Abstract
Purpose: In patients with major burn injuries mechanical ventilation is often required for longer periods. Tracheostomy (TS) plays an integral role in airway management. We investigated the effect of TS on ventilation parameters within 8 hours after TS.
Materials: A retrospective analysis of severely burned patients admitted to the burn unit of a German University Hospital was performed. Ventilation parameters 8 hours before and after TS were registered.
Results: A retrospective analysis of 20 patients which received surgical TS was performed. Mean age was 52±19 years. Mean abbreviated burned severity index (ABSI) was 8.3±2.2. A mechanical ventilation was required for 14.3±4.8 days. TS was performed on day 7±4. Inspiratory oxygen concentration (FiO2) (p<0.001), peak inspiratory pressure (p<0.001), positive end-expiratory pressure (p=0.003) and pulmonary resistance (p<0.001) were reduced significantly after TS. The arterial partial pressure of oxygen/FiO2-ratio increased significantly after TS (p<0.001).
Conclusions: We demonstrate that TS reduces invasiveness of ventilation in severely burned patients and by this can optimize lung protective ventilation strategy.
Keywords: pulmonary ventilation, pulmonary gas exchange, tracheostomy, critical care, intensive care
Abstract
Einleitung: Schwerbrandverletzte müssen häufig langfristig maschinell beatmet werden. Die Tracheostomie (TS) hat einen hohen Stellenwert in der Langzeitbeatmung. Wir untersuchen, ob eine Veränderung der Beatmungsparameter innerhalb von 8 Stunden nach TS festzustellen ist.
Material und Methoden: Retrospektive Analyse an schwerbrandverletzten Patienten einer deutschen Intensiveinheit für Schwerbrandverletzte. Die Beatmungsparameter wurden 8 Stunden vor und 8 Stunden nach der TS ausgewertet.
Ergebnisse: 20 Patienten mit einem mittleren Alter von 52±19 Jahren wurden eingeschlossen. Der mittlere ABSI-Wert betrug 8,3±2,2. Die mittlere Beatmungsdauer betrug 14,3±4,8 Tage. Die TS wurde im Mittel am 7. (±4) posttraumatischen Tag durchgeführt. Die inspiratorische Sauerstoffkonzentration (FiO2) (p<0,001), der inspiratorische Spitzendruck (p<0,001), der positive end-exspiratorische Druck (p=0,003) und der pulmonale Widerstand (p<0,001) waren innerhalb von 8 Stunden nach TS signifikant reduziert. Das Verhältnis von arteriellem Sauerstoffpartialdruck und FiO2 stieg innerhalb von 8 Stunden postoperativ signifikant an (p<0,001).
Schlussfolgerung: Wir konnten zeigen, dass frühzeitig nach einer TS eine reduzierte Invasivität der maschinellen Beatmung erreicht wird und somit die lungenprotektive Beatmungsstrategie optimiert werden kann.
Introduction
Patients following major burn injury often require artificial airway management and mechanical ventilation for prolonged periods due to inability of self-contained airway protection, persistence of excessive secretions, and insufficient spontaneous ventilation [1]. Therefore a deep continuous analgesia is required. In patients with extensive cutaneous burns capillary leak occurs not only at the injured site, but also in regions distant from the injury [2], [3]. Vascular hyperpermeability leads to lung edema formation due to an increased transpulmonary fluid flux (lung lymph flow) and lung water content [4], [5]. These abnormalities are associated with a subsequent increase in ventilatory pressures and a fall in arterial partial pressure of oxygen (paO2)/inspiratory oxygen concentration (FiO2)-ratio (PFR) [5].
Tracheostomy (TS) is frequently performed in critically ill and burned patients and plays an integral role in airway management [6]. In 1989, the American College of Chest Physicians Consensus Statement on Artificial Airways in Patients Receiving Mechanical Ventilation stated that translaryngeal intubation (TLI) is preferred for patients requiring up to 10 days of mechanical ventilation. In patients with an anticipated need for artificial airway ventilation for longer than 21 days, tracheostomy is recommended [7]. In all other patients, timing of TS is left to daily assessment and physician's preference. In 1994, the American-European Consensus Conference (AECC) introduced PFR to separate the adult respiratory distress syndrome (ARDS) patients into two stages [2]. Situations with PFR <300 are classified as acute lung injury (ALI) and patients with PFR <200 as ARDS. Neither positive end-expiratory pressure (PEEP) nor FiO2 settings were recommended. It has been demonstrated that PEEP levels merely influence PFR [8]. Elevation of FiO2 has shown to increase PFR [9].
We investigated the early postoperative effects of surgical tracheostomy on ventilation parameters.
Materials and methods
We performed a retrospective analysis of 20 patients which received open surgical TS after burn injury during the last 2 years. In all patients a I° to II° inhalation injury was diagnosed by bronchoscopy on admission. All patients were mechanically ventilated by an EVITA® XL (Fa. DraegerTM, Lübeck, Germany) in BIPAP-mode. Male patients were ventilated by standard with a 8.5 mm (internal diameter) endotracheal tube or after TS with a 9 mm (internal diameter) tracheostomy tube. Female patients were ventilated by standard with a 7.5 mm (internal diameter) endotracheal tube or after TS with an 8 mm (internal diameter) tracheostomy tube. Patients were ventilated with a tidal volume of 5 to 7 ml/kg bodyweight. We analyzed patients characteristics (age, sex, totally burned surface area (TBSA), abbreviated burned severity index (ABSI)) and mean ventilation parameters (FiO2, peak inspiratory pressure (PIP), PFR, pulmonary resistance, PEEP) 8 hours before and after TS. Ventilation parameters were registered every hour during the analyzed period. No muscle relaxant was applied. No changes of sedation were performed during observation period. All patients were in a supine position during the analyzed period and were transferred in to a 60°-lateral position every 60–120 minutes.
All surgical tracheostomies were performed by experienced plastic surgeons. After dermal incision (2–3 cm cranial to the Jugulum) the thyroidal isthmus was identified and separated from the surrounding tissue. In the next step the trachea was exposed and a tracheal incision was performed. After careful removal of the endotracheal tube the tracheal tube was placed under visual control. No complications occurred after open surgical TS in this study group.
Patients with a known pulmonary disease or an inhalation injury III° were excluded from this study. Prone position was an exclusion criterion.
Statistical analysis was performed using Wilcoxon-Singed-Ranks-Test (SPSS® 15.0, SPSS Inc., Chicago, USA). Level of significance was determined at p<0.05. Results are written in mean ± standard deviation.
Results
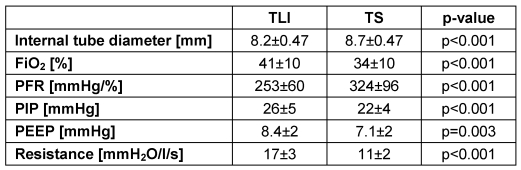
Mean age of the 6 women and 14 men was 52±19 years (minimum: 21 years; maximum: 83 years). Mean total burned surface area (TBSA) was 36±19% (minimum: 12%; maximum: 75%). Mean abbreviated burned severity index (ABSI) was 8.3±2.2 with a range from 4 to 12 (Table 1 (Tab. 1)). Mechanical ventilation was required in a mean of 14.3±4.8 days (minimum: 5 days; maximum: 24 days). Surgical TS was performed on day 7±4 with a range of day 2 to day 20. Mean endotracheal tube size was 8.2±0.47 mm and mean tracheal tube size was 8.7±0.47 mm (p<0.001).
Table 1. Patients characteristics (sex [count], age [years], totally burned surface [%] and ABSI-Score).
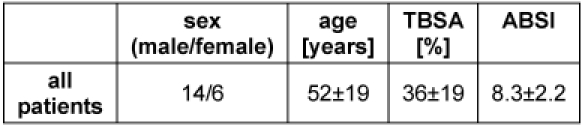
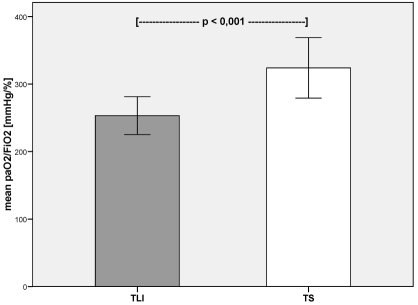
FiO2 was reduced after TS (TLI vs. TS: 41±10% vs. 34±10%; p<0.001). PFR increased significantly after TS (TLI vs. TS: 253±60 mmHg/% vs. 324±96 mmHg/%; p<0.001 (Figure 1 (Fig. 1))). PIP was significantly reduced after TS (TLI vs. TS: 26±5 mmHg vs. 22±4 mmHg; p<0.001 (Figure 2 (Fig. 2))). PEEP was also reduced significantly after TS (TLI vs. TS: 8.4±2 mmHg vs. 7.1±2 mmHg; p=0.003 (Figure 3 (Fig. 3)). After TS a significant reduction of pulmonary resistance was observed (TLI vs. TS: 17±3 mmH2O/l/s vs. 11±2 mmH2O/l/s; p<0.001 (Figure 4 (Fig. 4), Table 2 (Tab. 2))).
Figure 1. Mean arterial oxygen pressure (paO2)/inspiratory oxygen concentration (FiO2) – ratio [mmHg/%] before and after surgical tracheostomy (TLI – translaryngeal intubation; TS – tracheostomy).
Figure 2. Mean peak inspiratory pressure (PIP [mmHg]) before and after surgical tracheostomy (TLI – translaryngeal intubation; TS – tracheostomy).
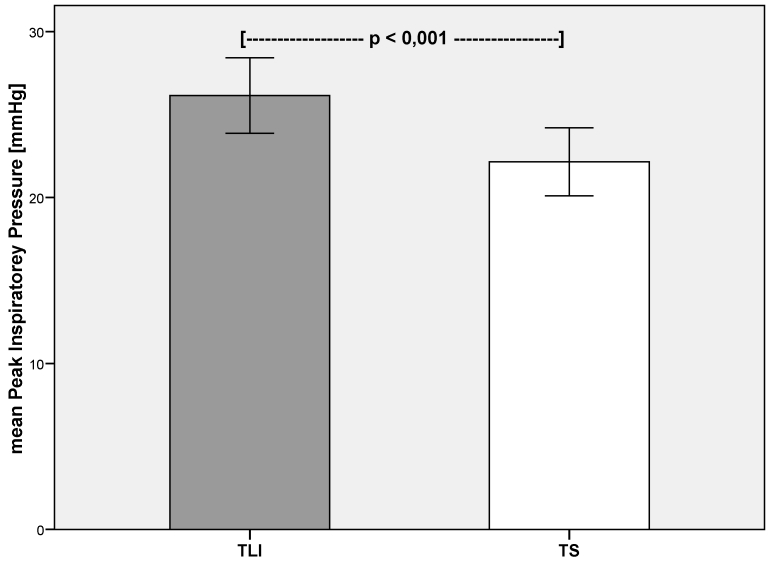
Figure 3. Mean positive end-expiratory pressure (PEEP [mmHg]) before and after surgical tracheostomy (TLI – translaryngeal intubation; TS – tracheostomy).
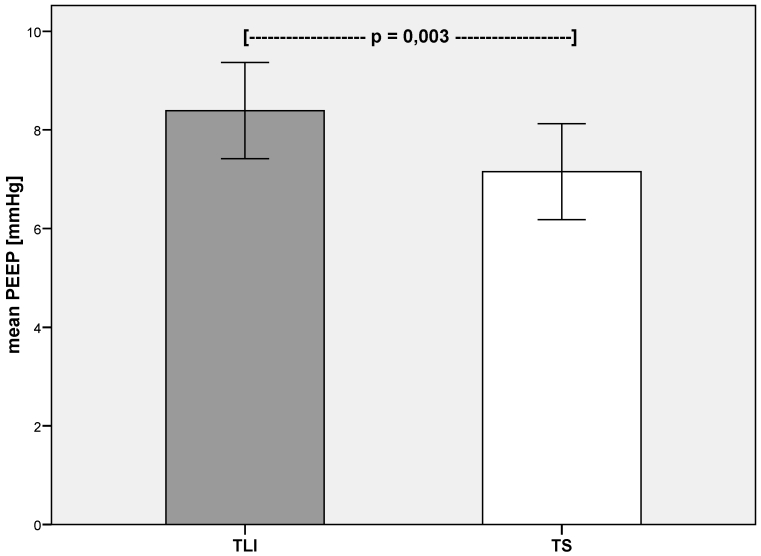
Figure 4. Mean pulmonary resistance (Resistance [mmH2O/l/sec]) before and after surgical tracheostomy (TLI – translaryngeal intubation; TS – tracheostomy).
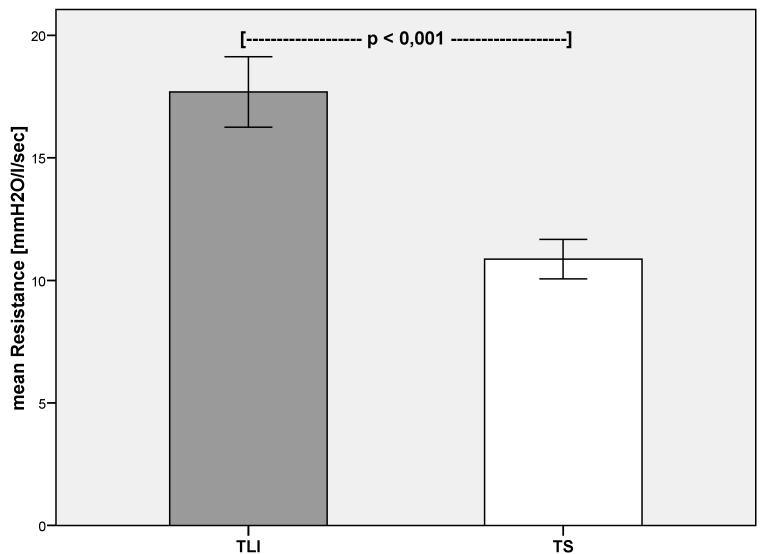
Table 2. Internal tube diameter [mm], inspiratory oxygen concentration (FiO2) [%], partial arterial oxygen pressure/FiO2 [mmHg/%], peak inspiratory pressure (PIP) [mmHg], positive end-expiratory pressure (PEEP) [mmHg] and pulmonary resistance [mmH2O/l/s]) given as mean ± standard deviation.
Discussion
Mechanical ventilation – even if sometimes life-saving – has its negative side effects. Marini et al. described in a review the potential diffuse lung injury due to mechanical ventilation. They also postulated a mechanism that could potentially extend primary focal lung injury by airway propagation [10].
There is a debate about lung protective ventilation strategies. The ventilation strategy described by Amato et al. intends to minimize shear stress in the lung tissue during inspiration [11]. Hereby pulmonary tissue barotrauma and mortality are reduced because of lower tidal volume (<6ml/kg) and driving pressures, permissive hypercapnia, and preferential use of pressure-limited ventilatory modes [11]. TS (surgical or dilatative) is described to have its benefit in case of suspected prolonged ventilation [7].
TS has its advantages compared with TLI, including reduced laryngeal alteration, reduced inspiratory load, better patient tolerance, and ease of nursing. Timing of tracheostomy is still debated upon. Therefore recommendations are given by the American College of Chest Physicians Consensus Statement [7] and the American-European Consensus Conference [2]. The prone position is not systematically used in hypoxemic patients. Patients that can benefit from prone position sessions are those with the most severe ARDS and those with dorsal lung infiltrates [12], [13].
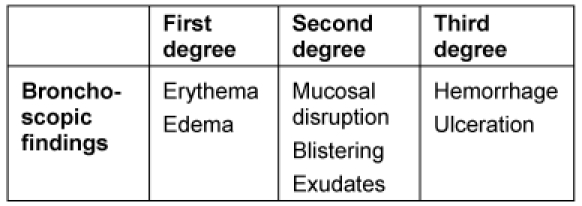
Pulmonary lesions are common in burn victims [14], [15], [16]. Inhalation injury can be caused by heat exposure and/or toxic agents. Highly volatile gases, smoke, or both are corrosive to the respiratory mucosa. Inhalation injury can affect the whole respiratory tree. Its severity depends on the nature of inhaled fumes and the length of exposure. Inhalation of hot air (over 500°C) or steam can also induce pulmonary burns [14]. Bronchoscopy is routinely used to determine inhalation injury [17], [18]. The severity of inhalation injury can be classified in three categories (Table 3 (Tab. 3)).
Table 3. Bronchoscopic findings and inhalation injury categories after inhalation injury.
In this study, TS was realized according to the American College of Chest Physicians Consensus Statement on Artificial Airways in Patients Receiving Mechanical Ventilation [7]. We demonstrate the early beneficial post-TS effects on mechanical ventilation parameters in severely burned patients. We found a significant PFR-elevation within 8 hours after TS although FiO2 was reduced. Furthermore significant decreases in PIP, PEEP and pulmonary resistance were measured after TS. Despite post-TS reduction of ventilation invasiveness (i. e. PIP, FiO2 and PEEP) better oxygen delivery was achieved (PFR elevation).
The increased internal diameter of the tracheal tube after TS may have contributed to the early postoperative benefits on mechanical ventilation. Especially PIP, PEEP and pulmonary resistance can be influenced by a larger tube diameter. But increased oxygen delivery after TS cannot be explained by the larger internal tube diameter.
Mechanical ventilation is supposed to exacerbate lung injury (VILI) [19]. Several strategies have been developed to combat VILI. Efforts to decrease alveolar over-distension have emphasized the global reduction of inspiratory pressures and their resultant ventilating volumes [20]. It has been reported, that even short periods of high-pressure mechanical ventilation can be harmful to injured as well as healthy lungs [21]. High PIP can lead to progressive impairment in pulmonary mechanics, lung function, acute respiratory failure, and alveolar cellular dysfunction. Several studies demonstrated the impact of PIP and FiO2-elevation to PFR, which is used as parameter for oxygen delivery in critically ill patients [8], [9], [11], [22], [23].
Bolivar et al. showed a reduced carinal PIP in an experimental study after tracheostomy [23]. The present study supports the experimental findings of Bolivar et al. [23]. We registered a significant PIP-decrease within 8 hours after TS. On the other hand high PEEP is tolerated to achieve nearly maximal alveolar recruitment and ventilation [22]. Specific PEEP and PIP recommendations cannot be given [7]. We measured a significant PEEP-reduction after TS in severely burned patients.
We postulate that due to TS, VILI can be reduced or even be avoided. This safe surgical procedure reduces distal-to-proximal airway propagation of initially focal injured/infected pulmonary areas [10]. The ideal ventilation strategy, type of artificial airway (translaryngeal intubation vs. tracheostomy) and timing of TS should be decided on individually and carefully. Griffiths et al. showed that early tracheostomy in critically ill patients could shorten the duration of mechanical ventilation and the length of stay in intensive care in a meta-analysis in 2005 [24]. Therefore, it should be investigated in the future whether an initially performed TS at admission to a burn unit has a beneficial effect on the pulmonary compromised severely burned patient.
Limitations
The interpretation of the results of the present study is limited due to retrospective study design, small number of patients, the short time period measured and the lack of a control comparison group without TS.
Conclusions
After TS, lung protective ventilation strategies can be optimized in severely burned patients. Hereby the invasiveness of ventilation can be reduced. Furthermore distal-to-proximal airway propagation can be diminished.
Notes
Conflicts of interest
None declared.
References
- 1.Ross BJ, Barker DE, Russell WL, Burns RP. Prediction of long-term ventilatory support in trauma patients. Am Surg. 1996;62(1):19–25. [PubMed] [Google Scholar]
- 2.Bert JL, Bowen BD, Reed RK, Onarheim H. Microvascular exchange during burn injury: IV; Fluid resuscitation model. Circ Shock. 1991;34(3):285–297. [PubMed] [Google Scholar]
- 3.Lund T, Bert JL, Onarheim H, Bowen BD, Reed RK. Microvascular exchange during burn injury; I: A review. Circ Shock. 1989;28(3):179–197. [PubMed] [Google Scholar]
- 4.Soejima K, Schmalstieg FC, Sakurai H, Traber LD, Traber DL. Pathophysiological analysis of combined burn and smoke inhalation injuries in sheep. Am J Physiol Lung Cell Mol Physiol. 2001;280(6):L1233–L1241. doi: 10.1152/ajplung.2001.280.6.L1233. [DOI] [PubMed] [Google Scholar]
- 5.Enkhbaatar P, Traber DL. Pathophysiology of acute lung injury in combined burn and smoke inhalation injury. Clin Sci (Lond) 2004;107(2):137–143. doi: 10.1042/CS20040135. Available from: http://dx.doi.org/10.1042/CS20040135. [DOI] [PubMed] [Google Scholar]
- 6.Arabi Y, Haddad S, Shirawi N, Al Shimemeri A. Early tracheostomy in intensive care trauma patients improves resource utilization: a cohort study and literature review. Crit Care. 2004;8(5):R347–R352. doi: 10.1186/cc2924. Available from: http://dx.doi.org/10.1186/cc2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plummer AL, Gracey DR. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest. 1989;96(1):178–180. doi: 10.1378/chest.96.1.178. Available from: http://dx.doi.org/10.1378/chest.96.1.178. [DOI] [PubMed] [Google Scholar]
- 8.Estenssoro E, Dubin A, Laffaire E, Canales HS, Sáenz G, Moseinco M, Bachetti P. Impact of positive end-expiratory pressure on the definition of acute respiratory distress syndrome. Intensive Care Med. 2003;29(11):1936–1942. doi: 10.1007/s00134-003-1943-4. Available from: http://dx.doi.org/10.1007/s00134-003-1943-4. [DOI] [PubMed] [Google Scholar]
- 9.Allardet-Servent J, Forel JM, Roch A, Guervilly C, Chiche L, Castanier M, Embriaco N, Gainnier M, Papazian L. FIO2 and acute respiratory distress syndrome definition during lung protective ventilation. Crit Care Med. 2009;37(1):202–7, e4. doi: 10.1097/CCM.0b013e31819261db. Available from: http://dx.doi.org/10.1097/CCM.0b013e31819261db. [DOI] [PubMed] [Google Scholar]
- 10.Marini JJ, Gattinoni L. Propagation prevention: a complementary mechanism for "lung protective" ventilation in acute respiratory distress syndrome. Crit Care Med. 2008;36(12):3252–3258. doi: 10.1097/CCM.0b013e31818f0e68. Available from: http://dx.doi.org/10.1097/CCM.0b013e31818f0e68. [DOI] [PubMed] [Google Scholar]
- 11.Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347–354. doi: 10.1056/NEJM199802053380602. Available from: http://dx.doi.org/10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 12.Guerin C. Ventilation in the prone position in patients with acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care. 2006;12(1):50–54. doi: 10.1097/01.ccx.0000198999.11770.58. Available from: http://dx.doi.org/10.1097/01.ccx.0000198999.11770.58. [DOI] [PubMed] [Google Scholar]
- 13.Voggenreiter G, Aufmkolk M, Stiletto RJ, Baacke MG, Waydhas C, Ose C, Bock E, Gotzen L, Obertacke U, Nast-Kolb D. Prone positioning improves oxygenation in post-traumatic lung injury - a prospective randomized trial. J Trauma. 2005;59(2):333–341. doi: 10.1097/01.ta.0000179952.95921.49. Available from: http://dx.doi.org/10.1097/01.ta.0000179952.95921.49. [DOI] [PubMed] [Google Scholar]
- 14.Herndon DN, Barrow RE, Linares HA, Rutan RL, Prien T, Traber LD, Traber DL. Inhalation injury in burned patients: effects and treatment. Burns Incl Therm Inj. 1988;14(5):349–356. doi: 10.1016/0305-4179(88)90002-2. Available from: http://dx.doi.org/10.1016/0305-4179(88)90002-2. [DOI] [PubMed] [Google Scholar]
- 15.Rue LW, 3rd, Cioffi WG, Mason AD, McManus WF, Pruitt BA., Jr Improved survival of burned patients with inhalation injury. Arch Surg. 1993;128(7):772–778. doi: 10.1001/archsurg.1993.01420190066009. [DOI] [PubMed] [Google Scholar]
- 16.Thompson PB, Herndon DN, Traber DL, Abston S. Effect on mortality of inhalation injury. J Trauma. 1986;26(2):163–165. doi: 10.1097/00005373-198602000-00012. Available from: http://dx.doi.org/10.1097/00005373-198602000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Masanès MJ, Legendre C, Lioret N, Saizy R, Lebeau B. Using bronchoscopy and biopsy to diagnose early inhalation injury: Macroscopic and histologic findings. Chest. 1995;107(5):1365–1369. doi: 10.1378/chest.107.5.1365. Available from: http://dx.doi.org/10.1378/chest.107.5.1365. [DOI] [PubMed] [Google Scholar]
- 18.Schneider W, Berger A, Mailander P, Tempka A. Diagnostic and therapeutic possibilities for fibreoptic bronchoscopy in inhalation injury. Burns Incl Therm Inj. 1988;14(1):53–57. doi: 10.1016/S0305-4179(98)90044-4. Available from: http://dx.doi.org/10.1016/S0305-4179(98)90044-4. [DOI] [PubMed] [Google Scholar]
- 19.Kolobov T, Gattinoni L, Moretti MP, Prato P, Mascheroni D, Tsuno K. Mechanical pulmonary ventilation at high airway pressures: is it safe? Int J Artif Organs. 1984;7(6):315–316. [PubMed] [Google Scholar]
- 20.Lain DC, DiBenedetto R, Morris SL, Van Nguyen A, Saulters R, Causey D. Pressure control inverse ratio ventilation as a method to reduce peak inspiratory pressure and provide adequate ventilation and oxygenation. Chest. 1989;95(5):1081–1088. doi: 10.1378/chest.95.5.1081. Available from: http://dx.doi.org/10.1378/chest.95.5.1081. [DOI] [PubMed] [Google Scholar]
- 21.Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M. Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation: An experimental study. Am Rev Respir Dis. 1987;135(2):312–315. doi: 10.1164/arrd.1987.135.2.312. [DOI] [PubMed] [Google Scholar]
- 22.Amato MB, Barbas CS, Medeiros DM, Schettino Gde P, Lorenzi Filho G, Kairalla RA, Deheinzelin D, Morais C, Fernandes Ede O, Takagaki TY, et al. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome: A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1835–1846. doi: 10.1164/ajrccm.152.6.8520744. [DOI] [PubMed] [Google Scholar]
- 23.Bolivar J, Hultquist K, Raszynski A, Torbati D, Sherry N, Sussmane JB, Wolfsdorf J. Intratracheal pulmonary ventilation versus conventional mechanical ventilation: continuous carinal pressure monitoring at low and high flows and frequencies. ASAIO J. 2001;47(3):215–219. doi: 10.1097/00002480-200105000-00010. Available from: http://dx.doi.org/10.1097/00002480-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330(7502):1243. doi: 10.1136/bmj.38467.485671.E0. Available from: http://dx.doi.org/10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]