Abstract
OBJECTIVE
To review interventions with adherence-promoting components and document their impact on glycemic control via meta-analysis.
RESEARCH DESIGN AND METHODS
Data from 15 studies that met the following criteria were subjected to meta-analysis: 1) randomized, controlled trial, 2) study sample included youth aged <19 years, 3) youth had type 1 diabetes, 4) study reported results on glycemic control; and 5) study reported use of adherence- or self-management–promoting components.
RESULTS
The 15 studies included 997 youth with type 1 diabetes. The mean effect size for pre- to posttreatment change for the intervention versus control group comparison was 0.11 (95% CI −0.01 to 0.23). This is a small effect, demonstrating very modest improvements in glycemic control. However, analysis for the pre- to posttreatment effects for the intervention group alone did show significant variability [Q(14) = 33.11; P < 0.05]. Multicomponent interventions, those that targeted emotional, social, or family processes that facilitate diabetes management, were more potent than interventions just targeting a direct, behavioral process (e.g., increase in blood glucose monitoring frequency).
CONCLUSIONS
Interventions that focus on direct, behavioral processes and neglect emotional, social, and family processes are unlikely to have an impact on glycemic control; multicomponent interventions showed more robust effects on A1C. Future clinical research should focus on refining interventions and gathering more efficacy and effectiveness data on health outcomes of the pediatric patients treated with these interventions.
Interventions with the aim of promoting diabetes management are rooted in the assumption that better adherence to diabetes management leads to better glycemic control. A recent meta-analysis in pediatric type 1 diabetes confirmed the link between adherence and glycemic control (1), supporting past research and practice guidelines documenting the critical nature of adherence (2,3). Further, it is well documented that the achievement of better glycemic control confers reduced risk of acute and long-term complications of type 1 diabetes (4–6).
Interventions with adherence-promoting components typically target direct, behavioral processes involved in diabetes management or the indirect processes that facilitate management; some interventions target both. Interventions may target the increase or improvement of knowledge and skills needed to effectively carry out a specific behavioral task. For example, these interventions target the promotion of blood glucose monitoring (BGM), insulin administration, and the coordination of those tasks with dietary intake and physical activity. Other interventions with adherence-promoting components may target the nature and quality of family communication (7) or an individual's coping skills (8,9) as they relate to diabetes management. In other words, there is an attempt to integrate and promote the multiple layers involved in effective diabetes management (10,11). Interestingly, no matter the type of intervention or targeted process, there is often a unifying “measuring stick” to determine the success of these adherence-promoting interventions: glycemic control.
In 2006, Winkley et al. (12) published a meta-analysis on psychological treatments for individuals with type 1 diabetes. The pediatric interventions were moderately successful (i.e., effect size of −0.46) in promoting psychological outcomes (e.g., reduction of distress); however, the mean effect size for glycemic control improvement was −0.35. This translated to a reduction in glycated hemoglobin of 0.48% across the 10 randomized, controlled trials included. The authors concluded that there is evidence of a modest benefit of psychological interventions for children and adolescents with type 1 diabetes; however, significant work remains, given the variability in effects across studies and the lack of highly potent psychological treatments for improved glycemic control.
Considering the findings from Winkley et al. and their challenge to develop more potent psychological interventions, we were interested in determining whether existing interventions that include adherence-promoting components would fare better with regard to improving glycemic control. That was not an aim of the study of Winkley et al. Thus, the aims of the current meta-analysis were to document the effect of interventions with adherence-promoting components on glycemic control and to detail the implications for clinical research and practice of the most effective interventions to date. We hypothesized that interventions with adherence-promoting components would demonstrate larger effects than previous findings (12), given their direct targeting of behavioral processes involved in diabetes management as well as facilitators (e.g., emotional, social, and family processes) of effective management.
RESEARCH DESIGN AND METHODS
Search strategy and study selection
A literature search of PubMed (1994–April 2009) and Scopus (1994–April 2009) was conducted using combinations of relevant keywords associated with pediatric type 1 diabetes, adherence- or self-management–promoting interventions, and glycemic control. The term type 1 diabetes was separately paired with each of the terms designating a pediatric population (children, adolescents, pediatric). Each resultant search combination was paired with an indicator of an adherence-promoting intervention (e.g., adherence, compliance, blood glucose monitoring interventions) and an indicator of glycemic outcomes (glycemic control, A1C). The results of these searches were then cross-checked and overlapping citations were removed. In addition, we reviewed several recent reviews and meta-analyses that included pediatric type 1 diabetes studies (12,13). Studies were included if they met the following criteria: 1) study was a randomized, controlled trial, 2) individuals in the study sample had type 1 diabetes, 3) study sample included youth aged <19 years, 4) study reported results on adherence and glycemic control; and 5) study reported using an intervention with adherence-promoting components.
Study coding and analysis of reliability
We categorized intervention type as direct or combined. Direct interventions were those that focused entirely (or almost entirely) on direct, behavioral processes. For example, an intervention that targeted an increase in the frequency of BGM and provided education or training on this topic was considered a direct intervention. Combined interventions focused on one or several behavioral tasks, but the emphasis of the intervention was on promoting coping or problem-solving skills or a family process involved in diabetes management. For example, a combined intervention may have targeted an increase in BGM adherence but was also focused on identifying and resolving barriers to improving BGM adherence. We also calculated the percentage of the intervention that explicitly targeted adherence promotion. For example, a study included in this meta-analysis (14) provided a description of the intervention as well as an extensive table detailing session objectives and components. Three raters (K.K.H., J.M.R., and C.M.P.) separately determined the percentage of the information described that focused on adherence promotion (e.g., education and skill development for adherence tasks and overcoming barriers to adherence). This was done for each study included in the meta-analysis. We also coded the control group as either “standard care” in which the control group only received their standard care in the diabetes clinic or as “standard care plus controlled variable” (e.g., attention, technological device, or service access).
In addition, two authors (J.M.R. and C.M.P.) coded studies across 10 characteristics of the sample (year of publication, mean age, percent female, percent ethnic minority, mean duration of type 1 diabetes, sample size [total, experimental, and control], mean A1C at baseline and follow-up [experimental and control], delivery format of the intervention [group versus individual], time to follow-up, and statistics reported for adherence and A1C). Time to follow-up was defined as the posttreatment time point designated by the authors as the primary focus of the analysis. This was either the posttreatment effect or the first follow-up effect, typically within 6 months of the end of treatment. Finally, we reversed the valence of the effect size to be consistent with typical health promotion interventions. In other words, a positive effect size showed that the A1C value was reduced: positive health promotion. A negative effect size in this meta-analysis indicates a worsening of glycemic control. The double-entered data were then compared and κ coefficients (for categorical variables) or intraclass correlations (for interval variables) were calculated.
Primary and secondary analyses
We were primarily interested in the magnitude of the effect size for change in glycemic control from pre- to posttreatment for the intervention group versus the control group. To arrive at this, we first calculated an effect size for 1) pre- to posttreatment change for the intervention group and 2) pre- to posttreatment change for the control group. Then, we calculated change scores for the pre- to posttreatment intervention versus control comparison using an approach similar to that described by Lipsey and Wilson (15) and Winkley et al. (12). Specifically, the mean change was divided by the pooled SD of the two groups in each study. It was necessary to proceed with these steps to not only test the primary treatment effect but also to be sure the studies were adequately controlled (i.e., there was no change in the control groups). We also examined the association among study effect size, characteristics of the sample, time to follow-up, and the rated percentage of adherence promotion in the intervention.
Statistical analysis
We used the analytic approach described in Lipsey and Wilson (15) and completed analyses in SAS (SAS Institute, Cary, NC). When calculating the mean effect size across studies, we used a weighted least squares approach in which each effect size was weighted by the inverse of its variance (16). This accounts for variability across individual observations (i.e., studies) while considering the size of the sample. Specifically, the mean effect size, its SE, and 95% CI were calculated. Homogeneity analyses (16) were conducted to determine whether the mean effect size was accurately predicted by each individual effect size. Homogeneity analyses provide a fuller understanding of similarities and differences among the studies included in the meta-analysis. We calculated the Q statistic and determined its statistical significance. Significant Q values indicate rejection of the null hypothesis of homogeneity (i.e., there is heterogeneity in study effect sizes).
RESULTS
Search results and coding reliability
Our search identified 27 studies; however, upon further review, 12 studies did not meet our inclusion criteria. These 12 studies were excluded because they were not randomized, controlled trials (n = 10), only a small fraction of the sample was aged <19 years (n = 1), or no data were provided (nor could be obtained via contact with authors) on A1C values (n = 1). Thus, we identified 15 studies that met our inclusion criteria (7,8,10,11,14,17–26). Coding of the study design, intervention components, and categories of interest in each study were completed and κ and intraclass correlation coefficients were all 1.00.
Study characteristics
Table 1 displays the characteristics of the 15 studies. Most studies were conducted in the U.S.; one study was conducted in the U.K. (25) and another in India (22). Study sample sizes ranged from 22 to 127, and the total sample size across studies was 997. All studies reported recruiting the study sample from the larger pediatric diabetes clinic population, suggestive of a convenience sample. However, two studies reported an inclusion criterion of “poor” glycemic control indicated by a certain A1C threshold (e.g., ≥8.5%) (11,18). The average age of the pooled samples was 13.55 ± 2.23 years. All but two studies reported the percentage of female participants; the average across studies was 50.2%. Eight studies reported the race/ethnicity of the sample; the average proportion of nonwhite individuals in those samples was 27.0%. However, there was considerable variability in that the studies ranged from 4 to 74% inclusion of minority participants. Very few studies reported indicators of socioeconomic status and family structure (e.g., proportion of families with two caregivers in home); thus, we did not collect data on these variables. Time to follow-up ranged from 12 to 52 weeks with an average length of 29.5 weeks. Of note, only five studies were less than 26 weeks. Attrition rates were available for nine of the studies; it ranged from 3.4 to 13.3%.
Table 1.
Characteristics of studies in meta-analysis
| First author | Year (ref.) | Sample size | Mean age in years (range) | Type of intervention* | Dose of intervention (time)† | % intervention targeting adherence‡ | Type of control group | No. weeks to follow-up | Effect size§ |
|---|---|---|---|---|---|---|---|---|---|
| Anderson | 1999 (10) | 55 | 12.70 (10–15) | Combined; delivered in clinic; individual families | 4 (1-h) | 80 | Standard care | 52.00 | −0.55 |
| Brown | 1997 (17) | 59 | No mean (8–16) | Direct; diabetes video game; individual play at home | 6 months of access to game | 80 | Video game: no diabetes content | 26.00 | −0.07 |
| Cook | 2002 (14) | 53 | 14.60 (13–18) | Combined; delivered in groups; problem-solving | 6 (2-h) | 100 | Standard care | 26.00 | 0.10 |
| Ellis | 2005 (11) | 127 | 13.25 (10–17) | Combined; individual multisystemic therapy | ∼3 per week/for 6 months | 70 | Standard care | 30.00 | 0.10 |
| Grey | 2000 (8) | 75 | 14.20 (12–20) | Combined; delivered in groups; coping skills | 6 weekly + 10 monthly (∼1 h) | 25 | Standard care | 52.00 | 0.49 |
| Howe | 2005 (18) | 54 | 12.40 (3–17) | Direct; individual family instruction, then phone calls | 12 weekly calls + 3 bimonthly calls | 25 | Standard care | 26.00 | 0.09 |
| Kumar | 2004 (19) | 40 | 13.60 (8–18) | Direct; diabetes motivational game, individual home play | Access for 4 weeks | 80 | PDA only | 15.00 | −0.22 |
| Laffel | 2003 (20) | 100 | 12.10 (8–17) | Combined; delivered in clinic; individual families | 4 (1-h) | 90 | Standard care | 52.00 | 0.39 |
| Marrero | 1995 (21) | 106 | 13.30 (no range) | Direct; individual instruction; home uploads of BGM | 26 calls + download of BGM | 80 | Standard care | 52.00 | −0.07 |
| Matam | 2000 (22) | 40 | 18.25 (15–22) | Combined; individual sessions; problem-solving | 15 (1-h) sessions | 100 | Standard care | 13.00 | 0.40 |
| McNabb | 1994 (23) | 22 | 9.86 (8–12) | Combined; delivered in groups; family-focused | 6 (1-h) | 50 | Standard care | 12.00 | 0.05 |
| Nansel | 2007 (24) | 78 | 13.80 (11–16) | Combined; individual families; problem-solving | 6 (1-h) | 100 | Standard care + educational booklet | 26.00 | 0.18 |
| Viner | 2003 (25) | 41 | 13.15 (10–17) | Combined; delivered in groups; problem-solving | 6 (1-h) | 90 | Standard care | 21.00 | 0.59 |
| Wysocki | 2000 (7) | 79 | 14.30 (12–17) | Combined; individual sessions; BFST | 10 (1-h) | 15 | Standard care | 13.00 | −0.05 |
| Wysocki | 2006 (26) | 68 | 14.17 (11–16) | Combined; individual sessions; BFST-D | 12 (1-h) | 20 | Standard care | 26.00 | 0.21 |
*Type of intervention is defined as combined (direct and indirect processes targeted) or direct (direct processes only).
†Dose of intervention refers to the number of sessions.
‡Percent intervention targeting adherence was determined by review of articles by three authors (K.K.H., J.M.R., and C.M.P.).
§Effect size is the pre- to posttreatment, intervention vs. control group effect size; positive effect sizes reflect improvement in glycemic control (i.e., health promotion) and negative effect sizes reflect deterioration in glycemic control. The methods of Viner et al. (25) suggest potential selection bias; recruited individuals were from a pool of assessed individuals. It is unclear whether they were randomly drawn in the assessment study. BFST, behavioral family systems therapy (D, diabetes).
Diabetes-specific variables consistently reported in studies were duration of type 1 diabetes and glycemic control. Across the 15 studies, mean duration of type 1 diabetes ranged from 2.7 to 8.7 years; average across the studies was 5.89 ± 3.60 years. The mean A1C for the experimental group was 9.61 ± 1.83% (range 7.8–11.9%) at baseline and 9.17 ± 1.53% (range 7.5–12.3%) at follow-up. The mean A1C for the control group at baseline was 9.75 ± 1.83% and at follow-up was 9.70 ± 1.76%.
Mean effect sizes
The mean effect size for the pre- to posttreatment change in glycemic control for the intervention group was 0.13, with individual study effects ranging from −0.50 to 0.99. Overall, there was modest improvement for individuals in the pooled intervention group. The mean effect size for the pre- to posttreatment change in the control group was −0.01, with individual study effects ranging from −0.24 to 0.32. This effect size indicates that glycemic control did not change over time for the pooled control group.
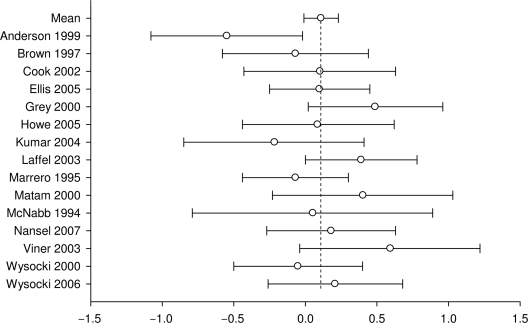
The mean effect size for pre- to posttreatment change for the intervention versus control group comparison was 0.11 (95% CI −0.01 to 0.23). Effects ranged from −0.55 to 0.59, and five were negative (i.e., deterioration in glycemic control). The mean effect size of 0.11 meets conventional standards for a small effect and indicates that there was very modest improvement in glycemic control over time. Effect sizes and confidence intervals for the individual studies are presented in Fig. 1. The association between the mean effect size for pre- to posttreatment change for the intervention versus control group and time to follow-up was not significant (r = −0.07, P > 0.05). The correlation between the pre- to posttreatment intervention versus control effect size and whether the intervention targeted direct, behavioral processes alone or had combined targets was significant (Spearman r = 0.56, P < 0.03). This finding indicates that multicomponent interventions (i.e., those that targeted direct and indirect processes together) were associated with larger effects on glycemic control. Finally, because only a small number of studies were delivered in a group format and all others were done individually, we did not conduct a comparison based on intervention delivery format.
Figure 1.
Effect sizes and confidence intervals for the individual studies.
Factors associated with mean effect size
Homogeneity analysis of the pre- to posttreatment intervention versus control group comparison revealed homogeneity across the 15 studies [Q(14) = 18.40; P > 0.05]. In other words, there was little variability in effects across these randomized, controlled trials. However, analysis for the pre- to posttreatment effects for the intervention group alone did show significant variability [Q (14) = 33.11, P < 0.05]. This result illustrates that even though studies were adequately controlled, the interventions produced different magnitudes of A1C change. We hypothesized that this variability could be attributed to the percentage of the intervention targeting adherence promotion. In other words, interventions that focused almost entirely on adherence promotion should do better than those that included components other than adherence promotion. However, the correlation was not statistically significant (P > 0.05).
CONCLUSIONS
Results of this meta-analysis show that the mean effect size for the pre- to posttreatment change between intervention and control groups was 0.11. Whereas the mean change of A1C values from baseline to follow-up for youth in the intervention groups of these studies was 9.6 to 9.2%, variability in effects and the weighting of effects based on sample size translates to just a modest 0.20% reduction in A1C values. Overall, this meta-analysis shows that the pooled effect on glycemic control of these 15 interventions was very modest.
Before identifying the implications of these meta-analytic results, we want to highlight the context of these findings as well as the positive aspects of these results. This meta-analysis included 14 studies not reviewed in the meta-analysis of Winkley et al. (12); the only overlapping study was by Wysocki, Harris, and colleagues (26). Thus, this meta-analysis extends the current evidence base for interventions deployed in pediatric type 1 diabetes. Interestingly, the interventions that we described as “adherence-promoting interventions” fared worse overall than the psychological interventions in the prior meta-analysis. Specifically, the mean effect size in this meta-analysis was 3 times smaller than that reported by Winkley et al. (12). One reason for this may be our inclusion of interventions targeting direct, behavioral processes because these studies conferred little benefit on glycemic control. In our meta-analysis, the interventions that fared the best were those that were multicomponent and addressed both the direct and indirect processes involved in diabetes management. For example, the coping skills training program of Grey et al. (8) produced a pre- to posttreatment intervention versus control effect size of 0.49. This program trains groups of youth with type 1 diabetes to “increase the[ir] ability…to cope with problems that they face on a day-to-day basis and to be more effective in achieving therapeutic goals” (8). Their inclusion of diabetes-specific social scenarios may have served to buttress the development of general coping skills. At least three other studies (20,22,25) were similarly multicomponent and had effect sizes of ∼≥0.40. Two other studies (24,26) also contained similar components and had effect sizes of ∼0.20. Overall, these interventions seem to be exemplars for the type of interventions that carry considerable benefit for improvement in glycemic control.
On the other hand, the mean effect size of this meta-analysis provides a sobering look at the current state of interventions with adherence-promoting components if improvement in glycemic control is the measuring stick. Why is the mean effect size so small and why do only a few interventions produce considerable benefit on glycemic control? This meta-analysis can rule out several answers to that question. First, the percentage of the intervention directly targeting adherence promotion does not seem to be a factor. What appears important is whether or not the indirect processes are targeted in the intervention. If so, the benefit on glycemic control should be more favorable. As noted nearly two decades ago by Johnson and her colleagues (2,27), adherence is just one of the multiple factors that influence glycemic control. Perhaps the primary focus on adherence behaviors and the neglect of other areas related to glycemic control (social support, family relationships, coping, and problem-solving skills) is what drove the present findings. Second, and related to the first point, the dose of the intervention does not appear to be a factor. A sizable effect on glycemic control was observed in the study by Laffel, Anderson, and colleagues (20), which included approximately four clinic-based intervention sessions across the year plus support from the “Care Ambassador” in scheduling appointments and working with clinic staff. The dose in this study was considerably less than that in other time- and resource-heavy interventions (11,26), both with more modest effects on glycemic control, as well as that in an earlier iteration of the Anderson and Laffel family-based intervention (10). Admittedly, the unmeasured competing needs of the participants across these studies may not make this a fair comparison. Nevertheless, dose appears to be less important than the inclusion of multiple components with the aim of facilitating adherence promotion. Third, there was no association between time to follow-up and effect sizes. Because these studies were controlled and there was little change in glycemic control for the control participants, simply stopping the deterioration of glycemic control that is so commonly seen across late childhood and adolescence (28–30) was not enough to demonstrate statistical significance. Although there is certainly clinical significance in preventing further deterioration, the interventions that reduced A1C values stood out and the length of time to the follow-up assessment did not matter.
The primary implication of these meta-analytic results is that there is considerable work left to be done to make a significant impact on glycemic outcomes. However, after a thorough review of the most potent interventions, we conclude there is no need to start over. For example, we should learn from the interventions that produce reductions in A1C values approaching 1.0% (e.g., from 9.5 to 8.5%). These should be replicated and deployed in clinics to further demonstrate their effectiveness. We should also obtain a better understanding of how much cost-savings these interventions provide. For example, to what extent do they reduce acute and long-term medical complications that show up in extra medical and emergency department visits? Further, what are the direct costs to the clinics in terms of staffing and supplies and will insurance companies reimburse for these services? Likewise, an evaluation of psychosocial functioning (e.g., health-related quality of life) will also provide critical information about the broader impact of these interventions.
At the same time efforts are made to document effectiveness, the interventions demonstrating modest effects on glycemic control may benefit from the addition of other components and then a reexamination of their efficacy. For example, the most efficacious interventions target processes other than direct, behavioral processes; they target the critical emotional, social, and family factors that youth with type 1 diabetes face on a daily basis. By focusing more so on these facilitators of adherence, these interventions may demonstrate improved efficacy. Considered together, the collection of effectiveness data on the most potent interventions and adapting and refining less potent interventions will push the field closer to providing evidence-based care in pediatric diabetes clinics.
The results of this meta-analysis and our recommendations should be considered in the context of several limitations. First, a meta-analysis pools studies and cannot account for differing methodologies and sampling strategies (31). Even with randomization and control conditions, the heterogeneity in individual effect sizes among the interventions included highlights that fact that there is considerable variability in the potency of these interventions. The extent to which that variability is related to the sampling methodology and features of study design cannot be ascertained through meta-analysis. Second, the teams of investigators from these 15 studies may not have viewed adherence promotion as the primary mechanism to change glycemic control. The primary targets of the interventions (i.e., hypothesized mechanism to promote change in A1C) may have been broader than adherence promotion and encompassed family, system, or emotional variables. We simply identified interventions with adherence-promoting components and may not be fully characterizing the whole treatment package. Third, and related to the last point, our team made decisions about the coding of multiple variables (time to follow-up, treatment components, and percentage of adherence promotion). Although we were guided by past research and clinically guided assumptions, others may have coded these variables in a different manner.
Fourth, other variables that influence glycemic control (e.g., growth, puberty, and insulin regimen) were not examined in this study, yet there is compelling evidence for their contribution to suboptimal glycemic outcomes (29,32,33). Further, there are inconsistent reports of sociodemographic variables such as socioeconomic status and family structure across these studies. In fact, some do not provide any data on these characteristics. Given the links between these variables and glycemic outcomes (34–36), future reports should include indicators of socioeconomic status such as family income, educational achievement, occupational status, or full socioeconomic scales. A related limitation is that few of the studies targeted “high-risk” youth, those who consistently demonstrate high A1C values and have fewer resources and support. These youth and their families may respond better to higher doses of treatment and attention to the multiple systems in which they attempt to manage diabetes. Indeed, there are compelling data on the effectiveness of these types of programs with these high-risk youth (37,38). Finally, we did not include an examination of changes in adherence in the included studies. Given the data that adherence is linked to glycemic control (1) and a focus on optimizing glycemic control in practice guidelines (3), we were primarily concerned with understanding whether these interventions alter glycemic outcomes. Although we do not suspect this to be the case, it is possible that some interventions included in this meta-analysis improved adherence significantly while not altering glycemic control.
In sum, this review and meta-analysis of interventions focused on adherence promotion in pediatric type 1 diabetes emphasizes two points. First, it is likely that glycemic control will not improve if interventions focus on direct, behavioral processes involved in diabetes management and neglect emotional, social, and family processes. Second, we need to implement the effective programs in pediatric diabetes clinics and obtain effectiveness data. It is important that we better understand the costs and savings from a monetary perspective and also from the perspective of health outcomes of the pediatric patients cared for in these clinics.
Acknowledgments
K.K.H. is supported by a career development award (K23-DK-073340) from the National Institute of Diabetes and Digestive and Kidney Diseases.
No potential conflicts of interest relevant to this article were reported.
We thank Drs. Thomas Frazier and Shoshana Kahana for their guidance on developing the study database and conducting data analysis.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Hood KK, Peterson CM, Rohan JM, Drotar D: Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics 2009; 124: e1171–e1179 [DOI] [PubMed] [Google Scholar]
- 2. Johnson SB, Kelly M, Henretta JC, Cunningham WR, Tomer A, Silverstein JH: A longitudinal analysis of adherence and health status in childhood diabetes. J Pediatr Psychol 1992; 17: 537–553 [DOI] [PubMed] [Google Scholar]
- 3. Silverstein JH, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N: Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 2005; 28: 186–212 [DOI] [PubMed] [Google Scholar]
- 4. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. Diabetes Control and Complications Trial Research Group. J Pediatr 1994; 125: 177–188 [DOI] [PubMed] [Google Scholar]
- 5. White NH, Cleary PA, Dahms W, Goldstein D, Malone J, Tamborlane WV: Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA 2002; 287: 2563–2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Svoren BM, Volkening LK, Butler DA, Moreland EC, Anderson BJ, Laffel LM: Temporal trends in the treatment of pediatric type 1 diabetes and impact on acute outcomes. J Pediatr 2007; 150: 279–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wysocki T, Harris MA, Greco P, Bubb J, Danda CE, Harvey LM, McDonell K, Taylor A, White NH: Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol 2000; 25: 23–33 [DOI] [PubMed] [Google Scholar]
- 8. Grey M, Boland EA, Davidson M, Li J, Tamborlane WV: Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr 2000; 137: 107–113 [DOI] [PubMed] [Google Scholar]
- 9. Boardway RH, Delamater AM, Tomakowsky J, Gutai JP: Stress management training for adolescents with diabetes. J Pediatr Psychol 1993; 18: 29–45 [DOI] [PubMed] [Google Scholar]
- 10. Anderson BJ, Brackett J, Ho J, Laffel LM: An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care 1999; 22: 713–721 [DOI] [PubMed] [Google Scholar]
- 11. Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham P, Cakan N: Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes in chronic poor metabolic control: a randomized controlled trial. Diabetes Care 2005; 28: 1604–1610 [DOI] [PubMed] [Google Scholar]
- 12. Winkley K, Ismail K, Landau S, Eisler I: Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 2006; 333: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kahana S, Drotar D, Frazier T: Meta-analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. J Pediatr Psychol 2008; 33: 590–611 [DOI] [PubMed] [Google Scholar]
- 14. Cook S, Herold K, Edidin DV, Briars R: Increasing problem solving in adolescents with type 1 diabetes: the choices diabetes program. Diabetes Educ 2002; 28: 115–124 [DOI] [PubMed] [Google Scholar]
- 15. Lipsey MW, Wilson DB: Practical Meta-Analysis. Thousand Oaks, CA, SAGE Publications, 2001 [Google Scholar]
- 16. Hedges LV, Olkin I: Statistical Methods for Meta-Analysis. Orlando, FL, Academic Press, 1985 [Google Scholar]
- 17. Brown SJ, Lieberman DA, Germeny BA, Fan YC, Wilson DM, Pasta DJ: Educational video game for juvenile diabetes: results of a controlled trial. Med Inform (Lond) 1997; 22: 77–89 [DOI] [PubMed] [Google Scholar]
- 18. Howe CJ, Jawad AF, Tuttle AK, Moser JT, Preis C, Buzby M, Murphy KM: Education and telephone case management for children with type 1 diabetes: a randomized controlled trial. J Pediatr Nurs 2005; 20: 83–95 [DOI] [PubMed] [Google Scholar]
- 19. Kumar VS, Wentzell KJ, Mikkelsen T, Pentland A, Laffel LM: The DAILY (Daily Automated Intensive Log for Youth) trial: a wireless, portable system to improve adherence and glycemic control in youth with diabetes. Diabetes Technol Ther 2004; 6: 445–453 [DOI] [PubMed] [Google Scholar]
- 20. Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ: Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr 2003; 142: 409–416 [DOI] [PubMed] [Google Scholar]
- 21. Marrero DG, Vandagriff JL, Kronz K, Fineberg NS, Golden MP, Gray D, Orr DP, Wright JC, Johnson NB: Using telecommunication technology to manage children with diabetes: the Computer-Linked Outpatient Clinic (CLOC) Study. Diabetes Educ 1995; 21: 313–319 [DOI] [PubMed] [Google Scholar]
- 22. Matam P, Kumaraiah V, Munichoodappa C, Kumar KM, Aravind S: Behavioural intervention in the management of compliance in young type-I diabetics. J Assoc Physicians India 2000; 48: 967–971 [PubMed] [Google Scholar]
- 23. McNabb WL, Quinn MT, Murphy DM, Thorp FK, Cook S: Increasing children's responsibility for diabetes self-care: the In Control study. Diabetes Educ 1994; 20: 121–124 [DOI] [PubMed] [Google Scholar]
- 24. Nansel TR, Iannotti RJ, Simons-Morton BG, Cox C, Plotnick LP, Clark LM, Zeitzoff L: Diabetes personal trainer outcomes: short-term and 1-year outcomes of a diabetes personal trainer intervention among youth with type 1 diabetes. Diabetes Care 2007; 30: 2471–2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Viner RM, Christie D, Taylor V, Hey S: Motivational/solution-focused intervention improves HbA1c in adolescents with type 1 diabetes: a pilot study. Diabet Med 2003; 20: 739–742 [DOI] [PubMed] [Google Scholar]
- 26. Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, Mauras N, White NH: Effects of behavioral family systems therapy for diabetes on adolescents' family relationships, treatment adherence, and metabolic control. J Pediatr Psychol 2006; 31: 928–938 [DOI] [PubMed] [Google Scholar]
- 27. Johnson SB: Psychological aspects of childhood diabetes. J Child Psychol Psychiatry 1988; 29: 729–738 [DOI] [PubMed] [Google Scholar]
- 28. Danne T, Mortensen HB, Hougaard P, Lynggaard H, Aanstoot HJ, Chiarelli F, Daneman D, Dorchy H, Garandeau P, Greene SA, Hoey H, Holl RW, Kaprio EA, Kocova M, Martul P, Matsuura N, Robertson KJ, Schoenle EJ, Søvik O, Swift PG, Tsou RM, Vanelli M, Aman J: Persistent differences among centers over 3 years in glycemic control and hypoglycemia in a study of 3,805 children and adolescents with type 1 diabetes from the Hvidore Study Group. Diabetes Care 2001; 24: 1342–1347 [DOI] [PubMed] [Google Scholar]
- 29. Moreland EC, Tovar A, Zuehlke JB, Butler DA, Milaszewski K, Laffel LM: The impact of physiological, therapeutic and psychosocial variables on glycemic control in youth with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 2004; 17: 1533–1544 [DOI] [PubMed] [Google Scholar]
- 30. Springer D, Dziura J, Tamborlane WV, Steffen AT, Ahern JH, Vincent M, Weinzimer SA: Optimal control of type 1 diabetes mellitus in youth receiving intensive treatment. J Pediatr 2006; 149: 227–232 [DOI] [PubMed] [Google Scholar]
- 31. Shapiro S: Meta-analysis/Shmeta-analysis. Am J Epidemiol 1994; 140: 771–778 [DOI] [PubMed] [Google Scholar]
- 32. Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV: Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med 1986; 315: 215–219 [DOI] [PubMed] [Google Scholar]
- 33. Grey M, Whittemore R, Tamborlane W: Depression in type 1 diabetes in children: natural history and correlates. J Psychosom Res 2002; 53: 907–911 [DOI] [PubMed] [Google Scholar]
- 34. Overstreet S, Holmes CS, Dunlap WP, Frentz J: Sociodemographic risk factors to disease control in children with diabetes. Diabet Med 1997; 14: 153–157 [DOI] [PubMed] [Google Scholar]
- 35. Hanson CL, Henggeler SW, Harris MA, Burghen GA, Moore M: Family system variables and the health status of adolescents with insulin-dependent diabetes mellitus. Health Psychol 1989; 8: 239–253 [DOI] [PubMed] [Google Scholar]
- 36. Harris MA, Greco P, Wysocki T, Elder-Danda C, White NH: Adolescents with diabetes from single-parent, blended, and intact families: health-related and family functioning. Fam Systems Health 1999; 17: 181–196 [Google Scholar]
- 37. Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham PB, Cakan N: The effects of multisystemic therapy on diabetes stress among adolescents with chronically poorly controlled type 1 diabetes: findings from a randomized, controlled trial. Pediatrics 2005; 116: e826–e832 [DOI] [PubMed] [Google Scholar]
- 38. Ellis DA, Naar-King S, Frey MA, Templin T, Rowland M, Greger N: Use of multi-systemic therapy to improve regimen adherence among adolescents with type 1 diabetes in poor metabolic control: a pilot investigation. J Clin Psychol Med Settings 2004; 11: 315–324 [Google Scholar]