Abstract
Objectives
To investigate provider and patient views about communication regarding cervical cancer screening follow-up.
Methods
Using qualitative analysis, we interviewed 20 providers and 10 patients from two urban clinics that serve low-income African American and Hispanic women. Semi-structured interviews and focus groups assessed familiarity with National Cancer Institute's Cancer Information Service (CIS) and reactions to a letter asking women with abnormal Pap test to telephone CIS. The letter suggested questions to ask prior to receiving follow-up.
Results
No patient or provider was familiar with CIS. Providers but not patients expressed discomfort with use of the word `cancer' in the letter and in CIS's name. Providers feared that reference to cancer would provoke fatalism and impede timely follow-up, whereas patients felt information about cancer risk was needed to prompt timely follow-up. Information providers found necessary to convey in order to accurately explain abnormal Pap tests surpassed patients' literacy levels.
Conclusion
Qualitative data suggest important gaps in perspective between providers and patients. There is a need to bridge the gap and overcome communication challenges to promote timely medical follow-up and have better health outcomes.
Practice Implications
Implications and strategies for improving patient-provider education and communication about abnormal pap test are discussed.
Keywords: Cervical Cancer Screening, Qualitative Research, Women's Health, Health Disparities
1. Introduction
Despite the vast body of research on follow-up of abnormal pap tests, as many as one-half of medically underserved women fails to receive appropriate follow-up [1]. There are many obstacles to follow-up and reaching diagnostic resolution of an abnormal Pap test, and they are heightened among medically underserved women who exhibit both increased incidence of and mortality from cervical cancer [2–6].
A decade ago, nearly 80% of low-income women failed to obtain adequate follow-up and treatment for their abnormal Pap, with follow-up being poorest among minorities [7,8]. Despite improvement, disparities persist and diagnostic resolution of abnormal test remains a conundrum. As many as 50% of medically underserved women in the National Breast and Cervical Cancer Early Detection Program failed to receive appropriate follow-up for an abnormal Pap test, with the likelihood of no follow-up being greatest for African American women [1]. Another recent study found an inadequate follow-up rate of 38%, even though 86% of women continued to receive care in the same place [7,9]. In this paper, we focus on illuminating some of the disconnect in patient-provider communication on Pap test results in the hopes of enhancing patient-provider communication.
Prior research has shown that patient-provider communication can influence behavioral adherence to cancer-related recommendations either positively or negatively [10]. Misunderstandings about Pap testing, colposcopy and cervical cancer are prevalent among low income, low literate women and are associated with poor follow-up [7,11–14]. Effective style and content of such communication can correct confusion and enhance likelihood that patients adhere to recommended follow-up [10]. Medically underserved patients prefer to receive health information verbally [13–15], without medical jargon [12], and primarily from health care providers [16,17]. These preferences heighten informational dependence on overburdened providers who are perceived by patients as lacking time for discussion [18]. Predictors of good patient follow-up in prior research have included: receiving a reminder from providers, knowing the Pap result, being able to report the Pap result correctly, understanding the purpose of colposcopy, and feeling confident the provider will understand the patient's needs [7,14,19,20]. Telephone outreach addressing these domains has been demonstrated to increase short-term (less than 6 months) follow-up adherence to colposcopy by low-income women [21]. Thus some patients who experience a multitude of barriers to follow-up of abnormal pap tests may benefit from more intensive and targeted counseling interventions.
Style as well as content of communications has been shown to be critically important in reaching the medically underserved. Low income minority populations express a strong cultural preference for receiving health information verbally [13,15] and primarily from health care providers [16,17]. That preference heightens informational dependence on overburdened providers who are accurately perceived by patients as lacking time for discussion [12]. Moreover, providers spend less time with the underserved [22], at least partly because low literacy patients ask few questions that medical professionals expect, [18] even when language barriers are absent [15,23,24]. Health illiteracy is prevalent and often hidden by embarrassed patients endeavoring to save face [13,18]. When tested in their native language, 35% of English-speaking and 62% of Spanish-speaking patients in one public hospital showed inadequate or marginal health literacy [19]. Low health literacy predicted recall of less than half of the critical information just given to patients by providers, low adherence, and expressed dissatisfaction with provider-patient communication [25–27]. Medically underserved patients frequently complain that doctors use medical jargon and provide too much technical information, whereas patients wish to be addressed empathically and in plain “living room language” [28].
The premise for this study was that the National Cancer Institute's (NCI) Cancer Information Service (CIS), a free public service providing the latest and most accurate cancer information to patients, their families, health professionals, and the public, could provide a reliable and trustable resource of information for medically underserved women with an abnormal pap test and their providers [29–32]. CIS could thus function as a bridge to enhance communication between underserved women and their providers. CIS offers service in English or Spanish through 1-800-4-CANCER telephone line staffed by highly-trained cancer information specialists [28,33].
This paper reports on the initial formative phase of a mixed methods study to test an intervention called ACCISS (Activating Collaborative CIS Support). ACCISS implements a targeted telephone call and letter from provider to patient reminding her of a scheduled colposcopy appointment, encouraging her to call CIS, and suggesting questions to ask. The target population is low-income, primarily African American and Hispanic women who receive an abnormal Pap test judged by their physician to warrant follow-up colposcopy. In this formative phase of research, providers and patients were asked their a) familiarity with and views about CIS; b) barriers and facilitators of telephoning CIS for information about cancer prevention and screening, c) perceived information support needs for following up abnormal pap tests; and d) feedback on letters planned for ACCISS.
2. Methods
2.1. Sampling
After Institutional Review Board (IRB) review and approval through Northwestern University, we recruited patients and providers from a purposive sample representative of two large clinics affiliated with Northwestern University that serve low-income women in Chicago. The first clinic (Clinic A) serves mostly Hispanic patients; most patients in the second clinic (Clinic B) are African American. At Clinic A on Chicago's West side, 82% of clients live at or below the federal poverty level; 57% have no health insurance; 90% are Hispanic or Latino. At Clinic B on Northwestern University's Chicago campus, outpatient services are provided to a population that is 90% Medicaid/Medicare and 85% minority (80% African American, 20% Hispanic).
We selected for interview five patients from Clinic A and five from Clinic B. All had received abnormal Pap tests previously in their respective clinics; half had received colposcopy. Half of the participants stated they had delayed their own follow-up to their abnormal pat test by more than 1 month. All providers who performed Pap tests and/or colposcopies at both clinics were invited to participate in a focus group, one at each clinic. Each focus group involved ten providers: obstetrician-gynecologists and certified midwives from Clinic A as well as medical residents from Clinic B. Transcripts and interviews were performed until we reached saturation in information or themes [34].
2.2. Data collection
Interviews and focus groups were conducted at the clinics and were tape-recorded using a digital recorder for later transcription. Participants provided written informed consent prior to being interviewed and were served a meal in appreciation. Patients were seen individually by one female investigator for a semi-structured interview in Spanish or English that lasted 30–45 minutes. Providers were seen in separate 80 minute focus groups led by Drs. Spring and Simon.
2.3. Data measurement and instruments
The following questions and prompts served as guides for interviews and focus groups: 1. Have you ever heard of CIS? [After response, the interviewer described CIS]. 2. Let's talk now about this research project and how it might affect you/your patients. What information do you hope you/your patient would know before receiving colposcopy? 3. Do you think that calling/having your patients call CIS could be helpful? 4. What worries do you have about calling/(having your patients call) CIS? 5. Here's the letter we plan to send to women who need colposcopy. What do you think of the letter? Would you recommend any revisions?; 6. [To provider only:] Would you feel comfortable calling the patient who needs colposcopy and suggesting she call CIS? 7. Do you think you/your patient would telephone CIS based on receiving the provider's telephone call and this letter? 8. How do you feel about this intervention? What can we do to improve it?
2.4. Data analysis
Interviews and focus group discussions were transcribed and then double checked by reviewing transcripts along with recordings. Interviews conducted in Spanish were transcribed in Spanish and then translated into English by a native Spanish speaker. Each transcribed interview was then read by two raters who worked independently to identify major themes. Themes were discussed and refined using a consensus process and coding instructions were developed to define each theme. Two coders from the research team independently reviewed responses and coded them according to theme. Discrepancies were discussed until the team reached consensus.
3. Results
3.1. Participant characteristics
Patient and provider demographic data appear in Table 1. All 5 patients from Clinic A were Caucasian and Hispanic and had a history of abnormal Pap test. Three patients admitted to delay in follow-up for over one month after learning of their abnormal test (two Spanish speaking patients and 1 English speaking patient). Three were born in the US, spoke English and were more comfortable being interviewed in English. Two spoke only Spanish and were interviewed in Spanish. Two had received colposcopy in the past. None had been diagnosed with cervical cancer. All 10 Clinic A providers (8 physicians and 2 certified nurse midwives) performed Pap tests; 4 physicians also performed colposcopy.
Table 1.
Demographic Characteristics
| Clinic A | Patients | Race – 5 Caucasian |
| Ethnicity – 5 Hispanic | ||
| English speaking – 3 | ||
| Spanish speaking - 2 | ||
| Abnormal Pap – 2 | ||
| Colposcopy – 2 | ||
| Cancer – 0 | ||
|
| ||
| Clinic A | Providers | Profession: 10 Providers (8 physicians, 2 CNM) (certified nurse midwife) |
| Perform Pap tests at Clinic A - 10 | ||
| Refer Clinic A patients for colposcopy – 6 | ||
| Perform colposcopy at Clinic A - 4 | ||
|
| ||
| Clinic B | Patients | Race - 3 AA*, 2 Caucasian |
| Ethnicity - 2 Hispanic | ||
| English speaking – 5 | ||
| Abnormal Pap – 2 | ||
| Colposcopy – 2 | ||
| Cervical Cancer – 1 | ||
|
| ||
| Clinic B | Providers | Profession - 10 physicians (medical residents ranging from post graduate year 1– 4) |
| Perform Pap tests at Clinic B - 10 | ||
| Refer Clinic B patients for colposcopy - 10 | ||
| Perform colposcopy at Clinic B - 5 | ||
AA: African American
Three of the five Clinic B patients were African American and non-Hispanic. Two were Hispanic. All spoke English. Two had received an abnormal Pap test result in the last five years. Two of these patients admitted to delay in follow-up for over one month after learning of their abnormal pap test (1 African American and 1 Hispanic). Two women had undergone colposcopy or further cervical visualization which may have included biopsies. One participant had been diagnosed with cervical cancer. All 10 Clinic B providers were resident physicians ranging from postgraduate year 1 through 4. All provided Pap tests and colposcopy.
3.2. Themes
The overarching themes concerned: 1) patient and provider knowledge of CIS; 2) reactions to this intervention; and 3) implementation suggestions regarding wording of the intervention letter.
3.2.1. Knowledge of CIS
No patient or provider was aware of CIS.
“The fact that none of us knew about CIS yet we all serve underserved women makes us realize that having information about CIS in our clinic would be useful for the patients.” – Clinic B Resident
3.2.2. Reactions to the intervention
Most patients and providers thought women would benefit from being informed about CIS.
“I was diagnosed with an abnormal Pap and did not get any information. I had a colposcopy and am still trying to find out more. I strongly feel that this information about CIS should be made available to patients. If I had this number earlier, I would have called and asked questions. Can I take this letter? I need this information.” – Clinic B Patient
Providers thought having more time to talk about cervical cancer screening would be helpful to patients. They felt that it would be useful for patients who spoke only Spanish to be able to speak with an information specialist in Spanish.
All patients said that they or a family member would contact CIS if prompted by their provider.
“I would be too scared to call but I would have my mother or sister call and she will definitely find out more and ask questions.” – Clinic A Patient
3.2.3. Suggestions about the intervention letter
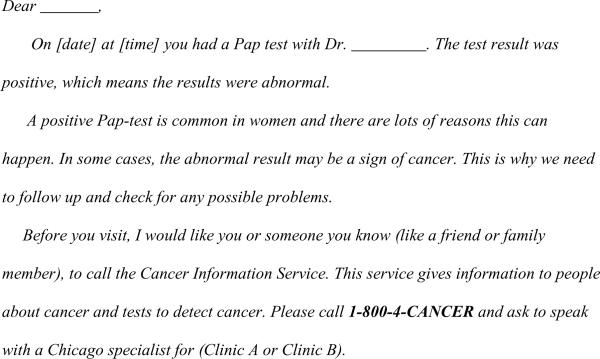
The original letter shown to patients and providers appears in Figure 1. The text was developed through multiple drafts with literacy analyses, input, feedback, and editing from project staff. The letter was written in both Spanish and English and printed on each respective clinic's letterhead.
Figure 1.
Original Intervention Letter
Some kinds of feedback about the letter were uniform. Nearly all patients commented the letter was easy to read and helpful. Many also stated that the phrase, “positive Pap test” was confusing because it sounded like a good thing. Consequently, we revised the letter to state that the Pap was “not normal.” Additional responses of Clinic A patients and providers to the intervention letter appear in Table 2, whereas responses of Clinic B patients and providers appear in Table 3.
Table 2.
Clinic A Reactions to the Letter*
| Clinic A Patients (n=5) | Clinic A Providers (n=10) |
|---|---|
| Good, gives important information (2) | “A lay person will think, `Oh my God, I have cancer'” (4) |
|
| |
| Makes me a little nervous (1) | Patient maybe too scared to show up for follow-up (1) |
|
| |
| Make it warm. Add feelings (1) | If patient can talk to someone (at CIS) and feel less anxious about the follow-up and know what to expect, it might help (1) |
|
| |
| Good, direct and short (1) | |
|
| |
| Probe: Would you be scared when you saw the word `cancer'? | All 10 providers did not like the use of the word cancer in the letter. |
| Yes - 2 | |
| No - 1 | |
| Yes but would still call – 3 | |
Note: `n' for each thematic response may not add to total `N' since participants may provide more than one response or no response
Table 3.
Clinic B Reactions to the Letter*
| Clinic B Patients (n=5) | Clinic B Providers (n=10) |
|---|---|
| Good. Great. Easy to understand. Straight to the point (4) | Word `cancer' very scary, may discourage patients from calling (5) |
| Word `cancer' scary, but important (2) | Use `abnormal' instead of positive & `pre-cancerous lesion' instead of cancer (3) |
| Need to use the word `cancer' `or we'll just blow it off (3) | Word `cancer' may work as fear factor. Encourage patients to take it seriously (2) |
| Just right, `Can I take it with me?'(1) |
• Note: `n' for each thematic response may not add to total `N' since participants may provide more than one response or no response
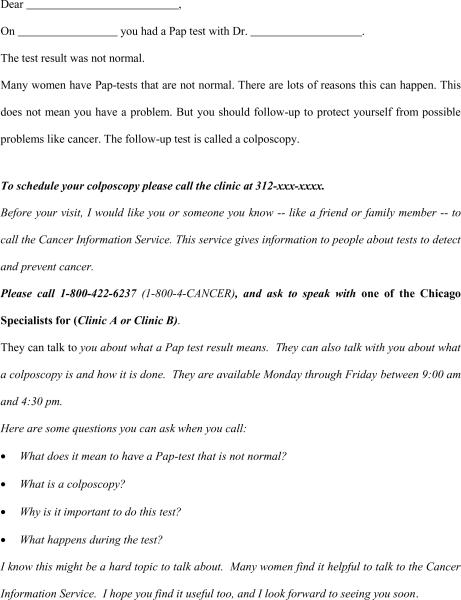
The major point of controversy concerned use of the word `cancer' in the letter. Approximately 50% of providers and some patients were hesitant about use of the word `cancer,' stating that it would invoke too much fear among patients. Providers at the predominantly Hispanic Clinic A expressed strong concern that reference to cancer would prompt fatalism. They predicted that patients would believe they have terminal cancer and would fail to return for medical follow-up. Indeed several Hispanic patients at both clinics did express some fear about reading the word cancer, but said they would still call CIS. However, most patients, particularly the African American women interviewed at Clinic B stated that it was essential to use the word cancer in order for them to take the letter seriously.
Providers also worried that inclusion of the word `cancer' in CIS's name would make patients think that the telephone information line was meant only for patients with a cancer diagnosis. That interpretation would make the CIS call service at best irrelevant and at worst too frightening to call for people with pre-cancer or an abnormal screening test. Patients, however, did not seem to object that the word `cancer' was included in the name of a service they would call for information about cancer prevention.
Many providers, particularly at Clinic B, wanted to add additional information to the letter in order to describe the Pap test result more accurately. They felt that key pieces of information such as “abnormal cells” and on human papilloma virus (HPV) were omitted. Instead of the word `cancer,' they recommended using the phrase `abnormal cells' or `precancerous changes.' They also suggested that the letter should include a paragraph about what HPV is, that it is sexually transmitted, and that abnormal change in the pap test may be due to HPV.
Providers in the Clinic B focus group suggested redrafting the letter:
An abnormal Pap-test is common in women and there are lots of reasons this can happen. In some cases, the abnormal result may be a sign of a pre-cancerous lesion or inflammation. It does need to be checked further as it could be abnormal but not necessarily cancerous condition. If treated in a timely fashion this could prevent the actual development of cancer. This is why we need to follow-up and check for any possible problems. The follow-up test is called a colposcopy. A colposcopy is a longer version of a Pap test where we magnify the cervix to look for possible problems.”
Through much discussion and feedback from patients and providers, the letter was modified to the version in Figure 2.
Figure 2.
Final Modified Intervention Letter
4. Discussion
4.1. Discussion
These qualitative data illustrate several challenges in provider-patient communication about cervical cancer screening follow-up. In particular, many providers feared using the word `cancer' when communicating to their patients about abnormal Pap test results. All providers suggested the term was unduly frightening to patients. Providers for Hispanic women stated that using the word `cancer' would trigger fatalistic beliefs in their patients. They feared that fatalism would be counterproductive and it would interfere with patients' likelihood of medical follow-up. Providers expressed amazement when we revealed that patients responded favorably to the intervention letter.
Although some patients did say they found the word cancer scary, none said they would be discouraged from calling CIS or completing medical follow-up. Most patients said it was important to have the word cancer in the letter since it conveyed the truth about the nature of their risk. Providers' discomfort about using the term `cancer' may reflect vestiges of medical paternalism [35]. In the past, physicians made decisions on their patients' behalves while endeavoring to shield them from harsh, upsetting realities. Today, however, full disclosure of information about risk is more consistent with shared medical decision-making as the standard of care [36–40]. Even though research shows that cancer thoughts elicit anxiety [41], our data do not bear out the worry that patients cannot handle potentially upsetting information about cancer risk. Although some patients acknowledge finding the information upsetting, most say they need to be informed of their risks in order to act appropriately and in a timely manner. This finding is consistent with prior research on patient's desire for shared and informed decision making [39,42] and research on threat and motivation [43]. Threat of the word `cancer' invokes an initial avoidance reaction in that the word is `scary,' but ultimately, the word `cancer' serves to motivate the patient towards a beneficial response to seek answers, in this case through CIS[43].
Additionally, all women in this sample (including those with a history of non-compliance with follow-up) stated that they or a close friend or family member would call CIS to obtain more information. This illustrates that medically underserved women, when offered a specific source of abnormal Pap test information directly from their provider, are more willing to try and access that resource. They were willing to accept direction in what to ask (the list of questions were on the proposed intervention letter) and to whom to ask the questions (CIS). Upon learning more about CIS and the accuracy of information given to callers, all providers expressed that they would be willing to support this intervention that gave a direct referral to CIS as a source of additional information. Providers were also comfortable in giving the patients a list of questions to ask CIS.
To communicate effectively and appropriately with medically underserved patients is a complex task influenced by many factors. Prior research has emphasized the importance of leveraging culture and language differences to incorporate into verbal and written cancer information given to patients [44,45]. In addition to culture and language, geography and social environment impact a woman's non-compliance with follow-up of an abnormal pap test [46]. Studies using data from Health Information National Trends Survey (HINTS) have demonstrated that Hispanic patients express minimal confidence in being able to obtain cancer information that they understand [29–32,44,47].
CIS has been studied as a mechanism to help provide information to the US public by responding to the cancer needs of callers through a one-on-one phone interaction. Referring patients to call CIS is a way to alleviate some of the burden of time constriction felt by providers. CIS information specialists can fill an important gap in the lack of accessible information to medically underserved patients. Also, CIS gives providers and patients up-to-date information on cancer, treatment, and clinical trials. Literature on CIS and its impact on medically underserved is less developed, but highlights the potential of CIS to build such a bridge in communication. Gustafson and colleagues studied how CIS could close the digital divide in internet use and render health information with facility among medically underserved populations [48]. In this paper we highlight the formative research phase involved with building an intervention that increases both awareness of CIS to medically underserved women and their providers within the prevue of encouraging follow-up to an abnormal cervical cancer screening test.
This study also builds on prior studies by Miller and colleagues who conducted a telephone follow-up study of women with abnormal pap tests [21]. Telephone counseling by a health educator improved adherence to the initial colposcopy follow-up visit over those that did not receive the telephone counseling. We built on Miller's results to see if the source of the information given via the phone could be larger and government funded, and have the word “cancer” in its title in light of the fact that not all women with abnormal pap tests have cancer. This study demonstrates acceptability among patients and their providers to refer or accept referral of an outside source of information.
The findings also illustrate a tension between the literacy level providers found necessary to convey cancer screening information accurately versus the level that could be comprehended readily by low literacy adults lacking medical training. What the providers felt to be valuable discussion of “precancerous lesions,” “inflammation,” or “HPV” was experienced by patients as technical jargon that did not provide useful information. From that disjunction arises a phenomenon we observed frequently. Providers asserted confidently that their patients understood all about cervical cancer screening because the provider devoted great time and effort to explaining everything at length. Meanwhile, patients stated with equal confidence that they had been given no information. This disconnect may be due to physicians communicating in a style or language that did not resonate for their patients. Research on meeting the literacy needs of patients echoes such gaps in communication encountered in this study and highlights the importance of integration of culture and messages derived from the community of interest into health education communication [49,50,51].
This research has limitations. The small sample was purposive rather than random and is not representative of all patients in the clinics. Moreover, generalizability of these results to other clinic settings or other populations is not possible. However, coders did reach saturation in identifying themes from patients and providers at both clinics. Another limitation is that the patient interviews may incorporate reporting bias. Because the interviews were conducted in the clinic setting, demand characteristics may have influenced patients to reveal answers they felt the study team wanted to hear. Steps taken to reduce reporting bias included: providers were absent during patient interviews and patients were absent during provider interviews. Patient interviewers were neither healthcare providers nor clinic staff.
Nevertheless, the study results contribute to an understanding of communication and follow-up regarding an abnormal cervical cancer screen via formative data collection. These data confirm two important communication gaps between providers and patients: one regarding use of the word `cancer', the other regarding the type and amount of explanation needed by patients. In the patients' opinions, reference to `cancer' in the provider's letter served to motivate timely medical follow-up. In the providers' opinion, use of the word cancer triggered fear and fatalism that served to deter follow-up. The second gap concerned disagreement about amount and literacy level of letter content needed to motivate patients to pursue timely medical follow-up. Patients thought the amount of content in the letter was sufficient to motivate follow-up. Providers, in contrast, thought that a considerable amount of technical information needed to be included.
Finally, this study demonstrated acceptance among both patients and providers to participate in such a referral process to an outside information source- CIS. Both patients and providers were also willing to receive/provide a list of specific questions with which to ask CIS.
4.2. Conclusion
This study's use of formative research to elicit patient and provider thoughts on communication via discussion of the intervention letter highlights an important strategy in behavioral research. The information gained from this formative research reveals the importance of deriving messages from the potential research participants to enhance the quality of communication interventions [52]. A sizeable communication gap between providers and underserved patients about cervical cancer screening follow-up became evident in this study.
Further qualitative study of barriers and facilitators of provider communication with medically underserved patients among a larger and more diverse sample is warranted to close the gap and promote follow-up adherence. Advancing such data with more information on attentional style and health behaviors as advocated by Miller and colleagues would help to further tailor appropriate interventions to improving follow-up to abnormal pap tests [53]. Such data would provide further insight into the salient characteristics of subgroups of medically underserved women that are essential to developing effective strategies to address cancer screening follow-up.
4.3. Practice implications
There are several implications for practice that follow from these findings. First, improved communication regarding abnormal pap testing should be prioritized. There is a clear gap between provider's perceptions of what their patients need to hear and patient's comments on their own needs in order to prompt follow-up. Whether results are verbal or written, they should be communicated in simple and clear language. Second, these findings suggest that more dialogue between patients and providers should occur around how or what the patient desires to hear abnormal results in order to more optimally prompt follow-up. As patient-provider communication strives to be patient-centered, tailoring plans for how to present results if they are abnormal to individual patients is an essential step in facilitating a patient's re-entry to the clinic for follow-up. Third, involving a third-party provider of patient education can potentially play a significant role in further facilitating tailored patient-provider communication and follow-up. Finally, ongoing education of women about the paucity of signs and symptoms of cervical cancer and screening guidelines is critical.
Acknowledgement
We extend our gratitude to: Katty Cavero for conducting and translating the interviews in Spanish; the providers and women in clinics for participating in the research; and NCI's Cancer Information Service for unyielding support of this project. The authors have no conflict of interest to disclose.
Financial Disclosure: Funded in part by NIH grants R21 CA126450 to Dr. Spring and by NICHD K-12 HD050121 to Dr. Simon
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
We confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
References
- [1].Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstetrics & Gynecology. 2005;105(6):1323–1328. doi: 10.1097/01.AOG.0000159549.56601.75. [DOI] [PubMed] [Google Scholar]
- [2].Engelstadt LP, Stewart SL, Nguyen BH, Bedeian KL, Rubin MM, Pasick RJ, Hiatt RA. Abnormal Pap smear follow-up in a high-risk population. Cancer Epidemiology, Biomarkers & Prevention. 2001;10:1015–1020. [PubMed] [Google Scholar]
- [3].Benard VB, Lee NC, Piper M, Richardson L. Race-specific results of Papanicolaou testing and the rate of cervical neoplasia in the National Breast and Cervical Cancer Early Detection Program, 1991–1998 (United States) Cancer Causes and Control. 2001;12:61–68. doi: 10.1023/a:1008959019019. [DOI] [PubMed] [Google Scholar]
- [4].Paskett ED, Carter WB, Chu J, White E. Compliance behavior in women with abnormal Pap smears: developing and testing a decision model. Med Care. 28(1990):643–656. doi: 10.1097/00005650-199007000-00009. E D. [DOI] [PubMed] [Google Scholar]
- [5].Paskett, Phillips KC, Miller ME. Improving compliance among women with abnormal Papanicolaou smears. Obstet Gynecol. 86(1995):353–359. doi: 10.1016/0029-7844(95)00176-R. [DOI] [PubMed] [Google Scholar]
- [6].Eggelston KS, Coker AL, Das IP, Corday ST, Luchok KJ. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Women's Health. 2007;16(3):311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- [7].Lerman C, Hanjani P, Caputo C, Miller S, Delmoor E, Nolte S, Engstrom P. Telephone counseling improves adherence to colposcopy among lower income minority women. J. Clin. Oncology. 1992;10(2):330–333. doi: 10.1200/JCO.1992.10.2.330. [DOI] [PubMed] [Google Scholar]
- [8].Marcus AC, Crane LA, Kaplan CP, Reading AE, Savage E, Gunning J, Bernstein G, Berek JS. Improving adherence to screening follow-up among women with abnormal Pap smears: results from a large clinic-based trial of three intervention strategies. Medical Care. 1992;30(3):216–230. doi: 10.1097/00005650-199203000-00004. [DOI] [PubMed] [Google Scholar]
- [9].Peterson NB, Han J, Freund K. Inadequate follow-up for abnormal Pap smears in an urban population. J. Natl Med Assn. 2003;95:825–832. [PMC free article] [PubMed] [Google Scholar]
- [10].Arora NK. Interacting with cancer patients: the significance of physicians' communication behavior. Social Science & Medicine. 2003;57:791–806. doi: 10.1016/s0277-9536(02)00449-5. [DOI] [PubMed] [Google Scholar]
- [11].Davis TC, Arnold C, Berkel HJ, Nandy I, Jackson RH, Glass J. Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer. 1996;78:1912–1920. doi: 10.1002/(sici)1097-0142(19961101)78:9<1912::aid-cncr11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- [12].Davis TC, Dolan NC, Ferreira MR, Tomori C, Green KW, Sipler AM, Bennett CL. The role of inadequate health literacy skills in colorectal cancer screening. Cancer Invest. 2001;19(2):193–200. doi: 10.1081/cnv-100000154. [DOI] [PubMed] [Google Scholar]
- [13].Davis TC, Williams MV, Marin E, Parker RM, Glass J. Health literacy and cancer communication. CA Cancer J Clin. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- [14].McKee MD, Lurio J, Marantz P, Burton W, Mulvihill M. Barriers to follow-up of abnormal Papanicolau smears in an urban community health center. Arch. Fam Med. 1999;8:129–134. doi: 10.1001/archfami.8.2.129. [DOI] [PubMed] [Google Scholar]
- [15].Mayeaux EJ, Murphy PW, Arnold C, Davis TC, Jackson RH, Sentell T. Improving patient education for patients with low literacy. Am Fam Physician. 1996;53:205–211. [PubMed] [Google Scholar]
- [16].Nguyen TT, McPhee SJ. Patient-provider communication in cancer screening. Journal of General Internal Medicine. 2003;18:402–403. doi: 10.1046/j.1525-1497.2003.30346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Revenson TA, Pranikoff JR. A contextual approach to treatment decision making among breast cancer survivors. Health Psychology. 2005;24:S93–S98. doi: 10.1037/0278-6133.24.4.S93. [DOI] [PubMed] [Google Scholar]
- [18].Anhang R, Goodman A, Goldie SJ. HPV communication: Review of existing research and recommendations for patient education. CA: A Cancer Journal for Clinicians. 2004;54:248–25. doi: 10.3322/canjclin.54.5.248. [DOI] [PubMed] [Google Scholar]
- [19].Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. [PubMed] [Google Scholar]
- [20].Khanna N, Phillips MD. Adherence to care plan in women with abnormal Papanicolaou smears: a review of barriers and interventions. J Am Board Fam Pract. 2001 Mar-Apr;14(2):123–130. [PubMed] [Google Scholar]
- [21].Miller SM, Siejak KK, Schroeder CM, Lerman C, Hernandez E, Helm CW. 1997 Enhancing adherence following abnormal Pap smears among low-income minority women: a preventive telephone counseling strategy. Journal of the National Cancer Institute. 1997;89(10):703–708. doi: 10.1093/jnci/89.10.703. [DOI] [PubMed] [Google Scholar]
- [22].Street RL. Communicative styles and adaptations in physician-parent consultations. Social Science & Medicine. 1992;34:1155–1163. doi: 10.1016/0277-9536(92)90289-3. [DOI] [PubMed] [Google Scholar]
- [23].Landrine H, Klonoff EA. Cultural diversity and health psychology. In: Baum A, Revenson TA, Singer JE, editors. Handbook of Health Psychology. Erlbaum; Hillsdale (NJ): 2001. pp. 851–91. [Google Scholar]
- [24].Doak LG, Doak CC, Meade CD. Strategies to improve cancer education materials. Oncol Nurs Forum. 1996;23(8):1305–12. [PubMed] [Google Scholar]
- [25].Dale W. Evaluating focus group data: Barriers to screening for prostate cancer patients. Cancer Treat Res. 1998;97:115–128. doi: 10.1007/978-0-585-30498-4_9. [DOI] [PubMed] [Google Scholar]
- [26].Friedell GH, Linville LH, Rubio A, Wagner WD, Tucker TC. What providers should know about community cancer control. Cancer Pract. 1997;5:367–374. [PubMed] [Google Scholar]
- [27].Ley P. Communication with Patients: Improving Communication, Satisfaction and Compliance. Chapman & Hall; London: 1993. [Google Scholar]
- [28].Squiers L, Rutten LJF, Treiman K, Bright MA, Hesse B. Cancer patients' information needs across the cancer care continuum: Evidence from the cancer information system. J. Health Communication. 2005;10:15–34. doi: 10.1080/10810730500263620. [DOI] [PubMed] [Google Scholar]
- [29].Marcus AC, Morra ME, Bettinghaus E, Crane LA, Davis S, Rimer BK, Thomsen C, Warnecke RB. The Cancer Information Service Research Consortium: An Emerging Laboratory for Cancer Control Research. Preventive Medicine. 1998;27(5):s3–s15. doi: 10.1006/pmed.1998.0245. [DOI] [PubMed] [Google Scholar]
- [30].Marcus AC, Morra ME, Bright MA, Fleisher L, Kreps G, Perocchia R. The CIS model for collaborative research in health communications: a brief retrospective from the current generation of research. J Health Comm. 2005;10(Suppl1):235–45. doi: 10.1080/10810730500263612. [DOI] [PubMed] [Google Scholar]
- [31].Marcus AC, Woodworth MA, Strickland CJ. The Cancer Information Service as a laboratory ofr research: the first 15 years. J NCI Monographs. 1993;14:67–79. [PubMed] [Google Scholar]
- [32].Wagner EH, Greene SM, Hart G, m Field TS, Fletcher S, Geiger AM, Herrinton LJ, Hornbrook MC, Johnson CC, Mouchawar J, Rolnick SJ, Stevens VJ, Taplic SH, Tolsma D, Bogt TM. Building a research consortium of large health systems: the Cancer Research Network. J NCI Monograph. 2005;35:3–11. doi: 10.1093/jncimonographs/lgi032. [DOI] [PubMed] [Google Scholar]
- [33].Bright MA. The National Cancer Institute's Cancer Information Service: A new generation of service and research to the nation. J Health Communication. 2005;10:7–13. doi: 10.1080/10810730500263687. [DOI] [PubMed] [Google Scholar]
- [34].Pope C, Ziebland S, Mays N. Qualitative research in health care: analyzing qualitative data. BMJ. 2000;320:114–6. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Quill TE, Brody H. Physician Recommendations and Patient Autonomy: Finding a Balance between Physician Power and patient choice. Annals of Internal Medicine. 1996;125:763–769. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- [36].Charles C, Ganfi A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–61. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- [37].Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA. 1992;267:2221–6. [PubMed] [Google Scholar]
- [38].Woolf SH, Chan ECY, Harris R, Sheridan SL, Braddock CH, Kaplan RM, et al. Promoting Informed Choice: Transforming Health Care To Dispense Knowledge for Decision Making. Ann Inter Med. 2005;143:293–300. doi: 10.7326/0003-4819-143-4-200508160-00010. [DOI] [PubMed] [Google Scholar]
- [39].Rimer BK, Briss PA, Zeller PK, Chan EC, Woolf SH. Informed decision making: what is its role in cancer screening. Cancer. 2004;101(5 Suppl):1214–28. doi: 10.1002/cncr.20512. [DOI] [PubMed] [Google Scholar]
- [40].Makoul G, Clayman M. An integrative model of shared decision making. Patient Education and Counseling. 2006;60:301–312. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- [41].Cameron LD, Leventhal Vulnerability beliefs, symptom experiences, and the processing of health threat information: A self-regulatory perspective. J of Applied Social Psychology. 1995;25:1859–83. [Google Scholar]
- [42].Edwards AG, Evans R, Dundon J, Haigh S, Hood K, Elwyn GJ. Personalized risk communication for informed decision making about taking screening tests. Cochrane Database Syst Rev. 2003;1:CD001865. doi: 10.1002/14651858.CD001865.pub2. [DOI] [PubMed] [Google Scholar]
- [43].Arndt J, Cock A, Goldenberg JL, Cox CR. Cancer and the threat of death: the cognitive dynamics of death-thought suppression and its impact on behavioral health intentions. J Pers Soc Pysch. 2007;92(1):12–29. doi: 10.1037/0022-3514.92.1.12. [DOI] [PubMed] [Google Scholar]
- [44].Vanderpool RC, Kornfeld J, Rutten LF, Squiers L. Cancer information-seeking experiences: the implications of Hispanic ethnicity and Spanish language. J Cancer Educ. 2009;24(2):141–7. doi: 10.1080/08858190902854772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Davis SW, Diaz-Mendez M, Garcia MT. Barriers to seeking cancer information among Spanish-speaking cancer survivors. J Cancer Educ. 2009;24(3):167–71. doi: 10.1080/08858190902873053. [DOI] [PubMed] [Google Scholar]
- [46].Katz ML, Wewers ME, Single N, Paskett ED. Key informants' perspectives prior to beginning a cervical cancer study in Ohio Appalachia. Qual Health Res. 2007;17(1):131–4. doi: 10.1177/1049732306296507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Bright MA. The National Cancer Institute's Cancer Information Service: a premiere cancer information and education resource for the nation. J Cancer Educ. 2007;22(1 Suppl):S2–7. doi: 10.1007/BF03174340. [DOI] [PubMed] [Google Scholar]
- [48].Gustafson DH, McTavish FM, Stengle W, Ballard D, Jones E, Julesberg K, McDowell H, Landucci G, Hawkins R. Reducing the digital divide for low-income women with breast cancer: a feasibility study of a population-based intervention. J Health Commun. 2005;10(Suool 1):173–93. doi: 10.1080/10810730500263281. [DOI] [PubMed] [Google Scholar]
- [49].Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Education and Counseling. 2008;71:328–32. doi: 10.1016/j.pec.2008.03.001. [DOI] [PubMed] [Google Scholar]
- [50].Watts T, Merrell J, Murphy F, Williams A. Breast health information needs of women from minority ethnic groups. J Adv Nurs. 2004;47(5):526–35. doi: 10.1111/j.1365-2648.2004.03125.x. [DOI] [PubMed] [Google Scholar]
- [51].Giordano L, Webster P, Anthony C, Szarewski A, Davies P, Arbyn M, et al. Improving the quality of communication in organized cervical cancer screening programs. Patient Education and Counseling. 2008;72(1):130–6. doi: 10.1016/j.pec.2008.02.010. [DOI] [PubMed] [Google Scholar]
- [52].Cameron KA, Francis L, Wolf MS, Baker DW, Makoul G. Investigating Hispanic/Latino perceptions about colorectal cancer screening: a community-based approach to effective message design. Patient Education and Counseling. 2007;68:145–52. doi: 10.1016/j.pec.2007.04.004. [DOI] [PubMed] [Google Scholar]
- [53].Miller SM, Buzaglo JS, Simms SL, Green V, Bales C, Mangan CE, Sedlacek TV. Monitoring styles in women at risk for cervical cancer: implications for the framing of health-relevant messages. Ann Behav Med. 1999;21:27–34. doi: 10.1007/BF02895030. [DOI] [PubMed] [Google Scholar]