Abstract
Contingency management (CM) is an efficacious intervention for cocaine abusing methadone patients, but typically only about half of patients respond. By investigating time to onset of cocaine abstinence and factors associated with abstinence, we may be able to more efficiently direct CM approaches to patients most likely to benefit. Onset of cocaine abstinence was evaluated in cocaine abusing methadone maintenance patients (N = 193) enrolled in one of three randomized clinical trials of CM. Participants received standard treatment with frequent urine toxicology monitoring or standard treatment plus CM during the trials. Slightly more than half the sample obtained at least one week of cocaine abstinence, and approximately a third of the sample obtained at least four weeks of cocaine abstinence. Discrete-time survival and hazard analyses found Weeks 1 and 2 of the intervention period had the greatest probability for the initiation of abstinence, and few participants initiated any period of abstinence after Week 4. Patients randomized to CM, those with more years of cocaine use, and those with less recent cocaine use were more likely to achieve abstinence. Overall, these results indicate onset of cocaine abstinence is likely to occur early in treatment and in individuals with less severe cocaine use. Practical implications of these results for designing and implementing CM interventions in methadone maintenance clinics are discussed.
Keywords: cocaine abstinence, contingency management, methadone maintenance, treatment response, discrete-time analysis
Approximately 40% to 60% of patients receiving methadone maintenance therapy use cocaine, which is associated with risky behaviors, adverse consequences, and poor treatment outcome (DeMaria, Steling, & Weinstein, 2000; Dunteman, Condelli, & Fairbank, 1992; Kidorf, Stitzer, & Brooner, 1994). Contingency management (CM) is an empirically supported intervention with demonstrated efficacy in promoting cocaine abstinence in methadone maintenance patients (Griffith, Rowan-Szal, Roark, & Simpson, 2000; Lussier, Heli, Mongeon, Badger, & Higgins, 2006; Prendergast, Podus, Finney, Greenwell, & Roll, 2006). It offers reinforcers, such as monetary vouchers or prizes, to patients who have refrained from drug use as assessed by frequent urinalysis testing. While highly efficacious, not all methadone patients receiving CM for cocaine abstinence initiate any period of abstinence or earn any reinforcement (Stitzer & Petry, 2006), which raises questions about how best to implement a CM intervention. Continuing to offer reinforcement for extended periods to patients who do not achieve abstinence may be inefficient.
Typically, CM interventions are in effect for 2 to 4 months in duration. While effect sizes of CM are medium to large in comparison to standard care conditions (Lussier et al., 2006; Prendergast et al., 2006), a proportion of patients continue to use drugs and do not receive contingencies despite intervention. For example, in a large multi-site study by Peirce and colleagues (2006), 30% of participants in the CM condition failed to provide even one negative specimen and thus did not receive any reinforcement. Moreover, only one in four participants in the CM condition ever achieved an extended period of abstinence (i.e., 4 weeks). Response rates in methadone maintenance patients are even lower when CM interventions target multiple drugs of abuse concurrently (Dallery, Silverman, Chutuape, Bigelow, & Stitzer, 2001; Downey, Helmus, & Schuster, 2000; Piotrowski et al., 1999). Overall, while CM improves abstinence rates compared to standard care, a substantial proportion of patients do not respond.
Those who do respond to CM interventions appear to do so early in treatment, and early response during first few weeks of treatment is predictive of long-term outcome in methadone patients (Morral, Belding, & Iguchi, 1999; Preston et al., 1998; Strain, Stitzer, Liebson, & Bigelow, 1998). For example, Silverman and colleagues (2004) found that while less than 20% of samples tested negative for stimulants during a baseline monitoring period, the percentage of negative samples quickly improved to approximately 50% within the first few weeks after randomization to the CM condition. Once abstinent, most participants remained drug-free during the intervention. Thus, early treatment response appears to be a robust indicator of overall treatment response.
While efficacious for many individuals, providing CM has programmatic costs beyond those of the reinforcers, and continuing to offer the intervention to individuals who are not benefiting may not be cost-effective. For example, staff time for meeting with clients along with the price of frequent urinalysis testing add significantly to the cost of the intervention (Olmstead, Sindelar, & Petry, 2007), and the longer CM interventions are kept in place, the greater the administrative costs. Identifying timeframes over which CM is most or least effective is important in a financially strapped treatment system.
The objective of the present study was to investigate the initiation of cocaine abstinence in methadone maintenance patients receiving CM treatments. To isolate the effects of CM relative to those associated with frequent urinalysis monitoring or motivational effects associated with entering a voluntary cocaine treatment study during methadone treatment, we compared onset of abstinence in patients randomized to CM to those randomized to standard care. Two durations of abstinence were examined: one or more weeks, and four or more weeks. On the basis of prior studies, we hypothesized most participants achieving a period of sustained abstinence would do so within the initial weeks of the study intervention period. However, if substantial proportions of patients who achieved abstinence did so later in the intervention period, such results would suggest CM interventions should be applied for longer durations of time, even among early non-responders. We also investigated demographic and drug use factors associated with achieving abstinence with the expectation that those with less recent cocaine use at baseline would be more likely to become abstinent during the study period.
Method
Participants
Participants were 193 methadone maintenance patients enrolled in one of three randomized clinical trials of CM conducted in an urban community methadone clinic (Petry, Alessi, Hanson, & Sierra, 2007; Petry & Martin, 2002; Petry, Martin, & Simcic, 2005). Across the trials, inclusion criteria included past-year diagnosis of cocaine abuse or dependence, stable methadone dose for at least one month, and ability to speak English. Exclusion criteria were cognitive impairment and uncontrolled psychiatric disorder. All participants provided written informed consent, approved by the university’s Institutional Review Board.
Procedures
Data collection procedures were identical across the three trials. Following informed consent, participants completed a baseline evaluation including basic demographic information, drug use and treatment histories, and the substance use disorders module of the Structure Clinical Interview for the DSM-IV (First, Spitzer, Gibbon, & Williams, 1996; Kranzler, Kadden, Babor, Tennen, & Rounsaville, 1996; Williams et al., 1992).
Participants in all three trials were randomly assigned to 12-week standard treatment, or 12-week standard treatment plus CM. Throughout the 12-week intervention period, a research assistant collected urine samples using OnTrak TesTstiks (Varian, Inc., Walnut Creek, CA), an onsite testing system, from participants 2 to 3 days per week with 2 to 4 days between tests. Up to 36 urine samples were collected over the 12-week period and tested for cocaine and opioids.
Abstinence was determined via the samples, with a week of abstinence defined as a 7-day period during which all urinalysis samples tested negative for cocaine. Unexcused, missed or positive samples ended a period of abstinence.
Standard Treatment
Standard treatment consisted of daily methadone doses and weekly individual and/or group counseling provided by clinic staff plus frequent sample monitoring, described above.
Contingency Management Treatment
In addition to receiving the standard treatment, participants randomized to the CM conditions could earn reinforcement for completion of target behaviors. Target behaviors and reinforcement varied by clinical trial and are described briefly below. Additional information about the procedures is available in the primary studies.
The Petry and Martin (2002) study used a prize CM procedure for cocaine and opiate abstinence. One draw from a prize bowl was earned when a sample tested negative for cocaine or opiates. Participants earned bonus draws if the sample was negative for both drugs, and bonus draws increased for successive weeks of abstinence. An unexcused sample, refusal to submit a sample, or a positive sample resulted in no draws for that week and the number of bonus draws was reset to the initial level. In total, participants could earn up to 234 draws if they provided negative samples throughout the 12-week treatment. On average, participants in the CM condition earned 108.2 draws (SD = 66.1) and $137 in prizes.
The Petry et al. (2005) study used a prize CM procedure for cocaine abstinence and group therapy attendance, with each target behavior reinforced independently. For cocaine abstinence, participants earned one draw for each urine sample that tested negative for cocaine. The number of draws earned escalated with each consecutive cocaine negative sample. In addition, participants earned draws for attending group therapy once per week. Draws started at one and escalated for each consecutive week they attended a group therapy session. Participants could earn up to 270 draws for abstinence and 78 draws for attendance from a prize bowl over the 12-week period. Reset contingencies were in place for unexcused samples, positive samples, refusal to submit a sample, or unexcused treatment absences. On average, participants in the CM condition earned 62.4 draws (SD = 88.2) for negative urine samples. Combined, participants earned on average $117 in prizes for both group therapy attendance and negative samples.
The Petry et al. (2007) study compared prize and voucher CM procedures to standard treatment. Draws and vouchers started at one draw from a prize bowl or $3, respectively, per cocaine negative sample, and increased by one draw or $3 for consecutive negative samples, up to 10 draws or $30 per negative sample. Draws and vouchers were reset to the initial level, respectively, for unexcused, refused, and positive samples. Participants could earn up to 195 draws or $585 in vouchers. In the prize CM condition, participants earned on average 89.4 draws (SD = 85.4) and $203 in prizes. In the voucher CM condition, participants earned on average $272 in vouchers.
Across the three clinical trials, the prize bowls contained slips of paper associated with $1, $20 and $100 prizes, as well as 50% non-winning slips. The overall average maximum value of prizes that could be earned varied according to trial, with a range of $350 to $500.
Data Analysis
As cocaine abstinence was the only common behavior reinforced across all trials, analyses focus on cocaine abstinence. Demographic and baseline substance use variables were compared between participants who achieved cocaine abstinence versus those who did not. Chi-squared tests were used for categorical variables, and ANOVA tested for differences in continuous variables.
Discrete-time survival analysis examined onset of cocaine abstinence (Singer & Willett, 2003). We evaluated two separate durations of cocaine abstinence: one or more weeks and four or more weeks, corresponding to the median and mean duration of cocaine abstinence achieved by the entire sample. Cocaine abstinence onset was recorded as the treatment week at which the individual began his/her period of abstinence. For example, someone who obtains one or four weeks of cocaine abstinence at the start of treatment will have onset of cocaine abstinence coded as Week 1. If a patient achieved durations of abstinence twice during the 12-week period, the first period was recorded. Survivor and hazard functions by treatment group detail week-by-week the onset of abstinence for each duration. The survivor function provides a week-by-week estimate on the proportion of the sample that does not experience cocaine abstinence across the intervention period (i.e., continued cocaine use). Conversely, the hazard function provides a conditional probability that the onset of abstinence will occur in a treatment week, given that the person did not obtain abstinence in the previous week. Thus, after Week 1, hazard probabilities indicate the proportion of individuals from the remaining sample who initiate abstinence.
Finally, we fit the discrete-time hazard model to the data using two separate maximum likelihood binary logistic regressions (Singer & Willett, 2003), investigating predictors of achieving at least one week of cocaine abstinence and achieving at least four weeks of abstinence. We constructed two person-period data files for the two periods of abstinence investigated, and in each date file, a participant had the number of records equal to the number of weeks up to either the onset of cocaine abstinence (i.e., event occurrence) or censoring occurs (i.e., study drop-out, or the end of treatment). Weeks of treatment were dummy coded and included up to 12 in the first analysis and up to 9 in the second analysis as onset of cocaine abstinence ≥4 weeks cannot occur Weeks 10 through 12. Initiation of cocaine abstinence was the dependent variable, and predictors of cocaine abstinence included in the model were treatment week, cocaine use variables, clinical trial, and treatment condition. We chose this analytical method as it easily allows for the inclusion of time (i.e., treatment week) in the regression model as compared to other methods, such as Cox proportional-hazards modeling.
Prior to analysis all variables were examined for fit between their distributions and the assumptions of multivariate analysis. Brown-Forsythe is reported for variables that violate the assumptions. All analyses were conducted using SPSS 15.0®, and alpha was set at less than 0.05, unless otherwise specified.
Results
Onset of ≥1 week of cocaine abstinence
Overall, 109 participants (56.5%) achieved one or more weeks of cocaine abstinence. Table 1 presents baseline demographic and clinical characteristics of the sample by abstinence status. Participants who achieved at least one week of abstinence used cocaine for more years but for fewer days in the past month than those who never achieved any abstinence during treatment. Also, participants who achieved cocaine abstinence were more likely to drink alcohol less in the past month, provide a negative baseline cocaine toxicology sample, be randomized to CM treatment, participate in the Petry et al. (2007) study, and provide more cocaine toxicology samples during treatment than non-abstinent individuals. All other variables did not differ significantly between the abstinence groups.
Table 1.
Demographic characteristics by abstinence.
| Variable | Abstinent Less Than One Week (n = 84) |
Abstinent One Week or More (n = 109) |
Statistic (df) | p-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender – Male | 31 | 36.9 | 34 | 31.2 | χ2(1) = 0.69 | .405 |
| Ethnicity | ||||||
| Caucasian | 12 | 14.3 | 24 | 22.0 | χ2(3) = 5.92 | .116 |
| African American | 40 | 47.6 | 36 | 33.0 | ||
| Hispanic | 32 | 38.1 | 47 | 43.1 | ||
| Other | 0 | 0.0 | 2 | 1.8 | ||
| Marital Status | ||||||
| Single | 55 | 65.5 | 67 | 61.5 | χ2(3) = 3.18 | .364 |
| Married/Cohabitating | 6 | 7.1 | 3 | 2.8 | ||
| Divorced/Separated | 20 | 23.8 | 33 | 30.2 | ||
| Widowed | 3 | 3.6 | 6 | 5.5 | ||
| Employment Status | ||||||
| Full-time | 18 | 21.4 | 17 | 15.6 | χ2(3) = 1.21 | .751 |
| Part-time | 11 | 13.1 | 14 | 12.8 | ||
| Unemployed | 54 | 64.3 | 77 | 70.7 | ||
| Other | 1 | 1.2 | 1 | 0.9 | ||
| Clinical Trial | ||||||
| Petry et al. (2002) | 11 | 13.1 | 31 | 28.4 | χ2(2) = 10.16 | .006 |
| Petry et al. (2005) | 43 | 51.2 | 34 | 31.2 | ||
| Petry et al. (2007) | 30 | 35.7 | 44 | 40.4 | ||
| Treatment Condition - CM | 38 | 48.1 | 75 | 68.8 | χ2(2) = 8.19 | .004 |
| Negative Baseline Cocaine Result | 6 | 7.1 | 66 | 60.6 | χ2(1) = 57.86 | .001 |
| M | SD | M | SD | |||
| Age (years) | 40.2 | 6.9 | 39.8 | 7.4 | F(1,191) = 0.16 | .690 |
| Years of Education | 10.9 | 2.1 | 11.0 | 1.9 | F(1,191) = 0.18 | .670 |
| Past Year Days on Methadone | 317.3 | 10.1 | 317.5 | 8.8 | F(1,183) = 0.00 | .984 |
| Current Methadone Dose (mg) | 77.4 | 27.4 | 74.6 | 30.6 | F(1,190) = 0.42 | .517 |
| Years of Cocaine Use | 13.0 | 8.7 | 16.7 | 9.2 | F(1,191) = 8.01 | .005 |
| Prior Treatment Episodes for Cocaine (lifetime) | 3.1 | 4.5 | 4.6 | 7.0 | F(1,186) = 3.36 | .069 |
| Past 30-Day Cocaine Use (days) | 14.8 | 11.8 | 6.0 | 8.5 | F(1,183) = 8.14 | .005 |
| Past 30-Day Alcohol Use (days) | 4.4 | 8.3 | 2.1 | 4.6 | F(1,122) = 5.24 | .024 |
| Past 30-Day Heroin Use (days) | 1.0 | 2.5 | 1.5 | 4.0 | F(1,184) = 1.00 | .318 |
| Past 30-Day Marijuana Use (days) | 1.9 | 6.6 | 2.2 | 6.4 | F(1,191) = 0.06 | .805 |
| Number of Urine Samples Provided During Treatment |
19.9 | 7.9 | 23.3 | 3.7 | F(1,191) = 15.80 | .001 |
Note. Numbers do not always add up to group size due to missing data. Brown-Forsythe statistic reported for past 30-day cocaine use, past 30-day alcohol use, and past 30-day heroin use.
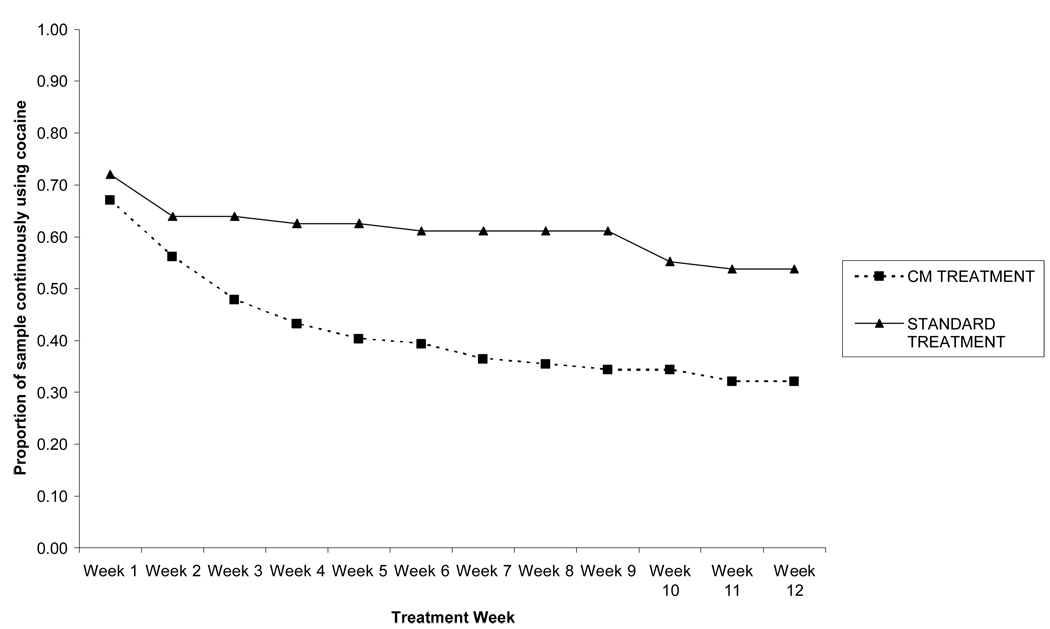
Estimated sample survivor probabilities for standard and CM treatments by treatment week (i.e., Week 1 through 12) were calculated via life tables. The probabilities indicate the proportion of the original sample that had not obtained at least one week of abstinence by the end of each treatment week. As shown in Figure 1, the sample survivor probabilities of the two treatment conditions are approximately similar at Week 1 and quickly diverge with a lower probability of individuals in CM treatment continuously using cocaine. The median survival time for onset of a week or more of cocaine abstinence is 12.00 weeks in the standard treatment condition indicating less than half ever achieved a week or more of abstinence during the treatment period. The median survival time for the CM treatment condition was 3.75 weeks.
Figure 1.
Survival function for onset of ≥1 weeks cocaine abstinence by treatment group.
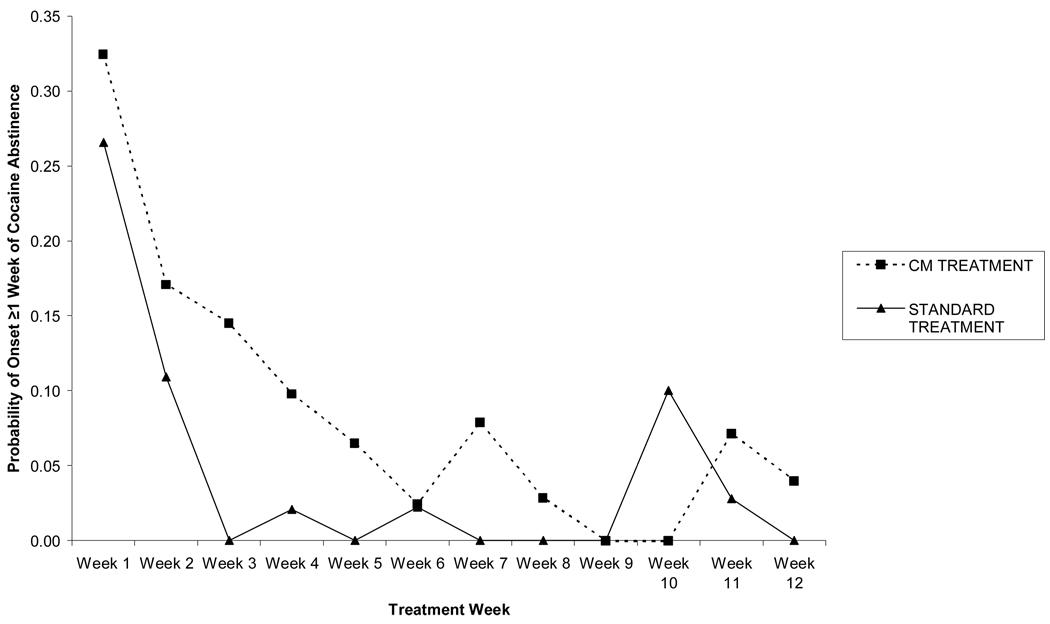
Figure 2 provides hazard probabilities for standard and CM treatments by treatment week. The probabilities indicate the proportion of the sample not abstinent in prior weeks who initiate a week or more of abstinence at that time point. For these figures, the denominator includes only the patients who have not yet achieved abstinence, such that at week 6, the denominator in the standard care condition is 45 (of the initial 79 standard care participants) and is 41 (of the initial 114 CM participants) for the CM condition. For standard treatment, the hazard function indicates few individuals initiate abstinence after Week 2. Meanwhile, for CM treatment the hazard function indicates initiation of abstinence occurs for several more weeks, out to approximately Week 4, with less than 10% of the remaining (not yet abstinent) sample achieving abstinence thereafter.
Figure 2.
Hazard function for onset of ≥1 weeks cocaine abstinence by treatment group.
Finally, maximum likelihood binary logistic regression was used to fit the discrete-time hazard model for onset of one or more weeks of cocaine abstinence. First, a time-only model examined when onset of abstinence is likely to occur, and was significant, χ2(11) = 121.26, p < .001. As shown in Table 2, Week 1 and Week 2 are the only time variables significantly associated with onset of cocaine abstinence, p < .05. A second model included additional predictors entered in a second step: years of cocaine use, days of cocaine use in the past 30-days, baseline cocaine toxicology result, clinical trial, and treatment condition. Using decrement-to-chi-square testing (i.e., -2LL test; Willett & Singer, 1993), the second model fits better than the time-only model, χ2(5) = 559.52 − 472.49 = 87.03, p < .001. As shown in Table 2, Week 1, treatment condition, years of cocaine use, days of cocaine use in the past 30-days, and baseline cocaine toxicology result are significant predictors of cocaine abstinence onset, p <.05. Specifically, those who received CM, used cocaine for more years, and had less recent use are more likely to achieve at least one week of abstinence. In addition, the only time period during the intervention associated with the onset of cocaine abstinence was the first week.
Table 2.
Discrete-time hazard model for onset of one or more weeks cocaine abstinence.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Predictor | Log-odds | Odds Ratio |
Log-odds | Odds Ratio |
| Week 1 | 3.30 | 27.07*** | 2.17* | 0.12 |
| Week 2 | 2.37 | 10.69** | 1.86 | 0.16 |
| Week 3 | 1.75 | 5.73 | 1.36 | 0.26 |
| Week 4 | 1.41 | 4.11 | 1.16 | 0.31 |
| Week 5 | 0.78 | 2.17 | 0.46 | 0.63 |
| Week 6 | 0.42 | 1.52 | 0.07 | 0.93 |
| Week 7 | 0.86 | 2.36 | 0.64 | 0.53 |
| Week 8 | −0.20 | 0.89 | −0.27 | 1.31 |
| Week 9 | −17.06 | 0.00 | −17.06 | 1.00 |
| Week 10 | 1.27 | 3.55 | 1.26 | 0.29 |
| Week 11 | 1.05 | 2.86 | 1.05 | 0.35 |
| Years of Cocaine Use | 0.04* | 1.04 | ||
| Past 30-Day Cocaine Use | −0.05*** | 0.95 | ||
| Baseline Cocaine Result | −1.91*** | 0.15 | ||
| Clinical Trial | ||||
| Petry et al. (2007) | 0.29 | 1.33 | ||
| Petry et al. (2002) | 0.48 | 1.62 | ||
| Treatment Condition | 0.94*** | 2.56 | ||
| −2LL | 559.52 | 472.49 | ||
Note. Reference categories: Baseline Cocaine Result, negative; Clinical Trial, Petry et al. (2005); Treatment Condition, Standard Treatment.
p < .05.
p < .01.
p < .001.
Onset of ≥ 4 week of cocaine abstinence
A parallel set of analyses investigated the onset of four or more weeks of cocaine abstinence. Approximately a third of the sample (n = 66) achieved four or more weeks of cocaine abstinence, and baseline demographic and clinical characteristics were examined for significant differences between the abstinence groups. The same variables differed between the two abstinence groups as was found previously: clinical trial, treatment condition, years of cocaine use, days of cocaine use in the past 30-days, days of alcohol use in the past 30-days, baseline cocaine toxicology result, and number of cocaine toxicology samples provided during the 12 weeks of treatment. In addition, days of heroin use in the past 30-days also differed significantly between the two abstinence groups. All other variables were not significantly different between the abstinence groups (data not shown).
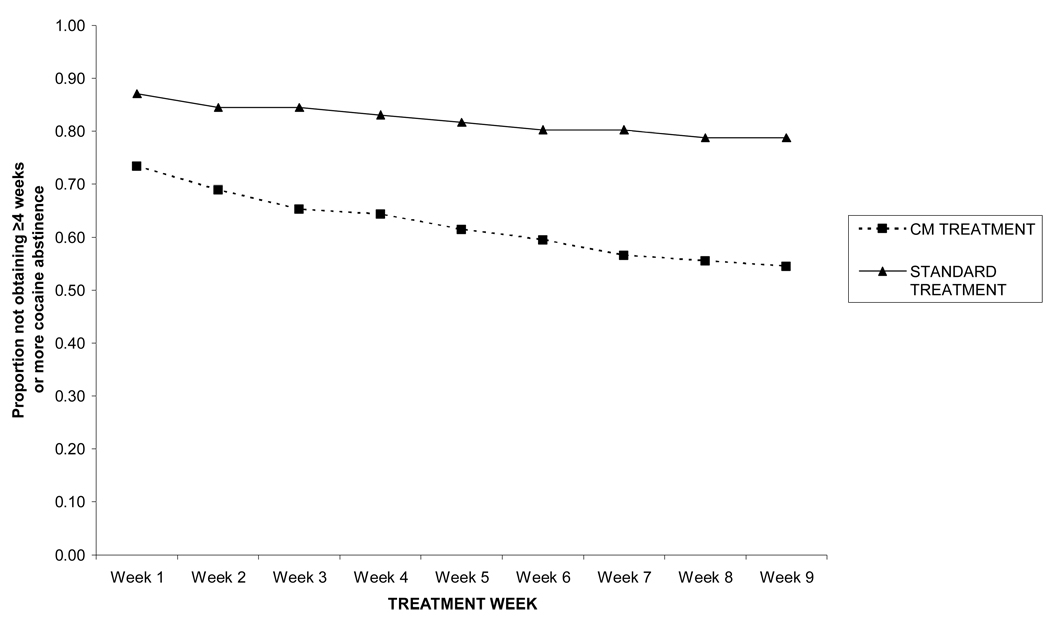
Estimated sample survivor probabilities for standard and CM treatments by treatment week (i.e., Week 1 through 9) were calculated via life tables. As shown in Figure 3, sample survivor probabilities of the two treatments are approximately parallel, albeit with a lower probability of continuous cocaine use for CM participants compared to standard treatment participants. The majority of participants who initiated four or more weeks of cocaine abstinence did so within the first week of treatment, with only nominal proportions achieving sustained abstinence thereafter. The median survival time for onset of four or more weeks of cocaine abstinence is 9.00 weeks for both treatment groups, as less than 50% of both samples achieved four or more weeks of cocaine abstinence. If only participants who achieved four or more weeks of abstinence are selected for inclusion in the analyses, the median survival time for onset is 1.00 weeks for both treatment groups.
Figure 3.
Survival function for onset of ≥4 weeks cocaine abstinence by treatment group.
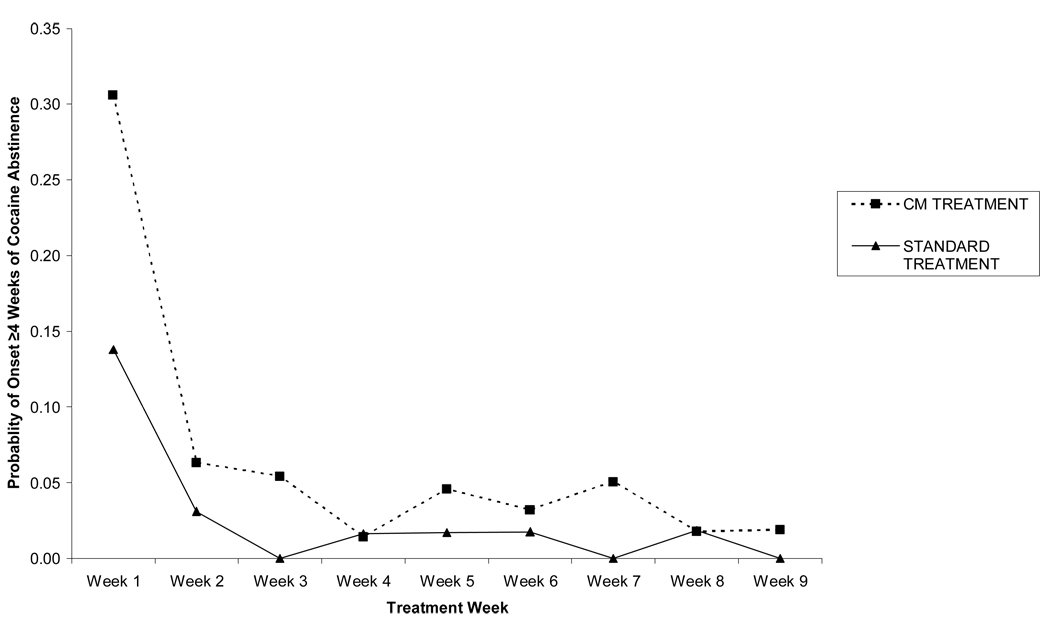
Figure 4 provides hazard probabilities for standard and CM treatments by treatment week. The probabilities indicate proportion of the sample not abstinent in prior weeks who initiate four or more weeks of cocaine abstinence at that time point. The hazard function for both treatment conditions indicates few individuals initiate four or more 4 weeks of continuous abstinence after Week 1. About 25% of CM treatment patients initiate abstinence in Week 1 versus about 12% of standard care patients. Also, throughout the intervention period, a higher proportion of CM participants initiate abstinence than standard care participants, although the percentages of CM participants initiating abstinence are 5% or less of the remaining individuals at each time point.
Figure 4.
Hazard function for onset of ≥4 weeks cocaine abstinence by treatment group.
A maximum likelihood binary logistic regression was used to fit the discrete-time hazard model for onset of four or more weeks of cocaine abstinence. First, a time-only model examined when onset of a month or more of abstinence was likely to occur. The overall time-only model was significant, χ2(9) = 80.80, p <. 001. As shown in Table 3, none of the time variables were significantly associated with onset of cocaine abstinence, p > .05. A second model included additional predictors entered in a second step: years of cocaine use, days of cocaine use in the past 30-days, baseline cocaine toxicology result, clinical trial, and treatment condition. Using decrement-to-chi-square testing, the second model fit better than the time-only model, χ2(5) = 430.25 − 320.22 = 110.03, p < .001. As shown in Table 3, years of cocaine use, days of cocaine use in the past 30-days, baseline cocaine toxicology result, clinical trial, and treatment condition were significant predictors of onset of sustained cocaine abstinence, p <.05. Specifically, those who used cocaine for more years and had less recent use were more likely to achieve four or more weeks of cocaine abstinence. Moreover, participants in the Petry et al. (2007) study and those who received CM were more likely than those in the other trials or those who received standard care to achieve four or more weeks of abstinence.
Table 3.
Discrete-time hazard model for onset of four or more weeks cocaine abstinence.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Predictor | Log-odds | Odds Ratio |
Log-odds | Odds Ratio |
| Week 1 | −22.57 | 0.00 | −20.28 | 0.00 |
| Week 2 | −24.21 | 0.00 | −21.62 | 0.00 |
| Week 3 | −24.72 | 0.00 | −22.02 | 0.00 |
| Week 4 | −25.39 | 0.00 | −22.70 | 0.00 |
| Week 5 | −24.64 | 0.00 | −21.88 | 0.00 |
| Week 6 | −24.88 | 0.00 | −22.10 | 0.00 |
| Week 7 | −24.84 | 0.00 | −21.96 | 0.00 |
| Week 8 | −25.21 | 0.00 | −22.24 | 0.00 |
| Week 9 | −25.88 | 0.00 | −22.87 | 0.00 |
| Years of Cocaine Use | 0.04* | 1.04 | ||
| Past 30-Day Cocaine Use | −0.11*** | 0.89 | ||
| Baseline Cocaine Result | −1.46*** | 0.23 | ||
| Clinical Trial | ||||
| Petry et al. (2007) | 1.02** | 2.77 | ||
| Petry et al. (2002) | −0.04 | 0.97 | ||
| Treatment Condition | 0.93** | 2.53 | ||
| −2LL | 430.25 | 320.22 | ||
Note. Reference categories: Baseline Cocaine Result, negative; Clinical Trial, Petry et al. (2005); Treatment Condition, Standard Treatment.
p < .05.
p < .01.
p < .001.
Discussion
Results of the study indicate that if methadone maintenance patients with cocaine abuse or dependence are to become abstinent from cocaine, the onset of abstinence is proximal, rather than distal, to the start of the frequent substance use monitoring period. We found that less than 10% of participants initiated any period of abstinence four weeks after treatment entry and proportions were even lower for an extended period of abstinence (i.e., ~5%). Thus, a positive response to frequent sample monitoring and CM treatment was likely to occur early in treatment or not at all, and is consistent with other clinical trials for cocaine dependence in which a positive response to treatment is typically occurs within the first few weeks of the intervention (Kampman et al., 2002; Plebani et al., in press).
The rapid response to treatment has several potential explanations. Some patients may have started making changes on their own prior to starting the research trial. While the mean self-reported days of cocaine use in the past month at treatment entry was 11 days and 63% of the sample provided a positive cocaine sample at baseline, some patients may have started a period of abstinence prior to enrolling in the trial and used the intervention to help maintain their abstinence. Thus, the rapid response may represent continuation of a change already made. Due to this concern, we re-ran the regression analyses excluding participants who reported no cocaine use in the past 30 days (n = 19). Results were consistent with the models presented in Table 2 and 3 (data not shown).
Another not mutually exclusive explanation for the rapid response to treatment is that the frequent monitoring had an effect. A small proportion of individuals in the standard treatment condition were able to initiate and/or maintain abstinence with the frequent monitoring that occurred in the context of the study. Consistent with the broader substance use disorders treatment literature, we also found a beneficial effect of the CM intervention; the CM participants were 2.5 times more likely to initiate abstinence than those receiving standard care. Furthermore, the CM intervention appears to expand this critical timeframe by a week or two for individuals to initiate abstinence.
A potential practical implication of these results with respect to CM implementation in methadone clinics is that methadone patients who do not respond fairly quickly to the CM procedures should not continue to be offered the same CM intervention, as most responders are early responders. Based on the results from this study, four weeks may be an appropriate timeframe to monitor initial patient response to CM interventions. Patients demonstrating good treatment response can continue on with the intervention. If a patient is unable to initiate abstinence within this timeframe, consideration of alternative treatment options is suggested.
Possible alternatives include the alteration of CM procedures. Previous studies of patients who failed to achieve abstinence during CM treatment have found increasing the magnitude of rewards improves abstinence rates (Silverman, Chutuape, Bigelow, & Stitzer, 1999); however, practical considerations prevent the widespread adoption of this procedure as patients may continue to use cocaine until offered the higher magnitude of rewards. Other alternatives within a CM framework include shaping, in which the response requirement for incentives is assessed via quantitative urinalysis and slowly increased (e.g., Preston, Umbricht, Wong, & Epstein, 2001), or abstinence initiation bonuses (e.g., Katz et al., 2002). More recently, an adaptive stepped-care approach that combines CM with behavioral contingencies for counseling attendance has demonstrated efficacy as well (Brooner et al., 2007). Beyond CM, other treatment alternatives could be implemented and include intensive outpatient treatment, pharmacological treatment, or even inpatient treatment.
An alternative conceptualization of CM is to use the intervention as a relapse prevention strategy. In this study and numerous others (e.g., Sofuoglu, Gonzalez, Poling, & Kosten, 2003; Stitzer et al., 2007), CM treatment outcome is significantly associated with recency of drug use. Individuals who are abstinent or who evidence infrequent use prior to CM treatment have better outcomes than those who are using cocaine heavily and provide positive samples at study initiation (Stitzer et al., 2007; Poling, Kosten, & Sofuoglu, 2007). Therefore, in a potential practical application of CM, patients could become eligible for CM programs only after they have demonstrated some reductions in cocaine usage or even brief abstinence.
Our results of the proximal onset for cocaine abstinence are in contrast to Silverman et al. (2004). In that study a portion of cocaine abusing methadone maintenance patients were randomized to a year long voucher CM intervention. A few patients, 4 of 26, continued to use cocaine and only after extended exposure (i.e., 2–3 months) to the CM procedures did they initiate long periods of sustained cocaine abstinence. However, the CM procedures in that study differed from the CM procedures use in this study (e.g., higher magnitude of rewards, contingencies for take home doses).
In this study, patients were on stable methadone doses for at least one month prior to starting the trial. The best timing for initiating a CM intervention in a methadone maintenance setting remains unaddressed. Further, the generalizability of these findings beyond the specific CM interventions employed and methadone maintenance settings is unclear. Different courses of initiating abstinence occur in non-methadone settings as the majority of patients in such settings test negative for substances throughout treatment (Petry, Alessi, Marx, Austin, & Tardif, 2005; Petry et al., 2005; Petry, Tedford, Austin, Nich, Carroll, & Rounsaville, 2004). Psychiatric comorbidity may also influence initiation of cocaine abstinence as individuals with greater psychiatric severity tend to do poorly in substance use disorders treatment; however CM interventions show promise for retaining these individuals in treatment (Weinstock, Alessi, & Petry, 2007).
Strengths of this study include the large sample size, objective measure of recent cocaine use, and the use of a community-based methadone clinic as the setting for the trials. While the differing CM procedures used across the three clinical trials could be perceived as a limitation of this study, they could also be considered a strength as they increase generalizability. As CM gets transported into community settings that serve diverse populations (Henggeler et al., 2008), it is likely to be implemented in different ways. The fact that these effects emerged from a multi-study dataset suggests they are robust overall. Nevertheless, effects were noted with respect to the onset of abstinence, despite similar inclusion and exclusion criteria across the three clinical trials. Participants in the Petry et al. (2007) study were more likely to become abstinent during the intervention than participants in the other trials. That study offered a greater magnitude of rewards than the other clinical trials and cocaine abstinence was the only behavior reinforced. Combined, these two factors most likely account for the observed differences. The Petry and Martin (2002) trial, in contrast, targeted two drugs of abuse (i.e., heroin and cocaine), and CM interventions for polydrug use are noted to have smaller effect sizes than those that target a single behavior (Lussier et al., 2006; Prendergast et al., 2006). Also, Petry et al. (2005) reinforced two target behaviors, cocaine abstinence and group therapy attendance, albeit independently from each other. Together, these factors may account for the differences found between the studies.
In summary, this study investigated the period during which abstinence is initiated in methadone maintenance patients with cocaine abuse or dependence who were beginning a CM treatment study. Baseline drug use severity was related to the initiation of abstinence in that individuals with more recent and heavy use were less likely to initiate abstinence. Results also suggest timeframes for decision making in the event that a patient does not respond. If patients were to become abstinent during the intervention period, they most often ceased using during the first one to four weeks of treatment. While CM patients achieved greater rates of abstinence than non-CM patients, few patients in either intervention condition initiated any period of sustained abstinence after the first few weeks of initiating treatment. Thus, continued application of CM beyond this time period is unlikely to benefit many patients, and alternate treatments may be warranted for this subpopulation.
ACKNOWLEDGEMENTS
This research and preparation of this report was funded by National Institutes of Health Grants P30-DA023918, R01-DA13444, R01-DA18883, RO1-DA016855, RO1-DA14618, R01-DA022739, R01-DA024667, P50-DA09241, P50-AA03510, T32-AA07290, and General Clinical Research Center Grant M01-RR06192.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/adb
References
- Brooner RK, Kidorf MS, King VL, Stoller KB, Neufeld K. Comparing adaptive stepped care and monetary-based voucher interventions for opioid dependence. Drug and Alcohol Dependence. 2007;88S:S14–S23. doi: 10.1016/j.drugalcdep.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Silverman K, Chutuape M, Bigelow G, Stitzer M. Voucher-based reinforcement of opiate plus cocaine abstinence in treatment-resistant methadone patients: Effects of reinforce magnitude. Experimental and Clinical Psychopharmacology. 2001;9:317–325. doi: 10.1037//1064-1297.9.3.317. [DOI] [PubMed] [Google Scholar]
- DeMaria PA, Sterling R, Weinstein SP. The effect of stimulant and sedative use on treatment outcome of patients admitted to methadone maintenance treatment. American Journal on Addictions. 2000;9:145–153. doi: 10.1080/10550490050173217. [DOI] [PubMed] [Google Scholar]
- Downey KK, Helmus TC, Schuster CR. Treatment of heroin-dependent polydrug abusers with contingency management and buprenorphine maintenance. Experimental and Clinical Psychopharmacology. 2000;8:176–184. doi: 10.1037//1064-1297.8.2.176. [DOI] [PubMed] [Google Scholar]
- Dunteman GH, Condelli WS, Fairbank JA. Predicting cocaine use among methadone patients: Analysis of findings from a national study. Hospital & Community Psychiatry. 1992;43:608–611. doi: 10.1176/ps.43.6.608. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Griffith JD, Rowan-Szal GA, Roark RR, Simpson DD. Contingency management in outpatient methadone treatment: A meta-analysis. Drug and Alcohol Dependence. 2000;58:55–66. doi: 10.1016/s0376-8716(99)00068-x. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Halliday-Boykins CA, Randall J, Shackelford J, et al. Statewide adoption and initial implementation of contingency management for substance-abusing adolescents. Journal of Consulting and Clinical Psychology. 2008;76:556–567. doi: 10.1037/0022-006X.76.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampman KM, Volpicelli JR, Mulvaney F, Rukstalis M, Alterman AI, Pettinati H, et al. Cocaine withdrawal severity and urine toxicology results from treatment entry predict outcome in medication trials for cocaine dependence. Addictive Behaviors. 2002;27:251–260. doi: 10.1016/s0306-4603(01)00171-x. [DOI] [PubMed] [Google Scholar]
- Katz EC, Robles-Sotelo E, Correira CJ, Silverman K, Stitzer ML, Bigelow G. The brief abstinence test: Effects of continued incentive availability on cocaine abstinence. Journal of Consulting and Clinical Psychology. 2002;69:643–654. doi: 10.1037//1064-1297.10.1.10. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Kadden RM, Babor TF, Tennen H, Rounsaville BJ. Validity of the SCID in substance abuse patients. Addiction. 1996;91:859–868. [PubMed] [Google Scholar]
- Kidorf M, Stitzer ML, Brooner RM. Characteristics of methadone patients responding to take-home incentives. Behavior Therapy. 1994;25:109–121. [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Morral AR, Belding MA, Iguchi MY. Identifying methadone maintenance clients at risk for poor treatment response: Pretreatment and early progress indicators. Drug and Alcohol Dependence. 1999;55:25–33. doi: 10.1016/s0376-8716(98)00176-8. [DOI] [PubMed] [Google Scholar]
- Olmstead TA, Sindelar JL, Petry NM. Clinic variation in the cost-effectiveness of contingency management. American Journal on Addiction. 2007;16:457–460. doi: 10.1080/10550490701643062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce JM, Petry NM, Stitzer ML, Blaine J, Kolodner K, Li R, et al. Lower-cost incentives increase stimulant abstinence in methadone maintenance community treatment: Results of the National Drug Abuse Treatment Clinical Trials Network Multi-Site Study. Archives of General Psychiatry. 2006;63:201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Hanson T, Sierra S. Randomized trial of contingent prizes versus vouchers in cocaine-using methadone patients. Journal of Consulting and Clinical Psychology. 2007;75:983–991. doi: 10.1037/0022-006X.75.6.983. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardif M. Vouchers versus prizes: Contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B. Low-cost contingency management for treating cocaine- and opioid-abusing methadone patients. Journal of Consulting and Clinical Psychology. 2002;70:398–405. doi: 10.1037//0022-006x.70.2.398. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Simcic F. Prize reinforcement contingency management for cocaine dependence: Integration with group therapy in a methadone clinic. Journal of Consulting and Clinical Psychology. 2005;73:354–359. doi: 10.1037/0022-006X.73.2.354. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, et al. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs. Archives of General Psychiatry. 2005;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treatment of cocaine abusers: How low can we go, and with whom? Addiction. 2004;99:349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piotrowski NA, Tusel DJ, Sees KL, Reilly PM, Banys P, Meek P, et al. Contingency contracting with monetary reinforcers for abstinence from multiple drugs in a methadone program. Experimental and Clinical Psychopharmacology. 1999;7:399–411. doi: 10.1037//1064-1297.7.4.399. [DOI] [PubMed] [Google Scholar]
- Plebani JG, Kampman KM, Lynch KG. Early abstinence in cocaine pharmacotherapy trials predicts successful treatment outcomes. Journal of Substance Abuse Treatment. doi: 10.1016/j.jsat.2009.02.001. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poling J, Kosten TR, Sofuoglu M. Treatment outcome predictors for cocaine dependence. American Journal of Drug and Alcohol Abuse. 2007;33:191–206. doi: 10.1080/00952990701199416. [DOI] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Preston KL, Silverman K, Higgins ST, Brooner RK, Montoay I, Schuster CR, Cone EJ. Cocaine use early in treatment predicts outcome in a behavioral treatment program. Journal of Consulting and Clinical Psychology. 1998;66:691–696. doi: 10.1037//0022-006x.66.4.691. [DOI] [PubMed] [Google Scholar]
- Preston KL, Umbricht A, Wong CJ, Epstein DH. Shaping cocaine abstinence by successive approximation. Journal of Consulting and Clinical Psychology. 2001;69:643–654. doi: 10.1037//0022-006x.69.4.643. [DOI] [PubMed] [Google Scholar]
- Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcement magnitude. Psychopharmacology. 1999;146:128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone maintenance patients who inject drugs. Journal of Consulting and Clinical Psychology. 2004;72:839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Sofuoglu M, Gonzalez G, Poling J, Kosten TR. Prediction of treatment outcome by baseline urine cocaine results and self-reported cocaine use for cocaine and opioid dependence. American Journal of Drug and Alcohol Abuse. 2003;29:713–727. doi: 10.1081/ada-120026256. [DOI] [PubMed] [Google Scholar]
- Stitzer M, Petry N. Contingency management for treatment of substance abuse. Annual Review of Clinical Psychology. 2006;2:411–434. doi: 10.1146/annurev.clinpsy.2.022305.095219. [DOI] [PubMed] [Google Scholar]
- Stitzer M, Petry N, Peirce J, Kirby K, Killeen T, Roll J, et al. Effectiveness of abstinence-based incentives: Interaction with intake stimulant test results. Journal of Consulting and Clinical Psychology. 2007;75:805–811. doi: 10.1037/0022-006X.75.5.805. [DOI] [PubMed] [Google Scholar]
- Strain EC, Stitzer ML, Liebson IA, Bigelow GE. Buprenorphine versus methadone in the treatment of opioid dependence: Self-reports, urinalysis, and addiction severity index. Journal of Clinical Psychopharmacology. 1996;16:58–67. doi: 10.1097/00004714-199602000-00010. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Alessi SM, Petry NM. Regardless of psychiatric severity the addition of contingency management to standard treatment improves retention and drug use outcomes. Drug and Alcohol Dependence. 2007;87:288–296. doi: 10.1016/j.drugalcdep.2006.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett JB, Singer JD. Investigating onset, cessation, relapse, and recovery: Why you should, and how you can, use discrete-time survival analysis to examine event occurrence. Journal of Consulting and Clinical Psychology. 1993;61:952–965. doi: 10.1037//0022-006x.61.6.952. [DOI] [PubMed] [Google Scholar]
- Williams JW, Gibbon M, First MB, Spitzer RL, Davies M, Bors J, et al. The structured clinical interview for DSM-III-R (SCID) II: Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]