Abstract
Background
Stroke incidence increases with age. Atrial fibrillation (AF) is an important risk factor for ischemic stroke and its incidence also increases with age. However oral anticoagulant therapy (OAT) tends to be underused in the elderly population.
Methods
Elderly patients (> = 80 years) with an ischemic stroke admitted in our department between 1/7/2003 and 31/6/2005 were prospectively evaluated. Baseline characteristics, risk factors, treatment and etiology according to TOAST criteria were recorded. Patients treated with OAT were followed up in order to assess any side effect and stroke recurrence. Mean follow-up was of 19.5 months (7-45) from discharge.
Results
Sixty four out of a hundred and fifty nine elderly patients (40.25%) were classified as cardioembolic; mean age was 84.5 years (80-97) and 64.6% were women. AF had been previously identified in 60% of them (16.9% were on OAT and 40.6% on antiplatelet therapy). At discharge, 32 patients (49.2%) were on OAT. In the follow-up 4 patients (12.5%) suffered systemic haemorrhages (3 urinary, 1 gastrointestinal bleeding), with no change in their functional status. Mean INR in this group was 5.9 [3-11] and, in 3 of them, OAT was cancelled. No brain haemorrhages were recorded. Ischemic stroke recurred in 4 patients (INR < 1.8 in 3 of them; the other, INR 2.35). Three patients had died at the end of the follow-up, one of them as a consequence of ischemic stroke recurrence.
Discussion
Twenty eight point eight of stroke patients admitted in the period of study were >80 years. The high proportion of cardioembolic strokes in this age segment contrasts with the general underuse of OAT as antithrombotic prophylaxis. Our study suggests that OAT is a safe strategy when carefully prescribed, even for elderly patients.
Introduction
Atrial fibrillation (AF) is present in more than 5% of >65 year-old population, increasing with age, as it is present in 10% of people ≥ 75 years [1]. Cardioembolism is the etiology in approximately 25% of strokes in patients age ≥ 80 years [2]. It is also known that paroxistic AF, very common in elderly people, raises the same risk of stroke as chronic AF [3]. Non-valvular atrial fibrillation (NVAF) is the most common cause of arrythmia, as the frequency of reumathic valvulopathy falls [1]. AF predisposes to left atrial thrombus formation and carries a sixfold increased anual risk for stroke, rising from 1.5% for those aged 50-59 years to 23.5% for those aged 80-89 years [1], [3]. Such cardioembolic strokes are very often more severe than other ischemic strokes, and are associated to a higher mortality [4], [5], [6]. The annual embolic rate attributed to AF is approximately 12% for patients >65 years-old [7], [8], [9]. It has been shown that the NIHSS and modified-Rankin scales, patients on oral anticoagulation therapy show less serious strokes and present a better functional situation at discharge than those who were not on that treatment [10]. This seems to endure as a controversial subject that leads physicians to a difficult decision when they prescribe these patients antithrombotic profilaxis.
The main objective or our study was to prospectively assess the efficacy and safety or oral anticoagulants (OA) in ≥ 80 year-old population as secondary prophylaxis of cardiembolic strokes.
Subjects and Methods
This is an observational prospective study conducted in tertiary hospital that covers an area of 400,000 habitants and it is the reference hospital of a department of one million habitants. To be eligible, patients had to be ≥ 80 years of age and a diagnosis of ischemic stroke or transient ischemic attack (TIA) had to be present. According to these inclusion criteria 159 patients were consecutively selected among all the stroke patients admitted in our Neurology Department starting July 1st 2003 until June 31st 2005. We analysed clinical characteristics, cardiovascular risk factors, previous treatment and at discharge treatment and follow-up, but also classified the stroke etiology according to TOAST criteria [11]. Patients treated with oral anticoagulants were followed up through periodical reviews, the first one at our Outpatient Clinic, 3 months from discharge; after that we have been in contact with the patients by phone every 6 months.
At admission in the Emergency Department, a brain computerized tomography (CT), blood ancillary tests including hemogram, glucose, electrolytes, vitamins, renal, liver and thyroid function, lipids, coagulation and INR (International Normalized Ratio) if having oral anticoagulants; electrocardiogram and thoracic radiography were performed in all patients.
Demographic data were recorded for all 159 patients, including age and sex, social status, previous treatment and treatment at discharge, previous stroke incidence (TIA, brain infarction or haemorrhagic brain infarction) or other neurological diseases. Other cardiovascular risk factors were also studied, including previous diagnoses of hypertension (BP ≥ 140/90), diabetes (basal glycaemia ≥ 110 mg/dl), dyslipemia (total cholesterol ≥ 220 mg/dl or LDL-cholesterol ≥ 160 mg/dl), ischemic cardiopathy, myocardiopathy, peripheral artery disease, smoking (one of more cigarettes per day) or alcohol intake (≥40 g/day). The severity of stroke and functional outcome were reflected by NIHSS, Barthel and Modified-Rankin scales.
The etiological classification has been led according to TOAST criteria [11] after practising ancillary studies, such as carotid ultrasonographic study, transcranial Doppler, Holter monitoring, echocardiogram and other specific blood analyses on an individual basis. Therefore, the strokes were classified as "cardioembolic strokes", "large-artery atherosclerosis", "small-artery occlusion", "stroke of other determined etiology" and "stroke of undetermined etiology".
We selected those patients diagnosed with cardioembolic stroke according to TOAST classification, summarizing 64 patients (42.1%) out of the total of the sample. According to the social status, risk of falls and mainly neurological and functional scales, we treated 32 of them (40.9%) with oral anticoagulants, avoiding this treatment in case of patients without social support, high risk of falls or m-Rankin score over 3. We have followed them up, analysing the adverse events related to these drugs and the clinical outcome.
Results
Five hundred and thirty patients were admitted in our Department with a diagnosis of ischemic stroke. One hundred and fifty nine of them (30%) were more than 80 years old and were selected for our study. Sixty five per cent were females, thirty five per cent were males, and mean age was 84.5 years. According to TOAST criteria, cardioembolic strokes represented 40.25% (64) of our patients, followed by large-artery atherosclerosis and small-artery occlusion representing 4.1% of our patients each. Fifty one point fifty five per cent were undetermined, twenty per cent of them for coexisting different etiologies. All the patients underwent electrocardiogram and carotid ultrasonography; holter monitoring was practised in 23% of patients and Echocardiography in 11.6% of patients.
Cardioembolic stroke population
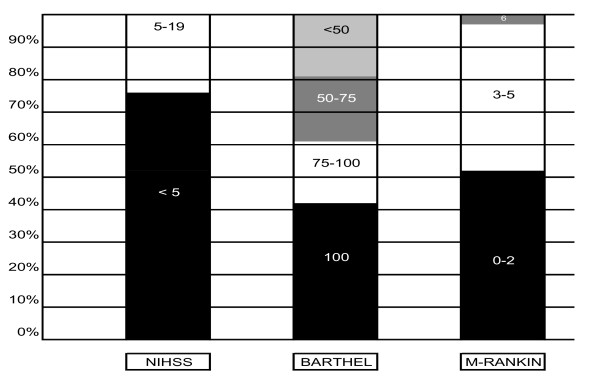
Looking at the cardioembolic subgroup, the clinical diagnosis was transient ischemic attack (TIA) in 7.8%, brain infarction in 90.6%, and haemorrhagic infarction in 1.6%. Cardiovascular risk factors (CVRF), previous treatments and neurological status at discharge are shown in Table 1, and clinical and dependency scales at discharge are also represented in Figure 1. Only 27% of patients with previously known AF were on anticoagulant therapy.
Table 1.
Clinical characteristics of cardioembolic stroke patients.
| CARDIOVASCULAR RISK FACTORS | |
|---|---|
| HT | 107 (67.2%) |
| AF | 92 (57.8%) |
| PREVIOUS STROKE | 56 (35.1) |
| DIABETES | 35 (21.9%) |
| ISCHEMIC CARDIOPATHY | 30 (18.8%) |
| DYSLIPEMIA | 21 (13.2%) |
| MYOCARDIOPATHY | 15 (9.5%) |
| PERIPHERAL ARTERY DISEASE | 5 (3.1%) |
| PREVIOUS TREATMENTS | |
| ANTIHYPERTENSIVES | 94 (59.4%) |
| STATINS | 23 (14.3%) |
| ANTIPLATELETS | 66 (41.3% ) |
| ANTICOAGULANTS | 25 (15.6%) (27% OF KNOWN AF) |
Cardiovascular risk factors, previous treatments, dependency scales at discharge.
Figure 1.
Clinical and dependency scales at discharge.
Cardioembolic stroke patients treated with oral anticoagulant
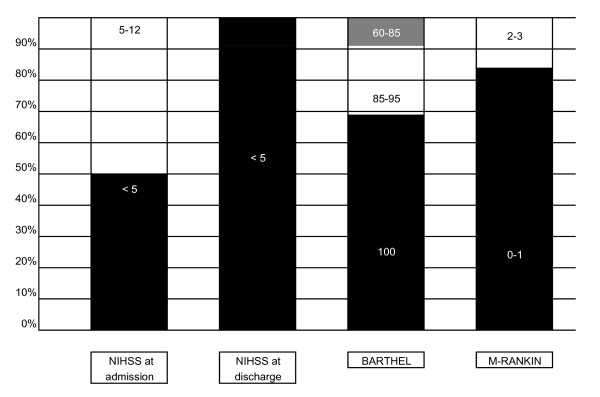
Out of all cardioembolic stroke patients, we treated with OA 40.9% of them (n = 32). Gender, age, CVRF, social support and clinical and dependency situation at discharge are showed in Table 2, and clinical and dependency scales at discharge are also represented in Figure 2. Patients on OA therapy were followed for a mean of 19.5 months (7-45) and the adverse events related to oral anticoagulation were as follow: Four patients (12.5%) suffered from a systemic haemorrhage: 3 had urinary bleeding and 1 had a gastrointestinal haemorrhage, although the M-Rankin scale score was not modified in any case. The mean INR in these patients was 5.95 [3-11]. On the other hand ischemic recurrence affected another 12.5% (4 patients) whose INR was less than 1.8 in three of them and an optimized level (INR = 2.35) in the other one. Three patients died during the follow-up because of myocardial infarction, pneumonia and recurrent ischemic stroke respectively. Withdrawal of treatment occurred in three cases, one because of a gastrointestinal haemorrhage, and the other two following the recommendations of primary healthcare physicians. There was not any intracranial haemorrhage.
Table 2.
Clinical characteristics of cardioembolic stroke patients treated with oral anticoagulant.
| GENDER AND AGE | |
|---|---|
| SEX | 40.6% male |
| AGE | 83.2 (80-89) |
| CARDIOVASCULAR RISK FACTORS | |
| HT | 21 (65.6%) |
| AF | 21 (65.6%) |
| DIABETES | 7 (21.9%) |
| DYSLIPEMIA | 6 (19.4%) |
| ISCHEMIC CARDIOPATHY | 5 (15.7%) |
| MIOCARDIOPATHY | 4 (12.9%) |
| CONGESTIVE CARDIOPATHY FAILURE | 4 (12.9%) |
| SYSTEMIC EMBOLISM EVENTS | 2 (6.3%) |
| PERIPHERAL ARTERY DISEASE | 1 (3.1%) |
| SOCIAL SUPPORT | |
| LIVING WITH FAMILY | 27 (84.4%) |
| LIVING ALONE | 4 (12.5%) |
| INSTITUTIONALIZED | 1 (3.1%) |
Figure 2.
Clinical and dependency scales at discharge.
Discussion
It has been previously demonstrated that AF is a powerful risk factor for stroke. Our results show that AF is very frequent among elderly stroke patients, rising cardioembolic stroke etiology to 40.25%. Oral anticoagulants have been proven to reduce the risk of stroke in AF by 68% compared with placebo, which is superior to the relative risk reduction of 21% associated with full-dose aspirin [12], [13], [14], [10], [15], [16]. Even more, a recently published study has suggested that aspirin at 150-200 mg per day is neither effective nor safe [17]. Despite the modest or even dubious effect associated to aspirin, this drug is widely used in antithrombotic atrial fibrillation prophylaxis as in spite of its proven benefits, numerous studies have documented an underuse of warfarin, particularly among elderly patients who would seem to benefit the most from anticoagulant therapy [18], [19]. However, OA as prophylactic treatment are fourfold increased in people younger than 80 years [17]. Haemorrhages, falls, and patient refusal or a history of nonadherence to therapy constituted nearly 80% of the physician-cited reasons for not prescribing warfarin to elderly patients [20], [21]. Other studies conclude that patients at high risk for falls with atrial fibrillation are at substantially increased risk of intracranial haemorrhage, especially traumatic haemorrhage; nevertheless, because of their high stroke rate, they appear to benefit from anticoagulant therapy if they have multiple stroke risk factors [22], [23], [24], [25]. Moreover it has been suggested that oral anticoagulation treatment not only prevents stroke but may also contribute to the development of less serious strokes with a better functional prognosis [16], [26], [25].
In our study, among 64 patients identified with AF, 40.9% (n = 32) were discharged on oral anticoagulants, selected according to the neurological and dependency scales and excluding other contraindications, as current evidence-based guidelines suggest [27], [28]. Throughout-the follow-up of these patients (7-45 months), OAT was shown as an efficient and safe treatment in these selected patients, despite being a very old population (80-89 years-old). With respect to haemorrhage risk, systemic haemorrhages were found in only four cases, without modifying the M-Rankin scale, and they corresponded to overtreated patients, as the INR reflected (mean 5.95). We did not find any intracranial haemorrhage. Although atrial fibrillation was present as a risk factor in more than a half of cardioembolic strokes, only a quarter of these patients were previously an adequate anticoagulant prophylaxis.
In summary, we would like to remark the importance of cardioembolic etiology in strokes of patients over 80 years, which contrasts with the scarcity in the appropriate use of OAT as prophylaxis. According to our results, stroke recurrence in patients on oral anticoagulation is mainly ischemic, and haemorrhagic complications that derive from oral anticoagulation would be related to overdosing. Having into account that the population is too small and the follow-up relatively short, this paper suggests that OAT might be safe in cardioembolism prophylaxis independently of age and may be effective if we compare with natural history of not anticoagulated patients [13], [14], [16], [20].
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LB carried out the search of data and patients management, drafted the manuscript and participated in the design of the study and performed the statistical analysis. SC conceived of the study and participated in its design and coordination, and also carried out patients' management and follow-up. VV and JG contributed to the data collection. CHL participated in the coordination. All authors read and approved the final manuscript.
Contributor Information
Lorena Benavente, Email: lbf_benfer@hotmail.com.
Sergio Calleja, Email: scallejap@gmail.com.
Vanessa de la Vega, Email: lbf_benfer@hotmail.com.
Jorge García, Email: lbf_benfer@hotmail.com.
Carlos H Lahoz, Email: lbf_benfer@hotmail.com.
References
- Averinos JF, Brown RD, Foley DA, Nkomo V, Petty G, Scott C, Enriquez-Sarano M. Cerebral events after diagnosis of mitral valve prolapse. A community-based study of incident and predictive factors. Stroke. 2003;34:1339–1345. doi: 10.1161/01.STR.0000072274.12041.FF. [DOI] [PubMed] [Google Scholar]
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: The Framingham study. Stroke. 1991;22:983–938. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- Hart RG, Halperin JL, Pearce LA, Anderson DC, Kronmal RA, McBride R, Nasco E, Sherman DG, Talbert RL, Marler JR. Stroke Prevention in Atrial Fibrillation Investigators. Ann Intern Med. 2003;138:831–838. doi: 10.7326/0003-4819-138-10-200305200-00011. [DOI] [PubMed] [Google Scholar]
- Sandercock P, Bamford J, Dennis M, Burn J, Slattery J, Jones L, Boonyakarnkul S, Warlow C. Atrial fibrillation and stroke: prevalence in different types of stroke and influence on early and long term prognosis (Oxfordshire community stroke project) BMJ. 1992;305:1460–1465. doi: 10.1136/bmj.305.6867.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, D'Agostino RB. Stroke severity in atrial fibrillation: the Framingham Study. Stroke. 1996;27:1760–1764. doi: 10.1161/01.str.27.10.1760. [DOI] [PubMed] [Google Scholar]
- Steger C, Pratter A, Martinek-Bregel M, Avanzini M, Valentin A, Slany J, Stollberger C. Stroke patients with atrial fibrillation have a worse prognosis than patients without: data from the Australian Stroke registry. Eur Heart J. 2004;25:1734–1740. doi: 10.1016/j.ehj.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Sage JI, Van Uitert RL. Risk of recurrent stroke in patients with atrial fibrillation and non-valvular heart disease. Stroke. 1983;14:537–540. doi: 10.1161/01.str.14.4.537. [DOI] [PubMed] [Google Scholar]
- EAFT (European Atrial Fibrillation Trial) Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischemic attack or minor stroke. Lancet. 1993;342:1255–1262. [PubMed] [Google Scholar]
- Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtytpes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population based study. Stroke. 2001;32:2735–2740. doi: 10.1161/hs1201.100209. [DOI] [PubMed] [Google Scholar]
- García J, Calleja S, de la Vega V, Benavente L, Rodríguez S, Lahoz CH. Adecuación de la profilaxis anticoagulante en pacientes con fibrilación auricular. Rev Neurol. 2005;41(7):399–403. [PubMed] [Google Scholar]
- Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 3. Vol. 24. 1993. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial; pp. 35–41. [DOI] [PubMed] [Google Scholar]
- Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta analyses. Ann Int Med. 1999;131:492–501. doi: 10.7326/0003-4819-131-7-199910050-00003. [DOI] [PubMed] [Google Scholar]
- Atrial Fibrillation Investigators, Atrial fibrillation, Aspirin, Anticoagulation Study, Boston Area Anticoagulation Trial for Atrial Fibrillation Study. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154:1449–1457. doi: 10.1001/archinte.154.13.1449. [DOI] [PubMed] [Google Scholar]
- Hylec EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, Singer DE. Effect of intensity of oral anticoagulation for stroke severity and mortality in atrial fibrillation. N. Engl. J. Med. 2003;349:1019–1026. doi: 10.1056/NEJMoa022913. [DOI] [PubMed] [Google Scholar]
- Investigators AF. The efficacy of aspirin in patients with atrial fibrillation. Analysis of pooled data from 3 randomized trials. Arch. Intern. Med. 1997;157:1237–1240. doi: 10.1001/archinte.157.11.1237. [DOI] [PubMed] [Google Scholar]
- Sato H, Ishikawa K, Kitabatake A, Ogawa S, Maruyama Y, Yokota Y, Fukuyama T, Doi Y, Mochizuki S, Izumi T, Takekoshi N, Yoshida K, Hiramori K, Origasa H, Uchiyama S, Matsumoto M, Yamahuchi T, Hori M. Japan Atrial Fibrillation Stroke Trial Group. Low-dose aspirin for prevention of stroke in low-risk patients with atrial fibrillation. Japan atrial fibrillation stroke trial. Stroke. 2006;37:447–451. doi: 10.1161/01.STR.0000198839.61112.ee. [DOI] [PubMed] [Google Scholar]
- Smith NL, Psaty BM, Furberg CD, White R, Lima JAC, Newman AB, Manolio TA. Temporal trenes in the use of anticoagulants among older adults with atrial fibrillation. Arch Intern Med. 1999;159:1574–1578. doi: 10.1001/archinte.159.14.1574. [DOI] [PubMed] [Google Scholar]
- Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000. pp. 41–46. [DOI] [PubMed]
- Gage BF, Boechler M, Doggette AL, Fortune G, Flaker GC, Rich MW, Radford MJ. Adverse outcomes and predictors of underuse of antithrombotic therapy in medicare beneficiaries with chronic atrial fibrillation. Stroke. 2000;31:822–827. doi: 10.1161/01.str.31.4.822. [DOI] [PubMed] [Google Scholar]
- Hylek EM, D'Antonio J, Evans-Molina C, Shea C, Henault LE, Regan S. Translating the results of randomized trials into clinical practice. The challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke. 2006;37:1075–1080. doi: 10.1161/01.STR.0000209239.71702.ce. [DOI] [PubMed] [Google Scholar]
- Albers GW, Amarenco P, Donald Easton J, Sacco RL, Teal P. Chest. 2008. pp. 630–669. [DOI] [PubMed]
- Gage BF, Birman-Deych E, Kerzner R, Radford MJ, Nilasena DS, Rich MW. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118(6):612–617. doi: 10.1016/j.amjmed.2005.02.022. [DOI] [PubMed] [Google Scholar]
- Lopes RD, Piccini JP, Hylek EM, Granger CB, Alexander JH. Antithrombotic therapy in atrial fibrillation: guidelines translated for the clinician. J Thromb Thrombolysis. 2008;26(3):167–174. doi: 10.1007/s11239-008-0272-4. [DOI] [PubMed] [Google Scholar]
- ACC/AHA/Physician Consortium 2008 Clinical Performance Measures for Adults With Nonvalvular Atrial Fibrillation or Atrial Flutter. A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and the Physician Consortium for Performance Improvement (Writing Committee to Develop Clinical Performance Measures for Atrial Fibrillation) Circulation. 2008;117:1101–1120. doi: 10.1161/CIRCULATIONAHA.107.187192. [DOI] [PubMed] [Google Scholar]
- Gattellari M, Worthington J, Warfarin Zwar N. An Inconvenient Truth. Stroke. 2009;40:5–7. doi: 10.1161/STROKEAHA.108.527903. [DOI] [PubMed] [Google Scholar]
- Indredavik B, Rohweder G, Lydersen S. Frequency and effect of optimal anticoagulation before onset of ischemic stroke in patients with known atrial fibrillation. J Intern Med. 2005;258:133–144. doi: 10.1111/j.1365-2796.2005.01512.x. [DOI] [PubMed] [Google Scholar]
- Fuster V, Ryden LE, Asinger RW, Cannom DS, Crijns HJ, Frye RL, Halperin JL, Kay GN, Klein WW, Levy S. For the American college of cardiology/American heart association/European society of cardiology: Guidelines for the management of patients with atrial fibrillation. J Am Coll Cardiol. 2001;38:1231–1265. doi: 10.1016/S0735-1097(01)01587-X. [DOI] [PubMed] [Google Scholar]
- Singer DE, Albers GW, Dalen JE, Go AS, Halperin JL, Manning WJ. Antithrombotic therapy in atrial fibrillation: The seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126:429S–456S. doi: 10.1378/chest.126.3_suppl.429S. [DOI] [PubMed] [Google Scholar]