Summary
Objective
Leptin is associated with blood pressure (BP) in experimental and cross-sectional studies, but only one previous prospective study of middle-aged men has reported the association between leptin and incident hypertension. We examined the association of leptin levels with incident hypertension in a population-based study of older men and women.
Design
Longitudinal cohort study
Population
Participants were 602 community-dwelling older adults with normal baseline BP levels who attended a research clinic visit between 1984 and 1987 and again 4.4 years later (mean age was 66.2±11.4; 60.6% were men; mean BMI 24.9±3.4 kg/m2).
Measurements
Hypertension was defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg and/or antihypertensive drug treatment. Leptin was measured by radioimmunoassay.
Results
After an average 4.4-year follow up (minimum 2 – maximum 7 years), 106 (17.6%) new cases of hypertension were identified. At baseline, participants who developed hypertension were older, and had higher systolic BP and higher total cholesterol compared to participants who remained normotensive. Baseline serum leptin levels were higher in participants who developed hypertension compared to persistent normotensives [median (25th – 75th range)] [8.8(5-16) vs. 7(4-11) ng/mL, P=0.002]. In logistic regression models, leptin (log-transformed) predicted incident hypertension before and after adjustments for baseline age, BMI, systolic BP, total cholesterol, medications, and previous cardiovascular disease (OR 1.75 95%CI 1.17-2.61, P = 0.006). This association persisted after exclusion of 45 obese participants.
Conclusion
Higher leptin levels were independently associated with increased odds of incident hypertension in older adults.
Keywords: hypertension, leptin, obesity
Introduction
Leptin is a neuroendocrine hormone regulating food intake, metabolism, and fat accumulation by decreasing appetite and increasing energy expenditure 1. Growing evidence suggests that leptin has wider actions influencing autonomic, cardiovascular, and endocrine function through vascular and renal sympathetic activation 2.
In animal models leptin affects blood pressure (BP) and contributes to hypertension 3. Cross-sectional studies in humans show an association of leptin with BP levels independent of body mass index (BMI) 4-6. In genetic studies leptin gene variants were related to BP in obese Brazilian7 and American women 8.
Although these previous studies consistently support a role for leptin in BP regulation, only one prospective study, an 8-year follow-up study of 489 middle-aged men, showed an association between baseline leptin and incident hypertension 9. No previous community-based studies have reported the association between leptin and incident hypertension in both sexes and older age. We report here the association of leptin levels with incident hypertension in older men and women.
Materials and methods
Study population
Participants in the Rancho Bernardo Study (established in 1972), were community-dwelling, middle to upper-middle class, Caucasian adults living in southern California. These individuals were initially enrolled in a study of heart disease risk factors as part of the Lipid Research Clinics Prevalence Program, and followed subsequently with periodic clinic visits and yearly mailed questionnaires. The details of the initial study have been described previously10. This analysis includes 602 participants with normal BP levels who attended a clinic visit between 1984 and 1987 and a follow-up visit an average of 4.4 years later (± 0.94; minimum 2 -maximum 7 years).
Normal BP (normotension) was defined as systolic BP <140 mm Hg and diastolic BP <90 mm Hg without use of anti-hypertensive medications 11. Incident hypertension was defined as systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg and/or the use of antihypertensive drug treatment initiated after the baseline visit.
All participants provided written informed consent. The study protocol was approved by the Human Research Protection Program at the University of California, San Diego.
Measurements
Height and weight of participants wearing light clothing and no shoes were measured using a regularly calibrated scale and stadiometer. BMI was calculated as weight (kilograms)/height (meters)2. Obesity was defined as BMI ≥30 kg/m2. Waist circumference was measured midway between the inferior lateral margin of the ribs and the superior lateral border of the iliac crest. Hip circumference was measured as the widest circumference of the hip.
Systolic and diastolic BP was measured twice in seated resting participants by certified staff according to a standard protocol 11-12. Participants were seated quietly in a chair, with feet on the floor, and arm supported at heart level for at least 5 minutes prior to BP measurement. A properly calibrated and validated instrument was used for the auscultatory method of BP measurement.
Current cigarette smoking, alcohol intake [more than 3 times/week – at least 1 unit of alcohol (~9 g) at a time], and physical activity (exercise ≥3 times/week) were self-reported using standard questionnaires. These behaviors assessed by questionnaire were indirectly validated by showing a correlation between them and clinical outcomes such as smoking with pulmonary function, alcohol intake with HDL-cholesterol, and physical activity with HDL-cholesterol and pulse rate. Previous cardiovascular disease (CVD) included stroke (by physician diagnosis), angina (by physician diagnosis, Rose questionnaire, or angina medication), physician-diagnosed myocardial infarction, cardiac revascularization, or congestive heart failure. Medication use was validated by a specially trained nurse who examined pills and prescriptions brought to the clinic for that purpose.
Blood samples were obtained after a requested 12-hour fast; venous blood was obtained in 1984-1987, and serum was separated and frozen at −70°C until 2004, when leptin levels were measured by radioimmunoassay (Linco Diagnostics Laboratory, St. Louis, MO). The sensitivity and the intra- and interassay coefficient of variation was 0.5 ng/mL, 4% and 5%, respectively.
Fasting total cholesterol, HDL, and triglyceride levels were measured in a Center for Disease Control Certified Lipid Research Clinic Laboratory. Total cholesterol and triglyceride levels were measured by enzymatic techniques using an ABA-200 biochromatic analyzer (Abbott Laboratories, Irving, TX). HDL was measured after precipitation of the other lipoproteins with heparin and manganese chloride. LDL was estimated using the Friedewald formula. Plasma glucose levels were measured by the glucose oxidase method, plasma insulin by double-antibody RIA, and serum creatinine by the Jaffe reaction method. The estimated glomerular filtration rate (eGFR) was calculated by the Cockcroft-Gault formula13. Homeostasis Model Assessment for Insulin Resistance (HOMA-IR) was used to estimate insulin resistance according to the formula: insulin (mU/l) x glucose (mmol/l))/22.5 14.
Statistical analysis
In univariate analyses, clinical characteristics were compared by the presence of incident hypertension using Student t tests, Mann-Whitney U, and Chi-square analysis. The association between leptin levels (log-transformed) and clinical characteristics (continuous variables) was analyzed by simple correlation (Pearson correlation coefficient).
Leptin was analyzed both as a continuous and categorical variable. For continuous analysis, because of its non-normal distribution, leptin was log-transformed; for categorical analysis, leptin levels were divided into tertiles and the lowest tertile was a priori selected as the reference group. Logistic regression models were used to examine the association of leptin with hypertension incidence adjusting for covariates in multivariate models: the first was age + BMI adjusted; the second was model 1 + baseline systolic BP + total cholesterol; the third was model 2 + medications (aspirin, cholesterol-lowering, and estrogen therapy in women); and the fourth was model 3 + previous CVD. All covariates were chosen based on univariate association with outcome and exposure (see table 2), and biological significance (previous CVD). The Hosmer and Lemeshow test was applied to evaluate whether the estimates of the model fit the data at an acceptable level (P >0.05). There was no collinearity [tested by simple correlation between variables; those highly correlated (correlation coefficient >0.6) were included in models separately] or significant interaction observed between independent variables. All analyses were performed using SPSS (version 13.1, SPSS, Inc., Chicago, IL); p-values (two-tailed) <0.05 were considered significant.
Table 2.
Simple correlation between leptin levels (log-transformed) and clinical characteristics
| Pearson correlation coefficient |
P value | |
|---|---|---|
| Age | 0.095 | 0.02 |
| Body mass index | 0.434 | <0.001 |
| Waist circumference | 0.113 | 0.006 |
| HOMA-IR (log) | 0.337 | <0.001 |
| Systolic blood pressure | 0.140 | 0.001 |
| Diastolic blood pressure | 0.011 | 0.80 |
| Total cholesterol | 0.261 | <0.001 |
| HDLc | 0.033 | 0.42 |
| LDLc | 0.218 | <0.001 |
| Triglycerides (log) | 0.287 | <0.001 |
| Fasting plasma glucose | 0.018 | 0.66 |
| eGFR | 0.030 | 0.46 |
Results
The 602 participants who were normotensive at baseline had a mean age of 66.2 years ± 11.4; 60.6% were men and 7.6% were obese (mean BMI 24.9±3.4 kg/m2). None of the 602 participants were taking anti-hypertensive medication; 19.6% were taking aspirin, 0.5% were taking cholesterol-lowering medication, and 17.1% of women were taking estrogen therapy. During the mean follow up of 4.4 ± 0.94 years (minimum 2 – maximum 7 years), 106 (17.6%) new cases of hypertension (mean of 2 seated blood pressures or new use of antihypertensive medication) were identified. Their baseline leptin levels were [median (25th – 75th range)] [7.3 (4-12) ng/mL]. Leptin levels were much higher in women [11.7 (8-19) ng/mL] than in men [5.6 (4-8) ng/mL, P <0.001].
As shown in Table 1, participants who developed hypertension were older (69.9 ± 8.2 vs. 65.4 ± 12.0 years, P <0.001), and had higher systolic BP (129.4 ± 7.0 vs. 121.0 ± 9.2 mm Hg, P <0.001), lower eGFR (61.4 ± 16.4 vs. 65.3 ± 20.6 ml/min, P = 0.04), and higher total cholesterol levels (5.87 ± 1.17 vs. 5.60 ± 1.04 mmol/L, P = 0.01) at baseline compared to participants who remained normotensive. They did not differ by sex or body size. Baseline leptin levels were higher in participants who developed hypertension [median (25th – 75th range)] [8.8 (5-16) vs. 7 (4-11) ng/mL, P = 0.002] compared to persistent normotensives.
Table 1.
Baseline characteristics by hypertension incidence status
| Persistent Normotensives (n = 496) |
New hypertensives (n = 106) |
P | |
|---|---|---|---|
| Mean age (yrs) | 65.4 ± 12.0 | 69.9 ± 8.2 | <0.001 |
| Men - n (%) | 308 (62.1) | 57 (53.8) | 0.11 |
| Regular exercise - n (%) | 397 (80.5) | 92 (86.8) | 0.12 |
| Current smoke - n (%) | 70 (14.1) | 12 (11.3) | 0.45 |
| Alcohol (3 times/week) - n (%) | 228 (46) | 48 (45.2) | 0.90 |
| Body mass index (kg/m2) | 24.9 ± 3.5 | 25.0 ± 3.4 | 0.82 |
| Waist circumference (cm) | 86.2 ± 11.4 | 86.9 ± 11.0 | 0.59 |
| Systolic blood pressure (mm Hg) | 121.0 ± 9.2 | 129.4 ± 7.0 | <0.001 |
| Diastolic blood pressure (mm Hg) | 72.9 ± 7.4 | 74.1 ± 7.4 | 0.13 |
| Fasting blood glucose (mmol/L) | 5.46 ± 0.99 | 5.76 ± 1.97 | 0.13 |
| Total cholesterol (mmol/L) | 5.60 ± 1.04 | 5.87 ± 1.17 | 0.01 |
| LDL-c (mmol/L) | 3.50 ± 0.95 | 3.74 ± 1.06 | 0.02 |
| HDL-c (mmol/L) | 1.53 ± 0.48 | 1.55 ± 0.40 | 0.63 |
| Triglycerides (mmol/L) | 1.05 (0.80) | 1.02 (0.80) | 0.73 |
| HOMA IR(mU*mmol/L2)* | 2.8 (1.8) | 2.8 (1.7) | 0.82 |
| Creatinine (μmol/L ) | 97.2 ± 17.7 | 88.4 ± 17.7 | 0.11 |
| Estimated glomerular filtration rate (ml/min) | 65.3 ± 20.6 | 61.4 ± 16.4 | 0.04 |
| Leptin (ng/mL) | 7 (7) | 8.8 (11) | 0.002 |
Data expressed as percentage, mean ± SD or median (interquartile range).
Homeostasis Model Assessment for Insulin Resistance.
Table 2 shows the linear association between leptin levels (log-transformed) and clinical characteristics. The greater the leptin level the higher the BMI, waist circumference, systolic BP, total cholesterol and LDLc (all P’s <0.05).
As a continuous variable (log transformed), leptin predicted incident hypertension in unadjusted (OR 1.72 95%CI 1.3-2.33, P <0.001) and fully adjusted models (age, BMI, systolic BP, total cholesterol, medications, and CVD) (OR 1.75 95%CI 1.17-2.61, P = 0.006) (Table 3). Further adjustment for HOMA-IR, triglycerides, waist circumference, or waist/hip ratio separately in the models (instead of BMI) did not materially change these results. In sex-specific analyses, leptin predicted hypertension in both sexes before (men: OR 1.72 95%CI 1.04-2.85, P = 0.03; women: OR 1.87 95%CI 1.10-3.17, P = 0.02) and after adjustment for covariates (fully adjusted model; men: OR 2.11 95%CI 1.00-4.46, P = 0.05; women: OR 3.19 95%CI 1.30-7.80, P = 0.01).
Table 3.
Unadjusted and multivariate adjusted odds ratio of log-transformed leptin for incident hypertension
| Overall | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Unadjusted | 1.72 | 1.30-2.33 | <0.001 | 1.72 | 1.04-2.85 | 0.03 | 1.87 | 1.10-3.17 | 0.02 |
| Model 1: age + BMI* | 1.78 | 1.25-2.54 | 0.001 | 2.70 | 1.37-5.4 | 0.004 | 2.25 | 1.02-5.00 | 0.04 |
| Model 2: model 1 + systolic BP + total cholesterol |
1.81 | 1.22-2.70 | 0.003 | 2.22 | 1.07-4.61 | 0.03 | 2.91 | 1.25-6.8 | 0.01 |
| Model 3: model 2 + medications** |
1.80 | 1.21-2.70 | 0.004 | 2.24 | 1.07-4.70 | 0.03 | 3.00 | 1.25-7.20 | 0.01 |
| Model 4: model 3 + co- morbidities*** |
1.75 | 1.17-2.61 | 0.006 | 2.11 | 1.00-4.46 | 0.05 | 3.19 | 1.30-7.80 | 0.01 |
BMI = body mass index
Medications: aspirin, cholesterol lowering, and estrogen therapy in women
Co-morbidities: previous cardiovascular disease (stroke, heart disease, or revascularization)
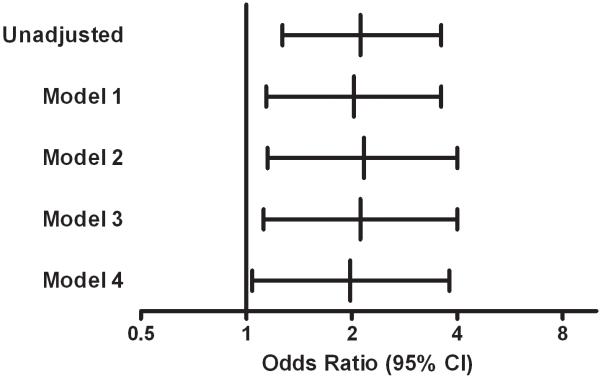
Because for clinical purposes results would be clearer if leptin is expressed in ng/mL, we also analyzed leptin as a categorical variable expressed in conventional units. Participants were divided into 3 groups by leptin tertiles [median (25th – 75th range)] [first tertile: 4.2 (3-5) ng/mL; second tertile: 8.3 (7-9) ng/mL; third tertile 18 (14-23) ng/mL]. The incidence of hypertension was higher in the highest leptin tertile compared to the lowest leptin tertile (26.4% vs. 14.4%, P = 0.008). Figure 1 shows the odds ratio for incident hypertension obtained by all logistic regression models. Compared to the lowest leptin tertile, the highest tertile was associated with an increased risk for incident hypertension before (OR 2.12 95%CI 1.2-3.6, P = 0.004) and after adjustments for covariates (fully adjusted model: OR 1.98 95%CI 1.04-3.8, P = 0.04). Further adjustment for HOMA-IR, triglycerides, waist circumference, or waist/hip ratio separately in the models (instead of BMI) did not materially change these results. Compared to the first tertile, the second tertile did not increase the risk for incident hypertension in either unadjusted or adjusted analysis (data not shown).
Figure 1.
Odds ratio for incident hypertension, highest tertile of leptin compared to the lowest tertile (reference category). Model 1: adjusted for age and body mass index; Model 2: model 1 + baseline systolic blood pressure + total cholesterol; Model 3: model 2 + medication (aspirin, cholesterol-lowering, and estrogen therapy in women); Model 4: model 3 + previous cardiovascular disease.
To investigate the effect of obesity, which is known to be associated with both leptin and BP, we repeated the analysis excluding all 45 obese participants; leptin levels remained positively and significantly associated with an increased risk for incident hypertension in all models in both continuous and categorical analyses. Next, we stratified participants by not overweight vs. overweight (BMI < and ≥25 kg/m2); in this analysis, leptin levels (log-transformed) were still associated with an increased odds of hypertension in fully adjusted models although statistical significance at P <0.05 was lost in this model for not overweight participants (BMI <25kg/m2: OR 1.48 95%CI 0.88-2.50, P = 0.10; BMI ≥25 kg/m2: OR 2.47 95%CI 1.31-4.65, P = 0.005), likely due to the small number of incident hypertension cases in the subset.
To consider the association of leptin with BP change over time, we examined a BP increment ≥1 SD in systolic (baseline systolic BP increase ≥12 mm Hg) or diastolic BP values (baseline systolic BP increase ≥7 mm Hg) during the follow up. Higher baseline leptin levels (log-transformed) were positively associated with BP change before and after adjustment for covariates using the same multivariate models described above (fully adjusted model: OR 1.4 95%CI 1.01-1.74, P = 0.04).
Discussion
In this prospective study, leptin levels independently predicted incident hypertension in older community-dwelling adults. Increased leptin levels were associated with an approximately 70% increase in the risk for subsequent hypertension. This association was observed in both sexes and persisted after excluding obese participants.
Several cross-sectional studies have reported an association between leptin levels and BP. Barba and colleagues found that leptin levels were associated with BP in 457 Italian men, independent of age, BMI, insulin, and creatinine 4. The same association was also seen among Swedish overweight women 15 and in a study of a rural Chinese population 16. To our knowledge only one prospective study has reported leptin levels and incident hypertension: Galletti and colleagues followed somewhat younger normotensive men (aged 50.1 ± 6.7 years) for 8 years; leptin levels were associated with increased risk for hypertension in models adjusted for age, BMI, systolic BP, and HOMA-IR 9. That study evaluated men but not women, had only a single baseline BP measurement, and defined hypertension differently (systolic BP ≥160 mm Hg or diastolic ≥95 mm Hg or anti-hypertensive medication) than the present study. Our results are consistent with their findings, but with the strength of an average of two baseline and follow-up BP measurements for better BP classification. Our study is also the first to show a prospective association of leptin with categorically defined hypertension, with change in BP, and in both sexes.
Sex differences in leptin were described in a Japanese population 5, and in the National Heart, Lung, and Blood Institute Family Study 8; the latter cross-sectional study reported leptin gene variants and leptin levels were associated with BP regulation in women but not men. In Rancho Bernardo an association between leptin and incident hypertension was observed in both sexes when leptin was analyzed as a continuous variable.
One mechanism whereby leptin may exert an effect on BP could be its effect on the sympathetic nervous system 2. Chronic hyperleptinemia increases sympathetic nervous system activity and leads to a decrease in nitric oxide-dependent vasodilatation and natriuresis 17. However, in animal experimental models, leptin did not affect the vasodilatation after sodium nitroprusside suggesting either a direct effect on vascular bed or BP regulation through inflammation18. A human experimental model demonstrated that leptin induced C-reactive protein mRNA transcription by human coronary artery endothelial cells in culture as well as the release of C-reactive protein in the culture medium in a concentration-dependent fashion19. Obesity is another potential mechanism that cannot be entirely excluded, as controlling for BMI or excluding categorical obesity does not exclude differences in percent body fat. However, leptin still predicted hypertension in models adjusted for waist or waist/hip ratio.
To date, leptin has been considered a “good” hormone because of its action in the satiety pathway 20. Leptin replacement has been evaluated in the treatment of diseases associated with complete or partial leptin deficiency, including genetic forms of obesity 21, lipodystrophy 22, and human immunodeficiency virus-associated lipodystrophy 23. In these clinical studies the main focus was on the metabolic effects of leptin, and information about BP was limited/absent or the sample size was too small to exclude an effect of leptin on BP. The present study highlights a possibly harmful effect of leptin on BP; this information adds a new potential side effect to be evaluated in future leptin replacement trials.
The Rancho Bernardo Study has several limitations; the population is almost entirely Caucasian and middle class and had a relatively low prevalence of obesity; results may not be generalizable to other populations. We did not address specific dietary factors that might alter leptin and BP (i.e., sodium intake), another area for future research. Serum samples had been frozen for an average of 18 years before leptin assays; we doubt that long-term storage distorted the levels of leptin, in that Rancho Bernardo levels are similar to those reported in other populations using the same assay methods 24.
In the present study BP was assessed in seated subjects according to a standard protocol by certified nurses, the gold standard for BP measurement in most epidemiological studies. However, 24-h BP monitoring is more accurate. Recently Thomopoulos and colleagues reported a cross-sectional study confirming an association between free leptin levels and hypertension in 494 adults who had 24-h ambulatory BP monitoring25.
In conclusion, higher leptin levels were independently associated with at least 70% increased odds of incident hypertension in older adults, an association independent of several potentially important covariates including obesity. These results need to be replicated in other prospective studies.
Acknowledgments
Funding: The Rancho Bernardo Study is funded by the National Institutes of Health/National Institute on Aging, grants AG07181 and AG028507, and the National Institute of Diabetes and Digestive and Kidney Diseases, grant DK31801. C.K.K is a recipient of a grant from CAPES (Coordenacao de Aperfeicoamento e Pessoal de Nivel Superior)/Brazil (Programa de Doutorado no Pais com Estagio no Exterior).
Footnotes
Declaration of interest: none to declare.
References
- 1.van Dijk G. The role of leptin in the regulation of energy balance and adiposity. J Neuroendocrinol. 2001;13:913–921. doi: 10.1046/j.1365-2826.2001.00707.x. [DOI] [PubMed] [Google Scholar]
- 2.Haynes WG, Sivitz WI, Morgan DA, Walsh SA, Mark AL. Sympathetic and cardiorenal actions of leptin. Hypertension. 1997;30:619–623. doi: 10.1161/01.hyp.30.3.619. [DOI] [PubMed] [Google Scholar]
- 3.Shek EW, Brands MW, Hall JE. Chronic leptin infusion increases arterial pressure. Hypertension. 1998;31:409–414. doi: 10.1161/01.hyp.31.1.409. [DOI] [PubMed] [Google Scholar]
- 4.Barba G, Russo O, Siani A, Iacone R, Farinaro E, Gerardi MC, Russo P, Della Valle E, Strazzullo P. Plasma leptin and blood pressure in men: graded association independent of body mass and fat pattern. Obes Res. 2003;11:160–166. doi: 10.1038/oby.2003.25. [DOI] [PubMed] [Google Scholar]
- 5.Takizawa H, Ura N, Saitoh S, Wang L, Higashiura K, Takagi S, Takada M, Togashi N, Nakano M, Hayashi Y, Shimamoto K. Gender difference in the relationships among hyperleptinemia, hyperinsulinemia, and hypertension. Clin Exp Hypertens. 2001;23:357–368. doi: 10.1081/ceh-100102673. [DOI] [PubMed] [Google Scholar]
- 6.Masuo K, Mikami H, Itoh M, Ogihara T, Tuck ML. Sympathetic activity and body mass index contribute to blood pressure levels. Hypertens Res. 2000;23:303–310. doi: 10.1291/hypres.23.303. [DOI] [PubMed] [Google Scholar]
- 7.Genelhu VA, Celoria BM, Pimentel MM, Duarte SF, Cabello PH, Francischetti EA. Association of a common variant of the leptin gene with blood pressure in an obese Brazilian population. Am J Hypertens. 2009;22:577–580. doi: 10.1038/ajh.2009.7. [DOI] [PubMed] [Google Scholar]
- 8.Ma D, Feitosa MF, Wilk JB, Laramie JM, Yu K, Leiendecker-Foster C, Myers RH, Province MA, Borecki IB. Leptin is associated with blood pressure and hypertension in women from the National Heart, Lung, and Blood Institute Family Heart Study. Hypertension. 2009;53:473–479. doi: 10.1161/HYPERTENSIONAHA.108.118133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galletti F, D’Elia L, Barba G, Siani A, Cappuccio FP, Farinaro E, Iacone R, Russo O, De Palma D, Ippolito R, Strazzullo P. High-circulating leptin levels are associated with greater risk of hypertension in men independently of body mass and insulin resistance: results of an eight-year follow-up study. J Clin Endocrinol Metab. 2008;93:3922–3926. doi: 10.1210/jc.2008-1280. [DOI] [PubMed] [Google Scholar]
- 10.Barrett-Connor E. The prevalence of diabetes mellitus in an adult community as determined by history or fasting hyperglycemia. Am J Epidemiol. 1980;111:705–712. doi: 10.1093/oxfordjournals.aje.a112948. [DOI] [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.The hypertension detection and follow-up program: Hypertension detection and follow-up program cooperative group. Prev Med. 1976;5:207–215. doi: 10.1016/0091-7435(76)90039-6. [DOI] [PubMed] [Google Scholar]
- 13.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 14.Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23:57–63. doi: 10.2337/diacare.23.1.57. [DOI] [PubMed] [Google Scholar]
- 15.Lindgarde F, Soderberg S, Olsson T, Ercilla MB, Correa LR, Ahren B. Overweight is associated with lower serum leptin in Peruvian Indian than in Caucasian women: A dissociation contributing to low blood pressure? Metabolism. 2001;50:325–329. doi: 10.1053/meta.2001.21033. [DOI] [PubMed] [Google Scholar]
- 16.Hu FB, Chen C, Wang B, Stampfer MJ, Xu X. Leptin concentrations in relation to overall adiposity, fat distribution, and blood pressure in a rural Chinese population. Int J Obes Relat Metab Disord. 2001;25:121–125. doi: 10.1038/sj.ijo.0801480. [DOI] [PubMed] [Google Scholar]
- 17.Beltowski J. Role of leptin in blood pressure regulation and arterial hypertension. J Hypertens. 2006;24:789–801. doi: 10.1097/01.hjh.0000222743.06584.66. [DOI] [PubMed] [Google Scholar]
- 18.Rahmouni K, Jalali A, Morgan DA, Haynes WG. Lack of dilator effect of leptin in the hindlimb vascular bed of conscious rats. Eur J Pharmacol. 2005;518:175–181. doi: 10.1016/j.ejphar.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 19.De Rosa S, Cirillo P, Pacileo M, Di Palma V, Paglia A, Chiariello M. Leptin Stimulated C-Reactive Protein Production by Human Coronary Artery Endothelial Cells. J Vasc Res. 2009;46:609–617. doi: 10.1159/000226229. [DOI] [PubMed] [Google Scholar]
- 20.Bluher S, Mantzoros CS. Leptin in humans: lessons from translational research. Am J Clin Nutr. 2009;89:991S–997S. doi: 10.3945/ajcn.2008.26788E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C, Sanna V, Jebb SA, Perna F, Fontana S, Lechler RI, DePaoli AM, O’Rahilly S. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest. 2002;110:1093–1103. doi: 10.1172/JCI15693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebihara K, Kusakabe T, Hirata M, Masuzaki H, Miyanaga F, Kobayashi N, Tanaka T, Chusho H, Miyazawa T, Hayashi T, Hosoda K, Ogawa Y, DePaoli AM, Fukushima M, Nakao K. Efficacy and safety of leptin-replacement therapy and possible mechanisms of leptin actions in patients with generalized lipodystrophy. J Clin Endocrinol Metab. 2007;92:532–541. doi: 10.1210/jc.2006-1546. [DOI] [PubMed] [Google Scholar]
- 23.Mulligan K, Khatami H, Schwarz JM, Sakkas GK, DePaoli AM, Tai VW, Wen MJ, Lee GA, Grunfeld C, Schambelan M. The effects of recombinant human leptin on visceral fat, dyslipidemia, and insulin resistance in patients with human immunodeficiency virus-associated lipoatrophy and hypoleptinemia. J Clin Endocrinol Metab. 2009;94:1137–1144. doi: 10.1210/jc.2008-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gavrila A, Chan JL, Yiannakouris N, Kontogianni M, Miller LC, Orlova C, Mantzoros CS. Serum adiponectin levels are inversely associated with overall and central fat distribution but are not directly regulated by acute fasting or leptin administration in humans: cross-sectional and interventional studies. J Clin Endocrinol Metab. 2003;88:4823–4831. doi: 10.1210/jc.2003-030214. [DOI] [PubMed] [Google Scholar]
- 25.Thomopoulos C, Papadopoulos DP, Papazachou O, Bratsas A, Massias S, Anastasiadis G, Perrea D, Makris T. Free leptin is associated with masked hypertension in nonobese subjects: a cross-sectional study. Hypertension. 2009;53:965–972. doi: 10.1161/HYPERTENSIONAHA.108.128041. [DOI] [PubMed] [Google Scholar]