Abstract
Background
With the rising prevalence rates of child and adolescent obesity over the last several decades it is important to examine the extant research in order to inform future research.
Objective
The aim of this paper is to review and critique research investigating familial correlates of child and adolescent obesity in the last decade.
Methods
A literature review was conducted between March 2008 and December 2008. Studies published after 2000 that assessed familial associations with child and adolescent obesity in the parental, family functioning, and sibling domains were included in the review. A total of 81 studies met inclusionary criteria.
Results
The majority of studies focused on the parental domain. Substantial evidence indicates an association between authoritative parenting style and child/adolescent lower BMI, healthy dietary intake and physical activity. Also, research on family meals has consistently shown an association between the frequency of family meals and child/adolescent lower BMI and healthy dietary intake.
Conclusion
To date, there is preliminary evidence that suggests that familial factors are associated with child and adolescent obesity, dietary intake, physical activity and weight control behaviors, but the majority of the evidence is cross-sectional and there are limitations with the research. Recommendations for future research are discussed.
Keywords: review, child obesity, adolescent obesity, family functioning, parenting, sibling
Over the last two decades obesity prevalence rates have doubled in children and tripled in adolescents (1–3). This seemingly uncontrollable problem has been deemed an “epidemic” by public health researchers and professionals (4). Numerous expert panels and national meetings have been convened to address the problem (5–8). These expert panels and committees, along with other researchers, have pointed to the importance of the family, and the multi-level influences in the family system that shape children and adolescents on a daily basis, as a neglected area of research (9–10). The main aim of this review is to investigate what findings exist related to familial correlates of child and adolescent obesity in the 21st century, in order to determine what gaps still exist and how researchers can improve the research in the next decade.
This review also aims to be more systemic than past reviews on childhood/adolescent obesity by reviewing literature that investigates multiple domains of the family system, rather than focusing on select components such as parenting (11–12), the food environment (13–14), or the individual child or adolescent (6, 15–16), in exclusion of the entire family system. This article will investigate the relationship between three central domains of the family and their associations with child/adolescent obesity. These include the: (a) parental domain, (b) family functioning domain, and (c) sibling domain.
FAMILY SYSTEMS THEORY
Family systems theory indicates that families live in complex systems in which multiple interactions occur simultaneously (17–19). Within family systems there are sub-systems, or domains (e.g., parental, family functioning, sibling). The multiple interactions that occur within the family domains are of specific interest when studying the associations between the family and child and adolescent obesity. According to family systems theory, the interactions that occur within the family are reciprocal. That is, each family member is shaping and being shaped by other family members’ actions. These mutual influencing patterns may give particular insight into the behaviors that ultimately determine dietary intake and physical activity in youth.
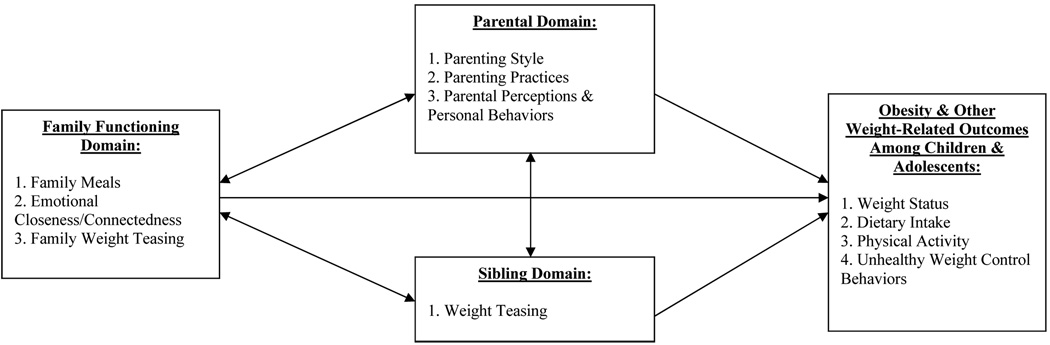
The multi-level influencing of health behaviors has gained recognition in the field of public health as well. Research has identified that health behaviors such as diet and physical activity are likely correlated, or co-occur, within individuals rather than being independent actions and are likely influenced by multiple sources (20–21). For instance, health behaviors occur within a family system that can either support and model them, or downplay the importance of them. In figure 1 a model is shown depicting the important family domains that are theoretically associated with child and adolescent obesity. This review will critique studies in each domain.
Figure 1.
Theoretical Model of Family Domains Correlated with Child and Adolescent Obesity and Weight-Related Outcomes
METHODS
Search Strategy
Studies were identified using three methods. First, reviews in the field of childhood and adolescent obesity were obtained and hand searched to identify key researchers and programs of work in this area. Publications arising from these reviews were identified and retrieved. Second, systematic searches of Medline, PubMed, CINAHL, ERIC, PsycInfo, and Family and Society Studies Worldwide (EBSCO) were conducted by using various combinations of the following keywords: obesity, overweight, weight status, weight gain, child, adolescent, parent, parenting style, authoritarian, authoritative, permissive, neglectful, parenting practices, family, sibling, family environment, family context, family factors, family meals, feeding styles, child feeding, caregiver feeding, feeding strategies, physical activity, exercise. Third, key researchers in the field of child and adolescent obesity were contacted to assess any new/emerging literature that would be published. An initial 157 studies were located and seven in-press articles.
Inclusion Criteria
A total of 81 empirical studies met the inclusion criteria for the review. Studies were included based on the following criteria: (a) the study investigated at least one domain of family life as the independent variable (parental domain, family functioning domain, or sibling domain), (b) the dependent variable was related to child or adolescent obesity (e.g. weight status, dietary intake, physical activity), (c) the study was quantitative in nature, (d) the study was not an intervention study, case study, review article or theoretical paper, (e) the study was published in the year 2000 or later, and (f) the study included children or adolescents from birth to 18 years old. Both child and adolescent samples were included because the majority of studies overlapped the ages of participants. Also, some studies had multiple independent variables. In these cases, specific findings were reported separately in the appropriate family domain. Although this increased the “n” count of the specific family domain, it did not count twice in the overall “n”. Thus, domain totals (n = 88) differ from the overall total (n = 81) for the review.
Coding
Studies were coded and organized (see table 1) according to the: (a) independent variable assessed (parent, family, or sibling domain), (b) study design, (c) sample size, (d) age group and gender, (e) assessments used, (f) outcome variable (DV), and (g) key results (associations between IV and DV).
Table 1.
Coded Characteristics of Reviewed Studies (N = 81)
| Study | Family Domain (IV) | Sample Size |
Age Range & Gender | Research Design |
Outcome (DV) | Associations IV & DV |
|---|---|---|---|---|---|---|
| PARENTING DOMAIN (N = 50) | ||||||
| Addessi, 2005 | Par; Parental Modeling & Encouraging | N = 27 | 2–5; 74% F, 26% M | CS; Lab | HDI | + |
| Agras, 2004 | Par; Parental Control of Feeding Environment | N = 150 | 0–9.5; 49% F,51% M | L; Lab | BMI, HDI | +, − |
| Arcan, 2007 | Par; Parental Modeling & Encouraging | N = 714 | 12–18; 51% F, 49% M | CS | HDI | + |
| Arredondo, 2006 | Par; Parenting Style (authoritative) | N = 812 | 5–12; 52% F, 48% M | CS | BMI, HDI, PA | −, +, + |
| Baughcum, 2001 | Par; Parental Control of Feeding Environment | N=1087 | 0–5; 50% F, 50% M | CS | BMI, HDI | +, − |
| Berge, in press | 1. Par; Parenting Style(authoritative) |
N=4,746 | 11–18; 51% F, 49% M | CS | BMI, HDI |
−, + |
| 2. Par; Parental Modeling & Encouraging | BMI | |||||
| Berge, in press | Par; Parenting Style(authoritative) | N=2,516 | 11–18; 54% F, 46% M | L | BMI, HDI, PA | −,+,+ |
| Birch, 2000 | Par; Parental Pressure/Restriction of Feeding | N = 197 | 5 yrs.; all female | CS | BMI, HDI | −, + |
| Birch, 2003 | Par; Parental Pressure/Restriction of Feeding | N = 140 | 5–7; all female | L | BMI, EAH | +, + |
| Bourcier, 2003 | Par; Parental Pressure/Restriction of Feeding | N = 282 | 0–17; 90% F, 10% M | CS | BMI | + |
| Boutelle Birkeland, 2007 |
Par; Parental Modeling & Encouraging | N = 714 | 11–18; 49% F,51% M | CS | HDI | + |
| Brown, 2004 | Par; Parental Control of Feeding Environment | N =112 | 9–13; 56% F, 44% M | CS | BMI, HDI | +, − |
| Carper, 2000 | Par; Parental Pressure/Restriction of Feeding | N = 197 | 5 yrs.; all female | CS | DR, DE | +, + |
| Campbell, 2006 | 1. Par; Parental Pressure/Restriction of Feeding |
N = | 5–6; 53% F, 47% M | CS | HDI, TV | −, + |
| 2. Fam; Frequency of Family Meals | 560 | HDI | + | |||
| Chen, 2004 | 1. Par; Parenting Style(authoritative) | N = 163 | 8–10, 55% F, 45% M | CS | BMI | − |
| 2. Fam; Family Closeness/Connection | BMI, HDI | −, + | ||||
| Crawford, 2006 | Par; Parental Modeling & Encouraging | N=1210 | 5–12; 53% F, 47% M | CS | BMI | − |
| Davison, 2001 | Par; Parental Modeling & Encouraging | N = 197 | 5–7; all female | L | BMI, PA, HDI | −, +, + |
| Duke, 2004 | Par; Parental Pressure/Restriction of Feeding | N = 135 | 1–7; 47% F, 53% M | L | BMI | + |
| Faith, 2003 | Par; Parental Pressure/Restriction of Feeding | N = 57 | 3–7; not reported | L | BMI | + Restriction − Pressure |
| Fisher, Birch, 2002 | Par; Parental Pressure/Restriction of Feeding | N = 192 | 5 yrs.; all female | L | BMI, HDI, EAH | +, −, + |
| Fisher, Mitchell, 2002 | Par; Parental Modeling & Encouraging | N = 197 | 5 yrs.; all female | CS | HDI | + |
| Francis, 2001 | Par; Parental Pressure/Restriction of Feeding | N = 104 | 5 yrs.; all female | CS; Exp | BMI | + Restriction − Pressure |
| Fulkerson, 2002 | Par; Parental Encouraging | N = 810 | 11–18; 53% F, 47% M | CS | D, EWC | +, + |
| Gable, 2000 | 1. Par; Parenting Style (authoritarian) | N = 65 | 6–10; 77% F, 23% M | CS | BMI, HDI, PA | +, −, − |
| 2. Par; Parental Control of Feeding | BMI, HDI, PA, TV | +, −, −, + | ||||
| 3. Fam; Family Meal Frequency | HDI | + | ||||
| Hanson, 2005 | Par; Parental Modeling & Encouraging | N = 902 | 11–18; 51% F, 49% M | CS | HDI | + |
| Hood, 2000 | Par; Parental Modeling & Encouraging | N = 92 | 4–10; 39% F, 61% M | L | BMI, DE, HDI | −, −, + |
| Hughes, 2005 | Par; Feeding Styles (authoritative) | N = 231 | 3–5; 55% F, 45% M | CS | HDI | + |
| Keller, 2004 | Par; Parental Modeling & Encouraging | N = 127 | 6–10; 53% F, 47% M | CS | BMI, HDI, PA | −, +, + |
| Kremers, 2003 | Par; Parenting Style (authoritative) | N = 643 | 16–17; 54% F, 46% M | CS | HDI | + |
| Lee, 2001 | Par; Parental Pressure/Restriction of Feeding | N = 192 | 0–5; all female | L | BMI, HDI | +, − |
| Lumeng, 2006 | Par; Parental Control of Feeding Environment | N = 71 | 3–6; 45% F, 55% M | CS; Lab | BMI, HDI | −, 0 |
| Matheson, 2006 | Par; Parental Pressure/Restriction of Feeding | N = 108 | 10 yrs.; 47% F ,53% M | CS | BMI | − |
| McGuire, 2002 | Par; Parental Encouraging | N = 900 | 11–18; 53% F, 47% M | CS | PA, TV | +, − |
| Mellin, 2002 | 1. Par; Parenting Style(Authoritative) | N=9,957 | 12–18; 47% F, 53% M | CS | BMI, HDI, PA, & EWC | −, +., +, − |
| 2. Fam; Family Closeness/Connectedness | BMI, HDI, PA | −, +, + | ||||
| Moens, 2007 | 1. Par; Parenting Style (authoritarian & permissive) | N = 28 | Exp=7–13;68%F,32%M | CS; Exp; Obs | BMI, HDI | +, − |
| 2. Fam; Frequency of Family Meals | N = 28 | Con=7–13;68%F,32%M | BMI, HDI | −, + | ||
| Neumark-Sztainer, Wall, 2008 |
Par; Encouraging (dieting) | N = 484 | 11–18; 51% F, 49% M | L | BMI, D | +, + |
| Nicklas, 2003 | Par; Parental Control of Feeding Environment | N=1562 | 10yrs.; 51% F, 49% M | CS | BMI | + |
| Patrick, 2005 | Par; Feeding Styles (authoritative) | N = 231 | 3–5; 55% F, 45% M | CS | HDI | + |
| Powers, 2006 | Par; Parental Pressure/Restriction of Feeding | N = 296 | 0–5; 48% F, 52% M | CS | BMI | + |
| Reinaerts, 2006 | Par; Parental Modeling & Encouraging | N=1,739 | 4–12; 55% F, 45% M | CS | HDI | + |
| Rhee, 2006 | Par; Parenting Style (authoritarian) | N = 872 | 4–7; 51% F, 49% M | L | BMI | + |
| Robinson, 2001 | Par; Parental Control of Feeding Environment | N = 792 | 8–9; 50% F, 50% M | CS | BMI | −, 0 |
| Schmitz, 2002 | Par; Parenting Style (authoritative) | N=3,798 | 8–12; 49% F, 51% M | CS | BMI, PA | −, + |
| Skinner, 2002 | Par; Parental Modeling & Encouraging | N = 70 | 2 month.-8;not reported | L | HDI | + |
| Spruijt-Metz, 2002 | Par; Parental Pressure/Restriction of Feeding | N = 120 | 7–14; 60% F, 40% M | CS | BMI | + |
| Tibbs, 2001 | Par; Parental Modeling & Encouraging | N = 456 | 0–5; not reported | CS; Exp | HDI | + |
| van der Horst, 2007 | Par; Parenting Style (authoritative) | N = 383 | 12–17; 55% F, 45% M | CS | HDI | −, + |
| Wardle,2000 | Par; Parental Control of Feeding Environment | N=100 | Exp=2–6; 55%F, 45%M | CS; Exp | BMI, HDI | 0, + |
| N =114 | Con=2–6; 49%F, 51%M | |||||
| Wardle, 2003 | Par; Parental Modeling & Encouraging | N = 98 | Exp=2–6; 46%F, 54%M | CS; Exp, | HDI | + |
| N = 45 | Con=2–6; 51%F, 49%M | Lab | ||||
| Wardle, 2006 | Par; Parental Control of Feeding Environment | N = 564 | 2–6; 50% F, 47% M | CS | HDI | + |
| FAMILY DOMAIN (N = 29) | ||||||
| Berge, in press | Fam; Family Closeness/Connection | N = 252 | 5–17; | CS | BMI, HDI, PA, TV | −,+,+,− |
| Bourdeaudhuij, 2000 |
Fam; Family Closeness/Connection | N = 208 | 12–18; 56% F, 44% M | CS | HDI | 0 |
| Boutelle, Fulkerson, 2007 | Fam; Fast-Food for Family Meals | N = 902 | 11–18; 53% F, 47% M | CS | HDI | − |
| Eisenberg, 2003 | Fam; Family Weight Teasing | N=4,746 | 11–18; 51% F, 49% M | CS | BMI | + |
| Eisenberg, 2004 | Fam; Frequency of Family Meals | N = 4,746 | 11–18; 51% F, 49% M | CS | HDI | + |
| Feldman, 2007 | Fam; Frequency of Family Meals with TV on | N = 4,746 | 11–18; 51% F, 49% M | CS | HDI | − |
| Fulkerson, Neumark-Sztainer, 2006 |
Fam; Frequency of Family Meals | N = 902 | 11–18; 53% F, 47% M | CS | HDI | + |
| Fulkerson, Story, 2006 |
Fam; Frequency of Family Meals | N=99,426 | 11–18; 50% F, 50% M | CS | HDI | + |
| Gillman, 2008 | Fam; Frequency of Family Meals | N=16,202 | 9–14; 54% F, 46% M | CS | HDI | + |
| Jacobs, 2007 | Fam; Frequency of Family Meals | N = 80 | 5–12; 35% F, 65% M | CS; Obs; Exp | BMI, HDI | −, + |
| Lamerz, 2000 | Fam; Family Closeness/Connection | N = 1,979 | 5–12; all female | CS | BMI | + |
| Larson, 2007 | Fam; Frequency of Family Meals | N = 1,710 | 11–18; 53% F, 47% M | L | HDI | + |
| Libbey, 2008 | Fam; Family Weight Teasing | N= 130 | 12–20; 65% F, 45% M | CS | EWC | + |
| Neumark-Sztainer (N-S), 2000 |
Fam; Frequency of Family Meals | N = 252 | 11–18; 51% F, 49% M | CS | HDI | |
| N-S, 2002 | Fam; Family Weight Teasing | N=4,746 | 11–18; 51% F, 49% M | CS | BMI, D, EWC | +, +, + |
| N-S, 2003 | Fam; Frequency of Family Meals | N=4,746 | 11–18; 51% F, 49% M | CS | HDI | + |
| N-S, Eisenberg, 2004 |
Fam; Frequency of Family Meals | N=2,516 | 11–18; 54% F, 46% M | L | EWC | − |
| N-S, Story, 2004 | Fam; Frequency of Family Meals | N=4,746 | 11–18; 51% F, 49% M | CS | HDI, EWC | +, − |
| N-S, Wall, 2004 | Fam; Frequency of Family Meals | N=4,746 | 11–18; 51% F, 49% M | CS | HDI, D, EWC | +, −, − |
| N-S, 2007 | Fam; Family Weight Teasing | N=2,516 | 11–18; 54% F, 46% M | L | BMI, EWC | +, + |
| N-S, Eisenberg, 2008 |
Fam; Frequency of Family Meals | N=2,516 | 11–18; 54% F, 46% M | L | EWC | − |
| Sen, 2006 | Fam; Frequency of Family Meals | N=5,014 | 12–14; 47% F, 53% M | L | BMI | − |
| Stradmeijer, 2000 | Fam; Family Closeness/Connectedness | N = 73 | Exp=9–16;44%F,56%M | CS; Exp | BMI | 0 |
| N = 70 | Con=9–16;40%F,60%M | |||||
| Taveras, 2005 | Fam; Frequency of Family Meals | N=14,431 | 19–14; 54% F, 46% M | L | BMI | − |
| Turner, 2005 | Fam; Family Closeness/Connectedness | N = 23 | 17–18; all female | CS; Exp | BMI, EWC | −, − |
| N = 23 | ||||||
| van den Berg, 2008 | Fam; Family Weight Teasing | N=4,746 | 11–18; 51% F, 49% M | CS | BMI | + |
| Vieweg, 2000 | Fam; Family Closeness/Connectedness | N=29,824 | 4–18; 49% F, 51% M | CS | BMI | + |
| Videon, 2003 | Fam; Frequency of Family Meals | N=18,177 | 13–18; 29% F, 51% M | CS | HDI | + |
| Zeller, 2007 | Fam; Family Closeness/Connectedness | N = 78 | Exp=8–16;59%F,41%M | CS, Exp | BMI | − |
| N= 71 | Con=8–16;55%F,45%M | |||||
| SIBLING DOMAIN (N = 2) | ||||||
| Keery, 2005 | Sib; Weight Teasing | N = 372 | 11–15; all female | CS | EWC | + |
| Taylor, 2006 | Sib; Weight Teasing | N = 455 | 18 yrs.; all female | CS | BMI | + |
Key: Fam = Family Domain; Par = Parenting Domain; Sib = Sibling Domain; F = Female; M = Male; Exp = Experimental; Con = Control Group; CS = Cross-Sectional; L = Longitudinal; Obs = Direct Observational Study; Lab = Laboratory; BMI = Body Mass Index; HDI = Healthy Dietary Intake; PA = Physical Activity; EWC = Extreme Weight Control Behaviors; D = Dieting; EAH = Eating in the Absence of Hunger; TV = Television Viewing Time; DE = Disinhibited Eating; DR = Dietary Restraint; FF = Fast-Food; (+) = there was a positive association between the IV and DV; (−) = there was a negative association between the IV and DV; (0) = no association was found between the IV and DV.
STATE OF THE LITERATURE PRIOR TO THE 21st Century
The majority of literature prior to the year 2000 looked at individual factors related to child and adolescents obesity. In particular, child and adolescent factors contributing to obesity such as, specific foods eaten, time spent in front of the television, time spent in physical activity and individual parent factors such as, control over the feeding environment were areas of focus (13–16). Towards the end of the 20th century researchers began to look at familial systemic associations with child and adolescent obesity by focusing on parent/child interactions, such as parenting style and family behaviors, such as family meals (11–12). Other systemic variables such as family closeness/connectedness, sibling weight teasing, or parental modeling of health behaviors had not been investigated. It was not until the late 1990’s when calls to the field by expert panels, national committees, and family intervention researchers pointed to the neglected influence of the family system on child and adolescent obesity that researchers began to include familial systemic variables in their research designs (8–12). This review focuses on studies after the year 2000 in order to identify research that had included familial variables in their research.
RESULTS
Parental Domain Associations with Child/Adolescent Obesity (total n = 52)
The parental domain is composed of general parenting behaviors, referred to as parenting style, and specific parenting practices. Parenting style describes a typology of attitudes and behaviors that characterize how a parent will interact with a child across domains of parenting that may result in individual differences among children on key outcomes (22). Whereas, parenting practices describe specific behavioral strategies employed by parents to socialize their children (22). Parenting styles are considered to be trait-like, whereas parenting practices are considered to be state dependent (16, 22). Both parenting style and parenting practices have been looked at in relation to child and adolescent obesity.
Parenting Style (n = 13)
Parenting style is characterized by the degree of parental demandingness (defined as structure/expectations) and responsiveness (defined as emotional availability/support) (23). The four parenting styles most commonly studied in the parenting literature are: authoritative, authoritarian, permissive, and neglectful (23–24). An authoritative parent balances high levels of demandingness with high levels of responsiveness. An authoritarian parent exhibits high levels of demandingness and low levels of responsiveness. A permissive parent expresses low levels of demandingness and high levels of responsiveness. A neglectful parent exhibits low levels of both demandingness and responsiveness. According to family systems theory, parenting style modifies or impacts the relationship between parent practices and child outcomes such that a child’s behavior exhibited within the context of a more positive parenting style (authoritative) will have a more beneficial impact on the child versus a behavior exhibited in a more negative parenting style (non-authoritative). General parenting style has been investigated, as well as, parenting style applied specifically to the feeding environment, called “feeding style”. Feeding styles are ways in which parents use authoritative, authoritarian, permissive or neglectful parenting styles in relation to feeding their children. According to family systems theory, it is expected that an authoritative feeding style will promote more healthy dietary intake and greater child ability to self-regulate eating behaviors, whereas, an authoritarian feeding style will promote rigid feeding practices and decreased ability to respond to satiety and hunger cues.
Cross-sectional studies (n = 11)
Cross-sectional studies looking at general parenting style have been conducted with children ages 3–10 and adolescents 10–17 from diverse ethnic backgrounds and have found similar results. These studies have consistently found that authoritative parenting style was associated with child and adolescent lower body mass index (BMI), availability of fruit and vegetables in the home, child consumption of fruit, vegetables, and dairy products, lower consumption of sugar sweetened beverages, and higher levels of physical activity (25–30). In contrast, authoritarian and neglectful parenting styles were positively associated with child and adolescent BMI, availability of sweets and unhealthy foods in the home, and negatively associated with vegetable consumption and physical activity (27–33). Mellin et. al. (30) further found that authoritarian parenting style was associated with lower breakfast consumption and higher emotional distress among overweight adolescent boys and higher rates of extreme dieting behaviors among adolescent overweight girls.
Researchers looking at specific feeding styles with children ages 3–6 years old, with diverse ethnicities, have found similar results as the general parenting style literature. Authoritative feeding styles were associated with healthy dietary intake and authoritarian feeding styles were associated with unhealthy dietary intake and increased availability of unhealthy food in the home (34–35). Hughes et.al. (34) also found that Hispanic parents were more likely to have permissive feeding styles and African-American parents were more likely to have neglectful feeding styles.
Longitudinal studies (n = 2)
In a longitudinal study of general parenting style with young children (majority white with mid to high SES) Rhee, et.al. (8) found that children of authoritarian mothers had an increased risk of being overweight (five times the odds), compared with children of authoritative mothers, and children of permissive and neglectful mothers were twice as likely to be overweight, compared with children of an authoritative mother. Berge, et. al. (36) found a negative association between authoritative parenting style and adolescent boys BMI and an interaction between maternal authoritarian parenting style and father neglectful parenting style that predicted higher BMI in boys.
Parenting Practices (n = 39)
Parental control over the child feeding environment, parental pressure/restricting behaviors in the food environment and parental encouraging or modeling of health behaviors are specific parental practices in the home that have been studied in relation to child and adolescent obesity.
Parental Control over the Feeding Environment (n =9)
Cross-sectional studies (n = 8)
Cross-sectional studies conducted with children ages birth-13 from diverse ethnic groups have found that children whose parents made greater attempts to control their diets reported higher BMI, intakes of both healthy and unhealthy snack foods, higher levels of body dissatisfaction, fewer physical activities and increased television viewing time (28, 37–39). Also, in Baughcum et.al.’s (37) study obese mothers were found to give their children less control in the feeding context than normal weight mothers.
In contrast, other cross-sectional studies have found that parental control over the child food environment did not predict poorer dietary intake or overweight in children. These studies found that parental control over children’s intake was inversely associated with overweight (in girls) and unrelated to vegetable intake (40–43). Of further interest, Wardle, et.al. (42) found that obese mothers prompted their children to eat less often and exerted less overall control of their child’s intake than normal weight mothers. This result directly contradicts Baughcum et.al.’s (37) study.
Longitudinal studies (n = 1)
There was one longitudinal prospective study with children birth to 9.5 years old from diverse ethnic backgrounds. Researchers found that future child overweight had bi-directional associations. First, whether a child became overweight after birth was dependent on the weight status of their parent, the parent’s control of the feeding environment, and the child’s own temperament. For thinner parents, persistent tantrums (temperament) over food by the child, and reactive overfeeding of the child by the parent created the highest risk. For overweight parents, the developmental pattern associated with parents’ low concern about their child’s thinness combined with a highly emotional child (temperament) conferred the highest risk for obesity (44).
Parental Pressure/Restricting of the Feeding Environment (n =13)
Cross-sectional studies (n = 8)
Cross-sectional studies with children and adolescents between the ages 0–17 from diverse ethnic backgrounds found that maternal pressure and restriction in the feeding environment was positively associated with child and adolescent BMI and decreased healthy dietary intake (45–51). Also, maternal restriction was positively associated with children’s BMI in the case of obese mothers, but not non-obese (49). Furthermore, Black mothers reported higher levels of restricting, pressuring to eat, and feelings of responsibility for adolescent’s weight (50). Carper et. al. (47) further found that daughters’ dietary restraint was positively associated with parental pressure to eat, while disinhibition was positively associated with parental restriction.
Two of the cross-sectional studies found that maternal pressure was inversely correlated with children’s BMI (48, 52). In Francis et.al.’s study this relationship was only significant when the mothers were normal weight and perceived their daughter’s as underweight.
Longitudinal studies (n = 5)
Longitudinal studies looking at parental pressure/restricting of the feeding environment have been conducted with primarily white children ages birth-9 years. These studies found that children with mothers who used restriction in feeding and/or pressured their child to eat had greater increase in BMI from age 5–9 (53–55). Birch, et.al. (53) and Fisher & Birch (54), further found that overweight girls at the age of 5 who received higher levels of maternal food restriction had the highest eating in the absence of hunger at age 9, and were more likely to be overweight at age 5 and 7. In contrast, Faith, et.al. (56) found that restriction by parents at age 5 predicted increased BMI at 7 years, but pressure to eat predicted reduced BMI.
Duke, et.al. (57) investigated precursors to parental pressuring and restricting. They found that parental pressure to eat for both genders was predicted by a higher level of parental body dissatisfaction at the birth of their child. For sons, three additional parental conditions predicted parental pressure and restriction to eat: minority status, parent being born outside of the US, mother’s early return to work, and authoritarian parenting style. For daughters, an early maternal pushy feeding style, parental hunger, a parental history of eating disorders and parent being born outside of the US was predictive of parental pressure and restriction.
Parental Encouraging and Modeling of Health Behaviors (n =17)
Cross-sectional studies (n = 13)
Cross-sectional studies looking at parental modeling of healthy behaviors with children ages 2–18 from diverse ethnic backgrounds found that parental modeling of healthful dietary behavior was associated with youths’ lower BMI, dietary fat intake, and higher consumption of fruits, vegetables and dairy products, and mothers serving more fruits and vegetables in the home (27, 58–64). Although, one study found these associations only with older youth (15–18 yrs. old) and not younger youth (11–14 yrs. old) (58), and two studies found that the relationships were modest to weak in magnitude (58–59). Two of the six cross-sectional studies investigating parental modeling were experimental and conducted in a laboratory setting. These studies found that children increased their liking of a novel food (including vegetables) when: the food was the same color as the adult model, when the adult was modeling the behavior, and after repeated exposure (65–66).
Three cross-sectional studies focusing on parental encouraging of health behaviors were conducted with a diverse group of 11–18 year old adolescents. Two studies found that parents’ reported encouragement to increase exercise and eat healthy were positively related to healthy dietary intake and physical activity in adolescent girls and white and black adolescent boys, although the associations were modest to weak (67–68). The other two studies looked at the effects of parental encouraging of dieting behaviors. Researchers found that adolescents who were encouraged by mothers to diet were significantly heavier. Also, boys who were encouraged to diet were more likely to be worried about gaining weight, currently dieting, and more likely to report unhealthy weight control behaviors compared to boys not encouraged to diet. White males reported the highest rates of dieting when their mothers encouraged them to diet (69).
Longitudinal studies (n = 4)
Longitudinal studies investigated parental modeling and encouraging of healthy behaviors with primarily white children ages 4–10 years old. These studies found that predicting future child BMI was related to increases in parent BMI, familial risk of overweight, parental disinhibited eating, parental restricted eating, and fathers’ enjoyment of physical activity (70–71). The relationship between physical activity and BMI was only significant in one study and was not associated with parental modeling in the other. Another longitudinal study with ethnically diverse children ages birth-8 years found that mothers’ modeling of food intake and childrens’ food preferences were significantly related over time and that mothers’ foods preferences limited which foods were offered to children (72). Neumark-Sztainer, et.al. (73) found that parents who perceived their adolescents as overweight were more likely to encourage them to diet. Parental encouragement to diet predicted poorer adolescent weight outcomes 5 years later, particularly for girls.
Summary of Parent Domain
Cross-sectional research indicates that authoritative parenting style is positively associated with child and adolescent obesity, dietary intake and physical exercise. Although these results are promising, the next important step will be for researchers to conduct more longitudinal and experimental studies to confirm cross-sectional results, identify temporal ordering of variables of interest, and use diverse socioeconomic and ethnic samples (discussed below).
Mixed results have been found for studies related to parenting practices and child and adolescent obesity. The variability in results from this review pose several questions related to measurement issues, self-report versus observational methods and confounding variables, which are discussed below. Also, several of the studies found the magnitude of the relationship between parenting practices and child/adolescent obesity to be weak or modest, and only true for certain groups (e.g. older cohort, males only, or for white and black adolescents only).
Family Functioning Domain (total n = 34)
The family functioning domain consists of the reciprocal interactions among all family members. These include the ability of the family to manage daily routines (e.g. family meals), communicate, problem-solve, be supportive and respond emotionally to each other. According to family systems theory, it is expected that families who are conflictual, cold, unsupportive, distressed and neglectful will create home environments that put children and adolescents at risk for unhealthy behaviors. The family functioning variables represented in the literature included: family meals, family connectedness/closeness, and family weight teasing.
Family meals (n = 20)
Family meals have become one of the most interesting and well-researched topics related to child and adolescent obesity. Numerous researchers have looked into family meals as a way of better understanding family functioning in relation to child and adolescent weight and weight-related behaviors. Family meals can be considered a proxy variable for measuring family functioning, in that, the organizing, preparing and eating of a family meal can be a stress inducing event. According to family systems theory, the way a family responds to a family meal is indicative of their overall family functioning. Researchers have also investigated the importance of family meals in relation to child/adolescent healthy dietary intake.
Cross-sectional studies (n = 15)
The results of the 15 cross-sectional studies will be discussed according to major findings for children and adolescents separately. There were four cross-sectional studies looking at associations between family meals and child weight and dietary intake. The age range of the children in these studies was between 5–12 years, and the majority of the participants were white. Two of the studies used direct observational methods. The main findings indicated that family meal frequency was associated with healthful dietary intake patterns, including more fruits and vegetables, less fried food and soda, less saturated and trans fat, lower glycemic load, more fiber and micronutrients from food (28, 31, 46, 76–77). Gable, & Lutz’s (28) research also found that the amount of TV viewed during family meals was associated with unhealthy dietary outcomes and obesity.
In a direct observational study, Jacobs & Fiese (77) found that families with obese children had difficulty with accomplishment, affect management, interpersonal involvement, and role division at family meals and had an increased presence of sugary beverages, shorter meal length, and fewer adults at the table. In Moens, et.al.’s (31) direct observational study, families with overweight children were found to have maladaptive control strategies and less parental support at meals versus the control group. In both of these studies, observations and self-reports differed slightly with self-reports indicating less maladaptive control strategies and more affect management and interpersonal involvement at family meals than was actually observed.
In the 10 cross-sectional studies with adolescents, 9 were conducted by the same research group. These studies were conducted with a diverse ethnic and socio-economic group of adolescents ages 11–18. Overall, the research team found that frequency of family meals was positively associated with intake of fruits, vegetables, grains, calcium rich foods, protein, calcium, iron, folate, fiber, and vitamins A, C, E, and B6, and negatively associated with soft drink consumption. Higher meal frequency and priority of family meals were also negatively associated with dieting, extreme weight control behaviors, and chronic dieting in girls (78–85). Videon & Manning (85) also found that parental presence at the evening meal was associated with higher adolescent consumption of fruits, vegetables and dairy foods, and decreased likelihood of skipping breakfast.
Researchers have also investigated the associations between television viewing and fast food on family meals. Results indicate that adolescents who watched television during family meals had lower intakes of vegetables, calcium-rich food, and grains and higher intakes of soft drinks compared to adolescents not watching television during family meals. However, watching television during family meals was still associated with more healthful diet than not eating regular family meals (86). Also, adolescents in homes with fewer than 3 fast-food family meals per week were significantly more likely than adolescents in homes with more fast-food family meals to report having vegetables and milk served with meals at home (87).
Longitudinal studies (n = 5)
Five longitudinal studies investigating the influence of family meals were conducted with a diverse ethnic and socio-economic group of youth ranging in age from 9–21. Researchers found that the frequency of family meals significantly reduced one’s odds of being overweight one year later and three years later, predicted higher intakes of fruits, vegetables, and lower intakes of soft drinks, more breakfast meals (in females), a higher priority for meal structure, and higher priority for social eating in young adulthood (88–90). Furthermore, researchers found that the frequency of family meals in adolescence was a protective factor against extreme weight control behaviors and disordered eating in young adult females (91–92).
Family Emotional Closeness/Connection (n = 9)
Cross-sectional studies (n = 9)
The cross-sectional studies investigating family closeness/connection included families with children and adolescents ages 10–18 from diverse ethnic backgrounds. Two studies used a comparison group. Family connectedness predicted lower BMI, higher breakfast consumption, more frequent family meals, lower family conflict, lower parent-child conflict specific to eating, and lower rates of emotional distress for overweight males and lower rates of extreme dieting among overweight girls (10, 26, 30, 93–96). Furthermore, Turner, et.al. (95) found that overweight girls perceived their fathers as being less caring and their mothers more caring compared to normal weight girls. In contrast, two studies found that family closeness did not distinguish between moderate and severely overweight adolescents, nor predict dietary intake, in a Dutch or Belgium sample (97–98).
Family Weight Teasing (n = 5)
Cross-sectional (n = 4)
Cross-sectional studies investigating the relationship between family weight teasing and adolescent weight and weight-related behaviors were conducted with a diverse ethnic group of adolescents ages 11–18. These researchers found that perceived family weight-teasing was significantly associated with BMI, disordered eating behaviors, low body satisfaction, low self-esteem, high depressive symptoms, and thinking about and attempting suicide, among overweight and non-overweight adolescents (99–102). Also, more Hispanic, Asian-American, and mixed/other girls reported weight teasing by family members, compared to white girls, but no difference among boys (102).
Longitudinal studies (n = 1)
One longitudinal study on family weight teasing was conducted with adolescents ages 11–18, from diverse ethnic backgrounds. Neumark-Sztainer et.al. (103) found that weight-teasing by family members, personal weight concerns, and dieting/unhealthy weight-control behaviors of adolescents strongly and consistently predicted overweight status, binge eating, and extreme weight-control behaviors 5 years later.
Summary of Family Functioning Domain
From cross-sectional and longitudinal research there is convincing evidence that family meals have an enduring protective factor for children and adolescents, girls and boys, and across diverse ethnic groups related to obesity, healthy dietary intake, and lower levels of extreme weight control behaviors (in girls). These results should allow researchers to move forward in asking questions regarding how to increase the occurrence of family meals in order for more children and adolescents to benefit from their protective factor.
Preliminary cross-sectional evidence is mixed concerning whether family connectedness/closeness is associated with obesity and health behaviors in youth. The studies that support this connection are cross-sectional and use single-group designs, making it unclear which factor preceded the other, or how both youth overweight and family functioning may be bi-directionally influencing each other.
Also, results from this review indicate that family weight teasing is associated with child/adolescent BMI, disordered eating behaviors, and low body satisfaction, but there were gender and race specific patterns that emerged that need to be explored further.
Sibling Domain (total n = 2)
The sibling domain is composed of the interactions between the offspring of the family. The relationships formed in the sibling domain are important because they tend to be the longest lasting relationship among family members—even longer than parent-child or husband-wife relationships (103). There is ample empirical evidence in the child development literature that indicates that siblings have a beneficial affect on one another’s cognitive, social, and emotional development (104). Family systems theory would also hypothesize that siblings have an impact, whether positive or negative, on each other’s health related behaviors. Sibling weight teasing was the only outcome studied in relation to the sibling domain.
Weight Teasing (n = 2)
Cross-sectional studies
There was one retrospective cross-sectional study conducted with 18 year old girls, from diverse ethnic backgrounds, assessing the effect of sibling weight teasing on weight status (105). They found that sibling weight teasing as a child was positively associated with greater maximum body size before 18. The higher rates of weight criticizing also positively correlated with emotional abuse. The other cross-sectional study with all females (majority white) found that girls who reported being teased by at least one sibling demonstrated significantly higher levels of body dissatisfaction, restriction, bulimic behaviors, depression and lower levels of self-esteem (106).
Summary of Sibling Domain
This domain is the most under-researched in connection with child and adolescent obesity. Preliminary cross-sectional studies suggest that sibling weight teasing has a significant impact on emotional health and physical health. Although there were only two cross-sectional studies on sibling teasing, the earlier research on family weight teasing also confirmed these findings. Due to the negative impact weight teasing can have on child and adolescent emotional and physical health it would be important for researchers to move to intervention work with prevention and treatment strategies to target this area of concern.
CRITIQUE AND RECOMMENDATIONS
To date, there is evidence that familial factors are correlated with child and adolescent obesity, dietary intake, physical activity and weight control behaviors. These results are promising but there are limitations in the studies related to: research design, assessment/measurement issues, units of analyses, covariates, and outcome measures. A critique of the current studies and recommendations for future research with families are relayed below.
Research Design
Critique
Of the 81 studies, 77% were cross-sectional studies and 23% were longitudinal studies. The preponderance of cross-sectional studies may be related to their lower cost. However, cross-sectional results are limited to associations between variables and an inability to examine the direction of effects. Also, stability versus change in family relationships and the impact of developmental stages or historical events on family process cannot be examined in cross-sectional studies.
Also, 88% of studies used single-group designs and only 12% used a comparison group. Although single-group designs provide useful information concerning the range of difficulties and problems obese children and adolescents experience and allow researchers to generate hypotheses for further studies, it is difficult to determine whether the problems identified are unique to having an obese child or adolescent. Comparison group designs, in which normal weight children are included, shed light on obesity-specific challenges and resources. Studies that include a normal weight comparison group contribute to the understanding of how the domains of family life contribute to child and adolescent obesity over and above the normative challenge of raising children.
Finally, only 6 of the studies (8%) in the review used direct observational methods. Direct observational methods are useful for studying variables that have consistently produced mixed results across existing studies. Variables not easily assessed accurately through self-report, such as interpersonal dynamics and bi-directional associations, may be more assessable through direct observational methods.
Recommendation
There is a need for longitudinal, experimental and direct observational research in all family domains. Because overweight and obesity has been conceptualized as a chronic condition (107), studies that follow the same children and families over time would provide much greater understanding of which families and children/adolescents struggle with what issues at which points in time. Longitudinal studies, with comparison groups, provide the strongest evidence for causality. Identifying causal pathways will also provide a stronger evidence-base for building obesity prevention and treatment programs targeting youth obesity. There is also a need for home observational studies to be conducted. Such studies will help to determine what behaviors are truly being used in the home and will contribute towards creating a more accurate definition of the behaviors of interest and their impact. These studies, however, are often costly and time-consuming to conduct. Observational studies in the laboratory setting are another alternative, but there is a question of validity regarding the behaviors being evaluated and whether these findings can be applied to real-world situations. Given these challenges, future studies need to consider the implications of their study design and how it will add to or clarify the existing body of literature in this area.
It would also be beneficial for future studies to incorporate mixed qualitative and quantitative designs. Elder & Conger (108) suggest that a descriptive picture through qualitative analyses and detailed statistical analyses can contribute greater understanding of family systems phenomena. Studies that integrate variable and case-centered approaches lead to a more thorough understanding of the underlying dynamics of complex relationships, such as family systems (109–110). Such a combination allows for a focus on individual life stories (case-centered approach) and group comparisons (variable centered approach).
Assessments
Self-report assessments were used in 92% of the studies (n = 71) and direct observational measures were used in 8% of the studies (n = 6). Table 2 lists the standardized assessment instruments used in the studies by family domain. The majority of studies (67%) used anthropometric measures of child BMI, calculated as the ratio kg/m2 and transformed into BMI z-scores (standardizes BMI across age and sex to allow for comparisons among different ages and sexes), 29% used self-report of BMI either by parent or youth, and 4% did not measure BMI. Also, there was strong agreement between studies regarding the definition of obesity and overweight. The majority of studies (93%) based their definition of obese vs. at risk for being overweight on the Centers for Disease Control and Prevention’s (CDC) guidelines or the American Medical Association’s (AMA) guidelines. A few studies (7%) used more rigorous measures such as Dual X-ray Absorptiometry (DEXA) body scans or skin fold thickness.
Table 2.
Measures used to Study Family Domains in Child and Adolescent Obesity
| Family Domain Measured |
Factors Assessed | Standardized Assessments Used |
|---|---|---|
| Parental | ||
| Parenting Styles | Child Rearing Practices Report (CRPR) | |
| Parenting Dimensions Inventory (PDI-S) | ||
| Attitudes Toward Child-Rearing Scale | ||
| Ghent Parental Behaviour Scale-GPBS | ||
| Parental Control of Food Environment |
Parental Control Index | |
| Parental Pressure/Restriction |
Original Child Feeding Questionnaire (CFQ) |
|
| Child Feeding Questionnaire (CFQ) | ||
| Comprehensive Feeding Practices Questionnaire |
||
| Child Eating Behavior Questionnaire | ||
| Caregiver’s Feeding Style Questionnaire (CFSQ) |
||
| Free Access Procedure | ||
| Food Frequency Questionnaire | ||
| Family | ||
| Emotional/Closeness or Conflict |
Family Assessment Device (FAD) | |
| Family Environment Scale (FES) | ||
| Family Adaptability and Cohesion Scale (FACES) |
||
| Family Dimension Scale (FDS) | ||
| Family Meals | McMaster Mealtime Family Interaction Coding System (MICS) |
|
Critique
One methodological concern with the studies in this review was the almost exclusive reliance on single informant measures to measure family-level data. The use of single informants is particularly problematic with measures that are based on global subjective items. Bulcroft & White (111) called this problem the “individualistic fallacy,” which occurs when individual units are analyzed and generalizations are made to group level relationships or properties. For instance, in many of the studies concerning family functioning or parenting style, only the child/adolescent or mother answered the questions, thus reporting only their perception of parenting style or family functioning, rather than assessing more, or all, of the family members to produce a more representative and accurate measure. A sole informant for multiple measures often inflates associations because of informant bias. Surveying multiple family members not only reduces informant bias but also provides a more systemic view of family relationships. In the studies that included paternal data (32%) there were not equal numbers of mother and father reports. Thus, the responses of a small number of fathers was collapsed into the larger number of mother responses, and the ratings were then categorized as “parent reports.” The practice of using these parent reports is questionable because fathers tend to report different, usually lower, rates of problems. Furthermore, the reports of two parents from the same family are not independent, thereby violating assumptions that often underlie statistical tests. Another concern with many of the studies was their use of single item measures (51%). Many of these studies were large, epidemiological studies. Although survey research with large community-based samples have realistic limitations related to survey length and participant fatigue, using single item measures can become problematic when trying to measure complex concepts like parenting style or family emotional closeness.
Recommendation
There is a need for more within-in family measurements that utilize multi-level and multi-measurement approaches. The inclusion of data from multiple informants (e.g. both parents, the child/adolescent, and siblings) would provide a more systemic picture of the family’s functioning. Multiple assessments also allow for the identification of specific, nonshared risk factors that may account for differential development of weight problems within the family system. In other research on children and adolescents, it has been shown that there is a low level of agreement among parent, sibling, and child reports on behavioral and psychological problems in children (112). Given the low agreement between informants, it is likely that various individuals provide different and equally valuable information, and using multiple informants to assess family domains more comprehensively would be beneficial. Also, standardized measures of family functioning (full scales or sub-scales) with sound psychometric properties, rather than single item measures need to be used. Relying on these measures will help with construct definition and measurement problems, in order to compare results across studies more accurately.
Units of Analysis
Critique
Most of the studies focused on the parent-child domain (61%). The family domain (37%) and sibling domain (2%) were underrepresented in the studies reviewed. However, even when an assessment focused on whole family functioning, such as family conflict or closeness, the respondent was one member of the family, usually the mother. There was little attempt to combine individual reports to create a meaningful family-level measure. Thus, there was limited family-level data in order to assess bi-directional associations between the three family domains and child and adolescent obesity outcomes.
Recommendation
There is a need to use systemic outcome variables. More family system variables should be studied, such as communication, boundaries, triangulation, self-regulation of the system, and so on. It would also be important for researchers to examine possible mediator or moderator effects of the family domains.
In this review, the preliminary evidence suggests that compared to normal weight youth, overweight youth are more likely to experience more nonauthoritative parenting, more family conflict, less family emotional closeness, more restrictive feeding styles, less parental modeling of health behaviors, and more weight teasing. The direction of cause and effect is still unclear, in that, the family domains may contribute to negative health behaviors associated with obesity, but the child/adolescent’s overweight condition may also effect negative changes in the family. It is most likely that there are bi-directional associations at work, and future research needs to appreciate these bi-directional associations occurring between the three family domains by incorporating these potential relationships into their study design. Also, the sibling domain needs to be further investigated. Because of the enduring relationships in this domain it would be important to better understand the impact of sibling relationships on child and adolescent obesity.
Covariates and Moderator/Mediator Effects
Critique
The majority of the studies (81%) adjusted for gender, SES and ethnicity as covariates, but left out other influential covariates such as maternal BMI and parental perception of child/adolescent weight, which may represent an overlooked characteristic in families that may have a moderating/mediating effect. Using covariates is important in all research designs, but especially with experimental and longitudinal studies. Experimental studies, where an independent variable is manipulated, while all other variables, including covariates, are held constant across experiment and control group provide the strongest evidence for causality. There were only 7 studies in the review that accomplished this. Also, the longitudinal studies in this review were commonly based on observational or survey data. This can make them susceptible to spurious relationships if all relevant covariates are not accounted for.
Recommendation
Studies need to continue to use covariates in their research on familial correlates of child and adolescent obesity. Because of the multiple levels within the family system and the potential bi-directional associations within family relationships, it would be important to use covariates in order to reduce confounding results. Gender, SES and ethnicity are typically used in these analyses and should be continued to be used. Other covariates such as maternal weight, education, or years in the country may also be used to underlie the importance of measurement and analysis of appropriate covariates to fully account for third-variable effects. Investigating mediator or moderator effects would also be important. Several family domains had inconsistent findings that need to be explored further. It may be that other variables that moderate or mediate the association were not investigated. Testing mediator/moderator effects will allow researchers to determine in what situations the associations among variables are stronger or weaker, to differentiate between direct and indirect (mediated) effects, and to account for the relationship between the IV and DV (moderator).
Future Questions to be Asked by Researchers
Based on the results from each of the family systems reviewed, several interesting questions for future research are warranted. First, for the parenting domain, it would be interesting to help tease out the mixed results found with the parenting practices research by looking at potential confounders. For instance, questions related to the impact of child weight and parent weight would be useful, including: (a) do mothers pressure their thinner children to eat, whereas they are concerned about their heavier children and restrict, thus eliciting either restrictive or pressured environments overtime? or, (b) do mothers restrict with their children because they are heavier themselves and don’t want their children to become heavy? Also, related to studies of parental control of the feeding environment it may be important to look at the difference between overt and covert control.
Second, future research questions related to family meals and weight teasing in the family domain that would be of interest, include: (a) does it matter which meal is the family meal, or what time of day the family meal is eaten? (b) does it matter which parent is present at the meal? (c) does it matter if the meal is home cooked versus pre-packaged or fast-food? (d) does it matter what the atmosphere of the family meal is like (e.g. TV watching, music playing)? Future research questions about family weight teasing include: (a) does it matter which family member does the teasing? (b) does peer weight teasing or family weight teasing have a stronger impact? Also, general questions about family lifestyle/habits related to weight, diet and activity patterns and how they affect children/adolescents’ weight status are needed.
Finally, interesting future research questions related to the sibling domain include: (a) what impact (positive and negative) do siblings have on each other related to food preferences, dietary intake and physical exercise? (b) does the relationship with a sibling have a stronger association with dietary intake and exercise compared to a parent, or a same aged peer? (c) are there any differences in parent feeding style between first, second, or later born children?
CONCLUSION
This review found that factors within the parental, family and sibling domains have significant associations with child and adolescent obesity. Although many factors within these domains are in need of further research, there remain numerous useful findings to guide future research. Parenting styles and family meals have been well-researched and provide exemplary studies to guide researchers. Also, in future research the importance of bi-directional associations cannot be overlooked in understanding the reciprocal effects of familial factors on child and adolescent health behaviors.
Acknowledgement
Research is supported by a Building Interdisciplinary Research Careers in Women’s Health Grant administered by the Deborah E. Powell Center for Women’s Health at the University of Minnesota. The project described is supported by Grant Number K12HD055887 from the National Institutes of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
References
- 1.Ogden C, Flegal K, Carroll M, Johnson C. Prevalence and trends in overweight among U.S. children and adolescents, 1999–2002. JAMA. 2003;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.The US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001. [Google Scholar]
- 4.Sheehan TJ, DuBRava S, DeChello LM, Fang Z. Rates of weight change for black and white Americans over a twenty year period. International Journal of Obesity. 2003;27:498–504. doi: 10.1038/sj.ijo.0802263. [DOI] [PubMed] [Google Scholar]
- 5. [Accessed July 27, 2008];Expert Committee Recommendations on the Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity. http://www.ama assnorg/ama1/pub/upload/mm/433/ped_obesity_recs.pdf.
- 6.Kitzman KM, Dalton WT, Buscemi J. Beyond parenting practices: Family context and the treatment of pediatric obesity. Family Relations. 2008;57:13–23. [Google Scholar]
- 7.Lindsay AC, Sussner KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Future Child. 2006;16(1):169–186. doi: 10.1353/foc.2006.0006. [DOI] [PubMed] [Google Scholar]
- 8.Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics. 2006;117:2047–2054. doi: 10.1542/peds.2005-2259. (2006) [DOI] [PubMed] [Google Scholar]
- 9.Woods BL, Miller BD. Families, health and illness: The search for mechanisms within a systems paradigm. In: Pinsof WM, Lebow JL, editors. Family Psychology: The Art of the Science. New York: Oxford University Press; 2005. pp. 493–520. [Google Scholar]
- 10.Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors on the obesigenic environment. Obesity. 2007;15:126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 11.Golan M, Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004;62(1):39–50. doi: 10.1111/j.1753-4887.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 12.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? International Journal of Behavioral Nutrition and Physical Activity. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faith MS, Berkowitz RL, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental feeding attitudes and styles and child body mass index: Prospective analysis of a gene-environment interaction. Pediatrics. 2003;114(4):429–436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- 14.Lindsay AC, Sussner KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Future Child. 2006;16(1):169–186. doi: 10.1353/foc.2006.0006. [DOI] [PubMed] [Google Scholar]
- 15.Benton D. Role of parents in the determination of the food preferences of children and the development of obesity. International Journal of Obesity. 2004;28:858–869. doi: 10.1038/sj.ijo.0802532. [DOI] [PubMed] [Google Scholar]
- 16.Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615:11–37. (2008) [Google Scholar]
- 17.Bertalanffy LV. Theoretical models in biology and psychology. In: Krech D, Klein GS, editors. Theoretical Models and Personality Theory. Durham, NC: Duke University Press; 1953. pp. 24–38. [Google Scholar]
- 18.Minuchin S. Families and Family Therapy. Cambridge, MA: Harvard University Press; 1974. [Google Scholar]
- 19.Whitchurch GG, Constantine LL. Systems Theory. In: Boss PG, Doherty WJ, LaRossa R, Schumm WR, Steinmetz SK, editors. Sourcebook of Family Theories and Methods: A Contextual Approach. New York, NY: Plenum Press; 1993. pp. 325–355. [Google Scholar]
- 20.Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behaviors in U.S. adults. Preventive Medicine. 2003;36:615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- 21.Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behaviour. Exerc Sport Sci Rev. 2000;27:153–158. [PubMed] [Google Scholar]
- 22.Darling N, Steinberg L. Parenting style as context: An integrative model. Psychological Bulletin. 1993;113:487–496. [Google Scholar]
- 23.Baumrind D. Rearing competent children. In: Damon, editor. Child Development Today and Tomorrow. San Francisco: Josey-Bass; 1989. pp. 349–378. [Google Scholar]
- 24.Maccoby EE. Parenting and its effects on children: On reading and misreading behavior genetics. Annual Reviews of Psychology. 2000;51:1–27. doi: 10.1146/annurev.psych.51.1.1. [DOI] [PubMed] [Google Scholar]
- 25.Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Education Research. 2006;21(6):862–871. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Kennedy C. Family functioning, parenting style, and Chinese children’s weight status. Journal of Family Nursing. 2004;10:262–279. (2004) [Google Scholar]
- 27.Berge JM, Wall M, Bauer K, Neumark-Sztainer D. Parenting Characteristics in the Home Environment and Adolescent Obesity: A Latent Class Analysis. doi: 10.1038/oby.2009.324. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gable S, Lutz S. Household, parent and child contributions to childhood obesity. Family Relations. 2000;4:293–300. [Google Scholar]
- 29.Kremers SPJ, Brug J, deVries H, Engels RCME. Parenting style and adolescent fruit consumption. Appetite. 2003;41:43–50. doi: 10.1016/s0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- 30.Mellin AE, Neumark-Sztainer D, Story M, Ireland M, Resnick MD. Unhealthy behaviors and psychosocial difficulties among overweight adolescents: The potential impact of familial factors. Journal of Adolescent Health. 2002;31:145–153. doi: 10.1016/s1054-139x(01)00396-2. [DOI] [PubMed] [Google Scholar]
- 31.Moens E, Braet C, Soetens B. Observation of family functioning at mealtime: A comparison between families of children with and without overweight. Journal of Pediatric Psychology. 2007;32(1):52–63. doi: 10.1093/jpepsy/jsl011. [DOI] [PubMed] [Google Scholar]
- 32.Schmitz KH, Lytle LA, Phillips GA, Murray DM, Birnbaum AS, Kubik MY. Psychosocial correlates of physical activity and sedentary leisure habits in young adolescents: The Teens Eating for Energy and Nutrition at School Study. Preventive Medicine. 2002;34:266–278. doi: 10.1006/pmed.2001.0982. [DOI] [PubMed] [Google Scholar]
- 33.van der Horst K, Kremers S, Ferreira I, Singh A, Oenema A, Brug J. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Education Research. 2007;22(2):295–304. doi: 10.1093/her/cyl080. [DOI] [PubMed] [Google Scholar]
- 34.Hughes SO, Power TG, Fisher JO, Mueller S, Nicklas TA. Revisiting a neglected construct: Parenting styles in a child-feeding context. Appetite. 2005;44:83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 35.Patrick H, Nicklas TA, Hughes SO, Morales M. The benefits of authoritative feeding style: Caregiver feeding styles and children’s food consumption patterns. Appetite. 2005;44:243–249. doi: 10.1016/j.appet.2002.07.001. [DOI] [PubMed] [Google Scholar]
- 36.Berge JM, Wall M, Neumark-Sztainer D, Loth K. Parenting Style as a Predictor of Adolescent Weight and Weight-Related Behaviors. doi: 10.1016/j.jadohealth.2009.08.004. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baughcum AE, Powers SW, Johnson SB, Chamberlin LA, Deeks CM, Jain A, Whitaker RC. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. Journal of Developmental and Behavioral Pediatrics. 2001;22(6):391–408. doi: 10.1097/00004703-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Brown R, Ogden J. Children’s eating attitudes and behaviour: A study of the modeling and control theories of parental influence. Health Education Research. 2004;19(3):261–271. doi: 10.1093/her/cyg040. [DOI] [PubMed] [Google Scholar]
- 39.Nicklas TA, Yang S, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: The Bogalusa Study. American Journal of Preventative Medicine. 2003;25(1):9–16. doi: 10.1016/s0749-3797(03)00098-9. [DOI] [PubMed] [Google Scholar]
- 40.Lumeng JC, Burke LM. Maternal prompts to eat, child compliance, and mother and child weight status. The Journal of Pediatrics. 2006;12:330–335. doi: 10.1016/j.jpeds.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 41.Robinson TN, Kiernan M, Matheson DM, Haydel KF. Is parental control over children’s eating associated with childhood obesity? Results from a population-based sample of third graders. Obesity Research. 2001;9(5):306–312. doi: 10.1038/oby.2000.38. [DOI] [PubMed] [Google Scholar]
- 42.Wardle J, Sanderson S, Guthrie CA, Rapoport L, Plomin R. Parental feeding style and the intergenerational transmission of obesity risk. Obesity Research. 2000;10(6):453–462. doi: 10.1038/oby.2002.63. [DOI] [PubMed] [Google Scholar]
- 43.Wardle J, Carnell S, Cooke L. Parental control over feeding and children’s fruit and vegetable intake: How are they related? Journal of the American Dietetic Association. 2006;105(2):227–232. doi: 10.1016/j.jada.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 44.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. Journal of Pediatrics. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 45.Bourcier E, Bowen DJ, Meischke H, Moinpour C. Evaluation of strategies used by family food preparers to influence healthy eating. Appetite. 2003;41:265–272. doi: 10.1016/s0195-6663(03)00104-1. [DOI] [PubMed] [Google Scholar]
- 46.Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. International Journal of Obesity. 2006;30:1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- 47.Carper JL, Fisher JO, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 35:121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 48.Francis LA, Hofer SM, Birch L. Predictors of maternal child-feeding style: maternal and child characteristics. Appetite. 2001;37:231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- 49.Powers SW, Chamberlain LA, van Schaick KB, Sherman SN, Whitaker RC. Maternal feeding strategies, child eating behaviors, and child BMI in low-income African-American preschoolers. Obesity. 2006;14:2026–2033. doi: 10.1038/oby.2006.237. [DOI] [PubMed] [Google Scholar]
- 50.Spruijt-Metz D, Lindquist CH, Birch LL, Fisher JO, Goran MI. Relation between mothers’ child-feeding practices and children’s adiposity. American Journal of Clinical Nutrition. 2002;75:581–586. doi: 10.1093/ajcn/75.3.581. [DOI] [PubMed] [Google Scholar]
- 51.Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. American Journal of Clinical Nutrition. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matheson DM, Robinson TN, Varady A, Killen JD. Do Mexican-American Mothers’ food-related parenting practices influence their children’s weight and dietary intake? Journal of the American Dietetic Association. 2006;106(11):1861–1865. doi: 10.1016/j.jada.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 53.Birch LL, Fisher JO, Davison KK. Learning to overeat: Maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. American Journal of Clinical Nutrition. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fisher JO, Birch LL. Eating in the absence of hunger. Am J Clin Nutr. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee Y, Mitchell DC, Smiciklas-Wright H, Birch LL. Diet quality, nutrient intake, weight status, and feeding environments of girls meeting or exceeding recommendations for total dietary fat of the American Academy of Pediatrics. Pediatrics. 2001;107(6):95–102. doi: 10.1542/peds.107.6.e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Faith MS, Berkowitz RL, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental feeding attitudes and styles and child body mass index: Prospective analysis of a gene-environment interaction. Pediatrics. 2003;114(4):429–436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- 57.Duke RE, Bryson S, Hammer LD, Agras WS. The relationship between parental factors at infancy and parent-reported control over children’s eating at age 7. Appetite. 2004;43(3):247–252. doi: 10.1016/j.appet.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 58.Arcan C, Neumark-Sztainer D, Hannan P, van den Berg P, Story M, Larson N. Parental eating behaviors, home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutrition. 2007;10:1257–1265. doi: 10.1017/S1368980007687151. [DOI] [PubMed] [Google Scholar]
- 59.Boutelle KN, Birkeland RW, Hannan PJ, Story M, Neumark-Sztainer D. Associations between Maternal Concern for Healthful Eating and Maternal Eating Behaviors, Home Food Availability, and Adolescent Eating Behaviors. Journal of Nutrition Education and Behavior. 2007;39:248–256. doi: 10.1016/j.jneb.2007.04.179. [DOI] [PubMed] [Google Scholar]
- 60.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. Journal of American Dietary association. 2002;102:58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutrition. 2005;8:77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- 62.Reinaerts E, de Nooijer J, Candel M, deVries N. Explaining school children’s fruit and vegetable consumption: The contributions of availability, accessibility, exposure, parental consumption and habit in addition to psychosocial factors. Appetite. 2006;48:248–258. doi: 10.1016/j.appet.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 63.Tibbs T, Haire-Joshu D, Schechtman KB, Brownson RC, Nanney MS, Houston C, Auslander W. The relationship between parental modeling, eating patterns, and dietary intake among African-American parents. Journal of the American Dietetic Association. 2001;101:535–541. doi: 10.1016/S0002-8223(01)00134-1. [DOI] [PubMed] [Google Scholar]
- 64.Keller B, Miner JL, Wigglesworth JK. The role of parents in factors that contribute to obesity in children. Medicine & Science in Sports & Exercise. 2004;36(5):S51. [Google Scholar]
- 65.Addessi E, Galloway AT, Visalbeghi E, Birch LL. Specific social influences on the acceptance of novel foods in 2–5 year old children. Appetite. 2005;45:264–271. doi: 10.1016/j.appet.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 66.Wardle J, Cooke LJ, Gibson EL, Sapochnik M, Sheiham A, Lawson M. Increasing children’s acceptance of vegetables; a randomized trial of parent-led exposure. Appetite. 2003;40:155–162. doi: 10.1016/s0195-6663(02)00135-6. [DOI] [PubMed] [Google Scholar]
- 67.McGuire MT, Hannan PJ, Neumark-Sztainer D, Falkner Crossrow NH, Story M. Parental correlates of physical activity in a racially/ethnically diverse adolescent sample. Journal of Adolescent Health. 2002;30:253–261. doi: 10.1016/s1054-139x(01)00392-5. [DOI] [PubMed] [Google Scholar]
- 68.Crawford D, Timperio A, Telford A, Salmon J. Parental concerns about childhood obesity and the strategies employed to prevent unhealthy weight gain in children. Public Health Nutrition. 2006;9(7):889–895. doi: 10.1017/phn2005917. [DOI] [PubMed] [Google Scholar]
- 69.Fulkerson J, McGuire MT, Neumark-Sztainer D, Story M, French SA, Perry CL. Weight-related attitudes and behaviors of adolescent boys and girls who are encouraged to diet by their mothers. International Journal of Obesity. 2002;26:1579–1587. doi: 10.1038/sj.ijo.0802157. [DOI] [PubMed] [Google Scholar]
- 70.Davison KK, Birch LL. Child and parent characteristics as predictors of change in girls’ body mass index. International Journal of Obesity. 2001;25:1834–1842. doi: 10.1038/sj.ijo.0801835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hood MY, Moore LL, Sundarajan-Ramamurti A, Singer M, Cupples LA, Ellison RC. Parental attitudes and the development of obesity in children. The Framingham Children’s Study. International Journal of Obesity. 2000;24:1319–1325. doi: 10.1038/sj.ijo.0801396. [DOI] [PubMed] [Google Scholar]
- 72.Skinner JD, Carruth BR, Bounds W, Ziegler PJ. Children’s food preferences: A longitudinal analysis. Journal of American Dietary Association. 2002;102:1638–1647. doi: 10.1016/s0002-8223(02)90349-4. [DOI] [PubMed] [Google Scholar]
- 73.Neumark-Sztainer D, Wall M, Story M, van den Berg P. Accurate parental classifications of overweight adolescents' weight status: Does it matter? Pediatrics. 2008;121:1495–1502. doi: 10.1542/peds.2007-2642. (e) [DOI] [PubMed] [Google Scholar]
- 74.Field AE, Camargo CA, Jr, Taylor B, Berkey CS, Frazier AL, Gilman MW. Overweight, weight concerns, and bulimic behaviors among girls and boys. J Am Acad Child Adolesc Psych. 1999;38:754–760. doi: 10.1097/00004583-199906000-00024. [DOI] [PubMed] [Google Scholar]
- 75.McKnight Investigators. Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight Longitudinal Risk Factor Study. Am J Psychiatry. 2003;160:248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- 76.Gillman MW, Rifas-Shiman SL, Frazier AL, Rockett HRH, Camargo CA, Field AE, Berkley CS, Colditz GA. Family dinner and diet quality among older children and adolescents. Archives of Family Medicine. 2008;9:235–240. doi: 10.1001/archfami.9.3.235. [DOI] [PubMed] [Google Scholar]
- 77.Jacobs MP, Fiese BH. Family mealtime interactions and overweight children with asthma: Potential for compounded risks? Journal of Pediatric Psychology. 2007;32(1):64–68. doi: 10.1093./jpepsy/jsl026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, Bearinger LH. Correlations between family meals and psychosocial well-being among adolescents. Archives of Pediatric and Adolescent Medicine. 2004;158:792–796. doi: 10.1001/archpedi.158.8.792. [DOI] [PubMed] [Google Scholar]
- 79.Neumark-Sztainer D, Story M, Ackard D, Moe J, Perry C. Family meals among adolescents: Finding from a pilot study. Journal of Nutrition Education. 2000;32:335–340. [Google Scholar]
- 80.Fulkerson JA, Neumark-Sztainer D, Story M. Adolescent and parent views of family meals. Journal of the American Dietetic Association. 2006;106(4):526–532. doi: 10.1016/j.jada.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 81.Fulkerson JA, Story M, Mellin A, Leffert N, Neumark-Sztainer D, French SA. Family dinner meal frequency and adolescent development: Relationships with developmental assets and high-risk behaviors. Journal of Adolescent Health. 2006;39:337–345. doi: 10.1016/j.jadohealth.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 82.Neumark-Sztainer D, Hannan PJ, Story M, Croll J. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. Journal of the American Dietetic Association. 2003;103:317–322. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 83.Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. tAre family meal patterns associated with disordered eating behaviors among adolescents? Journal of Adolescent Health. 2004;35:350–359. doi: 10.1016/j.jadohealth.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 84.Neumark-Sztainer D, Story M, Ackard D, Moe J, Perry C. Family meals among adolescents: Finding from a pilot study. Journal of Nutrition Education. 2000;32:335–340. [Google Scholar]
- 85.Videon TM, Mannung CK. Influences on adolescent eating patterns: The importance of family meals. Journal of Adolescent Health. 2003;32:365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- 86.Feldman S, Eisenberg ME, Neumark-Sztainer D, Story M. Associations between watching TV during family meals and dietary intake among adolescents. Journal of Nutrition, Education and Behavior. 2007;39(5):257–263. doi: 10.1016/j.jneb.2007.04.181. [DOI] [PubMed] [Google Scholar]
- 87.Boutelle KN, Fulkerson JA, Neumark-Sztainer D, Story M, French S. Fast food for family meals: Relationships with parent and adolescent food intake, home food availability and weight status. Public Health Nutrition. 2007;10(1):16–23. doi: 10.1017/S136898000721794X. [DOI] [PubMed] [Google Scholar]
- 88.Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. Journal of the American Dietetic Association. 2007;107:1502–1510. doi: 10.1016/j.jada.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 89.Sen B. Frequency of family dinner and adolescent body weight status: Evidence from the National Longitudinal Survey of Youth, 1997. Obesity. 2006;14(12):2266–2276. doi: 10.1038/oby.2006.266. [DOI] [PubMed] [Google Scholar]
- 90.Taveras EM, Rifas-Shiman SL, Berkley CA, Rockett HRH, Field AE, Frazier AL, Colditz GA, Gillman MW. Family dinner and adolescent obesity. Obesity Research. 2005;13(5):900–906. doi: 10.1038/oby.2005.104. [DOI] [PubMed] [Google Scholar]
- 91.Neumark-Sztainer D, Eisenberg MA, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents. Archives of Pediatric Adolescent Medicine. 2004;162(1):17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- 92.Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: Longitudinal findings from Project EAT. Archives of Pediatrics and Adolescent Medicine. 2008;162:17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- 93.Berge JM, French S, Gerlach A. Family Cohesion, Home Environment and Behaviors Associated with Child Obesity. in press. [Google Scholar]
- 94.Lamerz A, Kuepper-Nybelen J, Wehle C, Bruning N, Trost-Brinkhues G, Brenner H, Hebebrand J, Herpertz-Dahlman B. Social class, parental education, and obesity prevalence in study of 6-year old children in Germany. International Journal of Obesity. 2005;(29):373–380. doi: 10.1038/sj.ijo.0802914. [DOI] [PubMed] [Google Scholar]
- 95.Turner HM, Rose KS, Cooper MJ. Schema and parental bonding in overweight and nonoverweight female adolescents. International Journal of Obesity. 2005;29:381–387. doi: 10.1038/sj.ijo.0802915. [DOI] [PubMed] [Google Scholar]
- 96.Vieweg VR, Johnston CH, Lanier JO, Fernandez A, Pandurangi AK. Correlation between high risk obesity groups and low socioeconomic status in school children. Southern Medical Journal. 2007;100(1):8–13. doi: 10.1097/01.smj.0000253479.03665.6f. [DOI] [PubMed] [Google Scholar]
- 97.Bourdeaudhuij ID, Van Oost P. Personal and family determinants of dietary behaviour in adolescents and their parents. Psychology and Health. 2000;15:751–770. [Google Scholar]
- 98.Stradmeijer M, Bosch J, Koops W, Seidell J. Family functioning and psychosocial adjustment in overweight youngsters. International Journal of Eating Disorders. 2000;27:110–114. doi: 10.1002/(sici)1098-108x(200001)27:1<110::aid-eat14>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 99.Eisenberg M, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Archives of Pediatrics and Adolescent Medicine. 2003;157:733–738. doi: 10.1001/archpedi.157.8.733. [DOI] [PubMed] [Google Scholar]
- 100.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan P, Mulert S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity. 2002;1 doi: 10.1038/sj.ijo.0801853. 123-13. [DOI] [PubMed] [Google Scholar]
- 101.Libbey HP, Story MT, Neumark-Sztainer DR, Boutelle KN. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity. 2008;16 Supplement 2:S24–S29. doi: 10.1038/oby.2008.455. [DOI] [PubMed] [Google Scholar]
- 102.van den Berg P, Neumark-Sztainer D, Eisenberg ME, Haines J. Racial/ethnic differences in weight-related teasing in adolescents. Obesity. 2008;16 Supplement 2:S3–S10. doi: 10.1038/oby.2008.445. [DOI] [PubMed] [Google Scholar]
- 103.Neumark-Sztainer D, Wall M, Haines J, Story M, Sherwood NE, van den Berg P. Shared risk and protective factors for overweight and disordered eating in adolescents. American Journal of Preventive Medicine. 2007;33:359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 104.Noller P. Sibling relationships in adolescence: Learning and growing together. Personal Relationships. 2005;12:1–22. [Google Scholar]
- 105.Taylor CB, Bryson S, Doyle AAC, Luce KH, Cunning D, Abascal LB, Rockwell R, Field AE, Striegel-Moore R, Winselberg AJ, Wilfley DE. The adverse effect of negative comments about weight and shape from family and siblings on women at high risk for eating disorders. Pediatrics. 2006;118:731–738. doi: 10.1542/peds.2005-1806. [DOI] [PubMed] [Google Scholar]
- 106.Keery H, Boutelle K, van den Berg P, Thompson JK. The impact of appearance-related teasing by family members. Journal of Adolescent Health. 2005;37:120–127. doi: 10.1016/j.jadohealth.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 107.Rippe JM, Crossley S, Ringer R. Obesity as a chronic disease: Modern medical and lifestyle management. Journal of the American Dietetic Association. 1998;98:S9–S15. doi: 10.1016/s0002-8223(98)00704-4. [DOI] [PubMed] [Google Scholar]
- 108.Elder GH, Conger RD. Children of the Land: Adversity and Success in Rural America. Chicago: University of Chicago Press; 2001. [Google Scholar]
- 109.Grimm LG, Yarnold PR. Reading and Understanding MORE Multivariate Statistics. Washington, DC: American Psychological Association; 2000. [Google Scholar]
- 110.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Needham Heights MA: Allyn & Bacon; 2001. [Google Scholar]
- 111.Bulcroft RA, White JM. Family research methods and levels of analysis. Family Science Review. 1997;10:136–153. [Google Scholar]
- 112.Thompson RJ, Gustafson KE. Adaptation to Chronic Childhood Illness. Washington, DC: American Psychological Association; 1996. [Google Scholar]