Abstract
Background
Little is known about isolated systolic hypertension (ISH) in younger adults. We examined the prevalence and determinants of ISH in this age group using the 1999-2004 National Health and Nutrition Examination Surveys (NHANES) and made comparisons using data from NHANES III (1988-1994).
Methods
5,685 adults aged 18-39 years and not on antihypertensive medications were analyzed. Prevalence estimates of ISH and potential risk factors were estimated by age and sex. For comparison of prevalence estimates with published reports of NHANES III data, age cutoffs (18-24, 25-34, and 35-44) by sex were also employed. A multivariate logistic regression model tested independent determinants of ISH.
Results
ISH in young adults had a higher prevalence than systolic/diastolic hypertension (1.57 ± 0.23% vs. 0.93 ± 0.18%). ISH prevalence increased within the last decade particularly for males for each respective age category [males (0.8% vs. 2.2%, 1.3% vs. 2.4%, 1.3% vs. 2.4%), females (0.0% vs. 0.3%, 0.1% vs. 0.7%, 1.7% vs. 1.8%)]. On multivariate analysis, obesity (OR: 2.68, 95% CI: (1.06, 6.77), male sex (OR: 2.19, 95% CI: (1.10, 4.37), education level less than high school (OR: 2.98, 95% CI: (1.10, 8.06), and current smoking (OR: 2.06, 95% CI: (1.03, 4.11) were characteristics independently associated with higher odds of ISH among young adults. Relative increases in prevalence between the surveys were noted for current smoking (24.3% vs. 51.5%), obesity (33.9% vs. 42.7%) and low educational level (18.4% vs. 38.6%).
Conclusions
ISH among young adults is increasing in prevalence, and is more common than systolic/diastolic hypertension. Obesity, smoking, and low socioeconomic status appear to be important determinants of ISH among young adults and have all increased over the last decade.
Keywords: systolic hypertension, blood pressure, young adults, epidemiology, United States
Isolated systolic hypertension (ISH), defined as systolic blood pressure (SBP) ≥140 mm Hg and diastolic blood pressure (DBP) <90 mm Hg,1 is often characterized as a phenomenon of aging because SBP, unlike DBP, increases with age in response to increasing arterial stiffness and losses in arterial compliance particularly after the age of 40.2, 3 In younger subjects there has been an increasing interest in the occurrence of ISH, which is thought to have a different mechanism than ISH of the elderly.4 Risk factors for ISH may differ between young adults and the elderly, but findings from previous studies examining this question are inconclusive. The onset of hypertension during early adulthood warrants particular concern as even slight elevations in SBP during early adulthood increase one’s risk for further cardiovascular disease (CVD) morbidity in later life.1, 5 Furthermore, studies of hypertension among young adults have found associations with structural changes in the heart including increases in left ventricular wall thickness, left ventricular mass and higher prevalence of left ventricular hypertrophy.6
Prior prevalence estimates of ISH in adults 40 years old or younger vary dramatically, ranging from less than 2%,7, 8 to over 16%9 in cohorts limited to males. Estimates for the prevalence of ISH among younger women, although limited, suggest that ISH may be less common among females in this age group.7, 10, 11 Moreover, the use of different definitions for ISH (160/95mmHg, 160/90mmHg, 140/90mmHg) and inconsistent age cutoffs between studies have not only limited available data on overall ISH prevalence, but also make comparison across studies difficult. The existing prevalence estimates of ISH in the U.S. young adult population are based on the third National Health and Nutrition Examination Survey (NHANES III, 1988-1994)2, 10, 12 and do not reflect changes in the prevalence or distribution of correlated risk factors that occurred during the last decade. While ISH prevalence among young adults may actually be more common in more recent NHANES surveys, updated prevalence estimates by hypertensive subtype are not available. Risk factors for ISH such as obesity have become more prevalent in the U.S. than in the international settings of similar studies (e.g. United Kingdom,11 Netherlands,9 Korea7) and would be expected to influence the prevalence of ISH in the U.S.; however, earlier U.S.-based studies have not examined the distribution of known CVD hypertension risk factors in young adults with ISH.
The availability of data from the NHANES 1999-2004 affords the opportunity to examine ISH among adults ages 18 to 39 before and after accounting for traditional and non-traditional characteristics previously shown to be associated with hypertension among older adults, such as sex, race/ethnicity, and socioeconomic status.
METHODS
Study Population
The NHANES 1999-2000, NHANES 2001-2002 and NHANES 2003-2004 (Demographic Questionnaire and Examination files) public-use data files were used for this study. These surveys assessed the health status of a nationally representative sample of the civilian non-institutionalized U.S. population, selected through a stratified multistage probability sampling design. Full descriptions of the sample design in NHANES 1999-2000, NHANES 2001-2002 and NHANES 2003 -2004 have been reported elsewhere.13
Our analysis pools six years (1999-2004) of NHANES data, which is comparable to NHANES III (1988-1994). The stratified, multistage probability cluster sampling design used in NHANES 1999-2000 was very similar to the ones used in NHANES 2001-2002 and NHANES 2003 -2004. For the six-year survey estimate, a six-year weight was created by assigning 2/3 of the four-year weight for 1999-2002 and by assigning 1/3 of the two-year weight for 2003-2004 in accordance with the NCHS Analytic and Reporting Guidelines.14
NHANES 1999-2000, NHANES 2001-2002 and NHANES 2003-2004 examined a total of 9,965, 11,039 and 10,122 persons, respectively, one month of age or older (85 years of age was adjudicated to persons 85 years of age or older). Out of these, 5,733, 6,327 and 5,926 persons were 17 years of age or older in the NHANES 1999-2000, NHANES 2001-2002 and NHANES 2003-2004, respectively, for a total of 17,986. Of 7,091 adults aged 18 to 39 years, 734 individuals with incomplete SBP or DBP measurements and 123 individuals who reported antihypertensive medication use were excluded from the final analysis. Treated hypertensives were excluded from our analysis since once on treatment accurate classification of hypertension subtypes is not possible. Individuals not belonging to the major racial/ethnic categories of non-Hispanic white, non-Hispanic black, or Mexican-American (n=549) were also excluded, yielding a final sample of 5,685. To analyze differences in the prevalence of ISH and distribution of CVD risk factors over time, the 1999-2004 data were compared to NHANES III using the same population inclusion and exclusion criteria.
Blood Pressure and Hypertension Assessment
BP measurements were collected by trained physicians in accordance with the recommendations of the American Heart Association Human Blood Pressure Determination by Sphygmomanometers.15 Mid-arm circumference was measured for each participant prior to BP measurement for appropriate cuff size selection. Three and sometimes four consecutive right arm BP determinations were taken using a mercury sphygmomanometer after the subject had rested quietly in a sitting position for 5 minutes and the examiner determined the maximum inflation level.16 The cuff was deflated at a constant rate of 2 mm/s, and Korotkoff I and V sounds were obtained for the determination of SBP and DBP, respectively.17
The SBP and DBP values quoted in this study represent averages reported to the examinee. Consistent with World Health Organization conventions (1999) and the seventh Joint National Commission guidelines18, hypertension was defined as SBP ≥140mmHg or DBP ≥ 90mmHg. Hypertension subtypes in the analysis include: ISH, defined as SBP ≥140mmHg and DBP <90mmHg; isolated diastolic hypertension (IDH), defined as SBP <140mmHg and DBP ≥90mmHg; and systolic-diastolic hypertension (SDH), defined as SBP ≥140 mmHg and DBP ≥90 mmHg.
Baseline examination
Race/ethnicity was self-reported in the NHANES Demographic component. The analytic sample includes Mexican Americans, non-Hispanic whites, and non-Hispanic blacks. The results for the “other race – including multiracial” and “other Hispanic” groups were not included in the total sample analyses because of the heterogeneity of these categories. Three income variables were created using reported total family income: $19,999 or less, $20,000 - $34,999, and $35,000 or more. Sex and education categories follow the response choices in the Demographic questionnaire. Insured participants reported having health insurance or other type of health care plan at the time of the survey.
The NHANES included questions about smoking, alcohol consumption, and physical activity. Smoking status was derived from two questions in both surveys, “Do you smoke cigarettes now?” and “Have you smoked at least 100 cigarettes in your entire life?” Smoking status was defined as current smokers (subjects who answered “Yes” to both questions), former smokers (subjects who answered “No” to the first question and “Yes” to the second question), and never smokers (subjects who answered “No” to both questions). Alcohol status was dichotomized based on the question, “In any one year, have you had at least 12 drinks of any type of alcoholic beverage?” Individuals identified as physically active answered “Yes” to the question, “Over the past 30 days, did you do any vigorous activities for at least 10 minutes that caused heavy sweating, or large increases in breathing or heart rate?” Body Mass Index (BMI) was categorized in accordance with the National Institutes of Health Guidelines on Overweight and Obesity.19 Non-overweight individuals are those with a BMI < 25 kg/m2; individuals with a BMI between 25 kg/m2 and 30 kg/m2 are overweight, while individuals with a BMI of 30 kg/m2 or greater are obese. High total cholesterol (≥240 mg/dL) was defined in accordance with the National Institutes of Health Report on the Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.19
Data on diabetes and health insurance were obtained through self-report. To determine diabetes status, participants were dichotomized according to the question, “Have you ever been told by a doctor that you have diabetes?”
Statistical Analysis
Crude prevalences of ISH, IDH, and SDH are presented. A separate analysis examined hypertension subtype prevalence by age group and BMI category. Subjects with ISH were compared to individuals belonging to other hypertensive subtypes by CVD risk factors and other sociodemographic and physiologic characteristics. Within-group comparisons among those with ISH by sex were also performed. NHANES III data were also analyzed to contrast CVD risk factor distributions among those with ISH to individuals with ISH in NHANES 1999-2004. We present average values of BP indices including SBP, DBP, and pulse pressure (PP) to characterize ISH in the study population. To determine significant differences, Chi-square (discrete variables) and t-tests (continuous variables) were used.
Multiple logistic regression was used to estimate the strength of the association of selected characteristics and hypertension risk factors with the prevalence of ISH. Although neither physical activity level nor family history of hypertension exhibited a univariate association with ISH, they were included in our multiple regression model based on previous research showing their independent association with hypertension. Because some of the risk factors and the outcomes are differently distributed by sex, interactions between sex and age, race/ethnicity, and BMI were tested in the final model. The number of records included in the analyses varied depending on the covariates included in the model.
Data management procedures were carried out with SAS20 and the statistical analyses were conducted using SUDAAN to generate population estimates based on NHANES sampling weights.21 SUDAAN takes into account the complex sampling design yielding unbiased standard error estimates. Sample sizes included in Table 1 were unweighted. However, estimates for means, proportions, standard errors, and ORs with their 95 percent (%) confidence intervals (CI) presented in Tables 1, 2 and 3 were weighted. For all analyses, a p value of ≤ 0.05 was considered statistically significant.
Table 1.
Prevalence of hypertension subtypes by gender, age and BMI among adults ages 18-39, NHANES 1999-2004
| ISH | IDH | SDH | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Total | Males | Females | Total | Males | Females | Total | |
| Overall | 2.23 ± 0.39* | 0.92 ± 0.21 | 1.57 ± 0.23 | 4.09 ± 0.55* | 1.25 ± 0.29 | 2.66 ± 0.36 | 1.42 ± 0.33* | 0.46 ± 0.16 | 0.93 ± 0.18 |
| Age (years) | |||||||||
| 18-29 | 2.48 ± 0.54* | 0.49 ± 0.22 | 1.49 ± 0.32 | 2.32 ± 0.55* | 0.71 ± 0.24 | 1.52 ± 0.34 | 0.93 ± 0.40 | 0.16 ± 0.15 | 0.55 ± 0.15 |
| 30-39 | 1.94 ± 0.49 | 1.38 ± 0.36 | 1.65 ± 0.32 | 6.11 ± 1.02* | 1.84 ± 0.50 | 3.94 ± 0.62 | 1.97 ± 0.56 | 0.78 ± 0.30 | 1.37 ± 0.35 |
| BMI (kg/m2) | |||||||||
| < 25 | 1.13 ± 0.35 | 0.64 ± 0.33 | 0.87 ± 0.23 | 1.36 ± 0.48 | 0.95 ± 0.34 | 1.14 ± 0.33 | 0.62 ± 0.23 | 0.23 ± 0.16 | 0.41 ± 0.15 |
| 25 - 30 | 2.38 ± 0.60* | 0.70 ± 0.30 | 1.68 ± 0.39 | 3.84 ± 0.85* | 0.98 ± 0.60 | 2.65 ± 0.61 | 1.08 ± 0.60 | 0.96 ± 0.54 | 1.03 ± 0.42 |
| > 30 | 3.87 ± 1.20* | 1.62 ± 0.55 | 2.62 ± 0.71 | 9.79 ± 1.90* | 2.07 ± 0.63 | 5.49 ± 1.03 | 3.00 ± 1.12* | 0.14 ± 0.12 | 1.41 ± 0.52 |
Data are prevalences ± SE. Statistics are weighted to population level using weights provided with the NHANES data; sample size is unweighted.
P ≤ 0.05 .
NHANES, National Health and Nutrition Examination Survey; ISH, isolated systolic hypertension; IDH, isolated diastolic hypertension; SDH, systolic-diastolic hypertension; BMI, body mass index.
Table 2.
Distribution of selected characteristics and cardiovascular disease risk factors among adults ages 18-39 by hypertensive subtype and overall: NHANES 1999-2004
| Characteristic | ISH (n=90) |
IDH (n= 111) |
SDH (n= 38) |
Normotensive (n= 5,446 ) |
Total (n =5,685) |
p value† | p value‡ |
|---|---|---|---|---|---|---|---|
| Mean ± SE | Mean ± SE | Mean ± SE | Mean ± SE | Mean ± SE | |||
| Age (years) | 29.5 ± 0.84 | 32.3 (0.76) | 31.6 (0.98) | 28.5 +/− 0.16 | 28.6 ± 0.16 | 0.007 | 0.24 |
| Weight (kg) | 87.4 ± 3.25 | 93.2 (3.11) | 99.5 (9.14) | 77.8 +/− 0.40 | 78.6 ± 0.39 | 0.11 | 0.003 |
| Height (cm) | 172.1 ± 1.09 | 173.5 (0.94) | 173.9 (1.33) | 170.2 +/− 0.16 | 170.3 ± 0.17 | 0.28 | 0.09 |
| BMI (kg/m2) | 29.5 ± 1.00 | 30.9 (0.82) | 32.3 (2.69) | 26.8 +/− 0.13 | 26.9 ± 0.12 | 0.21 | 0.008 |
| Pulse Rate (bpm) | 74.7 ± 1.62 | 78.5 (1.25) | 77.2 (3.77) | 73.4 ± 0.28 | 73.6 ± 0.28 | 0.06 | 0.44 |
| Total Cholesterol (mg/dL) | 198.4 ± 6.45 | 206.6 (4.85) | 192.8 (5.96) | 187.7 ± 0.82 | 188.4 ± 0.75 | 0.55 | 0.11 |
| SBP (mm Hg) | 144.2 ± 0.45 | 128.6 (0.59) | 147.7 (1.97) | 112.5 ± 0.27 | 113.7 ± 0.31 | <0.001 | <0.001 |
| DBP (mm Hg) | 76.2 ± 1.26 | 92.9 (0.39) | 99.3 (1.21) | 68.2 ± 0.23 | 69.3 ± 0.26 | <0.001 | <0.001 |
| Pulse Pressure (mm Hg) | 68.0 ± 1.40 | 35.6 (0.67) | 48.4 (1.31) | 44.3 ± 0.32 | 44.5 ± 0.33 | <0.001 | <0.001 |
| % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | |||
|---|---|---|---|---|---|---|---|
| Age (years) | 0.02 | 0.65 | |||||
| 18 - 29 | 50.6 (6.99) | 29.9 (5.44) | 31.2 (8.04) | 53.7 (1.15) | 52.8 (1.11) | ||
| 30 - 39 | 49.4 (6.99) | 70.1 (5.44) | 68.8 (8.04) | 46.3 (1.15) | 47.2 (1.11) | ||
| Gender | 0.38 | <0.001 | |||||
| Male | 70.3 (5.54) | 76.0 (4.03) | 75.4 (8.15) | 48.2 (0.80) | 49.56 (0.79) | ||
| Female | 29.7 (5.54) | 24.0 (4.03) | 24.6 (8.15) | 51.8 (0.80) | 50.44 (0.79) | ||
| Race/Ethnicity | 0.05 | 0.08 | |||||
| Non-Hispanic White | 57.2 (7.34) | 73.5 (4.50) | 73.5 (7.64) | 73.5 (1.49) | 73.2 (1.53) | ||
| Non-Hispanic Black | 26.7 (5.02) | 16.6 (3.46) | 18.4 (6.24) | 13.5 (1.18) | 13.8 (1.19) | ||
| Mexican American | 16.1 (4.61) | 9.9 (2.60) | 8.1 (2.91) | 13.0 (1.27) | 12.9 (1.28) | ||
| Country of Birth | 0.46 | 0.74 | |||||
| U.S. | 88.2 (3.85) | 92.0 (2.66) | 90.6 (4.58) | 86.9 (1.03) | 87.2 (1.01) | ||
| Outside US | 11.8 (3.85) | 8.0 (2.66) | 9.4 (4.58) | 13.0 (1.03) | 12.8 (1.01) | ||
| Annual Household Income (in USD) | 0.04 | 0.01 | |||||
| ≤ $19,999 | 41.0 (5.75) | 21.3 (5.22) | 31.4 (11.43) | 27.5 (1.29) | 27.5 (1.34) | ||
| $20,000 - $34,999 | 18.0 (5.21) | 23.9 (3.85) | 28.6 (9.48) | 22.2 (0.97) | 22.2 (0.97) | ||
| ≥$35,000 | 40.9 (5.28) | 54.8 (5.52) | 40.0 (9.73) | 50.4 (1.52) | 50.3 (1.57) | ||
| Education Level | 0.04 | 0.002 | |||||
| < High School | 38.6 (6.74) | 21.7 (4.06) | 29.4 (10.48) | 19.3 (0.85) | 19.8 (0.82) | ||
| High School | 28.0 (5.48) | 30.3 (6.08) | 17.1 (6.63) | 27.9 (1.23) | 27.8 (1.16) | ||
| > High School | 33.4 (6.77) | 48.0 (6.89) | 53.4 (9.47) | 52.8 (1.38) | 52.4 (1.34) | ||
| Health Insurance | 0.02 | 0.003 | |||||
| Covered by health insurance | 54.6 (6.42) | 73.4 (4.27) | 74.9 (7.54) | 72.9 (1.13) | 72.7 (1.13) | ||
| Does not have health insurance | 45.4 (6.42) | 26.7 (4.27) | 25.1 (7.54) | 27.0 (1.13) | 27.3 (1.13) | ||
| Smoking Status | <0.001 | 0.001 | |||||
| Current | 51.6 (6.76) | 24.5 (4.37) | 18.3 (7.31) | 31.9 (1.26) | 31.9 (1.23) | ||
| Former | 13.4 (3.62) | 18.3 (4.49) | 26.4 (10.81) | 13.4 (0.76) | 13.7 (0.72) | ||
| Never | 35.0 (5.72) | 57.2 (5.17) | 55.3 (8.59) | 54.7 (1.33) | 54.4 (1.30) | ||
| Alcohol consumption | 0.06 | 0.33 | |||||
| ≥ 12 drinks in one year | 86.0 (3.92) | 81.1 (5.30) | 75.6 (9.29) | 77.7 (1.71) | 77.9 (1.70) | ||
| < 12 drinks during lifetime | 14.0 (3.92) | 18.9 (5.30) | 24.4 (9.29) | 22.3 (1.71) | 22.1 (1.70) | ||
| Total Cholesterol | 0.83 | 0.13 | |||||
| High (≥240 mg/dL) | 16.0 (4.14) | 19.5 (4.21) | 11.0 (6.43) | 9.4 (0.57) | 9.8 (0.57) | ||
| Normal (<240 mg/dL) | 84.0 (4.14) | 80.6 (4.21) | 88.9 (6.43) | 90.6 (0.57) | 90.2 (0.57) | ||
| Diabetic | 0.09 | 0.41 | |||||
| Yes | 0.5 (0.51) | 4.6 (2.32) | 0.3 (0.32) | 0.9 (0.18) | 1.1 (0.18) | ||
| No | 99.5 (0.51) | 95.4 (2.32) | 99.7 (0.32) | 99.0 (0.18) | 98.9 (0.18) | ||
| BMI | 0.47 | 0.003 | |||||
| < 25 | 24.9 (6.79) | 18.9 (5.37) | 21.5 (7.50) | 45.9 (1.21) | 44.6 (1.08) | ||
| 25 - 30 | 32.4 (6.42) | 29.5 (4.97) | 36.5 (11.93) | 29.9 (1.14) | 30.0 (1.06) | ||
| 30+ | 42.7 (7.83) | 51.7 (5.83) | 42.0 (11.24) | 24.2 (0.82) | 25.4 (0.79) | ||
| Physically Active | 0.33 | 0.37 | |||||
| Yes | 41.9 (5.77) | 36.7 (5.44) | 28.7 (8.11) | 47.0 (1.28) | 46.5 (1.24) | ||
| No | 58.1 (5.77) | 63.3 (5.44) | 71.3 (8.11) | 52.9 (1.28) | 53.5 (1.24) | ||
| Family History of Hypertension/Stroke | 0.13 | 0.28 | |||||
| Yes | 43.6 (7.28) | 52.8 (6.34) | 68.9 (9.59) | 36.2 (1.05) | 37.1 (1.08) | ||
| No | 56.3 (7.28) | 47.2 (6.34) | 31.2 (9.59) | 63.8 (1.05) | 62.9 (1.08) |
Source: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 1999-2004.
Note: Statistics are weighted to population level using weights provided with the NHANES data; sample size is unweighted.
P-values correspond to the t-test for continuous variables and the X2 test of independence for categorical variables.
P-values for ISH vs. Other Hypertensives (SDH + IDH)
P-values for ISH vs. Normotensives
Table 3.
Estimated unadjusted and adjusted odds ratios from logistic regressions of ISH by BMI, smoking, activity, and other characteristics for adults ages 18-39, NHANES 1999-2004
| Odds Ratio | 95% CI | Adjusted Odds Ratio |
95% CI | |
|---|---|---|---|---|
| Age (per year) | 1.02 | (0.98, 1.06) | 1.01 | (0.96, 1.06) |
| BMI (kg/m2) | ||||
| < 25 (reference) | 1.00 | 1.00 | ||
| 25 - 30 | 1.95 | (0.91, 4.18) | 1.83 | (0.78, 4.30) |
| 30+ | 3.06 | (1.31, 7.14) | 2.68 | (1.06, 6.77) |
| Smoking Status | ||||
| Current | 2.56 | (1.44, 4.53) | 2.06 | (1.03, 4.11) |
| Former | 1.52 | (0.79, 2.95) | 1.62 | (0.77, 3.42) |
| Never (reference) | 1.00 | 1.00 | ||
| Physical Activity | ||||
| Yes | 0.83 | (0.51, 1.33) | 1.26 | (0.70, 2.28) |
| No (reference) | 1.00 | 1.00 | ||
| Gender | ||||
| Male | 2.46 | (1.42, 4.28) | 2.19 | (1.10, 4.37) |
| Female (reference) | 1.00 | 1.00 | ||
| Race/Ethnicity | ||||
| Non-Hispanic White (reference) | 1.00 | 1.00 | ||
| Non-Hispanic Black | 2.52 | (1.35, 4.70) | 1.79 | (0.77, 4.17) |
| Mexican American | 1.63 | (0.78, 3.42) | 0.78 | (0.25, 2.44) |
| Annual Household Income (in USD) | ||||
| ≤ $19,999 | 1.89 | (1.21, 2.95) | 1.36 | (0.77, 2.42) |
| $20,000 - $34,999 | 1.06 | (0.51, 2.17) | 0.84 | (0.36, 1.91) |
| ≥$35,000 | 1.00 | 1.00 | ||
| Education Level | ||||
| < High School | 3.21 | (1.58, 6.52) | 2.98 | (1.10, 8.06) |
| High School | 1.62 | (0.81, 3.26) | 1.39 | (0.63, 3.10) |
| > High School (reference) | 1.00 | 1.00 | ||
| Health Insurance | ||||
| Covered by health insurance | 1.00 | 1.00 | ||
| Does not have health insurance | 2.25 | (1.36, 3.73) | 1.38 | (0.71, 2.68) |
| Family History of Hypertension/Stroke | ||||
| Yes | 1.32 | (0.75, 2.33) | 1.29 | (0.66, 2.49) |
| No | 1.00 | 1.00 |
N = 5,685. Statistics are weighted to population level using weights provided with the NHANES data; sample size is unweighted. NHANES, National Health and Nutrition Examination Survey; BMI, Body Mass Index; ISH, isolated systolic hypertension.
RESULTS
Prevalence of Hypertension Subtypes
Of the 5,685 subjects aged 18-39 in the NHANES 1999-2004 sample, 90 (1.57% ± 0.23) had blood pressure readings consistent with the clinical definition of ISH. The overall crude prevalence of ISH in the study population was 2.23% in males and 0.92% in females (p= 0.004). The overall prevalence of IDH and SDH in this population was 2.66% ± 0.36 and 0.93% ± 0.18, respectively. The prevalence of each hypertension subtype was consistently higher among males. ISH, IDH, and SDH prevalence generally rose by increasing age group and BMI, except for ISH prevalence in males, which was higher in the 18-29 age group than in the 30-39 group, and SDH prevalence in females, which fell in the BMI > 30 category. ISH was the most common form of hypertension among males ages 18 to 29 in the study population. (Table 1)
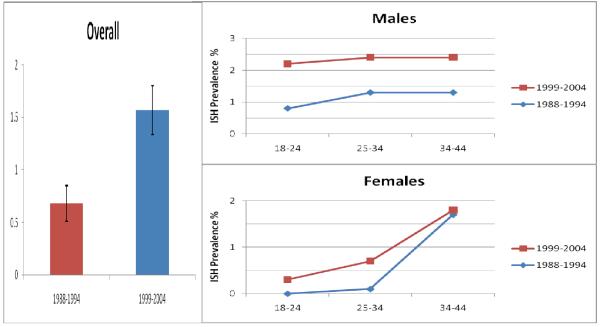
The most recent U.S. estimates by hypertensive subtype, using NHANES III (1988-1994) data, found the prevalence of ISH in males to be 0.8% for ages 18-24, 1.3% for ages 25-34, and 1.3% for ages 34-44. The results for females according to this age categorization were 0.0%, 0.1%, and 1.7%, respectively.10 For comparison of prevalence estimates, we analyzed the NHANES 1999-2004 data employing similar age categorization and found the prevalence of ISH among males to be 2.2% for ages 18-24, 2.4% for ages 25-34, and 2.4% for ages 34-44. Similarly among females, the prevalence of ISH increased to 0.3%, 0.7%, and 1.8% per the respective age categories. We performed a separate analysis to estimate the prevalence of ISH among adults ages 18-39 in NHANES III. The prevalence of ISH among young adults has more than doubled between the NHANES III and 1999-2004 surveys (0.66% vs. 1.57%) (Figure 1).
Figure 1.
Prevalence of ISH overall among adults ages 18-39 and contrast with published prevalence estimates by sex and age group in the National Health and Nutrition Examination Survey (NHANES) III and NHANES 1999-2004. Error bars represent 95% confidence intervals for the overall estimate.
Characteristics of Study Participants
Table 2 presents the distribution of selected characteristics overall and by hypertensive subtype. In general, the majority of participants were non-Hispanic white (73.2%), completed education beyond high school (52.4%), and reported an annual household income of at least $20,000 (72.5%). The distribution of CVD risk factors supports the low prevalence of hypertension in the overall sample. Only 10% of participants had high cholesterol, approximately 1% were diabetic, and over half had never smoked. One-quarter of individuals had no form of health insurance coverage. Average total cholesterol values for the overall study population were within normal ranges. Approximately fifty-five percent of the participants were overweight or obese.
Individuals with ISH differed significantly from the rest of the sample by mean blood pressure indices, height, weight, and BMI. Compared to IDH and SDH, individuals with ISH were significantly younger (p=0.007), and had higher mean weight and proportion of males when compared to normotensives. In contrast with both other subtypes and normotensives, individuals with ISH differed by smoking status, health insurance coverage, income, and educational attainment. Significant differences among those with ISH were observed in the distribution of sex (p=0.004), race/ethnicity (p=0.04), annual household income (p=0.05), education level (p=0.03), health insurance coverage (p=0.008), and smoking status (p=0.01).
Characteristics Based on Age Group and Sex
Although the overall prevalence of ISH was higher among males (p= 0.004), statistically significant differences by sex among individuals with ISH were limited to mean age, weight, and height. Males with ISH were, on average, taller (176.6 cm ± 1.0 vs. 161.4 cm ± 1.4; p<0.001), heavier (92.0 kg ± 2.8 vs. 79.1 kg ± 5.5; p=0.04), and younger (28.0 years ± 0.8 vs. 32.7 years ± 1.4; p=0.004) than females with ISH. Mean BMI, and distribution by BMI categories, did not vary significantly by sex.
Compared to individuals in the 18-29 age group, the ISH 30-39 age group had significantly higher DBP, significantly lower PP, a larger proportion of non-Hispanic blacks and Mexican-Americans, more current smokers, and more individuals who were overweight or obese. Individuals with ISH in the 18-29 age group, in contrast with the 30-39 age group, had a higher degree of alcohol consumption, were more likely to report a family history of hypertension or stroke, a larger proportion who completed education beyond high school, and had significantly lower household incomes. While the 18-29 group was predominantly male (83.70% ± 5.85), ISH in the 30-39 age group approached an even distribution by gender (56.59% ± 8.48 male). Among those with IDH, the older age group had higher DBP and more were physically inactive, whereas more individuals in the younger age group never smoked. Unlike ISH, the distributions of sociodemographic indices in IDH were similar across age groups. Among those with SDH, the older age group had a higher mean BMI, larger proportion of overweight/obese individuals and a higher percentage of non-Hispanic blacks, while individuals in the SDH 18-29 age group were more likely to be current smokers. (Data not shown)
Characteristics Based on Hypertensive Subtype
A separate analysis was performed comparing individuals with ISH to other hypertensive subtypes (IDH and SDH), and to those with normotensive status (Table 2). Compared to both normotensive and other hypertensive individuals, individuals with ISH were more likely to smoke, report a lower household income, have no form of health insurance coverage, and not have completed high school.
When compared to normotensives, participants with ISH were heavier, had a higher mean BMI, and notably higher mean DBP (76.2mmHg ± 1.3 vs. 68.2mmHg ± 0.2, p<0.001) and were more likely to be male. Individuals with ISH were not significantly taller than either normotensives or individuals with IDH and SDH. When compared to other hypertensives, participants with ISH were significantly younger (29.5 years ± 0.8 vs. 32.1 years ± 0.7; p<0.001) and more likely to be non-Hispanic black.
Factors Associated with ISH in Multivariate Analysis
Income, non-Hispanic black race/ethnicity, and absence of health insurance coverage were associated with ISH only in the unadjusted analysis. Height was not associated with ISH risk in crude regression analysis (p= 0.57). We found robust associations between male sex, BMI > 30, current smoking, and education less than high school with ISH as shown in Table 3. Males were more than twice as likely as females to have ISH, before and after controlling for other sociodemographic and CVD risk characteristics. Obese individuals were almost three times as likely as individuals with a BMI < 25 to have ISH in the unadjusted and adjusted models. Current smokers were more than twice as likely as non-smokers to have ISH in both analyses. Individuals with an educational level of less than high school exhibited the greatest risk for ISH in both the unadjusted and multivariable models. Physical activity did not show a significant association with ISH in either unadjusted or adjusted models. Tests for interaction between gender and BMI (p=0.21), gender and age (p= 0.08) and gender and race/ethnicity (p=0.57) were not statistically significant using the Wald F test.
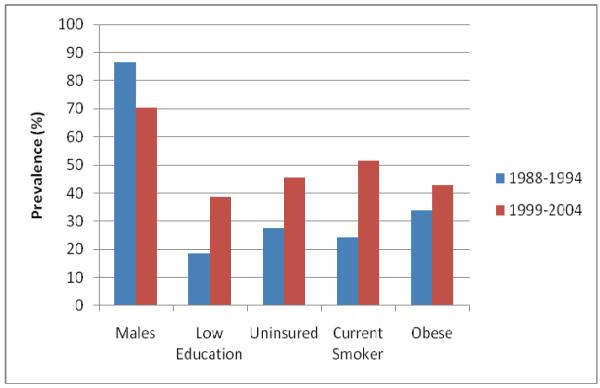
Figure 2 shows a comparison of weighted prevalence estimates of factors in NHANES III and NHANES 1999-2004 associated with ISH in the current multivariate analysis. In a comparison of young adults with ISH in both surveys, there has been a relative increase in prevalence of adverse socioeconomic indices such as low educational level and uninsured status as well as increases in traditional cardiovascular risk factors such as smoking and obesity. The largest relative increase between surveys was the prevalence of current smoking among young adults, with more than twice as many smokers in the more recent NHANES (51.6% vs. 24.3%).
Figure 2.
ISH risk factor prevalences among adults ages 18-39 in the National Health and Nutrition Examination Survey (NHANES) III and NHANES 1999-2004.
DISCUSSION
A limited amount of U.S. population data has been previously available about the prevalence of ISH in the young.2, 10, 12 Using the most recent U.S. population estimates, this study suggests that ISH may affect over one million adults ages 18 to 39. The weighted prevalence of ISH in the U.S. between 1999 and 2004 was 1.57%, corresponding to over 1.1 million (95% CI: 0.95 million to 1.3 million) individuals ages 18 to 39 using NHANES weighted population estimates. ISH is more common among young adults in our study than SDH. Furthermore, we show that the rates of ISH in the young, by age group and sex, have nearly doubled in almost every category in the decade between NHANES III and NHANES 1999-2004, and the overall prevalence of ISH among adults ages 18 to 39 has more than doubled between these surveys. The results also illustrate that while the overall prevalence of ISH is significantly higher among young adult males, the prevalence of ISH increases with age among young females. Our data also illustrate for the first time that cardiovascular risk factors as well as socioeconomic indices are independent determinants of ISH among young adults. Obesity, male sex, smoking, and low educational level were each associated with higher odds of ISH in our study population of young adults. Furthermore, we show that these risk factors have become more prevalent among young adults with ISH in the U.S. over the last decade.
Obesity affects more than one-third of adult Americans.22 It is not uncommon to see obese individuals with concomitant hypertension. In our cohort, obesity as defined by a BMI > 30kg/m2, was significantly associated with a higher risk of ISH among young adults. Increased blood viscosity is associated with obesity and might, by increasing the rheological component of peripheral resistance, contribute to obesity-associated changes in arterial blood pressure.23 Body fat has been shown to be a strong predictor of aortic stiffness in both young and older adults24, which may account for the isolated elevation in SBP among obese young adults.
Young adult males are shown in the current study to have an increased risk for ISH. Recent study also shows that teen boys are more likely to develop higher SBP levels as they get older than teen females.25 Male sex may confound previously reported associations between height and ISH.4, 9 Increases in body height have been positively correlated with systolic pressure amplification and elevated peripheral systolic pressure.26 In our sex-specific analysis, males were on average taller than females and are more likely to have elevated brachial SBP. However, height was not associated with ISH risk in our crude regression analysis and individuals with ISH were not significantly taller than either normotensives or individuals with IDH and SDH. Our results suggest that male sex, and not height, is a more significant determinant of ISH among young adults.
This study finds young adults with ISH are more likely to be current smokers than normotensives or other hypertensives, even though the association between smoking and ISH has been inconsistent in prior studies.7, 27 Both crude and adjusted regression analyses demonstrated a robust independent association between ISH and smoking. The persistent association between smoking and ISH risk supports a growing body of research about the effects of smoking on arterial compliance suggesting that smoking elevates SBP by increasing arterial stiffness, even among younger adults.11, 27, 28
Individuals with ISH had significantly greater disparities in socioeconomic factors including lower household income, lower educational attainment, and lack of health insurance. These socioeconomic factors may be particular to this age group compared to older adults. Such disparities may limit a young adult’s healthcare access, influence their risk of being overweight or obese, and can inhibit management of co-morbidities associated with ISH.29 On multivariate analyses including all socioeconomic indices in our regression model (income, education, and insurance coverage), only educational status was independently associated with a three-fold increased risk of ISH among young adults. Prior studies document an association between educational level and hypertension risk.29-31 This study extends these prior associations to the specific group of ISH in young adults. Causal mechanisms between socioeconomic status and hypertension among younger adults may be the same as those speculated for overall older hypertensives (i.e. - dietary factors, obesity, increased stress, differences in lifestyles and behavior patterns) but this will require further investigation.
Hypertension is known to be more common among non-Hispanic blacks in the U.S. when compared to non-Hispanic whites.18 Prior studies correspond to essential hypertension and not to ISH, particularly among this age group of young adults, so direct comparison to our results is difficult. However, prior studies had not looked at race/ethnicity as a determinant of ISH32 and we now provide some insight regarding this. Young adults of non-Hispanic black race/ethnicity had significantly higher odds of ISH relative to non-Hispanic whites in our unadjusted regression analysis. However, after controlling for other variables in our adjusted model, non-Hispanic black race/ethnicity was no longer associated with elevated ISH risk. Non-Hispanic black adults typically have higher blood pressure and tend to develop hypertension earlier than non-Hispanic whites33 so it is entirely plausible that non-Hispanic black young adults have more ISH. However, the association between non-Hispanic black race/ethnicity and ISH may be confounded or mediated by other factors and have diminished particularly because our full model also controlled for socioeconomic factors that differ by race/ethnicity (income, education, and insurance coverage).
Strengths and Limitations
The strengths of this study include a relatively large, nationally-representative, sample of young adults with ISH, including females, which can be weighted to U.S. population estimates on the basis of the complex NHANES survey design. The 1999-2004 pooled sample provides six years of data and use of the most recent NHANES at the time of this study. The study population is also limited to adults ages 18-39 to emphasize characteristics and risk factors specific to a younger adult population.
Despite these strengths, there are a few limitations pertaining to the use of the NHANES data for our study. First, the NHANES data is cross-sectional and therefore cannot be used to draw causal inferences about relationships between ISH and the characteristics presented in this study. Second, despite the pooling of data from three NHANES surveys, the number of women with ISH in the analytic sample is relatively small (n=29). This small sample limits the power of our multivariable regression to detect sex differences in risk of ISH and may explain why we failed to detect differences in the distribution of risk factors between men and women with ISH in our separate sex analysis. Third, the data on alcohol consumption, smoking, physical activity, and family history of hypertension are based on self-report with the possibility of misclassification of exposure. However, this bias, if non-differential, would be expected only to lead to an underestimation of the association between ISH and these risk factors.
This study illustrates that although individuals with ISH met diagnostic guidelines for normal DBP (<90mmHg), on average, their mean DBP was significantly higher than normotensives by almost 10mmHg. Individuals with ISH in this study population differ from normotensives by both higher SBP and DBP, which may bias risks based on elevated SBP towards the null. Thus pulse pressure should be an important consideration in identifying ISH as this measure is less sensitive to categorical cut-offs for hypertension. The clinical definitions of ISH and IDH should, in theory, yield individuals with higher mean pulse pressure than either normotensives or those with SDH. This remains to be tested in future studies.
Ambulatory BP was not measured in the NHANES and may provide a more accurate diagnostic tool for ISH.34 White coat hypertension, which is more prevalent in younger adults and has strong associations with obesity, may influence clinical identification of ISH.35, 36 White coat hypertension may have accentuated our association between ISH and obesity as well as possibly helping to overstate the prevalence of ISH in this population. However, this limitation would also be true of any prior study of ISH among young adults. Use of ambulatory BP monitoring in future studies may facilitate more accurate estimates of ISH in this study population.
Conclusions
ISH is more common than SDH among young adults in a nationally representative sample. The prevalence of the ISH hypertension subtype has nearly doubled among young adults during the last decade. This may reflect the observed increases over time in the prevalence of cardiovascular risk factors found to be associated with ISH among young adults, particularly obesity and smoking which are potentially modifiable co-morbidities.
The data also illustrate for the first time that socioeconomic factors are important determinants of ISH risk among young adults. Further research is necessary to elucidate the mechanisms by which socioeconomic factors affect ISH incidence among younger adults and whether intervention on both the traditional and non-traditional risk factors identified can help stem the apparent increasing prevalence of ISH among young adults.
Acknowledgments
Funding: CJR was supported by the Robert Wood Johnson Amos Medical Faculty Development Program and a National Heart, Lung, and Blood Institute’s Mentored Career Development Award (K23 HL079343-01A2). The first author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Potential Conflicts of Interest: NONE
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.World Health Organization Guidelines Subcommittee 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens. 1999:151–83. [PubMed] [Google Scholar]
- 2.Franklin SS, Jacobs MJ, Wong ND, L’Italien GJ, Lapuerta P. Predominance of Isolated Systolic Hypertension Among Middle-Aged and Elderly US Hypertensives : Analysis Based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37(3):869–74. doi: 10.1161/01.hyp.37.3.869. [DOI] [PubMed] [Google Scholar]
- 3.Nichols WW, O’Rourke, Michael F, editors. McDonald’s Blood Flow In Arteries: Theoretical, Experimental And Clinical Principles. 5 ed Hodder Headline Group; London, UK: 2005. [Google Scholar]
- 4.O’Rourke MF, Vlachopoulos C, Graham RM. Spurious systolic hypertension in youth. Vascular Medicine. 2000;5(3):141–5. doi: 10.1177/1358836X0000500303. [DOI] [PubMed] [Google Scholar]
- 5.Haider AW, Larson MG, Franklin SS, Levy D. Systolic Blood Pressure, Diastolic Blood Pressure, and Pulse Pressure as Predictors of Risk for Congestive Heart Failure in the Framingham Heart Study. Annals of Internal Medicine. 2003;138(1):10–6. doi: 10.7326/0003-4819-138-1-200301070-00006. [DOI] [PubMed] [Google Scholar]
- 6.Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and Systemic Hemodynamic Characteristics of Hypertension and Prehypertension in Adolescents and Young Adults: The Strong Heart Study. Circulation. 2007;115(2):221–7. doi: 10.1161/CIRCULATIONAHA.106.668921. [DOI] [PubMed] [Google Scholar]
- 7.Kim JA, Kim SM, Choi YS, et al. The prevalence and risk factors associated with isolated untreated systolic hypertension in Korea: The Korean National Health and Nutrition Survey 2001. J Hum Hypertens. 2006;21(2):107–13. doi: 10.1038/sj.jhh.1002119. [DOI] [PubMed] [Google Scholar]
- 8.Vardan S, Mookherjee S. Perspectives on Isolated Systolic Hypertension in Elderly Patients. 2000. pp. 319–23. [DOI] [PubMed]
- 9.Hulsen HT, Nijdam ME, Bos WJ, et al. Spurious systolic hypertension in young adults; prevalence of high brachial systolic blood pressure and low central pressure and its determinants.[see comment] J Hypertens. 2006;24(6):1027–32. doi: 10.1097/01.hjh.0000226191.36558.9c. [DOI] [PubMed] [Google Scholar]
- 10.Joffres MR, Hamet P, MacLean DR, L’Italien GJ, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. American Journal of Hypertension. 2001;14(11):1099–105. doi: 10.1016/s0895-7061(01)02211-7. [DOI] [PubMed] [Google Scholar]
- 11.McEniery CM, Yasmin, Wallace S, et al. Increased Stroke Volume and Aortic Stiffness Contribute to Isolated Systolic Hypertension in Young Adults. Hypertension. 2005;46(1):221–6. doi: 10.1161/01.HYP.0000165310.84801.e0. [DOI] [PubMed] [Google Scholar]
- 12.Burt VL, Whelton P, Roccella EJ, et al. Prevalence of Hypertension in the US Adult Population : Results From the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension. 1995;25(3):305–13. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention National Center for Health Statistics, editor. U.S. Department of Health and Human Services; Hyattsville, MD: National Health and Nutrition Examination Survey Data. 2006
- 14.Centers for Disease Control and Prevention National Center for Health Statistics, editor. U.S. Department of Health and Human Services; Hyattsville, MD: National Health and Nutrition Examination Survey Analytic and Reporting Guidelines. 2005
- 15.Perloff D, Grim CG, Flack J. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–9. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention National Center for Health Statistics, editor. U.S. Department of Health and Human Services; Hyattsville, MD: National Health and Nutrition Examination Survey Examination Protocol. 2006
- 17.National Heart L. Blood Institute Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. 1998. p. 228.
- 18.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 19.National Heart L. Blood Institute . Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III Final Report) National Institutes of Health; Bethesda, MD: Sep, 2002. 2002. [Google Scholar]
- 20.SAS Institute Inc. SAS/STAT 91 User’s Guide. SAS Institute Inc; Cary, NC: 2004. [Google Scholar]
- 21.Research Triangle Institute . SUDAAN Language Manual, Release 90 Research Triangle. Research Triangle Institute; Park, NC: 2004. [Google Scholar]
- 22.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. Jama. 2002;288(14):1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 23.Zhang R, Reisin E. Obesity-hypertension: the effects on cardiovascular and renal systems. Am J Hypertens. 2000;13(12):1308–14. doi: 10.1016/s0895-7061(00)01254-1. [DOI] [PubMed] [Google Scholar]
- 24.Wildman RP, Mackey RH, Bostom A, Thompson T, Sutton-Tyrrell K. Measures of obesity are associated with vascular stiffness in young and older adults. Hypertension. 2003;42(4):468–73. doi: 10.1161/01.HYP.0000090360.78539.CD. [DOI] [PubMed] [Google Scholar]
- 25.Dasgupta K, O’Loughlin J, Chen S, et al. Emergence of Sex Differences in Prevalence of High Systolic Blood Pressure: Analysis of a Longitudinal Adolescent Cohort. 2006. pp. 2663–70. [DOI] [PubMed]
- 26.Smulyan H, Marchais SJ, Pannier B, Guerin AP, Safar ME, London GM. Influence of Body Height on Pulsatile Arterial Hemodynamic Data. Journal of the American College of Cardiology. 1998;31(5):1103–9. doi: 10.1016/s0735-1097(98)00056-4. [DOI] [PubMed] [Google Scholar]
- 27.Mahmud A, Feely J. Spurious systolic hypertension of youth: fit young men with elastic arteries. American Journal of Hypertension. 2003;16(3):229–32. doi: 10.1016/s0895-7061(02)03255-7. [DOI] [PubMed] [Google Scholar]
- 28.Rehill N, Beck CR, Yeo KR, Yeo WW. The effect of chronic tobacco smoking on arterial stiffness. 2006. pp. 767–73. [DOI] [PMC free article] [PubMed]
- 29.Tyroler HA. Socioeconomic status in the epidemiology and treatment of hypertension. Hypertension. 1989;13(5 Suppl):I94–7. doi: 10.1161/01.hyp.13.5_suppl.i94. [DOI] [PubMed] [Google Scholar]
- 30.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment: the NHANES I epidemiologic followup study. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152(3):272–8. doi: 10.1093/aje/152.3.272. [DOI] [PubMed] [Google Scholar]
- 32.Wilking SV, Belanger A, Kannel WB, D’Agostino RB, Steel K. Determinants of isolated systolic hypertension. Jama. 1988;260(23):3451–5. [PubMed] [Google Scholar]
- 33.LaRosa JC, Brown CD. Cardiovascular risk factors in minorities. Am J Med. 2005;118(12):1314–22. doi: 10.1016/j.amjmed.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 34.Protogerou AD, Papaioannou TG, Blacher J, Papamichael CM, Lekakis JP, Safar ME. Central blood pressures: do we need them in the management of cardiovascular disease? Is it a feasible therapeutic target? J Hypertens. 2007;25(2):265–72. doi: 10.1097/HJH.0b013e3280114f23. [DOI] [PubMed] [Google Scholar]
- 35.Gan SK, Loh CY, Seet B. Hypertension in young adults--an under-estimated problem. Singapore Med J. 2003;44(9):448–52. [PubMed] [Google Scholar]
- 36.Pickering TG. Isolated Systolic Hypertension in the Young. The Journal of Clinical Hypertension. 2004;VI(1):47–8. doi: 10.1111/j.1524-6175.2004.02835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]