Abstract
Objective
To determine whether a telephone counseling program can improve psychosocial outcomes among breast cancer patients post-treatment.
Methods
A randomized trial was conducted involving 21 hospitals and medical centers, with assessments (self-administered questionnaires) at baseline, 12 and 18 months post-enrollment. Eligibility criteria included early stage diagnosis, enrollment during last treatment visit, and the ability to receive the intervention in English. Endpoints included distress (Impact of Event Scale), depression (Center for Epidemiologic Studies Depression Scale) and two study-specific measures: sexual dysfunction and personal growth. The control group (n = 152) received a resource directory for breast cancer; the intervention group (n = 152) also received a one year, 16 session telephone counseling program augmented with additional print materials.
Results
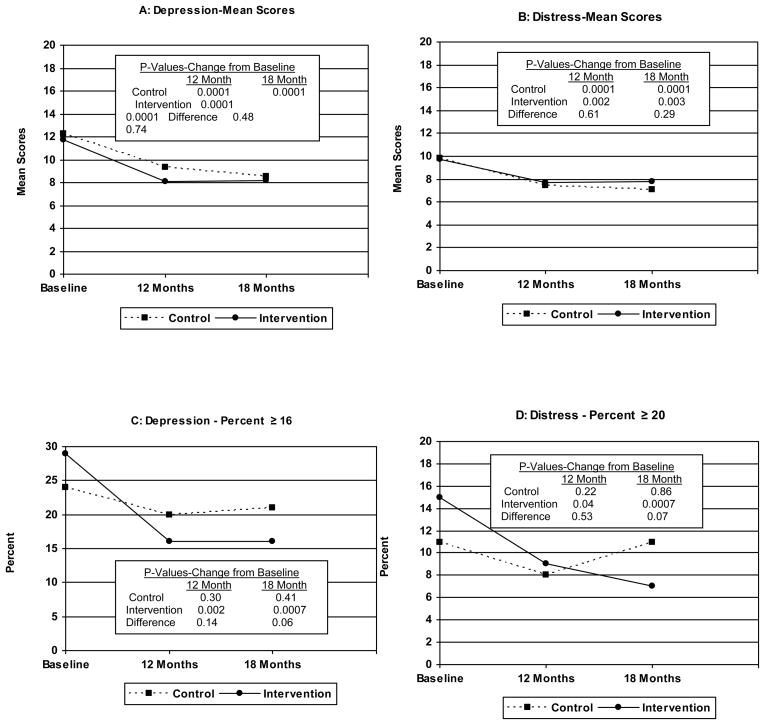
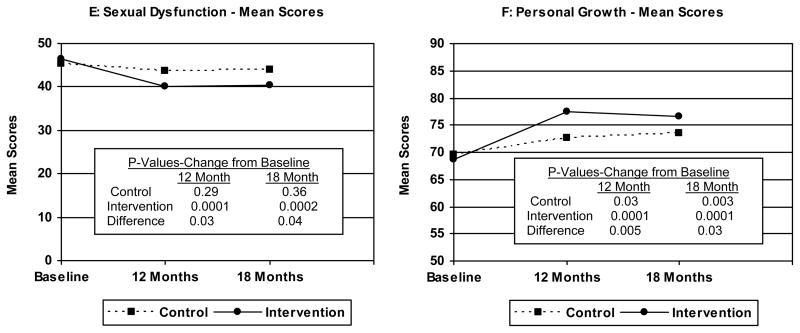
Significant intervention effects were found for sexual dysfunction at 12 (p = 0.03) and 18 months (p = 0.04) and personal growth (12 months: p = 0.005; 18 months: p = 0.03). No differences by group were found in mean scores for distress and depression, with both groups showing significant improvement at 12 and 18 months (all p values for within-group change from baseline were ≤ .003). However, when dichotomized at cutpoints suggestive of the need for a clinical referral, the control group showed virtually no change at 18 months while the intervention group showed about a 50% reduction for both distress (p = 0.07) and depression (p = 0.06).
Conclusions
Telephone counseling may provide a viable method for extending psychosocial services to cancer survivors nationwide.
Keywords: psychosocial oncology, psychosocial telephone counseling, breast cancer survivors
INTRODUCTION
It is now well established that psychosocial interventions can improve the quality of life (QOL) of cancer patients, especially during active treatment [1–8]. While many early stage patients adjust quite well to cancer post-treatment, significant psychosocial problems can also occur during this period, including feelings and concerns related to uncertainty, isolation and vulnerability, as well as overt manifestations of distress, depression and sexual dysfunction [9–23]. Despite these significant psychosocial sequelae, and in sharp contrast to the robust body of intervention research that has targeted cancer patients during treatment, there has been much less research focusing on cancer patients at this re-entry transition post-treatment [9,10].
This study examined whether a telephone counseling program, as a more convenient and exportable alternative to traditional in-person counseling programs, can improve psychosocial outcomes among early stage breast cancer patients. Previous research testing telephone counseling interventions in psychosocial oncology have produced both positive [24–27] and negative [28–36] results involving such endpoints as distress, depression, sexual dysfunction, and global or disease-specific QOL. Consistent with previous research involving in-person counseling programs, most of the studies targeting breast cancer patients have tested telephone counseling interventions during active treatment [32–36]. Other commonalities across these studies include interventions that were delivered to breast cancer patients over a 4-week to 6-month period, with the number of counseling sessions ranging from 4 to 10 [26,27,31–36], and the use of nurses [26,27,31,34,35], graduate students in psychology [32] or peer counselors [36] to deliver the counseling intervention by telephone. By way of contrast, this study tested a telephone counseling program that targeted breast cancer survivors post-treatment, included 16 sessions delivered over 12 months, and used professional telephone counselors in psychosocial oncology. Also included as an endpoint in this trial was “personal growth” or benefit-finding from the cancer experience [37–43], which has not, to the best of our knowledge, been examined previously in telephone counseling intervention research.
METHODS
Research and Intervention Design
All research procedures and materials were approved by the Institutional Review Board (IRB) of the AMC Cancer Research Center, Denver, Colorado. In addition, secondary IRB approval was obtained from all participating sites.
Patients were considered eligible for this study if: a) they were female and diagnosed with stage I, II or IIIA (< 10 positive lymph nodes) breast cancer, b) they had just completed definitive treatment for their breast cancer, c) there was no overt evidence of psychosis, dementia or suicidal behavior, d) the patient was not enrolled in another QOL study, e) the patient’s treatment plan did not include bone marrow transplantation, f) the patient could complete the assessments and receive the intervention in English, and g) the patient signed a written informed consent statement. Using these eligibility criteria, on-site study coordinators identified 354 eligible breast cancer patients who were approached for study enrollment during their last treatment visit. Of these, 304 (86%) agreed to participate and were subsequently enrolled.
The telephone counseling program was evaluated using a randomized two-group design. Twenty-one hospitals and medical centers nationwide participated as accrual sites. Baseline assessments occurred at the time of study enrollment by self-administered questionnaire. On-site staff also completed a medical information form at baseline that required abstracting data from the medical charts of enrolled patients. Follow-up assessments occurred by mail at 3, 6, 12 and 18 months post-enrollment. At baseline, participants assigned to the minimal intervention control condition (n = 152) were mailed a booklet listing psychosocial and other social service and rehabilitation resources in their community for breast cancer. These site-specific resource directories were prepared in collaboration with staff at each participating accrual site. In addition to the above, the intervention group (n = 152) also received a 16 session telephone counseling program that was prescheduled with clients over a 12 month period. Participants were notified of group assignment (based on sequential randomization within institutions) by mail concurrent with the mailing of the print materials specific to each experimental condition. The response rates at each follow-up, which did not differ by experimental condition, were as follows: 3 months = 93% (n = 282); 6 months = 88% (n = 266); 12 months = 86% (n = 261); 18 months = 80% (n = 243).
Overview of the Telephone Counseling Program
The telephone counseling program, which also included additional print materials, was delivered by four Masters-level psychosocial oncology counselors affiliated with the Cancer Information and Counseling Line (CICL) [44]. The 16 counseling sessions lasted on average about 45 minutes each. The first nine sessions were scheduled at approximately two-week intervals, while calls 10–16 were scheduled at approximately one-month intervals. During call 1, participants were introduced to the counseling program, and an overview was provided of the counseling materials and themes. During call 2, participants were invited to prioritize for delivery six thematic modules (booklets) that were mailed in advance of the call and presented in the form of a “Wellness Kit”. These modules included: a) Living with Uncertainty, b) Living with Physical Change, c) Living with Self-Change, d) Sexuality After Breast Cancer, e) Living in Relationships, and f) Living with Economic Change. Also included in the Wellness Kit were two progressive relaxation tapes and a Moving Through Breast Cancer Stress Management Guide.
The six thematic modules were used to structure and augment the psychoeducational counseling component of the intervention (calls 4–9). They were designed to enhance adaptation at re-entry by normalizing feelings of uncertainty and preparing breast cancer survivors for unanticipated disruptions across key QOL domains (physical, emotional, social, sexual and economic). The Stress Management Guide was reviewed during the third call. This guide introduced participants to an active coping process, drawing upon the Transactional Model of Stress and Coping as the underlying theoretical framework for the intervention [45,46]. Three cognition-focused worksheets were also provided: a) Cognitive Awareness/Self-monitoring Worksheet, which helped participants to understand the direct relationship between thoughts and feelings; b) Challenge Your Thoughts Worksheet, which encouraged participants to challenge automatic negative thoughts to determine if they were accurate and/or productive; and c) Automatic Thought Log, which allowed participants to monitor on a daily basis the relationship between thoughts and feelings, and to practice alternative thoughtful responses to replace automatic reactions to problems or stressful situations. In addition, two emotion-focused worksheets were included: a) Feelings Awareness Worksheet, which helped participants recognize and accurately name what they were feeling; and b) Feelings Reconciliation Worksheet, which encouraged participants to accept and/or actively cope with difficult emotions through such avenues as self-reflection, self-nurturance, journaling and seeking support.
During call 10, participants received a summary of their progress in working with issues that emerged during the previous telephone counseling sessions, and a list of orienting questions to generate thoughts and/or create a personal expression about the meaning of their cancer experience. During calls 11–15, the monthly sessions addressed persistent or emergent survivorship issues and reinforced the use of active coping strategies. Finally, to bring closure to the counseling program in call 16, participants were asked to summarize what they had learned from the program and about themselves, how they would apply this new knowledge to cope with future breast cancer-related and other stressors, and to share with the counselor their personal expressions.
Counselor Training, Supervision and Quality Control
Counselor training occurred over a two week period and included assigned reading, group discussion, lecture, skills demonstration and role play exercises. This training program was supplemental to a comprehensive 16 session training program that all counselors complete as part of standard CICL training. All intervention counseling sessions were tape-recorded. A random sample of 20% of these tapes were selected for internal quality control review and clinical supervision by the clinical team. An additional 10% of these tapes were also selected for external review by two consultants. All tapes reviewed for quality assurance were coded using standardized forms for intervention fidelity, with counselor feedback provided on a weekly basis by the clinical supervisor.
Assessments for Outcome Evaluation
Cancer-Specific Distress
Cancer-specific distress was assessed using the intrusion subscale of the Impact of Event Scale (IES). The IES is designed to assess current subjective distress for any specific life event [47,48]. The seven item intrusion subscale assesses the frequency of intrusive or distracting thoughts as a marker of distress, with scores ranging from 0–35. In this study, the adverse life event was breast cancer. The intrusion subscale was examined both as a continuous measure using mean scores, and as a dichotomous measure using a score of > 20 as suggestive of the need for clinical referral [47,49,50].
Depression
Depression was assessed using the Center for Epidemiologic Studies Depression Scale (CES-D) [51]. The CES-D is comprised of 20 items. Originally developed to measure depression in the general population, the CES-D has subsequently been validated among breast cancer patients [52]. Scores can range from 0–60, with higher scores indicating more symptoms. The CES-D was also examined both as a continuous measure using mean scores and as a dichotomous measure using a score of ≥16 as suggestive of the need for a clinical referral [51]. Although some have argued for using a more stringent cutpoint to reduce false positives [53–56], others have recommended more psychometric research in this context [55]. In these analyses, the more traditional cutpoint of ≥ 16 was used under the assumption that the greater risk would be to miss individuals (false negatives) who could still benefit from intervention. Another cautionary note for cancer patient populations is that the CES-D may be confounded by cancer stage and diagnosis and somatic items such as those related to cognitive functioning and fatigue [55,56]. However, this counseling intervention was not designed exclusively to address depression, but rather to improve adaptation across multiple life domains consistent with a more general stress and coping theoretical framework and counseling program.
Sexual Dysfunction
The Sexual Dysfunction scale consisted of 25 questions, several of which were developed specifically for this project. Factor analyses (principal components) of this item pool suggested three factors. The Behavioral Scale, which was comprised of 9 items and had a Cronbach α of 0.77, assessed various behavioral aspects of sexuality, including reports of vaginal dryness, pain with intercourse, and frequency of sexually intimate behaviors. The Evaluative Scale, which was comprised of 7 items and had a Cronbach α of 0.85, assessed the patient’s perceptions of sexual interest, arousal, and satisfaction. Finally, 9 items were combined to form the Body Image Scale (e.g., global sense of attractiveness, impact of weight change, impact of hair loss), with a Cronbach α of 0.80. As indicated elsewhere [57], these subscales were subsequently combined to form a summary or global index of sexual dysfunction, where scores can range from 0–100 with higher scores indicating greater sexual dysfunction.
Personal Growth
To assess whether the intervention had an impact on personal growth from the cancer experience, a composite measure was developed consisting of the following items: 1) where life is today compared to life before breast cancer (10 point scale, where −5 = totally different and worse, 0 = the same, +5 = totally different and better), 2) change in appreciation of life because of breast cancer (same metric as above), 3) able to use the breast cancer experience to help grow as an individual (4 point scale, where 1 = definitely true to 4 = definitely false), 4) stronger person because of the breast cancer experience (same 4 point scale as above), and 5) there have been positive life changes as a result of breast cancer (also 4 point scale, same as above). Exploratory factor analysis (principal components) revealed one underlying factor, with a Cronbach α of 0.76. A scoring algorithm was developed to allow each item to contribute equally to a summative scale, where scores could range from 0–100, with higher scores reflecting more positive growth from the breast cancer experience.
Statistical Analyses
To assess the initial equivalency of the two experimental conditions by sociodemographic, disease and treatment-related characteristics, chi-square or Fisher’s Exact tests were used for dichotomous variables, while the Cochran-Mantel-Haenszel chi-square test was used for ordered categorical variables. Repeated measures models for incomplete data were used to test for differences in outcome at 3, 6, 12 and 18 months post-enrollment [58]. The results reported herein include both the 12 and 18 month outcome data, corresponding to the end of the intervention and 6 months post-intervention, respectively. Effect sizes were estimated for all endpoints showing significant or borderline significant differences at 18 months follow-up [59].
RESULTS
Sample Characteristics
The breast cancer patients enrolled in this trial were well educated and most were non-Hispanic white. About half the sample was 50 years of age or less. There were no differences by experimental condition on any of the sociodemographic variables shown in Table 1. Similarly, there were no differences on any of the health status or breast cancer diagnostic or treatment variables obtained at baseline (see Table 2).
TABLE 1.
Sociodemographic Characteristics of Sample at Baseline
| Total (N=304) | Intervention (N = 152) | Control (N = 152) | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P Value | |
| Age | |||||||
| < 40 | 40 | 13.2 | 17 | 11.2 | 23 | 15.1 | |
| 41–50 | 110 | 36.2 | 53 | 34.9 | 57 | 37.5 | |
| 51–60 | 86 | 28.3 | 45 | 29.6 | 41 | 27.0 | |
| 61–70 | 40 | 13.2 | 22 | 14.5 | 18 | 11.8 | |
| 70+ | 28 | 9.2 | 15 | 9.9 | 13 | 8.6 | 0.78 |
| Education | |||||||
| High School | 89 | 29.3 | 47 | 30.9 | 42 | 27.6 | |
| Some College | 72 | 23.7 | 34 | 22.4 | 38 | 25.0 | |
| College Graduate | 65 | 21.4 | 30 | 19.7 | 35 | 23.0 | |
| Post College | 77 | 25.3 | 40 | 26.3 | 37 | 24.3 | |
| Missing | 1 | 0.3 | 1 | 0.7 | 0 | 0.0 | 0.73 |
| Race/Ethnicity | |||||||
| White (Non-Hispanic) | 275 | 90.5 | 141 | 92.8 | 134 | 88.2 | |
| African American | 19 | 6.3 | 5 | 3.3 | 14 | 9.2 | |
| Other | 8 | 2.6 | 5 | 3.3 | 3 | 2.0 | |
| Missing | 2 | 0.7 | 1 | 0.7 | 1 | 0.7 | 0.12 |
| Marital Status | |||||||
| Single | 25 | 8.2 | 12 | 7.9 | 13 | 8.6 | |
| Married/Living as married | 219 | 72.0 | 110 | 72.4 | 109 | 71.7 | |
| Separated | 8 | 2.6 | 6 | 3.9 | 2 | 1.3 | |
| Divorced Widowed | 32 | 10.5 | 14 | 9.2 | 18 | 11.8 | |
| Widowed | 20 | 6.6 | 10 | 6.6 | 10 | 6.6 | 0.64 |
| Currently Employed | |||||||
| No | 111 | 36.5 | 58 | 38.2 | 53 | 34.9 | |
| Part-time | 45 | 14.8 | 22 | 14.5 | 23 | 15.1 | |
| Full-time | 141 | 46.4 | 70 | 46.1 | 71 | 46.7 | |
| Missing | 7 | 2.3 | 2 | 1.3 | 5 | 3.3 | 0.71 |
TABLE 2.
Disease and Treatment Characteristics of Sample at Baseline
| Total (N=304) | Intervention (N = 152) | Control (N = 152) | |||||
|---|---|---|---|---|---|---|---|
| Sample Characteristics | N | % | N | % | N | % | P Value |
| Disease Stage | |||||||
| I | 106 | 34.9 | 52 | 34.2 | 54 | 35.5 | |
| II | 174 | 57.2 | 87 | 57.2 | 87 | 57.2 | |
| III | 11 | 3.6 | 6 | 3.9 | 5 | 3.3 | |
| Missing | 13 | 4.3 | 7 | 4.6 | 6 | 3.9 | 0.99 |
| Tumor Size | |||||||
| T1/T1B | 160 | 52.6 | 78 | 51.3 | 82 | 54.0 | |
| T2 | 124 | 40.8 | 63 | 41.4 | 61 | 40.1 | |
| T3 | 14 | 4.6 | 7 | 4.6 | 7 | 4.6 | |
| T4 | 1 | 0.3 | 1 | 0.7 | 0 | 0.0 | |
| Missing | 5 | 1.6 | 3 | 2.0 | 2 | 1.3 | 0.81 |
| Lymph Node Status | |||||||
| Positive | 123 | 40.5 | 61 | 40.1 | 62 | 40.8 | |
| Negative | 176 | 57.9 | 88 | 57.9 | 88 | 57.9 | |
| Missing | 5 | 1.6 | 3 | 2.0 | 2 | 1.3 | 1.00 |
| Chemotherapy | |||||||
| Yes | 226 | 74.3 | 109 | 71.7 | 117 | 77.0 | |
| No | 73 | 24.0 | 40 | 26.3 | 33 | 21.7 | |
| Missing | 5 | 1.6 | 3 | 2.0 | 2 | 1.3 | 0.56 |
| Radiation Therapy | |||||||
| Yes | 201 | 66.1 | 96 | 63.2 | 105 | 69.1 | |
| No | 103 | 33.9 | 56 | 36.8 | 47 | 30.9 | 0.28 |
| Surgery | |||||||
| Mastectomy | 127 | 41.8 | 69 | 45.4 | 58 | 38.2 | |
| Lumpectomy | 172 | 56.6 | 80 | 52.6 | 92 | 60.5 | |
| Missing | 5 | 1.6 | 3 | 2.0 | 2 | 1.3 | 0.49 |
| Tamoxifen | |||||||
| Yes | 158 | 52.0 | 82 | 53.9 | 76 | 50.0 | |
| No | 141 | 46.4 | 68 | 44.7 | 73 | 48.0 | |
| Missing | 5 | 1.6 | 2 | 1.3 | 3 | 2.0 | 0.74 |
| Length of Treatment | |||||||
| ≤ 3 months | 142 | 46.7 | 74 | 48.7 | 68 | 44.7 | |
| > 3 months | 152 | 50.0 | 74 | 48.7 | 78 | 51.3 | |
| Missing | 10 | 3.3 | 4 | 2.6 | 6 | 3.9 | 0.68 |
| Reconstruction | |||||||
| Yes | 63 | 20.7 | 32 | 21.0 | 31 | 20.4 | |
| No | 223 | 73.4 | 112 | 73.7 | 111 | 73.0 | |
| Missing | 18 | 5.9 | 8 | 5.3 | 10 | 6.6 | 0.91 |
| Chronic (non-cancer) Health Problems | |||||||
| No | 194 | 63.8 | 97 | 63.8 | 97 | 63.8 | |
| Yes | 104 | 34.2 | 54 | 35.5 | 50 | 32.9 | |
| Missing | 6 | 2.0 | 1 | 0.7 | 5 | 3.3 | 0.28 |
Implementation and Process Evaluation
Seventy-five percent (n = 114) of intervention participants received all 16 counseling sessions, with 22% (n = 34) declining to complete the program. Most of the drop-outs occurred during or immediately following session one (44%), or after sessions two or three (36%). When participants dropped from the counseling program, they were encouraged to complete the follow-up questionnaires, and 71% (n = 24) complied. These data were included in all analyses.
All of the thematic modules were read extensively as reported by intervention participants at 12 months post-enrollment. The percentage reading all or most of each module ranged from 96% for Living in Relationships to 89% for Living with Economic Change, with the single exception being the Resource Directory at 72%. Most were perceived as very or somewhat helpful by 80% or more of the intervention group, with both the Resource Directory (75%) and the Living with Economic Change module (71%) receiving somewhat lower ratings. Similar ratings were also obtained for the different coping strategies that were highlighted in both the Stress Management Guide and thematic modules, including problem-focused (80%), cognitive-focused (80%) and emotion-focused coping strategies (77%), as well as the list of cognitive distortions (77%). In addition, all of the specific worksheets included in the modules and the relaxation tape were rated as very or somewhat helpful by at least 70% of the intervention group. However, journal writing, which was not emphasized in this counseling program, received substantially lower ratings (34%).
Using a checklist at 12 months post-enrollment that allowed for multiple answers (see Table 3), a majority of the intervention group rated as “most helpful” the support provided through telephone counseling (e.g., having a counselor who understands, talking about my experience with someone who cares), as well as selected aspects of the print materials (especially reading survivorship stories). However, in terms of perceived utility by mode of contact, intervention participants clearly favored the telephone when compared to receiving print materials in the mail (42% vs. 18%).
TABLE 3.
Percentage of Intervention Participants at 12 Months Follow-Up Who Rated Selected Intervention Components as Most Helpful
| % Most Helpful (N = 129)1 | |
|---|---|
| Having a counselor who understands | 65.0 |
| Talking about my experience with someone who cares | 51.5 |
| Reading survivorship stories | 51.1 |
| Having a counselor who is responsive to my needs | 45.5 |
| Being contacted by telephone | 41.7 |
| Reading about survivorship issues | 40.8 |
| Expressing my feelings | 37.9 |
| Learning alternative ways to think about my situation | 35.9 |
| Talking about survivorship issues | 29.4 |
| Learning to manage stress | 24.3 |
| Receiving materials in the mail | 17.6 |
| Find out about resources | 7.8 |
Intervention participants were asked to check which of the above were “most helpful” to them, with multiple responses allowed for this question.
Outcome Analyses
None of the endpoints were significantly different by experimental group at baseline. Figure 1 reports change from baseline for the study endpoints by experimental condition. For both depression and distress (Figures 1A and 1B), mean scores for both groups showed a significant reduction over time, with no difference by experimental group in change from baseline. In contrast, when these scores were dichotomized (Figures 1C and 1D), a dramatically different pattern emerged. The control group showed no significant change from baseline to 18 months (depression: p = 0.41; distress: p = 0.86), while the intervention group showed significant improvement (depression: p = 0.0007; distress: p = 0.007), reflecting about a 50% reduction in the percentage scoring at or above the cutpoint suggestive of the need for a clinical referral. For both of these endpoints, group differences in change from baseline to 18 months approached statistical significance (depression: p = 0.06; distress: p = 0.07), with effect sizes of 0.23 and 0.24, respectively.
Figure 1.
Change from Baseline on Study Endpoints by Experimental Condition
For sexual dysfunction (Figure 1E), the control group showed no change from baseline to 18 months, while the intervention group showed significant improvement at both 12 and 18 months. Group differences in change from baseline were significant at both 12 (p = 0.03) and 18 months (p = 0.04) follow-up, with an effect size at 18 months of 0.23. Additional analyses involving the three subscales to this composite measure (i.e., the Behavioral, Evaluative and Body Image subscales for sexual dysfunction) failed to show any significant differences by experimental condition (data not shown), although non-significant trends in the expected direction were observed. Finally, for personal growth (Figure 1F), both groups showed significant improvement from baseline to 12 as well as 18 months follow-up, with greater improvement reported by the intervention group. Differences by experimental condition in change from baseline were also statistically significant at both 12 (p = 0.005) and 18 months (p = 0.03) follow-up, with an effect size at 18 months of 0.22.
Replication Costs
The replication costs for this program were estimated as follows: unit cost for production of the Wellness Kit = $45; unit cost per telephone counseling session = $50 x 16 counseling sessions = $800 per client (assumes annual salary of approximately $50,000 with an average of 45 minutes per counseling session, and a blending of local and long distance telephone charges), and finally, support for a clinical supervisor at approximately $100 per client at $50 per hour. These cost estimates yield a total cost per client of $945 or about $60 per session.
DISCUSSION
Beginning with informed consent, where the counseling program was described in detail, 86% of breast cancer patients approached for study enrollment agreed to participate. Following random assignment, 75% of the intervention group completed all 16 telephone counseling sessions. Although the intervention print materials received high positive ratings and were read or used extensively by participants, a much higher percentage rated as most helpful either the telephone counselor (65%) or being contacted by telephone (42%) when compared to receiving print material in the mail (18%). These positive findings regarding enrollment and retention rates and the perceived utility of this counseling program have been reported previously in other telephone counseling studies in psychosocial oncology [24,26,29,32,34,60–62]. Given the level of service provided, such programs would also appear to have relatively modest replication costs, as exemplified by this intervention.
The results obtained from the outcome analysis were mixed, more encouraging for sexual dysfunction and personal growth, less so for distress and depression. For sexual dysfunction, significant intervention effects were obtained at both 12 and 18 months follow-up. Of special note is that the control group showed virtually no change from baseline, suggesting that this source of psychosocial morbidity may be especially resistant to improvement in the absence of intervention, and thus should remain a high priority for psychosocial research [12,13,19,23,63,64]. Similarly, the findings from this study suggest that the capacity of early stage breast cancer patients to extract positive meaning from their cancer experience may likewise benefit from intervention, even when such patients, as in the case of the control group, report enhanced benefit-finding as a secular (non-intervention) trend post-treatment. Only a few previous intervention studies have examined post-traumatic growth among breast cancer survivors [41–43]. Although this intervention was grounded in a stress and coping theoretical model, it did include a “meaning-focused” copying strategy that allowed participants to explore the impact (both positive and negative) of breast cancer on their lives. Accordingly, as suggested by Stanton et al [65], it would appear that cognitive-behavioral intentions also have the potential to enhance personal growth among cancer survivors.
As noted above, the findings for distress and depression were less favorable. However, this observation should be tempered by the fact that the dichotomized versions of distress and depression had corresponding p values for intervention efficacy at 18 months (p = 0.07 and 0.06, respectively) that were only moderately different compared to sexual dysfunction (p = 0.04) and personal growth (p = 0.03), and all four of these endpoints had virtually identical effect sizes, ranging from 0.22 to 0.24. In addition, the results obtained for distress and depression may also be instructive in highlighting the need to target interventions for these endpoints based on significant psychosocial morbidity at baseline.
In this study, no such eligibility criteria were imposed, thus reflecting a key study limitation. As a case in point, if the baseline rates for clinically significant distress or depression had been as high as 50%, and the same proportional reduction by experimental condition was found as reported herein, the effect sizes would have increased substantially, from about 0.23 to 0.50, with the latter corresponding to a medium effect [59]. Moreover, while all of the effect sizes estimated in this study were modest, they are also consistent with the results obtained from several meta analyses of psychosocial interventions for adult cancer patients, where effect sizes of 0.19 to 0.36 have been reported [5, 7, 8]. The main point here, of course, is that these results were derived from studies that tested more traditional in-person psychosocial counseling programs, indicating that the telephone may provide comparable intervention efficacy in psychosocial oncology. Also noteworthy is that while these effect sizes are viewed as relatively modest from a statistical perspective, others have noted that effect sizes of this magnitude can still be clinically important [5, 66].
Finally, several limitations of this study include the following: the target population was restricted to breast cancer survivors; the design of this trial did not allow for separate assessments of intervention efficacy for telephone counseling vs. the intervention print materials; the intervention may be difficult to replicate as a service program because of its intensity and length; the follow-up period for outcome assessment was limited to six months post-intervention; and the sample was largely non-Hispanic white and highly educated, and psychosocial need at baseline was not included as a specific eligibility criterion for enrollment. Given the above, profitable directions for future research would include expanding the target population to other cancer sites, especially to allow for a gender comparison of intervention efficacy; assessing the comparative efficacy or value-added of telephone counseling to other intervention strategies, as well as the efficacy of telephone counseling interventions of different duration or intensity; extending the follow-up period longer-term; and determining whether more diverse cancer patient populations, including those who may have greater need for psychosocial intervention, will provide even stronger support for telephone counseling programs. As noted elsewhere, such research should remain a high priority [44,60], especially among cancer survivors post-treatment.
Acknowledgments
This study would not have been possible without the participation of those breast cancer patients who enrolled in this trial, agreed to be randomized, and graciously gave of their time to complete the baseline and follow-up questionnaires. Their contributions and perseverance are most gratefully acknowledged by the authors of this report. In addition, the authors are indebted to those hospitals and clinics that provided access to their patients, and especially to the on-site study coordinators who enrolled these patients into this study. These institutional partners are gratefully acknowledged as follows:
Columbia Mercy Medical Center, Canton, OH
Columbia Rose Medical Center, Denver, CO
Dean Medical Center, Madison, WI
Evanston Northwestern Healthcare, Evanston, IL
Fairfax Hospital, Falls Church, VA
Fox Chase Cancer Center, Philadelphia, PA
Frederick Memorial Hospital, Frederick, MD
Highland Park Hospital, Highland Park, IL
Indiana University Medical Center, Indianapolis, IN
Latrobe Area Hospital, Latrobe, PA
Lawrence Memorial Hospital, Medford, MA
Medical College of Wisconsin, Milwaukee, WI
Meriter Hospital, Madison, WI
Morristown Memorial Hospital, Morristown, NJ
New England Medical Center-Tufts University, Boston, MA
Rocky Mountain Cancer Center, Denver, CO
Rush Cancer Institute, Chicago, IL
St. Mary-Corwin Medical Center, Pueblo, CO
St. Mary’s Hospital, Rochester, NY
Suburban Hospital, Bethesda, MD
Waukesha Memorial Hospital, Waukesha, WI
Finally, the authors gratefully acknowledge the many useful recommendations made by the anonymous reviewers that significantly improved this manuscript.
The research reported herein was supported by grant CA-63009 from the National Cancer Institute (NCI). All interpretations and conclusions expressed herein are those of the authors and do not necessarily reflected those of the NCI.
Contributor Information
Alfred C. Marcus, Email: Al.marcus@ucdenver.edu, AMC Cancer Research Center of the University of Colorado Cancer Center, University of Colorado, Denver, 1600 Pierce Street, Denver, Colorado 80214, Phone: 303-239-3397, Fax: 303-233-1863.
Kathleen M. Garrett, AMC Cancer Research Center of the University of Colorado Cancer Center, University of Colorado, Denver.
David Cella, Northwestern University Feinberg School of Medicine.
Lari Wenzel, University of California, Irvine.
Marianne J. Brady, Iron Mountain, MI.
Diane Fairclough, University of Colorado, Denver, School of Public Health.
Meredith Pate-Willig, AMC Cancer Research Center of the University of Colorado Cancer Center, University of Colorado, Denver.
Denise Barnes, AMC Cancer Research Center of the University of Colorado Cancer Center, University of Colorado, Denver.
Susan Powell Emsbo, AMC Cancer Research Center of the University of Colorado Cancer Center, University of Colorado, Denver.
Brenda C. Kluhsman, Penn State College of Medicine, Hershey, PA.
Lori Crane, University of Colorado, Denver, School of Public Health.
Scot Sedlacek, Rocky Mountain Cancer Centers.
Patrick J. Flynn, Metro Minnesota Community Clinical Oncology Program.
References
- 1.Iacovino V, Reesor K. Literature on interventions to address cancer patients’ psychosocial needs: What does it tell us? J Psychosocial Oncology. 1997;15:47–71. [Google Scholar]
- 2.Andersen BL. Biobehavioral outcomes following psychological interventions for cancer patients. Journal of Consulting and Clinical Oncology. 2002;70:552–568. doi: 10.1037//0022-006X.70.3.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovejoy NC, Matteis M. Cognitive-behavioral interventions to manage depression in patients with cancer: research and theoretical initiatives. Cancer Nursing. 1997;20:155–167. doi: 10.1097/00002820-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Fawzy FI, Fawzy NW, Arndt LA, Pasnau RO. Critical review of psychosocial interventions in cancer care. Arch Gen Psychiatry. 1995;52:100–113. doi: 10.1001/archpsyc.1995.03950140018003. [DOI] [PubMed] [Google Scholar]
- 5.Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol. 1995;14:101–108. doi: 10.1037//0278-6133.14.2.101. [DOI] [PubMed] [Google Scholar]
- 6.Devine EC, Westlake SK. The effect of psychoeducational care provided to adults with cancer: Meta-analysis of 116 studies. Oncology Nursing Forum. 1995;22:1369–1381. [PubMed] [Google Scholar]
- 7.Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: Meta analysis of 37 published controlled outcome studies. Patient Edu Couns. 2003;50:179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- 8.Sheard T, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: results of two meta-analyses. Brit J Cancer. 1999;80:1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment after treatment for cancer. Cancer. 2005;104 (11 Suppl):2608–2613. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- 10.Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol. 2006;24:5132–5137. doi: 10.1200/JCO.2006.06.8775. [DOI] [PubMed] [Google Scholar]
- 11.Zabora JR, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: A follow-up study. J Natl Cancer Inst. 2002;94:39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 13.Ganz PA, Rowland JH, Desmond KA, Meyerowitz BE, Wyatt GE. Life after breast cancer: Understanding women’s health-related quality of life and sexual functioning. J Clin Oncol. 1998;16:501–514. doi: 10.1200/JCO.1998.16.2.501. [DOI] [PubMed] [Google Scholar]
- 14.Bleiker EM, Pouwer F, van der Ploeg HM, Leer JW, Adèr HJ. Psychological distress two years after diagnosis of breast cancer: frequency and prediction. Patient Edu Couns. 2000;40:209–217. doi: 10.1016/s0738-3991(99)00085-3. [DOI] [PubMed] [Google Scholar]
- 15.Helgeson VS, Snyder P, Siltman P. Psychological and physical adjustment to breast cancer over four years: Identifying distinct trajectories of change. Health Psychology. 2004;23:3–15. doi: 10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]
- 16.Golden-Kreutz DM, Andersen BL. Depressive symptoms after breast cancer surgery: Relationships with global, cancer-related, and life event stress. Psycho-Oncology. 2004;13:311–220. doi: 10.1002/pon.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ganz PA, Kwan L, Stanton AL, Krupnick JL, Rowland JH, Meyerowitz BE, Bower JE, Belin TR. Quality of life at the end of primary treatment of breast cancer: First results from the moving beyond cancer randomized trial. J Natl Cancer Inst. 2004;96:376–387. doi: 10.1093/jnci/djh060. [DOI] [PubMed] [Google Scholar]
- 18.Arora NK, Gustafson DH, Hawkins RP, McTavish F, Cella DF, Pingree S, Mendenhall JH, Mahvi DM. Impact of surgery and chemotherapy on quality of life of younger women with breast carcinoma: A prospective study. Cancer. 2001;92:1288–1298. doi: 10.1002/1097-0142(20010901)92:5<1288::aid-cncr1450>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 19.Broeckel JA, Thors CL, Jacobsen PB, Small M, Cox CE. Sexual functioning in long-term breast cancer survivors treated with adjuvant chemotherapy. Breast Cancer Res Treat. 2002;75:241–248. doi: 10.1023/a:1019953027596. [DOI] [PubMed] [Google Scholar]
- 20.Burwell SR, Case LD, Kaelin C, Avis NE. Sexual problems in younger women after breast cancer surgery. J Clin Oncol. 2006;24:2815–2821. doi: 10.1200/JCO.2005.04.2499. [DOI] [PubMed] [Google Scholar]
- 21.Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psycho-oncology. 2006;15:579–594. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- 22.Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. Journal of Clinical Oncology. 2005;23:3322–3330. doi: 10.1200/JCO.2005.05.130. [DOI] [PubMed] [Google Scholar]
- 23.Schover LR. Premature ovarian failure and its consequences. Vasomotor symptoms, sexuality, and fertility. Journal of Clinical Oncology. 2008;26:753–758. doi: 10.1200/JCO.2007.14.1655. [DOI] [PubMed] [Google Scholar]
- 24.Napolitano MA, Babyak MA, Palmer S, Tapson V, Davis RD, Blumenthal JA. Effects of a telephone-based psychosocial intervention for patients awaiting lung transplantation. Chest. 2002;122:1176–1184. doi: 10.1378/chest.122.4.1176. [DOI] [PubMed] [Google Scholar]
- 25.Nelson EL, Wenzel LB, Osann K, Dogan-Ates A, Chantana N, Reina-Patton A, Laust AK, Nishimoto KP, Chicz-DeMet A, du Pont N, Monk BJ. Stress, immunity, and cervical cancer: Biobehavioral outcomes of a randomized clinical trial. Clinical Cancer Research. 2008;14:2111–2118. doi: 10.1158/1078-0432.CCR-07-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meneses KD, McNees P, Loerzel VW, Su X, Zhang Y, Hassey LA. Transition from treatment to survivorship: Effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncology Nursing Forum. 2007;34:1007–1016. doi: 10.1188/07.ONF.1007-1016. [DOI] [PubMed] [Google Scholar]
- 27.Budin WC, Hoskins CN, Haber J, Sherman DW, Maislin G, Cater JR, Cartwright-Alcarese F, Kowalski MO, McSherry CB, Fuerbach R, Shukla S. Breast cancer: education, counseling and adjustment among patients and partners: a randomized clinical trial. Nurs Res. 2008;57:199–213. doi: 10.1097/01.NNR.0000319496.67369.37. [DOI] [PubMed] [Google Scholar]
- 28.Downe-Wamboldt BL, Butler LJ, Melanson PM, Coulter LA, Singleton JF, Keefe JM, Bell DG. The effects and expense of augmenting usual cancer clinic care with telephone problem-solving counseling. Cancer Nursing. 2007;30:441–453. doi: 10.1097/01.NCC.0000300164.90768.ec. [DOI] [PubMed] [Google Scholar]
- 29.Campbell LC, Keefe FJ, Scipio C, McKee DC, Edwards CL, Herman SH, Johnson LE, Colvin OM, McBride CM, Donatucci C. Facilitating research participation and improving quality of life for African American prostate cancer survivors and their intimate partners. Cancer. 2006;109:414–424. doi: 10.1002/cncr.22355. [DOI] [PubMed] [Google Scholar]
- 30.Mishel MH, Belyea M, Germino BB, Stewart JL, Bailey DE, Robertson C, Mohler J. Helping patients with localized prostate carcinoma manage uncertainty and treatment side effects. Cancer. 2002;94:1854–1866. doi: 10.1002/cncr.10390. [DOI] [PubMed] [Google Scholar]
- 31.Mishel MH, Germino BB, Gil KM, Belyea M, Laney IC, Stewart J, Porter L, Clayton M. Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psycho-Oncology. 2005;14:962–978. doi: 10.1002/pon.909. [DOI] [PubMed] [Google Scholar]
- 32.Sandgren AK, McCaul KD, King B, O’Donnell S, Foreman G. Telephone therapy for patients with breast cancer. Oncology Nursing Forum. 2000;27:683–688. [PubMed] [Google Scholar]
- 33.Sandgren AK, McCaul KD. Short-term effects of telephone therapy for breast cancer patients. Health Psychology. 2003;22:310–315. doi: 10.1037/0278-6133.22.3.310. [DOI] [PubMed] [Google Scholar]
- 34.Allen SM, Shah AC, Nezu AM, Nezu CM, Ciambrone D, Hogan J, Mor V. A problem-solving approach to stress reduction among younger women with breast cancer: A randomized controlled trial. Cancer. 2002;94:3089–3100. doi: 10.1002/cncr.10586. [DOI] [PubMed] [Google Scholar]
- 35.Badger T, Segrin C, Meek P, Lopez AM, Bonham E, Sieger A. Telephone interpersonal counseling with women with breast cancer: Symptom management and quality of life. Oncology Nursing Forum. 2005;32:273–279. doi: 10.1188/05.ONF.273-279. [DOI] [PubMed] [Google Scholar]
- 36.Gotay CC, Moinpour CM, Unger JM, Jiang CS, Coleman D, Martino S, Parker BJ, Bearden JD, Dakhil S, Gross HM, Lippman S, Albain KS. Impact of a peer-delivered telephone intervention for women experiencing a breast cancer recurrence. J Clin Oncol. 2007;25:2093–2099. doi: 10.1200/JCO.2006.07.4674. [DOI] [PubMed] [Google Scholar]
- 37.Cordova MJ, Cunningham LL, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: a controlled comparison study. Health Psychology. 2001;20:176–185. [PubMed] [Google Scholar]
- 38.Cordova MJ, Andrykowski MA. Responses to cancer diagnosis and treatment: Posttraumatic stress and posttraumatic growth. Seminars in Clinical Neuropsychiatry. 2003;8:286–296. [PubMed] [Google Scholar]
- 39.Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ, Horowitz MM, Sobocinski KA, Rizzo JD, Wingard JR. Long term health-related quality of life, growth and spiritual well- being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 40.Thornton AA, Perez MA. Posttraumatic growth in prostate cancer survivors and their partners. Psychooncology. 2006;15:285–296. doi: 10.1002/pon.953. [DOI] [PubMed] [Google Scholar]
- 41.Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, Yount SE, McGregor BA, Arena PL, Harris SD, Price AA, Carver CS. Cognitive behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 42.Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, Rowland JH, Leedham B, Belin TR. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23:6009–6018. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- 43.Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley A, Kirk SB, Austenfeld JL. Randomized controlled trial of written emotional expression and benefit-finding in breast cancer patients. J Clin Oncol. 2002;20(20):4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- 44.Marcus AC, Garrett KM, Kulchak-Rahm A, Barnes D, Dortch W, Juno S. Telephone counseling in psycho-oncology: A report from the Cancer Information and Counseling Line. Patient Educ Couns. 2002;46:267–275. doi: 10.1016/s0738-3991(01)00163-x. [DOI] [PubMed] [Google Scholar]
- 45.Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- 46.Folkman S, Greer S. Promoting psychological well-being in the face of serious illness. When theory, research and practice inform each other. Psycho-Oncology. 2000;9:11–19. doi: 10.1002/(sici)1099-1611(200001/02)9:1<11::aid-pon424>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 47.Horowitz M, Wilner A, Alverez W. Impact of Event Scale as a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 48.Sundin EC, Horowitz MJ. Impact of Event Scale. Psychometric properties. British J Psychiatry. 2002;180:205–209. doi: 10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- 49.Cella DF, Mahon SM, Donovan MI. Cancer recurrence as a traumatic event. Behavioral Medicine. 1990 Spring;:15–22. doi: 10.1080/08964289.1990.9934587. [DOI] [PubMed] [Google Scholar]
- 50.Kaasa S, Malt U, Hagen S, Wist E, Moum T, Kvikstad A. Psychological distress in cancer patients with advanced disease. Radiotherapy and Oncology. 1993;27:193–197. doi: 10.1016/0167-8140(93)90073-h. [DOI] [PubMed] [Google Scholar]
- 51.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. J Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 52.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Psychosomatic Res. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 53.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary clinics: the CES-D and the BDI. International Journal of Psychiatry in Medicine. 1990;20:259–277. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 54.Schulberg HC, Saul M, McClelland MN, Ganguli M, Christy W, Frank R, et al. Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry. 1985;42:1164–1170. doi: 10.1001/archpsyc.1985.01790350038008. [DOI] [PubMed] [Google Scholar]
- 55.Trask PC. Assessment of depression in cancer patients. JCNI Monographs. 2004;32:80–92. doi: 10.1093/jncimonographs/lgh013. [DOI] [PubMed] [Google Scholar]
- 56.Schein RL, Koenig HG. The Center for Epidemiological Studies Depression (CES-D) Scale: assessment of depression in medically ill elderly. Int J Geriat. 1997;12:436–446. [PubMed] [Google Scholar]
- 57.Wenzel LB, Fairclough DL, Brady MJ, Brady MJ, Cella D, Garrett KM, Kluhsman BC, Crane LA, Marcus AC. Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999;86:1768–1774. [PubMed] [Google Scholar]
- 58.Jennrich RI, Schluchter MD. Unbalanced repeated measures models with structural covariance matrices. Biometrics. 1986;42:805–820. [PubMed] [Google Scholar]
- 59.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Assoc; 1988. [Google Scholar]
- 60.Gotay CC, Bottomley A. Providing psycho-social support by telephone: What is its potential in cancer patients? European Journal of Cancer Care. 1998;7:225–231. doi: 10.1046/j.1365-2354.1998.00110.x. [DOI] [PubMed] [Google Scholar]
- 61.Marcus AC, Cella D, Sedlacek S, Crawford D, Crane LA, Garrett K, Quigel C, Gonin R. Psychosocial counseling of cancer patients by telephone: A brief note on patient acceptance of an outcall strategy. Psycho-Oncology. 1993;2:209–214. [Google Scholar]
- 62.Donnelly JM, Kornblith AB, Fleishman S, Zuckerman E, Raptis G, Hudis CA, Hamilton N, Payne D, Massie MJ, Norton L, Holland JC. A pilot study of interpersonal psychotherapy by telephone with cancer patients and their partners. Psycho-Oncology. 2000;9:44–56. doi: 10.1002/(sici)1099-1611(200001/02)9:1<44::aid-pon431>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 63.Ganz PA, Greendale GA, Petersen L, Zibecchi L, Kahn B, Belin TR. Managing menopausal symptoms in breast cancer survivors: results of a randomized controlled trial. J Natl Cancer Inst. 2000;92(13):1054–1064. doi: 10.1093/jnci/92.13.1054. [DOI] [PubMed] [Google Scholar]
- 64.Thors CL, Broeckel JA, Jacobsen PB. Sexual functioning in breast cancer survivors. Cancer Control. 2001;8(5):442–448. doi: 10.1177/107327480100800508. [DOI] [PubMed] [Google Scholar]
- 65.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of Posttraumatic Growth. Lawrence Erlbraum Associates; New York: 2006. pp. 138–175. [Google Scholar]
- 66.Hewitt M, Herdman R, Simone J. Institute of Medicine, National Research Council of the National Academies. The National Academies Press; Washington DC: 2004. Meeting Psychosocial Needs of Women with Breast Cancer. [PubMed] [Google Scholar]