Abstract
OBJECTIVE
We sought to compare perceptions of functional health status between children who had undergone a Fontan procedure and their parents.
METHODS
Fontan procedure survivors 10 to 18 years of age were included in the study if the child completed the Child Health Questionnaire (CHQ) and the parent completed the parent form to assess the child’s functional health status. Comparisons were made between raw domain scores for the parent- and child-completed CHQs.
RESULTS
Between March 2003 and April 2004, 1078 Fontan survivors were screened. Of the 546 eligible and consented patients, 354 were 10 –18 years of age and 328 parent/child pairs completed the CHQs. Parents reported significantly lower scores (worse functioning) for their children than the children reported for themselves in the domains of physical functioning (P < .01), impact on school or activities from emotional and behavioral problems (P < .01), impact on school or activities from physical health issues (P<.01), general behavior (P < .01), mental health (P < .01), self-esteem (P < .01), and general health perceptions (P<.01). No significant differences were noted for the domains of bodily pain, family cohesiveness, or family activities. For the physical functioning domain, factors contributing to lower scores for parent versus child reports included pulmonary artery anomalies and fenestration at the time of the Fontan operation. Lower parent-reported scores also were associated with more noncardiac health problems in the child.
CONCLUSIONS
Parents’ perceptions of the functional health status of their children after the Fontan procedure were worse than the children’s perceptions.
Keywords: Fontan procedure, congenital heart disease, single ventricle, functional health status, quality of life
Each year, ~4000 infants are born in the United States with congenital heart defects (CHDs) that result in single-ventricle physiologic features necessitating staged surgical palliation, culminating in the Fontan procedure.1 The population of Fontan procedure survivors continues to increase with advances in surgical and medical care for infants with a single ventricle. Despite this, Fontan procedure survivors remain at increased risk for death and morbidities, as well as for physiologic limitations imposed by the Fontan procedure circulation.2–4 Furthermore, survivors face social and psychological challenges in adulthood, such as employability, insurability, and decreasing social integration.5–7 Measurements of physical, psychological, and social well-being and studies of functional health status and health-related quality of life are important adjuncts to traditional analyses of mortality and morbidity rates.6
Generic questionnaires assessing the functional health status of children have been validated for both parents and children. In many studies, only the parent or the child, rather than both, completed the questionnaires. Parents’ perceptions of their children’s functional health status may differ from those of the children themselves. For example, children with cystic fibrosis tend to rate their own functional health status higher than do their parents,8 especially with regard to physical functioning. With long-term survival rates for patients with single-ventricle physiologic features improving, we sought to compare perceptions of functional health status between children who had undergone a Fontan procedure and their parents.
METHODS
Study Subjects
Seven clinical centers constituting the Pediatric Heart Network performed a multicenter, prospective, cross-sectional survey of children 6 to 18 years of age who had undergone a palliative Fontan procedure.4 With approval from the institutional review boards at the individual center sites, potential study subjects were identified from cardiology and cardiac surgery databases, screened at individual sites through medical record review, and deemed eligible4,9 if they were 6 to 18 years of age at the time of enrollment and had undergone a Fontan procedure ≥6 months before initial study testing. Prospective data collection for each patient occurred within a 3-month time window (ideally, same-day data collection) and included health status questionnaires completed by the parent and the child (≥10 years of age), cardiac MRI, echocardiography, serologic testing, and maximal exercise testing. Patients who were unable to contribute health status data, echocardiographic results, and serologic results within the 3-month time window were excluded from the study. Exclusion criteria included the presence of a noncardiac medical or psychiatric disorder, planned participation in another research protocol that would prevent successful completion of the minimal study testing (listed above) or would invalidate the results of study testing, lack of primary caregiver reading fluency in English or Spanish, and patient pregnancy or planned pregnancy before the completion of study testing. Informed consent was obtained from parents and children before study procedures were performed.
Functional Health Status Questionnaires
The Child Health Questionnaire (CHQ) is a generic measure of a child’s functional health status with respect to physical, mental, and social wellbeing. 10 The parent-completed questionnaire is the CHQ-PF50, and the corresponding self-report questionnaire for children 10 to 18 years of age is the CHQ-CF87. These instruments have been translated, validated, and used in many different countries.11
The CHQ-PF50 and CHQ-CF87 have domains in common that can be compared (Table 1). Domains in the parent and child questionnaires were derived from the same constructs but have minor differences. Specifically, the questionnaires differ with respect to the number of questions and the simplicity of wording and response choices. Of note, consistent numbers and contents of items for the 2 CHQ formats are present only for the domains of bodily pain, family activities, and family cohesion. The 2 domains related to impact on parents (parental impact, emotional, and parental impact, time) and the general medical questions are included in the parent-completed CHQ only. For both questionnaires, raw domain scores are scaled to a maximal score of 100. Higher scores on both the parent- and child-completed CHQs indicate better health or higher functioning for the child. Questionnaires were administered to each parent/child dyad at the individual sites by the same examiners. The administrator was blinded to all scores, because scoring was performed at the data coordinating centers. The responding parents were defined as the primary caregivers or legal guardians.
TABLE 1.
Interpretation of Scores for CHQ-PF50 Domains
| Domain | Low Score | High Score |
|---|---|---|
| Physical function | Child is limited in performing all physical activities, including self- care, because of health |
Child performs all types of physical activities, including the most vigorous, without limitations attributable to health |
| Role, emotional | Child is limited in school work or activities with friends as a result of emotional problems |
Child has no limitations in school work or activities with friends as a result of emotional problems |
| Role, physical | Child is limited in school work or activities with friends as a result of physical health |
Child has no limitations in school work or activities with friends as a result of physical health |
| Bodily pain | Child has severe, frequent, and limiting bodily pain | Child has no pain or limitations attributable to pain |
| General behavior | Child often exhibits aggressive, immature, and delinquent behavior | Child never exhibits aggressive, immature, or delinquent behavior |
| Mental health | Child has feelings of anxiety and depression all of the time | Child feels peaceful, happy, and calm all of the time |
| Self-esteem | Child is very dissatisfied with abilities, looks, family/peer relationships, and life overall |
Child is very satisfied with abilities, looks, family/peer relationships, and life overall |
| General healtha | Parent believes child’s health is poor and likely to get worse | Parent believes child’s health is excellent and will continue to be so |
| Family activitiesa | Child’s health often limits and interrupts family activities or is a source of family tension |
Child’s health never limits or interrupts family activities or is a source of family tension |
| Family cohesiona | Family’s ability to get along is rated poor | Family’s ability to get along is rated excellent |
Included in the Parent CHQ-PF50 only. Adapted from Klassen et al.25
Data Analyses
Data are presented as frequencies, medians with ranges, or means±SDs as appropriate. Where data were missing, the number of available values is given. Parent-completed CHQ-PF50 summary and domain scores were converted to z scores on the basis of published normative data and were tested for deviation from normality by using single-sample, signed-rank tests, because z score values were not normally distributed.10 Of note, normative data were not available for the domains of family activities and family cohesion. Because the distribution of paired differences was normal (as confirmed with plots and tests for normality), comparisons between raw domain scores for the parent- and child-completed questionnaires were made by using paired t tests. A positive difference between the child- and parent-completed questionnaires indicates that the child’s perception is better than the parent’s perception of the child’s health. Factors associated with differences between parent- and child-completed CHQ domain scores were explored with bivariate regression analyses only. Multivariate analyses were pursued but proved not to be feasible, given the large number of variables tested and the smaller numbers of subjects with complete data for all variables. All analyses were performed by using SAS 9 (SAS Institute, Cary, NC).
RESULTS
Participation
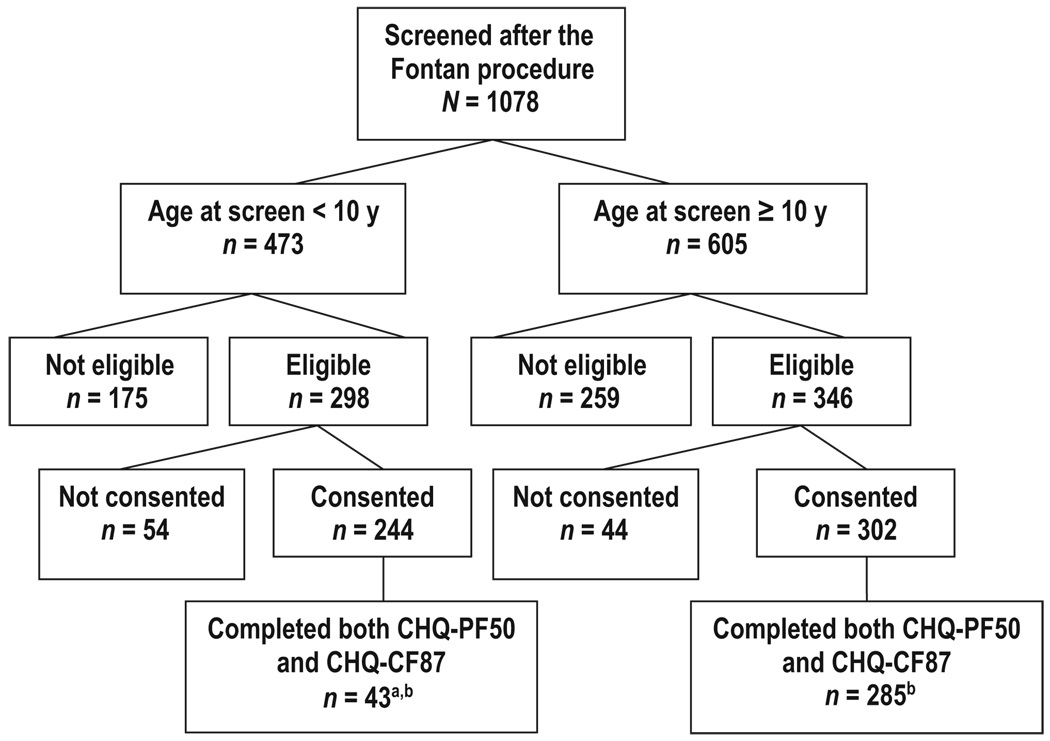
A total of 1078 subjects from 7 centers in the United States and Canada were screened; 644 (60%) were eligible for the study, and 546 (86%) consented to participate in the cross-sectional study. Enrollment began in March 2003 and was completed in April 2004. Age, time since the Fontan procedure, and health status scores were similar for enrolled subjects and eligible but not enrolled subjects.9 We reported previously on the demographic and medical history characteristics of the 537 enrolled subjects 6 to 18 years of age with both parent-completed CHQ-PF50 and medical record abstraction data.4 Of the 537 parents/guardians who completed the CHQ for the enrolled subjects, 457 (85%) were female, 77 (14%) male, and 3 (1%) of unknown gender. Among 354 subjects (65%) who were 10 to 18 years of age (Fig 1) and therefore were eligible to complete the child-completed CHQ-CF87 questionnaire, 328 parent/child pairs (93%) completed the respective CHQ (99% in English). At least some physical assistance (reading or writing) to complete the questionnaire was provided for 6 parents (<2%) and 43 children (14%). As part of the study protocol, 286 (87%) of 328 children underwent standardized cardiopulmonary exercise testing, the results of which were reported previously.12,13
FIGURE 1.
Fontan procedure study participants. a These 43 subjects reached 10 years of age after initial screening but before enrollment completion, thus becoming eligible to complete the CHQ-CF87. b 43 + 285 = 328 study patients.
Subject Characteristics
The characteristics of the 328 subjects for whom both parent and child CHQs were completed are shown in Table 2.
TABLE 2.
Demographic Characteristics and Medical Morbidities for 328 Subjects With Parent-Completed and Child-Completed CHQ Results
| Age at enrollment, y (N = 328) | |
| Mean ± SD | 13.9±2.6 |
| Median (interquartile range) | 13.6 (11.5–16.0) |
| Range | 10.0–18.9 |
| Prepubescent, n (%)a | 156 (48) |
| Male, n (%) | 195 (60) |
| Time since Fontan procedure, y (N = 328) | |
| Mean ± SD | 10.4±2.9 |
| Median (interquartile range) | 10.5 (8.3–12.4) |
| Range | 1.8–17.3 |
| Ethnicity, n (%) | |
| White | 273 (84) |
| Black | 31 (10) |
| Asian | 7 (2) |
| Other | 16 (5) |
| Missing data | 1 |
| Predominant ventricular morphologic features, n (%) | |
| Left ventricular | 172 (52) |
| Right ventricular | 101 (31) |
| Mixed | 55 (17) |
| Stage II (superior cavopulmonary anastamosis), n (%) | 211 (64) |
| Age at Fontan procedure, y (N = 328) | |
| Mean ± SD | 3.6±2.3 |
| Median (interquartile range) | 2.9 (2.2–4.4) |
| Range | 0.8–14.6 |
| Type of Fontan procedure, n (%) | |
| Atriopulmonary connection | 70 (21) |
| TCPC, intracardiac lateral tunnel | 199 (61) |
| TCPC, extracardiac lateral tunnel | 20 (6) |
| TCPC, extracardiac conduit | 29 (9) |
| Other | 10 (3) |
| Fenestration performed during Fontan procedure, n (%) | 198 (60) |
| Current pacemaker, n (%) | 44 (13) |
| Receiving cardiac medications, n (%) | 192 (59) |
| Post–Fontan procedure morbidities, n (%)b | |
| Stroke | 9 (3) |
| Thrombosis | 21 (6) |
| Protein-losing enteropathy | 12 (4) |
| Arrhythmia | 74 (24) |
| Ventricular dysfunction | 42 (13) |
TCPC indicates total cavopulmonary connection.
Male patients: <14 years; female patients: <12 years.
Excludes events that occurred before the Fontan procedure hospital discharge date.
Parent-Completed CHQ
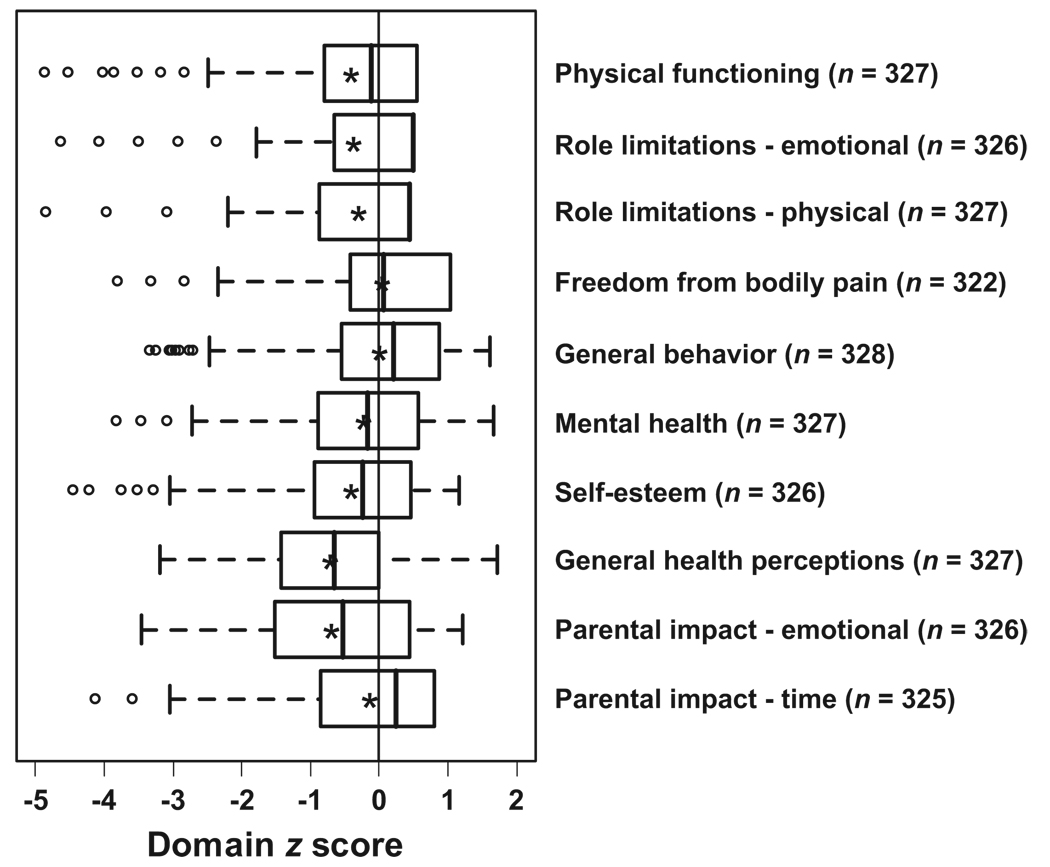
Raw domain scores were converted to z scores on the basis of available normative distributions in the general population. Mean z scores for the domains of physical functioning, self-esteem, general health perceptions, and impact on parents’ emotional wellbeing were significantly worse for questionnaires completed by parents of Fontan procedure survivors, compared with questionnaires completed by parents of children in the normative data set (Fig 2). In contrast, z scores for freedom from bodily pain were significantly higher for Fontan procedure survivors than for healthy children.
FIGURE 2.
Distribution of parent-completed CHQ (CHQ-PF50) domain z scores for the 328 subjects whose children completed the CHQ (CHQ-CF87). The middle line in each box indicates the median, asterisks indicate the means, the left and right edges of the boxes represent the 25th and 75th percentiles, respectively, and the whiskers indicate 1.5 times the interquartile range. Circles indicate outliers.
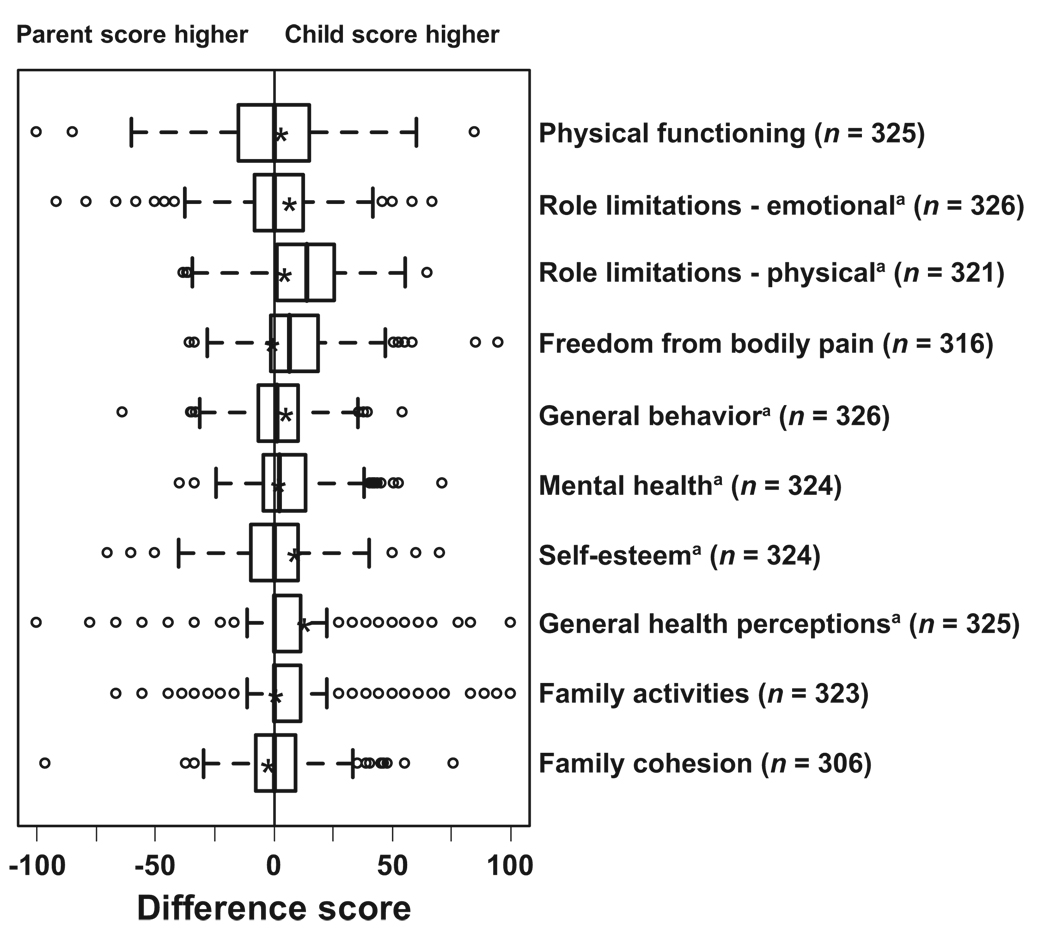
Parent- Versus Child-Completed CHQ Scores
Paired raw score comparisons between parent- and child-completed CHQs were made for common domains, as shown in Fig 3. Raw domain scores were significantly lower (worse functioning) for parent- versus child-completed CHQs for the domains of physical functioning, impact on school or activities from emotional and behavioral problems, impact on school or activities from physical health issues, general behavior, mental health, self-esteem, and general health perceptions. No significant differences were noted for the domains of bodily pain, family cohesiveness, or family activities.
FIGURE 3.
Differences in raw domain scores for the parent-completed CHQ (CHQ-PF50) for the 328 subjects whose children completed the CHQ (CHQ-CF87). The middle line in each box indicates the median, asterisks indicate the means, the left and right edges of the boxes represent the 25th and 75th percentiles, respectively, and the whiskers indicate 1.5 times the interquartile range. Circles indicate outliers. Significant differences between paired raw domain scores, determined with paired t tests and signed rank tests, are indicated.
Factors Associated With Parent-Versus Child-Completed CHQ Differences
An analysis was undertaken to determine possible factors associated with greater differences between parent- and child-completed CHQ scores for the domains of physical functioning and impact of physical limitations. Significant associations in bivariate analyses are reported with the parameter estimate (the amount by which the difference in parent/child raw domain scores changed in the presence of the variable tested) and P value. In general, the associations noted were weak (all R2 values were <0.05). Lower parent- versus child-reported scores for the physical functioning domain were significantly associated with older patient age at enrollment (−0.8 points per each year; P = .02), greater number of years since the Fontan procedure (−0.7 points per each additional year; P = .03), fenestration performed during the Fontan procedure (−6.0 points; P = .001), use of angiotensin-converting enzyme inhibitors at the time of hospital discharge after the Fontan procedure (−4.3 points; P = .02), greater number of post–Fontan procedure interventional cardiac catheterizations (−1.7 points per each additional catheterization; P = .02), greater number of currently used medications at the latest follow-up evaluation (−1.4 points per each additional medication; P = .003), and current use of angiotensin-converting enzyme inhibitors (−3.7 points; P = .04). Lower relative parent-reported scores also were related to both lower and higher levels of annual family income (−11.2 points for less than $20 000, −2.1 points for $20 000 to $39 000, −1.2 points for $40 000 to $59 000, 0 points for $60 000 to $79 000 [reference category], −7.7 points for $80 000 to $99 000, and −5.9 points for $100 000 or more; P = .02). For the 286 patients who completed the exercise testing, significant variables were associated with lower relative parent-reported scores, including higher percentage of predicted oxygen consumption at the anaerobic threshold (0.9 points per each 10% increase; P = .04) and lower percentage of predicted maximal oxygen pulse (1.1 points per each 10% increase; P = .02). From a list of parent-reported, associated, medical or psychosocial conditions for the children, including asthma, nonasthma respiratory problems, allergies, orthopedic problems, sleep problems, vision problems, speech problems, deafness, anxiety, depression, developmental delay, attention problems, learning problems, and behavior problems, only the presence of orthopedic problems was significantly associated with lower parent- versus child-reported physical functioning domain scores (−6.8 points; P = .009).
A similar analysis was performed with respect to the impact of physical limitations domain. Lower parent- versus child-reported scores were associated with and reached statistical significance for the following factors: presence of pulmonary artery abnormalities at the time of the Fontan procedure (−5.7 points; P = .04), fenestration performed during the Fontan procedure (−6.0 points; P = .04) and greater number of post–Fontan procedure cardiac catheterization interventions (−2.9 points per each additional catheterization; P = .008). Higher relative parent-reported scores were noted with older parent age (mean caregiver age: 43 years; range: 31– 64 years) at subject enrollment (0.5 points per year; P < .05). Differences in impact of physical limitations domain scores were not significantly related to any of the exercise testing variables. Lower relative parent-reported scores were associated with a greater number of parent-reported, associated, medical conditions for the child, including anxiety (−8.5 points; P = .02), attention problems (−8.9 points; P = .001), behavior problems (−8.6 points; P = .02), nonasthma respiratory problems (−14.6 points; P = .002), depression (−11.1 points; P = .02), developmental delay or mental retardation (−11.8 points; P < .001), learning problems (−9.3 points; P = .001), speech problems (−9.3 points; P = .004), and other chronic medical conditions (−9.6 points; P = .002).
DISCUSSION
We report the first comparison of parent- versus child-completed CHQ findings for children who have undergone the Fontan procedure. Compared with their children’s perceptions, parents reported significantly lower scores (worse functioning) for their children in the domains of physical functioning, impact on school or activities from emotional and behavioral problems, impact on school or activities from physical health issues, general behavior, mental health, self-esteem, and general health perceptions. In explorations of factors that might explain differences in child/parent pairs for the domains of physical functioning and impact of physical limitations, in general the associations were weak. For the physical limitations domain, lower parent- versus child-reported scores were associated with anatomic features such as pulmonary artery anomalies at the time of the Fontan operation and fenestration at the time of the Fontan operation. Lower parent- versus child-reported scores also were associated with the presence of multiple noncardiac medical conditions in the children.
Among patients with CHDs, those with a single ventricle who have undergone the Fontan procedure are among those most likely to have multiple morbidities. These morbidities include myocardial dysfunction, diminished exercise capacity, arrhythmias, protein-losing enteropathy, thrombotic complications, somatic growth retardation, and adverse neurodevelopmental outcomes.2,4,14 Certain noncardiac morbidities, such as asthma and nonasthma respiratory problems, allergies, orthopedic problems, sleep and speech problems, anxiety, developmental delays, and learning and behavior problems, have been identified as having an impact on functional health status.3,15 As this population reaches adolescence and adulthood, it becomes increasingly important to understand the impact of these comorbidities on functional outcomes and quality of life, to design useful interventions.
The terminology used to describe functional health status and health-related quality of life has been inconsistent in the CHD literature. Gill and Feinstein16 defined quality of life as follows: “Rather than being a description of patient’s health status, quality of life is a reflection of the way that patients perceive and react to their health status and to other, nonmedical aspects of their lives.” In a review of 70 articles published in the medical literature, using the 10 criteria developed by Gill and Feinstein,16 Moons et al17 found that “quality of life assessments in patients with CHDs showed major conceptual and methodological drawbacks.” They also found that the term “quality of life” often was used inappropriately. This observation was supported by several articles in which the authors drew conclusions about quality of life although it was not specifically measured. 17 The CHQ measures the magnitude of perceived overall functioning as affected by health-related issues, which we have equated with the term health status.3 Functional health status is subjective and should be assessed as perceived by patients themselves whenever possible.18
Few studies have examined differences between parent and child reports of functional health status.8,19–27 Similar to our findings, other studies reported a tendency for the parents of children with serious or chronic illnesses to report poorer health status for their children than the children reported for themselves. Britto et al8 suggested that differences may reflect a generally more optimistic future outlook by adolescents than by their parents or perhaps less-than-full disclosure of prognoses to the adolescents. Havermans et al24 evaluated 36 patients by using a validated cystic fibrosis questionnaire. Their findings were similar to those of Britto et al,8 in that the children reported their quality of life to be better than their parents reported, especially with regard to body image, emotional functioning, and treatment burden. The authors concluded that children may “adapt better to their situation and rate the impact of the illness to be less.”24 Klassen et al25 evaluated the agreement between parent and children reports of quality of life for children with attention-deficit/hyperactivity disorder, by using the CHQ. They also demonstrated a more-optimistic outlook for the adolescents, compared with their parents.
Theunissen et al26 studied 1105 Dutch children by using the Netherlands Organization for Applied Scientific Research Academic Medical Center (TNO-AZL) Children’s Quality of Life questionnaire to evaluate the agreement between child and parent reports of children’s health-related quality of life. In contrast to our study, the children reported significantly lower health-related quality of life than did their parents. In a large study by Waters et al,27 2096 parent/adolescent dyads with or without illness were evaluated by using the CHQ, with the aim of examining the extent to which parents and their adolescent children agreed or disagreed regarding physical, emotional, mental, and social domains of health and well-being. That study also showed a less-optimistic evaluation by the adolescents, compared with their parents, for both normal adolescents and children diagnosed as having generic chronic illnesses.27 The authors found that the most disagreement was observed for family activities, body pain, general health, and mental health, with significantly lower health experienced by those with illnesses. In both of those studies,26,27 the authors concluded that large differences between child and parent reports could exist and “relying on parent report will only partly inform the clinician of the severity of health experienced.”27
In CHDs, overprotective parental behavior is not necessarily related to the severity of the lesion.22,28 Cheuk et al29 assessed parents’ knowledge about their child’s heart disease, treatment, and prevention of complications for relatively simple defects. That study suggested that parents have important knowledge gaps. Parent/child differences in their assessments of health status also may be attributable to the adolescents’ state of cognitive development, because they view themselves as relatively invulnerable.8 Given that these children have been living with CHDs their entire lives, they may have a different definition of “healthy” than their parents. However, parents have additional stressors related to feelings of distress and hopelessness and to financial concerns,22,30 which can adversely affect their perceived quality of life and perceptions about their child. Consideration must be given to a family’s ability to return to “normalcy” after cardiac surgery. Families that do not develop appropriate coping mechanisms may underestimate the child’s health after the Fontan procedure; the reverse may be true for families that are more resilient.
Certain limitations pertain to this study. We relied on the use of published normative data rather than simultaneously studying a cohort of normal control subjects. We had only cross-sectional data and could not explore temporal trends in health perceptions, such as whether children’s ratings become more like those of their parents as the children become adults. A significant limitation of this study is the use of a generic functional health status instrument, rather than one with a disease-specific module. Generic measurements have been useful in comparisons of patient groups with each other and with normal subjects. 19,23–27,30 However, Britto et al8 pointed out in their study “significant concerns about the comparability of the adolescent and parent forms of the CHQ,” which may contribute to differences in reports between parents and adolescents. These potential measurement issues related to the CHQ must be viewed as a limitation. Finally, we evaluated only children 10 to 18 years of age, because the CHQ is not applicable to children <10 years of age. Similarly, available normative data for the parent-completed CHQ span a patient age range larger than that for our study population, which might influence generalizability. Therefore, our results may not be generalizable to children <10 years of age.
CONCLUSIONS
We conclude that the perceived functional health status of children who have undergone the Fontan procedure differs between parents and their children. It is important that clinicians consider both parent and patient viewpoints when counseling patients. Support groups, parent and patient education, and other interventions may be necessary to help parents and families cope with the long-term issues associated with Fontan procedure physiologic conditions.
Future research in the development of disease- and age-specific tools to measure child health-related quality of life would provide an important contribution to quality of life research. The development of parent and patient education tools may benefit families in developing coping mechanisms. Finally, it may be of interest to evaluate the impact of the parent’s gender in relationship to the gender of the child.
WHAT’S KNOWN ON THIS SUBJECT
Survival is now expected for patients with single-ventricle physiologic features after the Fontan procedure, and concerns about functional health status have arisen. The assessment of functional health status may differ depending on the perspective of parents versus patients.
WHAT THIS STUDY ADDS
Parents’ perceptions of the functional health status of their children after the Fontan procedure were worse than the children’s perceptions, and few factors associated with these differences were noted. Qualitative assessment may be more informative.
ACKNOWLEDGMENTS
This work was supported by grants from the National Heart, Lung, and Blood Institute (grants HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, and HL068288).
The Pediatric Heart Network Investigators were as follows: National Heart, Lung, and Blood Institute: Gail Pearson, Mario Stylianou, Judith Massicot-Fisher, Marsha Mathis, and Victoria Pemberton (data coordinating center): New England Research Institutes, Lynn Sleeper, Steven Colan, Paul Mitchell, Dianne Gallagher, Patti Nash, Gloria Klein, and Minmin Lu; network chair: Lynn Mahony, University of Texas Southwestern Medical Center; clinical site investigators: Children’s Hospital Boston, Jane Newburger (principal investigator), Stephen Roth, Roger Breitbart, Jonathan Rhodes, Jodi Elder, and Ellen McGrath; Children’s Hospital of New York, Welton M. Gersony (principal investigator), Seema Mital, Beth Printz, Ashwin Prakash, and Darlene Servedio; Children’s Hospital of Philadelphia, Victoria Vetter (principal investigator), Bernard J. Clark, Mark Fogel, Steven Paridon, Jack Rychik, Margaret Harkins, and Jamie Koh; Duke University, Page A. W. Anderson (principal investigator), Rene Herlong, Lynne Hurwitz, Jennifer S. Li, and Ann Marie Nawrocki; Medical University of South Carolina, J. Philip Saul (principal investigator), Andrew M. Atz, Andrew D. Blaufox, Girish Shirali, Jon Lucas, and Amy Blevins; Primary Children’s Medical Center, LuAnn Minich (principal investigator), Richard Williams, Linda Lambert, and Michael Puchalski; Hospital for Sick Children, Brian McCrindle (principal investigator), Timothy Bradley, Kevin Roman, Jennifer Russell, Shi- Joon Yoo, Elizabeth Radojewski, and Nancy Slater; core laboratories: cardiac MRI, Children’s Hospital Boston, Tal Geva (director) and Andrew J. Powell; echocardiography, Children’s Hospital Boston, Steven Colan (director), Marcy Schwartz, and Renee Margossian; protocol review committee: Michael Artman (chair), Dana Connolly, Timothy Feltes, Julie Johnson, Jeffrey Krischer, and G. Paul Matherne; data and safety monitoring board: John Kugler (chair), Kathryn Davis, David J. Driscoll, Mark Galantowicz, Sally A. Hunsberger, Thomas J. Knight, Catherine L. Webb, and Lawrence Wissow.
ABBREVIATIONS
- CHQ
Child Health Questionnaire
- CHD
congenital heart defect
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Steinberger EK, Ferencz C, Loffredo CA. Infants with single ventricle: a population-based epidemiological study. Teratology. 2002;65(3):106–115. doi: 10.1002/tera.10017. [DOI] [PubMed] [Google Scholar]
- 2.Marino BS. Outcomes after the Fontan procedure. Curr Opin Pediatr. 2002;14(5):620–626. doi: 10.1097/00008480-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 3.McCrindle BW, Williams RV, Mitchell PD, et al. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation. 2006;113(8):1123–1129. doi: 10.1161/CIRCULATIONAHA.105.576660. [DOI] [PubMed] [Google Scholar]
- 4.Sleeper LA, Anderson P, Hsu DT, et al. Design of a large cross-sectional study to facilitate future clinical trials in children with the Fontan palliation. Am Heart J. 2006;152(3):427–433. doi: 10.1016/j.ahj.2006.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kamphuis M, Zwinderman KH, Vogels T, et al. A cardiac-specific health-related quality of life module for young adults with congenital heart disease: development and validation. Qual Life Res. 2004;13(4):735–745. doi: 10.1023/B:QURE.0000021690.84029.a3. [DOI] [PubMed] [Google Scholar]
- 6.Moons P, Van Deyk K, De Geest S, Gewillig M, Budts W. Is the severity of congenital heart disease associated with the quality of life and perceived health of adult patients? Heart. 2005;91(9):1193–1198. doi: 10.1136/hrt.2004.042234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pike NA, Evangelista LS, Doering LV, Koniak-Griffin D, Lewis AB, Child JS. Health-related quality of life: a closer look at related research in patients who have undergone the Fontan operation over the last decade. Heart Lung. 2007;36(1):3–15. doi: 10.1016/j.hrtlng.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Britto MT, Kotagal UR, Chenier T, Tsevat J, Atherton HD, Wilmott RW. Differences between adolescents’ and parents’ reports of health-related quality of life in cystic fibrosis. Pediatr Pulmonol. 2004;37(2):165–171. doi: 10.1002/ppul.10436. [DOI] [PubMed] [Google Scholar]
- 9.Anderson PAW, Sleeper LA, Mahony L, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multi-center study. JAmColl Cardiol. 2008;52(2):85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landgraf JL, Abetz L, Ware JE. The CHQ User’s Manual. 1st ed. Boston, MA: The Health Institute; 1996. [Google Scholar]
- 11.Ruperto N, Ravelli A, Pistorio A, et al. Cross-cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries: review of the general methodology. Clin Exp Rheumatol. 2001;19 4 suppl 23:S1–S9. [PubMed] [Google Scholar]
- 12.McCrindle BW, Williams RV, Mital S, et al. Reduced physical activity levels after the Fontan procedure: related to exercise capacity or own health perception? Arch Dis Child. 2007;92(6):509–514. doi: 10.1136/adc.2006.105239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paridon SM, Mitchell PD, Colan SD, et al. A cross-sectional study of exercise performance during the first two decades of life following the Fontan operation. J Am Coll Cardiol. 2008;52(2):99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 14.Freedom RM, Hamilton R, Yoo SJ, et al. The Fontan procedure: analysis of cohorts and late complications. Cardiol Young. 2000;10(4):307–331. doi: 10.1017/s1047951100009616. [DOI] [PubMed] [Google Scholar]
- 15.Rose M, Kohler K, Kohler F, Sawitzky B, Fliege H, Klapp BF. Determinants of the quality of life of patients with congenital heart disease. Qual Life Res. 2005;14(1):35–43. doi: 10.1007/s11136-004-0611-7. [DOI] [PubMed] [Google Scholar]
- 16.Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA. 1994;272(8):619–626. [PubMed] [Google Scholar]
- 17.Moons P, Van Deyk K, Budts W, De Geest S. Caliber of quality-of-life assessments in congenital heart disease: a plea for more conceptual and methodological rigor. Arch Pediatr Adolesc Med. 2004;158(11):1062–1069. doi: 10.1001/archpedi.158.11.1062. [DOI] [PubMed] [Google Scholar]
- 18.Matza LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health. 2004;7(1):79–92. doi: 10.1111/j.1524-4733.2004.71273.x. [DOI] [PubMed] [Google Scholar]
- 19.Walker RE, Gauvreau K, Jenkins KJ. Health-related quality of life in children attending a cardiology clinic. Pediatr Cardiol. 2004;25(1):40–48. doi: 10.1007/s00246-003-0348-z. [DOI] [PubMed] [Google Scholar]
- 20.Goldbeck L, Melches J. Quality of life in families of children with congenital heart disease. Qual Life Res. 2005;14(8):1915–1924. doi: 10.1007/s11136-005-4327-0. [DOI] [PubMed] [Google Scholar]
- 21.Lara M, Duan N, Sherbourne C, et al. Differences between child and parent reports of symptoms among Latino children with asthma. Pediatrics. 1998;102(6) doi: 10.1542/peds.102.6.e68. Available at: 102/6/e68 www.pediatrics.org/cgi/content/full/ [DOI] [PubMed] [Google Scholar]
- 22.Lawoko S, Soares JJ. Quality of life among parents of children with congenital heart disease, parents of children with other diseases and parents of healthy children. Qual Life Res. 2003;12(6):655–666. doi: 10.1023/a:1025114331419. [DOI] [PubMed] [Google Scholar]
- 23.Russell KM, Hudson M, Long A, Phipps S. Assessment of health-related quality of life in children with cancer: consistency and agreement between parent and child reports. Cancer. 2006;106(10):2267–2274. doi: 10.1002/cncr.21871. [DOI] [PubMed] [Google Scholar]
- 24.Havermans M, Vreys M, Proesmans M, De Boeck C. Assessment of agreement between parents and children on health-related quality of life in children with cystic fibrosis. Child Care Health Dev. 2006;32(1):1–7. doi: 10.1111/j.1365-2214.2006.00564.x. [DOI] [PubMed] [Google Scholar]
- 25.Klassen AF, Miller A, Fine S. Agreement between parent and child report of quality of life in children with attention-deficit/hyperactivity disorder. Child Care Health Dev. 2006;32(4):397–406. doi: 10.1111/j.1365-2214.2006.00609.x. [DOI] [PubMed] [Google Scholar]
- 26.Theunissen NC, Bogels TG, Koopman HM, Verrips GH, Zwinderman KA. The proxy problem: child report versus parent report in health-related quality of life research. Qual Life Res. 1998;7(5):387–397. doi: 10.1023/a:1008801802877. [DOI] [PubMed] [Google Scholar]
- 27.Waters E, Stewart-Brown S, Fitzpatrick R. Agreement between adolescent self-report and parent reports of health and well-being: results of an epidemiological study. Child Care Health Dev. 2003;29(6):501–509. doi: 10.1046/j.1365-2214.2003.00370.x. [DOI] [PubMed] [Google Scholar]
- 28.Daliento L, Mapelli D, Volpe B. Measurement of cognitive outcome and quality of life in congenital heart disease. Heart. 2006;92(4):569–574. doi: 10.1136/hrt.2004.057273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheuk DK, Wong SM, Choi YP, Chau AK, Cheung YF. Parents’ understanding of their child’s congenital heart disease. Heart. 2004;90(4):435–439. doi: 10.1136/hrt.2003.014092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Majnemer A, Limperopoulos C, Shevell M, Rohlicek C, Rosenblatt B, Tchervenkov C. Health and well-being of children with congenital cardiac malformations, and their families, following open-heart surgery. Cardiol Young. 2006;16(2):157–164. doi: 10.1017/S1047951106000096. [DOI] [PubMed] [Google Scholar]