Abstract
It is widely accepted that acute demyelinating plaques in patients with multiple sclerosis (MS) demonstrate increased apparent diffusion coefficient (ADC) and increased diffusion weighted imaging (DWI) signals on MRI. These imaging characteristics in acute MS lesions have been postulated to be due to peripheral vasogenic edema that typically increases the apparent diffusion coefficient (ADC). This assumption is commonly used to differentiate stroke from MS lesions since acute and subacute stroke lesions demonstrate increased DWI signal with reduced ADC due to acute cytotoxic edema.
We report a case of active relapsing-remitting MS with two new symptomatic contrast-enhancing lesions. The lesions had reduced diffusion on the ADC map in the early acute phase of MS exacerbation. The reduced ADC signal was subsequently “converted” to increased ADC signal which coincided with the development of profound peripheral vasogenic edema seen on T2-weighted images. To our knowledge, this is the first serial MRI study describing decreased ADC signal in the early acute phase of contrast-enhancing MS lesion. The implications of decreased diffusion in the acute phase of MS lesions for the disease pathogenesis are discussed.
Introduction
It is widely accepted that acute demyelinating plaques in patients with multiple sclerosis (MS) demonstrate increased apparent diffusion coefficient (ADC) and increased diffusion weighted imaging (DWI) signals on MRI [1–4]. These imaging characteristics in acute MS lesions have been postulated to be due to peripheral vasogenic edema [5] that increases the apparent diffusion coefficient (ADC). This assumption is commonly used to differentiate stroke from MS lesions since acute and subacute stroke lesions demonstrate increased DWI signal with reduced ADC due to acute cytotoxic edema.
We report a case of active relapsing-remitting MS with two new symptomatic contrast-enhancing lesions. The lesions had reduced diffusion on the ADC map in the early acute phase of MS exacerbation. The reduced ADC signal was subsequently “converted” to increased ADC signal which coincided with the development of profound peripheral vasogenic edema seen on T2-weighted images. To our knowledge, this is a first report describing centrally decreased ADC signal in the early acute phase of contrast-enhancing MS lesion.
Case Report
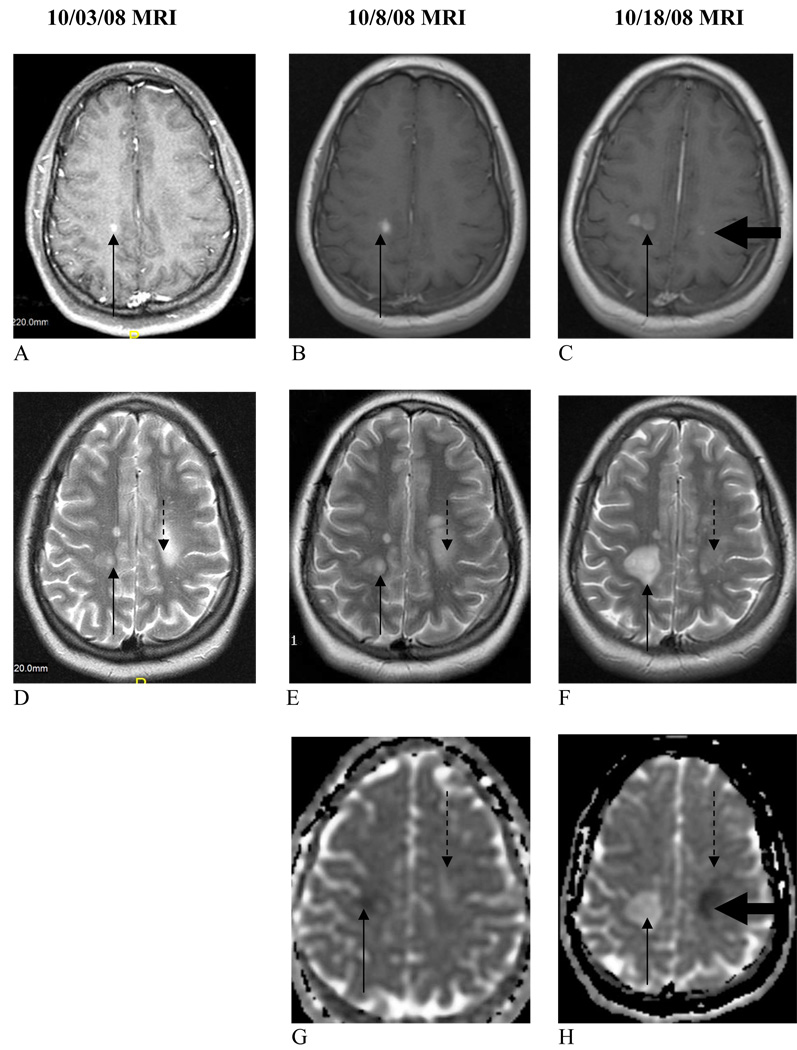
A 21-year-old woman developed right-sided weakness, right facial droop, ataxia, and aphasia on September 2, 2008. An initial brain MRI on September 3, 2008 (not shown) revealed multiple lesions including a large demyelinating enhancing lesion adjacent to the left lateral ventricle. The patient had a complete resolution of her symptoms one week later. A repeat brain MRI performed on October 3, 2008 revealed a new asymptomatic contrast-enhancing lesion (“10/3/08”lesion, Fig.1 A, D) in the white matter close to the right precentral gyrus which became symptomatic 2 days later with a new onset of left-sided weakness, mostly in her left leg, concordant with “10/3/08” lesion location. The patient was diagnosed with clinically definite MS based on the 2005 revised McDonald criteria. Serum studies were normal for B12, Lyme, TSH, RPR. CSF cytological study revealed elevated concentration of nucleated cells (20 cells/mm3) with 16 lymphocytes and 4 monocytes counted. Cytopathological report was negative for malignant cells. CSF Lyme screening by ELISA, microbiological cultures, protein and glucose levels were normal. CSF IgG level was elevated. Chest CT study was not consistent with sarcoidosis. The cervical spine MRI study did not reveal asymptomatic demeylinating plaques on conventional T2-weighted and FLAIR sequences. A repeat brain MRI performed on October 8, 2008 revealed the same enhancing “10/3/08”lesion (Fig. 1 B). The patient was treated with IV steroids but developed a new episode of right leg weakness on 10/17/08. Her 10/18/08 brain MRI revealed a new symptomatically concordant contrast-enhancing lesion in the white mater close to the left precentral gyrus (“10/17/08”lesion, Fig.1 C). After an additional course of IV steroids and plasmapheresis, the patient began to improve and was started on IFN-beta-1b. The patient was able to ambulate without support two months later.
Figure 1.
Brain MRI performed on 10/3/08 (A, D), 2 days prior symptom onset, and on 10/8/08 (B, E, G), 3 days after symptom onset, revealed the symptomatic lesion (“10/3/08” lesion, thin solid arrow). This lesion has contrast enhancement on T1WI (A, B), has surrounding restricted diffusion on the ADC map (G) and faint increased signal on the T2WI (D, E). The presenting lesion of 9-2-08 (thin dashed arrow) has typical imaging characteristics of a chronic MS lesion with hyperintense T2 signal (E) and increased diffusion (G). Brain MRI on 10/18/08 (C, F, H) revealed a new acute symptomatic lesion (“10/17/08” lesion, thick solid arrow) set. This lesion is contrast-enhancing on T1-weighted image (C) and has corresponding restricted diffusion on the ADC map (H). The 10/3/08 lesion (thin solid arrow) resembles a tumefactive lesion. It has increased in size, has increased T2WI signal (F), has increased ADC signal (F) and has increased enhancement post gadolinium administration (C). Both lesions had increased DWI signal and were negative for blood products based on GRE sequences (not shown).
Brain MRI analysis revealed that the “10/3/08”lesion had decreased diffusion surrounding the contrast-enhancing portion of the lesion on 10/8/09, which was 5 days after the enhancing lesions was detected for the first time. This atypical ADC signal intensity lesion converted to the more typical imaging characteristics in the ensuing two weeks with increased diffusion and increased T2 signal characteristic of peripheral vasogenic edema and MS. The other “10/17/08”lesion was also found to have decreased diffusion one day after the onset of symptoms.
Discussion
DWI and ADC map are valuable sequences in the evaluation of acute ischemic events. Within minutes after the onset of ischemia, a profound restriction in water diffusion may occur in the damaged brain tissue and last for 1–4 weeks [6]. There is increased signal on DWI and decreased signal on ADC in this acute phase presumably secondary to cytotoxic edema. In contrast, vasogenic edema is associated with increased diffusion and, therefore, increased ADC which is considered the ‘typical” imaging scenario for acute MS plaques [1].
In MS, most active symptomatic lesions are contrast-enhancing. This reflects a breakdown in the blood-brain barrier which predisposes to “leakage” of gadolinium contrast into the lesion and vasogenic edema producing increased signal on DWI and on ADC MRI. Due to a subacute onset of clinical symptoms in MS, the identification of new contrast-enhancing lesions on MRI is often delayed by several days in a real clinical setting. In addition, many MS lesions, e.g., the “10/3/08” lesion described in our case, may have a sub-clinical phase lasting for 2 days or longer. Therefore, the identification of early phase of MS lesion is quite challenging.
Tievsky et al reported increased central diffusion in acute MS lesions with peripheral contrast enhancement. However, the duration of clinical symptoms was more than 1 week in 7 from 8 patients analyzed. The authors explained the imaging characteristics of MS lesions seen as arising from peripheral vasogenic edema [5] producing the increased diffusion.
Rosso et al [7] reported a case of decreased ADC signal in new hyperacute brain lesion in a 36-year-old MS patient. However, no contrast-enhancing signal was documented raising the possibility that the lesions could have an etiology different from MS.
The two acute MS lesions described in this report (Fig.1) have central contrast enhancement and minimal surrounding vasogenic edema based on observation of faint T2-weighted hyperintensity on brain MRI performed 2 days prior or 1 and 3 days after the onset of clinical symptoms. It is perhaps this early acute phase of MS lesion progression, prior to the expression of vasogenic edema that leads to imaging characteristics akin to stroke and atypical for MS; that is increased signal on DWI with decreased signal on ADC suggesting cytotoxic edema. Still, the central enhancement of the above lesions is atypical for stroke. Recently, Barnett and Prineas reported a unique autopsy of a young MS patient, who died within 24 hours of the onset of a new symptomatic lesion. The extensive oligodendrocyte apoptosis in a circumscribed and relatively small area (2–10 mm in diameter) could be seen as the initial event in new lesion formation in this single case [8].
The finding of restricted diffusion in early MS lesions may have a number of implications. First, it makes the differential diagnosis of stroke versus MS in young patients more complicated if no contrast-enhancing MRI is performed. Second, more research is needed to understand the relationship of decreased diffusion in selected MS lesions to clinical prognosis and disease pathogenesis. Third, it remains to be determined if cytotoxic edema is unique for selected acute MS lesions and MS patients or simply not routinely appreciated on the ADC map in the majority of MS patients due to the “masking” effect of vasogenic edema on the delayed MRI.
Acknowledgments
Funding Sources:
This investigation was supported in part by NIH grant K23NS052553 and NMSS grant RG3953A2/1 (K.E.B).
Footnotes
The authors report no conflicts of interest.
Contributor Information
Konstantin E. Balashov, Department of Neurology, UMDNJ - Robert Wood Johnson Medical School.
Latt Latt Aung, Department of Neurology, UMDNJ - Robert Wood Johnson Medical School.
Suhayl Dhib-Jalbut, Department of Neurology, UMDNJ - Robert Wood Johnson Medical School.
Irwin A. Keller, Department of Radiology, UMDNJ - Robert Wood Johnson Medical School.
References
- 1.Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology. 2000;217(2):331–345. doi: 10.1148/radiology.217.2.r00nv24331. [DOI] [PubMed] [Google Scholar]
- 2.Horsfield MA, et al. Diffusion magnetic resonance imaging in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1998 64; Suppl 1:S80–S84. [PubMed] [Google Scholar]
- 3.Schaefer PW. Diffusion-weighted imaging as a problem-solving tool in the evaluation of patients with acute strokelike syndromes. Top Magn Reson Imaging. 2000;11(5):300–309. doi: 10.1097/00002142-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Castriota-Scanderbeg A, et al. Diffusion of water in large demyelinating lesions: a follow-up study. Neuroradiology. 2002;44(9):764–767. doi: 10.1007/s00234-002-0806-y. [DOI] [PubMed] [Google Scholar]
- 5.Tievsky AL, Ptak T, Farkas J. Investigation of apparent diffusion coefficient and diffusion tensor anisotrophy in acute and chronic multiple sclerosis lesions. AJNR Am J Neuroradiol. 1999;20(8):1491–1499. [PMC free article] [PubMed] [Google Scholar]
- 6.Chien D, et al. MR diffusion imaging of cerebral infarction in humans. AJNR Am J Neuroradiol. 1992;13(4):1097–1102. discussion 1103-5. [PMC free article] [PubMed] [Google Scholar]
- 7.Rosso C, et al. Diffusion-weighted MR imaging characteristics of an acute strokelike form of multiple sclerosis. AJNR Am J Neuroradiol. 2006;27(5):1006–1008. [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett MH, Prineas JW. Relapsing and remitting multiple sclerosis: pathology of the newly forming lesion. Ann Neurol. 2004;55(4):458–468. doi: 10.1002/ana.20016. [DOI] [PubMed] [Google Scholar]