Abstract
Purpose
The incidence of painful bone metastases increases with longer survival times. While External Beam Radiation Therapy (EBRT) is an effective palliative treatment, it often requires several days from the start of treatment to produce a measurable reduction in pain scores and a qualitative amelioration of patient pain levels. Meanwhile, the use of analgesics remains the best approach early on in the treatment course. We investigated the role of Radiation Therapists as key personnel for collecting daily pain scores to supplement assessments by physician and oncology nursing staff and manage pain more effectively, during radiation treatment.
Methods and Materials
Daily pain scores were obtained by the radiation therapists for 89 patients undertaking a total of 124 courses of EBRT for bone metastases and compared to pre-treatment pain score. The majority of patients (71%) were treated to 30 (20–37.5) Gy in 10 (8–15) fractions.
Results
A total of 119 treatment courses (96%) were completed. Pain Scores declined rapidly to 37.5%, 50% and 75% of the pretreatment levels by Days 2, 4, and 10 respectively. Pain was improved in 91 % of patients with only 4% of worse pain at the end of treatment. Improved pain scores were maintained in 83% of patients at 1 month follow up, but in 35% of them the pain was worse than at the end of treatment.
Conclusions
Collection of daily pain scores by radiation therapists was associated with an effective reduction in pain scores early on during EBRT of painful osseous metastases.
Keywords: radiotherapy, metastases, palliation, quality improvement
INTRODUCTION
Approximately nine million people are estimated to suffer from cancer annually worldwide and up to 75% of cancer patients experience pain in the advanced and terminal stages (1). Of particular note is that pain management has been deficient in healthcare in general and specifically in the Oncology setting, including Radiation Oncology (2, 3).
EBRT alleviates bone pain significantly in 75%–90% of cases, allowing for a reduction in the pain medications and their side effects (4, 5). This in turn improves quality of life (QoL), often dramatically. Since it may require at least a couple of weeks to reach maximum effectiveness, patients may be totally dependent on pain medications in the interim.
Although non steroids anti inflammatory drugs (NSAIDS) and/or opioids can be used to control pain, the related side effects of these drugs may result in a further reduction of QoL (6). A variety of interfering barriers and misconceptions exist surrounding pain management. Most specifically, poor assessment of pain levels and control options make inadequate pain treatment a major health issue in the U.S (7, 8). Recently, stringent efforts have been made to improve the situation including initiation of proposing pain scores as a “5th” vital sign (9). Although the current situation has improved, particularly in the Oncology field, it still seems to be far from what could be achieved (2, 3, 10–13).
Although radiation oncologists have a significant role in treating pain, there have been suggestions that pain management in radiation oncology (RO) departments has been generally poor and requires much more attention (6, 10, 14). To date, many RO departments do not have a Pain Management Program, or if they do, they usually only monitor pain during weekly “on treatment evaluations” which would occur every 5 fractions.
Lacking an institution wide pain program in the mid 1990’s, the radiation oncology department of Jameson Memorial Hospital, a community hospital, independently instituted one as part of the internal Quality Assurance (QA) program. Initially pain scores were recorded on every outpatient consult and follow up visit as a 5th vital sign and on a weekly basis for patients undergoing EBRT for painful osseous metastases. As a Quality Improvement (QI) initiative, an audit was conducted which unexpectedly indicated generally poor pain control. This was thought to be due to a failure to record pain scores more than once a week and an attempt was made to record daily pain scores in the hope that a more timely pain control intervention could lead to earlier and more effective relief. The clinic nurse (RN) agreed to obtain initial and daily pain assessments from patients undergoing external beam radiation therapy for skeletal metastases and at follow up. However this approach failed, due to conflicting duties in the clinic for the RN which prevented her from collecting daily pain scores. After considerable discussion, the responsibility was undertaken by the radiation therapists. A simple assessment form was inserted into the patient records for collection of daily pain scores during treatment sessions. Audits were conducted every three months to determine if the program was worthwhile.
The results of pain program audits over a period of 5 years are presented here in order to demonstrate how a simple time conserving method for daily pain assessment and the role of a team effort for a QA/QI initiative can be an efficient method of pain management, and help to enhance the quality of life for bone metastasis patients.
METHODS AND MATERIALS
This retrospective review has been approved as a QA/QI Study by the "QI Review committee of the Quality Patient Care Committee of the University of Pittsburgh Medical Center as well by the Jameson Hospital IRB.
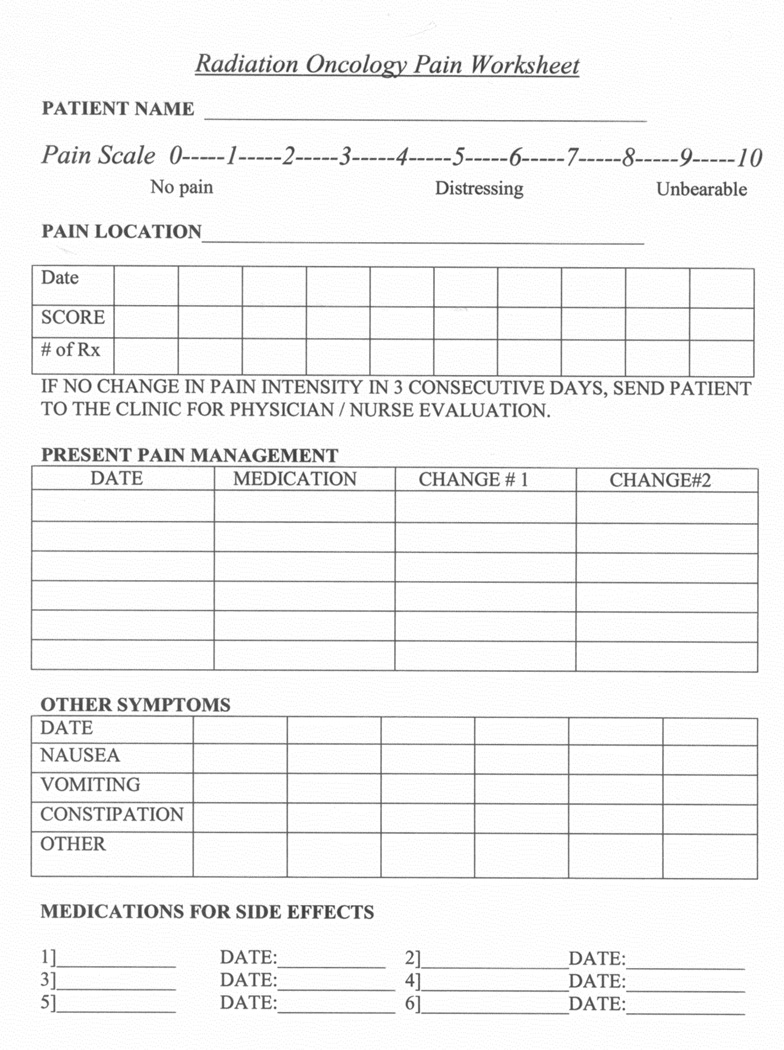
Patients were instructed initially in the use of a numeric rating scale for pain (0–10), and asked to rate their pain throughout radiation treatment. Pain management was handled based on the three step analgesic ladder (15), and most were managed with a long acting narcotic and a short acting narcotic for breakthrough pain. Pain scores were recorded in a designated form (Figure 1) at the time of initial consultation by the doctor and/or nurse and then subsequently by the therapists on a daily basis during treatment. If pain scores either increased or did not improve over a maximum of 3 days of treatment, the patient was referred to the nurse and doctor for additional evaluation and possible intervention. However patients could, and frequently did seek attention on Days 1 and 2. Follow up scores were also obtained by the nurse or doctor at the post-treatment visit usually 2–4 weeks after radiation. The pain scores were collected and an analysis of pain relief was made based on comparisons of scores taken at pre-treatment, during treatment, and after treatment at follow up (Figure 2).
Figure 1. Pain collection form.
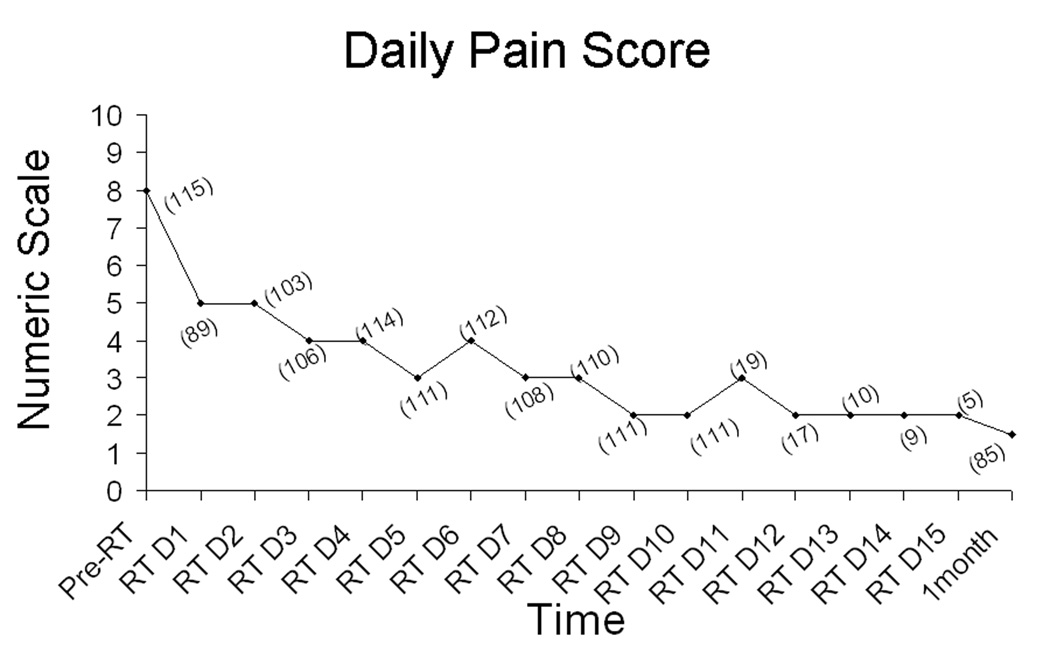
Figure 2. Pain score obtained during and after RT.
RTD1–15=radiation treatment days 1–15 and 1 month follow up; (n)= number of pain score for each treatment time, and at 1 month follow up.
From January 2002 to December 2006, 89 patients with painful metastatic bone lesions undertook 124 courses of palliative EBRT, consisting of 8 or more fractions. Bone lesions were irradiated to a median of 30Gy (20–37.5Gy) in approximately 10 fractions (8–15). During this period, 5 treatment courses were not completed: these cases and those receiving 5 fractions or less were excluded from analysis. The number of patients treated to various anatomical sites and the percentage of improved pain scores from start to end of treatment and start to follow up (F/U), as well as stable and improved scores from end of treatment to F/U are listed in Table1. Cases which were treated to hips, spine and sacrum were included under pelvis.
Table 1. Incidence of Pain Control by Site.
Improvement in pain control was calculated from Start to End of treatment and from Start to Follow Up (F/U). Stable or Improved scores were registered for F/U compared to End of treatment. % pain controlled = pain improved or stable.
| Sites | Treatments (n) | Pain Improved (%) | Pain Controlled (%) | |
|---|---|---|---|---|
| Start-End | Start-FU† | End-FU† | ||
| Spine | 50 | 91 | 79 | 61 |
| Pelvis | 25 | 89 | 80 | 79 |
| Lower Ext* | 26 | 91 | 89 | 75 |
| Upper Ext* | 16 | 93 | 89 | 61 |
| Ribs | 7 | 100 | 80 | 20 |
| Average | NA†† | 92.8 | 83.4 | 59.2 |
RESULTS
The pretreatment, daily, and follow up pain scores are summarized in Figure 2. The patient data collection rate was 87%, and the mean pre-treatment pain score was 8 (2–10). By Day 2 of treatment, there was a 37.5% mean reduction in pain scores which improved further to 50% by Day 4 and up to 75% by the end of treatment (Figure 3).
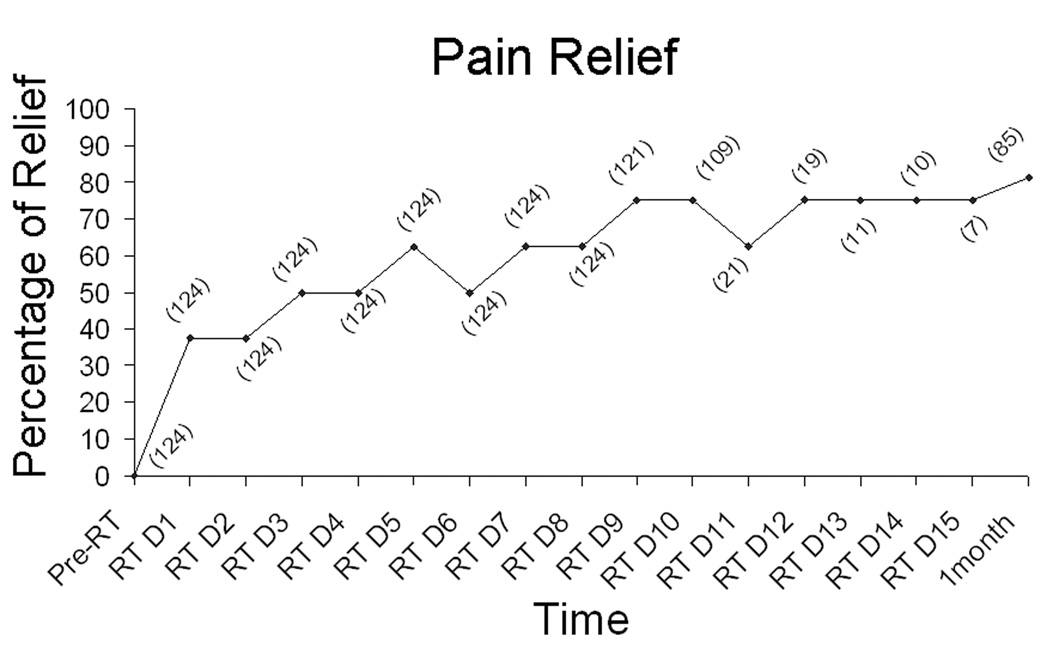
Figure 3. Pain relief observed during and after RT.
RTD1–15=radiation treatment days 1–15; (n)= number of treatments evaluated for each time fraction, and at one month follow up
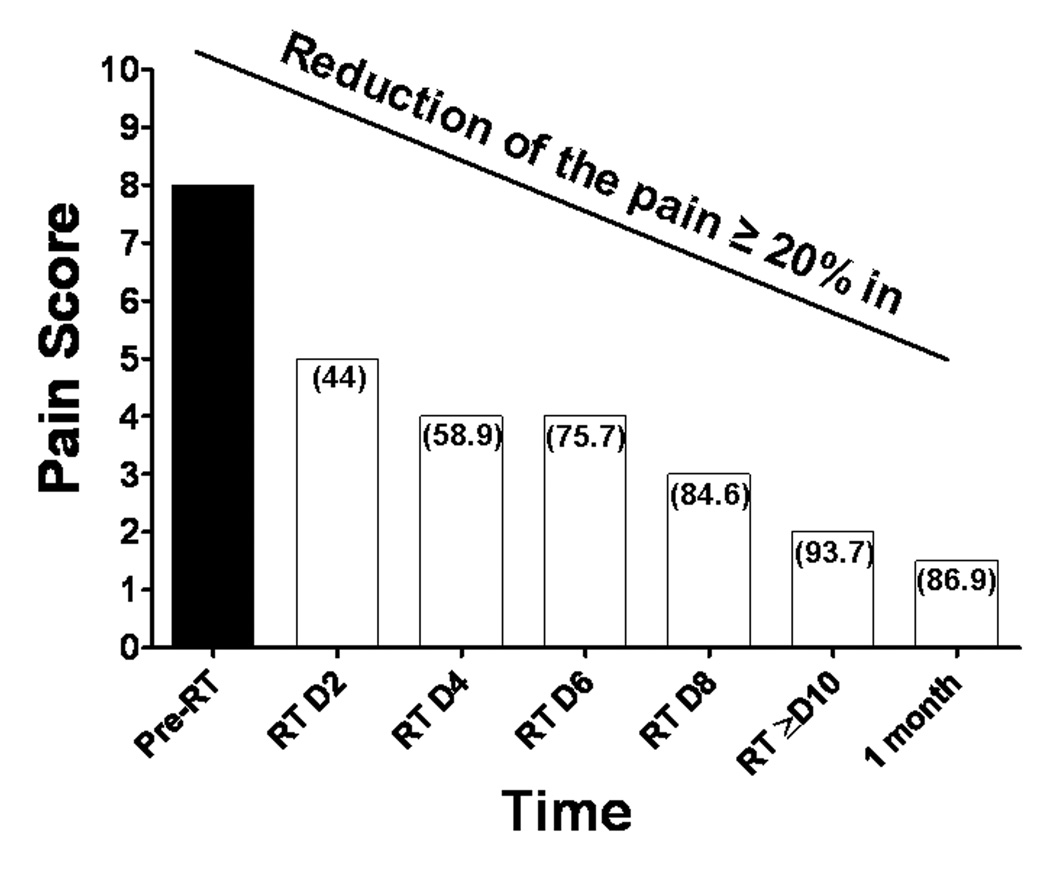
The percentage of patients with a 20% or greater improvement in pain was 44% at Day 1; 59% at Day 2; 75% at day 4, and 84% by Day 10 (Figure 4).
Figure 4. Percentage of patients that observed a pain relief of at least 20% during and after treatment.
(n) = percent of patients that had pain reduced =20%, pre-RT= pre radiotherapy treatment, RT D2–8= radiation treatment days 2–8, RT=10 = radiation treatment days 10–15, and at one month follow up.
The data was also analyzed for changes from the start of treatment to follow up and from the end of treatment to follow up. Pain scores were either stable or improved in 91% of the patients by the end of treatment. This was maintained 83% of the time at 1 month follow up. The pain scores, however, increased between the end of treatment and the F/U visit in 39% of the patients.
There was almost no difference in pain reduction between those receiving 20 to 30Gy in 8–10 fractions and those receiving 30Gy to 37.5Gy in 12 to 15 fractions. Mean pain scores for these groups at the start of treatment, the end of treatment, and at 1 month follow up were 6.9, 2.4 and 2.9, and 7.3, 1.3 and 2.2 respectively.
There was little evidence for differences in pain reduction throughout the study for the various anatomical sites (Table 1) except for the cases with rib metastases. Since there were only 7 of these patients, these differences were regarded as of no statistical consequence.
DISCUSSION
An overall QA/QI program is of particular value in community RO centers. Monitoring of pain control should be a priority in such programs. Inadequate pain management continues to be a critical issue worldwide, in general, and specifically for cancer patients who are living longer following the evolution of effective, newer treatments, but often with the resulting genesis of more widespread disease. The problem of inadequate pain control may often result from multiple factors including a mixture of patient, system, and care provider barriers (8, 16–18). In particular, barriers concerning care providers have been shown to result from a lack of opportunities to learn pain assessment and management techniques and a failure of the healthcare environment to promote attitudes that provide optimal pain control (6, 10, 13, 19). Not the least of these issues has been the failure, in free standing RO departments outside the major hospital systems to adopt pain as a 5th vital sign.
The lack of attention to palliative irradiation is exemplified by a paucity of presentations accepted at the annual American Society of Therapeutic Radiology meetings as has been noted previously (14). The most marked improvement in pain control has been demonstrated when interventions include daily assessment, patient education, and/or treatment algorithms for physicians (5, 20–23). In the radiation oncology setting, patients receive daily treatments during weekdays, and although there has been a move towards shorter dose/fractionation schemes, substantial numbers of these patients are potentially available for daily pain assessment over 5–10 fractions during a one- to two-week period (4). Our data showed a significant improvement by day 1 and 2, probably due to optimization of analgesia at the time of the pre-treatment assessment. Although the pain collection form allowed for a continuous record of changes in narcotic use, this data was collected too sporadically to be analyzed effectively. As a result we cannot rule out the possibility of a placebo effect, or of an early palliative response to EBRT. The latter is unlikely in view of our early experience with the program and those of three other ROCOG centers which have tried to repeat the study (Andrade and Proctor personal observations 2004–6). It should be noted that placebo effects in this setting are both side effect and cost free.
It is unlikely that the inadequate pain control observed initially, after a pain management program was introduced, would have been apparent without auditing the results as a QA initiative, or that a successful resolution of the perceived inadequate pain control could have been accomplished without continuous review as a QI initiative.
There has been increasing interest in using an “industrial style” approach to improving medical care and several successes have been published, including at least one Radiation Oncology initiative (24–26). Although we were not aware of the “Toyota system” at the time of the initial study, the current study represents another example of how the detailed “evaluation” of a “process” can result in incremental changes towards improvement in some aspects of medical care.
Pain management has traditionally been the responsibility of nurses and doctors but this proved to be impracticable on a daily basis in our clinic, and presumably in most other RO clinics, without requiring the patient to have a formal and potentially time consuming daily appointment. The extra time and effort, while potentially worthwhile, can disrupt a busy clinic. Happily the radiation therapists agreed to collect the daily pain scores and refer the patients back to the clinic when necessary.
Although at the time of the current study, the approach had been in place for several years, the collection rate (87%) was still not as good as intended. The time taken to actually to obtain a pain score from a properly educated patient and record it in the chart is around 5–10 seconds so that the total data collection time for an entire course of treatment (10 fractions) is around 1–3 minutes.
The deterioration in pain control a month out from completion of treatment was disappointing but complete relief rates at the end of treatment are generally reported to be between 65% and 85% (27), while those at 1 month are between 45% to 65 % (4).
This pain program was extended as a Quality Improvement initiative, to a group of 4 RO centers participating with Jameson in a Cancer Disparities Research Partnerships Program (CDRP) funded by the NCI. The evaluation of the program and adoption processes is presently being considered by these facilities.
CONCLUSIONS
In conclusion, the use of a simple and time conserving daily pain assessment approach by radiation therapists was associated with prompt medical intervention and a rapid and effective control of bone pain during the first 2 days for patients during the radiation treatment course. A team approach is essential and, the therapists’ role was vital here, although ordinarily this isn’t their responsibility.
Acknowledgements
We thank all the Jameson Radiation Oncology Department staff for their support. This effort was partially funded by NCI Cancer Research Disparities Program Grant (U56CA105486).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Notification
All authors have read and approved the final version of this manuscript, all believe that the information presented is true and correct, and all are willing to take public responsibility for the manuscript. None of the co-authors have any conflicts of interest.
REFERENCES
- 1.Jacox AK, Carr DB, Payne R. Preface: policy issues related to clinical practice guidelines. J Pain Symptom Manage. 1994;9(3):143–145. doi: 10.1016/0885-3924(94)90122-8. [DOI] [PubMed] [Google Scholar]
- 2.Janjan N. Do we need to improve pain management in the radiation oncology department? Nat Clin Prract Oncol. 2005;2(3):130–131. doi: 10.1038/ncponc0111. [DOI] [PubMed] [Google Scholar]
- 3.Pignon T, Fernandez L, Ayasso S, et al. Impact of radiation oncology practice on pain: a cross-sectional survey. Int J Radiat Oncol Biol Phys. 2004;60(4):1204–1210. doi: 10.1016/j.ijrobp.2004.04.040. [DOI] [PubMed] [Google Scholar]
- 4.Arcangeli G, Giovinazzo G, Saracino B, et al. Radiation therapy in the management of symptomatic bone metastases: the effect of total dose and histology on pain relief and response duration. Int J Radiat Oncol Biol Phys. 1998;42(5):1119–1126. doi: 10.1016/s0360-3016(98)00264-8. [DOI] [PubMed] [Google Scholar]
- 5.Vallieres I, Aubin M, Blondeau L, et al. Effectiveness of a clinical intervention in improving pain control in outpatients with cancer treated by radiation therapy. Int J Radiat Oncol Biol Phys. 2006;66(1):234–237. doi: 10.1016/j.ijrobp.2005.12.057. [DOI] [PubMed] [Google Scholar]
- 6.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330(9):592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 7.Simone CB, 2nd, Vapiwala N, Hampshire MK, et al. Internet-based survey evaluating use of pain medications and attitudes of radiation oncology patients toward pain intervention. Int J Radiat Oncol Biol Phys. 2008;72(1):127–133. doi: 10.1016/j.ijrobp.2008.03.071. [DOI] [PubMed] [Google Scholar]
- 8.Mortimer JE, Bartlett NL. Assessment of knowledge about cancer pain management by physicians in training. J Pain Symptom Manage. 1997;14(1):21–28. doi: 10.1016/S0885-3924(97)00002-X. [DOI] [PubMed] [Google Scholar]
- 9.Merboth MK, Barnason S. Managing pain: the fifth vital sign. Nurs Clin North Am. 2000;35(2):375–383. [PubMed] [Google Scholar]
- 10.Cleeland CS, Janjan NA, Scott CB, et al. Cancer pain management by radiotherapists: a survey of radiation therapy oncology group physicians. Int J Radiat Oncol Biol Phys. 2000;47(1):203–208. doi: 10.1016/s0360-3016(99)00276-x. [DOI] [PubMed] [Google Scholar]
- 11.Janjan NA, Martin CG, Payne R, et al. Teaching cancer pain management: durability of educational effects of a role model program. Cancer. 1996;77(5):996–1001. [PubMed] [Google Scholar]
- 12.Janjan NA, Weissman DE, Pahule A. Improved pain management with daily nursing intervention during radiation therapy for head and neck carcinoma. Int J Radiat Oncol Biol Phys. 1992;23(3):647–652. doi: 10.1016/0360-3016(92)90024-c. [DOI] [PubMed] [Google Scholar]
- 13.Lasch K, Greenhill A, Wilkes G, et al. Why study pain? A qualitative analysis of medical and nursing faculty and students' knowledge of and attitudes to cancer pain management. J Palliat Med. 2002 Feb;5(1):57–71. doi: 10.1089/10966210252785024. [DOI] [PubMed] [Google Scholar]
- 14.Barnes EA, Palmer JL, Bruera E. Prevalence of symptom control and palliative care abstracts presented at the Annual Meeting of the American Society for Therapeutic Radiology and Oncology. Int J Radiat Oncol Biol Phys. 2002;54(1):211–214. doi: 10.1016/s0360-3016(02)02919-x. [DOI] [PubMed] [Google Scholar]
- 15.Azevedo São Leão Ferreira K, Kimura M, Jacobsen Teixeira M. The WHO analgesic ladder for cancer pain control, twenty years of use. How much pain relief does one get from using it? Support Care Cancer. 2006;14(11):1086–1093. doi: 10.1007/s00520-006-0086-x. [DOI] [PubMed] [Google Scholar]
- 16.Cleeland CS, Gonin R, Baez L, et al. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med. 1997;127(9):813–816. doi: 10.7326/0003-4819-127-9-199711010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Brekken SA, Sheets V. Pain management: a regulatory issue. Nurs Adm Q. 2008;32(4):288–295. doi: 10.1097/01.NAQ.0000336725.03065.44. [DOI] [PubMed] [Google Scholar]
- 18.Xue Y, Schulman-Green D, Czaplinski C, et al. Pain attitudes and knowledge among RNs, pharmacists, and physicians on an inpatient oncology service. Clin J Oncol Nurs. 2007;11(5):687–695. doi: 10.1188/07.cjon.687-695. [DOI] [PubMed] [Google Scholar]
- 19.Von Roenn JH, Cleeland CS, Gonin R, et al. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med. 1993;119(2):121–126. doi: 10.7326/0003-4819-119-2-199307150-00005. [DOI] [PubMed] [Google Scholar]
- 20.Du Pen SL, Du Pen AR, Polissar N, et al. Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial. J Clin Oncol. 1999;17(1):361–370. doi: 10.1200/JCO.1999.17.1.361. [DOI] [PubMed] [Google Scholar]
- 21.Benedetti C, Brock C, Cleeland C, et al. NCCN Practice Guidelines for Cancer Pain. Oncology (Williston Park) 2000;14(11A):135–150. [PubMed] [Google Scholar]
- 22.Trowbridge R, Dugan W, Jay SJ, et al. Determining the effectiveness of a clinical-practice intervention in improving the control of pain in outpatients with cancer. Acad Med. 1997;72(9):798–800. doi: 10.1097/00001888-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Weissman DE, Abram SE, Haddox JD, et al. Educational role of cancer pain rounds. J Cancer Educ. 1989;4(2):113–116. doi: 10.1080/08858198909527983. [DOI] [PubMed] [Google Scholar]
- 24.Quality improvement guidelines for the treatment of acute pain and cancer pain. American Pain Society Quality of Care Committee. JAMA. 1995;274(23):1874–1880. doi: 10.1001/jama.1995.03530230060032. [DOI] [PubMed] [Google Scholar]
- 25.Ellerbroek NA, Brenner M, Hulick P, et al. Practice accreditation for radiation oncology: quality is reality. J Am Coll Radiol. 2006;3(10):787–792. doi: 10.1016/j.jacr.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Merrill DG. Hoffman's glasses: evidence-based medicine and the search for quality in the literature of interventional pain medicine. [see comment][erratum appears in Reg Anesth Pain Med 2004;29(1):79] Reg Anesth Pain Med. 2003;28(6):547–560. doi: 10.1016/s1098-7339(03)00234-7. [DOI] [PubMed] [Google Scholar]
- 27.Wu JS, Monk G, Clark T, et al. Palliative radiotherapy improves pain and reduces functional interference in patients with painful bone metastases: a quality assurance study. Clin Oncol (R Coll Radiol) 2006;18(7):539–544. doi: 10.1016/j.clon.2006.05.003. [DOI] [PubMed] [Google Scholar]