Summary
Background
Results of small trials suggest that early interventions for social communication are effective for the treatment of autism in children. We therefore investigated the efficacy of such an intervention in a larger trial.
Methods
Children with core autism (aged 2 years to 4 years and 11 months) were randomly assigned in a one-to-one ratio to a parent-mediated communication-focused (Preschool Autism Communication Trial [PACT]) intervention or treatment as usual at three specialist centres in the UK. Those assigned to PACT were also given treatment as usual. Randomisation was by use of minimisation of probability in the marginal distribution of treatment centre, age (≤42 months or >42 months), and autism severity (Autism Diagnostic Observation Schedule-Generic [ADOS-G] algorithm score 12–17 or 18–24). Primary outcome was severity of autism symptoms (a total score of social communication algorithm items from ADOS-G, higher score indicating greater severity) at 13 months. Complementary secondary outcomes were measures of parent-child interaction, child language, and adaptive functioning in school. Analysis was by intention to treat. This study is registered as an International Standard Randomised Controlled Trial, number ISRCTN58133827.
Results
152 children were recruited. 77 were assigned to PACT (London [n=26], Manchester [n=26], and Newcastle [n=25]); and 75 to treatment as usual (London [n=26], Manchester [n=26], and Newcastle [n=23]). At the 13-month endpoint, the severity of symptoms was reduced by 3·9 points (SD 4·7) on the ADOS-G algorithm in the group assigned to PACT, and 2·9 (3·9) in the group assigned to treatment as usual, representing a between-group effect size of −0·24 (95% CI −0·59 to 0·11), after adjustment for centre, sex, socioeconomic status, age, and verbal and non-verbal abilities. Treatment effect was positive for parental synchronous response to child (1·22, 0·85 to 1·59), child initiations with parent (0·41, 0·08 to 0·74), and for parent-child shared attention (0·33, −0·02 to 0·68). Effects on directly assessed language and adaptive functioning in school were small.
Interpretation
On the basis of our findings, we cannot recommend the addition of the PACT intervention to treatment as usual for the reduction of autism symptoms; however, a clear benefit was noted for parent-child dyadic social communication.
Funding
UK Medical Research Council, and UK Department for Children, Schools and Families.
Introduction
Autism is a severe, highly heritable1 neurodevelopmental disability, with an estimated prevalence of 0·4% for the core disorder and about 1% for the broad autism spectrum.2 Impairments in social reciprocity, communication, and behaviour have a profound effect on children's social development into adulthood3 and result in a high economic cost for families and the community.4 Diagnosis by 3–4 years of age is now common in developed health systems5,6 and the importance of early psychosocial intervention has been advocated in reviews.7,8 Nevertheless, there has been little rigorous assessment of treatment. Provision of training to parents of young children with autism spectrum disorder led to improved child communication and parent-child interaction, but the research design was inadequate in most studies.9,10 A significant treatment effect on the symptoms of autism was noted with the Autism Diagnostic Observation Schedule-Generic (ADOS-G11) algorithm in a randomised controlled pilot trial of 28 children in the UK, which is the basis for the current study.12 ADOS-G is a semistructured, assessor-administered, play-based assessment, videotaped for independent coding, that focuses on the domains of reciprocal social interaction, language and communication, and repetitive and stereotyped behaviours. Positive effects of direct communication interventions between therapist and child on language or interaction outcomes were reported in three randomised controlled studies in the USA (n=58,13,14 n=36,15 and n=4816), although the effect on core autism symptoms was not assessed13–15 or not significant.16 Other positive effects have also been reported in studies of behaviourally focused approaches,8,17 although evidence from the few randomised controlled trials done is equivocal.18 The conclusions derived from all these studies have been limited by sample size and heterogeneity. We therefore aimed to provide a stringent test of a parent-child communication-focused intervention in children aged 2 years to 4 years and 11 months with core autism.
Methods
Study design and participants
The trial was done at a total of three specialist centres in London, Manchester, and Newcastle, UK. Families with a child aged 2 years to 4 years and 11 months, and meeting criteria for core autism according to the international standard diagnostic tests (social and communication domains of the ADOS-G,11 and two of three domains of the Autism Diagnostic Interview Revised [ADI-R] algorithm19) were included in the study.
The test intervention was administered by six specially trained speech and language therapists, and supervised by senior speech and language therapists with expertise in autism (CA, VS, and Sam Barron [North Tyneside Primary Care Trust, North Tyneside, UK]). Interventions were administered on the premises of local primary care trusts (n=12); standard operating procedures for treatment were developed, and adherence was tested at every site during the fidelity procedure. When, for practical reasons, Preschool Autism Communication Trial (PACT) treatment sessions were administered at the family home (71 [7%] of 1087), rather than in the clinic (1016 [93%]), the functional treatment environment for the child was rated against the same standard operating procedures as those in the clinic (webappendix pp 5–6).
We excluded children with a twin with autism; a non-verbal age equivalent to 12 months or younger on the Mullen Early Learning Scales;20 epilepsy requiring medication; severe hearing or visual impairment in a parent or the child; or a parent with a severe psychiatric disorder requiring treatment. At home, participating parents spoke English with their child.
The study was approved by the central Manchester multicentre research ethics committee, and at least one parent provided written consent.
Interventions
The PACT intervention targeted social interactive and communication impairments in autism. The rationale was that children with autism would respond with enhanced communicative and social development to a style of parent communication adapted to their impairments. The intervention consisted of one-to-one clinic sessions between therapist and parent with the child present. The aim of the intervention was first to increase parental sensitivity and responsiveness to child communication and reduce mistimed parental responses by working with the parent and using video-feedback methods to address parent-child interaction. Second, further incremental development of the child's communication was helped by promotion of a range of strategies such as action routines, familiar repetitive language, and pauses. The intervention was manualised and staged to represent the developmental progression of prelinguistic and early language skills (webappendix pp 10–12).
After an initial orientation meeting, families attended biweekly 2 h clinic sessions for 6 months followed by monthly booster sessions for 6 months (total 18). Between sessions, families were also asked to do 30 min of daily home practice. Clinic sessions were videotaped. 44 of these clinic sessions (with 37 participants), selected by stratified randomisation to balance therapist and treatment stage, were double-coded for therapist fidelity against 14 criteria by PH, ALC, JG. Fidelity was shown for a median of 13·4 criteria (IQR 12·5–14·0) per session.
Families in both groups of the trial continued with treatment as usual as provided by their local services. In the experimental group, the PACT intervention was delivered completely separately to treatment as usual.
Randomisation and masking
After consent was obtained and baseline assessments were done, the PACT manager allocated a sequential identification number and provided a statistician at the independent Christie Clinical Trials Unit in Manchester with the child's number, treatment centre, age and autism severity. This statistician ran an allocation schedule that was computer-generated by use of probabilistic minimisation of imbalance in the marginal distribution of treatment centre, age (≤42 months or >42 months), and autism severity (ADOS-G algorithm score 12–17 or 18–24). The statistician then telephoned the treatment allocation to the trial manager, who informed clinical sites. Assessors and supervising research staff were unaware of the treatment allocation; however, treatment allocation could not be masked from families and therapists.
Strict separation was kept between assessment and clinical data; assessors and therapists were located and supervised separately. To avoid the effects of familiarity, materials and location for assessment were different from those for intervention. Endpoint ADOS-G ratings were made from anonymised videotapes by an assessor from a different trial site to the ADOS-G administrator, unaware of the case details and treatment status.
Outcomes
The primary outcome was the ADOS-G social communication algorithm score—a measurement of the severity of the symptoms of autism.11 Algorithm scores are proportional to the severity of symptoms (higher scores indicating greater severity), with cutoff points to classify autism, autism spectrum disorder, and non-spectrum disorder. After pretrial consultation with the scale developer (Lord C, University of Michigan, Ann Arbor, MI, USA, personal communication), the scoring procedure was modified to improve sensitivity to change: scores for children with no spoken words at baseline were adjusted to avoid a systematic rating bias, since children developing words during treatment become liable to increased scores for deviant language. Typically the ADOS-G is modularised by development level (module 1 for children with at most single words, and module 2 for children with phrase speech), but in the trial every child had the same module at both assessment points to avoid discontinuity of scores due to change in module; and we retained the full range of ADOS-G item codes (0–3) and did not recode 3 to 2 as in the standard diagnostic algorithm. Inter-rater reliability was estimated from 66 ratings made from 15 randomly sampled tapes during the trial; intraclass correlation among researchers was 0·79 for the standard social-communication algorithm score, and 0·83 with the described scoring modifications.
There were three secondary outcomes. First was parent-child interaction12 during naturalistic play in a standard (non-therapy) setting. Video ratings, masked to group status, assessment point, and prior hypothesis, were based on three prespecified variables: proportion of parental communications with the child that were synchronous; proportion of child communications with the parent that were initiations; and proportion of time spent in mutual shared attention. Inter-rater reliability between assessors (66 independent ratings made from 22 tapes throughout the study) showed intraclass correlations of 0·80 (parental synchrony), 0·59 (child initiations), and 0·58 (shared attention). Second was child language and social communication: assessed by the researcher using the Preschool Language Scales,21 and reported by the parent according to the MacArthur Communicative Development Inventory (MCDI;22 infant form raw scores) and the Communication and Symbolic Behavior Scales Developmental Profile (CSBS-DP;23 caregiver questionnaire) social composite raw scores. Third was adaptive functioning in school beyond the family: Vineland Adaptive Behavior Scales, Teacher Rating Form,24 rated at endpoint by face-to-face interview with teachers in nurseries, reception class, or other appropriate carer who was not a member of the family.
Statistical analysis
Target recruitment was 144 families, and was powered on the basis of the pilot study effect size for ADOS-G of 0·9212 and allowing for 10% attrition, to provide greater than 99%, 98%, 90%, and 75% power for effect sizes of 0·8 SD (reduction of about 4·0 points), 0·6 SD (reduction of about 3·0 points), 0·5 SD (reduction of about 2·5 points), and 0·4 SD (reduction of about 2·0 points), respectively, with a two-sided p value of 0·05. The clinical relevance of such reductions was modelled with data from 650 concurrent ADOS-G and Vineland Adaptive Behavior Scale assessments in US clinics (Lord C, University of Michigan, personal communication). A 4-point reduction in ADOS-G score was equivalent to a 7-month increase in age-equivalent adaptive functioning for the pilot cohort of children (2 years and 5 months to 5 years).
Analysis was agreed with the data monitoring and ethics committee, and then undertaken in Stata (version 10.1) after completion of endpoint assessments. Primary analysis was by intention to treat and regression ANCOVA, and the fixed-effect covariates were the baseline assessment scores, centre, age group, and baseline background assessments that showed evidence of treatment group imbalance. Multiple imputation, with the iterative-chained-equation method (ice procedure25), was used to complete the small amount of missing data. For convenience, the data for parent-child interaction were imputed separately from the rest of the data. Values were drawn from the regression-predicted posterior distribution for all variables except the parent-rated communication scores and interaction measures when non-normality suggested that prediction matching was preferable. The 500 imputed datasets were analysed jointly by use of the micombine procedure (version 1.1.6)25 that reports the average of the effect estimates from each dataset and applies Rubin's rule26 to allow for imputation uncertainty to be shown in the 95% CIs for effect estimates and the Wald test p values for interactions that we report. Percentages and frequencies reported in the text are based on complete data cases whereas effect estimates and tabulated data are for the whole intention-to-treat sample (following imputation).
Estimates of effect sizes were based on SD of the measure at baseline for both treatment groups combined, except for teacher-rated outcomes that were available only at the endpoint when SD within the group assigned to treatment as usual was used. For responses with distributions less well suited to ordinary regression—eg, showing floor or ceiling effects,27 analyses were repeated with ordinal logistic regression with both endpoint and baseline as quintile categories. We undertook tests for heterogeneity in treatment effect (ie, interaction) for baseline child variables of language level, non-verbal ability, autism severity, and family socioeconomic status (with standard classification of parental occupation). A detailed economic assessment will be reported separately, including ascertainment of family and service costs along with cost-effectiveness of PACT compared with treatment as usual.
This study is registered as an International Standard Randomised Controlled Trial, number ISRCTN58133827.
Role of the funding source
The study design was reviewed and approved by the UK Medical Research Council. Neither funder nor sponsor (University of Manchester) had any involvement with data collection, analysis, write up, or interpretation of the study. Execution of the study was overseen by an independent trial steering committee that approved the trial analysis and its interpretation. The corresponding author and AP had full access to the data. The corresponding author had final responsibility for the decision to submit for publication.
Results
Participants were recruited between September, 2006, and February, 2008; assessment at the 13-month endpoint was done between September, 2007, and March, 2009. Figure 1 shows the trial profile. The study over-recruited participants (final n=152) compared with the target, and attrition to endpoint was low (6 [4%] of 152 for primary endpoint and 101 [7%] of 1520 for all secondary endpoints). All families were telephoned by a senior trial clinician after randomisation to discuss allocation; only one family left the trial because of dissatisfaction with allocation.
Figure 1.
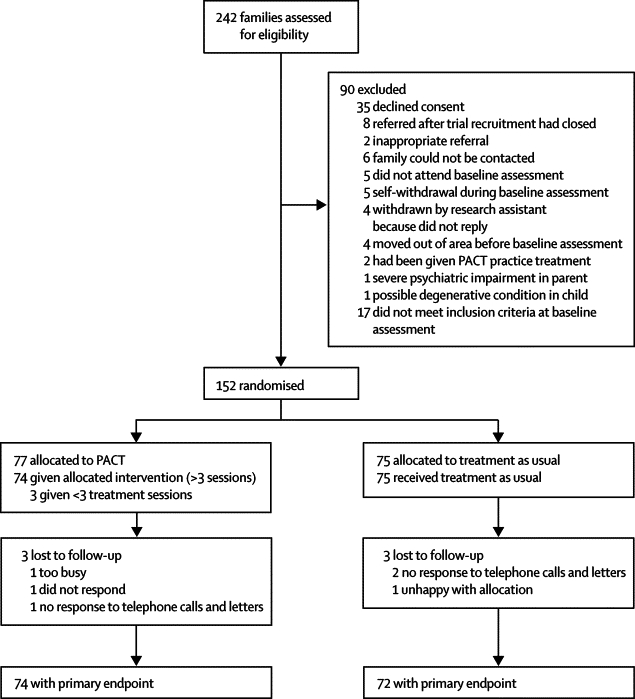
Trial profile
PACT=Preschool Autism Communication Trial.
Table 1 shows that the two treatment groups were well matched for demographic variables except that socioeconomic status and proportion of parents with qualifications gained after age 16 years were higher in the group given PACT than in the group given treatment as usual, particularly in London (Cohen's d index effect size28 for difference between groups was 0·48 for education qualifications and 0·14 for socioeconomic status). Baseline child measures were well balanced across treatment groups and trial sites (table 2). Minimisation factors were balanced for the two treatment groups. Assigned to the PACT group were 50% of children in the London centre, 50% in the Manchester centre, and 52% in the Newcastle centre (table 1); 44 (50%) of 88 children had low ADOS-G severity, and 33 (52%) of 64 had high ADOS-G severity; and 27 (48%) of 56 were aged 24–42 months, and 50 (52%) of 96 were 43–60.
Table 1.
Baseline characteristics of treatment groups by centre
|
London |
Manchester |
Newcastle |
Combined |
||||||
|---|---|---|---|---|---|---|---|---|---|
| PACT (n=26) | TAU (n=26) | PACT (n=26) | TAU (n=26) | PACT (n=25) | TAU (n=23) | PACT (n=77) | TAU (n=75) | ||
| Child age (months; mean, range) | 43 (29–55) | 43 (24–58) | 44 (26–58) | 45 (31–60) | 48 (33–60) | 47 (31–60) | 45 (26–60) | 45 (24–60) | |
| Girl | 2 (8%) | 2 (8%) | 2 (8%) | 4 (15%) | 2 (8%) | 2 (9%) | 6 (8%) | 8 (11%) | |
| Both parents live at home | 17 (65%) | 16 (62%) | 24 (92%) | 21 (81%) | 19 (76%) | 20 (87%) | 60 (78%) | 57 (76%) | |
| Parents' ethnic origin | |||||||||
| Both white | 9 (35%) | 4 (15%) | 16 (62%) | 18 (69%) | 21 (84%) | 19 (83%) | 46 (60%) | 41 (55%) | |
| Mixed* | 1 (4%) | 3 (12%) | 2 (8%) | 3 (12%) | 2 (8%) | 3 (13%) | 5 (6%) | 9 (12%) | |
| Non-white | 16 (62%) | 19 (73%) | 8 (31%) | 5 (19%) | 2 (8%) | 1 (4%) | 26 (34%) | 25 (33%) | |
| Mother's age at baseline (years; mean, range) | 34 (20–41) | 34 (22–47) | 32 (22–45) | 33 (23–46) | 32 (24–41) | 37 (25–48) | 33 (20–45) | 34 (22–48) | |
| Family size (mean, SD) | |||||||||
| Other children | 1·2 (0·3) | 1·2 (0·5) | 0·8 (0·3) | 0·9 (0·3) | 1·0 (0·2) | 1·2 (0·3) | 1·0 (0·3) | 1·1 (0·5) | |
| Adults | 1·7(1·2) | 1·7 (1·3) | 2·0 (1·3) | 1·8 (1·2) | 1·9 (1·2) | 1·9 (1·2) | 1·8 (1·3) | 1·8 (1·3) | |
| Education (one parent with qualifications after age 16 years) | 21 (81%) | 14 (54%) | 23 (88%) | 15 (58%) | 21 (84%) | 18 (78%) | 65 (84%) | 47 (63%) | |
| Socioeconomic status† | 17 (65%) | 9 (35%) | 18 (69%) | 14 (54%) | 16 (64%) | 21 (91%) | 51 (66%) | 44 (59%) | |
Data are number (%), unless otherwise indicated. PACT=Preschool Autism Communication Trial. TAU=treatment as usual.
One white parent and the other non-white.
Dichotomised as at least one parent in professional or administrative occupation versus all others.
Table 2.
Baseline values of Autism Diagnostic Interview Revised (ADI-R) and Autism Diagnostic Observation Schedule-Generic (ADOS-G) for treatment groups by centre
|
London |
Manchester |
Newcastle |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PACT (n=26) | TAU (n=26) | PACT (n=26) | TAU (n=26) | PACT (n=25) | TAU (n=23) | PACT (n=77) | TAU (n=75) | |||
| ADI-R* | ||||||||||
| Reciprocal social interaction | 17·6 (9–24) | 18·7 (8–26) | 18·9 (9–25) | 18·3 (8–26) | 17·0 (9–24) | 17·4 (9–24) | 17·9 (9–25) | 18·2 (8–26) | ||
| Restricted, repetitive, and stereotyped patterns | 6·2 (3–10) | 5·7 (0–10) | 5·2 (2–10) | 6·0 (3–10) | 4·1 (0–7) | 5·0 (2–8) | 5·2 (0–10) | 5·6 (0–10) | ||
| Communication | ||||||||||
| Non-verbal | 10·9 (4–14) | 11·5 (3–14) | 10·7 (3–14) | 10·6 (4–10) | 10·6 (6–14) | 10·8 (7–14) | 10·7 (3–14) | 11·0 (3–14) | ||
| Verbal | n=7 15·7 (9–20) |
n=4 15·2 (10–23) |
n=5 16·6 (10–21) |
n=9 15·6 (10–21) |
n=10 15·3 (12–19) |
n=11 16·0 (12–20) |
n=22 15·7 (9–21) |
n=25 15·7 (10–23) |
||
| ADOS-G† | ||||||||||
| Module 1 (at most single words) | n=21 | n=20 | n=22 | n=20 | n=17 | n=17 | n=60 | n=57 | ||
| Communication | 6·6 (4–8) | 6·7 (5–8) | 6·1 (4–8) | 5·8 (4–8) | 6·2 (4–8) | 5·8 (4–8) | 6·3 (4–8) | 6·1 (4–8) | ||
| Reciprocal social interaction | 11·2 (7–14) | 11·1 (7–14) | 10·8 (7–14) | 10·4 (7–14) | 10·5 (8–14) | 11·0 (8–14) | 10·9 (7–14) | 10·8 (7–14) | ||
| Module 2 (phrase speech) | n=5 | n=6 | n=4 | n=6 | n=8 | n=6 | n=17 | n=18 | ||
| Communication | 7·2 (6–8) | 7·2 (5–9) | 6·0 (5–7) | 6·0 (5–8) | 6·6 (5–9) | 7·0 (6–9) | 6·6 (5–9) | 6·7 (5–9) | ||
| Reciprocal social interaction | 9·2 (7–11) | 10·3 (9–13) | 9·5 (9–10) | 9·8 (7–13) | 8·9 (6–12) | 8·8 (6–14) | 9·1 (6–12) | 9·7 (6–14) | ||
| Module 1 and 2 RRB | 4·3 (1–6) | 4·1 (2–6) | 3·8 (0–6) | 3·7 (1–6) | 2·9 (1–5) | 3·2 (1–6) | 3·7 (0–6) | 3·7 (1–6) | ||
| Mullen non-verbal IQ age equivalent‡ | 25·0 (8·3) | 22·2 (7·6) | 24·8 (9·0) | 25·3 (8·0) | 31·3 (11·7) | 28·8 (11·9) | 27·0 (10·0) | 25·3 (9·5) | ||
Data are mean scores (range) or mean scores (SD). RRB=restricted and repetitive behaviour. IQ=intelligence quotient. PACT=Preschool Autism Communication Trial. TAU=treatment as usual.
Threshold scores are 8 for verbal communication and 7 for non-verbal communication; 10 for social; and 3 for RRBs.
Threshold scores for module 1 are: 4 for communication, 7 for social interaction, and 12 for communication-social total; and for module 2: 5 for communication, 6 for social interaction, and 12 for social-communication total.
Age-equivalents in months; for typically developing children, chronological age and IQ age-equivalents would be similar.
Analysis of the non-PACT treatment received across both groups of the trial during the treatment period showed that the contact time with different professional groups was similar in the two treatment groups—eg, families reported a mean of 9·5 h per case (SD 16·3) of non-PACT speech and language therapy per child in the groups assigned to PACT compared with 9·8 h (12·9) in the group assigned to treatment as usual. Type of intervention for parents (independent of profession) was also similar—eg, group-based autism psychoeducation (PACT: 28 [38%] of 74; treatment as usual: 34 [49%] of 70) and communication-focused interventions (PACT: 27 [36%] of 74; treatment as usual: 23 [33%] of 70). In the group assigned to PACT, one family used Early Intensive Behavioural Intervention and one used Son-Rise therapy; both were intensive home-based interventions. Ten families assigned to PACT and ten assigned to treatment as usual were given Portage (a weekly or fortnightly home-based play and development service). The same professionals might have participated in delivering these provisions in both groups but did not know details about the PACT intervention. All children attended an education or child-care setting for at least some of the trial period, with 30 (41%) of 74 assigned to PACT and 24 (34%) of 70 assigned to treatment as usual attending a setting for special educational needs, and eight (11%) of 74 and ten (14%) of 70, respectively, attended a setting with specific provision for autism spectrum disorder. These settings used a range of general and autism-specific strategies and were not committed to one strategy.
1087 PACT intervention sessions (independent of treatment as usual) were undertaken with 77 families. Adherence to treatment was high: 18 sessions were possible per case in the intervention, median number of sessions per case was 16 (IQR 13–17). The trial therapists shared proportionately the administration of treatment.
Table 3 shows the results of the primary outcome (ADOS-G social communication modified algorithm total) at the 13-month endpoint, and details of individual ADOS-G modified-domain totals. Treatment effect with ANCOVA estimates was −1·06 (95% CI −2·48 to 0·36) without baseline covariate adjustment; −1·00 (−2·38 to 0·39) with adjustment for centre and age group; and −1·00 (−2·45 to 0·46) with adjustment for the child's sex, verbal ability (Preschool Language Scales expressive raw score), non-verbal ability (Mullen mean non-verbal age-equivalent), and parental educational qualifications and socioeconomic status (that showed some lack of balance in table 1). This last adjusted estimate corresponded to an effect size of −0·24 (−0·59 to 0·11). The pre-planned tests of interactions with treatment were not significant for centre (p=0·52), non-verbal ability of more than 24 months (p=0·47), language level (Preschool Language Scale expressive raw score >12; p=0·51), severity of baseline symptoms of autism (ADOS-G algorithm >17; p=0·85); age group (>42 months; p=0·46), and socioeconomic status (p=0·10).
Table 3.
Baseline, 13-month endpoint and change in the Autism Diagnostic Observation Schedule-Generic (ADOS-G) social-communication modified algorithm total primary outcome and individual domains
|
London |
Manchester |
Newcastle |
Total |
|||||
|---|---|---|---|---|---|---|---|---|
| PACT (n=26) | TAU (n=26) | PACT (n=26) | TAU (n=26) | PACT (n=25) | TAU (n=23) | PACT (n=77) | TAU (n=75) | |
| Total social-communication algorithm score | ||||||||
| Baseline | 20·9 (3·8) | 21·0 (3·5) | 19·3 (4·4) | 18·1 (3·8) | 18·5 (4·1) | 18·7 (4·0) | 19·6 (4·2) | 19·3 (4·0) |
| Endpoint | 18·0 (5·8) | 20·1 (4·0) | 15·0 (5·8) | 13·8 (5·6) | 13·9 (5·3) | 15·4 (5·1) | 15·7 (6·0) | 16·5 (5·7) |
| Change | −2·9 (4·6) | −1·0 (3·5) | −4·3 (5·3) | −4·2 (4·0) | −4·6 (3·7) | −3·4 (3·5) | −3·9 (4·7) | −2·9 (3·9) |
| Social domain | ||||||||
| Baseline | 11·0 (2·1) | 11·1 (2·0) | 10·8 (2·3) | 10·4 (2·0) | 10·3 (2·1) | 10·7 (2·4) | 10·7 (2·2) | 10·7 (2·1) |
| Endpoint | 10·4 (2·9) | 11·7 (1·7) | 8·7 (2·7) | 8·3 (2·9) | 8·4 (3·0) | 9·5 (2·7) | 9·2 (3·0) | 9·8 (2·9) |
| Change | −0·6 (2·8) | 0·5 (2·0) | −2·1 (2·8) | −2·1 (2·4) | −1·9 (2·4) | −1·2 (2·4) | −1·5 (2·8) | −0·9 (2·5) |
| Communication domain | ||||||||
| Baseline | 9·9 (2·1) | 9·9 (2·1) | 8·5 (2·4) | 7·7 (2·4) | 8·2 (2·5) | 8·1 (2·3) | 8·9 (2·5) | 8·6 (2·5) |
| Endpoint | 7·6 (3·3) | 8·4 (2·7) | 6·3 (3·4) | 5·6 (3·2) | 5·6 (2·9) | 5·9 (3·1) | 6·6 (3·3) | 6·7 (3·2) |
| Change | −2·2 (2·3) | −1·5 (2·1) | −2·2 (3·1) | −2·1 (2·4) | −2·6 (2·2) | −2·2 (2·3) | −2·3 (2·6) | −1·9 (2·4) |
| Repetitive behaviours domain | ||||||||
| Baseline | 4·3 (1·3) | 4·1 (1·3) | 3·8 (1·5) | 3·8 (1·4) | 2·9 (1·2) | 3·3 (1·5) | 3·7 (1·5) | 3·7 (1·4) |
| Endpoint | 3·1 (1·4) | 3·9 (1·4) | 3·3 (1·9) | 3·3 (1·6) | 2·6 (1·8) | 3·4 (1·7) | 3·0 (1·7) | 3·5 (1·6) |
| Change | −1·2 (1·8) | 3·9 (1·4) | −0·5 (2·2) | −0·5 (1·8) | −0·2 (1·4) | 0·1 (1·4) | −0·7 (1·9) | −0·2 (1·6) |
Data are mean scores (SD). Missing data were multiply imputed for three endpoint ADOS-G assessments per treatment as usual (TAU) and Preschool Autism Communication Trial (PACT). To increase sensitivity to change, the standard item recodings were revised: all three scores were retained as equal to 3. For some items the nine codes were recoded; module 1: a01 (8=3), a03 (8=2), a04 (8=3), a05 (8=3), a06 (8=2), and b03 (8=2); module 2: a01 (7=3), a02 (7=2), and a03 (8=2). In ADOS-G, higher scores equate to greater severity of symptoms.
At endpoint, most children were still classified as having an ADOS-G diagnosis of core autism. In the group assigned to PACT, 22 (30%) of 74 had changed to autism spectrum disorder and four (5%) of 74 to non-spectrum; in the group assigned to treatment as usual, 17 (24%) of 72 changed to autism spectrum disorder and five (7%) of 72 to non-spectrum. After adjustment for initial ADOS-G category, age group, and centre, ordinal logistic regression resulted in a non-significant treatment effect (proportional odds ratio 1·15, 95% CI 0·56 to 2·35).
Table 4 shows results of the assessor-rated secondary outcomes. Treatment effect sizes, estimated with ANCOVA, of the Preschool Language Scales raw scores (since many children did not achieve the standard score norms), after adjustment for centre, age group, sex, non-verbal ability, socioeconomic status, and parental education, were small: 0·07 (95% CI −1·95 to 2·08) for receptive scores and −0·35 (−1·85 to 1·16) for expressive scores. Estimates of effect size for tests of parent-child interaction were larger. Use of ANCOVA to control for centre, age group, sex, verbal ability, non-verbal ability, socioeconomic status, and parental education resulted in estimates of 1·22 (0·85 to 1·59) for parental synchrony, 0·41 (0·08 to 0·74) for child initiations, and 0·33 (−0·02 to 0·68) for shared attention. When analysed as ordered quintiles, the corresponding estimates of odds ratios from proportional odds ordinal logistic regression were 9·10 (4·39 to 18·86), 2·32 (1·21 to 4·42), and 1·90 (1·01 to 3·60), respectively. For treatment by centre interactions, p value was 0·005 for parental synchrony, 0·06 for child initiations, and 0·56 for parent-child shared attention; centre differences were consistent across these three assessments with smallest treatment differences noted in Manchester.
Table 4.
Secondary blind rated baseline and 13-month endpoint measurements: Preschool Language Scales and video-rated parent-child interaction
|
London |
Manchester |
Newcastle |
Total |
|||||
|---|---|---|---|---|---|---|---|---|
| PACT (n=26) | TAU (n=26) | PACT (n=26) | TAU (n=26) | PACT (n=25) | TAU (n=23) | PACT (n=77) | TAU (n=75) | |
| Preschool Language Scales: receptive raw scores* | ||||||||
| Baseline | 13·0 (6·7) | 11·8 (7·0) | 15·2 (11·1) | 15·5 (9·6) | 18·6 (10·3) | 18·2 (11·1) | 15·6 (9·8) | 15·0 (9·7) |
| Endpoint | 17·4 (11·1) | 15·7 (10·1) | 19·9 (12·7) | 21·0 (10·8) | 27·5 (13·1) | 24·8 (15·4) | 21·5 (13·0) | 20·3 (12·8) |
| Change | 4·4 (7·7) | 3·9 (4·8) | 4·7 (4·4) | 5·5 (4·4) | 8·9 (6·8) | 6·6 (7·9) | 6·0 (6·7) | 5·3 (5·9) |
| Preschool Language Scales: expressive raw scores* | ||||||||
| Baseline | 12·5 (5·1) | 12·5 (5·8) | 15·9 (11·0) | 16·2 (7·2) | 16·5 (6·5) | 16·9 (9·7) | 15·0 (8·1) | 15·1 (7·9) |
| Endpoint | 15·2 (7·8) | 14·7 (7·1) | 20·3 (11·8) | 21·7 (9·7) | 24·9 (11·3) | 23·9 (14·2) | 20·0 (11·2) | 20·0 (11·3) |
| Change | 2·6 (3·9) | 2·3 (3·4) | 4·4 (4·4) | 5·6 (4·1) | 8·4 (6·5) | 7·0 (6·7) | 5·1 (5·6) | 4·9 (5·2) |
| Parent-child interaction: parental synchrony† | ||||||||
| Baseline | 28·5% (13·2) | 25·7% (12·8) | 32·9% (17·0) | 31·8% (13·8) | 34·2% (13·3) | 36·9% (15·1) | 31·8% (14·8) | 31·3% (14·6) |
| Endpoint | 58·4% (19·1) | 29·3% (15·6) | 40·4% (15·9) | 33·0% (12·3) | 55·4% (18·9) | 35·7% (12·8) | 51·3% (19·6) | 32·6% (14·0) |
| Change | 29·8% (18·7) | 3·6% (15·2) | 7·5% (20·4) | 1·2% (15·8) | 21·2% (19·1) | −1·2% (14·2) | 19·5% (21·3) | 1·4% (15·3) |
| Parent-child interaction: child initiations† | ||||||||
| Baseline | 22·7% (20·6) | 20·4% (16·0) | 22·8% (16·6) | 26·3% (17·3) | 23·5% (14·4) | 26·7% (21·4) | 23·0% (17·4) | 24·4% (18·5) |
| Endpoint | 33·6% (19·3) | 20·4% (19·6) | 31·1% (17·1) | 32·7% (13·9) | 40·1% (21·5) | 24·6% (16·1) | 34·9% (19·7) | 26·0% (17·5) |
| Change | 10·9% (20·6) | 0 (20·6) | 8·3% (22·9) | 6·5% (17·6) | 16·7% (22·0) | −2·1% (25·0) | 11·9% (25·6) | 1·6% (21·4) |
| Parent-child interaction: shared attention time† | ||||||||
| Baseline | 56·5% (24·1) | 54·7% (19·0) | 70·3% (19·9) | 74·1% (20·6) | 69·3% (19·0) | 72·9% (20·3) | 65·3% (22·0) | 67·0% (21·9) |
| Endpoint | 60·9% (26·3) | 47·4% (26·4) | 61·2% (25·0) | 61·8% (23·8) | 69·9% (24·6) | 57·8% (24·7) | 64·0% (25·7) | 55·6% (25·7) |
| Change | 4·3% (23·2) | −7·3% (30·3) | −9·0% (25·0) | −12·3% (24·6) | 0·6% (20·5) | −15·1% (29·4) | −1·4% (23·7) | −11·4% (28·4) |
Data are mean (SD) or percentage (SD).
Raw scores for Pre-school Language Scales are used because many children fell below the range of normed scores for their age; missing data were multiply imputed for one participant assigned to Preschool Autism Communication Trial (PACT) at baseline, and for three participants assigned to treatment as usual (TAU) and three assigned PACT at endpoint.
Missing data were multiply imputed for one participant assigned to PACT at baseline, and for five assigned to TAU and three to PACT at endpoint.
Table 5 shows the results of the outcome assessments that were rated by the parent and teacher. Parent ratings showed substantial differences by treatment group in favour of PACT. ANCOVA estimates of treatment effects, with adjustment for centre, age group, sex, verbal ability, non-verbal ability, socioeconomic status, and education qualifications were 2·28 (95% CI 0·17 to 4·39) for the CSBS-DP social composite scores, 30·28 (6·90 to 53·68) for the MCDI receptive scores, and 21·37 (−6·42 to 49·16) for the MCDI expressive scores. When analysed as ordered quintiles, the corresponding estimates of odds ratio from the proportional odds ordinal logistic regression were 2·49 (1·27 to 4·89), 3·40 (1·48 to 7·79), and 1·63 (0·76 to 3·51), respectively. No differences were noted with the teacher Vineland Communication and Adaptive Behavior Composite standard scores, with differences of −3·52 (−7·55 to 0·52) and −2·76 (−6·65 to 1·14), respectively.
Table 5.
Secondary baseline and 13-month endpoint measurements
|
Baseline |
Outcome |
Change |
|||||
|---|---|---|---|---|---|---|---|
| PACT (n=77) | TAU (n=75) | PACT (n=77) | TAU (n=75) | PACT (n=77) | TAU (n=75) | ||
| Parent CSBS-DP raw score* | 29·5 (7·1) | 28·3 (8·8) | 34·0 (8·2) | 30·8 (8·3) | 4·6 (7·0) | 2·5 (6·0) | |
| Parent MCDI* | |||||||
| Receptive raw score | 159·5 (114·4) | 162·0 (122·4) | 233·7 (129·6) | 209·0 (131·3) | 74·2 (66·9) | 47·0 (68·2) | |
| Expressive raw score | 93·5 (114·8) | 111·1 (128·6) | 171·9 (150·7) | 163·8 (144·3) | 78·5 (89·3) | 51·8 (73·2) | |
| Teacher Vineland† | |||||||
| Communication | .. | .. | 64·3 (17·7) | 67·7 (17·5) | .. | .. | |
| Adaptive behaviour composite | .. | .. | 60·3 (15·2) | 62·8 (14·8) | .. | .. | |
CSBS-DP=Communication and Symbolic Behavior Scales Developmental Profile (caregiver questionnaire) social composite score. MCDI=MacArthur Communicative Development Inventory.
Missing data were multiply imputed at baseline for one participant assigned to treatment as usual (TAU), and at endpoint for six assigned to TAU and eight assigned to Preschool Autism Communication Trial (PACT).
Unavailable at baseline because participants were generally too young; standard scores normed to population mean=100 and SD=15.
Discussion
The endpoint scores for symptoms of autism improved in both groups, with only a small estimated group difference in favour of the PACT intervention. Effect of the intervention on ADOS-G score in relation to diagnostic thresholds was small. There was no effect of child age, baseline autism severity, non-verbal ability, or socioeconomic status on intervention effect. There was no group difference in standardised assessor-rated measures of child language. However, parent ratings of language and social communication showed a strong effect in favour of the PACT intervention.
Intervention effects were strong for assessor-rated parent-child interactions (parent synchronous responses and child communication initiations, although less for shared attention). These represent the targeted proximal outcomes of the parent-training approach, and their presence has been associated with positive benefits for later social and communication functioning in independent prospective studies in children with autism.29,30 A positive intervention effect on parental synchrony was also noted in our pilot randomised controlled trial,12 in which it was associated with an endpoint improvement in autism symptoms. In the current study, however, we did not note an equivalent downstream effect on autism symptoms. Instead, a progressive attenuation of treatment effect was noted (figure 2) as assessment changed from parent behaviour with the child, to child behaviour with the parent, and then to child behaviour in a different setting with the ADOS administrator; and, in more generalised settings, with the nursery teacher as assessor.
Figure 2.
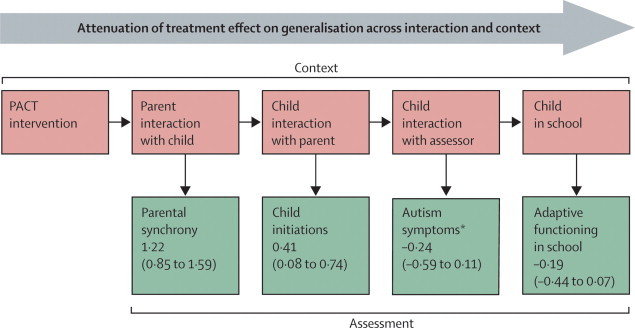
Context and assessment of Preschool Autism Communication Trial (PACT) intervention
Data are effect size (95% CI). *Negative value indicates lower abnormality in PACT group.
These findings suggest that the optimistic results from other studies should be reassessed. Several methodological factors should be considered. Large trial sizes generally produce small effects,31 and our trial was rigorously done with particular attention to methods of masking assessment, especially for our primary outcome. Importantly, we prespecified the primary and secondary outcomes to be analysed, whereas post-hoc analysis of several measured outcomes, a strategy subject to type 1 errors, was generally used in previous intervention studies. We only studied children with core autism rather than the range of the autism spectrum that was often included in previous trials.15,16 Although there was no evidence of a moderating effect of initial autism severity within this core range, we cannot generalise about the possible effect on children with broad autism spectrum disorder. Treatment as usual was balanced across the groups. The positive results reported in other autism trials have not been in autism symptomatology (although endpoint language was used in two),14,16 rather their positive endpoints have been the proximal aspects of dyadic interaction on which we too noted differential improvement.13,15,16 In a trial of a moderately intensive (16 h per week for 2 years) therapist delivered social communication intervention that included parent-training, benefits were reported, particularly in language, but not changes to ADOS-G severity score.16 We also noted positive effects for parent-reported assessments that, although not masked, benefited from parental knowledge of the child's communicative behaviour in a range of contexts. Our primary test for evidence of specific treatment effect on downstream symptoms of autism, with measurement that was distal to the intervention in terms of setting, materials, and participants, is particularly challenging since children with autism have difficulty in generalising across contexts. However, we argue this is the most valid objective test of intervention efficacy in this context.
We used ADOS-G as the primary outcome because it had external validity in relation to symptoms of autism, and because of its effect size in the pilot study. However, ADOS-G might lack sensitivity as a measure of change, since its initial validation focused on the establishment of cutoff points for diagnostic purposes. An important challenge will be the development of sensitive but still valid objective tests for measurement of change.7 In this context, we undertook a non-planned exploratory analysis that included all ADOS-G symptom items rather than those just related to the diagnostic algorithm. The results suggested only a small improvement in sensitivity in relation to treatment effect. The unexpected improvement in restricted and repetitive behaviours supports theoretical links between communicative competency and restricted and repetitive behaviours,32 and might suggest a benefit of reporting a range of targeted outcomes within endpoint ADOS-G ratings for communication interventions in the future.
The intensity and duration of our intervention was based on a pilot study and potential feasibility within the UK National Health Service; PACT was administered for more hours than were similar interventions in other studies.13,15 It was also parent-mediated (targeted in the first instance at altering parental responses to the child), unlike direct therapist-child interventions in other studies. Parent-mediated interventions might be particularly efficacious in improving parents' perceptions and sensitivity to their child's communication needs; and parent-reported outcomes in this trial were positive. In theory, the effect on parental behaviour will generalise to benefit the child's family environment and could generate cumulative effects in the child's development; however, longer follow-up would be needed to test this possibility.
On the basis of our findings, we cannot recommend the addition of this PACT intervention to treatment as usual for the purpose of reduction in autism symptoms. The intervention does however significantly alter parent-child dyadic social communication in ways that are associated with subsequent positive child outcomes in longitudinal studies of autism,29,30 and are likely to be also positive for parents themselves. Techniques to aid transmission of these gains in parent-child interaction to adaptive functioning in wider contexts need to be assessed. These might include naturalistic reinforcement of behaviour at home, increased periods of booster and generalisation intervention or adjunctive multimodal reinforcement in other settings. Although there might be a limitation to the effect of such environmental enrichment on reducing core autism impairments, further trials that build on the current approach and long-term follow-up studies are needed to define the limitation.
Acknowledgments
Acknowledgments
This study was sponsored by the University of Manchester. PACT was funded by the Medical Research Council (G0401546), the UK Department for Children, Schools and Families; with a UK Department of Health award for excess treatment and support costs. We gratefully thank all families participating in the study and the referring professionals. We acknowledge invaluable support and guidance from our trial steering committee (Eric Taylor, Alan Emond, Francis Creed, Richard Mills, and Tina McClelland), and our data monitoring and ethics committee (Patrick Bolton, Paula Williamson, and Brian Neville). Other support for trial design and management was provided by Barbara Farrell, and Richard Mills. We are grateful for the support and collaboration of the UK National Autistic Society throughout the trial. The study was adopted by the UK Mental Health Research Network, who provided valuable officer support for clinical studies.
Contributors
JG, TC, HM, AP, CA, VS, PH, ALC, SB, and WM designed the trial. KL, KH, SB, KT, and BB contributed to data gathering. AP was the trial statistician and analysed the data. JG led the writing of the report. All authors contributed to data interpretation and drafting the report, and have seen and approved the final version.
PACT Consortium
UK Lydia White, Clare Holt, Dharmi Kapadia, Katy Bourne, Laura Blazey (University of Manchester, Manchester); Tori Houghton, Carol Taylor (Stockport Primary Care Trust, Stockport); Anna Cutress, Sue Leach (Newcastle University, Newcastle); Sam Barron, Ruth Colmer, Sarah Randles (North Tyneside Primary Care Trust, North Tyneside); Karen Beggs (Southwark Primary Care Trust, Southwark); Julia Collino (Lewisham Primary Care Trust, Lewisham).
Conflicts of interest
We declare we have no conflicts of interest.
Web Extra Material
References
- 1.Bailey A, Le Couteur A, Gottesman I. Autism as a strongly genetic disorder: evidence from a British twin study. Psychol Med. 1995;25:63–77. doi: 10.1017/s0033291700028099. [DOI] [PubMed] [Google Scholar]
- 2.Baird G, Simonoff E, Pickles A. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006;368:210–215. doi: 10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- 3.Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry. 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 4.Knapp M, Romeo R, Beecham J. Economic cost of autism in the UK. Autism. 2009;13:317–336. doi: 10.1177/1362361309104246. [DOI] [PubMed] [Google Scholar]
- 5.Le Couteur A, Baird G, Mills R. The National Autism Plan for Children (NAPC) National Autistic Society; London: 2003. [Google Scholar]
- 6.Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. JAMA. 2001;285:3141–3142. doi: 10.1001/jama.285.24.3093. [DOI] [PubMed] [Google Scholar]
- 7.Lord C, Wagner A, Rogers S. Challenges of evaluating psychosocial interventions for autistic spectrum disorders. J Autism Dev Disord. 2005;35:695–708. doi: 10.1007/s10803-005-0017-6. [DOI] [PubMed] [Google Scholar]
- 8.Rogers SJ, Vismara LA. Evidence-based comprehensive treatments for early autism. J Clin Child Psychol. 2008;37:8–38. doi: 10.1080/15374410701817808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diggle T, McConachie HR, Randle VRL. Parent mediated early intervention for young children with autistic spectrum disorder (Cochrane review) John Wiley and Sons; Chichester: 2003. [DOI] [PubMed] [Google Scholar]
- 10.McConachie H, Diggle T. Parent implemented early intervention for young children with autism spectrum disorder: a systematic review. J Eval Clin Pract. 2007;13:120–129. doi: 10.1111/j.1365-2753.2006.00674.x. [DOI] [PubMed] [Google Scholar]
- 11.Lord C, Risi S, Lambrecht L, Cook EH., Jr The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. [PubMed] [Google Scholar]
- 12.Aldred C, Green J, Adams C. A new social communication intervention for children with autism: a pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry. 2004;45:1420–1430. doi: 10.1111/j.1469-7610.2004.00848.x. [DOI] [PubMed] [Google Scholar]
- 13.Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: a randomized controlled intervention study. J Child Psychol Psychiatry. 2006;47:611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- 14.Kasari C, Paparella T, Freeman S, Jahromi L. Language outcome in autism: randomized comparison of joint attention and play interventions. J Consult Clin Psychol. 2008;76:125–137. doi: 10.1037/0022-006X.76.1.125. [DOI] [PubMed] [Google Scholar]
- 15.Yoder P, Stone WL. Randomized comparison of two communication interventions for preschoolers with autism spectrum disorders. J Consult Clin Psychol. 2006;74:426–435. doi: 10.1037/0022-006X.74.3.426. [DOI] [PubMed] [Google Scholar]
- 16.Dawson G, Rogers S, Munson J. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125:17–23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howlin P, Magiati I, Charman T. A systematic review of early intensive behavioural interventions (EIBI) for children with autism. Am J Intellect Dev Disabil. 2009;114:23–41. doi: 10.1352/2009.114:23;nd41. [DOI] [PubMed] [Google Scholar]
- 18.Spreckley M, Boyd R. Efficacy of Applied Behavioral Intervention in preschool children with autism for improving cognitive, language, and adaptive behavior: a systematic review and meta-analysis. J Pediatr. 2009;154:338–344. doi: 10.1016/j.jpeds.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive development disorders. J Autism Dev Disord. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 20.Mullen EM. Mullen Scales of Early Learning. American Guidance Service; Circle Pines, MN: 1995. [Google Scholar]
- 21.Zimmer IL, Steiner VG, Pond RE. The Preschool Language Scales. British Psychological Corporation; London: 1992. [Google Scholar]
- 22.Fenson L, Dale P, Reznick S. The MacArthur communicative development inventories: user's guide and technical manual. Singular Publishing Group; San Diego, CA: 1993. [Google Scholar]
- 23.Wetherby AM, Prizant BM. Communication and Symbolic Behaviour Scales Developmental Profile. Paul H Brookes Publishing; Baltimore, MD: 2002. [Google Scholar]
- 24.Sparrow SS, Cicchetti DV, Balla DA. Vineland adaptive behavior scales: second edition, Teacher Rating Form. Pearson Assessments; Livonia, MN: 2006. [Google Scholar]
- 25.Royston P. Multiple imputation of missing values. Stata J. 2004;4:227–241. [Google Scholar]
- 26.Rubin DB. Multiple imputation for nonresponse in surveys. Wiley; New York: 1987. [Google Scholar]
- 27.Taylor A, Pickering K, Lord C, Pickles A. Mixed and multilevel models for longitudinal data: growth curve analysis of language development. In: Everitt B, Dunn G, editors. Recent advances in the statistical analysis of medical data. Arnold; London: 1998. pp. 127–144. [Google Scholar]
- 28.Cohen DJ. Statistical power analysis for the behavioural sciences. Academic Press; New York: 1977. [Google Scholar]
- 29.Siller M, Sigman M. The behaviors of parents of children with autism predict the subsequent development of their children's communication. J Autism Dev Disord. 2002;32:77–89. doi: 10.1023/a:1014884404276. [DOI] [PubMed] [Google Scholar]
- 30.Siller M, Sigman M. Modeling longitudinal change in the language abilities of children with autism: parent behaviors and child characteristics as predictors of change. Dev Psychol. 2008;44:1691–1704. doi: 10.1037/a0013771. [DOI] [PubMed] [Google Scholar]
- 31.McMahon B, Holly L, Harrington R, Roberts C, Green J. Do larger studies find smaller effects? The example of studies for the prevention of conduct disorder. Eur Child Adolesc Psychiatry. 2008;17:432–437. doi: 10.1007/s00787-008-0685-9. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein H. Communication intervention for children with autism: a review of treatment efficacy. J Autism Dev Disord. 2002;32:373–396. doi: 10.1023/a:1020589821992. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


