Abstract
BACKGROUND
The Norwood procedure with a modified Blalock–Taussig (MBT) shunt, the first palliative stage for single-ventricle lesions with systemic outflow obstruction, is associated with high mortality. The right ventricle–pulmonary artery (RVPA) shunt may improve coronary flow but requires a ventriculotomy. We compared the two shunts in infants with hypoplastic heart syndrome or related anomalies.
METHODS
Infants undergoing the Norwood procedure were randomly assigned to the MBT shunt (275 infants) or the RVPA shunt (274 infants) at 15 North American centers. The primary outcome was death or cardiac transplantation 12 months after randomization. Secondary outcomes included unintended cardiovascular interventions and right ventricular size and function at 14 months and transplantation-free survival until the last subject reached 14 months of age.
RESULTS
Transplantation-free survival 12 months after randomization was higher with the RVPA shunt than with the MBT shunt (74% vs. 64%, P = 0.01). However, the RVPA shunt group had more unintended interventions (P = 0.003) and complications (P = 0.002). Right ventricular size and function at the age of 14 months and the rate of nonfatal serious adverse events at the age of 12 months were similar in the two groups. Data collected over a mean (±SD) follow-up period of 32±11 months showed a nonsignificant difference in transplantation-free survival between the two groups (P = 0.06). On nonproportional-hazards analysis, the size of the treatment effect differed before and after 12 months (P = 0.02).
CONCLUSIONS
In children undergoing the Norwood procedure, transplantation-free survival at 12 months was better with the RVPA shunt than with the MBT shunt. After 12 months, available data showed no significant difference in transplantation-free survival between the two groups. (ClinicalTrials.gov number, NCT00115934.)
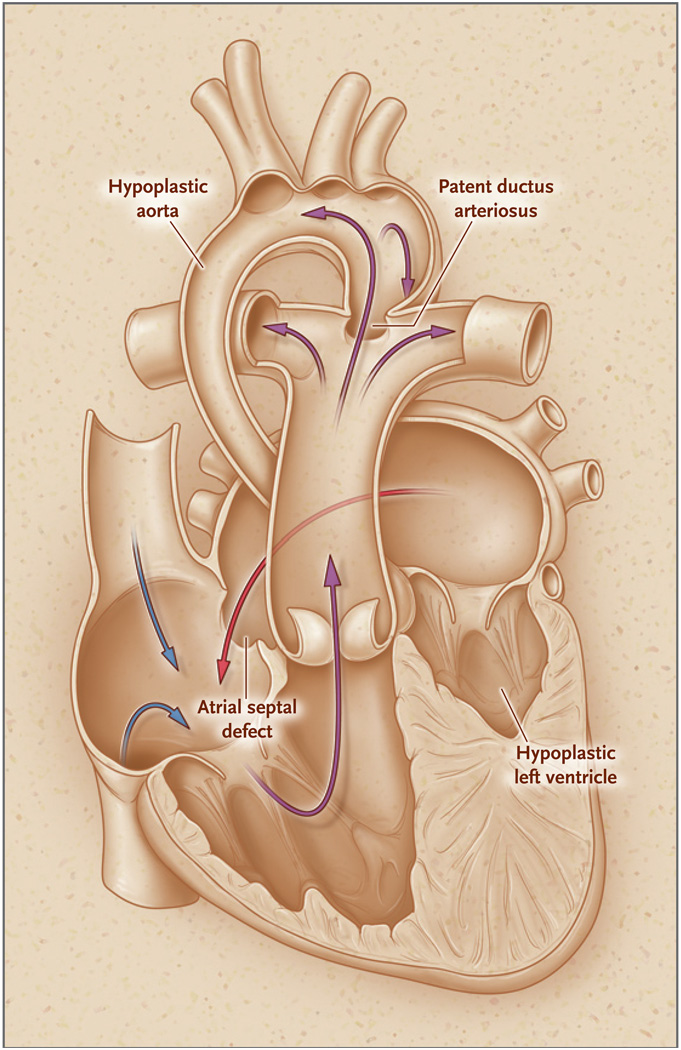
Hypoplastic left heart syndrome and related anomalies involving a single right ventricle are characterized by hypoplasia of the left heart and the aorta, with compromised systemic cardiac output (Fig. 1). Infants with the syndrome generally undergo a three-stage reconstruction culminating in the Fontan procedure. The first operation (stage I) is the Norwood procedure, in which the right ventricle is connected to a reconstructed aorta with the use of the proximal main pulmonary artery for systemic outflow. Pulmonary blood flow is reestablished by means of a shunt from the pulmonary artery to the systemic circulation. In the second operation (stage II), which is generally performed at 3 to 6 months of age, the shunt is removed and pulmonary blood flow is supplied by an anastomosis between the superior vena cava and the pulmonary artery. The Fontan procedure (stage III) is generally undertaken when the child is 18 to 48 months of age. In this operation, blood flow through the inferior vena cava is directed to the pulmonary artery, thus separating the pulmonary and systemic circulations.
Figure 1. Hypoplastic Left Heart Syndrome.
The hypoplastic left heart syndrome and related disorders involving the single right ventricle are characterized by a total admixture lesion. As in the normal heart, deoxygenated blood returns to the right atrium. Oxygenated blood returning from the left atrium crosses an atrial septal defect to join the deoxygenated blood in the right atrium. This mixed blood is then ejected by the right ventricle into the pulmonary artery. A portion of the blood in the pulmonary artery proceeds as normal to the lungs, as well as to the aorta through a patent ductus arteriosus, to supply the systemic circulation.
Mortality associated with the Norwood procedure remains the highest among common congenital heart procedures, ranging from 7 to 19%.1–6 An analysis of resource utilization for the 35 most common structural birth defects showed that the Norwood procedure is associated with the highest cost and the third longest length of stay.7 Between discharge after hospitalization for the Norwood procedure and the stage II procedure, 4 to 15% of infants die.8–10
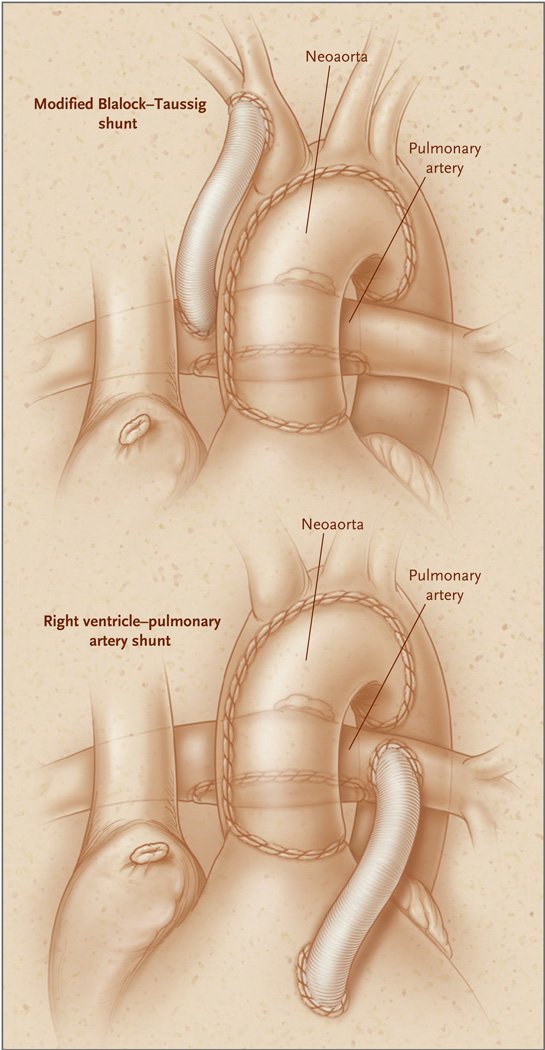
In the classic Norwood procedure, pulmonary blood flow is supplied by a modified Blalock–Taussig (MBT) shunt, a tube graft connecting the subclavian or innominate artery to the pulmonary artery (Fig. 2). The MBT shunt provides continuous forward flow of blood into the pulmonary artery during both systole and diastole, causing diastolic retrograde flow in the descending aorta and coronary arteries.11 Because coronary blood flow occurs primarily during diastole, “coronary steal” may cause myocardial ischemia and circulatory instability, which in turn may lead to death in the hospital or during the period between the Norwood procedure and stage II.9,12–14
Figure 2. The Norwood Procedure with a Modified Blalock – Taussig Shunt and a Right Ventricle – Pulmonary Artery Shunt.
In the completed Norwood procedure, one can see the reconstructed aorta (neoaorta) and the isolated pulmonary artery. Pulmonary blood flow is supplied by either a modified Blalock–Taussig shunt (top) or a right ventricle–pulmonary artery shunt (bottom).
Alternatively, a right ventricle–pulmonary artery (RVPA) shunt can be placed to provide pulmonary blood flow.15 A theoretical advantage of the RVPA shunt is the elimination of diastolic runoff, reducing the potential for coronary steal, which may thus lead to a lower perioperative and interstage mortality.4–6,11,16,17 Potential disadvantages include a negative effect on right ventricular function, arrhythmias or aneurysm formation related to the ventriculotomy, additional volume load due to regurgitation from the nonvalved RVPA shunt, impaired growth of the pulmonary artery, and the need for an earlier stage II procedure.17–20 To date, outcomes with the MBT shunt and those with the RVPA shunt have been compared only in small, nonrandomized case series, with limited follow-up and conflicting results.1–6,18 The Pediatric Heart Network21 conducted a randomized trial at 15 North American centers involving infants with hypoplastic left heart syndrome or related single right ventricular anomalies who were undergoing the Norwood procedure. (For a list of the investigators and participating institutions, see the Supplementary Appendix, available with the full text of this article at NEJM.org.)
METHODS
STUDY PATIENTS
Details of the trial design have been published previously.22 In brief, inclusion criteria consisted of a diagnosis of hypoplastic left heart syndrome or a related single, morphologic right ventricular anomaly and a planned Norwood procedure. Exclusion criteria were the preoperative identification of cardiac anatomy that would render either the MBT shunt or the RVPA shunt technically impossible and any major congenital or acquired extracardiac abnormality that could independently affect the likelihood of transplantation-free survival (the primary outcome).
STUDY DESIGN AND OUTCOMES
Infants were randomly assigned to either the MBT shunt or the RVPA shunt within strata according to the presence or absence of aortic atresia and obstructed pulmonary venous return, with dynamic allocation by the surgeon.23 The primary outcome was the rate of death or cardiac transplantation 12 months after randomization. Secondary outcomes included morbidity during the Norwood and stage II hospitalizations; the incidence of unintended cardiovascular interventions involving the shunt, pulmonary arteries, or neoaorta by 12 months; right ventricular function, right ventricular volume, and the degree of tricuspid-valve regurgitation at discharge after the Norwood procedure, before stage II, and at the age of 14 months on the basis of echocardiograms interpreted by the core laboratory; and the core laboratory interpretation of pulmonary-artery size by angiography before stage II. The right ventricular volumes and ejection fractions were calculated with the use of the biplane pyramidal method.24
Safety during the first 12 months after randomization was monitored with the use of three measurements: the rate of composite serious adverse events (death, acute shunt failure, cardiac arrest, extracorporeal membrane oxygenation, unplanned cardiovascular reoperation, or necrotizing enterocolitis), the rate of composite serious adverse events with death excluded, and the rate of other complications. The prespecified subgroups for analysis were as follows: birth weight (<2500 or ≥2500 g), preoperative tricuspid-valve regurgitation (proximal jet width, <2.5 or ≥2.5 mm), deep hypothermic circulatory arrest versus regional cerebral perfusion, the surgeon’s annual experience in performing Norwood procedures in infants randomly assigned to this procedure (<6, 6 to 10, 11 to 15, or >15 procedures), and the annual volume of Norwood procedures at each center (<11, 11 to 25, 26 to 40, or >40 procedures). The protocol was approved by each center’s institutional review board, and written informed consent was obtained from a parent or guardian.
STATISTICAL ANALYSIS
The intention-to-treat principle was applied to all primary analyses. Five infants were excluded from all analyses because they did not undergo a Norwood procedure. Fisher’s exact test was used to compare the rates of death or transplantation 12 months after randomization. The rate of crossover from the assigned shunt was higher than expected; therefore, the target sample size was increased from 466 infants to 554 in December 2007 to avoid potential dilution of the treatment effect. The critical P value for rejection of the null hypothesis was 0.044 because four interim analyses were performed. The stopping boundary was crossed at the fourth interim analysis (at the data and safety monitoring board meeting in October 2008) (observed P value, 0.012 [below the nominal P value for rejection, 0.018]; group difference, 10.4%); however, since enrollment had already been completed, the trial was not halted.
Overall transplantation-free survival was compared in the two shunt groups with the use of log-rank and Gehan–Wilcoxon tests. Nonproportional hazards were assessed by means of a treatment-by-time interaction test (<12 or ≥12 months) in a Cox regression model that included all available follow-up data. Total duration of ventilator use and length of hospital and intensive care unit stays were compared by means of the Wilcoxon rank-sum test. Length of hospital stay was also compared with the use of the log-rank test. Student’s t-test or the Wilcoxon rank-sum test was performed to compare echocardiographic variables in the two shunt groups, depending on the degree of skewness. Adverse-event rates were compared with the use of a Poisson regression model, and the proportions of infants with an adverse event were compared by means of Fisher’s exact test. Interactions between shunt type and the prespecified subgroup and stratification factors were evaluated. Two secondary analyses were performed for all end points: an analysis according to the actual shunt received at the end of the Norwood procedure, and an analysis that excluded two infants who were randomly assigned to a shunt group and were subsequently found to be ineligible because of cardiac anatomy. The results of the second analysis were similar to those of the primary analysis and are therefore not reported.
RESULTS
CHARACTERISTICS OF THE PATIENTS
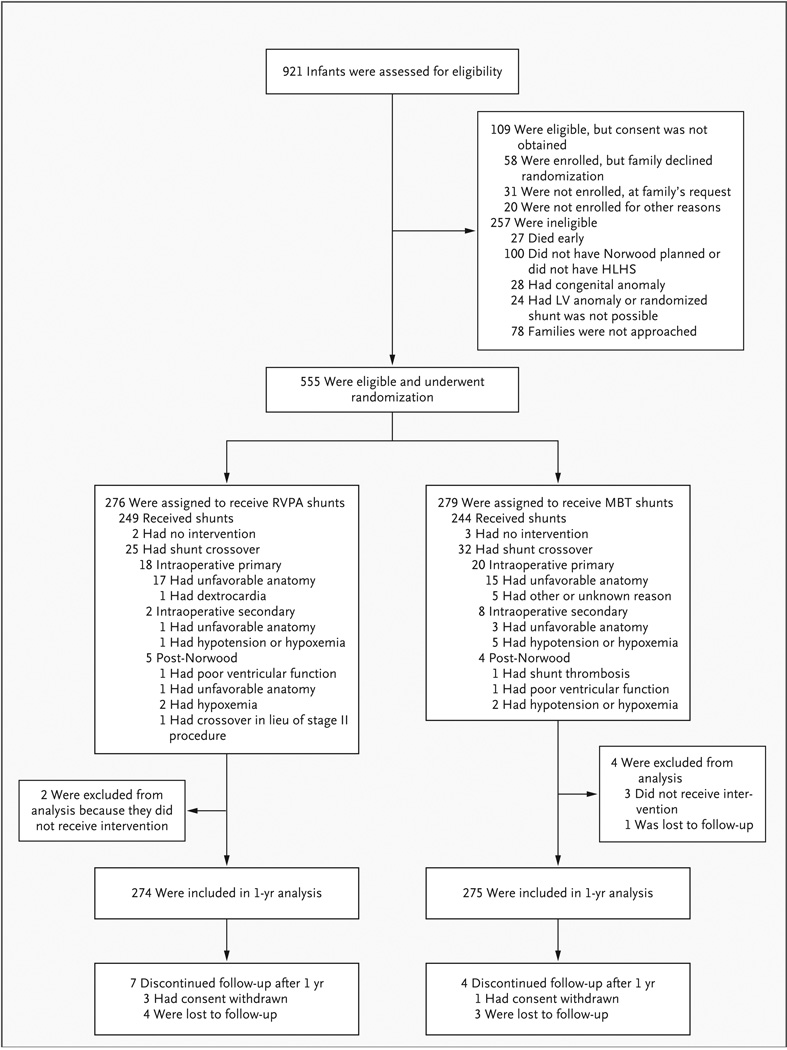
Of 921 infants with single ventricles who were screened between May 2005 and July 2008, 664 (72%) met the eligibility criteria, 555 (84%) of whom were enrolled in the study (Fig. 3). Baseline characteristics were similar between treatment groups and between subjects whose families declined enrollment and those whose families consented (Table 1).
Figure 3. Enrollment, Randomization, and Follow-up of Infants with Hypoplastic Left Heart Syndrome.
Five infants — two assigned to the right ventricle–pulmonary artery (RVPA) shunt group and three to the modified Blalock–Taussig (MBT) shunt group — did not undergo surgery and were therefore excluded from the 1-year analysis; the decision not to perform surgery was determined to be independent of the shunt assignment. Patients in the intraoperative primary category initially received a shunt that was not the one to which they were randomly assigned owing to some anatomical contraindication; those in the intraoperative secondary category initially received the assigned shunt but were switched to the other shunt because the first shunt was unsuccessful. HLHS denotes hypoplastic left heart syndrome, and LV left ventricular.
Table 1.
Baseline Characteristics of Eligible Patients According to Enrollment Status and Shunt Assignment.*
| Characteristic | Not Enrolled | Enrolled | |
|---|---|---|---|
| RVPA Shunt | MBT Shunt | ||
| No. of infants† | 109 | 274 | 275 |
| Age — days | |||
| At screening | 3.1±2.9 | 3.1±3.2 | 3.2±3.8 |
| At randomization | — | 5.0±4.0 | 5.1±4.1 |
| Male sex — % | 64 | 63 | 61 |
| Race or ethnic group — %‡ | |||
| White | 83 | 79 | 79 |
| Black | 8 | 15 | 16 |
| Asian | 3 | 2 | 2 |
| Hispanic | 15 | 21 | 16 |
| Other | 6 | 5 | 3 |
| Birth weight — kg | 3.1±0.5 | 3.1±0.5 | 3.1±0.6 |
| Gestational age | |||
| <38 wk — % | 29 | 24 | 27 |
| Median — wk (interquartile range)§ | 38 (37–39) | 38 (38–39) | 38 (37–39) |
| Apgar score — median (interquartile range) | |||
| At 1 min | — | 8 (8–9) | 8 (7–9) |
| At 5 min | — | 9 (8–9) | 9 (8–9) |
| Anatomical diagnosis — % | |||
| Hypoplastic left heart syndrome | 91 | 87 | 88 |
| Critical aortic stenosis | 0 | <1 | 1 |
| Single RV with systemic outflow obstruction | 5 | 4 | 4 |
| Right dominant AV canal with systemic outflow obstruction |
3 | 5 | 5 |
| Straddling mitral valve with LV hypoplasia and outflow obstruction |
1 | <1 | 0 |
| Other | 1 | 3 | 2 |
| Any associated anatomical diagnosis — % | 25 | 32 | 34 |
| Aortic atresia — % | 63 | 62 | 63 |
| Obstructed pulmonary venous return — % | 4 | 3 | 4 |
| Size of ascending aorta — cm | — | 0.4±0.2 | 0.4±0.2 |
| Moderate-to-severe tricuspid-valve regurgitation — % | — | 10 | 14 |
Plus–minus values are means ±SD. AV denotes atrioventricular, LV left ventricular, MBT modified Blalock–Taussig, RV right ventricle, and RVPA right ventricle–pulmonary artery.
Five infants who were randomly assigned to a shunt but did not undergo the Norwood procedure were excluded. There were no significant differences in characteristics according to shunt assignment.
Percentages may not add up to 100% because of rounding. Race and ethnic group were reported by study personnel; Hispanic patients were also included in other groups.
Gestational age was imputed to be 40 weeks for 12 full-term infants.
TRANSPLANTATION-FREE SURVIVAL
By 12 months after randomization, there were 72 events (68 deaths and 4 transplantations) among the 274 infants assigned to the RVPA shunt group as compared with 100 events (91 deaths and 9 transplantations) among the 275 infants assigned to the MBT shunt group (26.3% vs. 36.4%; absolute reduction in the RVPA group, 10.1 percentage points; 95% confidence interval [CI], −17.8 to −2.4; P = 0.01) (Table 2). The relative risk of death or transplantation with the RVPA shunt as compared with the MBT shunt was 0.72 (95% CI, 0.56 to 0.93). Events occurred in 28 of 274 infants in the RVPA shunt group (10%) and in 38 of 275 infants in the MBT shunt group (14%) from the time of the Norwood procedure to 30 days after-ward; in 29 of 243 infants (12%) and 52 of 236 (22%), respectively, from 30 days after the Norwood procedure to stage II; and in 15 of 213 infants (7%) and 10 of 184 (5%), respectively, from stage II to 12 months.
Table 2.
Outcomes and Adverse Events According to Shunt Assignment.*
| Outcome | Norwood Hospitalization | Stage II Hospitalization | From Randomization to 12 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RVPA Shunt (N = 274) |
MBT Shunt (N = 275) |
P Value | RVPA Shunt N = 214) |
MBT Shunt (N =184) |
P Value | RVPA Shunt (N = 274) |
MBT Shunt (N = 275) |
P Value | |
| Primary outcome | |||||||||
| Death or cardiac transplantation at 12 months —% |
26.3 | 36.4 | 0.01 | ||||||
| No. of outcome events | 72 | 100 | |||||||
| Hospital morbidity | |||||||||
| Time to initial extubation — hr | 0.41 | 0.19 | |||||||
| Median | 126 | 126 | 22.9 | 16.5 | |||||
| Interquartile range | 85–192 | 91–219 | 7.6–40.4 | 5.3–33.8 | |||||
| Median time on ventilator — days | 7 | 7 | 0.29 | 2 | 2 | ||||
| Median length of stay in intensive care unit — days | 14.0 | 14.0 | 0.82 | 4.0 | 4.0 | ||||
| Median length of postoperative hospital stay — days |
24.0 | 24.0 | 0.80 | 8.0 | 8.0 | ||||
| Open sternum — % | 74 | 76 | 0.62 | 0 | 0 | ||||
| Extracorporeal membrane oxygenation — % | 8 | 12 | 0.26 | 0 | 0 | ||||
| Cardiopulmonary resuscitation — % | 13 | 20 | 0.04 | 3 | 3 | ||||
| Norwood Hospitalization | Norwood Discharge to Stage II Discharge | Stage II Discharge to 12 Months of Age | |||||||
| RVPA Shunt (N = 274) |
MBT Shunt (N = 275) |
P Value | RVPA Shunt N = 233) |
MBT Shunt N=219) |
P Value | RVPA Shunt N=202) |
MBT Stunt (N = 176) |
P Value | |
|
Unintended cardiovascular procedures — no. of
events (rate/100 infants) |
|||||||||
| Balloon dilation of shunt or PA branch | 4 (1.5) | 15 (5.5) | 0.01 | 96 (41.2) | 56 (25.6) | 0.01 | 5 (2.5) | 3 (1.7) | 0.75 |
| Stent placement in shunt or PA branch | 8 (2.9) | 8 (2.9) | 0.99 | 17(7.3) | 4 (1.8) | 0.008 | 2 (1.0) | 0 (0.0) | 0.13 |
| Shunt revision | 14 (5.1) | 14(5.1) | 0.99 | 1 (0.4) | 2 (0.9) | 0.49 | 0 | 0 | |
| Shunt crossover | 24 (8.8) | 31 (11.3) | 0.36 | 0 | 105 (47.9) | 0 | 0 | ||
| Balloon dilation, stent placement, or surgical revision of neoaorta |
13 (4.7) | 7 (2.5) | 0.17 | 50(21.5) | 41 (18.7) | 0.72 | 14 (6.9) | 7 (4.0) | 0.36 |
| PA reconstruction† | 1 (0.4) | 2 (0.7) | 0.56 | 1 (0.4) | 2 (0.9) | 0.49 | 1 (0.5) | 0 | 0.29 |
| Total interventions | 64 (23.4) | 77 (28.0) | 0.29 | 165 (70.8) | 105 (47.9) | 0.008 | 22 (10.8) | 10(5.7) | 0.17 |
| Composite of serious adverse events | |||||||||
| Total events — no. (rate/100 infants) | 98 (36) | 133 (48) | 0.02 | 53 (23) | 61 (28) | 0.16 | 5(2) | 2 (1) | 0.43 |
| Infants with ≥1 event — no. (%) | 72 (26) | 102 (37) | 0.008 | 46 (20) | 56(26) | 0.15 | 4(2) | 2 (1) | 0.69 |
| Events, death excluded — no. (rate/100 infants) | 68 (25) | 99 (36) | 0.02 | 31 (13) | 27 (12) | 0.96 | 3(2) | 0 | 0.06 |
| Infants with ≥1 event, death excluded — no. (%) | 52 (19) | 77 (28) | 0.02 | 27 (12) | 26 (12) | 1.00 | 2(1) | 0 | 0.50 |
| Complications | |||||||||
| Total complications — no. (rate/100 infants) | 792 (289) | 850 (309) | 0.20 | 515 (221) | 367 (168) | 0.002 | 145 (72) | 81 (46) | 0.03 |
| Infants with ≥1 complication — no. (%) | 214 (78) | 217(79) | 0.84 | 163 (70) | 137 (63) | 0.11 | 79 (39) | 50 (28) | 0.03 |
| After Norwood Procedure | Before Stage II Procedure‡ | At 14 Months of Age | |||||||
| RVPA Shunt N=239) |
MBT Shunt (N=241) |
P Value | RVPA Shunt N = 214) |
MBT Shunt N = 181) |
P Value | RVPA Shunt N = 179) |
MBT Stunt N = 184) |
P Value | |
| Echocardiographic findings | |||||||||
| RV end-diastolic volume adjusted for BSA1.3 — ml/m2.6 § |
0.09 | 0.009 | 0.07 | ||||||
| Median | 86.5 | 91.2 | 105.2 | 113.4 | 88.9 | 83.3 | |||
| Interquartile range | 73.8–104.3 | 76.3–108.1 | 86.8–125.3 | 94.1–138.6 | 72.6–104.7 | 69.4–100.3 | |||
| RV end-systolic volume adjusted for BSA1.3 — ml/m2.6 § |
0.001 | 0.004 | 0.10 | ||||||
| Median | 44.2 | 50.1 | 57.9 | 63.2 | 50.5 | 45.4 | |||
| Interquartile range | 36.6–57.1 | 40.2–61.9 | 44.6–69.9 | 49.9–83.0 | 39.7–60.8 | 38.5–56.6 | |||
| RV ejection fraction — % | 48.5±7.6 | 44.5±7.6 | <0.001 | 44.7±8.3 | 42.9±7.9 | 0.07 | 42.7±8.0 | 42.7±7.4 | 0.97 |
| Moderate-to-severe tricuspid-valve regurgitation —% |
21.8 | 26.6 | 0.24 | 25.7 | 27.6 | 0.73 | 22.9 | 20.8 | 0.69 |
| Angiographic findings | |||||||||
| No. of subjects | 191 | 159 | — | ||||||
| Diameter of distal center PA — mm | 5.4±1.7 | 5.2±1.5 | 0.54 | ||||||
| Diameter of distal right PA— mm | 5.4±1.7 | 6.1±2.0 | <0.001 | ||||||
| Nakata index¶ | 0.009 | ||||||||
| Median | 145 | 169 | |||||||
| Interquartile range | 110–197 | 124–230 | |||||||
| Ratio of distal to proximal center PA diameter | 1.3±0.6 | 1.1±0.3 | 0.003 | ||||||
| Ratio of distal to proximal right PA diameter | 1.3±0.6 | 1.3±0.6 | 0.83 | ||||||
| Center PA stenosis — % of infants | 26 | 19 | 0.16 | ||||||
| Right PA stenosis — % of infants | 36 | 27 | 0.08 | ||||||
Plus–minus values are means ±SD. There were 274 infants in the right ventricle–pulmonary artery (RVPA) shunt group and 275 in the modified Blalock–Taussig (MBT) shunt group; under Angiographic findings, the corresponding totals were 191 and 159. P values were calculated with the use of Fisher’s exact test for categorical outcomes, a Poisson regression model was used for event rates, Student’s t-test was used to calculate means, and the Wilcoxon rank-sum test was used to determine medians. PA denotes pulmonary artery, and RV right ventricular.
These were pulmonary-artery reconstructions other than those undertaken as a standard component of the stage II procedure.
Five infants did not undergo stage II surgery, but their echocardiographic data were included in the analysis; the mean age of these infants at the time of echocardiography was 3.9±1.2 months.
Values for the RV end-diastolic and end-systolic volumes were adjusted for body-surface area (BSA) by dividing the volume by BSA1.3; since BSA is measured in meters squared, this unit is multiplied by 1.3, yielding m2.6.
The Nakata index (also known as the pulmonary-artery index) is calculated by dividing the sum of the areas of the right PA and the center PA by body-surface area. The optimal value is 200 or higher.25
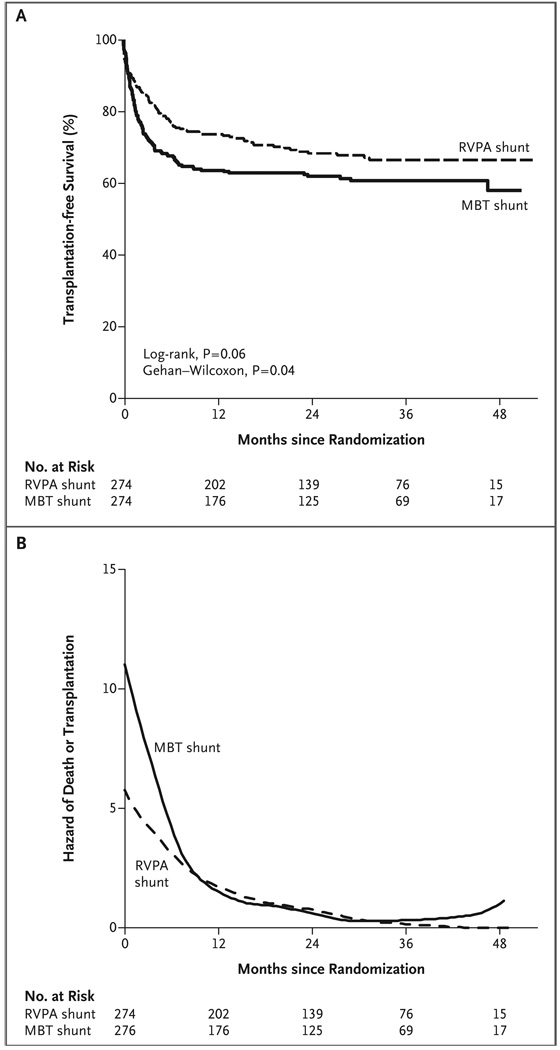
The mean (±SD) follow-up time for survivors who did not undergo transplantation was 32±11 months (range, 12 to 52). On the basis of all follow-up data, the difference in transplantation-free survival between the shunt groups was no longer significant because the higher mortality in the MBT shunt group primarily occurred early in the follow-up period (P = 0.06 by the log-rank test) (Fig. 4). The Wilcoxon–Gehan test, which gives greater weight to early group differences, did show a difference in transplantation-free survival (P = 0.04). Nonproportional-hazards testing showed that the treatment effect differed in the period before and the period after 12 months (P = 0.02). After 12 months, 10 deaths and 6 transplantations occurred in the RVPA shunt group, as compared with 7 deaths and 0 transplantations in the MBT shunt group (8% vs. 4% of infants who survived for more than 12 months).
Figure 4. Primary Outcome and the Hazard of Death or Transplantation at 12 Months, According to Shunt Assignment.
Panel A shows the Kaplan–Meier curves for transplantation-free survival among all infants who underwent the Norwood procedure, according to the intention-to-treat analysis. Panel B shows the estimated hazard of death or transplantation among all infants who underwent the Norwood procedure, according to the assigned shunt. The hazard is an instantaneous rate representing the predicted number of deaths or transplantations per month at a defined time point. P = 0.02 for the difference in the treatment effect for the period before and the period after 12 months. MBT denotes modified Blalock–Taussig, and RVPA right ventricle–pulmonary artery.
There were 57 crossovers to the unassigned shunt, for an overall crossover rate of 10%, and the rates were similar in the two shunt groups (Fig. 3); 48 of these crossovers (84%) occurred during the Norwood procedure, and the remaining 9 (16%) occurred during a later, separate procedure. The primary reason for crossover was cardiovascular anatomy that made it impossible to use the assigned shunt. In analyses based on the shunt actually received, the rate of death or transplantation at 12 months remained significantly lower in the RVPA shunt group than in the MBT shunt group (25.6% vs. 37.3%; absolute reduction of 11.7 percentage points; 95% CI, −19.4 to −4.0; P = 0.003). The overall transplantation-free survival rate based on all follow-up data was higher in the RVPA shunt group (P = 0.02).
SECONDARY OUTCOMES
Morbidity during hospitalizations for the Norwood and stage II procedures was similar for the two groups, except that fewer infants in the RVPA shunt group required cardiopulmonary resuscitation after the Norwood procedure (Table 2). Conversely, infants in the RVPA shunt group underwent more unintended cardiovascular interventions from the time of randomization to 12 months (92 vs. 70 per 100 infants, P = 0.003). This difference was largely attributable to the higher rate of balloon dilation or stent placement in the shunt or a branch of the pulmonary artery in the RVPA shunt group, particularly after discharge following the Norwood procedure (Table 2).
Median right ventricular end-diastolic and end-systolic volumes, adjusted for body-surface area, were lower in the RVPA shunt group than in the MBT shunt group on echocardiograms obtained before stage II procedures were performed, but there was no difference at 14 months (Table 2). The ejection fraction was greater in the RVPA shunt group after the Norwood procedure ( P<0.0 01) but was similar in the two groups at 14 months (P = 0.97). The incidence of moderate-to-severe tricuspid-valve regurgitation was similar in the two groups at 14 months (22% for the entire cohort).
On the basis of the Nakata index, the overall size of the pulmonary artery on angiography before the stage II procedure was smaller in the RVPA shunt group than in the MBT shunt group. When the individual pulmonary-artery branches were compared, the mean diameter of the distal right branch was smaller in the RVPA shunt group, whereas the mean diameters of the distal left branches were similar in the two groups (Table 2).
ADVERSE EVENTS AND COMPLICATIONS
The rate of serious adverse events, including death, for the entire trial period from randomization to 12 months was lower in the RVPA shunt group than in the MBT shunt group (57 vs. 71 events per 100 infants, P = 0.04). When death was excluded, the overall rates for the entire trial period did not differ significantly between the RVPA and MBT shunt groups (37 and 46 per 100 subjects, respectively; P = 0.13). The rates of serious adverse events broken down into the various time periods, from the time of the Norwood procedure to 12 months of age, are shown in Table 2.
During the period between discharge after the Norwood procedure and the stage II procedure, the complication rate was higher in the RVPA shunt group than in the MBT shunt group (220 vs. 168 events per 100 infants, P = 0.003), although the proportions of infants who had at least one complication were similar in the two groups (69% for RVPA shunts vs. 63% for MBT shunts, P = 0.17) (Table 2). After the stage II hospital discharge, the overall complication rate was higher in the RVPA shunt group, as was the proportion of infants with at least one complication. During the period between randomization and the age of 12 months, the rate of complications was higher in the RVPA shunt group than in the MBT shunt group (5.3 vs. 4.7 complications per infant, P = 0.002), although the proportion of infants with at least one complication was the same in the two groups (91%, P = 0.88). These events largely consisted of respiratory, neurologic, and infectious complications.
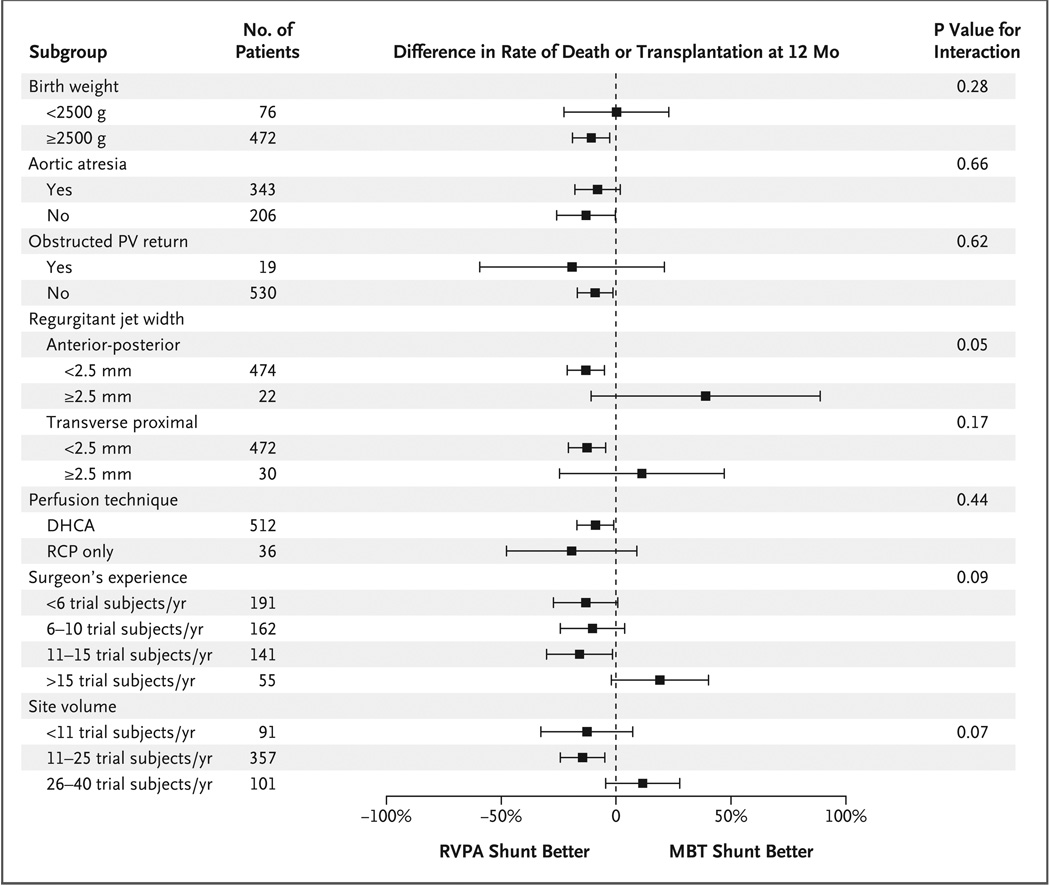
SUBGROUP ANALYSES
In prespecified subgroup analyses (Fig. 5), the effect of shunt type on the primary outcome did not differ according to stratification or prespecified subgroup factors. However, when the site volume was calculated on the basis of all screened infants (i.e., the total number of live births of infants with a single right ventricle per year) was analyzed as a continuous variable, the benefit of the RVPA shunt with respect to 12-month transplantation-free survival was inversely related to the annual number of procedures performed at the individual site (P = 0.04).
Figure 5. Difference in Rate of Death or Transplantation at 12 Months in Prespecified Subgroups, According to Shunt Assignment.
P values are from a logistic-regression test of the interaction between shunt assignment and treatment subgroup. The strata for surgeon’s experience and site volume were defined according to the annual number of randomly assigned infants. Bars represent 95% confidence intervals. DHCA denotes deep hypothermic circulatory arrest during the Norwood procedure, MBT modified Blalock–Taussig, PV pulmonary venous, RCP regional cerebral perfusion, and RVPA right ventricle–pulmonary artery.
DISCUSSION
The results of this multicenter, randomized trial showed that in infants with hypoplastic left heart syndrome or related single right ventricular anomalies, use of the Norwood procedure with an RVPA shunt, as compared with an MBT shunt, was associated with a higher rate of transplantation-free survival 12 months after randomization (the primary outcome). Secondary analyses of transplantation-free survival at 12 months, based on the shunt that was actually used rather than on the randomly assigned shunt, had similar results. With longer follow-up, however, we observed only a trend toward better outcomes with the RVPA shunt. Using a test of interaction for nonproportional hazards, we found that the nature of the treatment effect was different before and after 12 months. The reasons for the shift in the risk of death or need for transplantation between the early and intermediate periods are speculative. The MBT shunt generates continuous forward flow into the pulmonary arteries, leading to diastolic runoff, coronary steal, and an increased ratio of pulmonary blood flow to systemic blood flow. This physiological response may cause hemodynamic instability early after the Norwood procedure, as well as during the interstage period. The majority of deaths and transplantations occurred during the period from 30 days after the Norwood procedure to the time of the stage II procedure. The MBT shunt is removed at stage II, potentially allowing some of the negative factors related to use of the RVPA shunt to become evident. These factors may include damage to the right ventricle from the ventriculotomy and smaller pulmonary arteries, both of which would be potential disadvantages in infants with single-ventricle anomalies.
The secondary outcomes also differed with respect to early and late risks. Echocardiograms obtained before the stage II procedure showed that infants assigned to the RVPA shunt, as compared with those assigned to the MBT shunt, had smaller right ventricular end-systolic and end-diastolic volumes, when adjusted for body-surface area, and a higher right ventricular ejection fraction. However, by 14 months, the right ventricular end-diastolic volume was similar in the two groups, and the ejection fraction was also similar. These changes may continue over time. Tanoue and colleagues26 compared a group of subjects who underwent the Norwood procedure with an RVPA shunt with a group of historical control subjects who received an MBT shunt. The catheterization data before and after the Fontan procedure showed decreased right ventricular contractility in the RVPA shunt group, with preserved ventricular efficiency based on a lower systemic afterload. Furthermore, in our trial, the 12-month rate of unintended interventions was higher for the RVPA shunt group, in which the interventions consisted primarily of balloon dilation and stent placement. Continued follow-up of trial subjects will be needed to assess the longer-term effects of these two shunts on right ventricular function.
We explored whether the relative efficacy of the two shunts varied in subgroups of infants. The effect of shunt type on transplantation-free survival at 12 months was homogeneous across predetermined subgroups based on birth weight, the presence or absence of aortic atresia or obstructed pulmonary venous return, the degree of tricuspid-valve regurgitation before the Norwood procedure, use or nonuse of regional cerebral perfusion or deep hypothermic circulatory arrest during the Norwood procedure, and the surgeon’s experience. Only site volume showed an interaction, with higher volume negating the advantage of the RVPA shunt with respect to transplantation-free survival. This finding may reflect the expertise of individual surgeons or greater institutional experience in the perioperative care of patients with an MBT shunt. However, an analysis of multiple measures of morbidity for the Norwood hospitalization did not suggest differences in hospital course between groups, with the exception of a lower incidence of cardiopulmonary resuscitation in the RVPA shunt group after the Norwood procedure. In this regard, more extensive analyses of variations in practice patterns may be enlightening.
This trial should be viewed in light of its limitations. As with all surgical trials that compare two operations, it was not possible to keep the personnel who were caring for these infants unaware of the specific intervention. However, the components of the primary outcome (i.e., death and transplantation) were discrete, objective events. Echocardiographic and catheterization measurements were objectively defined and performed in core laboratories. The trial may not have been sufficiently powered to detect important differences in some of the secondary outcomes or interactions between shunt type and prespecified subgroup factors. The results of the intermediate follow-up represent the course of only a subgroup of all the enrolled infants, since not all of them have completed longer-term follow-up. The assessment of nonproportional hazards before and after 1 year was exploratory, and additional follow-up will be important to quantify the relative hazards associated with the two shunts. Using the number of screened infants to define center volume, we found that the category of greatest experience included infants from only two centers.
In summary, among infants with hypoplastic left heart syndrome and related single, right ventricular morphologic anomalies who underwent the Norwood procedure, 12-month transplantation-free survival was higher with the use of an RVPA shunt than with the use of an MBT shunt. However, the RVPA shunt was associated with a higher rate of unintended cardiovascular interventions and complications during the first 12 months after randomization. On the basis of available intermediate-term data, there was no significant difference between the two groups with respect to transplantation-free survival beyond 12 months. Continued surveillance of this cohort is needed to determine whether either of these shunts turns out to be superior over the long term.
Supplementary Material
Acknowledgments
Supported by grants (HL068269, HL068270, HL068279, HL068281, HL068285, HL068288, HL068290, HL068292, and HL085057) from the National Heart, Lung, and Blood Institute.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Tabbutt S, Dominguez TE, Ravishankar C, et al. Outcomes after the stage I reconstruction comparing the right ventricular to pulmonary artery conduit with the modified Blalock Taussig shunt. Ann Thorac Surg. 2005;80:1582–1590. doi: 10.1016/j.athoracsur.2005.04.046. [DOI] [PubMed] [Google Scholar]
- 2.Azakie A, Martinez D, Sapru A, Fineman J, Teitel D, Karl TR. Impact of right ventricle to pulmonary artery conduit on outcome of the modified Norwood procedure. Ann Thorac Surg. 2004;77:1727–1733. doi: 10.1016/j.athoracsur.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Mahle WT, Cuadrado AR, Tam VK. Early experience with a modified Norwood procedure using right ventricle to pulmonary artery conduit. Ann Thorac Surg. 2003;76:1084–1088. doi: 10.1016/s0003-4975(03)00343-6. [DOI] [PubMed] [Google Scholar]
- 4.Mair R, Tulzer G, Sames E, et al. Right ventricular to pulmonary artery conduit instead of modified Blalock-Taussig shunt improves postoperative hemodynamics in newborns after the Norwood operation. J Thorac Cardiovasc Surg. 2003;126:1378–1384. doi: 10.1016/s0022-5223(03)00389-1. [DOI] [PubMed] [Google Scholar]
- 5.Pizarro C, Malec E, Maher KO, et al. Right ventricle to pulmonary artery conduit improves outcome after stage I Nor- wood for hypoplastic left heart syndrome. Circulation. 2003;108 Suppl 1 doi: 10.1161/01.cir.0000087390.94142.1d. II-155-II-160. [DOI] [PubMed] [Google Scholar]
- 6.Sano S, Ishino K, Kado H, et al. Out-come of right ventricle-to-pulmonary artery shunt in first-stage palliation of hypoplastic left heart syndrome: a multi-institutional study. Ann Thorac Surg. 2004;78:1951–1957. doi: 10.1016/j.athoracsur.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 7.Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects — United States, 2003. MMWR Morb Mortal Wkly Rep. 2007;56:25–29. [PubMed] [Google Scholar]
- 8.Tweddell JS, Hoffman GM, Fedderly RT, et al. Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg. 2000;69:1893–1899. doi: 10.1016/s0003-4975(00)01349-7. [DOI] [PubMed] [Google Scholar]
- 9.Azakie T, Merklinger SL, McCrindle BW, et al. Evolving strategies and improving outcomes of the modified Norwood procedure: a 10-year single-institution experience. Ann Thorac Surg. 2001;72:1349–1353. doi: 10.1016/s0003-4975(01)02795-3. [DOI] [PubMed] [Google Scholar]
- 10.Hehir DA, Dominguez TE, Ballweg JA, et al. Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg. 2008;136:94–99. doi: 10.1016/j.jtcvs.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Ohye RG, Ludomirsky A, Devaney EJ, Bove EL. Comparison of right ventricle to pulmonary artery conduit and modified Blalock-Taussig shunt hemodynamics after the Norwood operation. Ann Thorac Surg. 2004;78:1090–1093. doi: 10.1016/S0003-4975(03)01386-9. [DOI] [PubMed] [Google Scholar]
- 12.Khouri EM, Gregg DE, Rayford CR. Effect of exercise on cardiac output, left coronary flow and myocardial metabolism in the unanesthetized dog. Circ Res. 1965;17:427–437. doi: 10.1161/01.res.17.5.427. [DOI] [PubMed] [Google Scholar]
- 13.Mahle WT, Spray TL, Gaynor JW, Clark BJ., III Unexpected death after reconstructive surgery for hypoplastic left heart syndrome. Ann Thorac Surg. 2001;71:61–65. doi: 10.1016/s0003-4975(00)02324-9. [DOI] [PubMed] [Google Scholar]
- 14.Charpie JR, Dekeon MK, Goldberg CS, Mosca RS, Bove EL, Kulik TJ. Serial blood lactate measurements predict early outcome after neonatal repair or palliation for complex congenital heart disease. J Thorac Cardiovasc Surg. 2000;120:73–80. doi: 10.1067/mtc.2000.106838. [DOI] [PubMed] [Google Scholar]
- 15.Norwood WI, Lang P, Casteneda AR, Campbell DN. Experience with operations for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 1981;82:511–519. [PubMed] [Google Scholar]
- 16.Pizarro C, Mroczek T, Malec E, Norwood WI. Right ventricle to pulmonary artery conduit reduces interim mortality after stage 1 Norwood for hypoplastic left heart syndrome. Ann Thorac Surg. 2004;78:1959–1963. doi: 10.1016/j.athoracsur.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 17.Lai L, Laussen PC, Cua CL, et al. Out-comes after bidirectional Glenn operation: Blalock-Taussig shunt versus right ventricle-to-pulmonary artery conduit. Ann Thorac Surg. 2007;83:1768–1773. doi: 10.1016/j.athoracsur.2006.11.076. [DOI] [PubMed] [Google Scholar]
- 18.Cua CL, Thiagarajan RR, Gauvreau K, et al. Early postoperative outcomes in a series of infants with hypoplastic left heart syndrome undergoing stage I palliation operation with either modified Blalock-Taussig shunt or right ventricle to pulmonary artery conduit. Pediatr Crit Care Med. 2006;7:238–244. doi: 10.1097/01.PCC.0000201003.38320.63. [DOI] [PubMed] [Google Scholar]
- 19.Kussman BD, Gauvreau K, DiNardo JA, et al. Cerebral perfusion and oxygenation after the Norwood procedure: comparison of right ventricle-pulmonary artery conduit with modified Blalock-Taussig shunt. J Thorac Cardiovasc Surg. 2007;133:648–655. doi: 10.1016/j.jtcvs.2006.09.034. [DOI] [PubMed] [Google Scholar]
- 20.Alsoufi B, Bennetts J, Verma S, Caldarone CA. New developments in the treatment of hypoplastic left heart syndrome. Pediatrics. 2007;119:109–117. doi: 10.1542/peds.2006-1592. [DOI] [PubMed] [Google Scholar]
- 21.Mahony L, Sleeper LA, Anderson PA, et al. The Pediatric Heart Network: a primer for the conduct of multicenter studies in children with congenital and acquired heart disease. Pediatr Cardiol. 2006;27:191–198. doi: 10.1007/s00246-005-1151-9. [DOI] [PubMed] [Google Scholar]
- 22.Ohye RG, Gaynor JW, Ghanayem NS, et al. Design and rationale of a randomized trial comparing the Blalock-Taussig and right ventricle-pulmonary artery shunts in the Norwood procedure. J Thorac Cardiovasc Surg. 2008;136:968–975. doi: 10.1016/j.jtcvs.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zelen M. The randomization and stratification of subjects to clinical trials. J Chronic Dis. 1974;27:365–375. doi: 10.1016/0021-9681(74)90015-0. [DOI] [PubMed] [Google Scholar]
- 24.Helbing WA, Bosch HG, Maliepaard C, et al. Comparison of echocardiographic methods with magnetic resonance imaging for assessment of right ventricular function in children. Am J Cardiol. 1995;76:589–594. doi: 10.1016/s0002-9149(99)80161-1. [DOI] [PubMed] [Google Scholar]
- 25.Nakata S, Imai Y, Takanashi Y, et al. A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg. 1984;88:610–619. [PubMed] [Google Scholar]
- 26.Tanoue Y, Kado H, Shiokawa Y, Fusazaki N, Ishikawa S. Midterm ventricular performance after Norwood procedure with right ventricular-pulmonary artery conduit. Ann Thorac Surg. 2004;78:1965–1971. doi: 10.1016/j.athoracsur.2004.06.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.