimoto R, Muroyama A, Yatsushiro S, Takeda J, Yamamoto A, Moriyama Y: Secretory granule-mediated co-secretion of L-glutamate and glucagon triggers glutamatergic signal transmission in islets of Langerhans. J Biol Chem 2003;278:1966–1974 [DOI] [PubMed] [Google Scholar]
- 4.Ishihara H, Maechler P, Gjinovci A, Herrera PL, Wollheim CB: Islet beta-cell secretion determines glucagon release from neighbouring alpha-cells. Nat Cell Biol 2003;5:330–335 [DOI] [PubMed] [Google Scholar]
- 5.Rorsman P, Berggren PO, Bokvist K, Ericson H, Möhler H, Ostenson CG, Smith PA: Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Nature 1989;341:233–236 [DOI] [PubMed] [Google Scholar]
- 6.Bailey SJ, Ravier MA, Rutter GA: Glucose-dependent regulation of gamma-aminobutyric acid (GABA A) receptor expression in mouse pancreatic islet alpha-cells. Diabetes 2007;56:320–327 [DOI] [PubMed] [Google Scholar]
- 7.Wendt A, Birnir B, Buschard K, Gromada J, Salehi A, Sewing S, Rorsman P, Braun M: Glucose inhibition of glucagon secretion from rat alpha-cells is mediated by GABA released from neighboring beta-cells. Diabetes 2004;53:1038–1045 [DOI] [PubMed] [Google Scholar]
- 8.Xu E, Kumar M, Zhang Y, Ju W, Obata T, Zhang N, Liu S, Wendt A, Deng S, Ebina Y, Wheeler MB, Braun M, Wang Q: Intra-islet insulin suppresses glucagon release via GABA-GABAA receptor system. Cell Metab 2006;3:47–58 [DOI] [PubMed] [Google Scholar]
- 9.Brissova M, Fowler MJ, Nicholson WE, Chu A, Hirshberg B, Harlan DM, Powers AC: Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy. J Histochem Cytochem 2005;53:1087–1097 [DOI] [PubMed] [Google Scholar]
- 10.Cabrera O, Berman DM, Kenyon NS, Ricordi C, Berggren PO, Caicedo A: The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Proc Natl Acad Sci U S A 2006;103:2334–2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taniguchi H, Okada Y, Seguchi H, Shimada C, Seki M, Tsutou A, Baba S: High concentration of gamma-aminobutyric acid in pancreatic beta cells. Diabetes 1979;28:629–633 [DOI] [PubMed] [Google Scholar]
- 12.Wang C, Ling Z, Pipeleers D: Comparison of cellular and medium insulin and GABA content as markers for living beta-cells. Am J Physiol Endocrinol Metab 2005;288:E307–E313 [DOI] [PubMed] [Google Scholar]
- 13.Yang W, Reyes AA, Lan NC: Identification of the GABAA receptor subtype mRNA in human pancreatic tissue. FEBS Lett 1994;346:257–262 [DOI] [PubMed] [Google Scholar]
- 14.Lake SP, Bassett PD, Larkins A, Revell J, Walczak K, Chamberlain J, Rumford GM, London NJ, Veitch PS, Bell PR, et al. : Large-scale purification of human islets utilizing discontinuous albumin gradient on IBM 2991 cell separator. Diabetes 1989;38(Suppl. 1):143–145 [DOI] [PubMed] [Google Scholar]
- 15.Ricordi C, Lacy PE, Finke EH, Olack BJ, Scharp DW: Automated method for isolation of human pancreatic islets. Diabetes 1988;37:413–420 [DOI] [PubMed] [Google Scholar]
- 16.Lernmark A: The preparation of, and studies on, free cell suspensions from mouse pancreatic islets. Diabetologia 1974;10:431–438 [DOI] [PubMed] [Google Scholar]
- 17.Braun M, Wendt A, Birnir B, Broman J, Eliasson L, Galvanovskis J, Gromada J, Mulder H, Rorsman P: Regulated exocytosis of GABA-containing synaptic-like microvesicles in pancreatic beta-cells. J Gen Physiol 2004;123:191–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braun M, Ramracheya R, Amisten S, Bengtsson M, Moritoh Y, Zhang Q, Johnson PR, Rorsman P: Somatostatin release, electrical activity, membrane currents and exocytosis in human pancreatic delta cells. Diabetologia 2009;52:1566–1578 [DOI] [PubMed] [Google Scholar]
- 19.Braun M, Ramracheya R, Bengtsson M, Zhang Q, Karanauskaite J, Partridge C, Johnson PR, Rorsman P: Voltage-gated ion channels in human pancreatic beta-cells: electrophysiological characterization and role in insulin secretion. Diabetes 2008;57:1618–1628 [DOI] [PubMed] [Google Scholar]
- 20.Zhang Q, Bengtsson M, Partridge C, Salehi A, Braun M, Cox R, Eliasson L, Johnson PR, Renström E, Schneider T, Berggren PO, Göpel S, Ashcroft FM, Rorsman P: R-type Ca(2+)-channel-evoked CICR regulates glucose-induced somatostatin secretion. Nat Cell Biol 2007;9:453–460 [DOI] [PubMed] [Google Scholar]
- 21.Angelotti TP, Macdonald RL: Assembly of GABAA receptor subunits: alpha 1 beta 1 and alpha 1 beta 1 gamma 2S subunits produce unique ion channels with dissimilar single-channel properties. J Neurosci 1993;13:1429–1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reetz A, Solimena M, Matteoli M, Folli F, Takei K, De Camilli P: GABA and pancreatic beta-cells: colocalization of glutamic acid decarboxylase (GAD) and GABA with synaptic-like microvesicles suggests their role in GABA storage and secretion. EMBO J 1991;10:1275–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braun M, Wendt A, Karanauskaite J, Galvanovskis J, Clark A, MacDonald PE, Rorsman P: Corelease and differential exit via the fusion pore of GABA, serotonin, and ATP from LDCV in rat pancreatic beta cells. J Gen Physiol 2007;129:221–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aspinwall CA, Huang L, Lakey JR, Kennedy RT: Comparison of amperometric methods for detection of exocytosis from single pancreatic beta-cells of different species. Anal Chem 1999;71:5551–5556 [DOI] [PubMed] [Google Scholar]
- 25.Finnegan JM, Pihel K, Cahill PS, Huang L, Zerby SE, Ewing AG, Kennedy RT, Wightman RM: Vesicular quantal size measured by amperometry at chromaffin, mast, pheochromocytoma, and pancreatic beta-cells. J Neurochem 1996;66:1914–1923 [DOI] [PubMed] [Google Scholar]
- 26.Gylfe E: Association between 5-hydroxytryptamine release and insulin secretion. J Endocrinol 1978;78:239–248 [DOI] [PubMed] [Google Scholar]
- 27.Takahashi N, Kadowaki T, Yazaki Y, Miyashita Y, Kasai H: Multiple exocytotic pathways in pancreatic beta cells. J Cell Biol 1997;138:55–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salehi A, Vieira E, Gylfe E: Paradoxical stimulation of glucagon secretion by high glucose concentrations. Diabetes 2006;55:2318–2323 [DOI] [PubMed] [Google Scholar]
- 29.Rhee JS, Ebihara S, Akaike N: Gramicidin perforated patch-clamp technique reveals glycine-gated outward chloride current in dissociated nucleus solitarii neurons of the rat. J Neurophysiol 1994;72:1103–1108 [DOI] [PubMed] [Google Scholar]
- 30.Michalik M, Erecińska M: GABA in pancreatic islets: metabolism and function. Biochem Pharmacol 1992;44:1–9 [DOI] [PubMed] [Google Scholar]
- 31.Henquin JC, Dufrane D, Nenquin M: Nutrient control of insulin secretion in isolated normal human islets. Diabetes 2006;55:3470–3477 [DOI] [PubMed] [Google Scholar]
- 32.Eberhardson M, Patterson S, Grapengiesser E: Microfluorometric analysis of Cl- permeability and its relation to oscillatory Ca2+ signalling in glucose-stimulated pancreatic beta-cells. Cell Signal 2000;12:781–786 [DOI] [PubMed] [Google Scholar]
- 33.Ben-Ari Y: Excitatory actions of gaba during development: the nature of the nurture. Nat Rev Neurosci 2002;3:728–739 [DOI] [PubMed] [Google Scholar]
- 34.Best L: Glucose-induced electrical activity in rat pancreatic beta-cells: dependence on intracellular chloride concentration. J Physiol 2005;568:137–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dong H, Kumar M, Zhang Y, Gyulkhandanyan A, Xiang YY, Ye B, Perrella J, Hyder A, Zhang N, Wheeler M, Lu WY, Wang Q: Gamma-aminobutyric acid up- and downregulates insulin secretion from beta cells in concert with changes in glucose concentration. Diabetologia 2006;49:697–705 [DOI] [PubMed] [Google Scholar]
- 36.Barnett DW, Pressel DM, Misler S: Voltage-dependent Na+ and Ca2+ currents in human pancreatic islet beta-cells: evidence for roles in the generation of action potentials and insulin secretion. Pflugers Arch 1995;431:272–282 [DOI] [PubMed] [Google Scholar]
- 37.Misler S, Barnett DW, Gillis KD, Pressel DM: Electrophysiology of stimulus-secretion coupling in human beta-cells. Diabetes 1992;41:1221–1228 [DOI] [PubMed] [Google Scholar]
- 38.Smismans A, Schuit F, Pipeleers D: Nutrient regulation of gamma-aminobutyric acid release from islet beta cells. Diabetologia 1997;40:1411–1415 [DOI] [PubMed] [Google Scholar]
- 39.Semyanov A, Walker MC, Kullmann DM, Silver RA: Tonically active GABA A receptors: modulating gain and maintaining the tone. Trends Neurosci 2004;27:262–269 [DOI] [PubMed] [Google Scholar]
- 40.Luef G, Abraham I, Hoppichler F, Trinka E, Unterberger I, Bauer G, Lechleitner M: Increase in postprandial serum insulin levels in epileptic patients with valproic acid therapy. Metabolism 2002;51:1274–1278 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.