Abstract
Abnormal patellofemoral joint motion is a possible cause of patellofemoral pain, and patellar braces are thought to alleviate pain by restoring normal joint kinematics. We evaluated whether females with patellofemoral pain exhibit abnormal patellofemoral joint kinematics during dynamic, weight-bearing knee extension and assessed the effects of knee braces on patellofemoral motion. Real-time magnetic resonance (MR) images of the patellofemoral joints of 36 female volunteers (13 pain-free controls, 23 patellofemoral pain) were acquired during weight-bearing knee extension. Pain subjects were also imaged while wearing a patellar-stabilizing brace and a patellar sleeve. We measured axial-plane kinematics from the images. Females with patellofemoral pain exhibited increased lateral translation of the patella for knee flexion angles between 0° and 50° (p = 0.03), and increased lateral tilt for knee flexion angles between 0° and 20° (p = 0.04). The brace and sleeve reduced the lateral translation of the patella; however, the brace reduced lateral displacement more than the sleeve (p = 0.006). The brace reduced patellar tilt near full extension (p = 0.001), while the sleeve had no effect on patellar tilt. Our results indicate that some subjects with patellofemoral pain exhibit abnormal weight-bearing joint kinematics and that braces may be effective in reducing patellar maltracking in these subjects.
Keywords: patellofemoral pain, kinematics, real-time MRI, bracing
Patellofemoral (PF) pain is a common, debilitating disorder, accounting for 25% of all knee injuries seen in some sports medicine clinics.1 The incidence of PF pain is higher in females than in males.2 Unfortunately, effective treatment is challenging because the causes of pain are unclear, and the mechanism of pain is likely multifactoral.3 PF pain typically arises during activities that place high loads across the knee, such as squatting, ascending/descending stairs, and running. Abnormal PF joint kinematics are thought to cause pain by increasing joint contact stress.3 To treat this disorder, a better understanding of the pain mechanisms is needed.
About half of patients with PF pain are diagnosed with maltracking or subluxation4 (the patella does not remain centered within the femoral trochlea during knee flexion and extension). This diagnosis is typically performed during a clinical exam or using static radiographs with the knee flexed. These tests do not mimic the functional tasks that often elicit pain, but nevertheless dictate the treatments prescribed by the clinician. To confirm whether patients with PF pain have altered kinematics that need correction, quantitative measurements of PF joint motion are required. Current techniques for studying joint kinematics include studies on cadavers,5 motion capture techniques,6 static and quasistatic magnetic resonance imaging (MRI) methods,7–10 fluoroscopy,11 or cine phase contrast MRI.12 Cine MR imaging of subjects in a supine, unloaded position showed that subjects with PF pain exhibit more lateral patellar translation and tilt than control subjects during knee flexion,13 while static MRI with an applied load of 152 N revealed only an increase in lateral translation of the patella at 19° of knee flexion between pain-free individuals and those with PF pain and maltracking.10 Since in vivo kinematics measurements during dynamic, highly loaded motions have not been obtained, it remains unclear whether subjects with PF pain experience abnormal kinematics during the tasks that often cause pain.
Patellofemoral braces are often prescribed as part of a rehabilitation program.14 Some braces reduce pain and improve joint stability,15 while others have not been shown to improve function or pain.16 Braces are thought to restore normal joint kinematics; however, the mechanism by which braces might alleviate pain remains unclear. Furthermore, several types of braces exist, but whether a simple sleeve is as effective as more complex, realignment braces in restoring normal motion is unknown. Some patellar realignment braces alter static alignment of the joint by shifting the patella medially by 2.4%–3.6% of patellar width.17 The joint likely responds differently to bracing during dynamic, weight-bearing situations when the quadriceps are active; therefore, the effects of patellar bracing should be assessed under these conditions.
Real-time MRI overcomes the limitations of previous techniques to measure human movement and has been used to study cardiac, joint, and muscle motion.18–21 The technique requires only one motion cycle to acquire a time series of single-slice images, allowing subjects to be imaged during dynamic, weight-bearing tasks. This study used real-time MRI to measure PF joint motion during weight-bearing knee extension. We addressed three questions: 1) Do females with PF pain exhibit abnormal joint kinematics compared to pain-free controls? 2) Does a patellar-stabilizing brace alter knee kinematics in females with PF pain? 3) Does a patellar sleeve alter joint kinematics in females with PF pain?
MATERIALS AND METHODS
Due to the higher incidence of PF pain among females, we investigated only women. Females with PF pain were recruited from Stanford’s Orthopaedic Clinics and Sports Medicine Center and were diagnosed by a sports medicine physician. Subjects were included if they experienced reproducible anterior knee pain during at least two of the following activities: stair ascent/decent, kneeling, squatting, prolonged sitting, or isometric quadriceps contraction. Subjects were excluded if they had experienced knee ligament instability, patellar tendonitis, joint line tenderness or knee effusion, previous knee trauma or surgery, patellar dislocation, or signs of osteoarthritis. We examined the PF joints of 13 active, pain-free female control subjects (26.8 ± 3 years, 1.66 ± 0.08 m, 59.8 ± 9.3 kg) and 23 females diagnosed with unilateral or bilateral PF pain (32 ± 7 years, 1.66 ± 0.07 m, 58.4 ± 6.2 kg). For subjects with bilateral pain, the most painful knee at the time of examination was studied. All subjects were between the ages of 18 and 45. On average, control subjects participated in 6 h of moderate to intense physical activities per week. Fourteen subjects with PF pain were clinically diagnosed with maltracking using a PF arthrometer22; however, all subjects were grouped together. To describe the level of function of the subjects with PF pain, we used the anterior knee pain scale.23 The average score was 70 ± 14 (100 indicates no anterior knee pain or disability). Subjects were informed about the nature of the study and provided prior consent according to the policies of the Institutional Review Board.
Single-slice, spiral real-time MR images24 were obtained of all subjects performing knee flexion/extension in a 0.5T GE Signa SP open-MRI scanner (Fig. 1A). Images were acquired using the RTHawk real-time system,24 which is implemented by interconnecting a desktop computer with the scanner’s data acquisition and sequence control systems, allowing the operator to control scan parameters and scan plane geometry interactively (HeartVista, Inc., Los Altos CA). A 5″ surface coil was taped to the knee, and the following scan parameters were used: field-of-view: 16 cm × 16 cm; number of interleaves: 6; pixel size: 1.88 mm; readout time: 16 ms; slice thickness: 5 mm (full width at half maximum). Each image was acquired in 171 ms (6 images/s). Continuous image reconstruction was performed using a sliding window algorithm25 resulting in a reconstructed frame rate of 35 frames/s. A backrest26 stabilized subjects in the scanner (Fig. 1B). The backrest was inclined 25° from vertical, so subjects supported about 90% of their body weight. Real-time MR images were acquired as subjects performed continuous knee flexion/extension from 0° to 60° at a rate of 6° –10°/s (Fig. 2). Based on a study measuring a phantom rotating within the plane of the images, the in-plane measurement accuracy is 1.9 mm for this movement speed.21 Oblique-axial images through the widest portion of the patella were acquired. The image plane was defined from a sagittal view as subjects remained still at about 30° of knee flexion. During subject movement, the image plane was continuously translated vertically to remain at the widest portion of the patella while keeping the posterior femoral condyles in the image.
Figure 1.
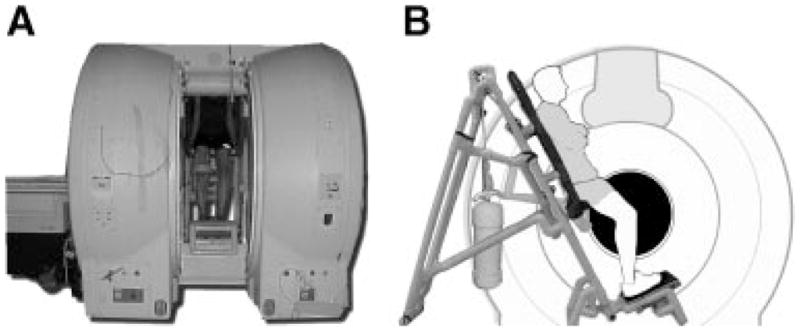
(A) Open-bore MRI scanner with subject performing a weight-bearing squat. (B) Side view of scanner and backrest used to stabilize subjects as they moved in the scanner. Subjects supported about 90% of their body-weight.
Figure 2.
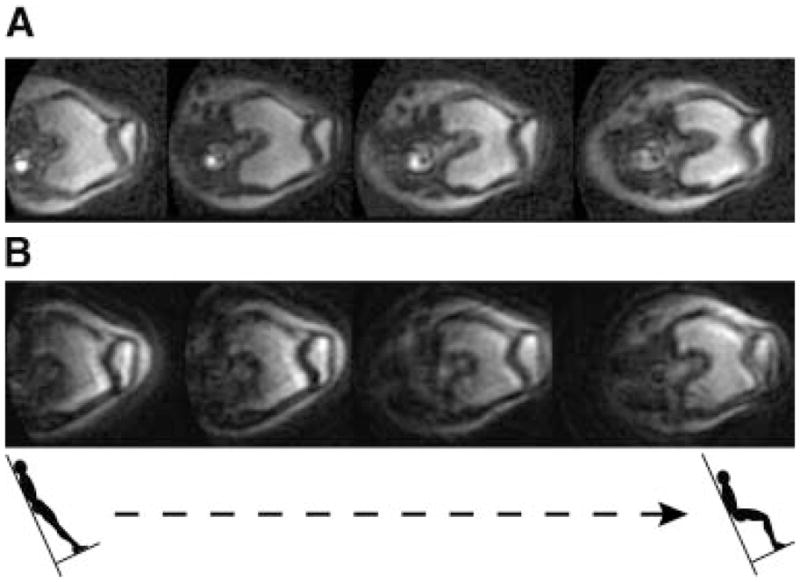
(A) Real-time MR images of the patellofemoral (PF) joint of a pain-free control subject during upright, weight-bearing knee extension. (B) Real-time MR images of the PF joint of a subject with pain during upright, weight-bearing knee extension. Notice the lateral position and rotation of the patella relative to the femur as the pain subject nears full extension. These are oblique-axial views through the knee corresponding to four knee flexion angles between 0 and 60°.
A Dynamic Patella Traction Brace (QLok,™ Cropper Medical, Inc., Ashland, OR) and an open patella knee support sleeve (McDavid, Woodridge, IL) were evaluated. The brace is designed to prevent lateral patellar tracking and has a buttress that is placed along the lateral aspect of the patella and tightened medially to stabilize the patella (Fig. 3A). The sleeve has an opening to reduce patellar compression (Fig. 3B) and was evaluated to determine if it provides as much support to the patella as the brace. One investigator applied the braces to all subjects with PF pain. Images were obtained of PF pain subjects performing knee bends while wearing the brace, the sleeve, and with no brace; the order of the three trials was randomized.
Figure 3.

(A) QLok Dynamic Patella Traction Brace. The vertical bar is placed along the lateral edge of the patella and is tightened medially to stabilize the patella. (B) Patellar sleeve.
Post-processing of the images was performed to measure PF joint kinematics. Using a semi-automatic tracking algorithm, implemented in MATLAB (The MathWorks, Inc., Natick, MA), 2D kinematics in an oblique-axial plane were measured by identifying bony landmarks. The landmarks were the deepest point of the trochlea, the most lateral and most medial points on the patella, and the most posterior points on the femoral condyles. Each landmark was manually identified on the first image of the series, and a template window was created surrounding each point. A search window, four times as large as the template window, defined the search space in the next image. The two windows were compared using normalized cross correlation:
where γ is the correlation coefficient, f is a window surrounding the pixel in the current image frame (search space), t is the template window (identified in the first frame), u and v represent the position of the template window (t), x and y are pixel positions in the search space (f) under the template window, t̄ is the mean of the template, and f̄ u,v is the mean of f(x,y) in the region under the template. The indices (u,v) that maximize the correlation coefficient represent the location within the search space that results in the best image similarity between the template and a template-sized region within the search space. The bony landmark is identified in the current image frame based on this location. The algorithm continues by defining a search space window in the subsequent image and comparing it to the template window. This process is repeated for all frames in the image sequence.
Clinical measurements of axial-plane patellar translation and rotation relative to the femur were computed from the bony landmarks (Fig. 4). Medial/lateral translation of the patella relative to the femur is often described using the bisect offset index, reported as the percentage of the patella lateral to the midline of the femur.13,27 Larger bisect offset values indicate that the patella is more lateral relative to the femur. Axial-plane patellar rotation is typically measured with the patellar tilt angle, the angle between the patella and the posterior femoral condyles.28 To account for measurement differences due to variations in scan plane orientation, we measured bisect offset and patellar tilt during two different knee extension trials for each subject. The kinematics were smoothed with a low-pass filter with a cut-off frequency of 1 Hz and averaged. We performed an intraobserver repeatability study using images taken during knee extension in two subjects. For each set of images, one investigator measured the kinematics over the entire range of motion three times. Each repeated measurement was separated by at least one day. The variance of the three measurements of each extension trial was computed for every knee flexion angle. The average variance over all flexion angles was found, and the combined average variance from the two subjects was computed and reported. We also compared kinematics measured using the semi-automatic tracking algorithm to those measured by manually identifying all bony landmarks for three different extension trials by computing the average root-mean-square (RMS) difference between the semi-automatic measurements and the manual measurements.
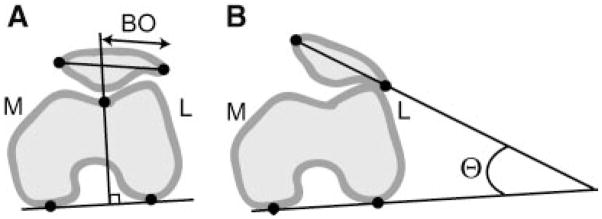
Figure 4.
Axial-plane patellofemoral (PF) joint kinematics. (A) Diagram of the bisect offset index (BO), a measure of the percentage of the patellar width lateral (L) to the midline of the femur. (B) Diagram of the patellar tilt angle (Θ), the angle formed by lines joining the posterior femoral condyles and the maximum width of the patella. Bony landmarks used to compute each measurement are indicated by the black circles. M, medial.
The real-time sequence provides a time series of single-slice images, making it impossible to measure knee flexion angle and axial-plane kinematics simultaneously. A goniometer was used during MRI scanning to indicate 60° of flexion, thereby ensuring that subjects were imaged over the same range of motion. We used optical motion capture techniques (Motion Analysis Corp., Santa Rosa, CA) to estimate knee flexion angles as a function of time during the movement. Two subjects performed the backrest-assisted knee bends in a motion analysis laboratory moving at the same rate as prescribed during the MRI study and with a goniometer positioned to indicate 60° of flexion. Knee Flexion angles were measured from markers at the hip, knee, and ankle. The flexion angle trajectories were averaged, resulting in a “typical” curve of knee flexion angles during the squatting motion. The total time to complete the squatting movement varied slightly between subjects and between trials, so the measured kinematics from the real-time images were correlated to the “typical” knee flexion angles according to their occurrence as a percentage of the total range of motion (e.g., the kinematics occurring at 50% of the squatting movement in the MRI scanner were defined to correspond to the knee flexion angle occurring at 50% of the squatting movement measured in the knee motion analysis laboratory).
Significant differences between groups were assessed by fitting a linear mixed-effects regression model to the data. We compared the kinematics of the pain-free controls to those of the subjects with PF pain. We performed a separate test comparing the brace kinematics, the sleeve kinematics, and the no brace or sleeve kinematics in the subjects with PF pain, accounting for the repeated measures on each subject. To identify the specific ranges of knee flexion angles over which kinematic differences occurred, we separated the data into ranges spanning 10° of flexion and fit separate regression models to the curves in each angle range.
In a post-hoc analysis, we separated subjects with PF pain into groups based on comparison of each subject’s kinematics with those of the controls. We defined abnormal bisect offset and tilt as being 2 SD > the average of the pain-free controls at full extension. Therefore, any subject with bisect offset ≥ this threshold was defined to have abnormal bisect offset. Similarly, any subject with patellar tilt ≥ the tilt threshold was defined to have abnormal patellar tilt. The remaining subjects were defined to have either normal bisect offset or normal tilt.
RESULTS
The average variance between measurements was 3% and 2° for bisect offset and patellar tilt, respectively. The average RMS differences between the manual and semi-automatic kinematics were 4% for bisect offset and 3° for patellar tilt.
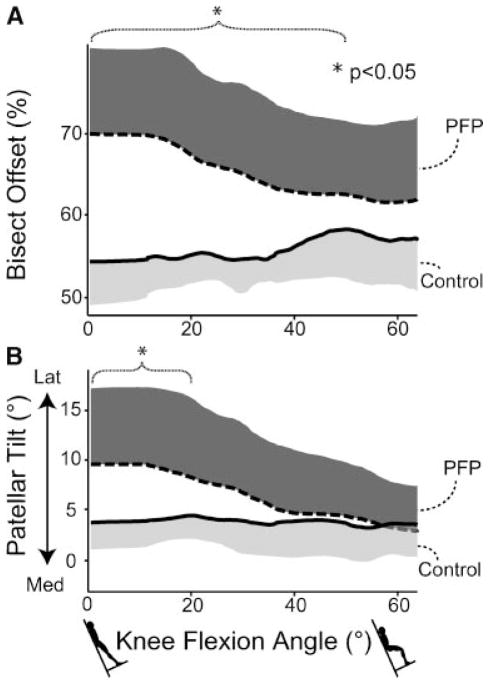
PF pain subjects exhibited greater bisect offset than control subjects for knee flexion angles between 0° and 50° (Fig. 5A). In this range of flexion angles, bisect offset was, on average, 10% larger in the pain subjects than in the controls (p = 0.03). The greatest difference between groups was 16% and occurred at full extension (bisect offset was 54% for controls vs. 70% for PF pain subjects; p = 0.001).
Figure 5.
Patellofemoral (PF) joint kinematics measured from real-time MRI in a group of 13 pain-free female control subjects and 23 females with patellofemoral pain (PFP). The solid and dashed lines represent the means of each subject group and the shaded regions ± 1 SD. (A) Relationship between bisect offset and knee flexion angle. The subjects with pain exhibited larger bisect offset for knee flexion angles ≤50°. (B) Relationship between patellar tilt angle and knee flexion angle. Pain subjects exhibited larger tilt for knee flexion angles <20°.
PF pain subjects exhibited greater lateral patellar tilt compared to control subjects for knee flexion angles between 0° and 20° (Fig. 5B). In this range of angles, patellar tilt was, on average, more than twice as large in individuals with pain compared to controls (p = 0.04). The greatest difference between groups occurred at full extension (tilt was 4° for controls vs. 10° for PF pain subjects; p = 0.01).
The patellar-stabilizing brace reduced the bisect offset of pain subjects from 0° to 60° of knee flexion (Fig. 6A). The brace decreased bisect offset by an average of 4% (p = 0.001). The largest reduction occurred at full extension (bisect offset was 70% with no brace vs. 64% with brace application). While the brace significantly reduced bisect offset, it did not restore normal joint motion. From 0° to 40° of knee flexion, the bisect offset of subjects with pain while wearing the brace was, on average, 6% larger than that of the pain-free control subjects (p = 0.01).
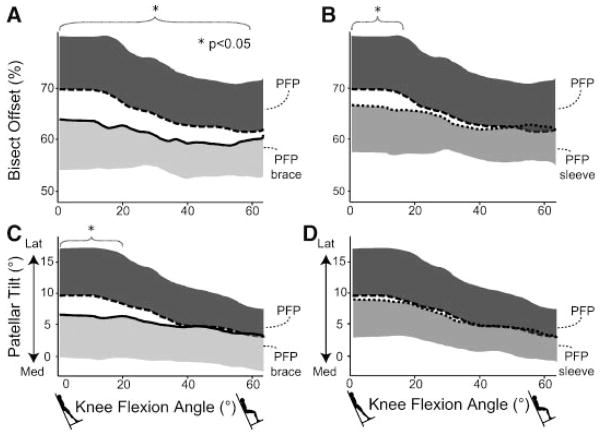
Figure 6.
Effects of a patellar-stabilizing brace and a sleeve on patellofemoral (PF) joint kinematics in 23 females with patellofemoral pain (PFP). The solid, dashed, and dotted lines represent the means of the PFP group, the PFP group with brace application, and the PFP group with sleeve application. The shaded regions are ± 1 SD. (A) Effect of brace on the bisect offset index. The brace reduced bisect offset for knee flexion angles <60°. (B) Effect of sleeve on bisect offset. The sleeve reduced bisect offset for knee flexion angles <20°. (C) Effect of brace on lateral tilt. The brace reduced tilt for knee flexion angles <20°. (D) Effect of sleeve on tilt. The sleeve did not change the tilt.
The patellar sleeve significantly reduced the bisect offset of PF pain subjects for knee flexion angles between 0° and 20° (Fig. 6B). On average, the sleeve reduced the bisect offset by 4% in this range of knee flexion angles (p = 0.005). The reduction in bisect offset provided with the brace was larger (6% at full extension) than that provided by the sleeve (4% at full extension) for all knee flexion angles (p = 0.006).
The patellar tilt of the PF pain subjects decreased with brace application for knee flexion angles between 0° and 20° (Fig. 6C). On average, the brace reduced tilt by 3° over this flexion range (p = 0.001). The largest reduction in tilt produced by the brace occurred at full extension (tilt was 10° without the brace vs. 6° with the brace). We did not detect changes in tilt with application of the sleeve (Fig. 6D).
Both bisect offset and patellar tilt varied substantially among subjects with PF pain, and several subjects with PF pain did not exhibit abnormal joint kinematics (Fig. 7). Based on the means and standard deviations of the control subjects in the study, resulting thresholds that defined abnormal kinematics were 65% for bisect offset and 9° for tilt. In this study, 16 subjects had abnormal bisect offset, 11 subjects had abnormal patellar tilt, 7 subjects had normal bisect offset, and 12 subjects had normal tilt (Fig. 7). During clinical exam, 14 of the 23 subjects were diagnosed with patellar maltracking using the arthrometer.22 However, the image-based classification did not correspond to the clinical classification in eight subjects (three clinically diagnosed maltrackers had bisect offset no different than controls, and five clinically diagnosed non-maltrackers had increased bisect offset compared to controls). Additionally, the change in kinematics with bracing depended on whether a subject had abnormal kinematics prior to applying the brace or sleeve (Fig. 8). The brace reduced bisect offset more in individuals with abnormal bisect offset than in individuals whose bisect offset was not different from controls (p = 0.03). Similar trends were seen with the application of the patellar sleeve, although these differences were not significant. Additionally, the brace reduced patellar tilt only in subjects who initially had patellar tilt greater than the controls.
Figure 7.
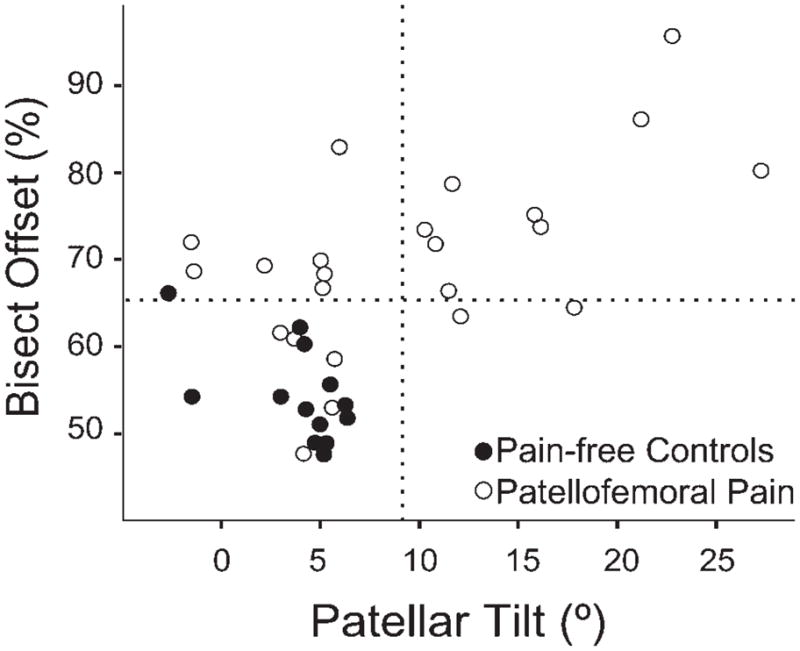
Relationship between bisect offset and patellar tilt at full extension. Pain-free controls are solid circles and patellofemoral (PF) pain subjects are hollow circles. The dashed lines represent 2 SD > the mean bisect offset and tilt of the pain-free subjects and were used to define abnormal kinematics. Five subjects with pain had bisect offset and tilt <2 SD above the mean of the controls, while nine with pain had increased bisect offset and tilt compared to controls.
Figure 8.
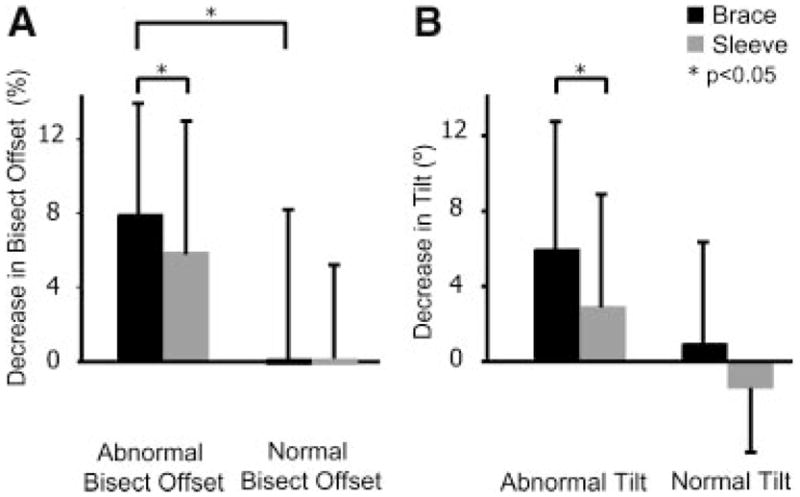
Decrease in bisect offset (A) and patellar tilt (B) with application of the brace and the sleeve. The subjects with patellofemoral (PF) pain are divided into those with abnormal kinematics (>2 SD above the mean of the pain-free subjects at full extension) and those with kinematics no different from the controls. The decrease in kinematics with brace application is plotted in black, and the decrease in kinematics with sleeve application in gray. With the brace, bisect offset was reduced more in subjects with abnormal kinematics compared to those with normal kinematics. The brace reduced the bisect offset and tilt more than the sleeve in the subjects with abnormal kinematics.
DISCUSSION
Our measurements of PF joint kinematics revealed that, on average, females with PF pain exhibited increased lateral translation and lateral tilt of the patella relative to the femur during upright, weight-bearing knee extension. The abnormal kinematics occurred primarily near full extension and were absent in deeper flexion angles when the patella was likely stabilized within the trochlear groove. With application of the brace, the lateral translation and tilt of the patella were reduced, but were not restored to normal. The sleeve reduced the lateral translation of the patella, but did not alter patellar tilt. While both the sleeve and the brace significantly reduced bisect offset, the brace reduced bisect offset over a larger range of knee flexion angles and by a larger amount compared to the sleeve, indicating that it may be more effective in correcting abnormal joint motion.
Our results suggest that different subsets of females with PF pain exist, and that bracing seems to have a mechanical effect in only one group, those with abnormal kinematics compared to the controls. This implies that treatments should be prescribed on a case-by-case basis to address a specific kinematic abnormality that may be related to the cause of a patient’s pain. Clinical assessment of maltracking is difficult because of the challenge in identifying the positions of the patella and the femur. Maltracking is often assessed clinically through palpation of the patella through a range of motion or by observing the motion of the skin over the patella. This assessment is typically performed in a seated, unloaded posture that may not reflect joint kinematics during functional, load-bearing tasks. The fact that eight subjects had kinematic assessments that did not correlate to the clinical diagnosis highlights the difficulty in clinically assessing patellar tracking and establishes the need for more accurate methods of examining patellar motions. Our results suggest that accurate assessment of kinematics near full extension can be used to identify whether a patellar-stabilizing brace will be effective in altering joint motion.
Our results agree with previous findings of increased lateral shift13,29 and tilt13,29–31 of the patella in subjects with PF pain compared to pain-free controls. Furthermore, our results agree with previous studies demonstrating a decrease in the lateral position of the patella with application of a stabilizing knee brace.17,32 Our results differ from some studies17,32–34 in that we observed a significant reduction in patellar tilt near full extension with application of the brace. Discrepancies between our study and previous measurements may be due to the different braces tested and the different loading and movement conditions during which images were acquired. The amount of joint loading experienced by our subjects is much greater than that applied in previous studies, and the resulting increases in muscle activation likely affected the kinematics. For example, significantly more internal femoral rotation occurs during weight-bearing extension than during unloaded motions,35 which can affect PF kinematics. The conditions during which we measured kinematics more closely reflect the situations that cause pain, resulting in an improved understanding of kinematic abnormalities that may be related to pain in these subjects.
Pain is likely caused by many factors, but abnormal PF joint kinematics during weight-bearing movement may be one mechanism. Abnormal joint motion could increase result in cartilage stress, thus stimulating pain receptors in the subchondral bone. We found the largest differences in kinematics near full extension. However, some patients experience pain in deeper knee flexion angles. Abnormal joint motion near full extension may also be an indication that increased stress occurs in deeper angles of knee flexion as a consequence of the patella being constrained within the trochlea. Future studies are necessary to test this hypothesis and to evaluate whether the small changes in kinematics observed with the brace and sleeve are sufficient to significantly alter joint contact stresses. Furthermore, the cause of abnormal kinematics may vary between subjects. Altered PF joint motion may arise from excessive femoral internal rotation, abnormal bone alignment, abnormal muscle forces, or other causes. More effective treatments can be developed once the underlying cause of the abnormal joint motion in a given subject is known.
While this study provided some of the first measurements of PF joint kinematics during upright weight-bearing motions, it was limited to a 2D analysis during relatively slow movement. A future 3D analysis would account for out-of-plane motion. The 2D nature of the images also prevented us from measuring knee flexion angles directly, requiring us to correlate the kinematics to a generic knee flexion angle curve that was not specific to each subject. The measurement accuracy of the real-time MR images is about 1.9 mm, which prevents this technique from being used to detect very small motions. This limitation likely did not affect our results as we detected kinematic differences larger than the measurement accuracy (2–8 mm). A final limitation was that the study was limited to females; the results may be inapplicable to males. A future study investigating differences in PF joint motion between genders and evaluating the effects of bracing on joint kinematics in males should be performed.
Real-time MRI addresses several limitations affecting current methods of measuring joint kinematics. As a result, this study has provided an assessment of PF motion during weight-bearing movement and may help clinicians diagnose and treat patellar maltracking.
Acknowledgments
Financial support provided by NIH (EB0002524-01, EB005790-01, U54 GM072970, RO1HD33929, RO1HD046814, R90 DK071508), NSF, and a Robert and Ruth Halperin SGF. This material is based upon work supported in part by the Office of Research and Development (Rehabilitation R&D Service grant #A2592R), Department of Veterans Affairs. We thank May Liu, Chand John, Mark Cheng, and Rich Souza for help with data collection; and Jarrett Rosenberg and Alexander Sox-Harris for statistics help. Braces provided by Cropper Medical, Inc.
References
- 1.Devereaux MD, Lachmann SM. Patellofemoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- 3.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31:977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Dehaven KE, Dolan WA, Mayer PJ. Chondromalacia patellae in athletes. Clinical presentation and conservative management. Am J Sports Med. 1979;7:5–11. doi: 10.1177/036354657900700102. [DOI] [PubMed] [Google Scholar]
- 5.Amis AA, Senavongse W, Bull AM. Patellofemoral kinematics during knee flexion-extension: an in vitro study. J Orthop Res. 2006;24:2201–2211. doi: 10.1002/jor.20268. [DOI] [PubMed] [Google Scholar]
- 6.Lin F, Wang G, Koh JL, et al. In vivo and noninvasive three-dimensional patellar tracking induced by individual heads of quadriceps. Med Sci Sports Exerc. 2004;36:93–101. doi: 10.1249/01.MSS.0000106260.45656.CC. [DOI] [PubMed] [Google Scholar]
- 7.Fellows RA, Hill NA, Gill HS, et al. Magnetic resonance imaging for in vivo assessment of three-dimensional patellar tracking. J Biomech. 2005;38:1643–1652. doi: 10.1016/j.jbiomech.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Patel VV, Hall K, Ries M, et al. Magnetic resonance imaging of patellofemoral kinematics with weight-bearing. J Bone Joint Surg [Am] 2003;85-A:2419–2424. doi: 10.2106/00004623-200312000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Witonski D, Goraj B. Patellar motion analyzed by kinematic and dynamic axial magnetic resonance imaging in patients with anterior knee pain syndrome. Arch Orthop Trauma Surg. 1999;119:46–49. doi: 10.1007/s004020050353. [DOI] [PubMed] [Google Scholar]
- 10.MacIntyre NJ, Hill NA, Fellows RA, et al. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg [Am] 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 11.Nha KW, Papannagari R, Gill TJ, et al. In vivo patellar tracking: clinical motions and patellofemoral indices. J Orthop Res. 2008;26:1067–1074. doi: 10.1002/jor.20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheehan FT, Zajac FE, Drace JE. In vivo tracking of the human patella using cine phase contrast magnetic resonance imaging. J Biomech Eng. 1999;121:650–656. doi: 10.1115/1.2800868. [DOI] [PubMed] [Google Scholar]
- 13.Brossmann J, Muhle C, Schroder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 14.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 15.Greenwald AE, Bagley AM, France EP, et al. A biomechanical and clinical evaluation of a patellofemoral knee brace. Clin Orthop Relat Res. 1996;324:187–195. doi: 10.1097/00003086-199603000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Lun VM, Wiley JP, Meeuwisse WH, et al. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15:235–240. doi: 10.1097/01.jsm.0000171258.16941.13. [DOI] [PubMed] [Google Scholar]
- 17.Powers CM, Ward SR, Chan LD, et al. The effect of bracing on patella alignment and patellofemoral joint contact area. Med Sci Sports Exerc. 2004;36:1226–1232. doi: 10.1249/01.mss.0000132376.50984.27. [DOI] [PubMed] [Google Scholar]
- 18.Asakawa DS, Nayak KS, Blemker SS, et al. Real-time imaging of skeletal muscle velocity. J Magn Reson Imaging. 2003;18:734–739. doi: 10.1002/jmri.10422. [DOI] [PubMed] [Google Scholar]
- 19.Quick HH, Ladd ME, Hoevel M, et al. Real-time MRI of joint movement with trueFISP. J Magn Reson Imaging. 2002;15:710–715. doi: 10.1002/jmri.10120. [DOI] [PubMed] [Google Scholar]
- 20.Nayak KS, Cunningham CH, Santos JM, et al. Real-time cardiac MRI at 3 tesla. Magn Reson Med. 2004;51:655–660. doi: 10.1002/mrm.20053. [DOI] [PubMed] [Google Scholar]
- 21.Draper CE, Santos JM, Kourtis LC, et al. Feasibility of using real-time MRI to measure joint kinematics in 1.5T and open-bore 0.5T systems. J Magn Reson Imaging. 2008;28:158–166. doi: 10.1002/jmri.21413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ota S, Ward SR, Chen YJ, et al. Concurrent criterion-related validity and reliability of a clinical device used to assess lateral patellar displacement. J Orthop Sports Phys Ther. 2006;36:645–652. doi: 10.2519/jospt.2006.2263. [DOI] [PubMed] [Google Scholar]
- 23.Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 24.Santos JM, Wright GA, Pauly JM. Flexible real-time magnetic resonance imaging framework. Conf Proc IEEE Eng Med Biol Soc. 2004;2:1048–1051. doi: 10.1109/IEMBS.2004.1403343. [DOI] [PubMed] [Google Scholar]
- 25.Riederer SJ, Tasciyan T, Farzaneh F, et al. MR fluoroscopy: technical feasibility. Magn Reson Med. 1988;8:1–15. doi: 10.1002/mrm.1910080102. [DOI] [PubMed] [Google Scholar]
- 26.Besier TF, Draper CE, Gold GE, et al. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J Orthop Res. 2005;23:345–350. doi: 10.1016/j.orthres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 27.Stanford W, Phelan J, Kathol MH, et al. Patellofemoral joint motion: evaluation by ultrafast computed tomography. Skeletal Radiol. 1988;17:487–492. doi: 10.1007/BF00364042. [DOI] [PubMed] [Google Scholar]
- 28.Fulkerson JP, Schutzer SF, Ramsby GR, et al. Computerized tomography of the patellofemoral joint before and after lateral release or realignment. Arthroscopy. 1987;3:19–24. doi: 10.1016/s0749-8063(87)80005-1. [DOI] [PubMed] [Google Scholar]
- 29.Yamada Y, Toritsuka Y, Horibe S, et al. In vivo movement analysis of the patella using a three-dimensional computer model. J Bone Joint Surg [Br] 2007;89:752–760. doi: 10.1302/0301-620X.89B6.18515. [DOI] [PubMed] [Google Scholar]
- 30.Wittstein JR, Bartlett EC, Easterbrook J, et al. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy. 2006;22:643–649. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther. 2000;80:965–978. [PubMed] [Google Scholar]
- 32.Worrell T, Ingersoll CD, Bockrath-Pugliese K, et al. Effect of patellar taping and bracing on patellar position as determined by MRI in patients with patellofemoral pain. J Athl Train. 1998;33:16–20. [PMC free article] [PubMed] [Google Scholar]
- 33.Muhle C, Brinkmann G, Skaf A, et al. Effect of a patellar realignment brace on patients with patellar subluxation and dislocation. Evaluation with kinematic magnetic resonance imaging. Am J Sports Med. 1999;27:350–353. doi: 10.1177/03635465990270031401. [DOI] [PubMed] [Google Scholar]
- 34.Powers CM, Shellock FG, Beering TV, et al. Effect of bracing on patellar kinematics in patients with patellofemoral joint pain. Med Sci Sports Exerc. 1999;31:1714–1720. doi: 10.1097/00005768-199912000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Powers CM, Ward SR, Fredericson M, et al. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33:677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]