Abstract
BACKGROUND
Childhood adversity is associated with adult mental disorders, but the mechanisms underlying this association remain inadequately understood. Stress sensitization, whereby childhood adversity increases vulnerability to mental disorders following adult stressful life events, has been proposed as a potential mechanism. We provide a test of the stress sensitization hypothesis in a national sample.
METHODS
We investigated whether the association between past-year stressful life events and the 12-month prevalence of major depression, posttraumatic stress disorder (PTSD), other anxiety disorders, and perceived stress varies according to exposure to childhood adversity. We used data from the National Epidemiological Survey of Alcohol and Related Conditions (n=34,653).
RESULTS
Past-year stressful life events were associated with an increased risk of major depression, PTSD, anxiety disorders, and perceived stress. However, the magnitude of the increased risk varied according to respondents’ history of childhood adversity. For example, past-year major stressors were associated with a 27.3% increase in the 12-month risk of depression among individuals with 3+ childhood adversities and a 14.8% increased risk among individuals without childhood adversities. Stress sensitization effects were present for depression, PTSD, and other anxiety disorders in women and men, although gender differences were found in the threshold of past-year stress needed to trigger such effects. Stress sensitization was most evident among individuals with 3+ childhood adversities.
CONCLUSIONS
Childhood adversity is associated with increased vulnerability to the deleterious mental health effects of adult stressors in both men and women. High levels of childhood adversity may represent a general diathesis for multiple types of psychopathology that persists throughout the life-course.
Childhood adversities (CAs) including family violence (Fantuzzo et al., 1991, Sternberg et al., 2006), physical and sexual abuse (Molnar et al., 2001, Mullen et al., 1996, Springer et al., 2001), and neglect (Gauthier et al., 1996) are associated with the development of psychiatric disorders, and these associations persist into adolescence and adulthood (Collishaw et al., 2007, Kessler et al., 1997). CAs are associated with liability to mood, anxiety, and substance use disorders, with little meaningful variation in these associations across disorders (Green et al., in press, Kessler et al., 1997), suggesting that CAs represent a common developmental origin to adult psychiatric disorders.
One possible explanation for this increased liability to adult psychopathology is that exposure to CA increases vulnerability to the effects of later stressful life events. Hammen and colleagues (2000) proposed a stress sensitization model which posits that risk for adult depression following stressful life events is higher among individuals with a history of CAs than among individuals without a history of CA exposure. In a study examining this model, they reported that low levels of recent stressful events were associated with an increased risk for MDE only among women with a history of CAs including parental death, divorce, and family violence. In contrast, CA had no involvement in the association between high levels of recent stress and MDE. These results suggest that CA can “sensitize” individuals to psychopathology by lowering their tolerance to relatively minor stressors (Hammen et al., 2000).
Since this study, stress sensitization effects have been documented in at least five other investigations (Dougherty et al., 2004, Espejo et al., 2006, Harkness et al., 2006, Kendler et al., 2004, Rudolph and Flynn, 2007). Each of these studies finds an interaction between CA and later stress such that depression risk associated with stressful events is particularly heightened among individuals with a history of CAs. Elevated risk for MDE among those with CA exposure was evident after low levels of subsequent stress exposure in some of these studies (Harkness et al., 2006), whereas in others heightened vulnerability to MDEs associated with CA exposure was observed only after high levels of stress exposure (Espejo et al., 2006, Kendler et al., 2004). Stress sensitization effects have also been reported among individuals with dysthymia, such that the association between chronic stress and the severity of depressive symptoms was stronger among individuals with a history of CAs (Dougherty et al., 2004).
A number of questions regarding the role of stress sensitization in explaining life-course associations between CAs and psychiatric disorders remain unanswered, however. Evidence of stress sensitization effects is based on clinical or community samples of primarily females and studies that have focused exclusively on depressive disorders (Dougherty et al., 2004, Espejo et al., 2006, Hammen et al., 2000, Harkness et al., 2006, Rudolph and Flynn, 2007). As a result, the generalizability of these findings, particularly to males, remains unclear. Moreover, the stress sensitization model has not been tested for psychiatric disorders other than depression, with the exception of PTSD. Individuals who have been exposed to prior trauma, particularly childhood maltreatment, are more likely to develop PTSD following subsequent traumatic events than individuals with no prior trauma history (Bremmer et al., 1993, Breslau et al., 1999, Brewin et al., 2000), although recent prospective data raise questions about these findings (Breslau et al., 2008).
Prior research examining stress sensitization also has examined a narrow set of CAs, ranging from divorce and parental loss (Rudolph and Flynn, 2007) to abuse and neglect (Harkness et al., 2006), with little consistency across studies. CAs reflecting family dysfunction, such as maltreatment inter-parental violence, have stronger associations with psychopathology than other CAs (Green et al., in press, McLaughlin et al., in press), and thus may be most likely to set the stage for stress sensitization effects. Prior research has yet to examine these effects as a function of exposure to a broader set of CAs reflecting maladaptive family environments.
To address these gaps in the literature, we test the stress sensitization hypothesis in a national sample of men and women. We examine whether the association between stressful life events in adulthood and the 12-month prevalence of mood and anxiety disorders differs according to past exposure to CAs. We also examine whether the association between past-year stressful life events and perceived stress differs according to past exposure to CAs. Such a pattern would suggest that individuals with a history of CA perceive such events to be more negative or overwhelming and thus may be more vulnerable to the mental health consequences of stress exposure. We hypothesize that the association between past-year life events and psychiatric disorders, and between past-year life events and perceived stress, will be strongest among individuals with a history of CAs. We extend the literature by examining these effects separately for women and men.
METHODS
Sample
Data are drawn from the National Epidemiologic Study of Alcohol and Related Conditions (NESARC), a population-based psychiatric epidemiological study of civilian, non-institutionalized U.S. adults aged 18 years and older. In 2001–2002, 43,093 respondents completed Wave 1 of the NESARC (81.0% response rate). Between 2004–2005, 34,653 respondents completed a second interview (86.7% response rate). The cumulative response rate for both waves was 70%. Analyses reported here are based on Wave 2 data, which assessed CAs and stressful life events (Grant et al., 2008, Ruan et al., 2008).
Measures
Psychiatric disorders
DSM-IV(American Psychiatric Association, 1994) mood and anxiety disorders were assessed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) (Grant et al., 2001). The AUDADIS-IV assesses major depression (MDE) and anxiety disorders including generalized anxiety disorder (GAD), panic disorder with or without agoraphobia, social phobia, and post-traumatic stress disorder (PTSD). Substance-induced mood and anxiety disorders, those due to somatic illnesses, or (in the case of major depression) bereavement were ruled out as per DSM-IV definition. AUDADIS-IV diagnoses have been found to be reliable in a number of general population and clinical reappraisal studies, and the reliability of AUDADIS-IV mood and anxiety disorder diagnosis and symptom items range from fair (kappa for GAD = 0.41) to good (kappa for PTSD diagnosis = 0.77) (Grant et al., 2003a, Grant et al., 1995, Ruan et al., 2008). The current analysis focuses on the presence of 12-month 1) MDE, 2) PTSD, and 3) other anxiety disorders (ADs) including: panic disorder with/without agoraphobia, generalized anxiety disorder, and social phobia.
Childhood Adversity
Respondents completed a series of questions regarding exposure to CAs occurring before age 17. Emotional and physical abuse and family violence were assessed using questions from the Conflict Tactics Scale (Straus, 1979). Emotional abuse items assessed how often caregivers insulted, swore at, said hurtful things, and threatened respondents with violence. Physical abuse items ascertained the frequency of caregiver violent behavior toward the respondent that resulted in marks or injuries. Questions regarding violent behavior directed at respondents’ mother or female caregiver were used to assess family violence.
Neglect was assessed using questions from the Children’s Trauma Questionnaire (CTQ) (Bernstein et al., 1994) which queried how often respondents were left unsupervised when they were too young to be alone, went without things they needed (e.g., clothes, shoes), were not provided with regular meals, or did not receive necessary medical treatment. The CTQ also includes an endangerment item that assesses whether respondents were made to do chores that were dangerous for someone their age. Previously validated questions (Wyatt, 1985) regarding sexual experiences that were unwanted, that involved an adult, or that occurred when the respondent was too young to know what was happening were used to assess sexual abuse. We also analyzed an item from the PTSD trauma section that assessed whether or not respondents had been sexually assaulted, raped, or experienced unwanted sexual contact. Respondents reported the frequency of these CAs (with the exception of sexual assault) on a scale ranging from (1) never to (5) very often. Physical or sexual abuse, endangerment, and exposure to domestic violence were coded as present if respondents endorsed any exposure. Emotional abuse and neglect were coded as present if respondents endorsed that they occurred sometimes, fairly often, or very often.
Three other CAs reflecting the presence or absence of parental dysfunction were assessed: serious mental illness (hospitalization for a mental illness, suicide attempt or completion), criminality (incarceration), and substance abuse.
Stressful Life Events
The AUDADIS-IV assessed stressful life events occurring in the 12-months prior to the interview (Ruan et al., 2008). Eleven events from this section were classified as minor life stressors: respondent moving or having someone new live with him or her; interpersonal problems at work; changes in work or job responsibilities; serious problems with a neighbor, friend, or relative; legal problems; being the victim of theft; intentional damage to respondent’s property; being mugged; family member or close friend being mugged or assaulted; expected death of a family member or close friend; and legal problems of family member or close friend.
Major life events and traumas were also assessed and included the following 14 events: being fired or laid off; being unemployed and looking for work for more than one month; marital separation, divorce, or the breakup of a steady relationship; serious financial crisis or bankruptcy; unexpected death of a family member or close friend; war exposure; life-threatening illness or accident; natural disaster exposure; sexual assault; being the victim of interpersonal violence; being kidnapped or held hostage; being stalked; witnessing someone seriously injured or killed; and respondent or someone close to respondent being the victim of a terrorist attack.
Past-year stressors and CAs were treated as categorical variables (0, 1–2, or 3+ events).
Perceived Stress
Respondents completed the 4-item Perceived Stress Scale (PSS) (Cohen and Cohen, 1983), a widely-used measure of stress appraisal. Items assessed the extent to which respondents felt: able to control important things in their life; confident about their ability to handle personal problems; that things were going their way; and that difficulties were piling up so high that they couldn’t overcome them. Respondents provided ratings of perceived stress for the 12-month period prior to the interview on a scale ranging from 0 (never) to 4 (very often).
Analysis Methods
According to the stress sensitization model, the association between stressful life events in adulthood and psychopathology varies according to past exposure to CAs. Therefore, in prediction models for past-year disorders, we expect to observe an interaction between CA exposure and adult stressors, with stronger effects of adult stressors observed among individuals exposed to higher levels of CAs. Accordingly, the analytic strategy proceeds as follows.
Logistic regression analyses were conducted for each psychiatric outcome (MDE, PTSD, and ADs). We included CA, past-year stress exposure (either minor or major), and the interaction between CA and stress exposure in each model along with participants’ age, nativity, and race-ethnicity; a statistically significant interaction term supports the presence of a sensitization effect. Consistent with stress-sensitization theory, we predicted that the difference in the risk of psychopathology between individuals experiencing high vs. low levels of stressful life events would vary according to past exposure to CA (i.e., would be larger among individuals with a history of CA than among individuals without a history of CA). Accordingly, we evaluated the interaction between CA and stress exposure on an additive scale (Rothman, 1974, Rothman et al., 1980) by computing risk differences for psychopathology according to CA exposure. Proportions of individuals with each psychiatric outcome at each level of stress and CA exposure in the population were estimated directly from the logistic regression model containing the interaction term. Model-based risk differences (the difference between the proportions of individuals with a psychiatric outcome at low (1–2 events) or high (3+ events) levels of past-year stress exposure compared to no past-year stress exposure) were estimated for each CA exposure group (0, 1–2, 3+). All analyses were conducted separately for males and females; gender differences in stress sensitization were tested through 3-way interaction terms between CA, adult stressful events, and gender in predicting mood and anxiety disorder outcomes.
Mean levels of perceived stress were computed by gender, type (minor, major) and level of past-year stressor exposure. We examined two linear regression models predicting perceived stress from CAs, past-year life events (major, minor), and their interaction to determine whether the association between stressful life events and perceived stress is modified by level of exposure to CAs.
Analyses were conducted using SUDAAN v.10.0 software (Research Triangle Institute, 2008) which adjusts variance estimates for the complex sampling design. NESARC sampling weights were used to account for selection and response probabilities. Statistical significance was evaluated using 2-tailed .05-level tests.
RESULTS
Prevalence of Childhood Adversities and Stressful Life Events
Nearly half of respondents reported at least one CA reflecting family dysfunction (49.4%). The prevalence of CA exposure was similar among men and women. (Table 1) Parental substance abuse (23.0%) and emotional abuse (22.5%) were the most commonly reported adversities. Exposure to multiple CAs was common, with 19.0% of respondents reporting exposure to 1 CA, 11.0% reporting exposure to 2 CAs, and 19.8% reporting 3 or more CAs.
Table 1.
Demographic characteristics of the National Epidemiological Survey on Alcohol and Related Conditions sample (NESARC), n=34,653, 2004–2005
| Total Sample N=34,653 | Women n=20,089 | Men n=14,564 | ||||
|---|---|---|---|---|---|---|
| n* | %† | n | % | n | % | |
| Age | ||||||
| 20–29 | 4,913 | 16.3 | 2,787 | 15.7 | 2,126 | 17.1 |
| 30–39 | 6,621 | 18.7 | 3,945 | 18.1 | 2,676 | 19.3 |
| 40–49 | 7,539 | 21.5 | 4,224 | 21.1 | 3,315 | 22.0 |
| 50–59 | 6,117 | 17.7 | 2,701 | 17.6 | 3,416 | 17.9 |
| 60–69 | 4,174 | 11.5 | 2,363 | 11.4 | 1,811 | 11.6 |
| ≥ 70 | 5,289 | 14.2 | 3,354 | 16.1 | 1,935 | 12.2 |
| Nativity | ||||||
| US-born | 29,287 | 86.1 | 17,010 | 86.6 | 12,277 | 85.7 |
| Foreign-born | 5,363 | 13.9 | 3,076 | 13.4 | 2,287 | 14.3 |
| Race-Ethnicity | ||||||
| White | 20,161 | 70.9 | 11,308 | 70.6 | 8,853 | 71.2 |
| Black | 6,587 | 11.1 | 4,261 | 11.9 | 2,326 | 10.1 |
| Native American | 578 | 2.2 | 338 | 2.3 | 240 | 2.1 |
| Asian & Pacific Islander | 968 | 4.3 | 542 | 4.2 | 426 | 4.4 |
| Hispanic | 6,359 | 11.6 | 3,640 | 10.9 | 2,719 | 12.3 |
| Past-year Psychiatric Disorders | ||||||
| Major Depressive (MDD) | 3,023 | 8.3 | 2,203 | 10.8 | 820 | 5.5 |
| Post Traumatic Stress Disorder (PTSD) |
2,496 | 6.5 | 1,828 | 8.7 | 668 | 4.1 |
| Other Anxiety Disorders (GAD, Panic, Social Phobia, Agoraphobia) |
2,585 | 7.1 | 1,827 | 8.9 | 758 | 5.1 |
| Childhood Adversities | ||||||
| None | 16,489 | 50.6 | 9,509 | 50.6 | 6,980 | 50.6 |
| 1–2 | 10,381 | 30.2 | 5,800 | 28.7 | 4,581 | 31.8 |
| 3+ | 6,848 | 19.3 | 4,188 | 20.7 | 2,660 | 17.7 |
| Past-year Minor Stressors | ||||||
| None | 12,307 | 36.4 | 7,149 | 36.9 | 5,158 | 35.9 |
| 1–2 | 17,277 | 50.2 | 9,991 | 49.9 | 7,286 | 50.5 |
| 3+ | 4,740 | 13.4 | 2,757 | 13.2 | 1,983 | 13.6 |
| Past-year Major Stressors | ||||||
| None | 19,985 | 60.3 | 11,438 | 59.9 | 8,547 | 60.8 |
| 1–2 | 11,567 | 34.2 | 6,841 | 34.8 | 4,726 | 33.7 |
| 3+ | 1,971 | 5.4 | 1,154 | 5.4 | 817 | 5.5 |
Unweighted counts
Weighted proportions
A majority of respondents experienced a minor stressful event in the year preceding the interview (63.6%). Major life events were less prevalent, but still common (39.7%). There were no gender differences in the prevalence of minor or major events.
Life Events, Childhood Adversities, and Psychiatric Disorders
We examined the proportions of respondents who met DMS-IV criteria for 12-month mood and anxiety disorders as a function of both past-year stressful life events and exposure to CAs, adjusting for covariates. Among both women (Table 2) and men (Table 3), the prevalence of MDE, PTSD, and ADs increased with greater exposure to past-year life events and CAs. The prevalence of MDE, PTSD, and ADs also is greater among respondents with higher levels of exposure to CAs.
Table 2.
Prevalences1 of 12-month psychiatric disorders among women, by level of exposure to past-year stressors and childhood adversity, NESARC 2004–2005
| Women (n=20,089) |
|||||||
|---|---|---|---|---|---|---|---|
| Childhood Adversities | |||||||
| None | 1–2 | 3+ | |||||
| Disorder | Past-Year Minor Stressors |
% | 95% CI | % | 95% CI | % | 95% CI |
| MDD | |||||||
| Disorder | None | 3.4 | (2.8, 4.0) | 6.3 | (4.9, 7.6) | 11.5 | (9.1, 14.0) |
| Prevalence1 | 1–2 | 7.1 | (6.2, 8.0) | 10.2 | (8.8, 11.5) | 18.6 | (16.6, 20.6) |
| 3+ | 16.4 | (13.2, 19.5) | 20.7 | (17.5, 23.9) | 30.6 | (26.8, 34.3) | |
| χ24 (p-value)2 | 8.4 (.077) | ||||||
| Risk | None | - | - | - | |||
| Differences3 | 1–2 | 3.7 | (2.6, 4.9) | 3.9 | (2.0, 5.8) | 7.1 | (3.9, 10.2) |
| 3+ | 13.0 | (9.7, 16.2) | 14.4 | (11.0, 17.9) | 19.0 | (14.7, 23.3) | |
| PTSD | |||||||
| Disorder | None | 3.1 | (2.5, 3.8) | 5.7 | (4.2, 7.1) | 13.5 | (10.9, 16.2) |
| Prevalence | 1–2 | 4.3 | (3.6, 5.0) | 7.9 | (6.7, 9.1) | 17.1 | (15.0, 19.1) |
| 3+ | 9.7 | (6.9, 12.5) | 14.8 | (11.6, 18.0) | 27.0 | (23.8, 30.2) | |
| χ24 (p-value) | 9.1 (.056) | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 1.1 | (0.2, 2.1) | 2.2 | (0.4, 4.0) | 3.5 | (0.3, 6.7) |
| 3+ | 6.6 | (3.7, 9.4) | 9.1 | (5.9, 12.4) | 13.5 | (9.1, 17.9) | |
| ANX | |||||||
| Disorder | None | 2.9 | (2.3, 3.4) | 5.1 | (3.8, 6.4) | 10.5 | (8.1, 13.0) |
| Prevalence | 1–2 | 5.5 | (4.7, 6.3) | 8.3 | (6.9, 9.6) | 14.8 | (13.0, 16.6) |
| 3+ | 14.2 | (11.1, 17.4) | 19.1 | (15.7, 22.5) | 24.7 | (21.5, 27.9) | |
| χ24 (p-value) | 3.1 (.539) | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 2.6 | (1.6, 3.6) | 3.2 | (1.3, 5.1) | 4.2 | (1.3, 7.2) |
| 3+ | 11.4 | (8.1, 14.6) | 14.0 | (10.3, 17.7) | 14.2 | (10.3, 18.1) | |
|
Past-Year Major Stressors |
|||||||
| MDD | |||||||
| Disorder | None | 3.7 | (3.1, 4.2) | 6.8 | (5.6, 7.9) | 12.9 | (10.9, 14.8) |
| Prevalence | 1–2 | 10.4 | (9.1, 11.6) | 14.2 | (12.4, 16.1) | 22.2 | (19.7, 24.7) |
| 3+ | 18.5 | (12.9, 24.1) | 23.4 | (17.9, 28.9) | 40.1 | (35.0, 45.3) | |
| χ24 (p-value) | 15.1 (.005)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 6.7 | (5.3, 8.0) | 7.5 | (5.3, 9.6) | 9.3 | (6.2, 12.5) |
| 3+ | 14.8 | (9.2, 20.4) | 16.6 | (11.0, 22.2) | 27.3 | (21.5, 33.0) | |
| PTSD | |||||||
| Disorder | None | 2.6 | (2.1, 3.1) | 4.9 | (3.9, 5.9) | 12.3 | (10.5, 14.1) |
| Prevalence | 1–2 | 6.4 | (5.3, 7.5) | 11.0 | (9.2, 12.8) | 22.5 | (19.9, 25.0) |
| 3+ | 16.4 | (11.2, 21.6) | 21.0 | (15.7, 26.4) | 30.9 | (26.2, 35.7) | |
| χ24 (p-value) | 20.1 (<.001)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 3.8 | (2.6, 5.0) | 6.1 | (4.2, 8.0) | 10.2 | (7.1, 13.2) |
| 3+ | 13.8 | (8.7, 18.9) | 16.1 | (10.7, 21.5) | 18.6 | (13.4, 23.9) | |
| ANX | |||||||
| Disorder | None | 3.6 | (3.0, 4.2) | 5.5 | (4.4, 6.5) | 10.3 | (8.5, 12.1) |
| Prevalence | 1–2 | 6.9 | (5.9, 7.9) | 11.9 | (10.1, 13.7) | 19.5 | (17.2, 21.9) |
| 3+ | 14.9 | (10.0, 19.8) | 20.6 | (15.0, 26.3) | 25.6 | (20.5, 30.7) | |
| χ24 (p-value) | 20.6 (<.001)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 3.3 | (2.0, 4.6) | 6.5 | (4.3, 8.6) | 9.2 | (6.3, 12.2) |
| 3+ | 11.3 | (6.4, 16.2) | 15.2 | (9.5, 20.8) | 15.3 | (9.9, 20.7) | |
Abbreviations: MDD, Major depressive disorder; PTSD, Post-traumatic stress disorder; ANX, Other anxiety disorders (panic disorder with and without agoraphobia, generalized anxiety disorder, and social phobia).
Significant at the .05 level
Prevalences and risk differences adjusted for age, nativity, and race-ethnicity.
Chi-square test (df=4) of the interaction between childhood adversities and past-year stressors in models for 12-month disorders.
Difference in the risk of disorders between individuals reporting 1–2 or 3+ past-year stressors, compared to no past-year stressors, across categories of childhood adversity.
Table 3.
Prevalences1 of 12-month psychiatric disorders among men, by level of exposure to past-year stressors and childhood adversity, NESARC 2004–2005
| Men (n=14,564) |
|||||||
|---|---|---|---|---|---|---|---|
| Childhood Adversities | |||||||
| None | 1–2 | 3+ | |||||
| Disorder | Past-Year Minor Stressors |
% | 95% CI | % | 95% CI | % | 95% CI |
| MDD | |||||||
| Disorder | None | 1.1 | (0.7, 1.5) | 2.6 | (4.1, 3.8) | 6.45 | (3.9, 9.0) |
| Prevalence1 | 1–2 | 3.0 | (2.4, 3.7) | 5.7 | (4.6, 6.8) | 10.3 | (8.1, 12.5) |
| 3+ | 6.4 | (4.4, 8.5) | 10.3 | (7.6, 12.9) | 22.0 | (18.2, 25.8) | |
| χ24 (p-value)2 | 22.3 (<.001)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 1.9 | (1.1, 2.7) | 3.1 | (1.6, 4.6) | 3.9 | (0.7, 7.1) |
| 3+ | 5.3 | (3.2, 7.4) | 7.7 | (4.7, 10.6) | 15.6 | (11.1, 20.1) | |
| PTSD | |||||||
| Disorder | None | 2.1 | (0.7, 1.6) | 2.4 | (1.5, 3.3) | 7.0 | (4.7, 9.3) |
| Prevalence | 1–2 | 1.9 | (1.4, 2.5) | 4.0 | (3.1, 4.9) | 7.3 | (5.6, 9.0) |
| 3+ | 4.6 | (2.7, 6.5) | 7.3 | (4.5, 9.8) | 15.6 | (12.3, 18.9) | |
| χ24 (p-value) | 10.0 (.040)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 0.8 | (0.1, 1.4) | 1.6 | (0.3, 2.9) | 3.0 | (−2.6, 3.3) |
| 3+ | 3.4 | (1.5, 5.4) | 4.8 | (2.0, 7.5) | 8.6 | (4.5, 12.7) | |
| ANX | |||||||
| Disorder | None | 1.5 | (1.0, 2.0) | 1.4 | (0.8, 1.9) | 5.1 | (3.2, 7.0) |
| Prevalence | 1–2 | 2.8 | (2.2, 3.4) | 5.6 | (4.5, 6.7) | 10.1 | (8.1, 12.2) |
| 3+ | 6.6 | (4.6, 8.6) | 9.6 | (7.2, 12.1) | 15.0 | (11.7, 18.3) | |
| χ24 (p-value) | 24.1 (<.001)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 1.3 | (0.5, 2.1) | 4.3 | (3.0, 5.5) | 5.0 | (2.4, 7.6) |
| 3+ | 5.1 | (3.0, 7.3) | 8.3 | (5.7, 10.8) | 9.9 | (6.2, 13.6) | |
|
Past-Year Major Stressors |
|||||||
| MDD | |||||||
| Disorder | None | 1.2 | (9.0, 1.6) | 3.1 | (2.3, 3.9) | 5.7 | (4.2, 7.2) |
| Prevalence | 1–2 | 4.5 | (3.5, 5.6) | 7.5 | (5.9, 9.1) | 15.5 | (12.6, 18.5) |
| 3+ | 10.9 | (6.5, 15.3) | 13.3 | (8.3, 18.3) | 28.4 | (21.9, 35.0) | |
| χ24 (p-value) | 25.8 (<.001)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 3.3 | (2.1, 4.5) | 4.4 | (2.7, 6.1) | 9.9 | (6.7, 13.0) |
| 3+ | 9.7 | (5.3, 14.1) | 10.2 | (5.1, 15.3) | 22.7 | (16.0, 29.5) | |
| PTSD | |||||||
| Disorder | None | 1.0 | (0.7, 1.4) | 2.0 | (1.5, 2.5) | 6.1 | (4.5, 7.7) |
| Prevalence | 1–2 | 3.3 | (2.4, 4.2) | 5.2 | (4.0, 6.3) | 9.5 | (7.6, 11.5) |
| 3+ | 5.3 | (2.6, 8.0) | 14.5 | (8.8, 20.3) | 21.6 | (15.6, 27.6) | |
| χ24 (p-value) | 14.1 (.007)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 2.2 | (1.3, 3.1) | 3.2 | (1.9, 4.4) | 3.4 | (0.9, 6.0) |
| 3+ | 4.3 | (1.5, 7.0) | 12.5 | (6.7, 18.3) | 15.5 | (9.1, 21.9) | |
| ANX | |||||||
| Disorder | None | 1.8 | (1.4, 2.2) | 3.1 | (2.3, 3.9) | 6.7 | (4.9, 8.4) |
| Prevalence | 1–2 | 3.7 | (2.8, 4.6) | 6.1 | (4.7, 7.6) | 12.7 | (10.2, 15.2) |
| 3+ | 9.0 | (5.2, 12.8) | 14.3 | (8.9, 19.7) | 14.8 | (9.9, 19.7) | |
| χ24 (p-value) | 11.1 (.026)* | ||||||
| Risk | None | - | - | - | |||
| Differences | 1–2 | 1.9 | (0.9, 2.9) | 3.0 | (1.3, 4.7) | 6.1 | (3.0, 9.1) |
| 3+ | 7.2 | (3.3, 11.1) | 11.2 | (5.7, 16.7) | 8.2 | (3.1, 13.2) | |
Abbreviations: MDD, Major depressive disorder; PTSD, Post-traumatic stress disorder; ANX, Other anxiety disorders (panic disorder with and without agoraphobia, generalized anxiety disorder, and social phobia).
Significant at the .05 level
Prevalences and risk differences adjusted for age, nativity, and race-ethnicity.
Chi-square test (df=4) of the interaction between childhood adversities and past-year stressors in models for 12-month disorders.
Difference in the risk of disorders between individuals reporting 1–2 or 3+ past-year stressors, compared to no past-year stressors, across categories of childhood adversity.
Stress Sensitization Effects
To examine the stress sensitization hypothesis, we examined interactions between exposure to CAs and past-year stressful events to determine whether CA exposure modified the effect of life events on risk for mood and anxiety disorders.
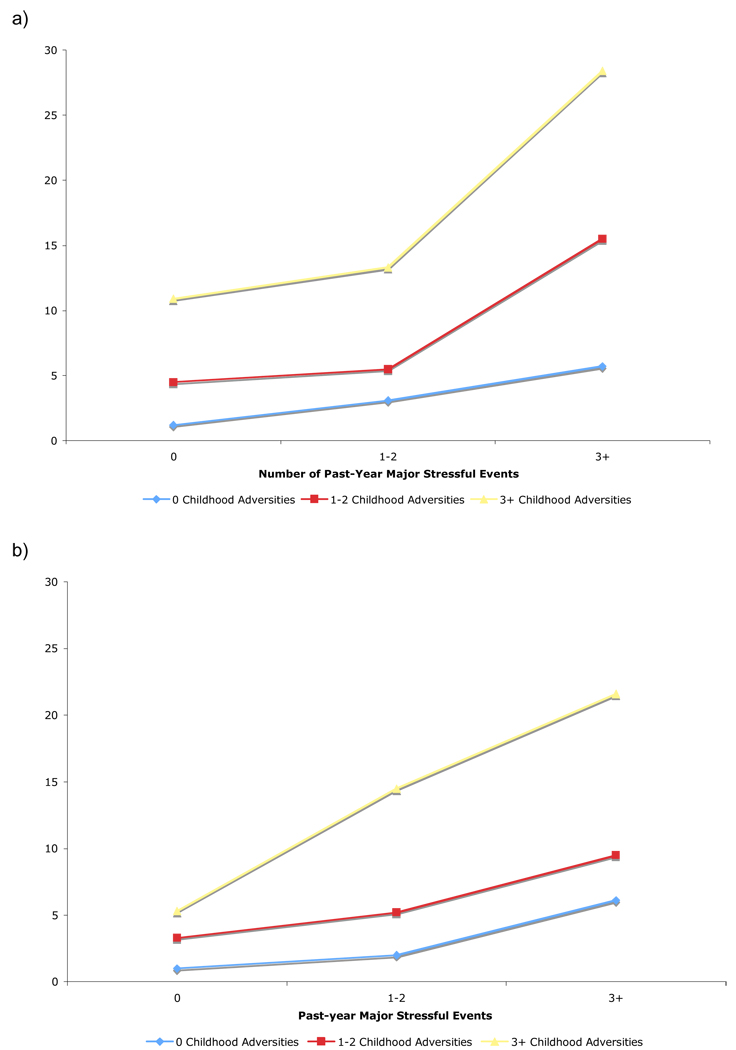
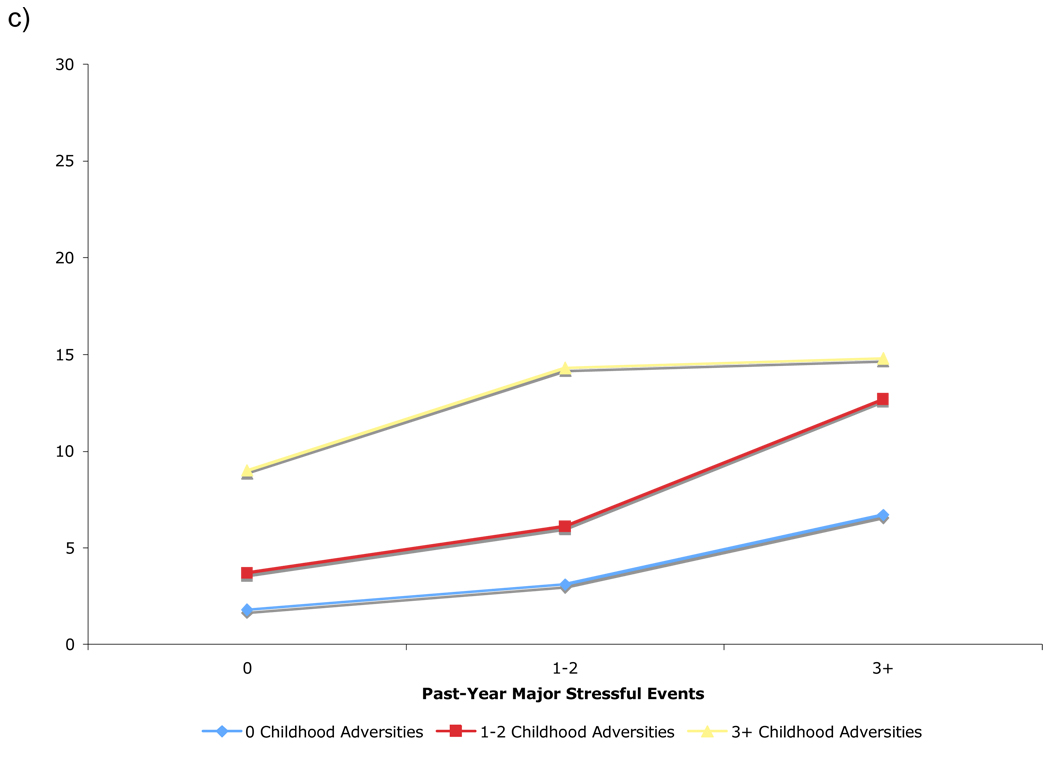
Major Depressive Episodes
We find support for stress sensitization in MDE among both women (χ24=15.1, p=.005) and men (χ24=25.8, p<.001) exposed to major life events. (Figure 1) Stress sensitization effects are evident for women with 3+ major events (compared to women with no past-year major events). The risk difference of MDE for women with 3+ major events vs. no major events is significantly higher among women with a history of 3+ CAs (27.3%) than among women with no CAs (14.8%, p=.002), and 1–2 CAs (16.6%, p=.012). (Table 2) Among men, the risk difference of MDE for those with 3+ major events vs. no major events is significantly higher among those exposed to 3+ CAs (22.7%) than men with 1–2 CAs (10.2%, p=.005) and with no CAs (9.7%, p<.001). (Table 3) The risk difference of MDE among men exposed to 1–2 major life events also is significantly higher among those exposed to 3+ CAs (9.9%) than men with 1–2 CAs (4.4%, p=.004) and with no CAs (3.3%, p<.001).
Figure 1.
The prevalence of 12-month (a) major depressive episodes, (b) PTSD, and (c) other anxiety disorders among men according to past-year exposure to major stressful life events and exposure to childhood adversities.
We also find stress sensitization effects for MDE among men exposed to minor life events (χ24=22.3, p<.001). The risk difference of MDE among men exposed to 3+ minor life events vs. no events is significantly higher among those exposed to 3+ CAs (15.6%) than men with 1–2 CAs (7.7%, p=.006) and with no CAs (5.3%, p<.001).
PTSD
We also find significant stress sensitization effects associated with 12-month PTSD among women (χ24=20.1, p<.001) and men (χ24=14.1, p=.007) exposed to major life events. For women, stress sensitization is evident for respondents who experienced 1–2 major events, where the risk difference of PTSD is greater among respondents with 3+ CAs (10.2%) than among those with 1–2 CAs (6.1%, p=.022) and no CA exposure (3.8% p<.001). Among men, however, stress sensitization is evident among those with past-year exposure to 3+ major events. The risk difference of PTSD is greater among men with both 3+ CAs (15.5%, p=.003) and 1–2 CAs (12.5%, p=.018) than among men with no CAs (4.3%).
Stress sensitization effects associated with PTSD are also evident among men exposed to minor life events (χ24=10.0, p=.040). The risk difference of PTSD is greater among men with 3+ CAs (8.6%) than among men with 0 CAs (3.4%, p=.025).
Other Anxiety Disorders
Significant stress sensitization effects associated with 12-month anxiety disorders were also present among women (χ24=20.6, p<.001) and men (χ24=11.1, p=.026) exposed to major life events. For women exposed to 1–2 major life events, the risk difference was significantly greater among those with 3+ CAs (9.2%, p<.001) and 1–2 CAs (6.5%, p=.011) than among women with no CAs (3.3%). We find a similar pattern in men. Among men exposed to 1–2 major life events, the risk difference of anxiety disorders is higher in those with 3+ CAs (6.1%) than men with no CA exposure (1.9%, p=.012).
Finally, we find evidence of stress sensitization among men exposed to 1–2 minor life events (χ24=24.1, p<.001). The risk difference of anxiety disorders is higher among men with 1–2 CAs (4.3%, p<.001) and with 3+ CAs (5.0%, p=.011) as compared to men with no CA exposure (1.3%).
Gender Differences
To examine gender differences in stress sensitization effects, we tested 3-way interactions between CA, adult stressful events, and gender in predicting mood and anxiety disorders. The only significant interaction of the six examined is between CA, major life events, and gender in predicting PTSD (χ24=14.1, p=.024). As reported above, stress sensitization effects were evident among women exposed to 1–2 major life events and among men exposed to 3+ major life events.
Perceived Stress as a Function of Life Events and Childhood Adversity
Respondents with greater exposure to CAs had higher perceived stress scores than respondents with fewer CAs at a given level of past-year stressful life events. (Table 4) There was a significant interaction between CA and past-year major (χ24=94.6, p<.001) and minor life events (χ24=32.0, p<.001) in predicting perceived stress. As exposure to past-year stressful events increases, the corresponding increases in perceived stress are greater among individuals reporting 3+ CAs than among individuals with no CAs. Perceived stress was significantly higher among women with greater exposure to CAs in 17 of 18 (94.4%) possible comparisons within a given level of past-year life events and in 11 of 18 (61.1%) comparisons among men.
Table 4.
Mean perceived stress scores and 95% CI by type and level of exposure to past-year stressors and childhood adversity, separately for women and men (n=33,536), NESARC 2004–2005
| Women (n=20,089) |
||||||
|---|---|---|---|---|---|---|
| MINOR STRESSORS | MAJOR STRESSORS | |||||
| Childhood Adversities | Childhood Adversities | |||||
| Past-Year Stressors |
None | 1–2 | 3+ | None | 1–2 | 3+ |
| None | 7.4 (7.2,7.5) | 7.8 (7.6, 8.0) | 8.6 (8.3, 8.9) | 7.3 (7.2, 7.4) | 7.7 (7.6, 7.9) | 8.3 (8.1, 8.5) |
| 1–2 | 7.7 (7.6, 7.8) | 8.2 (8.1, 8.4) | 8.7 (8.6, 8.9) | 8.1 (7.9, 8.2) | 8.8 (8.6, 8.9) | 9.4 (9.2, 9.6) |
| 3+ | 8.5 (8.2, 8.7) | 9.4 (9.1, 9.7) | 10.3 (10.0, 0.6) | 9.5 (9.1, 10.0) | 10.0 (9.6, 10.4) | 11.0 (10.5, 11.4) |
| Men (n=14,564) | ||||||
| MINOR STRESSORS | MAJOR STRESSORS | |||||
| Childhood Adversities | Childhood Adversities | |||||
|
Past-Year Stressors |
None | 1–2 | 3+ | None | 1–2 | 3+ |
| None | 7.1 (6.9, 7.3) | 7.3 (7.1, 7.5) | 7.7 (7.5, 8.0) | 7.0 (6.9, 7.1) | 7.3 (7.2, 7.5) | 7.6 (7.4, 7.8) |
| 1–2 | 7.3 (7.2, 7.4) | 7.7 (7.5, 7.8) | 8.2 (8.0, 8.4) | 7.6 (7.4, 7.8) | 7.8 (7.6, 8.0) | 8.7 (8.5, 8.9) |
| 3+ | 7.8 (7.5, 8.1) | 8.3 (8.0, 8.6) | 9.5 (9.2, 9.8) | 8.9 (8.3, 9.4) | 9.2 (8.7, 9.7) | 10.1 (9.6, 10.6) |
DISCUSSION
Our results provide empirical support for stress sensitization effects—an interaction between CA and adult stress—in liability to mood and anxiety disorders in both men and women in a national sample. Our findings are consistent with prior research suggesting that risk for MDEs among women exposed to stressful life events is heightened among those with a history of CA (Espejo et al., 2006, Hammen et al., 2000, Kendler et al., 2004). We extend this literature by documenting stress sensitization effects for PTSD and other anxiety disorders, as well as among men. Although the pathways linking CAs to later stress vulnerability remain to be identified, accumulating evidence suggests that CA exposure is associated with chronic dysregulation in the physiological stress response system that may increase both reactivity to stress and risk for mood and anxiety disorders (Heim and Nemeroff, 2001), thereby representing a generalized diathesis to psychopathology that persists across the life-course (Monroe and Simons, 1991).
One of the most consistent findings in our analysis was that stress sensitization effects occurred among individuals who experienced three or more CAs. This was true for MDEs, PTSD, and ADs. To our knowledge, these findings are novel, as previous studies have not examined degree of CA exposure as a predictor of stress sensitization. Because co-occurring CAs tend to be severe and are strongly associated with poor mental health outcomes (Arata et al., 2007, Finkelhor et al., 2007), these results suggest that CAs may need to cross a severity threshold to impact later stress vulnerability.
The basic pattern of findings is consistent for women and men: stress sensitization effects in liability to MDEs, PTSD, and other anxiety disorders are present for both women and men exposed to three or more CAs. Gender differences were found, however, in the number of stressful life events needed to trigger such effects. Fewer major events are necessary to trigger stress sensitization effects in liability to PTSD among women compared to men. This finding may reflect differences in the severity of events experienced by women and men. For example, sexual assault is strongly associated with PTSD onset and is more prevalent among women (Kessler et al., 1995). The opposite pattern occurred for MDEs, however, such that stress sensitization effects were evident for men with fewer past-year major events than women. It is possible that sensitization effects are triggered when there is a match between the domain of the recent stressor (e.g., interpersonal violence) and of the CA event (e.g., physical abuse) (Hammen and Goodman-Brown, 1990, Rudolph and Flynn, 2007), or that individuals are at greater risk for psychopathological reactions that are similar to their response to the initial CA. Either of these possibilities could have produced the observed gender differences in the magnitude of current stressors necessary to trigger sensitization effects. Because this is the first study to examine stress sensitization effects in both men and women, these findings warrant replication in future research.
One noteworthy difference between our findings and the results of prior research involves the level of current exposure to stressful life events that generates stress sensitization effects. Such effects were most commonly observed in our analysis among respondents exposed to three or more major life events. In contrast, previous studies have found increased risk for MDEs among females exposed to CAs (compared to those with no exposure) at low levels of current stress, but no difference in MDE risk at high levels of stress (Hammen et al., 2000, Rudolph and Flynn, 2007). These previous studies utilized smaller clinical and/or community samples of young women, which may have led to this discrepancy. It also may have resulted from differences in the way that stress was operationalized: the current study focused exclusively on stressful life events, whereas both chronic stressors and acute events were assessed in studies that reported sensitization at low levels of exposure to stressors (Hammen et al., 2000, Rudolph and Flynn, 2007). Consistent with our findings, however, Kendler and colleagues (2004) also found that the difference in MDE risk between those with and without CA exposure is greater for individuals who experienced high levels of stress, using a measure of both chronic and acute stress exposure. We anticipate that advancements in the measurement of life stress (Monroe, 2008) will facilitate the ascertainment of the level of stress exposure needed to elicit stress sensitization effects, in part, by ensuring comparability in the assessment of stress exposure across future studies.
Finally, we document an interaction between CA and adult exposure to stressful life events in predicting stress appraisal. These findings suggest that individuals exposed to CAs may be more vulnerable to mood and anxiety disorders following adult stressful events because they perceive those events to be more overwhelming or unmanageable. Moreover, they suggest that greater emotional reactivity to daily events among individuals with a history of CAs (Glaser et al., 2006, Wichers et al., 2009) may result from more negative appraisals of those events, a possibility that remains to be examined directly in future research.
Several limitations of the current study must be acknowledged. The first involves our use of a stress checklist rather than a stressor interview (Hammen, 1991), which did not allow us to ascertain the severity of events or the temporal sequencing of stressors and disorder onset. We attempted to address this first concern by categorizing events as minor and major stressors, although this strategy undoubtedly involved some degree of misclassification. Moreover, because we examined associations between past-year stressors and 12-month disorders, it is possible that some disorder onsets occurred prior to stressor occurrence. Second, this study is limited by retrospective assessment of CAs. Past research suggests that recall bias of CAs primarily involves underreporting of CA (Hardt and Rutter, 2004), and that the presence of current psychopathology does not result in reporting or memory biases that inflate estimates of the prevalence of CAs (Brewin et al., 1993). Moreover, prior work examining the validity of retrospective reports of CAs finds that although such reports may be biased, they are sufficiently valid to be used in epidemiologic research, particularly when CAs are well-defined and do not rely on subjective interpretations (Brewin et al., 1993, Hardt and Rutter, 2004). Underreporting of CAs in this study would have resulted in attenuation of the associations between CAs and psychopathology, whereas over-reporting of CA occurrence among individuals with past-year disorders would have led to an overestimation of these associations. Consequently, our findings therefore warrant replication in prospective studies. Third, because measures of perceived stress have been found to overlap with measures of distress (Dohrenwend and Shrout, 1985) our perceived stress measure may have been confounded by current mood and anxiety disorders. Our findings regarding stress sensitization effects on perceived stress should thus be interpreted with caution.
An alternative interpretation of the interactions between CAs and adult stressful life events in predicting psychopathology is that adult stressful life events act as mediators of the association between CAs and psychiatric disorders. In other words, CAs are associated with adult psychopathology because they increase the risk for stressful events in adulthood (Hazel et al., 2008). Kraemer and colleagues (2008) suggest that when a correlation exists between two exposures (e.g., CAs and adult stressors), a statistical interaction between those exposures in predicting an outcome should be interpreted as evidence of mediation rather than moderation. Therefore, tests of the stress sensitization hypothesis are needed that focus on adult stressors which are uncorrelated with prior adversities (e.g., so-called “independent” life events (Brown and Harris, 1978)). Such tests would not be subject to this alternative interpretation.
Our findings have implications for theory, research and practice. First, we find that exposure to CAs increases perceived stress and vulnerability to psychopathology in the context of later stressful life events, providing support for stress sensitization as an etiological model linking CA exposure to a range of mood and anxiety disorders. Although prior research on stress-diathesis models of psychopathology have conceptualized the diathesis as an innate characteristic of the individual, such as a genetic vulnerability (Caspi et al., 2003, Monroe and Simons, 1991), the current findings suggest that a generalized diathesis to psychopathology may arise from environmental exposures early in life. Second, these findings point to important avenues for future research. The extent to which stress sensitization plays a role in the development of other psychiatric disorders, such as substance use disorders, represents one such area. Most importantly, the mechanisms underlying stress sensitization effects remain to be identified. It is likely that these mechanisms operate through a variety of cognitive, emotion regulation, and physiological pathways (Hammen et al., 2000, Repetti et al., 2002, Rudolph and Flynn, 2007). Identification of such mechanisms is critical to the development of interventions aimed at reducing the deleterious mental health consequences of CAs. Finally, our findings suggest that individuals with a history of CA exposure represent potential targets for interventions aimed at reducing stress-related psychiatric morbidity in adulthood.
Acknowledgement
This research was supported by the Robert Wood Johnson Foundation [Grant Number 053572] and by the National Institutes of Health [Grant Numbers MH087544, MH078928, MH070627, and DA080887].
Footnotes
Disclosure: The authors have no competing interests to report.
REFERENCES
- Agretsi A. Categorical data analysis. 2nd ed. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- Arata CM, Langhinrichsen-Roling J, Bowers D, O'Brien N. Differential correlates of multi-type maltreatment among urban youth. Child Abuse and Neglect. 2007;31:393–415. doi: 10.1016/j.chiabu.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Hondelsman L, Foote J, Lovejoy M. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bremmer JD, Southwick SM, johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. American Journal of Psychiatry. 1993;150:235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiologic study. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: A reappraisal of retrospective reports. Psychological Bulletin. 1993;113:82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: A study of psychiatric disorders in women. New York: Free Press; 1978. [Google Scholar]
- Caspi A, Sugden K, Moffit TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;5631:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse and Neglect. 2007;31:211–229. doi: 10.1016/j.chiabu.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Shrout PE. "Hassles" in the conceptualization and measurement of life stress variables. American Psychologist. 1985;40:780–785. [Google Scholar]
- Dougherty LR, Klein DN, Davila J. A growth curve analysis of the course of dysthymic disorder: The effects of chronic stress and moderation by adverse parent-child relationships and family history. Journal of Consulting and Clinical Psychology. 2004;72:1012–1021. doi: 10.1037/0022-006X.72.6.1012. [DOI] [PubMed] [Google Scholar]
- Espejo EP, Hammen C, Connolly NP, Brennan PA, Najman JM, Bor W. Stress sensitization and adolescent depressive severity as a function of childhood adversity: A link to anxiety disorders. Journal of Abnormal Child Psychology. 2006;35:287–299. doi: 10.1007/s10802-006-9090-3. [DOI] [PubMed] [Google Scholar]
- Fantuzzo JW, DePaola LM, Lambert L, Martino T, Anderson G, Sutton S. Effects of interparental violence on the psychological adjustment and competencies of young children. Journal of Consulting and Clinical Psychology. 1991;59:258–265. doi: 10.1037//0022-006x.59.2.258. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod R, Turner H. Polyvictimization and trauma in a national longitudinal cohort. Development and Psychopathology. 2007;19:149–166. doi: 10.1017/S0954579407070083. [DOI] [PubMed] [Google Scholar]
- Gauthier L, Stollak G, Messé L, Aronoff J. Recall of childhood neglect and abuse as differential predictors of current psychological functioning. Child Abuse and Neglect. 1996;20:549–559. doi: 10.1016/0145-2134(96)00043-9. [DOI] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research. 2006;61:229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Kay W, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003a;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton W. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2008 doi: 10.1038/mp.2008.41. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou SP, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003b. [Google Scholar]
- Green JG, McLaughlin KA, Berglund P, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. doi: 10.1001/archgenpsychiatry.2009.186. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. The generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C, Goodman-Brown T. Self-schemas and vulnerability to specific life stress in children at risk for depression. Cognitive Therapy and Research. 1990;14:215–227. [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68:782–787. [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology. 2006;115:730–741. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, Najman JM. Early childhood adversity and adolescent depression: the mediating role of continued stress. Psychological Medicine. 2008;38:581–589. doi: 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events, and risk for major depression in women. Psychological Medicine. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex MJ, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27:S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber M, Sampson NA, Zaslavsky A, Kessler RC. Childhood adversities and adult psychopathology in the National Comorbidity. Psychological Medicine. doi: 10.1017/S0033291709991115. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Buka L, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: Implications for depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The long-term impact of the physical, emotional, and sexual abuse of children: A community study. Child Abuse and Neglect. 1996;20:7–21. doi: 10.1016/0145-2134(95)00112-3. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–336. [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN: Professional Software for Survey Data Analysis [computer program] Research Triangle Park, N.C.: Research Triangle Institute; 2008. [Google Scholar]
- Rothman KJ. Synergy and antagonism in cause-effect relationships. American Journal of Epidemiology. 1974;99:385–388. doi: 10.1093/oxfordjournals.aje.a121626. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Walker AM. Concepts of interaction. American Journal of Epidemiology. 1980;112:467–470. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Flynn M. Childhood adversity and youth depression: Influence of gender and pubertal status. Development and Psychopathology. 2007;19 doi: 10.1017/S0954579407070241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: Results from a population-based sample of men and women. Child Abuse and Neglect. 2001;31:517–530. doi: 10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternberg KJ, Lamb ME, Guterman E, Abbott CB. Effects of early and later family violence on children’s behavior problems and depression: A longitudinal, multi-informant perspective. Child Abuse and Neglect. 2006;30:283–306. doi: 10.1016/j.chiabu.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Wichers M, Schrijvers D, Geschwind N, Jacobs N, Myin-Germeys I, Thiery E, Derom C, Sabbe B, Peeters F, Delespaul P, van Os J. Mechanisms of gene-environment interactions in depression: evidence that genes potentiate multiple sources of adversity. Psychological Medicine. 2009;39:1077–1086. doi: 10.1017/S0033291708004388. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sexual abuse of Afro-American and White American women in childhood. Child Abuse and Neglect. 1985;9:507–519. doi: 10.1016/0145-2134(85)90060-2. [DOI] [PubMed] [Google Scholar]