Abstract
Tobacco carcinogen and toxicant biomarkers are metabolites or protein or DNA adducts of specific compounds in tobacco products. Highly reliable analytical methods, based mainly on mass spectrometry, have been developed and applied in large studies of many of these biomarkers. A panel of tobacco carcinogen and toxicant biomarkers is suggested here, and typical values for smokers and non-smokers are summarized. This panel of biomarkers has potential applications in the new and challenging area of tobacco product regulation and in development of rational approaches to cancer prevention by establishing carcinogen and toxicant uptake and excretion in people exposed to tobacco products.
Keywords: tobacco carcinogens, tobacco toxicants, biomarkers
Introduction
Tobacco products present a perfect storm consisting of an addictive constituent, nicotine, and a complex mixture of toxicants and carcinogens. Attesting to their addictive power is the fact that more than one billion people in the world smoke cigarettes and other tobacco products while hundreds of millions use smokeless tobacco (1). The consequences are enormous: 33% of all cancer mortality in the U.S. and 21 % worldwide is due to tobacco products (2). The latest evaluation by the International Agency for Research on Cancer lists 19 cancers for which there is sufficient evidence that tobacco smoking is a cause, and 3 caused by smokeless tobacco use (3). On average, three thousand people succumb daily to lung cancer in the world, about 90% of which is caused by cigarette smoking (4).
The U.S. President’s Cancer Panel Report states: “Ridding the nation of tobacco is the single most important action needed to dramatically reduce cancer mortality and morbidity” (5). Tobacco control efforts in the U.S. have been quite successful, as the combination of smoke free legislation, taxation, and aggressive anti-tobacco advertising among other approaches has decreased smoking prevalence to the current level of 20.6%; four states have prevalence of less than 15% (6). Worldwide, the results are varied, and there are still major areas of high tobacco use such as China which has more male smokers than there are people in the U.S. (1). There is a great deal of work left to do in tobacco control.
This perspective will discuss the potential use of tobacco carcinogen and toxicant biomarkers in tobacco product regulation with respect to cancer. Tobacco products are also a cause of cardiovascular and pulmonary disease, but those effects and their biomarkers are not considered here (7,8). Major recent regulatory legislative actions have changed the landscape with respect to tobacco. The World Health Organization in its Framework Convention on Tobacco Control (FCTC) recognized the need for tobacco product regulation. In 2009, the U.S. Congress passed, and President Obama signed into law, the Family Smoking Prevention and Tobacco Control Act which gives FDA unprecedented power to regulate tobacco products.
This perspective will also discuss the application of tobacco carcinogen and toxicant biomarkers in cancer prevention. Assessment of non-smokers’ exposure to secondhand tobacco smoke is already a success story of biomarkers in cancer prevention. Biomarkers also promise to increase our understanding of the mechanisms by which tobacco products cause cancer. This can lead to innovative approaches to cancer prevention by identifying and targeting those individuals who are particularly susceptible to the cancer causing effects of tobacco products.
The term “biomarker” has varied meanings. In the cancer research field in particular, this term is often associated with early detection of cancer. That is not the context here. Merriam-Webster’s Collegiate Dictionary defines biomarker as “a distinctive biological or biologically derived indicator (as a metabolite) of a process, event, or condition.” A biomarker in this paper is any quantifiable substance, such as a metabolite, that can be specifically related to the uptake or effects of tobacco carcinogens or toxicants.
A Panel of Biomarkers
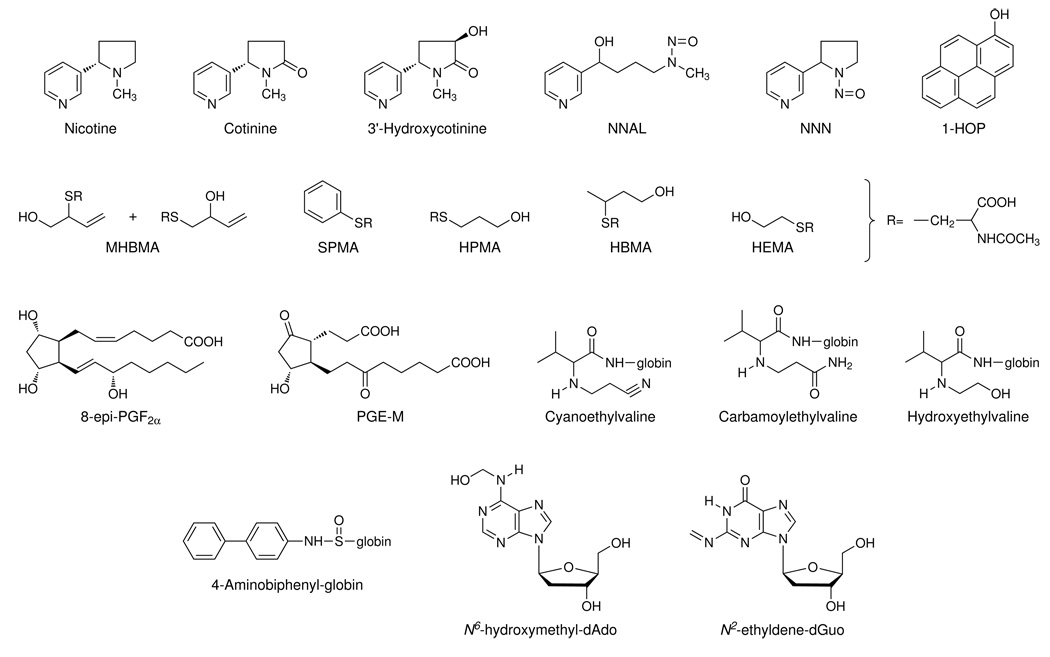
A panel of tobacco toxicant and carcinogen biomarkers that could be used in product regulation and studies on prevention of tobacco-induced cancer is presented in Table 1 and their structures are illustrated in Figure 1. All biomarkers have been validated analytically. Most have been used in multiple studies on hundreds or even thousands of smokers and non-smokers. (The exceptions are HBMA, HEMA, N6-hydroxymethyl-dAdo and N2-ethylidene-dGuo). Some typical recent data are summarized in Table 1. Although some of the ranges of values overlap between smokers and non-smokers for certain biomarkers, biomarker levels are consistently higher in smokers compared to non-smokers in individual studies. Biomarkers of the tobacco-specific compounds are similar in smokers and smokeless tobacco users, while those of the volatile organic compounds are considerably lower in smokeless tobacco users, based on our unpublished data.
Table 1.
A panel of biomarkers for investigating tobacco carcinogen and toxicant uptake and their possible relationship to cancer.
| Range of recent mean values (nmol/24h unless noted otherwisea) |
|||||
|---|---|---|---|---|---|
| Urinary biomarkers | Source | Smokers | Non-smokers | References (smokers) | References (non-smokers) |
| Nicotine equivalentsb | Nicotine | 70.4–154 µmol/24 h | NAc | (42,52,77–81) | |
| Total NNAL | NNK | 1.1 – 2.9 | NA | (16,42,52,79,81–85) | |
| Total NNN | NNN | 0.049 – 0.24 | NA | (13,83,84,86) | |
| 1-HOP | Pyrene | 0.50 – 1.45 | 0.18 – 0.50 | (16,42,52,79,80,82,87,88) | (42,52,80,87,88) |
| MHBMA | 1,3-Butadiene | 15.5 – 322 | 0.65 – 7.5 | (16,42,78,82) | (16,42,82) |
| SPMA | Benzene | 3.2 – 32.1 | 0.17 – 3.14 | (16,52,78–80,82,87,89) | (16,52,78,80,82,87,89) |
| HPMA | Acrolein | 5,869 – 11,190 | 1,131 – 1,847 | (16,42,52,78–80,82,89) | (16,42,52,78,80,82) |
| HBMA | Crotonaldehyde | 1,965 – 26,000 | 242 – 3,200 | (16,78,90) | (16,78,90) |
| HEMA | Ethylene oxide | 19.1 – 102 | 6.51 – 38.8 | (16,89) | (16,89) |
| Cd | Cadmium | 2.3 – 12.8 | 1.34 – 8.04 | (91–94) | (91–94) |
| 8-epi-PGF2αd | Oxidative damage | 1.48 – 2.80 | 0.62 – 1.13 | (95–97) | (95,97) |
| PGE-M | Inflammation | 54 – 60 | 31.6 – 45.3 | (27,98) | (27,98) |
|
Recent data (pmol/g globin; mean ± S.D.) |
|||||
| Hemoglobin adducts | Source | Smokers | Non-smokers | References (smokers) | References (non-smokers) |
| Cyanoethylvaline | Acrylonitrile | 112 ± 81 | 6.5 ± 6.4 | (52,99) | (52,99) |
| Carbamoylethylvaline | Acrylamide | 84.1 ± 41.8 | 27.8 ± 7.1 | (52,99) | (52,99) |
| Hydroxyethylvaline | Ethylene oxide | 132 ± 92 | 21.1 ± 12.7 | (52,99) | (52,99) |
| 4-Aminobiphenyl-globin | 4-Aminobiphenyl | 0.26 ± 0.006e | 0.067 ± 0.009e | (42,99) | (42,99) |
|
Recent data (fmol/µmol dN; mean ± S.D.) |
|||||
| Leukocyte DNA adducts | Source | Smokers | Non-smokers | References (smokers) | References (non-smokers) |
| N6-hydroxymethyl-dAdo | Formaldehyde | 179 ± 205 | 15.5 ± 33.8 | (100) | (100) |
| N2-ethylidene-dGuo | Acetaldehyde | 1,310 ± 1,720 | 705 ± 438 | (101) | (101) |
| Mean concentrations | |||||
| Other | Source | Smokers | Non-smokers | References (smokers) | References (non-smokers) |
| Exhaled CO | Carbon monoxide | 17.4 – 34.4 ppm | 2.6 – 6.5 ppm | (34,52) | (34,52) |
| Carboxyhemoglobin | Carbon monoxide | 3.4 – 7.1 % | 0.35 – 1.45 % | (34,42,52,81) | (34,42,52,81) |
Based on 1.3g creatinine per 24h in smokers and 1.5g creatinine per 24h in non-smokers, or 1.5 l urine per 24h. Creatinine determinations were mainly by a modified Jaffe reaction using a certified automated clinical analyzer.
Abbreviations
nicotine equivalents, the sum of nicotine, cotinine, 3'-hydroxycotinine, and their glucuronides;
total NNAL, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol and its glucuronides;
total NNN, N'-nitrosonornicotine and its glucuronides;
1-HOP, 1-hydroxypyrene and its glucuronides/sulfates;
MHBMA, the sum of 1-hydroxy-2-(N-acetylcysteinyl)-3-butene and 1-(N-acetylcysteinyl)-2-hydroxy-3-butene;
SPMA, S-phenyl mercapturic acid;
HPMA, 3-hydroxypropyl mercapturic acid;
HBMA, 4-hydroxybut-2-yl mercapturic acid;
HEMA, 2-hydroxyethyl mercapturic acid;
8-epi-PFG2α, 9,11,15-trihydroxyprosta-5,13-dien-1-oic acid;
PGE-M, 11α-hydroxy-9,15-dioxo-2,3,4,5-tetranorprostane-1,20-dioic acid
NA=Not applicable as these are not detected in the urine of non-smokers unless they use other tobacco products, nicotine replacement products (for nicotine equivalents, and sometimes NNN (13)), or are exposed to secondhand smoke, in which case levels are usually less than 5% of smoker levels (102,103).
Determined by mass spectrometry
Weighted mean ± S.D.
Figure 1.
Structures of the biomarkers.
“Nicotine equivalents”, the sum of nicotine, cotinine, 3′-hydroxycotinine and their glucuronides, comprise 73–96% of the nicotine dose received by a tobacco user (9), and is a superb biomarker of nicotine uptake directly measuring a high percentage of the nicotine dose. This is obviously crucial for any study of a tobacco product, since nicotine is the major known addictive constituent. Total NNAL and total NNN, the sum of free and glucuronidated NNAL and NNN, respectively, are biomarkers of uptake of the carcinogenic tobacco-specific nitrosamines NNK and NNN (10). NNK and NNN always occur together in tobacco products and are found in the particulate phase of tobacco smoke (11). NNK is a potent lung carcinogen in rodents and also induces tumors of the pancreas, liver, and nasal mucosa in rats (12). NNN causes esophageal and nasal tumors in rats and respiratory tract tumors in mice and hamsters (12). Among the biomarkers discussed here, nicotine equivalents, total NNAL, and total NNN are unique because of their tobacco-specificity. They are only detected in people exposed to tobacco products or (for nicotine equivalents and occasionally NNN) in people who use nicotine replacement products (13).
1-HOP is a biomarker of exposure to polycyclic aromatic hydrocarbons (PAH), particulate phase constituents of tobacco smoke and products of incomplete combustion, many of which are potent carcinogens inducing tumors of the rat lung, hamster trachea, and mouse forestomach and skin among other sites (14,15). The prototypic PAH carcinogen is benzo[a]pyrene (BaP). PAH always occur as mixtures, and 1-HOP, a metabolite of the non-carcinogen pyrene, a component of these mixtures, is widely accepted as a biomarker of PAH exposure. The mercapturic acids MHBMA, SPMA, HPMA, HBMA, and HEMA are biomarkers of the tobacco smoke gas phase constituents 1,3-butadiene, benzene, acrolein, crotonaldehyde, and ethylene oxide, respectively (16). 1,3-Butadiene is a multi-organ carcinogen in mice and rats (17,18). Sites of tumor induction in mice include the hematopoietic system, heart, lung, forestomach, Harderian gland, preputial gland, liver, mammary gland, ovary, and kidney, while in rats tumors are observed in pancreas, testis, thyroid gland, mammary gland, uterus, and Zymbal gland. Benzene causes multiple types of tumors in both rats and mice exposed by various routes including oral administration, inhalation, injection, and dermal application (19). Ethylene oxide administered by inhalation causes alveolar/bronchiolar adenomas and carcinomas of the lung in male and female B6C3F1 mice. Tumors of the Harderian gland, malignant lymphomas, uterine adenocarcinomas, and mammary gland carcinomas are also observed (18). Acrolein is an intense irritant and has a range of toxic effects including cilia-toxicity to the lung (20). Both acrolein and crotonaldehyde are associated with lipid peroxidation and perhaps inflammation (21,22). Acrolein reacts with the p53 gene at hot spots associated with lung cancer, a phenomenon which has also been observed in studies of PAH diol epoxides (23). Inhalation exposure to cadmium compounds causes lung tumors in rats (24,25). 8-epi-PGF2α is one of the isoprostanes, prostaglandin-like compounds which are formed by non-enzymatic free radical-induced peroxidation of arachidonic acid. It is an accepted biomarker of oxidative damage (26). PGE-M is a metabolite of cyclooxygenase-derived prostaglandin E2 (PGE2) (27). PGE2 is associated with inflammation, tumor development, and a variety of other physiological responses (27).
Acrylonitrile is an important industrial chemical as well as a tobacco smoke constituent. It induces tumors at multiple sites in rats including forestomach, central nervous system, and mammary gland (28,29). Acrylamide occurs widely in cooked starchy foods as well as in tobacco smoke. It causes a variety of tumors in rats including mesotheliomas of the testes, thyroid tumors, and mammary gland tumors (30). 4-Aminobiphenyl induces bladder tumors in rabbits and dogs and causes neoplasms at various sites in mice, while administration to rats produces tumors of the mammary gland and intestine (31).
Formaldehyde is genotoxic in multiple systems and causes squamous cell carcinomas of the nasal cavities in rats, while other studies produced mixed results (32). Acetaldehyde is genotoxic in a variety of in vitro systems and produces adenocarcinoma and squamous cell carcinoma of the nasal mucosa in rats, and laryngeal carcinoma in hamsters upon administration by inhalation (33). Carbon monoxide competes with oxygen for binding to Hb and impairs the release of oxygen from Hb. Although acute CO related symptoms are unlikely to occur in smokers (34), CO is believed to reduce oxygen delivery and promote complications of atherosclerosis and other cardiovascular diseases in smokers (8).
Overall then, the biomarkers in Table 1 represent a broad cross-section of carcinogens and toxicants in tobacco products. Among these compounds, NNK and NNN, BaP, 1,3-butadiene, benzene, ethylene oxide, cadmium, 4-aminobiphenyl, and formaldehyde are considered “carcinogenic to humans” by IARC (11,18,25,31,32,35) and are likely causes of different types of cancer caused by tobacco use, a topic which is beyond the scope of this perspective but has been discussed elsewhere (36–38). Many of these compounds also have considerable toxic effects. While these constituents represent only a small percentage of the over 5000 identified compounds in cigarette smoke (39), they are collectively a powerful group and include all of those singled out by the WHO for regulation under the FCTC: acetaldehyde, acrolein, benzene, BaP, 1,3-butadiene, carbon monoxide, formaldehyde, NNN and NNK (40). It is virtually inconceivable that a major reduction in their biomarker levels would not significantly impact cancer incidence in smokers.
Some fairly well known biomarkers are not included in Table 1. BaP-DNA and Hb adducts, 4-hydroxy-1-(3-pyridyl)-1-butanone (HPB) releasing DNA and Hb adducts, other PAH metabolites such as phenanthrene tetraol and hydroxyfluorenes, DNA adducts as determined by 32P postlabelling or immunoassay, and 3-ethyladenine in urine are examples. These have been omitted because they may require further validation, either analytically or with respect to tobacco use in large studies, or may provide similar information as those listed in Table 1.
Some Strengths and Limitations of Biomarkers
It is axiomatic that dose is related to risk in toxicology. In the setting of this perspective, toxicant and carcinogen dose are expected to be related to cancer risk. The key advantage of the biomarkers discussed here is that they are reliable metrics of dose in a person who uses tobacco products. This is evident from the studies listed in the Table, most of which find significantly higher levels of all biomarkers in the high risk group - smokers - compared to the low risk group - non-smokers.
Tobacco product use is highly complex. There are many different types of smoked and smokeless products and each has differing amounts of the carcinogens and toxicants listed in Table 1. These have been classically measured in cigarette smoke by machine smoking protocols. These protocols are useful for comparing different products under standard conditions, but they may fail when one tries to reproduce complex and varied human smoking conditions or relate machine measured values to cancer risk. These aspects are beyond the scope of this perspective, but have been discussed in detail in a recent review (41). Biomarkers have the potential to bypass these uncertainties and provide a realistic and direct assessment of carcinogen and toxicant dose in an individual. This is particularly true in cases such as nicotine equivalents where one is directly measuring most of the toxicant dose. But nicotine dose alone is not likely to be a good biomarker with respect to carcinogenic potential because cigarette smoke from different brands differs in the amounts of the other constituents in Table 1 when expressed per amount of nicotine (40). Thus, one large study found a strong relationship between nicotine equivalents and total NNAL (R2 = 0.5) and HPMA (R2 = 0.48), but only moderate or poor correlations with several other biomarkers including COHb, MHBMA, 1-HOP, and 4-ABP Hb adducts (42). Therefore, a panel of biomarkers selected from those in Table 1 likely will be necessary to obtain comprehensive and accurate information on toxicant and carcinogen dose.
The biomarkers listed in Table 1 measure different points in the continuum from exposure to internal dose to cellular effects. Nicotine equivalents, total NNAL, total NNN, 1-HOP, the mercapturic acids, and Cd in urine are all measures of exposure or dose, but to differing extents. Nicotine equivalents captures 73–96% of nicotine dose (9), total NNAL about 12 – 17% of NNK dose (43,44), and total NNN an estimated 1% of NNN dose (45). Similar data do not seem to be available for the mercapturic acids and Cd. The DNA and Hb adducts are biomarkers of internal dose, indicating how much material reaches a cellular target (DNA) or its surrogate (Hb). 8-epi-PGF2α and PGE-M are not directly related to cigarette smoke constituents but rather to their cellular effects, oxidative damage and inflammation. While it is often assumed that biomarkers further along the continuum from exposure to cellular effects would be more closely related to risk, that is not necessarily the case, and must be validated for each biomarker. For example, levels of the “exposure biomarkers” cotinine and total NNAL have been related to lung cancer risk in recent studies, discussed in more detail in the next section (46–48), but none of the other biomarkers discussed here have yet been validated with respect to cancer risk.
A limitation of the biomarker approach to estimation of dose is inter-individual differences in metabolism, particularly in cases where a nearly complete metabolite profile is not being obtained. An example is total NNAL. It is a measure of the metabolism of NNK by carbonyl reduction and glucuronidation. But it does not take into account the pathways of metabolic activation of NNK, which lead to different metabolites. Increased metabolic activation of NNK would presumably increase cancer risk but would decrease total NNAL levels thus blunting the effect of total NNAL as a risk biomarker. The solution to this problem is the use of a metabolic activation biomarker such as NNK-DNA adducts in conjunction with total NNAL. The effects of metabolism on some of the biomarkers listed in Table 1 require further investigation.
Potential Application of Biomarkers in Tobacco Product Regulation
The panel of biomarkers in Table 1, or perhaps a subset, should be used as part of a strategy to regulate tobacco products. The critical question is: what are the mean biomarker values below which one would see a decrease in tobacco-induced cancer? As an ultimate goal, we should aim for the levels observed in non-smokers, who are clearly at far lower risk for almost all tobacco-related cancers. But, recognizing that this is not likely to be feasible, one should set a realistic yet meaningful target level.
One approach to setting this target level is to carry out prospective epidemiologic studies, or “cohort” studies, of biomarkers and disease risk. In these studies, samples from healthy subjects are collected and stored, and demographic and lifestyle data are obtained using questionnaires. The subjects are then followed for years, and eventually cancers will occur in some of them. The stored samples from these subjects are retrieved, along with samples from appropriately matched controls without cancer, to form a “nested case-control” study. These samples can be analyzed for the biomarkers to determine their relationship to disease. The magnitude of the relationship to disease risk for each biomarker and/or their combinations can be evaluated using standard statistical analysis methods. Mean target biomarker levels related to minimal risk of disease could be established. Although there are certain limitations of this approach which have been discussed (49), such epidemiologic studies with prospective study design and objective measurements of biomarkers in bio-specimens would provide a direct link of the disease of interest to the biomarker and its parent compound. The relationship of tobacco carcinogen and toxicant biomarkers such as those discussed here to cancer has been examined in only limited prospective studies to date. Examples are cotinine and total NNAL with respect to lung cancer. In one prospective study, serum cotinine was related linearly to lung cancer risk, with no suggestion of a plateau at high exposure levels (46). Two recent molecular epidemiology studies related total NNAL to lung cancer risk. In one study, urinary levels of total NNAL were significantly associated with risk of lung cancer in a dose-dependent manner in smokers (48). Relative to the lowest tertile, risks associated with the second and third tertiles of total NNAL were 1.43 [95% CI, 0.86–2.37] and 2.11 (95% CI, 1.25–3.54], respectively (P for trend = 0.005) after adjustment for number of cigarettes per day, number of years of smoking, and total cotinine (cotinine plus its glucuronide). Smokers in the highest tertiles of urinary total NNAL and total cotinine exhibited an 8.5 fold increased risk for lung cancer relative to smokers in the lowest tertiles but otherwise comparable in smoking history. Based on this study, if urinary levels of both total NNAL and cotinine were reduced to the lowest third for all smokers, lung cancer incidence would have decreased by approximately three-fourths in smokers of the target population. Similar results were obtained using prospective measurements of total NNAL in serum, although no relationship with cotinine was seen (47). Further studies are needed to explore the relationship to cancer risk to total NNAL, nicotine equivalents, and the other biomarkers in Table 1. This is feasible because there are many ongoing prospective cancer epidemiology studies in the world, and analytical methods for the panel listed in Table 1 are for the most part amenable to large sample sizes.
Once the mean biomarker target levels have been established using approaches such as those just discussed, the next step would be to design a tobacco product that met those target levels. This tobacco product, a cigarette for example, would be tested using standard machine smoking methods to determine the level of each constituent that would correspond to each mean biomarker target level in the panel. Such testing would provide an approximation of the new product’s potential for reduced exposure. Then, clinical studies which included a representative sample of smokers would be carried out to determine whether those who used this product actually met the mean target biomarker levels. Furthermore, subsequent post-marketing epidemiologic studies would also be conducted to provide a broader assessment of the mean levels of biomarkers achieved by the product, and their relationship to cancer. The design of such studies is a science in itself and is beyond the scope of this perspective. Recent reviews discuss this subject comprehensively (50,51).
While measurements of cigarette “tar” and nicotine using smoking machines generally do not correlate well with biomarker levels in smokers (52–55), it should be possible to establish predictable relationships of individual cigarette smoke constituents and the desired mean biomarker levels, as measured by smoking machines under defined conditions. If this can be accomplished, then these constituent levels as determined on smoking machines could be used in a practical approach to regulation.
The suggested regulatory approach under the FCTC is more conservative than that discussed here (40). The WHO study group on tobacco regulation decided against the use of biomarkers in regulation because “distinguishing the differences in biomarker levels due to variations between products from the differences due to smoker behavior (e.g. who uses the product and how they use it), is a formidable scientific challenge.” The ultimate recommendation of the panel was to regulate based on levels of certain constituents as measured on smoking machines under the “intense smoking regimen” used by Health Canada, and expressed per mg nicotine, since smokers will adjust their pattern of smoking to obtain their desired dose of nicotine (40). The panel also took into account the number of cigarette brands that would be eliminated from the market by their proposed standards. This aspect is not considered here.
When “light cigarettes” began to appear on the market in the 1970s and were heralded by many, including some in the public health community as less harmful, biomarkers such as those discussed here were mainly unavailable. Cancer risk from smoking “light cigarettes” did not decrease, nor did most biomarkers (52–57), If these biomarkers had been available and applied at the time “light cigarettes” were introduced, then these cigarettes could not have been accepted as less harmful and large numbers of cancer deaths presumably could have been prevented.
In summary, the approach described here is comprised of 3 major steps: 1. set a panel of mean target biomarker levels based on molecular epidemiologic studies of biomarkers and cancer risk; 2. determine the product constituent levels that correspond to the mean target biomarker levels in the panel; and 3. regulate based on these determined constituent levels.
Application of Biomarkers in Cancer Prevention
Multiple epidemiologic studies, buttressed by tobacco carcinogen and biomarker studies – particularly cotinine and total NNAL- have established that secondhand smoke (SHS) causes immediate and long-term adverse health effects in non-smokers, including lung cancer and heart disease (58). Exposure occurs mainly in homes and workplaces (6). These facts have spurred legislation which has had a major impact on tobacco control. In one recent survey of 11 states, most people reported having smoke-free home rules (6). Anti-tobacco legislation, such as clean air statutes that make indoor public places and worksites completely smoke-free are now law in 21 states of the U.S. and the District of Columbia (6). These positive developments, which are still in progress, would have been unimaginable in the 1980s when the first studies demonstrating the presence of cotinine in the serum and urine of non-smokers exposed to SHS were published (59–61). According to the National Health and Nutrition Examination Survey (NHANES) study, the percentage of non-smokers aged >4 years in the U.S. with detectable serum cotinine declined from 83.9% in 1988 to 46.4% in 1999–2004 (6,62). The specificity of cotinine as a biomarker of nicotine exposure is the obvious strength of these studies. Cotinine and nicotine are however not carcinogenic. Total NNAL emerged in the 1990s as a biomarker of SHS exposure with impact because it is not only tobacco-specific but also represents uptake of NNK, a lung carcinogen (10,63). An additional advantage of total NNAL is its relatively long elimination half-life of up to 40–45 days compared to 3 days for cotinine (64,65). Thus, cotinine and total NNAL have played a significant role in establishing secondhand smoke as a cause of disease, thus providing impetus for smoke free legislation, which has been important in decreasing cigarette smoking in the U.S., resulting in a steady decline in lung cancer mortality (66).
Although smoking causes up to 90% of lung cancer, about 11–24% of smokers will get lung cancer, and presently there is no way to reliably identify which user is susceptible (4). Tobacco carcinogen and toxicant biomarkers have the potential to identify those smokers at highest risk for cancer, but have yet to be applied for this purpose. Susceptibility must be related, at least in part, to carcinogen dose and processing (e.g. extent of metabolic activation, DNA adduct formation, and repair). Several recent studies have described approaches to the development of a risk prediction model for lung cancer, and these have been summarized (67). Variables in these models include mainly traditional epidemiologic parameters such as family history of cancer, smoking history, dust exposure, prior respiratory disease, and others (68–70). One recent model also includes host DNA repair capacity (67). The results to date are modest with respect to prediction of lung cancer susceptibility. The inclusion of traditional smoking data such as pack-years of smoking detracts from the utility of such models, as it necessarily makes them retrospective in nature. Being able to predict lung cancer susceptibility in a young person who has just embarked on a regular pattern of smoking would be potentially much more powerful in cancer prevention. Biomarker measurements in these young smokers could perhaps provide a risk profile, thus leading to targeted smoking cessation intervention. What is needed are further prospective molecular epidemiology studies of the type discussed earlier in order to establish a panel of biomarker levels demonstrably related to cancer incidence in smokers.
It seems likely that genetic polymorphism data ultimately will be included along with biomarkers in a tobacco and cancer risk algorithm. Many individual gene candidate studies have been carried out examining polymorphisms and cancer susceptibility in smokers, but to date with the possible exception of polymorphisms in cytochrome P4501A1 and glutathione transferases, the results have been generally quite modest (71,72). Genome wide association studies in contrast have identified a locus at 15q24/15q25.1 which includes the nicotinic acetylcholine receptor A subunits 3 and 5 (CHRNA3 and CHRNA5) genes associated with lung cancer (73–75). Our biomarker data demonstrated that carriers of these variants extract a greater amount of nicotine and have higher levels of total NNAL per cigarette than non-carriers (76). In this case, a combination of genotyping and biomarker studies provided mechanistic insight. The power of current genomic sequencing techniques argues for the potential inclusion of genetic data together with tobacco carcinogen and toxicant biomarker data in a predictive algorithm for cancer in tobacco users.
Conclusions
The use of tobacco carcinogen and toxicant biomarkers has expanded rapidly in recent years and large amounts of new data are available. Sensitive, quantitative, and reliable analytical methods, mainly using mass spectrometry, are now available for assessment of these biomarkers, which are almost uniformly elevated in smokers. The methods are now sufficiently routine that their application in large studies is feasible, and this has been demonstrated for many of the biomarkers in the panel. The biomarkers can assess dose or dose plus metabolic processing, factors demonstrably related to risk, in people who use tobacco products. Therefore, they have great potential in tobacco product regulation and in the identification of individuals at high risk for cancer upon exposure to tobacco products.
Acknowledgements
Our studies on tobacco carcinogen and toxicant biomarkers are supported by grants CA-81301, CA-85702, CA-92025, CA-129534, DA-13333 and ES-11297, and contract NO1-CP-64402 from the National Institutes of Health. We thank Bob Carlson for outstanding editorial assistance.
References
- 1.Shafey O, Eriksen MP, Ross H, Mackay J. The Tobacco Atlas. 3rd Edition. Atlanta, GA: American Cancer Society and World Lung Foundation; 2009. [Google Scholar]
- 2.Boyle P, Levin P. Lyon, FR: IARC; World Cancer Report. 2004;2008
- 3.Secretan B, Straif K, Baan R, Grosse Y, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V. A review of human carcinogens--Part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol. 2009;10:1033–1034. doi: 10.1016/s1470-2045(09)70326-2. [DOI] [PubMed] [Google Scholar]
- 4.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 83. Lyon, FR: IARC; 2004. Tobacco Smoke and Involuntary Smoking; pp. 53–1187. [PMC free article] [PubMed] [Google Scholar]
- 5.President's Cancer Panel 2007–2008 Annual Report. 2009 http://deainfo.nci.nih.gov/advisory/pcp/pcp.htm.
- 6.State-specific secondhand smoke exposure and current cigarette smoking among adults - United States, 2008. MMWR Morb. Mortal. Wkly. Rep. 2009;58:1232–1235. [PubMed] [Google Scholar]
- 7.Hatsukami DK, Benowitz NL, Rennard SI, Oncken C, Hecht SS. Biomarkers to assess the utility of potential reduced exposure tobacco products. Nicotine and Tob. Res. 2006;8:600–622. doi: 10.1080/14622200600858166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S.Department of Health and Human Services. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health; The Health Consequences of Smoking: A Report of the Surgeon General. 2004
- 9.Hukkanen J, Jacob P, III, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacol. Rev. 2005;57:79–115. doi: 10.1124/pr.57.1.3. [DOI] [PubMed] [Google Scholar]
- 10.Hecht SS. Progress and challenges in selected areas of tobacco carcinogenesis. Chem. Res. Toxicol. 2008;21:160–171. doi: 10.1021/tx7002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 89. Lyon, FR: IARC; 2007. Smokeless tobacco and tobacco-specific nitrosamines; pp. 421–583. [PMC free article] [PubMed] [Google Scholar]
- 12.Hecht SS. Biochemistry, biology, and carcinogenicity of tobacco-specific N-nitrosamines. Chem. Res. Toxicol. 1998;11:559–603. doi: 10.1021/tx980005y. [DOI] [PubMed] [Google Scholar]
- 13.Stepanov I, Carmella SG, Briggs A, Hertsgaard L, Lindgren B, Hatsukami DK, Hecht SS. Presence of the carcinogen N'-nitrosonornicotine in the urine of some users of oral nicotine replacement therapy products. Cancer Res. 2009;69:8236–8240. doi: 10.1158/0008-5472.CAN-09-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen AM, Mathiesen L, Pedersen M, Knudsen LE. Urinary 1-hydroxypyrene (1-HP) in environmental and occupational studies--a review. Int J Hyg. Environ. Health. 2008;211:471–503. doi: 10.1016/j.ijheh.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Dipple A, Moschel RC, Bigger CAH. Polynuclear aromatic hydrocarbons. In: Searle CE, editor. Chemical Carcinogens, Second Edition, ACS Monograph 182. vol. 1. Washington, D.C: American Chemical Society; 1984. pp. 41–163. [Google Scholar]
- 16.Carmella SG, Chen M, Han S, Briggs A, Jensen J, Hatsukami DK, Hecht SS. Effects of smoking cessation on eight urinary tobacco carcinogen and toxicant biomarkers. Chem Res Toxicol. 2009;22:734–741. doi: 10.1021/tx800479s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S.Department of Health and Human Services. Report on Carcinogens. Research Triangle Park, N.C: 2004:III-37–III-39.
- 18.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 97. Lyon, FR: IARC; 2008. 1,3-Butadiene, ethylene oxide and vinyl halides (vinyl fluoride, vinyl chloride and vinyl bromide) pp. 45–309. [PMC free article] [PubMed] [Google Scholar]
- 19.U.S.Department of Health and Human Services. Report on Carcinogens. Research Triangle Park, N.C: 2004:III-26–III-28.
- 20.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 63. Lyon, FR: IARC; 1995. Acrolein; pp. 337–391. [Google Scholar]
- 21.Thompson CA, Burcham PC. Genome-wide transcriptional responses to acrolein. Chem. Res. Toxicol. 2008;21:2245–2256. doi: 10.1021/tx8001934. [DOI] [PubMed] [Google Scholar]
- 22.Chung FL, Zhang L, Ocando JE, Nath RG. Role of 1,N2-propanodeoxyguanosine adducts as endogenous DNA lesions in rodents and humans. In: Singer B, Bartsch H, editors. Exocyclic DNA Adducts in Mutagenesis and Carcinogenesis. Lyon, France: International Agency for Research on Cancer; 1999. pp. 45–54. [Google Scholar]
- 23.Feng Z, Hu W, Hu Y, Tang M-S. Acrolein is a major cigarette-related lung cancer agent. Preferential binding at p53 mutational hotspots and inhibition of DNA repair. Proc. Natl. Acad. Sci. USA. 2006;103:15404–15409. doi: 10.1073/pnas.0607031103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.U.S.Department of Health and Human Services. Report on Carcinogens. Research Triangle Park, N.C: 2004:III-42–III-44.
- 25.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 58. Lyon, FR: IARC; 1999. Beryllium, cadmium, mercury, and exposures in the glass manufacturing industry; pp. 119–237. [PMC free article] [PubMed] [Google Scholar]
- 26.Morrow JD. Quantification of isoprostanes as indices of oxidant stress and the risk of atherosclerosis in humans. Arterioscler. Thromb. Vasc. Biol. 2005;25:279–286. doi: 10.1161/01.ATV.0000152605.64964.c0. [DOI] [PubMed] [Google Scholar]
- 27.Gross ND, Boyle JO, Morrow JD, Williams MK, Moskowitz CS, Subbaramaiah K, Dannenberg AJ, Duffield-Lillico AJ. Levels of prostaglandin E metabolite, the major urinary metabolite of prostaglandin E2, are increased in smokers. Clin Cancer Res. 2005;11:6087–6093. doi: 10.1158/1078-0432.CCR-05-0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.U.S.Department of Health and Human Services. Report on Carcinogens. Research Triangle Park, N.C: 2004:III-6–III-8.
- 29.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 71. Lyon, FR: IARC; 1999. Re-evaluation of some organic chemicals, hydrazine and hydrogen peroxide (part one) pp. 43–108. [PMC free article] [PubMed] [Google Scholar]
- 30.Klaunig JE. Acrylamide carcinogenicity. J Agric. Food Chem. 2008;56:5984–5988. doi: 10.1021/jf8004492. [DOI] [PubMed] [Google Scholar]
- 31.International Agency for Research on Cancer. IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Lyon, France: International Agency for Research on Cancer; 1987. pp. 91–122. [Google Scholar]
- 32.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 88. Lyon, FR: IARC; 2006. Formaldehyde, 2-butoxyethanol and 1-tert-butoxypropan-2-ol; pp. 37–325. [PMC free article] [PubMed] [Google Scholar]
- 33.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. vol. 71. Lyon, FR: IARC; 1999. Re-evaluation of some organic chemicals, hydrazine and hydrogen peroxide (part two) pp. 319–335. [PMC free article] [PubMed] [Google Scholar]
- 34.Scherer G. Carboxyhemoglobin and thiocyanate as biomarkers of exposure to carbon monoxide and hydrogen cyanide in tobacco smoke. Exp. Toxicol. Pathol. 2006;58:101–124. doi: 10.1016/j.etp.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Straif K, Baan R, Grosse Y, Secretan B, El Ghissassi F, Cogliano V. Carcinogenicity of polycyclic aromatic hydrocarbons. Lancet. Oncol. 2005;6:931–932. doi: 10.1016/s1470-2045(05)70458-7. [DOI] [PubMed] [Google Scholar]
- 36.Hecht SS. Tobacco smoke carcinogens and lung cancer. J. Natl. Cancer Inst. 1999;91:1194–1210. doi: 10.1093/jnci/91.14.1194. [DOI] [PubMed] [Google Scholar]
- 37.Hecht SS. Tobacco carcinogens, their biomarkers, and tobacco-induced cancer. Nature Rev. Cancer. 2003;3:733–744. doi: 10.1038/nrc1190. [DOI] [PubMed] [Google Scholar]
- 38.Hecht SS. Tobacco smoke carcinogens and lung cancer. In: Penning TM, editor. Chemical Carcinogenesis. Springer: 2010. [Google Scholar]
- 39.Rodgman A, Perfetti T. The Chemical Components of Tobacco and Tobacco Smoke. Boca Raton, FL: CRC Press; 2009. pp. 1483–1784. [Google Scholar]
- 40.Burns DM, Dybing E, Gray N, Hecht S, Anderson C, Sanner T, O'Connor R, Djordjevic M, Dresler C, Hainaut P, Jarvis M, Opperhuizen A, Straif K. Mandated lowering of toxicants in cigarette smoke: a description of the World Health Organization TobReg proposal. Tob. Control. 2008;17:132–141. doi: 10.1136/tc.2007.024158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marian C, O'Connor RJ, Djordjevic MV, Rees VW, Hatsukami DK, Shields PG. Reconciling human smoking behavior and machine smoking patterns: implications for understanding smoking behavior and the impact on laboratory studies. Cancer Epidemiol Biomarkers Prev. 2009;18:3305–3320. doi: 10.1158/1055-9965.EPI-09-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roethig HJ, Munjal S, Feng S, Liang Q, Sarkar M, Walk RA, Mendes PE. Population estimates for biomarkers of exposure to cigarette smoke in adult U.S. cigarette smokers. Nicotine Tob Res. 2009;11:1216–1225. doi: 10.1093/ntr/ntp126. [DOI] [PubMed] [Google Scholar]
- 43.Stepanov I, Upadhyaya P, Feuer R, Jensen J, Hatsukami DK, Hecht SS. Extensive metabolic activation of the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in smokers. Cancer Epidemiol. Biomarkers & Prev. 2008;17:1764–1773. doi: 10.1158/1055-9965.EPI-07-2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hecht SS, Carmella SG, Stepanov I, Jensen J, Anderson A, Hatsukami DK. Metabolism of the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone to its biomarker total NNAL in smokeless tobacco users. Cancer Epidemiol. Biomarkers Prev. 2008;17:732–735. doi: 10.1158/1055-9965.EPI-07-2843. [DOI] [PubMed] [Google Scholar]
- 45.Urban M, Scherer G, Kavvadias D, Hagedorn HW, Feng S, Serafin R, Kapur S, Muhammad R, Jin Y, Mendes P, Roethig H. Quantitation of N'-nitrosonornicotine (NNN) in smokers' urine by liquid chromatography-tandem mass spectrometry. J Anal. Toxicol. 2009;33:260–265. doi: 10.1093/jat/33.5.260. [DOI] [PubMed] [Google Scholar]
- 46.Boffetta P, Clark S, Shen M, Gislefoss R, Peto R, Andersen A. Serum cotinine level as predictor of lung cancer risk. Cancer Epidemiol. Biomarkers & Prev. 2006;15:1184–1188. doi: 10.1158/1055-9965.EPI-06-0032. [DOI] [PubMed] [Google Scholar]
- 47.Church TR, Anderson KE, Caporaso NE, Geisser MS, Le C, Zhang Y, Benoit AR, Carmella SG, Hecht SS. A prospectively measured serum biomarker for a tobacco-specific carcinogen and lung cancer in smokers. Cancer Epidemiol. Biomarkers & Prev. 2009;18:260–266. doi: 10.1158/1055-9965.EPI-08-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yuan JM, Koh WP, Murphy SE, Fan Y, Wang R, Carmella SG, Han S, Wickham K, Gao YT, Yu MC, Hecht SS. Urinary levels of tobacco-specific nitrosamine metabolites in relation to lung cancer development in two prospective cohorts of cigarette smokers. Cancer Res. 2009;69:2990–2995. doi: 10.1158/0008-5472.CAN-08-4330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rundle A, Ahsan H. Molecular epidemiological studies that can be nested within cohorts. In: Wild C, Vineis P, Garte S, editors. Molecular Epidemiology of Chronic Diseases. J.W. Wiley; 2008. pp. 23–37. [Google Scholar]
- 50.Hatsukami DK, Hanson K, Briggs A, Parascandola M, Genkinger JM, O'Connor R, Shields PG. Clinical trials methods for evaluation of potential reduced exposure products. Cancer Epidemiol Biomarkers Prev. 2009;18:3143–3195. doi: 10.1158/1055-9965.EPI-09-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O'Connor RJ, Cummings KM, Rees VW, Connolly GN, Norton KJ, Sweanor D, Parascandola M, Hatsukami DK, Shields PG. Surveillance methods for identifying, characterizing, and monitoring tobacco products: potential reduced exposure products as an example. Cancer Epidemiol Biomarkers Prev. 2009;18:3334–3348. doi: 10.1158/1055-9965.EPI-09-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scherer G, Engl J, Urban M, Gilch G, Janket D, Riedel K. Relationship between machine-derived smoke yields and biomarkers in cigarette smokers in Germany. Regul. Toxicol. Pharmacol. 2007;47:171–183. doi: 10.1016/j.yrtph.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 53.Hecht SS, Murphy SE, Carmella SG, Li S, Jensen J, Le C, Joseph AM, Hatsukami DK. Similar uptake of lung carcinogens by smokers of regular, light, and ultra-light cigarettes. Cancer Epidemiol. Biomarkers & Prev. 2005;14:693–698. doi: 10.1158/1055-9965.EPI-04-0542. [DOI] [PubMed] [Google Scholar]
- 54.Bernert JT, Jain RB, Pirkle JL, Wang L, Miller BB, Sampson EJ. Urinary tobacco-specific nitrosamines and 4-aminobiphenyl hemoglobin adducts measured in smokers of either regular or light cigarettes. Nicotine. Tob. Res. 2005;7:729–738. doi: 10.1080/14622200500259762. [DOI] [PubMed] [Google Scholar]
- 55.Benowitz NL, Jacob P, III, Bernert JT, Wilson M, Wang L, Allen F, Dempsey D. Carcinogen exposure during short-term switching from regular to "light" cigarettes. Cancer Epidemiol. Biomarkers & Prev. 2005;14:1376–1383. doi: 10.1158/1055-9965.EPI-04-0667. [DOI] [PubMed] [Google Scholar]
- 56.Benowitz NL, Burns DM. Smoking and Tobacco Control Monograph No. 13. Risks Associated with Smoking Cigarettes with Low Machine-Measured Yields of Tar and Nicotine. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2001. Public health implications of changes in cigarette design and marketing; pp. 1–12. [Google Scholar]
- 57.Harris JE, Thun MJ, Mondul AM, Calle EE. Cigarette tar yields in relation to mortality from lung cancer in the cancer prevention study II prospective cohort, 1982–8. BMJ. 2004;328:72. doi: 10.1136/bmj.37936.585382.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.U.S.Department of Health and Human Services. Washington, D.C: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health; The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. 2006
- 59.Lee PN. Uses and abuses of cotinine as a marker of tobacco smoke exposure. In: Gorrod JW, Jacob P III, editors. Analytical Determination of Nicotine and Related Compounds and Their Metabolites. Amsterdam: Elsevier; 1999. pp. 669–719. [Google Scholar]
- 60.Jenkins RA, Guerin MR, Tomkins BA. The Chemistry of Environmental Tobacco Smoke: Composition and Measurement. Second Edition. Boca Raton, FL: Lewis Publishers; 2000. pp. 173–214. [Google Scholar]
- 61.International Agency for Research on Cancer. IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. vol. 38. Lyon, FR: IARC; 1986. Tobacco Smoking; pp. 37–375. [Google Scholar]
- 62.Disparities in secondhand smoke exposure--United States, 1988–1994 and 1999–2004. MMWR Morb. Mortal. Wkly. Rep. 2008;57:744–747. [PubMed] [Google Scholar]
- 63.Hecht SS, Carmella SG, Murphy SE, Akerkar S, Brunnemann KD, Hoffmann D. A tobacco-specific lung carcinogen in the urine of men exposed to cigarette smoke. N. Engl. J. Med. 1993;329:1543–1546. doi: 10.1056/NEJM199311183292105. [DOI] [PubMed] [Google Scholar]
- 64.Hecht SS, Carmella SG, Chen M, Koch JFD, Miller AT, Murphy SE, Jensen JA, Zimmerman CL, Hatsukami DK. Quantitation of urinary metabolites of a tobacco-specific lung carcinogen after smoking cessation. Cancer Res. 1999;59:590–596. [PubMed] [Google Scholar]
- 65.Goniewicz ML, Havel CM, Peng MW, Jacob P, III, Dempsey D, Yu L, Zielinska-Danch W, Koszowski B, Czogala J, Sobczak A, Benowitz NL. Elimination kinetics of the tobacco-specific biomarker and lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol. Cancer Epidemiol Biomarkers Prev. 2009;18:3421–3425. doi: 10.1158/1055-9965.EPI-09-0874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Cancer Institute. SEER Program SEER*Stat Database. 2009 www.seer.cancer.gov/faststats.
- 67.Spitz MR, Etzel CJ, Dong Q, Amos CI, Wei Q, Wu X, Hong WK. An expanded risk prediction model for lung cancer. Cancer Prev Res (Phila Pa) 2008;1:250–254. doi: 10.1158/1940-6207.CAPR-08-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Spitz MR, Hong WK, Amos CI, Wu X, Schabath MB, Dong Q, Shete S, Etzel CJ. A risk model for prediction of lung cancer. J. Natl. Cancer Inst. 2007;99:715–726. doi: 10.1093/jnci/djk153. [DOI] [PubMed] [Google Scholar]
- 69.Bach PB, Kattan MW, Thornquist MD, Kris MG, Tate RC, Barnett MJ, Hsieh LJ, Begg CB. Variations in lung cancer risk among smokers. J. Natl. Cancer Inst. 2003;95:470–478. doi: 10.1093/jnci/95.6.470. [DOI] [PubMed] [Google Scholar]
- 70.Cassidy A, Myles JP, van Tongeren M, Page RD, Liloglou T, Duffy SW, Field JK. The LLP risk model: an individual risk prediction model for lung cancer. Br. J. Cancer. 2008;98:270–276. doi: 10.1038/sj.bjc.6604158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carlsten C, Sagoo GS, Frodsham AJ, Burke W, Higgins JP. Glutathione S-transferase M1 (GSTM1) polymorphisms and lung cancer: a literature-based systematic HuGE review and meta-analysis. Am J Epidemiol. 2008;167:759–774. doi: 10.1093/aje/kwm383. [DOI] [PubMed] [Google Scholar]
- 72.Vineis P, Veglia F, Benhamou S, Butkiewicz D, Cascorbi I, Clapper ML, Dolzan V, Haugen A, Hirvonen A, Ingelman-Sundberg M, Kihara M, Kiyohara C, Kremers P, Le Marchand L, Ohshima S, Pastorelli R, Rannug A, Romkes M, Schoket B, Shields P, Strange RC, Stucker I, Sugimura H, Garte S, Gaspari L, Taioli E. CYP1A1 T3801 C polymorphism and lung cancer: a pooled analysis of 2,451 cases and 3,358 controls. Int. J. Cancer. 2003;104:650–657. doi: 10.1002/ijc.10995. [DOI] [PubMed] [Google Scholar]
- 73.Thorgeirsson TE, Geller F, Sulem P, Rafnar T, Wiste A, Magnusson KP, Manolescu A, Thorleifsson G, Stefansson H, Ingason A, Stacey SN, Bergthorsson JT, Thorlacius S, Gudmundsson J, Jonsson T, Jakobsdottir M, Saemundsdottir J, Olafsdottir O, Gudmundsson LJ, Bjornsdottir G, Kristjansson K, Skuladottir H, Isaksson HJ, Gudbjartsson T, Jones GT, Mueller T, Gottsater A, Flex A, Aben KK, de Vegt F, Mulders PF, Isla D, Vidal MJ, Asin L, Saez B, Murillo L, Blondal T, Kolbeinsson H, Stefansson JG, Hansdottir I, Runarsdottir V, Pola R, Lindblad B, van Rij AM, Dieplinger B, Haltmayer M, Mayordomo JI, Kiemeney LA, Matthiasson SE, Oskarsson H, Tyrfingsson T, Gudbjartsson DF, Gulcher JR, Jonsson S, Thorsteinsdottir U, Kong A, Stefansson K. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452:638–642. doi: 10.1038/nature06846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Amos CI, Wu X, Broderick P, Gorlov IP, Gu J, Eisen T, Dong Q, Zhang Q, Gu X, Vijayakrishnan J, Sullivan K, Matakidou A, Wang Y, Mills G, Doheny K, Tsai YY, Chen WV, Shete S, Spitz MR, Houlston RS. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat. Genet. 2008;40:616–622. doi: 10.1038/ng.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hung RJ, McKay JD, Gaborieau V, Boffetta P, Hashibe M, Zaridze D, Mukeria A, Szeszenia-Dabrowska N, Lissowska J, Rudnai P, Fabianova E, Mates D, Bencko V, Foretova L, Janout V, Chen C, Goodman G, Field JK, Liloglou T, Xinarianos G, Cassidy A, McLaughlin J, Liu G, Narod S, Krokan HE, Skorpen F, Elvestad MB, Hveem K, Vatten L, Linseisen J, Clavel-Chapelon F, Vineis P, Bueno-de-Mesquita HB, Lund E, Martinez C, Bingham S, Rasmuson T, Hainaut P, Riboli E, Ahrens W, Benhamou S, Lagiou P, Trichopoulos D, Holcatova I, Merletti F, Kjaerheim K, Agudo A, Macfarlane G, Talamini R, Simonato L, Lowry R, Conway DI, Znaor A, Healy C, Zelenika D, Boland A, Delepine M, Foglio M, Lechner D, Matsuda F, Blanche H, Gut I, Heath S, Lathrop M, Brennan P. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature. 2008;452:633–637. doi: 10.1038/nature06885. [DOI] [PubMed] [Google Scholar]
- 76.Le Marchand L, Derby KS, Murphy SE, Hecht SS, Hatsukami D, Carmella SG, Tiirikainen M, Wang H. Smokers with the CHRNA lung cancer-associated variants are exposed to higher levels of nicotine equivalents and a carcinogenic tobacco-specific nitrosamine. Cancer Res. 2008;68:9137–9140. doi: 10.1158/0008-5472.CAN-08-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zedler BK, Kinser R, Oey J, Nelson B, Roethig HJ, Walk RA, Kuhl P, Rustemeier K, Schepers G, Von Holt K, Tricker AR. Biomarkers of exposure and potential harm in adult smokers of 3–7 mg tar yield (Federal Trade Commission) cigarettes and in adult non-smokers. Biomarkers. 2006;11:201–220. doi: 10.1080/13547500600576260. [DOI] [PubMed] [Google Scholar]
- 78.Scherer G, Urban M, Engl J, Hagedorn HW, Riedel K. Influence of smoking charcoal filter tipped cigarettes on various biomarkers of exposure. Inhal. Toxicol. 2006;18:821–829. doi: 10.1080/08958370600747945. [DOI] [PubMed] [Google Scholar]
- 79.Mendes P, Kapur S, Wang J, Feng S, Roethig H. A randomized, controlled exposure study in adult smokers of full flavor Marlboro cigarettes switching to Marlboro Lights or Marlboro Ultra Lights cigarettes. Regul. Toxicol Pharmacol. 2008;51:295–305. doi: 10.1016/j.yrtph.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 80.Roethig HJ, Zedler BK, Kinser RD, Feng S, Nelson BL, Liang Q. Short-term clinical exposure evaluation of a second-generation electrically heated cigarette smoking system. J. Clin. Pharmacol. 2007;47:518–530. doi: 10.1177/0091270006297686. [DOI] [PubMed] [Google Scholar]
- 81.Lowe FJ, Gregg EO, McEwan M. Evaluation of biomarkers of exposure and potential harm in smokers, former smokers and never-smokers. Clin Chem Lab Med. 2009;47:311–320. doi: 10.1515/CCLM.2009.069. [DOI] [PubMed] [Google Scholar]
- 82.Sarkar M, Kapur S, Frost-Pineda K, Feng S, Wang J, Liang Q, Roethig H. Evaluation of biomarkers of exposure to selected cigarette smoke constituents in adult smokers switched to carbon-filtered cigarettes in short-term and long-term clinical studies. Nicotine Tob Res. 2008;10:1761–1772. doi: 10.1080/14622200802443718. [DOI] [PubMed] [Google Scholar]
- 83.Stepanov I, Hecht SS. Tobacco-specific nitrosamines and their N-glucuronides in the urine of smokers and smokeless tobacco users. Cancer Epidemiol. Biomarkers & Prev. 2005;14:885–891. doi: 10.1158/1055-9965.EPI-04-0753. [DOI] [PubMed] [Google Scholar]
- 84.Kavvadias D, Scherer G, Urban M, Cheung F, Errington G, Shepperd J, McEwan M. Simultaneous determination of four tobacco-specific N-nitrosamines (TSNA) in human urine. J Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2009;877:1185–1192. doi: 10.1016/j.jchromb.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 85.Melikian AA, Djordjevic MV, Chen S, Richie J, Jr, Stellman SD. Effect of delivered dosage of cigarette smoke toxins on the levels of urinary biomarkers of exposure. Cancer Epidemiol Biomarkers Prev. 2007;16:1408–1415. doi: 10.1158/1055-9965.EPI-06-1097. [DOI] [PubMed] [Google Scholar]
- 86.Kavvadias D, Scherer G, Cheung F, Errington G, Shepperd J, McEwan M. Determination of tobacco-specific N-nitrosamines in urine of smokers and nonsmokers. Biomarkers. 2009;14:547–553. doi: 10.3109/13547500903242883. [DOI] [PubMed] [Google Scholar]
- 87.Feng S, Roethig HJ, Liang Q, Kinser R, Jin Y, Scherer G, Urban M, Engl J, Riedel K. Evaluation of urinary 1-hydroxypyrene, S-phenylmercapturic acid, trans,trans-muconic acid, 3-methyladenine, 3-ethyladenine, 8-hydroxy-2'-deoxyguanosine and thioethers as biomarkers of exposure to cigarette smoke. Biomarkers. 2006;11:28–52. doi: 10.1080/13547500500399730. [DOI] [PubMed] [Google Scholar]
- 88.Suwan-ampai P, Navas-Acien A, Strickland PT, Agnew J. Involuntary tobacco smoke exposure and urinary levels of polycyclic aromatic hydrocarbons in the United States, 1999 to 2002. Cancer Epidemiol Biomarkers Prev. 2009;18:884–893. doi: 10.1158/1055-9965.EPI-08-0939. [DOI] [PubMed] [Google Scholar]
- 89.Ding YS, Blount BC, Valentin-Blasini L, Applewhite HS, Xia Y, Watson CH, Ashley DL. Simultaneous determination of six mercapturic acid metabolites of volatile organic compounds in human urine. Chem Res Toxicol. 2009;22:1018–1025. doi: 10.1021/tx800468w. [DOI] [PubMed] [Google Scholar]
- 90.Scherer G, Urban M, Hagedorn HW, Feng S, Kinser RD, Sarkar M, Liang Q, Roethig HJ. Determination of two mercapturic acids related to crotonaldehyde in human urine: influence of smoking. Hum Exp Toxicol. 2007;26:37–47. doi: 10.1177/0960327107073829. [DOI] [PubMed] [Google Scholar]
- 91.Hoffmann K, Becker K, Friedrich C, Helm D, Krause C, Seifert B. The German Environmental Survey 1990/1992 (GerES II): cadmium in blood, urine and hair of adults and children. J. Expo. Anal. Environ. Epidemiol. 2000;10:126–135. doi: 10.1038/sj.jea.7500081. [DOI] [PubMed] [Google Scholar]
- 92.Paschal DC, Burt V, Caudill SP, Gunter EW, Pirkle JL, Sampson EJ, Miller DT, Jackson RJ. Exposure of the U.S. population aged 6 years and older to cadmium: 1988– 1994. Arch. Environ. Contam. Toxicol. 2000;38:377–383. doi: 10.1007/s002449910050. [DOI] [PubMed] [Google Scholar]
- 93.Batariova A, Spevackova V, Benes B, Cejchanova M, Smid J, Cerna M. Blood and urine levels of Pb, Cd and Hg in the general population of the Czech Republic and proposed reference values. Int J Hyg. Environ. Health. 2006;209:359–366. doi: 10.1016/j.ijheh.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 94.McElroy JA, Shafer MM, Trentham-Dietz A, Hampton JM, Newcomb PA. Urinary cadmium levels and tobacco smoke exposure in women age 20–69 years in the United States. J Toxicol Environ. Health A. 2007;70:1779–1782. doi: 10.1080/15287390600754953. [DOI] [PubMed] [Google Scholar]
- 95.Reilly M, Delanty N, Lawson JA, Fitzgerald GA. Modulation of oxidant stress in vivo in chronic cigarette smokers. Circulation. 1996;94:19–25. doi: 10.1161/01.cir.94.1.19. [DOI] [PubMed] [Google Scholar]
- 96.Pilz H, Oguogho A, Chehne F, Lupattelli G, Palumbo B, Sinzinger H. Quitting cigarette smoking results in a fast improvement of in vivo oxidation injury (determined via plasma, serum and urinary isoprostane) Thromb. Res. 2000;99:209–221. doi: 10.1016/s0049-3848(00)00249-8. [DOI] [PubMed] [Google Scholar]
- 97.Yan W, Byrd GD, Ogden MW. Quantitation of isoprostane isomers in human urine from smokers and nonsmokers by LC-MS/MS. J Lipid Res. 2007;48:1607–1617. doi: 10.1194/jlr.M700097-JLR200. [DOI] [PubMed] [Google Scholar]
- 98.Duffield-Lillico AJ, Boyle JO, Zhou XK, Ghosh A, Butala GS, Subbaramaiah K, Newman RA, Morrow JD, Milne GL, Dannenberg AJ. Levels of prostaglandin E metabolite and leukotriene E(4) are increased in the urine of smokers: evidence that celecoxib shunts arachidonic acid into the 5-lipoxygenase pathway. Cancer Prev Res (Phila Pa) 2009;2:322–329. doi: 10.1158/1940-6207.CAPR-09-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Scherer G. Biomonitoring of inhaled complex mixtures--ambient air, diesel exhaust and cigarette smoke. Exp Toxicol. Pathol. 2005;57 Suppl 1:75–110. doi: 10.1016/j.etp.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 100.Wang M, Cheng G, Balbo S, Carmella SG, Villalta PW, Hecht SS. Clear differences in levels of a formaldehyde-DNA adduct in leukocytes of smokers and non-smokers. Cancer Res. 2009;69:7170–7174. doi: 10.1158/0008-5472.CAN-09-1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen L, Wang M, Villalta PW, Luo X, Feuer R, Jensen J, Hatsukami DK, Hecht SS. Quantitation of an acetaldehyde adduct in human leukocyte DNA and the effect of smoking cessation. Chem. Res. Toxicol. 2007;20:108–113. doi: 10.1021/tx060232x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Scherer G, Richter E. Biomonitoring exposure to environmental tobacco smoke (ETS): a critical reappraisal. Hum. Exp. Toxicol. 1997;16:449–459. doi: 10.1177/096032719701600806. [DOI] [PubMed] [Google Scholar]
- 103.Hecht SS. Carcinogen derived biomarkers: applications in studies of human exposure to secondhand tobacco smoke. Tob. Control. 2003;13 Suppl 1:i48–i56. doi: 10.1136/tc.2002.002816. [DOI] [PMC free article] [PubMed] [Google Scholar]