Abstract
Background
Whole-body magnetic resonance imaging (WB-MRI) is a modern imaging method, free of ionizing radiation, which provides high-resolution display of individual organ systems and of the anatomy of the entire body.
Methods
Selective literature review
Results
Multi-channel WB-MRI scanners enable both the high-resolution imaging of the entire body and focused studies of individual organs, through the use of various sequence techniques and contrast modes. The initial application of combined cardiovascular and oncological imaging protocols for the screening of asymptomatic persons has already revealed many cases of cardiovascular disease and of tumors with serious clinical implications. The diagnostic accuracy of M staging with WB-MRI lies in the range of 93% to 97%. WB-MRI provides good contrast of the bone marrow, and has thus been used for the diagnosis of malignant bone marrow disease as well: in particular, it is especially sensitive for multiple myeloma and plays an important role in prognostication and therapeutic decision-making in this disorder. To date, WB-MRI has not been shown to be superior to other diagnostic techniques with respect to hard endpoints, such as prolongation of survival. It also carries the risk of false positive findings.
Conclusion
Despite these encouraging results, undirected screening by WB-MRI without an appropriate indication, as is currently being practiced in many institutions, is decidedly inadvisable in view of its predicted diagnostic yield below 2% and the lack of evidence for its cost-effectiveness.
The recent introduction of whole-body magnetic resonance imaging (WB-MRI) has profoundly changed the diagnostic concepts for various systemic diseases. In clinical practice, whole-body imaging is increasingly being used as a routine alternative to incremental, multimodal diagnostic imaging, particularly for comprehensive evaluation of malignant diseases. The introduction of modern whole-body MR scanners has paved the way for clinically practicable and efficient WB-MRI. Moreover, innovations in sequence design and image acquisition have significantly reduced examination times with no loss of image quality. High-resolution MRI of various organ systems with appropriate contrast and the corresponding contrast-medium dynamics can be combined with head-to-toe anatomical coverage. This article presents the findings of a selective literature review on recent technical innovations in the field of WB-MRI and the clinical uses of this new method, with particular emphasis on diagnostic imaging in oncology. Furthermore, potential false indications are critically reviewed.
Technical advances in WB-MRI
The differing demands on examination set-up posed by various parts of the body meant that MRI was previously used principally to assess focal lesions in a circumscribed anatomical region. A further limiting factor was the time required: Examinations typically took more than an hour, because the patient had to be repositioned repeatedly.
Advances in receiver coils and higher field strength
The introduction of 1.5-T multichannel WB-MR scanners in combination with free, automatic table motion now enables high-resolution WB-MRI from head to toe in less than 1 h. These scanners are furnished with receiver coils that cover the whole body with a matrix of flexible individual elements. This permits whole-body examination of a patient of up to 205 cm (80.7 in.) in height without any repositioning. Thus not only high-resolution WB-MR images can be obtained, but also focused examinations of individual organs, e.g., abdominal organs, lungs, brain, or skeletal system, with differing sequences and contrasts.
Modern whole-body systems with field strength of 3 T have become increasingly available over the past few years. This theoretical doubling of image signal compared with 1.5-T scanners can be exploited either to shorten examination time still further or to improve spatial resolution (1).
WB-MRI with continuous table motion
The year 2002 saw the introduction of MRI data acquisition during continuous movement of the table, similar to the examination technique in computed tomography (CT) (2). In contrast to CT, MRI faces the challenge that in most sequences it is not possible to acquire a complete measurement slice with every movement of the table. This means that the raw data have to be buffered prior to complete acquisition of the slice, with the table moving during acquisition of image data. Moreover, the specific acquisition and adjustment parameters now have to be altered and adapted during table movement. Nevertheless, this method possesses enormous potential. Extensive anatomical regions can be swiftly acquired in a seamless series of images over a short time, thus making redundant the conventional incremental imaging of individual parts of the body.
Protocol design
A comprehensive WB-MRI protocol for oncological diagnosis must be based on sequence techniques with high soft-tissue and bone-marrow contrast. High-resolution images of the lung parenchyma and mediastinum should be obtained, as well as contrast-enhanced images of the abdomen and CNS, for detection and differentiation of parenchymatous lesions. Naturally this is just a representative example of a general oncological WB-MRI concept; the WB imaging protocol must always be adjusted according to the clinical problem and the specific tumor entity concerned. Challenges are also presented by integration of the sometimes complex protocols for specific MRI examinations of frequent tumors, such as cancers of the prostate, colon, and breast, into a clinically practicable WB protocol. An important role may be played by adaptation of WB protocols to specific tumor types or risk profiles, permitting further refinement and clinical implementation of WB-MRI concepts.
WB-MRI in tumor screening
In view of the absence of ionizing radiation, WB-MRI may have potential for the screening of asymptomatic populations, particularly compared with modalities such as CT that feature ionizing radiation. Early studies using combined cardiovascular and oncological examination protocols in asymptomatic individuals found not only numerous cases of cardiovascular disease but also severe tumors (3, 4). Kramer et al. investigated 200 asymptomatic patients by means of a protocol that comprised WB-MRI angiography, functional cardiac imaging, and morphological imaging of the thorax and abdomen. As well as varying manifestations of atherosclerosis in 6% to 14% of cases, two of those examined were found to have cancer—one bronchial carcinoma and one renal cell carcinoma (4). In a similarly conceived study of 855 patients that included MRI coloscopy in the protocol, Baumgart et al. demonstrated benign polyps exceeding 10 mm in size in 8.4% of patients. In the same study neoplasms were detected in a number of persons, including five early-stage renal cell carcinomas and two bronchial carcinomas (5). Despite these early findings of serious conditions with therapeutic consequences, it must be pointed out that these oncological diseases were found by complete coincidence. Goehde et al. (2) stated there was only one false-positive finding, namely a bone lesion classified as a possible tumor. According to these authors, all findings classified as definitely malignant were subsequently confirmed to be malignant. Overall, however, the non-specific use of this new method has to be viewed very critically, among other reasons because of the low expected prevalence of <2% and the absence, to date, of proven cost-effectiveness, as potentially false-positive or unclear findings need to be clarified involving additional, perhaps even invasive, procedures.
WB-MRI for tumor staging and detection of recurrence
Precise, efficient oncological staging and tumor monitoring have a decisive influence on the prognosis and appropriate-to-stage treatment of patients with malignant tumors (6). Multimodal diagnostic approaches (MRI, CT, ultrasound, nuclear medicine) are often selected to this end. However, this can be more time-consuming, costly, and stressful for the patient (7). Whole-body diagnostic procedures are therefore becoming increasingly routine in clinical practice in order to map a tumor, with its potential pathways of metastasis, as a systemic disease (figure 1) (8). Our own investigation of 41 patients with tumors of the gastrointestinal tract, breast cancer, or malignant melanoma showed high diagnostic accuracy of 91% for TNM staging by WB-MRI, comparable with competing procedures such as combined positron emission tomography and CT (PET-CT) (9). However, MRI’s susceptibility to artifacts of motion and organ pulsation means that it has certain limitations for the detection of lymph node (LN) metastases, particularly in the thorax and diaphragm region, leading to reduced diagnostic accuracy (79% to 82%) in N-staging (6, 11). Moreover, the lack of metabolic information in borderline large lesions ≤ 1 cm in diameter constitutes a disadvantage versus PET-CT in dignity assessment. The so-called diffusion-weighted WB-MRI procedures promise to facilitate the detection of LN metastases (10). The published studies on diffusion-weighted WB-MRI indicate that this method can distinctly improve the sensitivity for LN metastases. With the exception of recent findings regarding the locoregional LN metastasis of rectal carcinoma, no systematic studies on improved specificity are yet available (11).
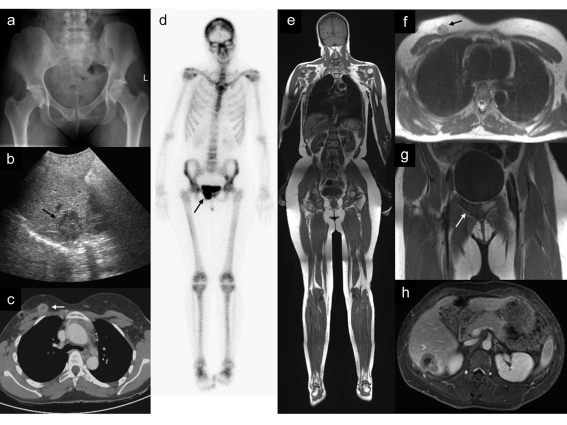
Figure 1.
From multimodal diagnosis to whole-body examination: repeat staging in a 29-year-old female patient after treatment for breast cancer and an increase in levels of tumor markers during follow-up
a+b) Pelvic radiography shows a suspicious irregularity of the cortical bone in the anterior right os pubis. Ultrasound shows a suspected metastasis in the liver.
c) Subsequent staging CT demonstrates a suspected focal recurrence in the right breast.
d) Pathological tracer accumulation on skeletal scintigraphy reinforces the suspicion of a bony metastasis in the right os pubis.
e) High-resolution WB-MRI with T1 contrast
f+g) The tumor recurrence in the breast and the bony metastasis are demonstrated in one single examination.
h) Dynamic contrast-enhanced abdominal imaging clearly depicts the liver metastasis with central necrosis.
Owing to its higher intrinsic soft-tissue contrast, MRI has distinct advantages for the detection of distant metastases, especially in the skeleton, the brain, soft tissues, and the liver (12, 13). The diagnostic accuracy of M-staging with WB-MRI is 93% to 97% (6, 14). WB-MRI would therefore be particularly suitable for tumors that frequently metastasize to these organs, e.g., breast cancer, colorectal carcinoma, or malignant melanoma (15). The results in such cases are comparable with those of PET-CT in tumors with good storage of (18)F-fluorodeoxyglucose. In the detection of lung metastases or the staging of pulmonary tumors, however, WB-MRI has limitations, in terms of diagnostic sensitivity, compared to conventional procedures such as CT or PET-CT owing to organ motion artifacts and the lower lung parenchyma contrast (13, 14).
A recently published study presented WB-MRI as a method for detecting recurrence of primarily curatively treated mammary carcinoma (16). Thirty-three patients with clinical suspicion of tumor recurrence, e.g., displaying clinical symptoms or elevated tumor markers, were investigated by WB-MRI using 1.5-T and 3-T scanners. Tumor recurrence was found in 61% of this high-risk population, particularly LN and organ metastases; the recurrences were validated in diagnostic follow-up investigations at a 6-month interval. WB-MRI showed high diagnostic accuracy (91%) for the demonstration or exclusion of tumor recurrence, with sensitivity of 93% and specificity of 86%. In one patient, however, there was a false-positive finding of local recurrence. It should be borne in mind that WB-MRI is currently generally performed with the patient in supine position without breast compression and therefore cannot replace dedicated breast MRI in respect of spatial resolution and soft-tissue depiction.
Finally, WB-MRI can also demonstrate numerous metastases beyond the range of a standard staging protocol (CT of the neck, thorax, and abdomen), e.g., brain metastases and bone metastases in the peripheral skeleton (6). In another study, the discovery of such metastases in 10% of the patients among other things prompted a revision of the treatment strategy (17). It must be pointed out, however, that neither comprehensive investigations of large numbers of patients nor valid cost–effect studies have yet been carried out.
WB-MRI for staging of hematological diseases
Because of its good bone-marrow contrast, WB-MRI has been described as a promising method for investigation of malignant diseases of the bone marrow with potential systemic manifestations, e.g., multiple myeloma (19). The detection rate of MRI or WB-MRI is superior to that of the conventional radiographic diagnosis, particularly with regard to diffuse forms of infiltration, which often escape detection by radiography or even multislice CT (MS-CT) (18, 19).
In a recently published study 41 patients with plasma cell neoplasms were examined by WB-MRI and MS-CT (19). WB-MRI showed a significantly higher detection rate than MS-CT. In 11 patients MS-CT underestimated the disease stage relative to WB-MRI. In particular, WB-MRI reliably detected early stages of disease with less extensive osteolyses and a diffuse pattern of infiltration. Diffuse bone-marrow infiltration or small foci are particularly at risk of being falsely classified as benign osteoporosis on MS-CT (figure 2) (20). Baur et al. showed that integration of the MRI findings into the Durie and Salmon staging system (PLUS classification) allows more precise staging of patients with multiple myeloma. Thereby MRI significantly influenced the prognosis and the choice of treatment in this disease (21). In a recently published study by Dinter et al., 19 of 60 patients were assigned to a higher stage in the PLUS classification by virtue of the WB-MRI findings. In 10 of these 19 patients (53%) the WB-MRI diagnosis was decisive for the choice of treatment, the most important factors being the extent of tumor infiltration, the demonstration or exclusion of extramedullary tumor extension, and fracture risk (22).
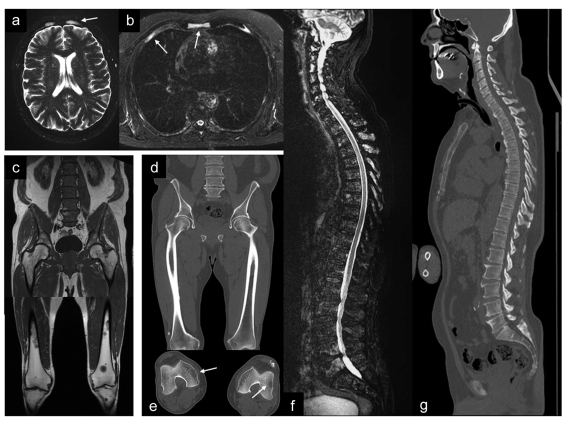
Figure 2.
A 65-year-old patient with multiple myeloma
a+b) WB-MRI demonstrates multifocal osteolyses in the cranial vault, sternum, and ribs.
c) Moreover, diffuse infiltration of the lumbar spine and pelvis is shown by the homogeneous signal decrease in bone marrow. Further osteolyses are seen in the lower extremities.
d+e) MS-CT demonstrates only the large osteolyses in the extremities.
f+g) Diffuse spinal involvement on MRI (Figure 2 f) and MS-CT (Figure 2 g). MRI demonstrates disseminated spinal involvement, particularly in the superior segment. MS-CT is not able to visualize these changes; there is merely a discrete decrease in density that could be interpreted as a sign of osteoporosis.
Uses of WB-MRI in benign systemic diseases
Rheumatic diseases and diabetes mellitus
MRI yields particularly useful information in the early stages of rheumatic joint diseases. Even pre-erosive changes such as synovitis, bone marrow edema, and osteitis can be demonstrated. Furthermore, MRI is able to detect signs of tendinitis or ligamentous pathology. Since rheumatoid arthritis may affect the whole body—small joints in the extremities as well as the large joints of the axial skeleton—WB-MRI could potentially be used specifically to visualize early manifestations of this disease. Weckbach et al. described WB-MRI in the evaluation of psoriatic arthritis, with a total examination time of no more than 60 min. Image quality was described as excellent in 22 of 25 patients. Moreover, significantly more regions with synovialitides and enthesitides were discovered by WB-MRI than by clinical examination (Weckbach et al.: Comprehensive diabetes imaging with whole body MRI at 1.5 and 3T in patients with longstanding diabetes. 2006; ISMRM Book of Abstracts: 389).
WB-MRI protocols adapted for the examination of patients with longstanding diabetes mellitus have recently been discussed. These comprise imaging of the CNS, MRI angiography of the cerebral arteries, whole-body angiography, dynamic imaging of cardiac function and myocardial vitality, and high-resolution plain and contrast-enhanced imaging of the feet. Early experience showed higher rates of vascular pathology in 45 asymptomatic patients with longstanding type 1 or type 2 diabetes than in an asymptomatic normal group without diabetes (n = 200), e.g., stenoses of the carotids (54% vs. 6%) or peripheral vessels (51% vs. 14%). Furthermore, the incidence of silent myocardial infarction was 18% in the diabetes group compared with 1% in the control group. In 9 patients the WB-MRI findings indicated immediate therapeutic intervention. WB-MRI seems suitable for early diagnosis of secondary complications and for potentially more effective treatment planning in patients with diabetes mellitus, who have a high prevalence of cardiovascular diseases (23).
Systemic imaging of benign tumors
Patients with multiple cartilaginous exostoses are at considerable risk of malignant transformation to chondrosarcoma. Moreover, a high proportion of the patients are young, so repeated radiographic examinations are problematic. WB-MRI is a good alternative, particularly because the osteochondromas may occur in many different locations and it must be determined whether there is a tendency towards malignant transformation, recognizable by a thickening of the layer of cartilage covering the osteochondromas.
Early experience of WB-MRI has also been reported for Langerhans cell histiocytosis, chronic recurring multifocal osteomyelitis (CRMO), Paget’s disease, and skeletal developmental disorders such as osteochondrodysplasia and polyostotic fibrous dysplasia; however, the reports concerned are all case studies or observations of small groups of patients.
Conclusion
Whole-body MRI achieves comprehensive imaging from head to toe in one single examination. Therefore, in common with PET-CT, WB-MRI seems in principal well suited to take the place of the current, often time-consuming multimodal diagnosis of diseases with systemic or multilocular manifestations. Recent technical advances enable the WB-MRI examination to be completed in a time tolerable to the patients—from 45 to 60 min, depending on the protocol. No compromises with regard to image quality versus dedicated MRI sequences are involved. Despite these encouraging findings, non-specific screening without adequate indication, though sometimes offered, can by no means be justified because of the low anticipated prevalence of disease (<2%) and the lack of proof of cost-effectiveness to date.
In contrast, the use of WB-MRI appears promising in high-risk populations such as patients with diabetes mellitus, rheumatic diseases, or primary benign bone tumors with potential for malignant transformation.
Several studies have shown that WB-MRI is capable of high accuracy both in the staging of various tumor entities and in demonstrating or excluding recurrence. Especially metastases in the liver, the skeleton, and the CNS are demonstrated with greater accuracy than can be achieved with other imaging procedures; for this reason, WB-MRI is likely to prove particularly valuable in diagnosing breast cancer and colorectal carcinoma.
Because the bone marrow is imaged directly by MRI and often displays diffuse or multilocular involvement in multiple myeloma, WB-MRI is particularly sensitive to this disease; its findings are important for the prognosis and play a substantial role in therapeutic decision making. MRI has therefore been incorporated into the staging system for multiple myeloma.
Key Messages.
Whole-body magnetic resonance imaging (WB-MRI) is increasingly being adopted into clinical routine as an alternative to incremental, multimodal diagnostic approaches, particularly for comprehensive evaluation of malignant diseases.
Recent technical advances permit WB-MRI to be carried out in less than 1 h, improving patient tolerance. Image quality matches that attained with conventional MRI examination.
Studies have shown that WB-MRI is capable of high accuracy both in the staging of various tumor entities and in excluding recurrence. Especially distant metastases in liver, skeleton, and CNS are demonstrated more accurately than with other imaging procedures.
Because of its good medullary contrast WB-MRI represents a particularly sensitive method for staging malignant diseases of the bone marrow, e.g., multiple myeloma.
Non-specific application of this new method for the screening of asymptomatic populations should be viewed critically because of the low expected prevalence and the absence, to date, of proven cost-effectiveness.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Dr. Schmidt and PD Dr. Dinter declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors. Prof. Reiser and Prof. Schoenberg declare scientific cooperation with Siemens Health Care.
References
- 1.Schmidt GP, Wintersperger B, Graser A, Baur-Melnyk A, Reiser MF, Schoenberg SO. High-resolution whole-body magnetic resonance imaging applications at 1.5 and 3 Tesla: a comparative study. Invest Radiol. 2007:449–459. doi: 10.1097/01.rli.0000262089.55618.18. [DOI] [PubMed] [Google Scholar]
- 2.Kruger DG, Riederer SJ, Grimm RC, Rossman PJ. Continuously moving table data acquisition method for long FOV contrast-enhanced MRA and whole-body MRI. Magn Reson Med. 2002;47:224–231. doi: 10.1002/mrm.10061. [DOI] [PubMed] [Google Scholar]
- 3.Goehde SC, Hunold P, Vogt FM, et al. Full-body cardiovascular and tumor MRI for early detection of disease: feasibility and initial experience in 298 subjects. AJR. 2005;184:598–611. doi: 10.2214/ajr.184.2.01840598. [DOI] [PubMed] [Google Scholar]
- 4.Kramer H, Michaely K, Nikolaou K, Reiser MF, Schoenberg SO. State of the art cardiovascular imaging with parallel imaging techniques on a whole body MR scanner: experience in more than 200 individuals. Eur Radiol. 2006;16(S) [Google Scholar]
- 5.Baumgart D, Egelhof T. Präventives Ganzkörperscreening unter Einbeziehung moderner Bildgebung mit Hilfe der Magnetresonanztomographie. Herz. 2007;32:387–394. doi: 10.1007/s00059-007-3020-1. [DOI] [PubMed] [Google Scholar]
- 6.American Joint Committee on Cancer. AJCC Cancer Staging Manual. (6th edition) New York: Springer; 2002. [Google Scholar]
- 7.Plathow C, Walz M, Lichy MP, et al. Kostenüberlegungen zur Ganzkörper-MRT und PET-CT im Rahmen des onkologischen Stagings Radiologe. 2008;48:384–396. doi: 10.1007/s00117-007-1547-z. [DOI] [PubMed] [Google Scholar]
- 8.Goyen M, Schlemmer HP. Ganzkörper-MRT - diagnostische Strategie der Zukunft? Radiologe. 2004;47:904–914. doi: 10.1007/s00117-006-1411-6. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt GP, Baur-Melnyk A, Herzog P, et al. High-resolution whole-body MRI tumor staging with the use of parallel imaging versus dual modality PET-CT: experience on a 32-channel system. Invest Radiol. 2005;40:743–753. doi: 10.1097/01.rli.0000185878.61270.b0. [DOI] [PubMed] [Google Scholar]
- 10.Takahara T, Imay Y, Yamashita T, Yasuda S, Nasu S, Van Cauteren M. Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med. 2004;22:275–282. [PubMed] [Google Scholar]
- 11.Rao SX, Zeng MS, Chen CZ, et al. The value of diffusion-weighted imaging in combination with T2-weighted imaging for rectal cancer detection. Eur J Radiol. 2008;65:299–303. doi: 10.1016/j.ejrad.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Steinborn M, Tiling R, Heuck A, Brügel M, Stäbler A, Reiser M. Diagnostik der Metastasierung im Knochenmark mittels MRT. Der Radiologe. 2000;40:826–834. doi: 10.1007/s001170050830. [DOI] [PubMed] [Google Scholar]
- 13.Semelka RC, Worawattanakul S, Kelekis NL, et al. Liver lesion detection, characterization, and effect on patient managment: comparison of single-phase spiral CT and current MR techniques. J Magn Reson Imaging. 1997;7:1040–1047. doi: 10.1002/jmri.1880070616. [DOI] [PubMed] [Google Scholar]
- 14.Antoch G, Vogt FM, Freudenberg LS, et al. Whole-body dual-modality PET/CT and whole-body MRI for tumor staging in oncology. JAMA. 2003;290:3199–3206. doi: 10.1001/jama.290.24.3199. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt GP, Baur-Melnyk A, Haug A, et al. Whole-body MRI at 1.5 T and 3 T compared with FDG-PET-CT for the detection of tumour recurrence in patients with colorectal cancer. Eur Radiol. 2009;19:1366–1378. doi: 10.1007/s00330-008-1289-y. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt GP, Baur-Melnyk A, Haug A, et al. Comprehensive imaging of tumor recurrence in breast cancer patients using whole-body MRI at 1.5 and 3 T compared to FDG-PET-CT. Eur J Radiol. 2008;65:47–58. doi: 10.1016/j.ejrad.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Schlemmer HP, Schäfer J, Pfannenberg C, Radny P, Korchidi S, Müller-Horvat C. Fast whole-body assessment of metastatic disease using a novel magnetic resonance imaging system: initial experiences. Invest Radiol. 2005;40:64–71. doi: 10.1097/01.rli.0000149250.37033.7c. [DOI] [PubMed] [Google Scholar]
- 18.Ghanem N, Lohrmann C, Engelhardt M, et al. Whole-body MRI in the detection of bone marrow infiltration in patients with plasma cell neoplasms in comparison to the radiological skeletal survey. Eur Radiol. 2006;16:1005–1014. doi: 10.1007/s00330-005-0055-7. [DOI] [PubMed] [Google Scholar]
- 19.Baur-Melnyk A, Buhmann S, Becker C, et al. Whole-body MRI versus whole-body MDCT for staging of multiple myeloma. Am J Roentgenol. 2008;190:1097–1104. doi: 10.2214/AJR.07.2635. [DOI] [PubMed] [Google Scholar]
- 20.Baur A, Stäbler A, Nagel D, et al. Magnetic resonance imaging as a supplement for the clinical staging system of Durie and Salmon? Cancer. 2002;95:1334–1345. doi: 10.1002/cncr.10818. [DOI] [PubMed] [Google Scholar]
- 21.Dinter DJ, Neff WK, Klaus J. Comparison of whole-body MR imaging and conventional X-ray examination in patients with multiple myeloma and implications for therapy. Ann Hematol. 2009;88:457–464. doi: 10.1007/s00277-008-0621-6. [DOI] [PubMed] [Google Scholar]
- 22.Weckbach S, Michaely HJ, Friedrich D, Schewe S, Reiser MF, Glaser C. Whole body MR Imaging in psoriatic arthritis: development of an imaging protocol and evaluation in 25 patients. Eur Radiol. 2007;17(Suppl.1) [Google Scholar]
- 23.Weckbach S, Findeisen HM, Schoenberg SO, et al. Systemic cardiovascular complications in patients with long-standing diabetes mellitus: comprehensive assessment with whole-body magnetic resonance imaging/magnetic resonance angiography. Invest Radiol. 2009;44:242–250. doi: 10.1097/RLI.0b013e31819a60d3. [DOI] [PubMed] [Google Scholar]