Abstract
OBJECTIVE
Individuals with type 1 diabetes have a less atherogenic fasting lipid profile than those without diabetes but paradoxically have increased rates of cardiovascular disease (CVD). We investigated differences in lipoprotein subfraction cholesterol distribution and insulin resistance between subjects with and without type 1 diabetes to better understand the etiology of increased CVD risk.
RESEARCH DESIGN AND METHODS
Fast protein liquid chromatography was used to fractionate lipoprotein cholesterol distribution in a substudy of the Coronary Artery Calcification in Type 1 Diabetes (CACTI) study (n = 82, age 46 ± 8 years, 52% female, 49% with type 1 diabetes for 23 ± 8 years). Insulin resistance was assessed by a hyperinsulinemic-euglycemic clamp.
RESULTS
Among men, those with type 1 diabetes had less VLDL and more HDL cholesterol than control subjects (P < 0.05), but among women, those with diabetes had a shift in cholesterol to denser LDL, despite more statin use. Among control subjects, men had more cholesterol distributed as VLDL and LDL but less as HDL than women; however, among those with type 1 diabetes, there was no sex difference. Within sex and diabetes strata, a more atherogenic cholesterol distribution by insulin resistance was seen in men with and without diabetes, but only in women with type 1 diabetes.
CONCLUSIONS
The expected sex-based less atherogenic lipoprotein cholesterol distribution was not seen in women with type 1 diabetes. Moreover, insulin resistance was associated with a more atherogenic lipoprotein cholesterol distribution in all men and in women with type 1 diabetes. This lipoprotein cholesterol distribution may contribute to sex-based differences in CVD in type 1 diabetes.
Cardiovascular disease (CVD) is the major cause of mortality in type 1 diabetes, and, in addition to glycemic control and blood pressure, dyslipidemia is an important and modifiable CVD risk factor (1–8). Curiously, despite higher rates of CVD in type 1 diabetes, including a relative loss of sex protection in women with type 1 diabetes (9–11), and the role of dyslipidemia as a determinant of CVD (8), individuals with type 1 diabetes have similar or less atherogenic lipid profiles than age-, sex-, and BMI-matched nondiabetic subjects (5,12). This paradox is well known (13), but few data exist to explain this phenomenon. Lipoprotein differences in type 1 diabetes have been investigated in the Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) study but lack a nondiabetic comparison group (14–17).
Furthermore, it has been known for nearly 40 years that insulin resistance is a prominent CVD risk factor in type 1 diabetes (18,19), and recent studies have demonstrated increased insulin resistance in people with type 1 diabetes compared with age-, sex-, and BMI-matched nondiabetic control subjects (20,21). The hyperinsulinemic-euglycemic clamp is considered the “gold standard” method for measuring insulin resistance in a wide variety of circumstances (22), especially in individuals with type 1 diabetes, in whom prediction models of insulin resistance that rely on glucose and insulin levels cannot be used. The effect of insulin resistance on lipoproteins has been investigated in individuals with type 2 diabetes and in those without diabetes (23–25), but to our knowledge, the effect of insulin resistance on lipoproteins has not been investigated in individuals with type 1 diabetes.
Therefore, to examine beyond the ability of the standard fasting lipid profile to assess CVD risk, we investigated differences in lipoprotein subfraction cholesterol distribution between subjects with and without type 1 diabetes and how insulin resistance affects this distribution. We hypothesized that differences would exist in lipoprotein subfraction cholesterol distribution by type 1 diabetes status, and, furthermore, we hypothesized that subjects with more insulin resistance as measured by a hyperinsulinemic-euglycemic clamp would have a more atherogenic lipoprotein subfraction cholesterol distribution.
RESEARCH DESIGN AND METHODS
Subjects were recruited from the Coronary Artery Calcification in Type 1 Diabetes (CACTI) study cohort for a hyperinsulinemic-euglycemic clamp substudy. Inclusion criteria for initial enrollment of type 1 diabetic subjects in the CACTI study were age 19–56 years, no history of coronary artery disease (CAD), receiving insulin therapy within 1 year of diagnosis and current insulin therapy, diagnosis before age 30 years, and diabetes duration ≥10 years (4). Nondiabetic control subjects were recruited from friends and spouses and were of similar age and had no history of CAD. We present data from 82 subjects (40 type 1 diabetic and 42 nondiabetic control subjects) recruited between 2005 and 2008 who underwent a hyperinsulinemic-euglycemic clamp after their 6-year CACTI follow-up visit. Inclusion criteria for the clamp substudy included A1C ≤9.5%, albumin excretion rate <200 μg/min, and triglycerides <400 mg/dl. Reported physical activity and computed tomographic measures of visceral fat from the third CACTI visit (2005–2008) are presented (26). Subjects in the clamp study were similar in age, BMI, visceral fat, and physical activity to subjects in the full cohort seen at the third CACTI visit within sex and diabetes strata. All participants provided informed consent, and the study was approved by the Colorado Combined Institutional Review Board.
Hyperinsulinemic-euglycemic clamp visit.
Subjects were maintained for 3 days before their study day on a provided diet with standardized macronutrient composition (50% carbohydrate, 20% protein, and 30% fat) and were asked to refrain from vigorous physical activity. Computed tomography dual-energy X-ray absorptiometry scans for body composition measures were performed. Subjects were admitted to the inpatient clinical research unit before a standard dinner the evening before their clamp. Women who were premenopausal were scheduled to have their clamp performed between days 2 and 10 of the menstrual cycle. Type 1 diabetic subjects were instructed to take their last long-acting insulin injections at least 12 h before admission. A standard dinner was provided on the unit, and subjects then fasted overnight and through the clamp protocol. Type 1 diabetic subjects received their rapid-acting insulin for dinner per their usual regimen. All type 1 diabetic subjects were maintained overnight on intravenous regular insulin with adjustments by a standard protocol to maintain near euglycemia until starting the clamp in the morning. Blood samples for determination of baseline hormone and substrate concentrations (insulin, glucose, C-peptide, free fatty acid, glycerol, and lactate) were drawn over the final 30 min before initiation of the clamp protocol. A three-stage hyperinsulinemic-euglycemic clamp was then initiated and continued for the next 4.5 h using the method of DeFronzo et al. (22). Briefly, a primed continuous infusion of insulin was administered at 4 mU/m2/min for 1.5 h, 8 mU/m2/min for 1.5 h, and then 40 mU/m2/min for the final 1.5 h. A variable amount of 20% dextrose was infused to maintain blood glucose ∼90 mg/dl. Arterialized blood was sampled every 5 min for bedside determination of glucose concentration (Analox, Lunenburg, MA), and the dextrose infusion was adjusted as necessary. Arterialized blood samples were taken twice during the last 10 min of each stage of the clamp for hormone and substrate measurements as above. A hyperinsulinemic-euglycemic steady state was achieved in the final 30 min of the clamp, and the glucose infusion rate (milligrams per kilogram per minute) was measured and is presented in these data as milligrams per kilogram fat-free mass (FFM) per minute. Fasting plasma samples obtained before initiation of the clamp were stored at −80°C and then thawed immediately before fast protein liquid chromatography (FPLC) analysis in all subjects in the clamp study who had available samples.
Lipoprotein analysis.
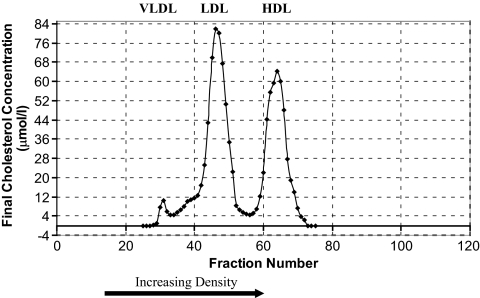
Individual subject's EDTA plasma samples (250 μl) were chromatographed using two Superose 6 columns in series (27), and 51 0.5-ml fractions were collected. Cholesterol was measured in each fraction using a commercially available kit (Cayman Chemical Company, Ann Arbor, MI) following procedures outlined in the package insert. An example of an individual FPLC lipoprotein subfraction cholesterol distribution profile with fractions labeled as VLDL, LDL, and HDL (increasing density from left to right) is shown in Fig. 1.
FIG. 1.
FPLC lipoprotein cholesterol distribution in a 49-year-old nondiabetic woman with a fasting lipid panel total cholesterol of 152 μmol/l, LDL cholesterol of 84 μmol/l, HDL cholesterol of 53, and triglycerides of 74 μmol/l and not on statin therapy.
Statistical analyses.
Variables were examined for normality and nonnormally distributed variables were log-transformed for analysis. Differences in clinical and clamp parameters between type 1 diabetic and nondiabetic subjects and between men and women within each group were examined using unpaired Student t tests. Differences in categorical variables were examined using χ2 tests. P < 0.05 was considered statistically significant. SAS (version 9.2) was used for analyses, and Sigma Plot was used for generating difference figures.
Methods for presentation of figures.
The cholesterol content in each fraction obtained from the FPLC is expressed as a percentage of the total cholesterol in all subfractions to adjust for differences in total cholesterol levels among subjects, adapting the methodology previously used in DCCT/EDIC (14). This is calculated by summing the cholesterol for an individual in all 51 fractions and expressing the result for each fraction as the cholesterol in that fraction divided by the summed cholesterol and multiplied by 100. To test the significance of differences in cholesterol distributions among groups of subjects, a difference plot is generated by subtracting the mean percent cholesterol value of each fraction in one group from the mean percent cholesterol value in the same fraction of the second group and determining the 95% CI for this difference. A difference in fractional cholesterol content between groups is significant (P < 0.05) when the 95% CI does not cross the zero line.
RESULTS
Characteristics of study subjects are presented in Table 1 stratified by sex and type 1 diabetes status. As previously reported in the full CACTI cohort, type 1 diabetic subjects had a less atherogenic fasting lipid profile than nondiabetic subjects (5). For example, in both male and female subjects with type 1 diabetes, LDL cholesterol was ∼30 mg/dl lower than in nondiabetic subjects. As expected, type 1 diabetic subjects had a higher preclamp fasting glucose and insulin level than nondiabetic subjects, but there were no differences at the end of the clamp. Furthermore, type 1 diabetic subjects were more insulin resistant than nondiabetic subjects, for both women (6.2 ± 3.4 vs. 15.5 ± 4.8 mg/kg FFM/min; P < 0.0001) and men (5.4 ± 3.7 vs. 10.0 ± 5.2 mg/kg FFM/min; P = 0.004). Type 1 diabetic subjects were also more likely to be receiving statin treatment (women 52 vs. 9%, P = 0.002; men 68 vs. 15%, P < 0.0001) and have higher A1C (women 7.5 ± 0.9 vs. 5.4 ± 0.3%, P < 0.0001; men 7.5 ± 0.8 vs. 5.4 ± 0.3%, P < 0.0001). Among women, there was no difference in the prevalence of menopause or the use of oral contraceptive hormones by diabetes status. There was no difference in BMI, reported physical activity, or visceral fat by sex or diabetes status.
TABLE 1.
Baseline characteristic of subjects by type 1 diabetes status and sex
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Type 1 diabetes | Control | P | Type 1 diabetes | Control | P | |
| n | 21 | 22 | 19 | 20 | ||
| Age (years) | 44 ± 9 | 44 ± 8 | 0.75 | 47 ± 10 | 47 ± 6 | 0.89 |
| Type 1 diabetes duration (years) | 22 ± 8 | NA | NA | 23 ± 8 | NA | NA |
| Glucose infusion rate (mg/kg FFM/min) | 6.2 ± 3.4 | 15.5 ± 4.8 | <0.0001 | 5.4 ± 3.7 | 10.0 ± 5.2 | 0.004 |
| A1C (%) | 7.5 ± 0.9 | 5.4 ± 0.3 | <0.0001 | 7.5 ± 0.8 | 5.4 ± 0.3 | <0.0001 |
| Fasting glucose (mg/dl) | 109 ± 19 | 92 ± 6 | 0.0008 | 124 ± 53 | 99 ± 9 | 0.06 |
| Final clamp glucose (mg/dl) | 89 ± 4 | 89 ± 3 | 0.90 | 89 ± 2 | 91 ± 3 | 0.10 |
| Baseline insulin (μU/ml) | 36 ± 35 | 8 ± 2 | 0.001 | 27 ± 16 | 10 ± 5 | 0.0002 |
| Final clamp insulin (μU/ml) | 108 ± 40 | 108 ± 33 | 0.96 | 104 ± 31 | 87 ± 23 | 0.06 |
| Body fat (%) | 32.4 ± 6.7 | 34.7 ± 6.6 | 0.27 | 24.3 ± 6.1 | 24.2 ± 3.2 | 0.92 |
| BMI (kg/m2) | 25.8 ± 4.3 | 25.8 ± 4.3 | 0.99 | 28.3 ± 4.3 | 27.2 ± 3.6 | 0.41 |
| Visceral fat (cm2) | 10.5 ± 0.6 | 10.5 ± 0.3 | 0.93 | 10.9 ± 0.4 | 11.0 ± 0.5 | 0.31 |
| Physical activity (log kcal) | 7.2 ± 1.3 | 7.4 ± 1.1 | 0.52 | 7.3 ± 1.0 | 7.5 ± 0.8 | 0.50 |
| Total cholesterol (mg/dl) | 135 ± 33 | 171 ± 33 | 0.0009 | 145 ± 32 | 171 ± 25 | 0.007 |
| HDL cholesterol (mg/dl) | 56 ± 13 | 57 ± 10 | 0.74 | 61 ± 30 | 45 ± 9 | 0.03 |
| Triglycerides (mg/dl) | 69 ± 42 | 99 ± 40 | 0.02 | 70 ± 22 | 126 ± 73 | 0.003 |
| LDL cholesterol (mg/dl) | 66 ± 25 | 95 ± 29 | 0.0009 | 70 ± 25 | 101 ± 25 | 0.0004 |
| Taking statins (%) | 52 | 9 | 0.002 | 68 | 15 | 0.001 |
| Oral contraceptive pill use (%) | 86 | 73 | 0.46 | NA | NA | NA |
| Postmenopausal (%) | 19 | 32 | 0.49 | NA | NA | NA |
Data are means ± SD or %. NA, not applicable.
Differences by type 1 diabetes.
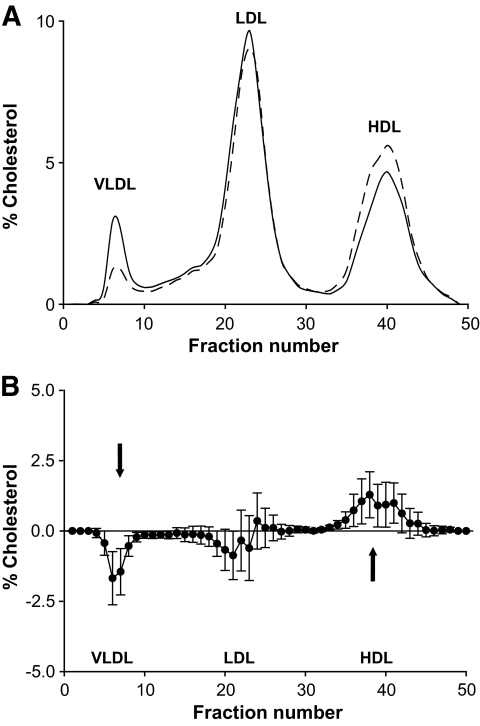
The mean lipoprotein subfraction cholesterol distributions are displayed within subjects with type 1 diabetes (Fig. 2A, hatched line) and within nondiabetic control subjects (Fig. 2A, solid line). As shown in Fig. 2B, subjects with type 1 diabetes had less VLDL and more HDL cholesterol than control subjects (P < 0.05 for both). Next, differences by sex in lipoprotein subfraction cholesterol distribution are displayed within subjects with type 1 diabetes (Fig. 3A) and within nondiabetic control subjects (Fig. 3B). Nondiabetic control men had more cholesterol distributed as VLDL and LDL but less as HDL than women (P < 0.05), as expected, but no significant differences existed by sex in type 1 diabetic subjects.
FIG. 2.
A: Means of FPLC lipoprotein cholesterol distribution in subjects with type 1 diabetes (hatched line) and nondiabetic control subjects (solid line). B: Differences in FPLC lipoprotein distribution by type 1 diabetes status (type 1 − nondiabetic, so that a mean above the zero indicates more cholesterol in type 1 diabetic subjects and a mean below the zero line indicates less). Arrows indicate fractions in which statistically significant differences exist.
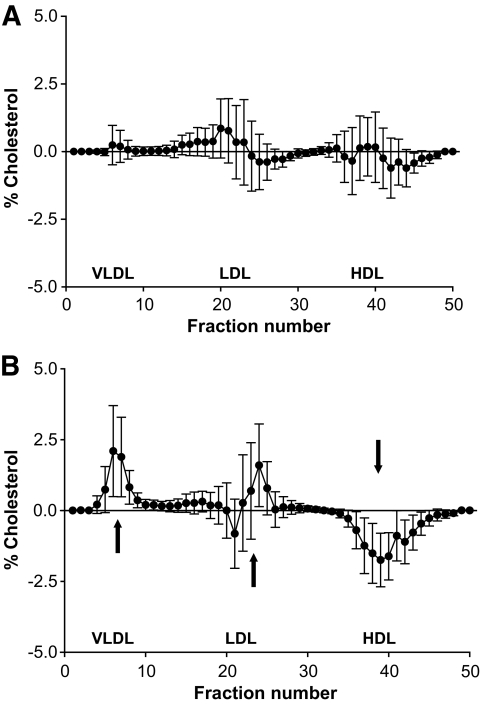
FIG. 3.
A: Differences in FPLC lipoprotein distribution by sex in type 1 diabetic subjects (male type 1 diabetic − female type 1 diabetic). B: Differences in FPLC lipoprotein distribution by sex in nondiabetic subjects (male nondiabetic − female nondiabetic).
Differences by sex.
We next investigated differences in lipoprotein subfraction cholesterol distribution by type 1 diabetes status in men (Fig. 4A) and women (Fig. 4B). Among men, those with type 1 diabetes had less VLDL and more HDL cholesterol than control subjects. In women, however, those with type 1 diabetes had more LDL cholesterol with an apparent shift of cholesterol distribution within LDL to smaller (atherogenic) LDL fractions in those with diabetes compared with those without.
FIG. 4.
A: Differences in FPLC lipoprotein distribution by type 1 diabetes in male subjects (male type 1 diabetic − male nondiabetic). B: Differences in FPLC lipoprotein distribution by type 1 diabetes in female subjects (female type 1 diabetic − female nondiabetic).
Glycemia and statins.
Because statin use and glycemic control are both likely major confounders of lipoprotein subfraction cholesterol distribution differences by diabetes status, we next examined the differences by statin use (yes/no) in type 1 diabetic men and women and then by glycemic control as measured by the highest versus lowest tertiles of A1C (data not shown). No differences in the fasting lipid profile existed within type 1 diabetic men and women based on statin status. LDL cholesterol was similar in men with type 1 diabetes by statin status (72 ± 34 vs. 69 ± 22 mg/dl, P = 0.82) and in women with type 1 diabetes (64 ± 24 vs. 67 ± 26 mg/dl, P = 0.81). However, men with type 1 diabetes in the lowest tertile of A1C (<7.2%) had less cholesterol distributed in LDL compared with men with type 1 diabetes in the highest A1C tertile (>8.0%), but there were no differences in VLDL or HDL cholesterol. In women with type 1 diabetes, no difference existed in lipoprotein subfraction cholesterol distribution between the lowest A1C tertile (6.9%) and the highest A1C tertile (8.2%).
Insulin resistance.
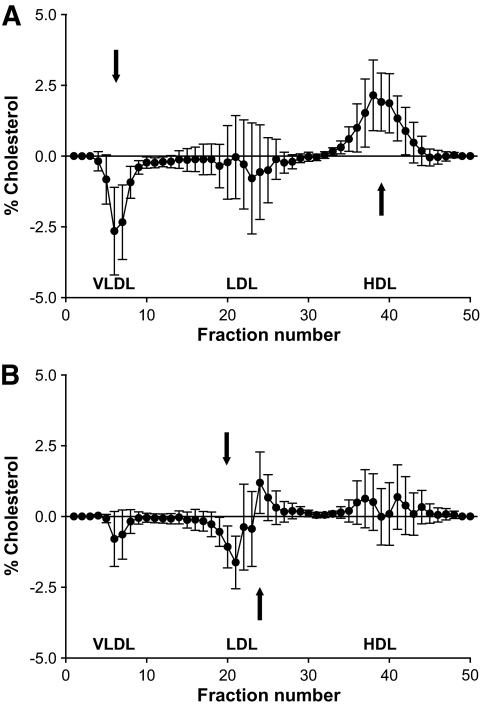
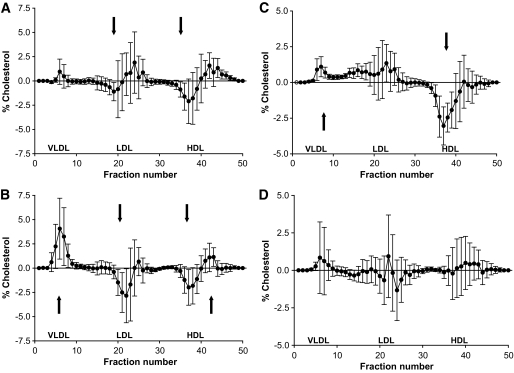
To further investigate these differences and to test the hypothesis that insulin resistance affects lipoprotein subfraction cholesterol distribution, we plotted the differences between the highest and lowest tertiles of insulin resistance as measured by the hyperinsulinemic-euglycemic clamp protocol within each sex and type 1 diabetes strata. Differences in lipoprotein subfraction cholesterol distribution by these strata were as follows. For men with type 1 diabetes, those with the most insulin resistance compared with those with the least insulin resistance had a shift to increased cholesterol in denser LDL and HDL (Fig. 5A). For male control subjects, those with the most insulin resistance compared with those with the least insulin resistance had more VLDL cholesterol as well as a shift to increased cholesterol in denser LDL and HDL (Fig. 5B). For women with type 1 diabetes, those with the most insulin resistance compared with those with the least insulin resistance had more cholesterol distributed in VLDL and less distributed in HDL (Fig. 5C). However, in contrast, for female control subjects, there were no differences in lipoprotein subfraction cholesterol distribution between subjects with the most and least insulin resistance (Fig. 5D).
FIG. 5.
A: Differences in FPLC lipoprotein distribution by insulin resistance (highest vs. lowest tertiles) in male type 1 diabetic subjects. B: Differences in FPLC lipoprotein distribution by insulin resistance (highest vs. lowest tertiles) in male nondiabetic subjects. C: Differences in FPLC lipoprotein distribution by insulin resistance (highest vs. lowest tertiles) in female type 1 diabetic subjects. D: Differences in FPLC lipoprotein distribution by insulin resistance (highest vs. lowest tertiles) in female nondiabetic subjects.
Also, of note, the pattern for differences in the largest (but not the smallest) lipoprotein HDL cholesterol distribution by insulin resistance tertiles for women with type 1 diabetes in Fig. 5D was similar to that of men with type 1 diabetes (Fig. 5A) and male control subjects (Fig. 5B) by insulin resistance tertiles. Therefore, it appears that the effect of insulin resistance on lipoprotein subfraction cholesterol distribution was similar in men with and without type 1 diabetes (Fig. 5A and B) and also in women with type 1 diabetes (Fig. 5D) but not in nondiabetic women (Fig. 5C).
Visceral fat.
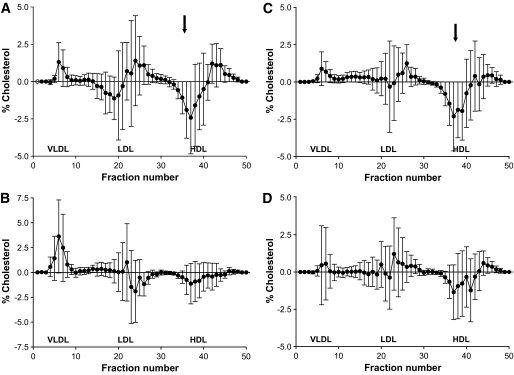
Finally, visceral fat was more strongly correlated with glucose infusion rate in type 1 diabetic subjects (r = −0.51, P = 0.017, in women and r = −0.43, P = 0.066, in men) than in nondiabetic subjects (r = −0.29, P = 0.19, and r = −0.24, P = 0.31, in women and men, respectively). A modest effect was observed on HDL cholesterol distribution when the highest visceral fat tertiles were compared with the lowest visceral fat tertiles in men and women with type 1 diabetes (Fig. 6A–D).
FIG. 6.
A: Differences in FPLC lipoprotein distribution by visceral fat (highest vs. lowest tertiles) in male type 1 diabetic subjects. B: Differences in FPLC lipoprotein distribution by visceral fat (highest vs. lowest tertiles) in male nondiabetic subjects. C: Differences in FPLC lipoprotein distribution by visceral fat (highest vs. lowest tertiles) in female type 1 diabetic subjects. D: Differences in FPLC lipoprotein distribution by visceral fat (highest vs. lowest tertiles) in female nondiabetic subjects.
DISCUSSION
The main findings of this study are that men with type 1 diabetes have a less atherogenic lipoprotein subfraction cholesterol distribution than nondiabetic men, perhaps due to increased statin use, but women with type 1 diabetes have a more atherogenic distribution compared with nondiabetic women with more LDL cholesterol and an apparent shift of cholesterol to a smaller LDL despite the higher prevalence of statin therapy. Furthermore, women with type 1 diabetes have a lipoprotein subfraction cholesterol distribution similar to that of type 1 diabetic men not the less atherogenic profile that is the expected sex-based difference seen in the nondiabetic control subjects. Next, when we investigated the association of insulin resistance and lipoprotein subfraction distribution, a pronounced association of higher insulin resistance with a more atherogenic lipoprotein subfraction cholesterol distribution was noted among men with and without type 1 diabetes and in women with type 1 diabetes. These data are novel because most previous investigations of lipoprotein distribution in people with type 1 diabetes lacked a nondiabetic control group, and, furthermore, the role of insulin resistance was not investigated. Therefore, these findings suggest that the fasting lipid profile may inadequately assess CVD risk in people with type 1 diabetes and that insulin resistance may play an important role in these differences, especially in women with type 1 diabetes.
When we examined the effect of glycemic control in type 1 subjects, there was only a minimal effect on lipoprotein subfraction cholesterol distribution (data not shown). The type 1 diabetic subjects had reasonably good glycemic control with a small difference between the highest and lowest A1C tertiles, perhaps explaining this limited association of glycemic control with lipoprotein subfraction cholesterol distribution.
Not unexpectedly, there were no differences in LDL subfraction cholesterol distribution in type 1 diabetic subjects based on statin use (data not shown). Previous studies have shown that statins do not change the LDL cholesterol subfraction distribution (28,29), whereas higher doses of a potent statin, that is, rosuvastatin, can increase buoyant HDL more than small HDL (30). We also did not find a difference in the fasting LDL cholesterol in subjects with type 1 diabetes by statin treatment. It is likely that the type 1 diabetic subjects receiving statin treatment were being treated because of previous lipid abnormalities. Regardless of statin treatment, the type 1 diabetic subjects had mean LDL cholesterol levels near 70 mg/dl. Moreover, an effect of statins on LDL cholesterol distribution would be unexpected. In fact, this emphasizes the finding of a more atherogenic lipoprotein profile seen in women with type 1 diabetes compared with nondiabetic women, despite the type 1 diabetic women being much more likely to be taking statins. In contrast, on the fasting lipid profile, both men and women with type 1 diabetes had LDL cholesterol ∼30 mg/dl lower than nondiabetic subjects. This highlights how the fasting lipid profile may not adequately represent CVD risk in people with type 1 diabetes. Because only five nondiabetic subjects were taking statins, we are unable to compare the effect of statins on lipoprotein subfraction cholesterol distribution between type 1 diabetic and nondiabetic subjects.
Our data on differences in lipoprotein subfraction cholesterol distribution between type 1 diabetic and nondiabetic control subjects are consistent with previous reports using nuclear magnetic resonance (NMR) (31) and of a less atherogenic lipid profile in people with type 1 diabetes compared with nondiabetic control subjects (5,12,13). Furthermore, because a measurement of insulin resistance in type 1 diabetes requires a clamp, the CACTI clamp substudy provided a unique opportunity to investigate the reported association of lipoprotein cholesterol distribution with insulin resistance in people with type 1 diabetes to extend previous research (23–25) performed in subjects without diabetes and those with type 2 diabetes. For example, our results on the differences by diabetes status or the differences by insulin resistance are greater than the <1% differences reported by Purnell et al. (14) in the DCCT/EDIC cohort when the first and fourth quartiles of weight gain (a surrogate of insulin resistance) were compared within treatment arms. The differences we report in lipoprotein subfraction cholesterol distribution related to the differences in insulin resistance are similar to or greater than the magnitude of the differences in cholesterol subfractions reported in the DCCT/EDIC cohort between the intensively and conventionally treated arms of the study in which there was a 2% difference in A1C. However, unlike the DCCT, the CACTI study is an observational cohort. Thus, the association of glycemia, obesity, and insulin resistance to lipoprotein metabolism and CVD are complex in type 1 diabetes and require further investigation.
Further data from the DCCT/EDIC study using NMR lipoprotein analysis show that male sex and poor glycemic control are associated with a more atherogenic lipoprotein profile (16), which is in turn associated with increased carotid intima-media thickness (17) and renal dysfunction (32). In contrast, Colhoun et al. (31) have reported a lack of association between lipoprotein subclasses and particle size with coronary artery calcium in adults with type 1 diabetes. The type 1 diabetic subjects had more large and less small HDL than nondiabetic subjects (31), although we observed this HDL effect only in men. Of note, in this study, among people with type 1 diabetes, a sex difference in lipoproteins was also reported; women with type 1 diabetes had less large and more small dense LDL and reduced LDL size, and this effect of type 1 diabetes on LDL size was significantly different in women than in men (31). Also, our data are consistent with those reported by Colhoun et al. and uniquely extend this finding by implicating insulin resistance as part of the pathophysiologic mechanism of sex differences in lipoproteins.
Additional data exist on lipoproteins and insulin resistance in people with type 2 diabetes. Goff et al. (24) have reported data from the Insulin Resistance Atherosclerosis Study (IRAS) family study using NMR technology and an intravenous glucose tolerance test to assess the associations between insulin resistance and lipoproteins in a mixed-race cohort with type 2 diabetes, impaired glucose tolerance, and normal glucose tolerance. They reported associations of insulin resistance with a variety of lipoprotein measures (size and subclass concentrations) and using factor analysis accounted for 41% of the variance across lipoprotein measures, which was correlated with insulin resistance (24). Similarly, Garvey et al. (23) reported data on the association of glucose disposition rate as determined by a hyperinsulinemic-euglycemic clamp to lipoprotein sizes and concentrations (as measured by NMR) in insulin-sensitive, insulin-resistant, and untreated type 2 diabetic subjects. Insulin resistance, although not type 2 diabetes per se, was associated with more atherogenic lipoprotein size and subclass particle concentrations for VLDL, LDL, and HDL, but these differences were not apparent in conventional fasting lipid profiles (23).
Although lipid levels in patients with type 1 diabetes have been found to be comparable to or better than those in nondiabetic control subjects (lower total cholesterol, LDL, and triglyceride and higher HDL) (5,12,13), adults with type 1 diabetes still commonly have dyslipidemia and are known to be at higher risk for atherosclerotic disease and for worse outcomes of CVD compared with the general population (7). Dyslipidemia is clearly a major risk factor for atherosclerosis and CVD in adults with both type 1 and type 2 diabetes (8). The National Cholesterol Education Program considers the presence of diabetes to be the risk equivalent of a history of coronary disease with similar goals for lipid lowering (33). Although the effectiveness of statin treatment on elevated LDL cholesterol in adults with type 2 diabetes is well established (8), no clinical trials exist in people with type 1 diabetes, demonstrating that LDL cholesterol reduction results in improved CVD outcomes. However, the Heart Protection Study included 615 subjects with type 1 diabetes and the magnitude of reduction in CVD events was similar in type 1 and type 2 diabetic subjects, although this study was underpowered to be statistically significant in subgroup analysis (34). There is consideration that lipids may be more atherogenic in those with diabetes. Possible mechanisms include differences in lipoprotein particle size, LDL oxidation, and increased transvascular and macrophage LDL transport in patients with type 1 diabetes (31,33,35).
Insulin resistance is a well-known component of type 2 diabetes but is not always considered as part of type 1 diabetes. Despite the relative lack of dyslipidemia and obesity in type 1 diabetic patients, studies using the hyperinsulinemic-euglycemic clamp have demonstrated increased insulin resistance in type 1 diabetic patients compared with nondiabetic individuals (20,21,36–39), and glucose disposal rate was statistically significantly associated with triglycerides (r = −0.51, P < 0.01) but not HDL cholesterol (r = 0.13) in a clamp study with 24 subjects with type 1 diabetes (40). It has been proposed that this increased insulin resistance may be due to the subcutaneous delivery of insulin in supraphysiologic doses in patients with type 1 diabetes (39). This treatment modality may increase peripheral insulin resistance but would not be expected to affect the liver and lipoprotein production because subcutaneous insulin does not expose the liver to high insulin levels as does endogenous insulin production in hyperinsulinemic type 2 diabetic patients and nondiabetic individuals. In the general population, insulin resistance is an important component of accelerated atherosclerosis (41). It is plausible that CAD develops earlier in type 1 diabetic patients who are insulin resistant (26,42,43). However, direct measurement of insulin resistance in insulin-treated patients is difficult and requires the euglycemic insulin clamp approach with careful stabilization of glycemia. Glucose clamps have good intrasubject reproducibility but are time-consuming, costly, and labor-intensive and, therefore, are difficult to perform in large epidemiologic trials. Methods for estimating insulin resistance in nondiabetic individuals (homeostasis model assessment and the quantitative insulin sensitivity check index) have been developed but cannot be applied to patients with type 1 diabetes because they are severely insulin deficient and therefore unable to secrete insulin in response to glycemic challenge. Moreover, fasting plasma insulin levels only reflect their exogenous insulin treatment regimen.
This study does have limitations. Because of the time-intensive nature of the hyperinsulinemic-euglycemic clamp protocol, we have complete data on only these 82 subjects, and although they are representative of the full CACTI cohort, they may not be representative of other type 1 diabetic populations. However, this study is much larger than most previous clamp studies performed in individuals with type 1 diabetes and includes a nondiabetic control group. Also, it is possible that the control women in the least insulin resistance tertile were still sufficiently insulin sensitive to not demonstrate a relationship between insulin resistance and an effect on lipoprotein cholesterol distribution. However, sex differences in nondiabetic subjects are well described, with 41% (44) and 45% (45) greater insulin sensitivity reported in women compared with men, similar to the difference in our nondiabetic subjects. Furthermore, we present data on lipoprotein subfraction cholesterol distribution in fasting samples collected before initiation of the hyperinsulinemic clamp only, and the effects of insulin infusion on lipoprotein distribution cannot be examined in this study. Additionally, other analytes were not measured in the lipoprotein subfractions such as triglycerides, and these may differ by type 1 diabetes and insulin resistance and represent future directions to investigate. Finally, the data presented in this study are cross-sectional and so causation of the reported associations cannot be determined.
In conclusion, a less atherogenic lipoprotein profile is seen in men but not in women with type 1 diabetes. This is in contrast to the well-described sex difference seen in nondiabetic women who have a less atherogenic lipid and lipoprotein profile and lower rates of CVD, especially before menopause. In men with and without type 1 diabetes and in women with type 1 diabetes, insulin resistance was associated with a more atherogenic lipoprotein profile. These data suggest that differences in lipoprotein cholesterol distribution may contribute to sex-based differences in CVD risk in type 1 diabetes and that insulin resistance may explain some of this increased relative risk in women with type 1 diabetes. In general, our data reflect the important need for further investigation of the contribution of insulin resistance to lipoprotein metabolism and CVD risk in patients with type 1 diabetes.
ACKNOWLEDGMENTS
Support for this study was provided by the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute Grants R01-HL-61753 and HL-79611, American Diabetes Association Postdoctoral Fellowship (7-09-CVD-06), and Diabetes Endocrinology Research Center Clinical Investigation Core P30-DK-57516. The study was performed at the Adult General Clinical Research Center at the University of Colorado Denver Health Sciences Center supported by the NIH (M01-RR00051), at the Barbara Davis Center for Childhood Diabetes, at the Colorado Heart Imaging Center in Denver, and in the laboratory of R.H.E. D.M.M. was supported by grant K23-DK-075360. I.E.S. was funded in part by grants that are supported by the NIH, Office of Research in Women's Health, Building Interdisciplinary Research Careers in Women's Health (BIRCHW), and the BIRCWH K12 Program.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Maahs DM, Wadwa RP, Bishop F, Daniels SR, Rewers M, Klingensmith GJ: Dyslipidemia in youth with diabetes: to treat or not to treat? J Pediatr 2008;153:458–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman BDiabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snell-Bergeon JK, Hokanson JE, Jensen L, MacKenzie T, Kinney G, Dabelea D, Eckel RH, Ehrlich J, Garg S, Rewers M: Progression of coronary artery calcification in type 1 diabetes: the importance of glycemic control. Diabetes Care 2003;26:2923–2928 [DOI] [PubMed] [Google Scholar]
- 4.Maahs DM, Kinney GL, Wadwa P, Snell-Bergeon JK, Dabelea D, Hokanson J, Ehrlich J, Garg S, Eckel RH, Rewers MJ: Hypertension prevalence, awareness, treatment, and control in an adult type 1 diabetes population and a comparable general population. Diabetes Care 2005;28:301–306 [DOI] [PubMed] [Google Scholar]
- 5.Wadwa RP, Kinney GL, Maahs DM, Snell-Bergeon J, Hokanson JE, Garg SK, Eckel RH, Rewers M: Awareness and treatment of dyslipidemia in young adults with type 1 diabetes. Diabetes Care 2005;28:1051–1056 [DOI] [PubMed] [Google Scholar]
- 6.Lipid and lipoprotein levels in patients with IDDM diabetes control and complication. Trial experience. The DCCT Research Group. Diabetes Care 1992;15:886–894 [DOI] [PubMed] [Google Scholar]
- 7.Soedamah-Muthu SS, Chaturvedi N, Toeller M, Ferriss B, Reboldi P, Michel G, Manes C, Fuller JHEURODIAB Prospective Complications Study Group Risk factors for coronary heart disease in type 1 diabetic patients in Europe: the EURODIAB Prospective Complications Study. Diabetes Care 2004;27:530–537 [DOI] [PubMed] [Google Scholar]
- 8.Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJAmerican Heart Association, American Diabetes Association Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2007;30:162–172 [DOI] [PubMed] [Google Scholar]
- 9.Laing SP, Swerdlow AJ, Slater SD, Burden AC, Morris A, Waugh NR, Gatling W, Bingley PJ, Patterson CC: Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 2003;46:760–765 [DOI] [PubMed] [Google Scholar]
- 10.Colhoun HM, Rubens MB, Underwood SR, Fuller JH: The effect of type 1 diabetes mellitus on the gender difference in coronary artery calcification. J Am Coll Cardiol 2000;36:2160–2167 [DOI] [PubMed] [Google Scholar]
- 11.Lloyd CE, Kuller LH, Ellis D, Becker DJ, Wing RR, Orchard TJ: Coronary artery disease in IDDM: gender differences in risk factors but not risk. Arterioscler Thromb Vasc Biol 1996;16:720–726 [DOI] [PubMed] [Google Scholar]
- 12.Guy J, Ogden L, Wadwa RP, Hamman RF, Mayer-Davis EJ, Liese AD, D'Agostino R, Jr, Marcovina S, Dabelea D: Lipid and lipoprotein profiles in youth with and without type 1 diabetes: the SEARCH for Diabetes in Youth case-control study. Diabetes Care 2009;32:416–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howard BV: Lipoprotein metabolism in diabetes mellitus. J Lipid Res 1987;28:613–628 [PubMed] [Google Scholar]
- 14.Purnell JQ, Hokanson JE, Marcovina SM, Steffes MW, Cleary PA, Brunzell JD: Effect of excessive weight gain with intensive therapy of type 1 diabetes on lipid levels and blood pressure: results from the DCCT. Diabetes Control and Complications Trial. JAMA 1998;280:140–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Purnell JQ, Dev RK, Steffes MW, Cleary PA, Palmer JP, Hirsch IB, Hokanson JE, Brunzell JD: Relationship of family history of type 2 diabetes, hypoglycemia, and autoantibodies to weight gain and lipids with intensive and conventional therapy in the Diabetes Control and Complications Trial. Diabetes 2003;52:2623–2629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenkins AJ, Lyons TJ, Zheng D, Otvos JD, Lackland DT, McGee D, Garvey WT, Klein RLDCCT/EDIC Research Group Serum lipoproteins in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Intervention and Complications Cohort: associations with gender and glycemia. Diabetes Care 2003;26:810–818 [DOI] [PubMed] [Google Scholar]
- 17.Lyons TJ, Jenkins AJ, Zheng D, Klein RL, Otvos JD, Yu Y, Lackland DT, McGee D, McHenry MB, Lopes-Virella M, Garvey WTDCCT/EDIC Research Group Nuclear magnetic resonance-determined lipoprotein subclass profile in the DCCT/EDIC cohort: associations with carotid intima-media thickness. Diabet Med 2006;23:955–966 [DOI] [PubMed] [Google Scholar]
- 18.Martin FI, Stocks AE: Insulin sensitivity and vascular disease in insulin-dependent diabetics. Br Med J 1968;2:81–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeFronzo RA, Hendler R, Simonson D: Insulin resistance is a prominent feature of insulin-dependent diabetes. Diabetes 1982;31:795–801 [DOI] [PubMed] [Google Scholar]
- 20.Schauer IE, Bergman B, Snell-Bergeon J, Maahs DM, Kretowski A, Eckel RH, Rewers M: Insulin sensitivity and free fatty acid suppression differ in persons with type 1 diabetes compared to non-diabetic controls: the CACTI study. In Proceedings of the 68th Annual Meeting of the American Diabetes Association, San Francisco, CA, 6–10 June, 2008 Arlington, VA, American Diabetes Association, 2008 [Google Scholar]
- 21.Nadeau KJ, Regensteiner JG, Bauer TA, Brown MS, Dorosz JL, Hull A, Zeitler P, Draznin B, Reusch JE: Insulin resistance in adolescents with type 1 diabetes and its relationship to cardiovascular function. J Clin Endocrinol Metab 2010;95:513–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeFronzo RA, Tobin JD, Andres R: Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 1979;237:E214–E223 [DOI] [PubMed] [Google Scholar]
- 23.Garvey WT, Kwon S, Zheng D, Shaughnessy S, Wallace P, Hutto A, Pugh K, Jenkins AJ, Klein RL, Liao Y: Effects of insulin resistance and type 2 diabetes on lipoprotein subclass particle size and concentration determined by nuclear magnetic resonance. Diabetes 2003;52:453–462 [DOI] [PubMed] [Google Scholar]
- 24.Goff DC, Jr, D'Agostino RB, Jr, Haffner SM, Otvos JD: Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metabolism 2005;54:264–270 [DOI] [PubMed] [Google Scholar]
- 25.Festa A, Williams K, Hanley AJ, Otvos JD, Goff DC, Wagenknecht LE, Haffner SM: Nuclear magnetic resonance lipoprotein abnormalities in prediabetic subjects in the Insulin Resistance Atherosclerosis Study. Circulation 2005;111:3465–3472 [DOI] [PubMed] [Google Scholar]
- 26.Dabelea D, Kinney G, Snell-Bergeon JK, Hokanson JE, Eckel RH, Ehrlich J, Garg S, Hamman RF, Rewers MCoronary Artery Calcification in Type 1 Diabetes Study Effect of type 1 diabetes on the gender difference in coronary artery calcification: a role for insulin resistance? The Coronary Artery Calcification in Type 1 Diabetes (CACTI) Study. Diabetes 2003;52:2833–2839 [DOI] [PubMed] [Google Scholar]
- 27.Goldberg IJ, Hu Y, Noh HL, Wei J, Huggins LA, Rackmill MG, Hamai H, Reid BN, Blaner WS, Huang LS: Decreased lipoprotein clearance is responsible for increased cholesterol in LDL receptor knockout mice with streptozotocin-induced diabetes. Diabetes 2008;57:1674–1682 [DOI] [PubMed] [Google Scholar]
- 28.van Tits LJ, Smilde TJ, van Wissen S, de Graaf J, Kastelein JJ, Stalenhoef AF: Effects of atorvastatin and simvastatin on low-density lipoprotein subfraction profile, low-density lipoprotein oxidizability, and antibodies to oxidized low-density lipoprotein in relation to carotid intima media thickness in familial hypercholesterolemia. J Investig Med 2004;52:177–184 [DOI] [PubMed] [Google Scholar]
- 29.Kostapanos MS, Milionis HJ, Filippatos TD, Nakou ES, Bairaktari ET, Tselepis AD, Elisaf MS: A 12-week, prospective, open-label analysis of the effect of rosuvastatin on triglyceride-rich lipoprotein metabolism in patients with primary dyslipidemia. Clin Ther 2007;29:1403–1414 [DOI] [PubMed] [Google Scholar]
- 30.Kostapanos MS, Milionis HJ, Filippatos TD, Christogiannis LG, Bairaktari ET, Tselepis AD, Elisaf MS: Dose-dependent effect of rosuvastatin treatment on HDL-subfraction phenotype in patients with primary hyperlipidemia. J Cardiovasc Pharmacol Ther 2009;14:5–13 [DOI] [PubMed] [Google Scholar]
- 31.Colhoun HM, Otvos JD, Rubens MB, Taskinen MR, Underwood SR, Fuller JH: Lipoprotein subclasses and particle sizes and their relationship with coronary artery calcification in men and women with and without type 1 diabetes. Diabetes 2002;51:1949–1956 [DOI] [PubMed] [Google Scholar]
- 32.Jenkins AJ, Lyons TJ, Zheng D, Otvos JD, Lackland DT, McGee D, Garvey WT, Klein RLDCCT/EDIC Research Group Lipoproteins in the DCCT/EDIC cohort: associations with diabetic nephropathy. Kidney Int 2003;64:817–828 [DOI] [PubMed] [Google Scholar]
- 33.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 34.Collins R, Armitage J, Parish S, Sleigh P, Peto RHeart Protection Study Collaborative Group MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003;361:2005–2016 [DOI] [PubMed] [Google Scholar]
- 35.Orchard TJ, Virella G, Forrest KY, Evans RW, Becker DJ, Lopes-Virella MF: Antibodies to oxidized LDL predict coronary artery disease in type 1 diabetes: a nested case-control study from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes 1999;48:1454–1458 [DOI] [PubMed] [Google Scholar]
- 36.Perseghin G, Lattuada G, Danna M, Sereni LP, Maffi P, De Cobelli F, Battezzati A, Secchi A, Del Maschio A, Luzi L: Insulin resistance, intramyocellular lipid content and plasma adiponectin in patients with type 1 diabetes. Am J Physiol Endocrinol Metab 2003;285:1174–1181 [DOI] [PubMed] [Google Scholar]
- 37.Ekstrand AV, Groop PH, Grönhagen-Riska C: Insulin resistance precedes microalbuminuria in patients with insulin-dependent diabetes mellitus. Nephrol Dial Transplant 1998;13:3079–3083 [DOI] [PubMed] [Google Scholar]
- 38.Nijs HG, Radder JK, Frölich M, Krans HM: The course and determinants of insulin action in type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1989;32:20–27 [DOI] [PubMed] [Google Scholar]
- 39.Greenfield JR, Samaras K, Chisholm DJ: Insulin resistance, intra-abdominal fat, cardiovascular risk factors, and androgens in healthy young women with type 1 diabetes mellitus. J Clin Endocrinol Metab 2002;87:1036–1040 [DOI] [PubMed] [Google Scholar]
- 40.Williams KV, Erbey JR, Becker D, Arslanian S, Orchard TJ: Can clinical factors estimate insulin resistance in type 1 diabetes? Diabetes 2000;49:626–632 [DOI] [PubMed] [Google Scholar]
- 41.Ginsberg HN: Insulin resistance and cardiovascular disease. J Clin Invest 2000;106:453–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orchard TJ, Olson JC, Erbey JR, Williams K, Forrest KY, Smithline Kinder L, Ellis D, Becker DJ: Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2003;26:1374–1379 [DOI] [PubMed] [Google Scholar]
- 43.Martin FI, Hopper JL: The relationship of acute insulin sensitivity to the progression of vascular disease in long-term type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1987;30:149–153 [DOI] [PubMed] [Google Scholar]
- 44.Nuutila P, Knuuti MJ, Mäki M, Laine H, Ruotsalainen U, Teräs M, Haaparanta M, Solin O, Yki-Järvinen H: Gender and insulin sensitivity in the heart and in skeletal muscles: studies using positron emission tomography. Diabetes 1995;44:31–36 [DOI] [PubMed] [Google Scholar]
- 45.Yki-Järvinen H: Sex and insulin sensitivity. Metabolism 1984;33:1011–1015 [DOI] [PubMed] [Google Scholar]