Abstract
BACKGROUND
Trans abdominal cervicoisthmic cerclage is a procedure carried out to increase the fetal salvage rates in women who are poor candidates for the more usual procedure of transvaginal cerclage or for those with previously failed vaginal procedures. Although several modifications have been applied to the original procedure in an attempt to reduce the morbidity, bleeding arising from trauma to the uterine vessels during suture placement remains problematic.
CASE
Our technique involves transilluminating the uterine vessels during placement of the 5-mm-wide Mersilene (Ethicon Inc., Peterborough, Ontario, Canada) tape suture through an a vascular space above the junction of the cervix and the uterine isthmus. This obviates the need to dissector tunnel into the broad ligament. Simultaneous intra operative transvaginal ultrasonography is used to enhance high suture placement at the isthmus and monitor the fetoplacental unit. We have used this technique in a series of five women with cervical incompetence for seven pregnancies. All but one procedure resulted in live term births. There were no major complications.
CONCLUSION
Simultaneous intraoperative ultrasonography and uterine vessel transillumination simplified suture placement during abdominal cerclage, and reduced the amount of dissection and bleeding.
An abdominal approach to cerclage placement around the uterine isthmus is occasionally indicated in a subset of patients who are poor candidates for transvaginal cerclage. This includes patients with extremely short, congenitally deformed, deeply lacerated, deformed or scarred cervices from previous cervical surgery, those in whose cases the vaginal approach is not feasible, and those with failed transvaginal cerclage procedures. Since the introduction of second-trimester transabdominal isthmic cerclage by Benson and Durfee in 1965,1 several modifications2–5 have been made to the technique. The changes have been designed to avoid trauma to the uterine vessels and their branches during needle insertion for suture placement. Novy3 reported reduced blood loss with elevation of the uterus out of the pelvis by an assistant to allow visualization and manual retraction of the uterine vessels. However, excessive uterine manipulation may precipitate uterine activity and abortion. In an effort to avoid trauma to the uterine vessels, we developed the technique of transillumination of the uterine vessels during lateral isthmic suture placement combined with simultaneous intraoperative transvaginal ultrasonography. Here we describe the enhanced suture placement technique at abdominal cerclage and report our experience with this new technique.
CASE
All women are assessed preoperatively by transvaginal ultrasonography to determine fetal viability and placental localization, exclude major anomalies, and measure the cervical length. Transabdominal cervicoisthmic cerclage is performed at 10–12 weeks’ gestation using a regional or general anesthesia and with the patient in the dorsal lithotomy position. The abdomen is opened through a subumbilical midline or Pfannenstiel incision and the bladder peritoneal fold is dissected off the anterior lower uterine segment. Continuous intraoperative transvaginal ultrasonographic monitoring (Advanced Technology Laboratories, Bothell, WA, with a 5.0-MHz vaginal transducer) of the fetal heart rate and uterine contractions that may occur is commenced. During the sonographic examination, the boundary between the amniotic cavity, cervix, and isthmus is sharply contrasted by sterile water introduced into the uterovesical space. Ultrasonography and the tip of a Kelly clamp are used to demarcate the internal cervical os and demarcate the site of anchoring the suture anteriorly at the isthmus. A bite is taken through the vesicocervical fascia anteriorly in the midline at this level using a 5-mm-wide tape (Mersiline RS-21; Ethicon Inc., Peterborough, Ontario, Canada) on a round-bodied needle. With the uterus gently retracted superiorly by an assistant, a laparoscope with attached light source is introduced through the abdominal incision by an assistant and placed anteriorly against the broad ligament. It is then used to transilluminate the uterine vessels and its branches, thus permitting clear visualization of the vessels, isthmus, and uterosacral ligaments (Figure 1). The suture is introduced anteroposteriorly through an a vascular area of the paracervicalt issue medial to the vessels, and at the level of the uterine isthmus, above the confluence and insertion of both uterosacral ligaments, taking care to avoid bleeding from going into the substance of the cervix. The tip of the needle is visually guided through the soft tissues to pierce the posterior leaf of the broad ligament and retrieved posteriorly, with gentle elevation of the uterus by an assistant. The same procedure is performed on the opposite side with the needle entering in an anteroposterior direction above the uterosacral ligaments, while the uterine vessels are transilluminated. Anchoring bites are taken through the uterosacral ligament on each side. The Mersilene tape is laid flat and the knot is tied posteriorly. Anteriorly, the suture is covered by loose peritoneal folds. Continuous ultrasonography is used to monitor fetal activity and uterine blood flow during the procedure and estimate the final cervical length at the conclusion of the procedure (Figure 2). Pre- and postoperatively, indomethacin rectal suppositories are used for uterine quiescence. During the procedure and postoperatively the patients receive prophylactic antibiotics.
Figure 1.
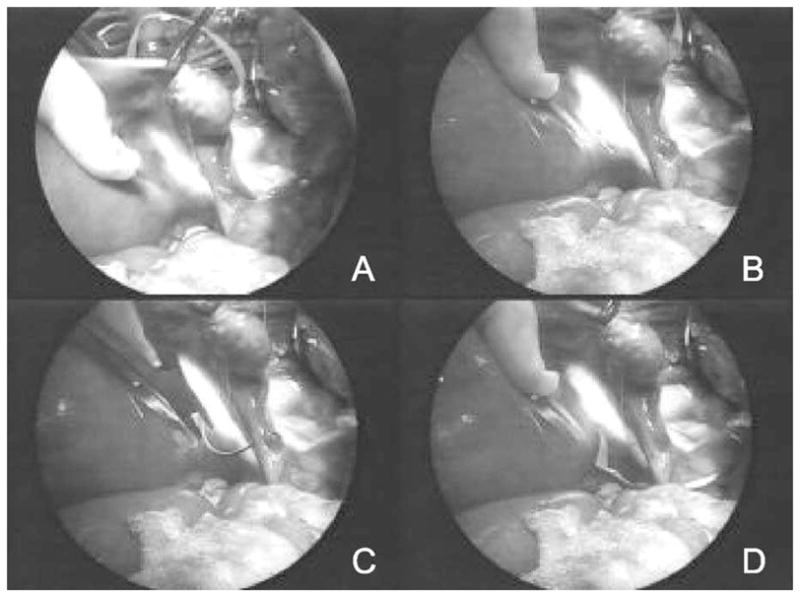
Transillumination of the broad ligament and Mersilene tape (A, B). This facilitates passing the needle and Mersilene tape through an a vascular area of the paracervical tissue adjacent to the isthmus (C). The needle and suture are visually guided through the posterior leaf of the broad ligament (D).
Figure 2.
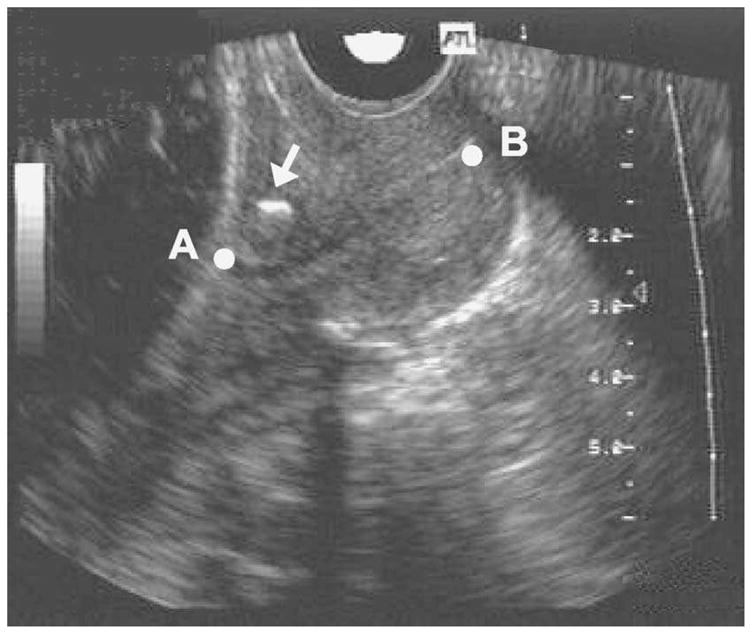
Intraoperative transvaginal ultrasound showing prominent echogenic suture knot (arrow) and cervical length after cerclage. A = amniotic membranes; B = external cervical os.
We have used this technique on five women for seven pregnancies. The women had clinical histories of failed vaginal cerclage or cervical conization, and underwent transabdominal isthmic cerclage between 12 and 14 weeks’ gestation. The mean age of the women was 30.2 years (Table 1). The fetal salvage rate from the previous 11 pregnancies was 18%, and it increased to 86% after abdominal cerclage. The mean operative time for the complete operation was 61.3 minutes (95% confidence interval [CI] 45.0, 62.4), and the mean blood loss, 120 mL (95% CI 75.3, 130.0). All patients were discharged within 4–8 days after surgery. The length and status of the cervix were assessed biweekly initially with transvaginal and, later, transabdominal ultrasonography. Four of our five patients delivered live-born infants by elective cesarean at 37 to 38 weeks. We left the Mersilene sutures during the initial cesarean delivery in two patients (patient 3 and patient 4) for use in their next pregnancies, and they were removed at the next cesarean delivery. One patient with twins went into preterm labor at 20 weeks (7 weeks post operatively). To colysis was unsuccessful, and she had laparotomy for suture removal and delivered twins who died of extreme prematurity.
Table 1.
Patient Characteristics and Outcomes
| Patient | Age (y) | Gravidity | Parity | Surgical history | Cervical length (pre- and postoperative [cm]) | Outcome |
|---|---|---|---|---|---|---|
| 1 | 26 | 3 | 2 | Lazer conization of cervix; failed vaginal cerclage | 1.5, 4.0 | Preterm delivery of nonviable twins |
| 2 | 29 | 2 | 1 | Wide cervical conization × 2 | 1.0, 3.0 | Live female |
| 3 (1)* | 32 | 4 | 1 | Failed vaginal cerclage | 2.0, 4.0 | Twins (female stillborn fetus and live male) |
| 3 (2)† | 35 | 5 | 2 | – | Live female | |
| 4 (1)* | 32 | 3 | 1 | Failed vaginal cerclage; classic cesarean delivery | 3.5, 4.9 | Live female |
| 4 (2)† | 35 | 4 | 2 | – | Live female | |
| 5 | 30 | 2 | 1 | Preterm delivery of nonviable twins | 2.5, 4.0 | Live male |
First pregnancy with one abdominal cerclage.
Second pregnancy with one abdominal cerclage.
COMMENT
The risk of excessive bleeding during suture placement at transabdominal cervical isthmic cerclage poses a problem for surgeons. In their earlier series, Novy2 and colleagues reported “serious operative bleeding” in two of 16 patients, whereas Herron and Parer5 reported an average blood loss of 500 mL with four operations, and three patients required transfusion. To reduce this complication, several modifications have been introduced, including laparoscopic cervicoisthmic cerclage as an interval procedure.6 Our technique of using fiberoptic lighting to illuminate the uterine vessels reduces the risk of vascular injury and operative blood loss during suture placement. Adjunctive use of vaginal ultrasonography also facilitates high suture placement and monitoring of the fetal placental unit. These modifications emphasize improvements in the surgical techniques, which offer potential benefits for patients undergoing second-trimester abdominal cervical isthmic cerclage. The technique provides a unique opportunity for the surgeon to visually identify vessels and other soft tissues in front of the penetrating needle. Transillumination helps the surgeon to avoid dissecting into the highly vascular broad ligament and reduce the risk of vascular puncture and bleeding. With color Doppler sonography, vessels were easily identified, thereby avoiding their inadvertent occlusion by the Mersilene suture. In addition, adjunctive use of transvaginal ultrasonography facilitates high suture placement at the isthmus and reduces the risk of suture slippage due to low placement. As well, being able to estimate the desired final length of the cervix immediately after tying the suture is important to the success of the procedure. Rarely, a reinforcing suture above the first may be required if the ultrasound measurement shows the final length of the cervix to be inadequate, further enhancing the success of this procedure.
Despite its advantages over other methods of isthmic cerclage, there are some practical limitations to our technique. For instance, there are often many small veins apposed to the isthmus and difficult to avoid unless pinched between the thumb and forefinger and drawn laterally. Bleeding from puncture to these small veins is easily controlled with sutures. As well, our preference for tying the Mersilene suture posteriorly requires some retraction of the uterus to accomplish, there by subjecting the uterus to manipulation. In rare cases when there is funneling of the membranes into an effaced or previously amputated cervix, it is obvious that vaginal sonography would need to be used with extreme caution to avoid rupture of the membranes. Overall, our results for prolonging pregnancy and improving fetal salvage rates are comparable to those in other published works.3,6–8 Our approach offers an option with less morbidity from bleeding than the traditional procedure of abdominal cerclage. Indeed, it is particularly advantageous when the patient has pelvic adhesions or increased varicosity of pelvic vessels. Because tunneling into this highly vascular area is avoided, the potential for ureteral injury is also reduced.
In conclusion, our experience suggests that transillumination of the uterine vessels clearly improves visualization of the uterine vessels during cervicoisthmic suture placement. In addition, high suture placement at the isthmus may also be improved by ultrasonographic guidance. Further experience with our technique will be needed to confirm these benefits.
Acknowledgments
Source of funding: University of Saskatchewan Department Head Research Support Fund.
References
- 1.Benson RC, Durfee R. Transabdominal cervicouterine cerclage during pregnancy for the treatment of cervical incompetence. Obstet Gynecol. 1965;25:145–55. [PubMed] [Google Scholar]
- 2.Novy MJ. Transabdominal cervicoisthmic cerclage for the management of repetitive abortion and premature delivery. Am J Obstet Gynecol. 1982;143:44–54. doi: 10.1016/0002-9378(82)90682-2. [DOI] [PubMed] [Google Scholar]
- 3.Novy MJ. Transabdominal cervicoisthmic cerclage: A reappraisal 25 years after its introduction. Am J Obstet Gynecol. 1991;164:1635–41. doi: 10.1016/0002-9378(91)91448-6. [DOI] [PubMed] [Google Scholar]
- 4.Craig S, Fliegner JR. Treatment of cervicalin competence by transabdominal cervicoisthmic cerclage. Aust N Z J Obstet Gynaecol. 1997;37:407–11. doi: 10.1111/j.1479-828x.1997.tb02448.x. [DOI] [PubMed] [Google Scholar]
- 5.Herron MA, Parer JT. Transabdominal cerclage for fetal wastage due to cervical incompetence. Obstet Gynecol. 1988;71:865–8. [PubMed] [Google Scholar]
- 6.Lesser KB, Childers JM, Surwit EA. Transabdominal cerclage: A laparoscopic approach. Obstet Gynecol. 1998;91:855–6. doi: 10.1016/s0029-7844(97)00655-8. [DOI] [PubMed] [Google Scholar]
- 7.Davis G, Berghella V, Talucci M, Wapner RJ. Patients with a prior failed transvaginal cerclage: A comparison of obstetric outcomes with either transabdominal or transvaginal cerclage. Am J Obstet Gynecol. 2000;183:836–9. doi: 10.1067/mob.2000.108837. [DOI] [PubMed] [Google Scholar]
- 8.Turnquest MA, Britton KA, Brown HL. Outcome of patients undergoing transabdominal cerclage: A descriptive study. J Matern Fetal Med. 1999;8:225–7. doi: 10.1002/(SICI)1520-6661(199909/10)8:5<225::AID-MFM5>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]


