Abstract
Products that contain twig extracts of pawpaw (Asimina triloba, Annonaceae) are widely consumed anticancer alternative medicines. Pawpaw crude extract (CE) and purified acetogenins inhibited hypoxia-inducible factor-1 (HIF-1)-mediated hypoxic signaling pathways in tumor cells. In T47D cells, pawpaw CE and the acetogenins 10-hydroxyglaucanetin (1), annonacin (2), and annonacin A (3) inhibited hypoxia-induced HIF-1 activation with IC50 values of 0.02 μg/mL, 12 nM, 13 nM, and 31 nM, respectively. This inhibition correlates with the suppression of the hypoxic induction of HIF-1 target genes VEGF and GLUT-1. The induction of secreted VEGF protein represents a key event in hypoxia-induced tumor angiogenesis. Both the extract and the purified acetogenins blocked the angiogenesis-stimulating activity of hypoxic T47D cells in vitro. Pawpaw extract and acetogenins inhibited HIF-1 activation by blocking the hypoxic induction of nuclear HIF-1α protein. The inhibition of HIF-1 activation was associated with the suppression of mitochondrial respiration at complex I. Thus, the inhibition of HIF-1 activation and hypoxic tumor angiogenesis constitutes a novel mechanism of action for these anticancer alternative medicines.
It is estimated that well over 50% of cancer patients use at least one or more complementary and alternative medicine (CAM) therapies as part of their treatment.1 Among the alternative medicines, products (e.g. Paw Paw Cell-Reg, Graviola Max, Royal Graviola, Graviola Liquid Extract) that contain twig extracts of pawpaw (Asimina triloba L. Dunal, Annonaceae) or Brazilian pawpaw (Annona muricata L., a.k.a. graviola or soursop) are reported to have exhibited antitumor efficacy both in animal models and in a limited number of clinical studies.2,3 However, the lack of rigorously controlled clinical trials has cast a shadow on the observation that the administration of pawpaw capsules rich in acetogenins decreased tumor size, reduced tumor blood flow, suppressed metastasis, and improved survival in cancer patients. Natural compounds, known as annonaceous acetogenins, are considered the active ingredients in pawpaw products.2 Found only in Annonaceae species, the annonaceous acetogenins are derivatives of long-chain fatty acids (C32 or C34) bearing a terminal γ-lactone ring that potently inhibit the activity of NADH-ubiquinone oxidoreductase, a component of the mitochondrial electron transport chain (ETC).4 In general, the inhibition of ATP production is believed to account for the broad range of antitumor, antiviral, and pesticidal activities exhibited by pawpaw extract and purified acetogenins.2
This study describes the inhibitory effects exerted by pawpaw crude extract and purified acetogenins on the important anticancer molecular target hypoxia-inducible factor-1 (HIF-1). The transcription factor HIF-1 activates the expression of more than 100 target genes that promote cellular adaptation and survival under hypoxic conditions.5–9 It is a heterodimer of the oxygen-regulated HIF-1α and the constitutively expressed HIF-1β/ARNT subunits. The classical oxygen-dependent post-translational modification of HIF-1α protein includes the prolyl hydroxylation that tags HIF-1α for pVHL-mediated ubiquitination and subsequent proteasome degradation, and the asparaginyl hydroxylation that inactivates HIF-1.5–9 Hypoxia inhibits the hydroxylases and leads to HIF-1α protein stabilization, nuclear translocation, dimerization with HIF-1β, and HIF-1 activation. Numerous clinical studies indicate that HIF-1α protein expression is associated with advanced disease stage, metastasis, and poor prognosis in cancer patients.5–9 In animal models, reduced tumor vascularization and decreased tumor growth were observed when HIF-1 was inhibited by methods that range from genetic manipulation to the administration of small molecules.5–9 In addition, HIF-1 inhibition in combination with chemotherapy or radiation yielded enhanced treatment outcomes.10,11 Currently, the following HIF-1 inhibitors have entered early phase clinical trials for cancer in the US: EZN2968 (a HIF-1A RNA antagonist), PX-478 (decreases HIF-1A gene expression and translation), and topotecan (topoisomerase inhibitor).12
Employing a combined approach that incorporates natural product chemistry and established human tumor cell lines as in vitro models, we have established that the inhibition of HIF-1-mediated hypoxic signaling pathways represents a novel mechanism of action for the alternative anticancer medicine pawpaw and its active acetogenin constituents. This discovery may aid future application of pawpaw and acetogenins as adjunct agents that inhibit HIF-1 in combined chemotherapy or radiation.
Results and Discussion
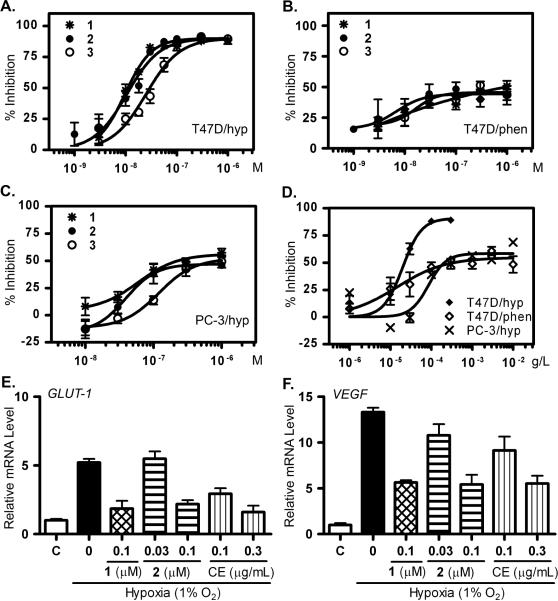
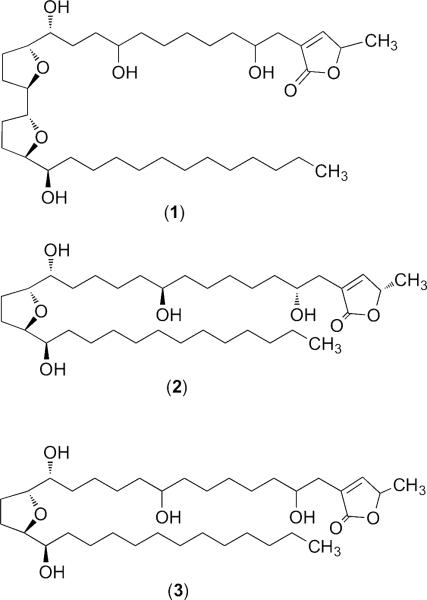
The dietary supplement containing standardized pawpaw twig extracts (Paw Paw Cell-Reg) was extracted with CH2Cl2. The crude extract (CE) inhibited hypoxia-induced HIF-1 activation by 93% at 0.5 μg/mL in a T47D cell-based reporter assay.13 Bioassay-guided isolation of the active extract yielded three known annonaceous acetogenins: 10-hydroxyglaucanetin (1), annonacin (2), and annonacin A (3). These compounds served as representative compounds suitable for confirmatory mechanistic studies. The bulk of the acetogenins remained as unresolved mixtures of compounds in the active chromatographic fractions. Concentration-response studies were performed to determine the effects of CE and purified acetogenins on HIF-1 activation. In T47D cells, compounds 1 and 2 inhibited hypoxia (1% O2)-induced HIF-1 activation with IC50 values of 12 and 13 nM, respectively (Figure 1A). Compound 3, an isomer of 2, inhibited hypoxic activation of HIF-1 with an IC50 of 31 nM (Figure 1A). All three compounds were less effective at inhibiting chemical hypoxia (10 μM 1,10-phenanthroline)-induced HIF-1 activation (IC50 > 1 μM, Figure 1B). In human prostate tumor PC-3 cells, the level of inhibition exerted by 1 – 3 appeared to plateau at ~50% on hypoxia-induced HIF-1 activation (Figure 1C). However, the EC50 values for 1 – 3 to inhibit HIF-1 activation by hypoxia were comparable in T47D and PC-3 cells. Since PC-3 cells have a modest level of HIF-1 activation under normoxic conditions,14 one possible scenario is that the pathway(s) suppressed by 1 – 3 plays a major role in hypoxic activation of HIF-1 in T47D cells, and functions as part of a complex signaling network that regulates HIF-1 activation in PC-3 cells. A similar profile of HIF-1 inhibition was observed with the pawpaw crude extract (Figure 1D). In T47D cells, pawpaw CE inhibited hypoxia-induced HIF-1 activation with an IC50 value of 0.02 μg/mL.
Figure 1. Acetogenins and pawpaw crude extract inhibit hypoxic activation of HIF-1 and its target genes.
(A – C) Concentration-response results of 1 – 3 in cell-based reporter assays: hypoxia (1% O2)-induced HIF-1 activation in T47D cells (A); chemical hypoxia (10 μM 1,10-phenanthrolin)-induced HIF-1 activation in T47D cells (B); and hypoxia (1% O2)-induced HIF-1 activation in PC-3 cells (C). (D) Concentration-response results of CE on hypoxia-induced (◆) and 1,10-phenanthroline-induced (◇) HIF-1 activation in T47D cells, and hypoxia-induced (C) HIF-1 activation in PC-3 cells. Data shown are averages ± SEM (n = 3). (E) Inhibition of the hypoxic induction (1% O2, 16 h) of GLUT-1 mRNA in T47D cells by 1, 2, or CE. The levels of GLUT-1 mRNA were normalized to 18S rRNA and presented as relative mRNA level of the normoxic control (mean ± SD, n = 3). (F) Inhibition of the hypoxic induction of VEGF mRNA by 1, 2, or CE. Data collection and analysis are the same as (E).
Around 100 genes have been identified as “HIF-1 target genes”.5–9 Some are regulated by HIF-1 in a ubiquitous fashion [e.g., vascular endothelial growth factor (VEGF)], while others respond to HIF-1 activation in a cell line-specific manner. The effects of 1, 2, and CE on hypoxic induction of HIF-1 target genes VEGF and GLUT-1 (glucose transporter-1) were examined in T47D cells. The more potent isomer 2 was used as a representative of an annonacin-type planar structure, common to both 2 and 3. The levels of VEGF and GLUT-1 mRNAs were normalized to that of 18S rRNA, an internal control. Hypoxic exposure increased GLUT-1 expression to 5.2-fold of the normoxic control (Figure 1E). Compounds 1 (0.1 μM), 2 (0.1 μM), and CE (0.3 μg/mL) inhibited the hypoxic induction of GLUT-1 gene expression by 80%, 72%, and 86%, respectively (Figure 1E). For VEGF, compounds 1, 2, and CE inhibited the 12.3-fold hypoxic induction by 62%, 64%, and 63%, respectively (Figure 1F). At lower concentrations, 2 and CE inhibited the hypoxic induction of GLUT-1 and VEGF mRNAs to a lesser degree.
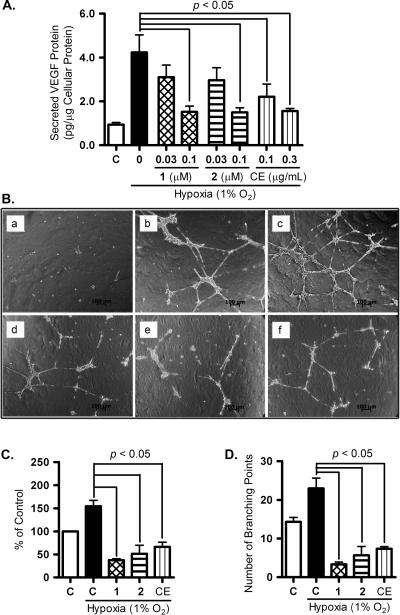
HIF-1 promotes tumor angiogenesis by increasing tumor cell production of angiogenic factors.5–9 The HIF-1 target gene VEGF is a potent angiogenic factor and agents that inhibit VEGF function are in clinical use for cancer.15 In T47D cells, hypoxia significantly increased the level of secreted VEGF protein. Compounds 1, 2, and CE each suppressed this induction of secreted VEGF protein (Figure 2A). To investigate if the decrease in secreted VEGF protein can translate into the suppression of angiogenesis, the effects of 1, 2, and CE on tumor angiogenesis were examined in a human umbilical vein endothelial cell (HUVEC)-based tube formation assay.16 In the absence of stimuli, HUVEC cells were dispersed throughout the Matrigel-coated plate (Figure 2B, panel a). Addition of recombinant VEGF protein induced HUVEC cells to form a network of tube-like structures (tube formation, Figure S1). Similar angiogenic activity was observed when the normoxic T47D cell conditioned media (CM) were used in place of recombinant VEGF protein (Figure 2B, panel b). Enhanced angiogenic activity was observed with the CM collected from hypoxic T47D cells (Figure 2B, panel c), relative to that from normoxic cells. Compounds 1, 2, and CE suppressed the ability of hypoxic T47D cells to stimulate angiogenesis (Figure 2B, panels d, e, and f, respectively). The length of tubes and the number of branching points are two criteria used to quantify the extent of angiogenesis in the tube formation assay. The quantification results (tube length - Figure 2C; number of branching points - Figure 2D) correlated with those observed (Figure 2B). Compounds 1, 2, and CE exerted significantly less pronounced effects on the angiogenic activity of normoxic T47D cells (Figure S1). Under experimental conditions, neither the purified compounds nor the extract affected HUVEC cell viability (data not shown). Thus, the anti-angiogenic activity exhibited by acetogenins and pawpaw extract is most likely achieved by reducing the level of angiogenic factors secreted by hypoxic tumor cells.
Figure 2. Compounds 1, 2, and pawpaw crude extract inhibit the induction of secreted VEGF protein and tumor angiogenesis.
(A) Levels of VEGF protein secreted by T47D cells exposed to hypoxia in the presence of 1, 2, or pawpaw crude extract (CE). The p values are provided when there is a statistically significant difference between the hypoxia-induced and the compound treated samples (mean + SD, n = 3). (B) The effects of T47D cell conditioned media (CM) on angiogenesis were evaluated in a HUVEC tube formation assay. The conditions are: a) basal media (negative control); b) CM from normoxic cells; c) CM from hypoxic cells; d) CM from hypoxic cells treated with 1 (0.1 μM); e) CM from hypoxic cells treated with 2 (0.1 μM); and f) CM from hypoxic cells treated with CE (0.1 μg/mL). (C) The length of tubes in three randomly selected fields was quantified for conditions b through f in Figure 2B. The data (mean ± SD) are presented as % of the normoxic cells (“C”). (D) The number of branching point in the conditions described in Figure 2C.
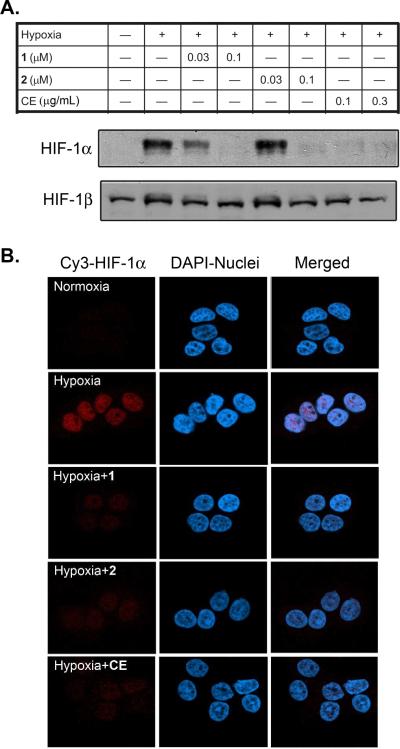
To investigate the mechanism of action for acetogenins and CE to inhibit HIF-1 activation, the accumulation of nuclear HIF-1α and HIF-1β proteins were examined by Western blot (Figure 3A). The level of HIF-1α protein was undetectable in the nuclear extract sample prepared from normoxic T47D cells. Hypoxic exposure (1% O2, 4 h) induced the accumulation of HIF-1α protein in the nucleus. Compounds 1, 2, and CE inhibited the hypoxic induction of HIF-1α protein in a concentration-dependent fashion. In contrast, levels of the constitutively expressed HIF-1β protein were not affected by 1, 2, or CE. An immunofluorescence-based approach was used to probe the effects of 1, 2 and CE on the intracellular localization of HIF-1α protein (Figure 3B). In T47D cells, HIF-1α protein was not detected under normoxic conditions. Hypoxic exposure induced the accumulation of HIF-1α protein in the nucleus. Compounds 1 and 2, and CE suppressed the induction of nuclear HIF-1α protein. This observation mirrors the findings from the Western blot analysis (Figure 3A).
Figure 3. Compounds 1, 2, and pawpaw crude extract inhibit the induction of HIF-1α protein in the nucleus.
(A) Western blot analysis of HIF-1α and HIF-1β proteins in nuclear extract samples from T47D cells exposed to hypoxia in the presence and absence of 1, 2, and CE. (B) Subcellular localization of HIF-1α protein in T47D cells exposed to hypoxia in the presence and absence of 1 (0.3 μM), 2 (0.3 μM), and CE (0.3 μg/mL). The left column shows an immunofluorescence stain for HIF-1α protein, the middle column DAPI stain for nuclei, and the right column merged images.
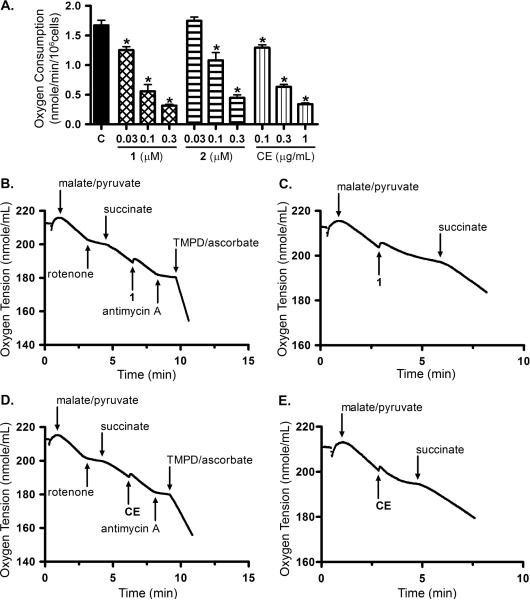
Inhibitors of mitochondrial respiration constitute one group of HIF-1 inhibitors that selectively suppress HIF-1 activation by hypoxia, relative to chemical hypoxia-induced HIF-1 activation.17,18 Acetogenins inhibited NADH oxidation by blocking mitochondrial respiratory chain complex I.4 To test the hypothesis that the suppression of mitochondrial respiration plays a major role in the inhibition of HIF-1 activation by pawpaw extract and acetogenins, the effects of 1, 2, and CE on respiration were examined in T47D cells. Both the purified acetogenins and CE inhibited cell respiration (reflected by the decreased rate of oxygen consumption) in a concentration-dependent manner (Figure 4A). The concentrations that suppressed respiration were within the range that inhibited HIF-1 activation by hypoxia. Mechanistic studies were performed to investigate if 1, 2, and CE act on complex I to suppress respiration in tumor cell-based studies. Previous studies that concluded acetogenins inhibit mitochondrial complex I were based on the observation that these compounds inhibited the oxidation of NADH, using either bovine heart submitochondrial particles or rat tissue homogenate as an enzyme source.4 In the T47D cell-based studies, mitochondrial respiration at complex I (NADH-ubiquinone oxidoreductase) was initiated upon addition of a mixture of malate and pyruvate to digitonin (30 μM)-permeabilized cells (Figures 4B to 4E). Rotenone, a known inhibitor of complex I, suppressed T47D cell respiration (Figures 4B, 4D). The inhibition exerted by complex I inhibitors (e.g., rotenone) was overcome by succinate, a substrate for complex II. The observation that 1 did not affect mitochondrial respiration in the presence of succinate suggested that 1 did not inhibit complex II, III or IV (Figure 4B). To ensure that the electron transport chain (ETC) was still functional, antimycin A (complex III inhibitor) was added to inhibit respiration and a mixture of TMPD (N,N,N′,N′-tetramethyl-p-phenylenediamine) and ascorbate (complex IV substrates) was added to re-initiate respiration that had been suppressed by complex III blockade (Figure 4B). As in the case of the complex I inhibitor rotenone, addition of succinate overcame the inhibition of cellular-respiration imposed by 1 (Figure 4C). These observations indicated that 1 selectively inhibited mitochondrial respiration at complex I, just as observed with the well characterized complex I inhibitor annonacin (2) (Figure S2). Most of the published studies on pawpaw focus on purified compounds.2 To investigate if commercially available pawpaw crude extract (Paw Paw Cell-Reg) also inhibits respiration at mitochondrial ETC complex I, further mechanistic studies were performed in the T47D cell-based system (Figs. 4D, 4E). Just as in the case of the pure compounds 1 and 2, the pawpaw crude extract inhibited mitochondrial respiration at complex I.
Figure 4. Compounds 1, 2 and pawpaw crude extract inhibit oxygen consumption in T47D cells by suppressing mitochondrial respiration at complex I.
(A) Compounds 1, 2, and CE inhibited oxygen consumption by T47D cells in a concentration-dependent manner. Data are mean ± SD from three independent experiments. An asterisk indicates p < 0.05 when compared to the control. (B) Compound 1 (0.3 μM) did not affect mitochondrial respiration at complex II, III, or IV. (C) Compound 1 suppressed mitochondrial respiration by inhibiting complex I. (D) CE (1 μg/mL) did not affect complex II, III, or IV. (E) CE inhibited complex I.
One of the mechanisms employed by tumor cells to survive under hypoxic conditions is to activate HIF-1 and its downstream signaling pathways.5–9 Concentration-response studies were performed to determine if 1 – 3 and CE suppress hypoxic tumor cell viability. Similar experiments were conducted under normoxic conditions as controls. Among the human tumor cell lines examined (T47D, MDA-MB-231, PC-3, and DU-145), neither the acetogenins (1 to 100 nM in half-log increments) nor the CE (0.01 to 1 μg/mL in half-log increments) suppressed cell proliferation/viability by more than 50% relative to the untreated control under either normoxic (95% air, 48 h) or hypoxic conditions (1% O2, 48 h, data not shown). It was reported that an extended exposure time (i.e., 6 days) is required for mitochondrial ETC inhibitors such as acetogenins to exhibit pronounced cytostatic/cytotoxic activities.2 A six-day exposure study was carried out under normoxic conditions to assess the cytostatic/cytotoxic effects of 1 – 3 and CE. All three compounds suppressed T47D cell proliferation/viability by approximately 50% at concentrations as low as 10 nM (Supporting Information, Figure S3A). The effects on MDAMB-231, PC-3, and DU-145 cells were less pronounced (< 30% at 100 nM, data not shown). A similar cell line-dependent profile of growth inhibition (T47D was most sensitive while the others were less sensitive) was observed in the presence of CE (Supporting Information, Figure S3B). The cytostatic/cytotoxic effects of CE were further evaluated in a T47D cell-base clonogenic survival assay.19 Hypoxic exposure (1% O2, 24 h) increased the number of colonies (Figure S3C). Pawpaw extract suppressed the colony formation ability of T47D cells under both normoxic and hypoxic conditions (Supporting Information, Figure S3C). Because HIF-1 is inactive in normoxic T47D cells, mechanism(s) other than HIF-1 inhibition may also contribute to the cytostatic/cytotoxic activity of pawpaw extract.
A recent survey revealed that over 47% of approved anticancer agents are natural products or derived from natural product scaffolds.20 Meanwhile, there is a growing trend of using complementary and alternative medicine therapies for cancer treatment. To ensure chemical and biological reproducibility, herbal medicines that are typically mixtures of plant-derived chemical are sometimes standardized to a specific chemical fingerprint. The identification of molecular targeted natural products will not only facilitate the development of new chemotherapeutic agents, but also aid the bioactivity-based standardization of herbal medicines.
This study revealed that the inhibition of HIF-1 activation constitutes a novel mechanism of antitumor action for the natural products known as annonaceous acetogenins and for the herbal products (i.e., Paw Paw Cell-Reg) that contain crude plant extracts with mixtures of these acetogenins. At the molecular level, acetogenins are potent inhibitors of mitochondrial ETC complex I.4 The inhibition of mitochondrial respiration and subsequent ATP production may account for the broad biological activities exhibited by acetogenins and pawpaw extracts that range from anticancer, antimalarial, antiviral, antimicrobial, antiparasitic, to pesticidal activities.2 Antitumor studies on acetogenins have focused on the cytotoxic/cytostatic effects of these compounds that are presumed to be caused by the overall depletion of cellular ATP.2 Under the conditions that suppressed hypoxia-induced HIF-1 activation, neither the purified acetogenins nor the crude extract significantly affected cellular ATP levels (Supporting Information, Figure S4). This observation mirrors an earlier finding that bullatacin did not decrease the levels of ATP in human CEM leukemic cells until the exposure time was extended to three days.2
Because the concentrations of acetogenins and pawpaw crude extract that inhibited HIF-1 activation correlated with those that suppressed mitochondrial respiration, it is possible that the HIF-1 inhibitory activities may result from the down-regulation of mitochondria-mediated signaling pathways. One of the well-supported theories is that hypoxia increases the levels of reactive oxygen species (ROS) released by ETC complex III, which then inactivate the non-heme iron-dependent hydroxylases that destabilize and inactivate HIF-1α protein.21 This results in the activation of HIF-1. Inhibitors of ETC complex I (i.e., acetogenins) may suppress ROS production at complex III by blocking the electron flow.
Both the HIF-1 inhibitory and cytotoxic/cytostatic activities of acetogenins and CE appear to be cell line-dependent. Tumor cell populations that rely solely on mitochondria to generate ATP are most sensitive to inhibitors of ETC function. In contrast, aggressive and malignant tumor cells often utilize aerobic glycolysis to fuel cellular metabolism and function. Thus, they are less sensitive to antitumor agents that affect mitochondria. Although neither purified acetogenins nor pawpaw crude extracts have been approved by the FDA for cancer treatment, dietary supplements that contain these substances are consumed by cancer patients as alternative medicines. Findings from this study suggest that these compounds/herbal medicines may be only effective against certain tumor cell populations and that those patients who use pawpaw-based CAM therapy should also consider other therapies.
Experimental Section
General Procedures
Optical rotations were measured on a digital polarimeter (AP IV/589-546). The NMR spectra were recorded in CDCl3 on AMX-NMR spectrometers (Bruker) operating at 400, 500, 600 MHz for 1H and 100, 125, 150 MHz for 13C, respectively. Residual solvent peaks (δ 7.27 for 1H) and (δ 77.23 for 13C) were used as internal references for the NMR spectra recorded running gradients. The ESIMS spectra were determined on a Bruker Daltonic micro TOF fitted with an Agilent 1100 series HPLC and an electrospray ionization source. All solvents were from Fisher Scientific and used without further purification.
Extraction of Pawpaw and Isolation of Annonaceous Acetogenins
Paw Paw Cell-Reg (Asimina triloba L. Dunal, Nature's Sunshine) was extracted with CH2Cl2 to obtain the crude extract (CE). Bioassay-guided chromatographic separation was applied to purify compounds 1 – 3 (detailed method in Supporting Information). The proton and carbon NMR, and HRMS data of 1 – 3 (Supporting Information) match those published for 10-hydroxyglaucanetin (1),22 annonacin (2),23 and annonacin A (3).24 For biological evaluation, the samples were dissolved in isopropyl alcohol and stored at −20 °C. The final concentration of solvent was less than 0.5% (v/v) in all assays.
Cell Culture, Hypoxic Treatment, and Cell Based Reporter Assay for HIF-1 Activity
Human breast tumor T47D and MDA-MB-231, prostate tumor PC-3 and DU-145 (ATCC), and human umbilical vein endothelial cells (HUVEC, Lonza) were maintained as previously described.16 Hypoxic treatment and the cell-based pHRE3-TK-Luc reporter assay for HIF-1 activity were performed as described.13
Quantitative Real Time RT-PCR
Compound treatment, extraction of total RNA samples, gene-specific primer sequences, experimental conditions, and data analysis were previously described.25
ELISA Assay for VEGF Protein and HUVEC-Based Tube Formation Assay
The level of secreted VEGF protein in the conditioned media and the level of cellular VEGF protein in the lysate were determined by ELISA, and normalized to the amount of cellular protein.25 The procedures for the HUVEC tube formation assay, image acquisition, and data analysis were previously described.16
Nuclear Extract Preparation and Western Blot Analysis for HIF-1α and HIF-1β Proteins
Compound treatments, hypoxic exposure, nuclear extract preparation, and Western blot analysis for HIF-1α and HIF-1β proteins were performed as described.16
Immunofluorescence Analysis for HIF-1α Protein
Detailed procedure was provided in the Supporting Information. Briefly, T47D cells were exposed to hypoxic conditions in the presence and absence of compounds, fixed, permeabilized, and incubated with a primary anti-HIF-1α antibody and a secondary Cy3-conjugated goat anti-mouse IgG. A laser scanning confocal microscope (Zeiss, 510 META) was used to visualize the samples and acquire the images.
Cell and Mitochondria Respiration
An Oxytherm system equipped with a Clarke-type electrode (Hansatech) was utilized to measure cellular oxygen consumption as described.16
Statistical Analysis
Data were compared using one-way ANOVA followed by Bonfferoni post hoc analyses (GraphPad Prism 4). Differences were considered significant when p < 0.05.
Supplementary Material
Acknowledgement
The authors thank S.L. McKnight (UT Southwestern) for the pHRE-TK-luc construct, K.W. Pomper (Kentucky State University), W.J. Keller (Nature's Sunshine), and Nature's Sunshine Products, Inc. for the photograph used in the graphical abstract and Paw Paw Cell-Reg product information, S.W. Morris (St. Jude Children's Research Hospital) for reviewing the manuscript, and the UM Light Microscopy Core (NSF support DBI-0619774) for image acquisition. This research was supported in part by NIH Grants CA98787, P20RR021929, and NOAA/NIUST Grant NA16RU1496. This work was conducted in a facility constructed with NIH Research Facilities Improvement Grant C06 RR-14503-01.
Footnotes
Supporting Information Available: Detailed isolation methods, spectroscopic and spectrometric data (1H, 13C NMR spectra, specific rotations, and ESIMS for 1 – 3), angiogenesis/HUVEC tube formation assay data, mitochondrial respiration, ATP production, and cell proliferation/viability studies. The material is available free of charge via the Internet at http://pubs.acs.org.
References
- (1).Richardson MA, Sanders T, Palmer JL, Greisinger A, Singletary SE. J. Clin. Oncol. 2000;18:2505–2514. doi: 10.1200/JCO.2000.18.13.2505. [DOI] [PubMed] [Google Scholar]
- (2).McLaughlin JL. J. Nat. Prod. 2008;71:1311–1321. doi: 10.1021/np800191t. [DOI] [PubMed] [Google Scholar]
- (3).Cuendet M, Oteham CP, Moon RC, Keller WJ, Peaden PA, Pezzuto JM. Pharm. Biol. 2008;46:3–7. [Google Scholar]
- (4).Ahammadsahib KI, Hollingworth RM, McGovren JP, Hui YH, McLaughlin JL. Life Sci. 1993;53:1113–1120. doi: 10.1016/0024-3205(93)90547-g. [DOI] [PubMed] [Google Scholar]
- (5).Weidemann A, Johnson RS. Cell Death Differ. 2008;15:621–627. doi: 10.1038/cdd.2008.12. [DOI] [PubMed] [Google Scholar]
- (6).Rankin EB, Giaccia AJ. Cell Death Differ. 2008;15:678–685. doi: 10.1038/cdd.2008.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Brahimi-Horn MC, Pouysségur J. J. Cell Sci. 2009;122:1055–1057. doi: 10.1242/jcs.035022. [DOI] [PubMed] [Google Scholar]
- (8).Semenza GL. Drug Discov. Today. 2007;12:853–859. doi: 10.1016/j.drudis.2007.08.006. [DOI] [PubMed] [Google Scholar]
- (9).Poon E, Harris AL, Ashcroft M. Expert Rev. Mol. Med. 2009;11:e26. doi: 10.1017/S1462399409001173. [DOI] [PubMed] [Google Scholar]
- (10).Unruh A, Ressel A, Mohamed HG, Johnson RS, Nadrowitz R, Richter E, Katschinski DM, Wenger RH. Oncogene. 2003;22:3213–3220. doi: 10.1038/sj.onc.1206385. [DOI] [PubMed] [Google Scholar]
- (11).Moeller BJ, Dreher MR, Rabbani ZN, Schroeder T, Cao Y, Li CY, Dewhirst MW. Cancer Cell. 2005;8:99–110. doi: 10.1016/j.ccr.2005.06.016. [DOI] [PubMed] [Google Scholar]
- (12).U.S. NIH database [accessed March 20, 2010]; http://www.clinicaltrials.gov/ct2/search.
- (13).Hodges TW, Hossain CF, Kim YP, Zhou YD, Nagle DG. J. Nat. Prod. 2004;67:767–771. doi: 10.1021/np030514m. [DOI] [PubMed] [Google Scholar]
- (14).Zhong H, Agani F, Baccala AA, Laughner E, Rioseco-Camacho N, Isaacs WB, Simons JW, Semenza GL. Cancer Res. 1998;58:5280–5284. [PubMed] [Google Scholar]
- (15).Ferrara N, Mass RD, Campa C, Kim R. Annu. Rev. Med. 2007;58:491–504. doi: 10.1146/annurev.med.58.061705.145635. [DOI] [PubMed] [Google Scholar]
- (16).Liu Y, Veena CK, Morgan JB, Mohammed KA, Jekabsons MB, Nagle DG, Zhou YD. J. Biol. Chem. 2009;284:5859–68. doi: 10.1074/jbc.M806744200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Nagle DG, Zhou YD. Curr. Drug Targets. 2006;7:355–369. doi: 10.2174/138945006776054979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Lin X, David CA, Donnelly JB, Michaelides M, Chandel NS, Huang X, Warrior U, Weinberg F, Tormos KV, Fesik SW, Shen Y. Proc. Natl. Acad. Sci. U.S.A. 2008;105:174–179. doi: 10.1073/pnas.0706585104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Mohammed KA, Hossain CF, Zhang L, Bruick RK, Zhou YD, Nagle DG. J. Nat. Prod. 2004;67:2002–2007. doi: 10.1021/np049753f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Newman DJ, Cragg GM. J. Nat. Prod. 2007;70:461–477. doi: 10.1021/np068054v. [DOI] [PubMed] [Google Scholar]
- (21).Hamanaka RB, Chandel NS. Curr. Opin. Cell Biol. 2009;21:894–899. doi: 10.1016/j.ceb.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Waechter AI, Hocquemiller R, Laurens A, Cavé A. Nat. Prod. Lett. 1997;10:205–212. [Google Scholar]
- (23).McCloud TG, Smith DL, Chang CJ, Cassady JM. Experientia. 1987;43:947–949. doi: 10.1007/BF01951681. [DOI] [PubMed] [Google Scholar]
- (24).Lieb F, Nonfon M, Wachendorff-Neumann U, Wendisch D. Planta Med. 1990;56:317–319. doi: 10.1055/s-2006-960968. [DOI] [PubMed] [Google Scholar]
- (25).Zhou YD, Kim YP, Li XC, Baerson SR, Agarwal AK, Hodges TW, Ferreira D, Nagle DG. J. Nat. Prod. 2004;67:2063–2069. doi: 10.1021/np040140c. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.