Abstract
Objective
This article explores the effect of conflicting information, defined as contradictory information about medication topics from different sources, on medication adherence in a sample of chronically ill patients. We specifically investigate whether conflicting information and physician support directly affect medication adherence or whether the effect is mediated by adherence self-efficacy and outcome expectations for medications.
Methods
Vasculitis patients (n=228) completed two on-line questionnaires which contained measures of conflicting information, adherence self-efficacy, outcome expectations, physician support, and medication adherence. We conducted a mediation analysis using a bootstrapping approach to generate point estimates and 95% confidence intervals to test the significance of each mediated effect.
Results
A majority of patients (51.3%) received conflicting medication information. Conflicting information had a direct negative effect on medication adherence, which was not mediated by self-efficacy or outcome expectations. Alternatively, self-efficacy mediated the positive effect of physician support on medication adherence.
Conclusion
Patients who encounter conflicting medication information are less adherent to their medications. The presence of a supportive physician may counteract the negative effect of conflicting medication information.
Practice Implications
Physicians should initiate conversations about conflicting medication information with their patients. Consensus-based guidelines that address medication discrepancies may also reduce the availability of conflicting information.
Keywords: conflicting information, medication adherence, information seeking, social support, self-efficacy
1. Introduction
Health-related information helps patients cope with illness by increasing knowledge, reducing feelings of uncertainty, and enhancing emotional and social adjustment [1]. When seeking information, patients have a number of sources from which to choose, including health professionals like physicians [2-5], pharmacists [3,6], and nurses [2,7,8], health-related websites [4,5], patient information leaflets [4], mass media sources such as newspapers, magazines, and television [2,4,5], and family and friends [2,6,9]. The opportunity to encounter conflicting information arises when health information is obtained from more than one source and may vary based on whether information is received passively (i.e. from two different physicians) or actively obtained by patients during information searches (i.e. Internet information contradicts physician recommendations).
A burgeoning, primarily qualitative, literature has begun to document the extent to and conditions under which chronic disease patients receive conflicting information. The results from these studies demonstrate that people living with chronic conditions, such as cancer [7,10], cardiopulmonary disease [3], rheumatic disease [11], low back pain [12] as well as mental illness [13] receive conflicting information about their illness and its management. Furthermore, several studies have documented that patients receive conflicting information about their medications [11,14,15], although no published research has focused specifically on patients with rare health conditions.
Preliminary evidence suggests that receipt of conflicting information may negatively influence patients' perceptions of care [16], increase anxiety [13], alter risk perceptions [17], and complicate patients' ability to assess the reliability of information sources [12]. Health behavior models like the Information-Motivation-Behavioral Skills (IMB) Model [18] offer insight into the potential mechanisms through which conflicting information may affect adherence. Specifically, the IMB model posits that adherence information, or factual information about medication adherence, has a positive effect on both adherence self-efficacy and medication adherence, and that self-efficacy acts as a mediator of the relationship between information and adherence. The IMB model also posits that motivation (i.e. perceptions of social support and adherence outcome expectations) influence adherence directly and indirectly through increased self-efficacy. Four cross-sectional tests of the model lend support to the posited relationships [19-22], although the effect of information appears to be mediated through increased self-efficacy as opposed to having a direct effect on medication adherence.
1.1 Significance
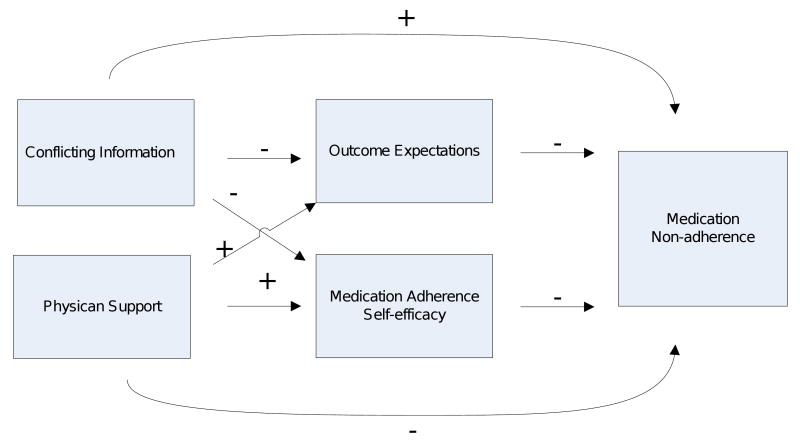
In order to build upon the limited understanding of how conflicting information affects medication adherence, we collected longitudinal survey data from a sample of chronically ill patients. The IMB model served as the organizing framework for our conceptual model (Figure 1), in which we hypothesize that a greater amount of conflicting information will result in more medication non-adherence. Additionally, we believe that self-efficacy and outcome expectations will partially mediate the relationship between conflicting information and non-adherence. Specifically, we posit that patients who receive more conflicting information will have decreased self-efficacy and more negative outcome expectations for medications, which will result in more non-adherence. Moreover, we hypothesize that social support from patients' physicians will result in less medication non-adherence and that this effect will be partially mediated through increased self-efficacy and more positive outcome expectations for medications.
Figure 1.
Predicted relationships among conflicting information, physician support, outcome expectations, adherence self-efficacy, and medication non-adherence
2. Methods
2.1 Overview
All data were collected as part of the Accessing Social Support in Symptom Treatment (ASSIST) Study, which assessed the information seeking behaviors of vasculitis patients. Vasculitis is a rare autoimmune disease that causes blood vessel inflammation and is characterized by an unpredictable course of relapse and remission. The ASSIST Study consisted of two on-line questionnaires administered three months apart. To be eligible for participation, patients must have a self-reported diagnosis of vasculitis, be at least 18 years old, be able to read and write in English, have Internet access, and currently take at least one vasculitis medication. This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
We recruited participants for the ASSIST Study in four ways. We distributed study brochures at a vasculitis patient conference, which yielded 45 interested patients, 39 of whom were eligible. Additionally, we mailed study announcement letters to known vasculitis patients (n=361) who were part of the Glomerular Disease Collaborative Network (GDCN). The GDCN is a collaboration of the University of North Carolina and community nephrology offices across the southeastern United States. Of the 67 GDCN patients who returned correspondence, 38 were eligible to participate. For our third recruitment method, we contacted physician-diagnosed vasculitis patients (n=124) who were part of two studies at the Thurston Arthritis Research Center; 29 of the 39 (74%) patients who responded were eligible and interested. Our last method involved posting general announcements (including a study podcast) on vasculitis websites and in patient newsletters. Information about the study was also distributed at local support group meetings and circulated on eight vasculitis email groups and list serves; 147 of the 155 patients who contacted us in response to these general announcements were eligible.
Thus, 306 patients, 253 (83%) of whom were eligible and interested, responded to our various recruitment efforts. Reasons for ineligibility included not taking vasculitis medications (n=25), patient death (n=9), not having access to the Internet (n=9), being too busy to participate (n=4) and not having a diagnosis of vasculitis (n=1). An additional five patients refused to participate after learning more about the study.
Two-hundred thirty-two of the 253 eligible patients (91.7%) completed the one-hour baseline questionnaire. Reasons for non-completion included technical issues (n=7), being too sick (n=4) or too busy (n=3) to participate, or never responding to study correspondence (n=7). When compared with completers, non-completers were not significantly different in terms of gender or self-reported vasculitis type.
Our three-month follow-up response rate was 98.2%; only four of the 232 participants did not complete the second questionnaire. One participant experienced technical difficulties and the remaining three did not respond to study correspondence. Participants received a ten dollar gift card after completing the second questionnaire.
2.2 Measures
The three-month follow-up questionnaire contained measures for our mediating variables (adherence self-efficacy, outcome expectations) and our outcome variable (medication non-adherence), while the independent variables (conflicting medication information and physician support) and sociodemographic variables were measured as part of the baseline questionnaire.
Medication non-adherence
To measure medication non-adherence, we used the Vasculitis Self-Management Survey (VSMS) medication adherence subscale, which asks respondents to describe their medication taking behavior during the past four weeks [23]. The scale consists of seven items measured on a five-point Likert scale; the response scale for six items ranges from 1= “none of the time” and 5 = “all of the time,” while the seventh item (percentage of medication doses taken exactly as directed) ranges from 1 = “0-24%” and 5 = “100%.” The VSMS medication adherence subscale has demonstrated acceptable internal consistency (Cronbach α = 0.77) and test-retest reliability of 0.60 in a previous study of vasculitis patients [23]. Higher summary scores indicate greater non-adherence. Cronbach's alpha was 0.89 in our study.
Adherence self-efficacy
We used the difficulty subscale from the Self-Efficacy for Appropriate Medication Use Scale (SEAMS) [24] to measure adherence self-efficacy. The difficulty subscale asked respondents to rate their level of confidence to take medications correctly in a number of difficult situations, including when they have a busy day planned, are away from home, or have multiple medications to take. Originally, the seven difficulty items were measured on a three-point Likert-scale ranging from 1 = “not confident” to 3 = “very confident.” We changed the response scale from three points to five points in an attempt to capture greater variability in adherence self-efficacy. The modified scale ranged from 1= “not at all confident” to 5= “very confident.” We created a summary score by averaging item responses; higher scores represent greater levels of adherence self-efficacy (Cronbach α= 0.88).
Outcome expectations
Patients' medication-related outcome expectations were measured using the specific-necessity subscale of the Beliefs about Medicines Questionnaire (BMQ) [25]. The specific-necessity subscale includes five items that, “represent the perceived role of medication in protecting against deterioration of present and future health status of the patient” (p. 20) and has demonstrated good internal consistency and test-retest reliability in previous studies [25]. Response options ranged from 1= “strongly disagree” to 5= “strongly agree.” Again, we created a summary score by averaging item responses. In this case, higher summary scores indicated stronger patient beliefs that vasculitis medications were necessary to maintain health (Cronbach α=0.80).
Conflicting information
Because a conflicting medication information scale has not been reported in the literature, we developed six items that asked respondents to report whether they had ever received conflicting information about: the time of day to take their medications, how to take their medications, proper dosing, duration (i.e. 6 months versus 1 year), side effects, and side effect severity. Respondents were asked to include conflicting information that they received from any two sources (i.e. two physicians, a physician and the Internet) and could choose between the following response options: “have not received conflicting information”, “have received conflicting information”, or “don't remember.” We recoded “don't remember” responses as missing and then calculated a summary score by adding the six items. Using tetrachoric correlations, we found that all scale items loaded at 0.70 or greater onto one factor, which indicated a one-factor solution. KR-20, a measure of internal consistency, was 0.75.
Physician support
Participants completed four items about perceived adherence support from their primary vasculitis physician. Specifically, participants indicated how often their physician supported them in taking their vasculitis medications, shared new information about vasculitis medicines, provided helpful hints about how to deal with the side effects of vasculitis medicines, and provided enough support when it came to taking the medications as prescribed. Response options ranged from 1= “does not do this” to 4= “does this a lot.” Respondents could also select “N/A” if they thought the question did not apply to their situation. In these cases, we recoded N/A as a “1” because the physician did not provide that type of support. We created a summary score by averaging the four items; higher scores reflected more adherence support (Cronbach α=0.80).
For the multiple-item scales described above, summary scores were not calculated if more than 25 percent of the scale items were missing. In those cases, participants' scores were treated as missing.
Socio-demographics
Participants answered one item each about gender, race, age, education (in years), year of vasculitis diagnosis, self-reported vasculitis type, and health insurance status (insured versus not insured). Participants also indicated the time period since their last vasculitis relapse or flare, with 1= “I am currently experiencing a flare-up or relapse”, 2= “less than 1 year ago”, 3= “more than 1 year ago”, and 4= “I have never experienced a relapse or flare-up or relapse.”
2.3 Data analysis
We used SAS version 9.2 to conduct all analyses. First, we calculated descriptive statistics, including skewness and kurtosis. Then, we used a bootstrapping approach [26] to determine whether self-efficacy and outcome expectations mediated the effects of conflicting information and physician support on medication adherence, controlling for age, gender, education, and time since last flare. We chose bootstrapping over a causal steps approach to test for mediation for several reasons. First, bootstrapping is a nonparametric procedure that does not impose the constraint of multivariate normality; thus, this technique is more robust for situations in which data are skewed. Because most vasculitis patients are relatively adherent [23], a mediation approach that was less affected by skewness offered certain advantages. Second, bootstrapping calculates an overall point estimate and confidence interval for each mediated (indirect) effect by generating a sampling distribution from 5,000 samples (with replacement) from the full data set, which can reduce Type I error rates [26]. Third, bootstrapping produces contrasts to test the relative strength of each mediated effect; multiple mediators cannot be contrasted using a conventional causal steps approach [27]. Last, bootstrapping with bias-corrected confidence intervals has greater power to detect significant specific indirect effects; power exceeds 0.80 for samples of 250 [28]. We used bias-corrected 95% confidence intervals to determine whether the point estimates for each indirect effect were significant; confidence intervals that contained zero were considered insignificant.
3. Results
3.1 Sample characteristics
Table 1 summarizes the demographic and clinical characteristics of the final study sample (n=228). A majority of participants were female (70%), white (91%), and had a diagnosis of ANCA-associated granulomatous vasculitis (59%), which is the most common form of vasculitis. On average, participants were middle-aged (M= 51.0 years) and reported some college education (M= 15.6 years of education). Patients had been living with vasculitis for an average of 6.4 years and 28.4% were experiencing a relapse or flare at the time of the baseline survey. Ninety-three percent of patients reported having health insurance.
Table 1.
Participant characteristics (n=228)
| Characteristic | Mean (SD) or % | Range | Skewness | Kurtosis |
|---|---|---|---|---|
| Socio-demographic | ||||
| Age | 51.0 (13.3) | 21.0- 82.0 | -0.1 | -0.7 |
| Male | 30.3% | - | - | - |
| White | 91.3% | - | - | - |
| Education (in years) | 15.6 (2.8) | 4.0-22.0 | -0.2 | 1.7 |
| Clinical | ||||
| Self-reported vasculitis type | ||||
| ANCA-associated granulomatous | 59.2% | |||
| Churg Strauss Syndrome | 12.7% | |||
| Microscopic Polyangiitis | 7.9% | - | - | - |
| Takayasu Arteritis | 4.8% | |||
| Other | 15.4% | |||
| Years with disease | 6.4 (6.2) | 0.5-36.5 | -2.0 | 5.2 |
| Currently experiencing flare/relapse | 28.4% | - | - | - |
| Have health insurance | 93.4% | - | - | - |
| Other | ||||
| Medication non-adherence† | 1.7 (0.7) | 1.0-4.4 | 1.2 | 1.6 |
| Adherence self-efficacy‡ | 4.0 (0.9) | 1.0-5.0 | -0.6 | -0.4 |
| Outcome expectations* | 4.4 (0.6) | 2.2-5.0 | -1.3 | 1.6 |
| Conflicting information** | 1.6 (1.8) | 0.0-6.0 | 0.8 | -0.4 |
| Physician support*** | 3.1 (0.7) | 2.0-4.0 | 0.1 | -0.8 |
Response options ranged from 1 to 5; higher scores reflect greater non-adherence
Response options range from 1= ‘not at all confident’ to 5= ‘very confident’
Response options range from 1= ‘strongly disagree’ to 5= ‘strongly agree’
Higher scores reflect greater amounts of conflicting information
Response options range from 1= ‘does not do this’ to 4= ‘does this a lot’
3.2 Descriptive statistics
Descriptive statistics also are presented in Table 1. On average, patients' reported fairly low levels of medication non-adherence, whereas their adherence self-efficacy was quite high. Patients also had very positive outcome expectations for their medications. Additionally, patients' physicians provided them with a fair amount of adherence support.
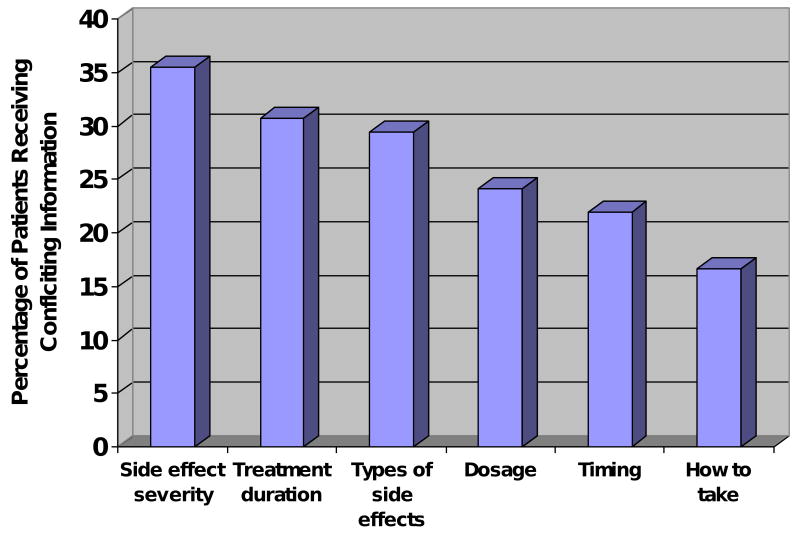
More than half of patients (51.3%) reported receiving conflicting information about at least one aspect of their vasculitis medications. In terms of the amount of conflicting information, 32.5% received no conflicting information, 36.4% received conflicting information about 1-3 medication topics, 14.9% received conflicting information about 4-6 medication topics, and 16.2% could not remember if they had received conflicting information. Patients were most likely to receive conflicting information about the severity of medication side effects (35.5%), the duration of treatment (30.7%), and the types of side effects associated with their vasculitis medications (29.4%). Conflicting information about correct dosage (24.1%), correct timing (21.9%), and how to take medications correctly (with or without food) (16.6%) was encountered less often (Figure 2).
Figure 2.
Percentage of patients receiving conflicting information by medication topic
3.3 Mediation analyses
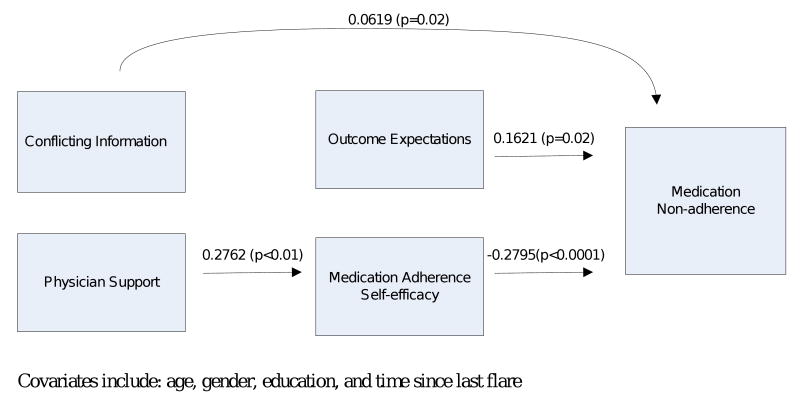
Table 2 displays the point estimates and p-values for the hypothesized relationships in our conceptual model (adjusted R2 = 0.25). Conflicting information was not significantly related to outcome expectations or adherence self-efficacy. In contrast, physician support was significantly positively related to self-efficacy but not outcome expectations. Both outcome expectations and self-efficacy were significantly related to medication non-adherence; however, outcome expectations were positively associated with non-adherence while self-efficacy had a negative association. The direct effect of conflicting information on non-adherence was significant, whereas physician support was not. Only one covariate, gender, was significantly associated with non-adherence; women were more nonadherent than men.
Table 2.
Summary of mediation results for the effect of conflicting information and physician support on medication non-adherence (5000 bootstrap samples)
| Estimate (SE) | t-statistic | p-value | |
|---|---|---|---|
| Independent variables to mediating variables | |||
| Conflicting information→ Outcome expectations | -0.0066 (0.0308) | -0.21 | 0.83 |
| Conflicting information→ Self-efficacy | -0.0185 (0.0412) | -0.45 | 0.65 |
| Physician support→ Outcome expectations | -0.0029 (0.0740) | -0.04 | 0.97 |
| Physician support→ Self-efficacy | 0.2762 (0.0990) | 2.79 | <0.01 |
| Mediating variables to dependent variable | |||
| Outcome expectations→ Medication non-adherence | 0.1621 (0.0697) | 2.32 | 0.02 |
| Self-efficacy→ Medication non-adherence | -0.2795 (0.0522) | -5.36 | <0.0001 |
| Independent variables to dependent variable (direct effects) | |||
| Conflicting information→ Medication non-adherence | 0.0619 (0.0279) | 2.22 | 0.03 |
| Physician support→ Medication non-adherence | -0.0422 (0.0684) | -0.62 | 0.54 |
| Covariates | |||
| Age | -0.0030 (0.0037) | -0.81 | 0.42 |
| Gender (males vs. females) | 0.2063 (0.0976) | 2.11 | 0.04 |
| Education (years) | -0.0000 (0.0163) | -0.00 | 1.00 |
| Time since last relapse/flare | 0.0492 (0.0450) | 1.09 | 0.28 |
| Adjusted R2=0.25 | |||
A more detailed examination of the mediated effects is presented in Table 3. As demonstrated by the confidence intervals, neither outcome expectations nor self-efficacy was a significant mediator of the relationship between conflicting information and non-adherence. Alternatively, self-efficacy did significantly mediate the relationship between physician support and non-adherence. Moreover, the significant contrast indicates that self-efficacy is a stronger mediator of physician support on non-adherence than outcome expectations.
Table 3.
Specific indirect effects of conflicting information and physician support on medication non-adherence
| Bias-corrected 95% CI | |||
|---|---|---|---|
| Specific indirect effect | Point estimate (SE) | Lower | Upper |
| Conflicting Information | |||
| Outcome expectations | -0.0011 (0.0132) | -0.0140 | 0.0082 |
| Self-efficacy | 0.0052 (0.0117) | -0.0161 | 0.0303 |
| Total indirect effect | 0.0041 (0.0132) | -0.0198 | 0.0326 |
| Contrast | |||
| Outcome expectations vs. self-efficacy | -0.0062 (0.0124) | -0.0325 | 0.0169 |
| Physician support | |||
| Outcome expectations | -0.0005 (0.0136) | -0.0245 | 0.0300 |
| Self-efficacy | -0.0772 (0.0319) | -0.1491 | -0.0231 |
| Total indirect effect | -0.0777 (0.0356) | -0.1554 | -0.0133 |
| Contrast | |||
| Outcome expectations vs. self-efficacy | 0.0767 (0.0338) | 0.0155 | 0.1470 |
4. Discussion and Conclusion
4.1 Discussion
We explored whether conflicting information and physician support affected medication adherence for patients living with a chronic illness. A majority (51.3%) of patients in our sample encountered conflicting information about their medications. Patients were most likely to receive conflicting information about the severity of medication side effects (35.5%) and treatment duration (30.7%). The fact that we measured six aspects of conflicting information, as opposed to just one, may explain why the percentage of patients encountering conflicting information in our study was more than double what has been found in previous studies [11,14,15]. Contrary to our expectations, receipt of conflicting information did not negatively impact adherence self-efficacy; instead, it had a direct positive relationship with non-adherence such that patients who received more conflicting information were more nonadherent than patients who received less conflicting information.
Using the Information-Motivation-Behavioral Skills Model [18] as a theoretical guide, we hypothesized that self-efficacy would act as a mediator between conflicting information and medication adherence, which was not supported by our data. We believe that the lack of mediation may have occurred because conflicting information is conceptually distinct from information. Specifically, conflicting information may work through pathways other than self-efficacy to affect behavior. To our knowledge, no theoretical model attempts to explain the effects of conflicting information on behavior; hence, we should integrate what is known from other theories and models to better understand the mechanisms through which conflicting information works to affect medication adherence. Specifically, the Cognitive-Social Health Information Processing (C-SHIP) model offers a useful starting point [29].
It is possible that information seeking style (categorized as monitors or blunters within the C-SHIP model), may moderate the effect of conflicting information on adherence. Patients that are high monitors actively scan for threatening health information, which can result in increased anxiety and, ultimately, avoidance behavior [29]. It is likely that high monitors would actively seek information about medication side effects, which may increase their chances of encountering conflicting information. In these cases, patients may become anxious about conflicting information and possibly less adherent. In contrast, high blunters (low monitors) tend to deny the existence of health risks and may be less likely to seek information from alternative sources. In the face of conflicting information, high blunters may defer to the source they believe is most credible, especially if that source provides positive information and assessments [30]. If patients view their physicians as the most credible source of medication information, which has been demonstrated in previous studies [5,31], then they may ignore conflicting information from other sources and adhere to their physicians' advice. Moreover, if high blunters truly ignore other sources of information, then their self-efficacy may be essentially unaffected. Thus, conflicting information may interact with patients' information seeking styles to influence affective states, such as anxiety, as well as medication adherence.
As we hypothesized, patients with supportive physicians felt more confident that they could take their medications in different difficult situations. This, in turn, led to greater medication adherence. This suggests that physicians who specifically discuss medications, including how to cope with side effects, increase patients' adherence self-efficacy. Because physicians are typically viewed as the most credible health information source [5,31], it may be especially important for them to discuss adherence with patients.
We were surprised that more positive outcome expectations for medications were associated with worse medication adherence. Lack of variability in outcome expectations may explain this finding. As noted earlier, patients' outcome expectations for medications were high (4.4 on a 5.0 scale), which is unsurprising given that vasculitis medications are critical to patient survival; there is an 80% mortality rate for untreated vasculitis within the first year of diagnosis [33]. Alternatively, our paradoxical finding could be due to the way instances of non-adherence are encoded in patients' memories. For example, patients with the strongest beliefs that their medications maintain health may be more likely to remember instances in which they did not take their medications correctly than patients who do not believe that their medications are health-protective. Thus, patients with the most positive outcome expectations for medications also may be the most likely to recall instances of non-adherence. On a cautionary note, this finding may not generalize to other patient populations, especially those patients whose survival is not so critically dependent on their medications (e.g. arthritis and hypertension patients).
Gender was the only significant covariate in our regression analyses. Women reported greater levels of non-adherence than men. Previous research about the effect of gender on medication adherence has been mixed [34]. However, it is well-known that women seek more health information than men [2,9,31]. In fact, our own research has demonstrated that female vasculitis patients consult more sources for medication information than male patients [32]. Thus, women may be more likely than men to encounter conflicting information, ultimately resulting in greater non-adherence.
4.2 Limitations
Our study findings should be interpreted with caution for several reasons. First, patients tend to over-report medication adherence on self-reported questionnaires [35], which may be due to patients forgetting instances of non-adherence as well as social desirability bias. However, this likely biased our result towards the null by weakening the relationship between conflicting information and adherence. Additionally, patients in our sample may be more likely to encounter conflicting information because they use the Internet, which was required for participation in the on-line survey. Thus, our results cannot be generalized to other patient populations. Moreover, our low response rate for mailed recruitment efforts represents a selection bias, which precludes our ability to generalize the study results to the greater vasculitis population. The relative lack of diversity (91% white, well-educated, 70% female) further limits the study's generalizability, although our sample characteristics are similar to those of other vasculitis study samples. Future research should attempt to recruit more diverse samples, including patients who do not use the Internet. Because we did not have a pen-and-paper version of the survey, we could not compare Internet users to non-Internet users.
Last, our conflicting information measure possesses several shortcomings. First the reliability and validity for this measure has not been established, although our factor analysis suggests a one-factor solution. Second, our measure asks about lifetime receipt of conflicting information and is thus subject to recall bias; we conservatively treated the 14.9% of patients who could not remember if they had received conflicting information as missing. Additionally, we could not verify whether patients actually received conflicting information or mistakenly perceived that concordant information was conflicting. This highlights the difficulty of accurately measuring conflicting information, especially when information can be both passively received and actively obtained. Last, it is possible that conflicting information received several years ago is not as salient as recently received conflicting information in terms of self-efficacy and medication adherence. These limitations could be addressed by designing a prospective study that tracks patients' information seeking behavior over a several month period after receiving a new prescription.
4.3 Conclusion
Conflicting medication information is a clear threat to patient medication adherence. If vasculitis patients receive conflicting medication information, then it is almost certain that patients with more common diseases encounter just as much, if not more, conflicting information, especially from media sources and family and friends [2]. For this reason, researchers should assess the extent to which patients with more common diseases, like cancer, diabetes, arthritis, and asthma, encounter conflicting medication information. Moreover, qualitative research that explores how patients resolve situations in which conflicting information is encountered is warranted. For example, it is possible that patients defer to their most trusted source or they may develop some type of hybrid medication taking behavior that incorporates advice from multiple trusted sources. This type of research could guide the development and refinement of theoretical models that explain how conflicting information affects self-management behavior. Lastly, physicians can increase patients' adherence self-efficacy by offering adherence-related advice and support. Patient perceptions of physician support also may increase if physicians provide patients with reliable secondary information sources; however, it is possible that secondary sources may contain medication information that is in conflict with physician's recommendations. For this reason, it may be best to assess if and where patients obtain additional medication information and directly address any discrepancies between sources.
4.4 Practice implications
In an ideal world, physicians would thoroughly discuss medications with patients as well as provide them with secondary non-conflicting information sources, such as medication websites and written materials. In-depth physician-patient discussion about medications and alternative information sources would have the double benefit of increasing patients' perceptions of physician support, which increases self-efficacy, as well as potentially reducing the direct negative impact of conflicting information on medication adherence. Given the time constraints and range of topics that must be covered during a typical office visit, it may be impractical to ask physicians to devote extra time to this issue.
It may be more practical for other medical staff, like nurses or receptionists, to direct patients to high quality secondary information sources that have been pre-screened by the physician. An intervention of this type may require additional vasculitis-specific education for office staff. Additionally, identifying high quality sources may be more difficult than it seems because there are often inconsistencies in medication treatment guidelines at the physician level [36]. Expert panels of physicians, pharmacists, nurses, and patient advocates may need to convene to create consensus-based treatment guidelines that directly address some of the discrepancies in medication recommendations (i.e. proper dosage adjustment) that are present in physician resources. This may curb any ‘trickle down’ effect of physician-level conflicting information to the patient.
“I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.”
Figure 3.
Reduced model for the relationships among conflicting information, physician support, outcome expectations, adherence self-efficacy, and medication non-adherence
Acknowledgments
We would like to thank the Vasculitis Foundation, its support group leaders, Vasculitis Foundation Canada, Wegener's Granulomatosis Support Group Of Australia Inc, the Glomerular Disease Collaborative Network, the UNC Kidney Center (especially Ronald J. Falk, Kristen Hendrickson, and Caroline E. Jennette) and Jim Bornac for their help with recruitment. We would also like to thank Chris Wiesen at the ODUM Institute and Todd Schwartz for statistical assistance.
Funding Support: This research was supported by the Renal Epidemiology Predoctoral Traineeship at the UNC Kidney Center and the ACR REF/Abbott Health Professional Graduate Student Research Preceptorship.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Johnson JD. Cancer-related information seeking. Cresskill, NJ: Hampton Press, Inc; 1997. [Google Scholar]
- 2.Rutten LJF, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: A systematic review of research (1980-2003) Patient Educ Couns. 2005;57:250–61. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Trewin VF, Veitch BA. Patient sources of drug information and attitudes to their provision: A corticosteroid model. Pharm World Sci. 2003;25:191–96. doi: 10.1023/a:1025810603241. [DOI] [PubMed] [Google Scholar]
- 4.Narhi U. Sources of medicine information and their reliability evaluated by medicine users. Pharm World Sci. 2007;29:688–94. doi: 10.1007/s11096-007-9131-1. [DOI] [PubMed] [Google Scholar]
- 5.Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK, et al. Trust and sources of health information: The impact of the Internet and its implications for health care providers: Findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165:2618–24. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 6.Sleath B, Wurst K, Lowery T. Drug information sources and antidepressant adherence. Community Ment Hlt J. 2003;39:359–68. doi: 10.1023/a:1024080410284. [DOI] [PubMed] [Google Scholar]
- 7.Mills M, Davidson R. Cancer patients' sources of information: Use and quality issues. Psycho-Oncol. 2002;11:371–78. doi: 10.1002/pon.584. [DOI] [PubMed] [Google Scholar]
- 8.Luker KA, Beaver K, Leinster SJ, Owens RG. Information needs and sources of information for women with breast cancer: A follow-up study. J Adv Nurs. 1996;23:487–95. doi: 10.1111/j.1365-2648.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 9.Huber JT, Cruz M. Information needs and information-seeking of HIV positive men and women. Med Ref Serv Q. 2000;19:39–48. doi: 10.1300/J115v19n03_03. [DOI] [PubMed] [Google Scholar]
- 10.Gray RE, Fitch MI, Phillips C, Labrecque M, Klotz L. Presurgery experiences of prostate cancer patients and their spouses. Cancer Pract. 1999;7:130–35. doi: 10.1046/j.1523-5394.1999.07308.x. [DOI] [PubMed] [Google Scholar]
- 11.Lim AYN, Ellis C, Brooksby A, Gaffney K. Patient satisfaction with rheumatology practitioner clinics: Can we achieve concordance by meeting patients' information needs and encouraging participatory decision making? Ann Acad Med Singap. 2007;36:110–14. [PubMed] [Google Scholar]
- 12.McIntosh A, Shaw CFM. Barriers to patient information provision in primary care: Patients' and general practitioners' experiences and expectations of information for low back pain. Health Expect. 2003;6:19–29. doi: 10.1046/j.1369-6513.2003.00197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pollock K, Grime J, Baker E, Mantala K. Meeting the information needs of psychiatric inpatients: Staff and patient perspectives. J Ment Health. 2004;13:389–401. [Google Scholar]
- 14.Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med. 2005;165:1842–47. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 15.Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K. Common concerns amid diverse systems: Health care experiences in five countries. Health Affair. 2003;22:106–21. doi: 10.1377/hlthaff.22.3.106. [DOI] [PubMed] [Google Scholar]
- 16.Zapka JG, Puleo E, Taplin SH, Goins KV, Yood MU, Mouchawar J, et al. Processes of care in cervical and breast cancer screening and follow-up--the importance of communication. Prev Med. 2004;39:81–90. doi: 10.1016/j.ypmed.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: Relationship to perceptions of cancer preventability, risk, and worry. J Health Commun. 2006;11:51–69. doi: 10.1080/10810730600637541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisher JD, Fisher WA. The Information-Motivation Behavioral Skills Model. In: DiClemente R, Crosby R, Kegler M, editors. Emerging theories in health promotion practice and research. San Francisco, CA: Jossey Bass Publishers; 1992. pp. 40–70. [Google Scholar]
- 19.Amico KR, Toro-Alfonso J, Fisher JD. An empirical test of the Information, Motivation and Behavioral Skills model of antiretroviral therapy adherence. AIDS Care. 2005;17:661–673. doi: 10.1080/09540120500038058. [DOI] [PubMed] [Google Scholar]
- 20.Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, et al. The Information-Motivation-Behavioral Skills model of ART adherence in a deep south HIV+ clinic sample. AIDS Behav. 2009;13:66–75. doi: 10.1007/s10461-007-9311-y. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Starace F, Massa A, Amico KR, Fisher JD. Adherence to antiretroviral therapy: An empirical test of the Information-Motivation-Behavioral Skills Model. Health Psychol. 2006;25:153–62. doi: 10.1037/0278-6133.25.2.153. [DOI] [PubMed] [Google Scholar]
- 22.Kalichman SC, Rompa D, DiFonzo K, Simpson D, Austin J, Luke W, et al. HIV treatment adherence in women living with HIV/AIDS: Research based on the Information-Motivation-Behavioral Skills Model of health behavior. J Assoc Nurse AIDS C. 2001;12:58–67. doi: 10.1016/S1055-3290(06)60217-3. [DOI] [PubMed] [Google Scholar]
- 23.Thorpe C. Dissertation Abstracts International. 2007. Illness Self-management among adults living with ANCA Small Vessel Vasculitis. AAT 3239196. [Google Scholar]
- 24.Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the Self-Efficacy for Appropriate Medication Use Scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15:203–19. doi: 10.1891/106137407783095757. [DOI] [PubMed] [Google Scholar]
- 25.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 26.Preacher KJ, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 27.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 28.Briggs NE. Dissertation Abstracts International. Vol. 37. 2006. Estimation of the standard error and confidence interval of the indirect effect in multiple mediator models; p. 4755B. [Google Scholar]
- 29.Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: Breast self-examination in cancer screening. Psychol Bull. 1996;119:70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- 30.Viscusi WK. Alarmist decisions with divergent risk information. Econ J. 1997;107:1657–70. [Google Scholar]
- 31.Mayer DK, Terrin NC, Kreps GL, Menon U, McCance K, Parsons SK, et al. Cancer survivors' information seeking behaviors: A comparison of survivors who do and do not seek information about cancer. Patient Educ Couns. 2007;65:342–350. doi: 10.1016/j.pec.2006.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carpenter DM, DeVellis RF, Hogan SL, DeVellis BM, Fisher EB. Use and perceived credibility of medication information sources for vasculitis patients: Differences by gender. doi: 10.1080/10810730.2011.551995. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walton EW. Giant cell granuloma of the respiratory tract (Wegener's granulomatosis) Brit Med J. 1958;2:265–70. doi: 10.1136/bmj.2.5091.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haynes RB. A critical review of “determinants” of patient compliance with therapeutic regimens. In: Sackett DL, Haynes RB, editors. Compliance with therapeutic regimens. Baltimore, MD: Johns Hopkins University Press; 1976. pp. 26–39. [Google Scholar]
- 35.Treharne GJ, Lyons AC, Hale ED, Douglas KMJ, Kitas GD. ‘Compliance’ is futile but is 'concordance' between rheumatology patients and health professionals attainable? Rheumatology. 2006;45:1–5. doi: 10.1093/rheumatology/kei223. [DOI] [PubMed] [Google Scholar]
- 36.Vidal L, Shavit M, Fraser A, Paul M, Lleibovici L. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. Brit Med J. 2005;331:263–65. doi: 10.1136/bmj.38476.471088.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]