Abstract
Background
A partogram is a universal tool for monitoring labour. It is used for labour management in Rujumbura HSD, Rukungiri District. However, the District Health Officer reported only 30% use of a partogram. The study intended to find out why the low use, and suggest strategies in scaling up.
Objectives
To establish extent of use of a partogram, health facility and health workers' factors that affected its use during labour plus the relationship between foetal Apgar score and its use.
Materials and Methods
A cross-sectional study involving observations, record reviews and interviewing of staff in 8 health facilities (4 Public and 4 Private Not For Profit) in Rujumbura HSD in Rukungiri district was conducted from May 23rd to 27th June 2008. It employed both qualitative and quantitative methods of data collection.
Results
The partogram was used in 69.9% of deliveries. The partographs that fulfilled the standard monitoring of foetal heart rate were only 2%. There were few trained health workers and lack of guidelines on partogram use. A good Apgar score was associated with standard foetal monitoring and was statistically significant (P < 0.001).
Conclusions and recommendations
There was poor use of partograms during labour mainly affected by health input factors. We recommended training of health workers on partogram use, provision of guidelines and adequate resources.
Introduction
A partogram is one of the valuable appropriate technologies in use for improved monitoring of labour progress, maternal and foetal wellbeing. It is an important tool for managing labour. This is through enabling clinicians (midwives and doctors) to plot examination findings from their assessments on the partogram. The belief that its use was applicable in developed and developing settings led to its introduction worldwide1,2. A number of common partogram designs incorporate an alert and action line3. The development of the partogram provided health professionals with a pictorial overview of labour progress, maternal and foetal condition to allowearly identification and diagnosis of pathological labour. Its use is critical in preventing maternal and perinatal morbidity and mortality.
The World Health Organization (WHO) recommends partograms with a 4-hour action line from alert line, denoting the timing of intervention for prolonged labor; others recommend earlier intervention to allow for referral4,5. This tool is now widely used across African Countries including Uganda to monitor labour progress, foetal and maternal wellbeing. The core issue is to prevent obstructed labour through early detectionof abnormal progress of labour, and appropriate clinical responses rendered in accessible, equipped and staffed health units2. Appropriate use of a partogram requires adequate number of skilled health workers5,6 with a positive attitude towards its use especially midwives at various levels of health care facilities and actual availability of the partogram tools at all times.
Rukungiri district health facilities' teams use a partogram to monitor labour progress and conditions of the mother and foetus. However, the District Health Officer reported that the proportion of the health units in which it was actively used was so low at a third of health units and of uncertain quality. The reasons for this state were not known to the District Health Team (DHT). The use of a partogram for intrapartum monitoring was expected to be fully carried out at HC III, IV and Hospitals.
On the other hand, human resource for health database in the district indicated the Doctor: population ratio of 1:18,513; Clinical Officer: population ratio of 1:13,464; Nurse: population ratio of 1:895; Midwife: child bearing women ratio of 1:987. The population's outpatient services utilization rate is at 1.46/person/year with only 45% mothers delivering at health units. The Infant Mortality Rate and estimated Maternal Mortality Ratio (MMR) are high estimated at 76/1,000 live births and 475/100,000 live births with life expectancy in the district at 50 years7.
Despite these facts and that there was good knowledge on the availability of partograms in the health units, the actual level of use and quality was not known and documented in Rukungiri District and yet the DHT recognizes it as an important tool for improved labour management. In addition to that there was a reported high MMR in Rukungiri District as stated above compared to national average of 435/100,000 live births for Uganda8. The District Health Officer (DHO) reported that many maternal deaths actually occurred at the hospitals. The extent and quality of use of a partogram in the management of labour was a major concern to him and his team. The DHO reported the partogram use to be very low at the various maternity units at HC III, IV and hospitals.
The estimated proportion of health units in which the partogram was used in the district to monitor labour was at 30%9. The District Health Team (DHT) thought this was due to poor attitude of health workers, lack of confidence and skills in its use. However, in order to improve on its use at least one midwife had been trained in each facility on the use of a partogram. It was expected that trained midwives would practice and subsequently build the capacity of their colleagues on the use of a partogram. The DHT member reported that copies of partograms were availed to all the maternity units in the Health Units on regular basis. Inspite of these, the use of a partogram remained low and reasons were unclear to the District Health Officer (DHO). The DHO was convinced that quality in the management of labour would not be improved without effective use of a partogram.
Materials and methods
Study site and population: The study was conducted in Rujumbura Health Sub District (HSD) in Rukungiri District which is in the South Western part of Uganda. The District borders with the districts of Bushenyi in the North, Ntungamo in the East, Kabale in the South and Kanungu in the West. It is about 400 km from Kampala the capital city of Uganda. The district has a total area of 1524.6 square kilometers with a population projected from 2002 to be 300,80010. There are two counties, 11 sub counties including the town council, 77 parishes and 825 villages. Rukungiri District has physically established: 2 Hospitals, 2 Health Centre IVs and at least one Health Centre III in all the 11 Subcounties (16 in total) and 42 HC II7. The Health Centre IIIs, HC IVs and Hospitals by design should utilize a partogram.
Rujumbura HSD is one of the four HSDs in Rukungiri District. It is the Central HSD in the district that includes Rukungiri Town Council in her catchment. It borders Bushenyi in the north, Kebisoni HSD in the East, Rubabo HSD in the South and Bugangari HSD in the West. It has 7 sub counties, 7 HC III and 1 Hospital. The study reference population comprised of all partographs in all health units in Rukungiri District. The study population comprised of the partographs at Nyakibale Hospital and HC IIIs in Rujumbura HSD. These included both public and private not for profit health facilities.
The district has two nurse/midwifery training schools located in the two hospitals. The trainees and working midwives were reported to be familiar with the partogram by District Health Team (DHT).
Inclusion and Exclusion criteria
All partographs with adequate information from the HC IIIs and the Hospital in Rujumbura HSD that were in establishment at least three years preceding the study and in which respondents provided informed consent were included in the study. Partographs in the HC III and Hospital facilities that were in establishment at least three years preceding the study but had part of the record misplaced/missing (inadequate) were excluded.
Study design
This was a cross sectional study involving review of records and interviewing of staff in health units. It involved review of partograph records and interviewing staff in the public and private not for health facilities in Rujumbura HSD in Rukungiri district. It employed both qualitative and quantitative methods of data collection. The study was carried out between 23rd May – 27th June 2008.
Sample size
The sample size was all the partographs used for monitoring labour, foetal and maternal wellbeing that were available and had adequate information at the 8 health facilities during the six randomly selected months. We used this to establish level and quality of use of partographs during labour. The factors that affected use of a partogram were assessed through key informant interviews. The sample size was 1170 partographs from eight sampled health facilities that were got from six randomly selected months (Aug 07, Oct 07, Nov 07, Jan 08, Feb 08 and Mar 08) out of 12 months (period Jun 1st 2007 to May 31st 2008) in Rujumbura Health Sub District. We interviewed 8 in-charges of health units and 8 midwives in-charge of maternity departments, 1 in-charge of the HSD, 1 Medical Officer in-charge of maternity, 1 Senior Nursing Officer at the hospital as Key Informants.
Sampling procedure
Health Units
The health facilities were clustered into a hospital and HC III. The hospital was included in the study based on its role in maternal health care services; it supervised HC III and other lower service providers in the catchment area. Seven HC IIIs out of 7 in the HSD were all included for the study. They included four from government and three for Private Not For Profit (PNFP) units. The lists of all the HC III units were obtained from the DHO.
Key Informants
Staff in-charge of the health units and departments were purposively included in the study.
Partographs
Six months were randomly selected from 12 months for the period 1st Jun 2007 to 31st May 2008. This was done by writing all the 12 months on a square piece of paper, mixing them in a bowel and then selecting six of them by simple random sampling method (none replacement). The six selected included: Aug 07, Oct 07, Nov 07, Jan 08, Feb 08 and Mar 08. All the 1170 partograms used during labour for these six months and had adequate information were included in the study and reviewed.
Study variables
Dependent variables
The dependent variable was use of partograms during labour.
Independent variables
The independent variables for this study included: availability of partograms and protocols on use of a partogram in the health units, number of partograms filled (full/not), number of partograms filled to standard, training of midwives in partogram use, workload at the health unit, number of midwives at the health unit and perceptions of health workers on the use of a partogram
Data collection
Data collection was undertaken from the hospital and HC III units in Rujumbura HSD. Partographs constituted study units. We also interviewed staff in-charge of HSD, health units and maternity departments (midwives and doctor) after obtaining informed consent from each of them. A total of 8 health facilities were visited.
Checked in labour ward delivery book for the number of deliveries. Then looked for the files. Reviewed the files for use of partographs. Checked for the completeness of partographs. In the complete filling of the partographs, we checked for cervical dilatation, uterine contractions, foetal heart rate, action line crossed/not, pulse and blood pressure, descend of foetal head, state of membranes.
The standards11 that were adapted for this study were: cervical dilation monitored at least once every four hours; foetal heart rate, blood pressure and maternal temperature monitored on hourly basis; were judged to be substandard, or not recorded if no information is documented on the partogram/ completely absent from the file and standard if the criteria are met. The condition of the baby should have been recorded in the appropriate section of the delivery to include the Apgar score (7 was considered good in this study12). We also noted the actual deliveries in each of the health units.
Key informant interviews were conducted with eight health unit in-charges, eight heads of departments, one in-charge of HSD, one Senior Nursing Officer and one Medical Officer in-charge maternity department. All interviews were conducted by the first author using a guide agreed upon by all the investigators. All interviews were carried out at the in-charges' and heads of departments' work places in private. Key informant interviews were carried out to capture the experiences of the health workers that engaged directly with filling the partogram or ensuring that the partogram is filled. Some of the guiding questions included; how many midwives/nurses provide delivery services at this unit? Do you have partograms in this health unit? Are partograms used during labour at this unit? If yes, explain how you use a partogram at this health unit? Have you had an in-service training on the use of a partogram? (with probing for duration and nature) What is your personal opinion on the use of a partogram during labour? (with probing for reasons if not in use) What recommendations would you give on the use of the partogram for monitoring labour? The key informant interviews took between 30 and 40 minutes.
Training of research assistant
One research assistant who eventually worked alongside the Principal Investigator (PI) was trained for two days by the PI to ensure quality data collection.
Pre-testing
The data collection tools were pre-tested at health units that had not been sampled for the study.
Field editing of data
Data were checked before leaving the field for correctness and completeness (normality) daily.
Data Management and Analysis
Data management
Quantitative data were captured using EPI INFO statistical software package version 3.3.2 of 2005. Prior to analysis, data cleaning, coding, checking for normality and transformation plus data entry was done. Qualitative data were entered into a master sheet.
Data analysis
Quantitative data were analysed using EPI INFO statistical package version 3.3.2 of 2005. Basic statistics were generated. The risk ratios and P-values computed from the StatCal on the utilities menu of the Epi Info so as to determine risk for apgar score <7 for substandard monitoring of parameters on the partographs (cervical dilatation, action line crossed yes/no, foetal heart rate and uterine contractions).
Ethical considerations
The collection of data at the health facilities followed approval by DHO. Informed consent was received from all the key informants after explaining the purpose of the study. The respondents were reassured on confidentiality on responses during and after the study. There were no invasive procedures involved.
Study limitations
The study could not assess biochemical aspects on the partographs like testing for urine sugars as this were expected to have been rarely performed due to non-availability of required supplies in all the units (not a common practice in the HSD, District and Country). The missing files and data from the partograph records were other limitations. In order to minimize bias at interview,key informant interviews were conducted by the first author himself. The research assistant worked under close supervision of the first author to ensure adherence to correct data collection procedures so as to miminize any possible errors.
Results
Use of the partogram
We conducted record reviews of 1170 partographs out of estimated 1674 partographs (representing the total actual deliveries during the period) that had been used for labour management during the period of this study and were accessible to the study team. This was only 69.9% of the total 1674 expected partographs
The table 1 shows the findings on labour parameters following the partographs review at the eight health facilities.
Table 1.
Numbers of partograms with records of parameters of labour progress at Health units in Rujumbura HSD
| Parameters of labour |
Nyakibale Hospital (n = 1290) |
Rukungiri (n= 51) |
Ruhinda (n= 95) |
Buhunga (n = 47) |
North Kigezi (n = 74) |
Nyakagyeme (n = 41) |
Kibirizi (n = 39) |
Rusheshe (n = 37) |
Total (n =1674) |
|
Cervical dilatation |
|||||||||
| Not recorded |
347 | 51 | 91 | 29 | 66 | 41 | 39 | 37 | 701 |
| Substandard | 213 | 0 | 3 | 16 | 6 | 0 | 0 | 0 | 238 |
| Monitored to Standard |
730 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 735 |
| Action line crossed | |||||||||
| Yes | 11 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 13 |
| No | 932 | 0 | 3 | 18 | 7 | 0 | 0 | 0 | 960 |
| Uterine contractions | |||||||||
| Not recorded | 560 | 51 | 91 | 29 | 66 | 41 | 39 | 37 | 914 |
| Substandard | 341 | 0 | 3 | 15 | 5 | 0 | 0 | 0 | 364 |
| Recorded to standard |
389 | 0 | 1 | 3 | 3 | 0 | 0 | 0 | 396 |
From table 1 we noted that there were 1674 deliveries across all the health units but only 735 of the cervical dilation and 396 uterine contractions were plotted on the partograms to recommended standard. Action line crossed were in 13 partographs. Nyakagyeme, Kibirizi and Rusheshe and Rukungiri HC III facilities were found not to have used a partogram on any mother as shown.
We then looked into maternal blood pressure monitoring. The findings are as in table 2 below.
Table 2.
Numbers of partograms with records of parameter of maternal condition in Rujumbura HSD Health units
| Parameters of labour |
Nyakibale Hospital (n = 1290) |
Rukungiri (n= 51) |
Ruhinda (n= 95) |
Buhunga (n = 47) |
North Kigezi (n = 74) |
Nyakagyeme (n = 41) |
Kibirizi (n = 39) |
Rusheshe (n = 37) |
Total (n =1674) |
| Blood pressure | |||||||||
| Not recorded | 448 | 51 | 91 | 29 | 66 | 41 | 39 | 37 | 802 |
| Substandard | 678 | 0 | 4 | 18 | 8 | 0 | 0 | 0 | 708 |
| Monitored to standard |
164 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 164 |
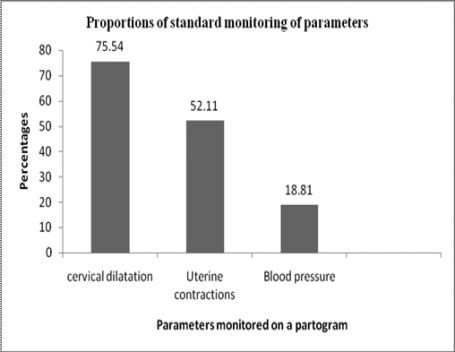
The table 2 indicates that 52.1% (872/1674) deliveries during the period of study had their blood pressure monitored. Ten percent were monitored to standard. Nyakibale hospital was the one health unit that monitored blood pressure to the recommended standard. Overall the figure 1 below shows the proportion of standard monitoring of parameters.
From the figure 1, we noted that cervical dilatation was better monitored at 75.5%. The least standard monitored parameter was 18.8% for blood pressure.
Quality of partographs used and Agpar score values
We tested for relationship between foetal Apgar score and quality of monitoring of foetal heart rate, cervical dilatation, uterine contractions and whether action line was crossed or not. The interest was to generate a relationship between foetal Apgar Score and quality of monitoring specific parameters that are usually plotted on the partogram. The table 3 below shows the findings.
Table 3.
Relationship between foetal Apgar Score and the quality of monitoring the parameters during labour at Nyakibale hospital and HC III units selected for this study
| Births with Apgar score <7/N |
% of births with Apgar score < 7 |
RR | 95% CI | |
|
Parameter monitored Foetal heart rate |
||||
| Substandard | 29/426 | 6.8 | 3.5 | (1.84, 6.46)* |
| Standard | 14/744 | 1.9 | 1 | |
| Cervical dilatation | ||||
| Substandard | 35/238 | 14.7 | 4.2 | (2.54, 7.02)* |
| Standard | 23/735 | 3.1 | 1 | |
| Action line crossed | ||||
| Yes | 05/13 | 38.5 | 1.6 | (0.76, 3.44) |
| No | 199/960 | 20.7 | 1 | |
| Uterine contractions | ||||
| Substandard | 33/364 | 9.1 | 1.7 | (0.97, 2.80) |
| Standard | 21/396 | 5.3 |
Note *statistically significant at 95% CI, P < 0.05
From table 3 we noted that substandard monitoring of foetal heart rate and cervical dilatation had over three and four times risk of getting baby with Apgar score less than seven respectively.
Key Informants - Interviews: Health facility factors
We interviewed the two categories of Key Informants on availability and pattern of use of partogram. We noted that the partograms were available at health units but actual use was a problem. This is illustrated in the following quotations from the eight in-charges:
“We have copies of partograms in our health units but sometimes one midwife on duty providing antenatal care services, health education delivery services, family planning, treatment makes her not be able to really sit and plot the partogram”.
On the other hand two of the in-charges added that:
“The use of a partogram leads to increase in caesarean sections especially among prime gravid mothers. Sometimes we plot a second partograph on the same patient till it crosses action line on the second one then we take action”.
We found out that some health centre III had no copies of a partogram. This is demonstrated in the quotation that:
“We do not have even copies of the partograms and where can one find them? Since I came to work in this health unit I have never seen one. Again the problem with such tools is the need to photocopy. It would be good if the District Health Team photocopies for us because we have no money at the health units most of the time”.
It was also noted that 6 out of 10 Heads of departments reported having no guidelines on partogram use. Even though the majority of the in-charges, 7/10 felt it was a useful tool in detecting abnormal labour progress so as to take action, the lack of guidelines was highlighted. This was illustrated by the following quote:
“We do not have any guidelines on the use of a partogram. Infact even the partogram we have here is an old one compared to the one we had recently been using at school. I am new in this unit but I can only see old unused partograms without any guidelines and I would not be comfortable using this old type! The District Health Team should get for us the revised copies of the partograms”.
Health worker factors
We interviewed the Heads of department on whether they had had training on how to use a partogram as a skill building in-service training. We found that 8/10 had never, as illustrated by the quote:
“We have never had training of any kind in the last one year especially on partogram use”. The in-charges have been the ones benefiting from the recent workshops and a few of us on Prevention of mother to child transmission training”.
On the other hand, on average there are two midwives per HC III and only 7 at the hospital. All the three interviewees from the hospital expressed to be experiencing heavy workload saying:
“There is a lot of work here and yet you can be one midwife at night managing the labour ward, postnatal ward and seven other wards. In such a situation when an emergency gets in, you can be forced to abandon the client at hand to rescue the other. Sometimes one even ends up not continuing with plotting of a partogram as it should be”.
We explored then the Key Informant perceptions on the use of a partogram. Seven out of 9 in-charges were positive on the use of the partogram. This can be illustrated in the following quote:
“It is good to use it because complications can be diagnosed early and enables to make a decision on next step to manage the mother. It is simple and good exercise helps to detect dangers in the baby and mother. We also use it for handing over mothers in labour when going out off duty for the next midwife to know where each mother has reached.
However, on the interview with Heads of maternity departments we noted negative perceptions. Six of the Heads on department expressed their concerns on the use of a partogram saying:
“A Partogram is too detailed, yet one midwife on duty at a time makes it very difficult to plot it to the standard. This is because she has to conduct many activities like Family Planning,Antenatal Care, Maternity care service and others. It would therefore be important to sensitize mothers to come early. However, it is good to use since it safe guards the mother and health worker in case of any problem”.
Key Informants - Socio-demographic characteristics In-charges of Health Units
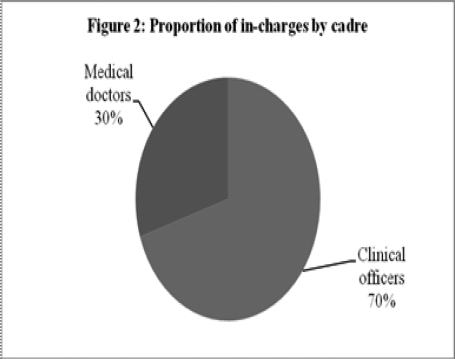
There were 9 in-charges (7 Clinical Officers and 2 Medical doctors) whom we interviewed as Key Informants. The Clinical Officers are all in-charge of the Heath Centre III facilities, 1 Medical doctor is In-charge of Nyakibale hospital and the other is in-charge of Rujumbura Health Sub District.
Figure 2 indicates that majority (70%) of the in-charges were Clinical Officers. There were 3 females and 6 males. The mean age of the in-charges was 29 years (SD = 3.30) and range of 25 – 35 years.
Figure 2.
Proportion of in-charges by cadre, n = 9
Heads of maternity departments
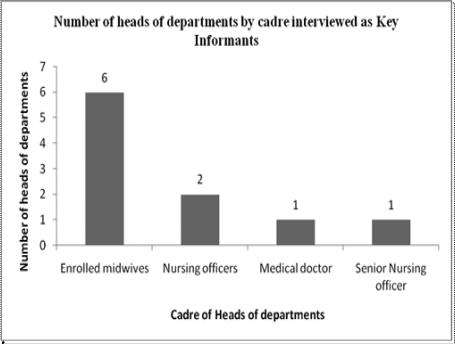
There were 10 heads of maternity departments whom we interviewed as also Key Informants.
The figure 3 shows their distribution by cadre.
Figure 3.
Heads of Departments interviewed as Key Informants
Figure 3 shows that most of the heads of maternity departments were Enrolled midwives. The six Enrolled midwives were all in-charges of maternity sections in the HC III facilities, 1 Nursing Officer heads midwifery department at a HC III and the other in-charge of the Nyakibale hospital maternity unit. The Senior Nursing oversees all nursing services at Nyakibale hospital (Midwifery and Nursing). The Medical doctor is the officer assigned to be in-charge of maternity unit at Nyakibale hospital.
There were 9 females and 1 male among heads of departments. The mean age for the Heads of departments was 26.6 years (SD = 4.58) with a range of 22 – 38 years.
Discussion
All the health units had partograms available. The study has shown that most 57.1% (4/7) of the health workers at health centre III facilities never used partograms to monitor any mother in labour. Even in other facilities where partograms were used the partograms were not used according to the recommended standard. Only 2% was used according to the standard for monitoring foetal heart rate. This was similar to the findings in a Benin study15. The high frequency of recording of cervical dilatation in this study compared to other parameters such as uterine contractions and foetal heart rate was similar to the findings elsewhere12. In the latter there was low uterine contractions recording compared to what we have found in this study in Rukungiri District. This is due to the good supervision by the Medical Officer In-charge, Senior Nursing Officer and Midwifery Tutors who closely supervise the practice to enhance learning of midwifery trainees.
The study indicated that there was poor monitoring of parameters on the partogram against standards. There was statistical significance between foetal outcomes and quality of monitoring foetal heart rate, RR = 3.5 (P < 0.0001) and cervical dilatation, RR = 4.2 (P < 0.0001). The findings of the foetal heart rate are in agreement with the findings in the Dar es Salaam study12. However, this study revealed that there was statistical significance between cervical dilatation monitoring and foetal outcome. This confirms that a partogram when used to monitor labour progress determines the foetal outcome. It is particularly striking to note that the partogram is better used at Nyakibale hospital compared to all the health centre III. This is due to better and available technical supervision at the hospital compared to the health centres.
From this study we found that most health units had partograms but were never used. A few never had them and their health workers could not even tell where to access them. This could be due to gaps in the health system support function or gaps in the health workers knowledge as they don't know their use and where to order for them. All the health units never had guidelines/protocols on the use of the partograms. This was similar to the findings of the study at the hospitals in Dar es Salaam12. This does not only demotivate the users but can affect the quality of partogram use during labour. The study further revealed that most of the midwives had never been trained on the use of a partogram in the last one year. All the midwives mentioned in this study had formal education and training while at school; however, they required in-service training tailored to the need to develop a critical mass of those who can have confidence in monitoring parameters on the partogram to the standard15.
The study has further revealed that majority of health unit teams never had skills on the use of a partogram as only two parameters were monitored by over 50%. Yet for a partogram to be useful all parameters should be measured and information used for monitoring maternal and foetal wellbeing. This underpins the critical importance of having skilled health workers to deliver a health service that has been reiterated elsewhere6, 14. It has been demonstrated that other cadres of health care workers when trained on partogram use contribute to desired and acceptable practice6. On the other hand, the health workers perceived the partogram to be useful in helping them to detect abnormal labour. However, a few health workers were of the opinion that the partogram was a detailed tool that was not practical to use where there is one midwife in the unit as she has to execute other duties like administering treatment, managing labour, giving health education, offering family planning services among others. In the Dar es Salaam study, the latter perception of health workers in this study seems to correlate with its findings12. The seemingly contradictory views of the key informants in this study were similar to what was found elsewhere15.
Conclusion and recommendations
This study showed a poor use of the partograms during labour. Use of partograms during labour is affected by input factors like lack of guidelines, training health workers on its use and actual availability of the tools in all health facilities and health workers having a positive attitude on the use of a partogram. Training of health workers on partogram use, provision of guidelines and adequate resources is recommended.
Acknowledgements
Rukungiri District Health Office for logistical support. The Health workers at the health units in Rujumbura HSD and the Research Assistants. The Makerere University School of Public Health, Dr. Elizabeth Nabiwemba for technical support and Mr. Halage for field work support.
References
- 1.Lennox CE, Kwast BE. The partograph in community obstetrics. Tropical Doctor. 1995;25:56–63. doi: 10.1177/004947559502500204. [DOI] [PubMed] [Google Scholar]
- 2.Friedman EA. Graphic analysis of labor. American Journal of Obstetrician Gynecology. 1954;68:1568–1575. doi: 10.1016/0002-9378(54)90311-7. [DOI] [PubMed] [Google Scholar]
- 3.Philpott RH, Castle WM. Cervicographs in the management of labour in primigravidae. II. The action line and treatment of abnormal labour. Journal of Obstetrics Gynaecology British Commonwealth. 1972;79:599–602. doi: 10.1111/j.1471-0528.1972.tb14208.x. [DOI] [PubMed] [Google Scholar]
- 4.Starrs A. Improve access to good quality maternal health services: the safe motherhood action agenda: priorities for the next decade. Colombo: 1997. pp. 29–50. [Google Scholar]
- 5.Mercer W Stewart, Sevar Katherine, Sadutshan D Tsetan. Using clinical audit to improve the quality of obstetric care at the Tibetan Delek Hospital in North India: a longitudinal study. Reproductive Health. 2006;3(4):3. doi: 10.1186/1742-4755-3-4. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fatusi O A, Makinde N O, Adeyemi B A, Orji O E, Onwudiegwu U. Evaluation of health workers' training in use of the partogram. International Journal of Gynecology and Obstetrics. 2007:3. doi: 10.1016/j.ijgo.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Rukungiri District Local Government, author. District Health Statistical Abstract. 2007. [Google Scholar]
- 8.Uganda Bureau of Statistics, author. Uganda Demographic and Health Survey. 2006. [Google Scholar]
- 9.Rukungiri District Local Government, author. District Health Officer report. 2008. [Google Scholar]
- 10.Rukungiri District Local Government, author. District Health Sector Strategic Plan, 2005/06 - 2009/2010. 2005. [Google Scholar]
- 11.World Health Organization, author. Safe Motherhood Needs Assessment version 1.1, Maternal and Newborn Health/Safe Motherhood. Geneva: Division of Reproductive Health, Family and Reproductive Health; 2001. [Google Scholar]
- 12.Nyamtema AS, Urassa D P, Massawe S, Massawe A, Lindmark G, Van Roosmalen J. Partogram use in the Dar es Salaam perinatal care study. International Journal of Gynaecolgy and Obstetrics. 2008;100:37–40. doi: 10.1016/j.ijgo.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 13.Lavender T, Wallymahmed A, Walkinshaw S. Managing labor using partograms with different actions lines: a prospective study of women's views. Birth. 1999;26:89–96. doi: 10.1046/j.1523-536x.1999.00089.x. [DOI] [PubMed] [Google Scholar]
- 14.Steven Harvey A, Blandön Yudy Carla Wong, McCaw-Binns Affette, Sandino Ivette, Urbina Luis, Rodríguez César, Gómez Ivonne, Ayabaca Patricio, Djibrinaf Sabou, Nicaraguan maternal and neonatal health quality improvement group Are skilled birth attendants really skilled? A measurement method, some disturbing results and a potential way forward. Bulletin of the World Health Organization. 2007;85:783–790. doi: 10.2471/BLT.06.038455. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azandegbe N, Testa J, Makoutode M. Assessment of partogram utilisation in Benin [article in French] Sante. 2004;14:251–255. [PubMed] [Google Scholar]