Abstract
This study evaluated the effectiveness of a group mentoring program that included components of empirically supported mentoring and cognitive behavioral techniques for children served at a community mental health center. Eighty-six 8- to 12-year-old children were randomly assigned to either group mentoring or a wait-list control group. Group mentoring significantly increased children’s reported social problem-solving skills and decreased parent-reported child externalizing and internalizing behavior problems after controlling for other concurrent mental health services. Attrition from the group mentoring program was notably low (7%) for children. The integration of a cognitive behavioral group mentoring program into children’s existing community mental health services may result in additional reductions in externalizing and internalizing behavior problems.
Keywords: children, emotional and behavioral problems, group mentoring
The formats and settings of structured child mentoring programs have increased substantially in recent years. Mentoring programs that provide positive role models and supportive relationships to children have been developed to serve a wide range of youth (Rhodes, Bogat, Roffman, Edelman, & Galasso, 2002; Rhodes, Grossman, & Resch, 2000). The implementation of mentoring in different formats and settings has resulted in the development of a new generation of programs. Programs are now conducted in dyadic, group, and peer formats and in community, school, after-school, and workplace settings (Hamilton & Hamilton, 2005; Hernandez, Hayes, Balcazar, & Keys, 2001; Herrera, Vang, & Gale, 2002; Hirsch & Wong, 2005; Portwood & Ayers, 2005; Rhodes et al., 2000). Further, programs have been developed to serve special youth populations such as abused and neglected youth, youth with disabilities, pregnant adolescents, adolescent parents, juvenile offenders, academically at-risk students, and children with emotional and behavioral disturbances (Blechman, Maurice, Buecker, & Helberg, 2000; Herrera, Sipe, & McClanahan, 2000; Jent & Niec, 2006; Rhodes, Ebert, & Fischer, 1992; Rhodes, Haight, & Briggs, 1999; Watkins, Pittman, & Walden, 1998).
While community initiatives to offer more mentoring programs are widespread, mentoring generally has small to moderate positive effects on youths’ emotional, behavioral, and academic functioning (e.g., DuBois, Holloway, Valentine, & Cooper, 2002; Grossman & Tierney, 1998; Jackson, 2002; Jent & Niec, 2006; Rhodes et al., 2000; Rhodes, Reddy, & Grossman, 2005). DuBois and colleagues (2002) suggested that at-risk youth are likely to receive the greatest benefit from mentoring services, but specific special populations of youth may benefit differently from mentoring programs specifically tailored to meet their needs.
To address the significant gap between implementing new mentoring programs and the empirical support for their use, the National Research Summit on Mentoring developed a National Research Agenda for Youth Mentoring to promote effective evidence-based youth mentoring services (Rhodes & DuBois, 2004). The National Research Agenda described the need for mentoring research in numerous areas including evaluation of alternate mentoring formats (e.g., group, peer) and settings (e.g., school, church), development of “Best Practices” in mentoring, examination of programs that are integrated into other services, and investigation of mechanisms such as gender, age, ethnicity, and the mentoring relationship on outcomes (Rhodes & DuBois, 2004).
In response to this call for more focused mentoring research, we evaluated the effectiveness of a new generation mentoring program (i.e., group) for children with emotional and behavioral disturbances. That is, we developed a group mentoring program based on best practices for mentoring and cognitive behavioral intervention principles for children’s behavior problems (Eyberg, Nelson, & Boggs, 2008; Denham & Almeida, 1987; DuBois et al., 2002; Sukhodolsky, Kassinove, & Gorman, 2004; see Table 1). Specifically, our group mentoring program included features of best mentoring practices including ongoing training for group mentors, structured activities for the children, consistent contact between group mentors and children, and monitoring of program implementation (DuBois et al., 2002). The program also includes cognitive behavioral principles that have demonstrated efficacy in reducing childhood externalizing (e.g., aggression) and internalizing (e.g., withdrawal, depressive symptoms) behavior problems including components of social problem-solving, social skills training, live coaching, token economies, and modeling (Filcheck, McNeil, Greco, & Bernard, 2004; Frye & Goodman, 2000; Reitman, Murphy, Hupp, & O’Callaghan, 2004; Sukhodolsky et al., 2004; Vostanis, Feehan, Grattan, & Bickerton, 1996). The addition of cognitive behavioral principles to group mentoring provides the opportunity for mentors to shape children’s positive social interactions with other children in vivo.
TABLE 1.
An Examination of Mentoring and Cognitive Behavioral Components in a Group Mentoring Program
| Program feature | Mentoring | Cognitive behavioral therapy | Group mentoring with cognitive behavioral principles |
|---|---|---|---|
| Time | Relationships are variable in length | Therapy is typically time-limited | Expectations about the length of the program is given to children prior to the start of the program |
| Activities | Child-determined activities | Treatment protocols typically direct all activities | Combination of skills training and child-determined activities |
| Length of meeting | Children typically meet at least 3 hours weekly | Sessions are typically 1 to 2 hours in length | Sessions are 4 hours long allowing time for didactic, coaching, child-determined activities, and supportive conversations with mentors |
| Parent involvement | Parent involvement varies significantly (e.g., participate in activities with mentor, child, informed of what mentor and child are doing) | Parent involvement varies (e.g., behavioral parent training, cognitive behavioral social skills training groups) | Parents are provided summaries of what their children are learning, but are not directly involved in services |
| Relationship | Mentors model appropriate behavior for children | Therapists teach and model specific coping skills to children and parents | Children learn specific strategies to problem solve, but also engage in natural interactions with group mentors and peers in which mentors model appropriate behavior and reinforce children for appropriate behavior |
| Level of training | Mentors are generally volunteers that are interested in helping children | Therapists are trained professionals that have a background in providing services to children with behavior problems | Group mentors are provided training on how to implement the program Group mentors receive ongoing weekly supervision |
| Transportation | Mentors typically provide transportation for children | Parents typically provide transportation for children. | Group mentors provide all transportation |
| Employment status | Mentors are typically unpaid volunteers | Therapists are employed professionals | Group mentors are employed in order to compensate them for training, weekly supervision, and to reduce mentor attrition |
In summary, while numerous formats of mentoring programs have been developed to serve children, the positive effects of mentoring programs on children’s behavioral, emotional, and academic functioning have generally been small to moderate. Preliminary evidence exists for the use of dyadic mentoring with children with emotional and behavioral disturbances, but the effect of group mentoring for children in community mental health center settings has yet to be examined. We predicted that children who completed a group mentoring program would be viewed as displaying more positive emotional and behavioral functioning than children who were assigned to a wait-list control group. Specifically, children who participated in the group mentoring program would report more adaptive social problem-solving skills and better parent–child relationships. We predicted that parents of mentored children would report less parenting-related stress and perceive their children as having more adaptive child social communication skills and fewer child behavior problems than wait-listed families at posttreatment. Finally, we predicted that the effects of the group mentoring program would account for improvement in functioning after controlling for other mental health services received and psychotropic medication status.
METHOD
Participants
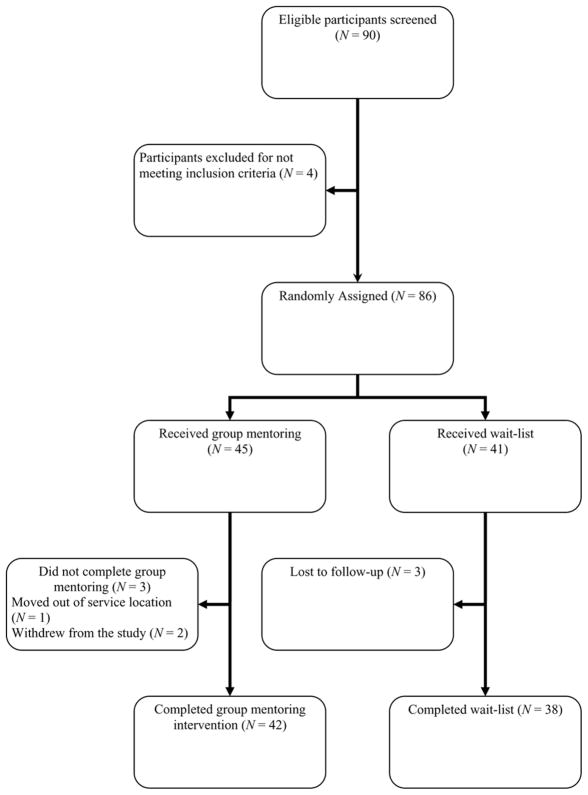
All families with children 8- to 12-years-old referred for mentoring services at a rural Midwestern community mental health center (n=90) were invited to enroll in this study and were assessed for study eligibility (see Figure 1). Informed parental consent and child assent were obtained from all families prior to enrollment in the study. Exclusion criteria included (a) parents and children who would not commit to attend a 12-session weekly group mentoring program; and (b) child Peabody Picture Vocabulary Test-III (PPVT-III; Dunn & Dunn, 1997) score of two standard deviations lower than the mean. Four families were excluded because they were not willing to commit to the time constraints of the group intervention and were offered individual mentoring services instead.
FIGURE 1.
Flow of participants through a randomized trial of a cognitive behavioral group mentoring program for children.
Using a computer-generated randomization list, eligible families (n=86) were randomly assigned to either the intervention condition or a control group wait-list. The details of the randomized series were contained in a set of appropriately numbered sealed envelopes that were opened by study personnel once a participant met inclusion criteria for the study. Forty-five children (27 boys, 18 girls) were assigned to group mentoring and 41 children (30 boys, 12 girls) were assigned to the control group wait-list. Three participants in the intervention group discontinued treatment and three control group participants withdrew from the study. The group mentoring attrition rate was 7% and none of the group mentors withdrew from their matched children during the study.
Initially, five intervention groups were conducted concurrently. Following completion of the five groups, three more intervention groups were conducted concurrently, for a total of eight separate intervention groups. Children in the wait-list control group received no contact with group mentors during data collection, but were offered group mentoring once they completed the 3-month wait-list.
Procedure
All participating parents completed multiple standardized measures of family functioning at intake and at posttreatment/end of wait-list. The length of the program was 12 sessions and measures were completed within 2 weeks prior to the first session and during the last session. Control group families were administered post-treatment measures within 1 week of the last session. Participating children completed the PPVT-III, the Inventory of Parent and Peer Attachment (IPPA; Armsden & Greenberg, 1987), and the Social Problem-Solving Inventory-Adolescent (SPSI-A; Frauenknecht & Black, 1995). Measures were read to children to prevent reading difficulties from influencing responses. Maternal caregivers of children participating in the study completed the Behavior Assessment System for Children–Parent Report Form (BASC; Reynolds & Kamphaus, 1992), the Parenting Stress Index-Short Form (PSI-SF; Abidin, 1995), and the Social Skills Rating System (SSRS; Greshham & Elliott, 1990).
Program
Group mentors were employed by a rural community mental health center. Eight group mentors provided services. Mentor-to-child ratio within sessions ranged from two mentors to eight children to two mentors to four children. In regard to education, two of the group mentors were completing graduate coursework in clinical social work or counseling and six were enrolled in a 4-year college. Group mentors received a minimum of 24 hours of initial training to increase adherence to the group mentoring protocol. All group mentors received training in positive reinforcement, live coaching, implementing token economies, maintaining a positive therapeutic milieu, and the group mentoring protocol (Jent, 2004). In addition, group mentors received a minimum of a half hour of supervision per week with a master’s level clinician who had substantial clinical experience in treating children’s externalizing behavior problems in a group setting.
One of the goals of the group mentoring program was to reduce treatment barriers to families. Thus, all children were transported to sessions by their group mentors. Group mentors met with the children weekly for a period of 4 hours for 12 weeks. During each session, children participated in group discussion and received didactics related to social problem-solving and social interaction skills (see Table 2 for session topics and activities). Didactics and discussion were followed by child-determined activities based on the specific group’s interest (e.g., billiards, sports, arts and crafts). This activity time was conceptualized as a period when appropriate interaction skills could be shaped, rehearsed, and reinforced. Beyond activities within the community center, children were also provided the opportunity to engage in similar activities to traditional mentoring programs (e.g., going to restaurants, going to the park, playing putt–putt golf, watching movies, going to the library, going swimming). During all components of the sessions, group mentors positively reinforced children’s appropriate use of problem-solving skills through praise and a token economy. Specifically, children were awarded bonus points every time they were observed engaging in a positive behavior (e.g., contributing to group discussion, remaining calm during a conflict, helping another child). In addition, group mentors used live coaching to encourage children to use appropriate social communication and problem-solving skills during all aspects of sessions. During child-determined activities and transportation, group mentors also engaged in goal-directed and supportive conversations with children, similar to individual mentor relationships. At the end of each session, group mentors briefly spoke with parents, discussing the completed activities, how the children behaved, and the extent of goal progress. While several mentoring and cognitive behavioral studies have noted the importance of parental involvement in treatment outcome, group mentoring limited parent involvement as many of the families served were already engaged in other types of mental health services or had previously demonstrated resistance to participation in services.
TABLE 2.
Summary of Group Mentoring by Session
| 1 | Discussion Topic: | Welcome, group rules, and token economy |
| Primary Goal: | Begin to develop rapport, group cohesion, and behavior expectations | |
| Activity: | Team-building activities | |
| 2 | Discussion Topic: | Problem identification and emotional reaction |
| Primary Goal: | Identify interpersonal problems and learn physiological indicators, thoughts, and expressions, associated with emotions | |
| Activity: | Emotional education activity: practice identifying emotions through role-playing | |
| 3 | Discussion Topic: | Relaxation techniques |
| Primary Goal: | Teach children several methods of affect regulation | |
| Activity: | Practice relaxation techniques while playing a freeze tag game | |
| 4 | Discussion Topic: | Perspective taking and goal setting |
| Primary Goal: | Enhance children’s understanding of others’ behaviors and teach children how to define an optimal solution for problems | |
| Activity: | Review learned problem-solving skills through playing a frustration-tolerance game | |
| 5 | Discussion Topic: | Generating and evaluating solutions to interpersonal problems |
| Primary Goal: | Generate solutions to common problems and learn how to evaluate potential solutions | |
| Activity: | Game that encourages cooperation and group problem solving | |
| 6 | Discussion Topic: | Steps to social problem-solving |
| Primary Goal: | Review the steps of social problem-solving with children | |
| Activity: | Fun activity based on what the group earned from their token economy | |
| 7 | Discussion Topic: | Appropriate interpersonal behaviors in public |
| Primary Goal: | Improve children’s social skills in public settings | |
| Activity: | Travel to a local restaurant to practice appropriate social behavior | |
| 8 | Discussion Topic: | Non-verbal communication |
| Primary Goal: | Learn how to observe and interpret non-verbal behaviors | |
| Activity: | Game that reinforces children for identifying children’s nonverbal communication skills | |
| 9 | Discussion Topic: | How to give and receive compliments |
| Primary Goal: | Enhance children’s prosocial behavior and appropriate response to praise | |
| Activity: | Children practice giving and receiving compliments through a “Warm Fuzzy Game” | |
| 10 | Discussion Topic: | The use of problem-solving skills and manners when playing games or sports |
| Primary Goal: | Help children interact and respond to problems appropriately during competitive play | |
| Activity: | A competitive game where mentors award children team spirit, and sportsmanship points | |
| 11 | Discussion Topic: | Managing socially embarrassing situations and initiating conversations with peers |
| Primary Goal: | Improve response to embarrassment through problem-solving and enhancing social communication skills with peers | |
| Activity: | Mentors model appropriate responses to embarrassing situations through role-playing | |
| 12 | Discussion Topic: | Summary of social communication and problem-solving skills learned |
| Primary Goal: | Review skills learned during the program and reinforce children’s use of skills | |
| Activity: | Fun activity based on what the group earned through their token economy |
Child Measures
Peabody picture vocabulary test-third edition
The PPVT-III is a picture vocabulary test designed to assess children’s receptive vocabulary (Dunn & Dunn, 1997). The internal consistency of the PPVT-III for children ages 8–12 on Form IIIA ranges from α=.92 for age 8 years to .94 for age 12 years. Test-retest reliability was high for Form IIIA when examinees (ages 6–17) were retested 1 month later (r=.93 for ages 6–11 and .91 for ages 12–17). The PPVT-III Form IIIA correlated highly with the Verbal Scale of the WISC-III (r=.91) supporting concurrent validity.
Inventory of parent and peer attachment
The Inventory of Parent and Peer Attachment is a 53-item self-report scale containing questions related to a child’s relationship with his or her primary caregiver and peers. The IPPA consists of a Parent Scale and a Peer Scale with each containing three subscales: Communication (i.e., Talking over my problems with my mother makes me feel ashamed or foolish), Trust (i.e., My mother trusts my judgment), and Alienation (i.e., My mother has her own problems so I do not bother her with mine). Internal consistency on the Parent Scale, which was the only scale administered for the current study, ranged from α=.86 (Alienation and Trust) to α=.91 (Communication). In pre-adolescent children, the IPPA Parent Scale scores possess adequate internal consistency (α=.78) and test-retest reliability over 1 year (r=.63; Abela, Adams, & Hankin, 2005). The Parent Scale has been significantly correlated with family and social self-concept, family cohesion, expressiveness, and utilization of family resources (Armsden & Greenberg, 1987).
Social problem-solving inventory-adolescent: short form
The SPSI-A Short Form is a 30-item, self-report inventory used to assess dispositions in problem solving (Frauenknecht & Black, 1995). Items are rated on a 5-point Likert-type scale with scores ranging from Not true at all of me to Extremely true of me and reflect positive and negative attitudes and beliefs about problem solving. Test-retest reliability over a 2-week period was stable (SPSI-A Total Score r=.83; Frauenknecht & Black, 1995). Construct validity was assessed by correlating the SPSI-A with the Problem-Solving Inventory, a measure for adults (Heppner & Peterson, 1982). The SPSI-A Total Score correlated with the Total Scale on the Problem-Solving Inventory at r=.82, p<.001. In addition, the SPSI-A negatively correlates with the Brief Symptom Inventory Global Severity Index, r = −.27, p<.001 (Frauenknecht & Black, 1995). The internal consistency for the SPSI-A total scale for the current sample at pretreatment was adequate (α=.88).
Parent Measures
Behavior assessment system for children
The BASC-Parent Report Form is a broad-band rating scale of child and adolescent behavior as perceived by the parent (Reynolds & Kamphaus, 1992). It is a 138-item scale that assesses the frequency with which children portray specific behaviors (i.e., Never, Sometimes, Often, and Almost Always). The BASC assesses three domains of behavior including the Externalizing Problems Composite (e.g., Threatened to hurt others), the Internalizing Problems Composite (e.g., Is sad), and the Adaptive Skills Composite (e.g., Attends after school activities) for children 2- to 18-years-old. Test-retest reliability coefficients are also high for the composites ranging from r=.62 to .94 over 2 months for ages 6–18 (Reynolds & Kamphaus, 1992). The BASC-PRS highly correlates with similar scales on the Child Behavior Checklist (CBCL) demonstrating convergent validity.
Social skills rating system
The Social Skills Rating System-Parent Report Form is a broad-band assessment of child and adolescent social skills and problem behaviors as perceived by the parent (Gresham & Elliott, 1990). It is a 55-item parent report form that assesses the frequency that a child portrays appropriate social skills and behavior (i.e., Never, Sometimes, and Very Often) and parent perception of the importance of the behavior for the child’s social development (i.e., Not Important, Important, and Critical). The SSRS assesses two domains including the Social Skills Scale (e.g., Answers the phone appropriately) and Problem Behaviors Scale (e.g., Disobeys rules or requests). Test-retest reliability is high for the Social Skills Scale at r=.87 over 1 month for elementary school aged students (Gresham & Elliott, 1990). The SSRS Social Skills Scale correlates r=.58 with the corresponding scale on the CBCL.
Parenting stress index-short form
The Parenting Stress Index-Short Form (PSI-SF) is a 36-item parent-report measure that assesses the level of stress a parent is experiencing in relation to their parenting and the sources of that stress (Abidin, 1995). The Total Stress Scale of the PSI assesses parents’ stress in the areas of personal parental distress, parent-child interactions, and child behavioral characteristics (Abidin). The test-retest reliability for the Total Stress Scale was r=.84 over a 6-month period for ages 2–12 with an internal consistency of α=.91 (Abidin).
RESULTS
Participants (n=80) who completed pre-treatment and post-treatment measures were included in analyses. Intervention and control group families did not differ in age, gender, receptive language ability, the number of hours of mental health services (i.e., hours of outpatient therapy, home-based therapy, school-based therapy, medication management, and case management) received in the last year, the number of hours of mental health services received during the data collection period, or the number of children prescribed psychotropic medication (Table 3). Participants’ race and ethnicity significantly differed between groups. However, when race/ethnicity was entered as a covariate into all treatment analyses, the results did not change. Therefore, race was removed as a covariate from final outcome analyses.
TABLE 3.
Demographic and Clinical Characteristics of Participants
| Mentored group |
Wait-listed group |
Test of significance | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Boys | 25 | 59.5 | 28 | 73.7 | χ2(1) = 1.79 |
| Girls | 17 | 40.5 | 10 | 26.3 | |
| Caucasian | 38 | 90.5 | 26 | 68.4 | χ2(2) = 7.40* |
| Hispanic | 4 | 9.5 | 8 | 21.1 | |
| African American | 0 | 0 | 4 | 10.5 | |
| Prescribed Psychiatric Medication | 17 | 40.50 | 13 | 34.20 | χ2(1) = .33 |
| No Medication | 25 | 59.50 | 25 | 65.80 | |
| N | M | SD | N | M | SD | Test of significance | |
|---|---|---|---|---|---|---|---|
| Age | 42 | 10.52 | 1.72 | 38 | 9.92 | 1.71 | F(1, 81) = 1.51 |
| PPVT-III Standard Score | 42 | 95.50 | 10.51 | 38 | 96.84 | 11.04 | F(1, 81) = .31 |
| Hours of Mental Health Services Received in Past Year | 42 | 28.60 | 20.87 | 38 | 20.16 | 21.60 | F(1, 78) = 3.16 |
| Hours of Mental Health Service | 42 | 9.69 | 8.49 | 38 | 6.97 | 8.37 | F(1, 78) = 2.30 |
Note. PPVT-III = Peabody Picture Vocabulary Test-Third Edition; Hours of Mental Health Service = Hours of mental health service received between pretreatment and posttreatment;
p<.05.
Group Mentoring Fidelity
To assess group mentoring protocol fidelity, one group mentor completed a log at the end of each session. Logs tracked the activities and discussions completed, the data administered and collected, and the explanations if the group mentoring protocol was not followed. Group mentors reported that activities related to the mentoring protocol were completed 92% of the time. However, deviations from the protocol were always corrected during the next session. Ongoing weekly supervision of group mentors maintained fidelity and reduced drift.
Effectiveness of Group Mentoring
Table 4 presents group means and standard deviations on the primary measures at pretreatment and posttreatment for the mentored and control group children. Primary outcome measures for the study are the BASC Externalizing Problems Composite, BASC Internalizing Problems Composite, PSI-SF Total Raw Score, SPSI-A Total Raw Score, IPPA Parent Scale, and the SSRS Social Skills Standard Score. The statistical model for the primary outcome measures was a linear mixed model that included fixed effect terms for intervention group, time, group by time interaction; covariate terms for the number of hours of mental health services received during the data collection period (i.e., total number of hours child received medication management services, case management, school-based therapy, outpatient therapy, and/or home-based therapy) and the child’s prescribed psychiatric medication status (i.e., 1=child prescribed psychiatric medication during data collection period; 0=child not prescribed psychiatric medication during data collection period); and a random effect term for different intervention groups (n=8), in order to control for the lack of independence among ratings collected within the same mentoring groups (Norusis, 2005).
TABLE 4.
Outcome Measures by Group and Time Using a Mixed Linear Model
| Measure | N | Pretreatment |
Posttreatment |
Group × Time |
|||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | F | |||
| BASC Externalizing Problems Composite T Score | Treatment | 42 | 76.36 | 15.95 | 59.17 | 7.64 | 7.42** |
| Control | 38 | 73.87 | 19.34 | 68.76 | 13.64 | ||
| BASC Internalizing Problems Composite T Score | Treatment | 42 | 66.98 | 19.03 | 59.52 | 14.51 | 5.24* |
| Control | 38 | 58.21 | 14.59 | 61.66 | 11.82 | ||
| PSI Total Stress | Treatment | 42 | 97.38 | 25.03 | 97.24 | 28.02 | .37 |
| Control | 38 | 97.05 | 19.88 | 101.58 | 26.73 | ||
| SSRS Social Skills Standard Score | Treatment | 42 | 80.05 | 13.56 | 86.60 | 16.96 | .87 |
| Control | 38 | 80.58 | 11.92 | 83.18 | 11.22 | ||
| IPPA Total Score | Treatment | 42 | 104.07 | 19.54 | 105.05 | 25.10 | 1.26 |
| Control | 38 | 102.89 | 16.87 | 97.00 | 13.92 | ||
| SPSI-A Total Score | Treatment | 42 | 25.15 | 8.10 | 31.58 | 6.68 | 5.91* |
| Control | 38 | 23.64 | 7.75 | 24.43 | 6.65 | ||
Note.
p<.05;
p<.01.
Primary outcome hypotheses were supported in that children who received mentoring demonstrated positive changes in self-reported social problem-solving and parent-reported externalizing and internalizing behavior problems. The intervention group reported a statistically significant group by time interaction on social-problem solving scores, F(1, 154) = 5.91, p<.05. Follow-up t tests of parameter estimates showed that children who received mentoring reported significant increases in social problem-solving skills, t(154) = 2.43, p<.05. There was a significant group by time interaction in children’s externalizing behaviors from pretreatment to posttreatment, F(1, 154) = 7.42, p<.01. That is, parents of group-mentored children viewed their children as displaying significantly greater reductions in externalizing behaviors, t(154) = −2.72, p<.01, than the wait-list controls. Specifically, 11(26%) mentored children who were reported as having at-risk or clinically significant externalizing behaviors at pretreatment were reported as having externalizing behaviors within normal limits at posttreatment. An additional 22(52%) mentored children who were viewed as having clinically significant externalizing behaviors at pretreatment were reported as having at-risk externalizing behaviors at posttreatment. A significant group by time interaction was also found for parents’ reports of children’s internalizing behavior problems, F(1, 154) = 5.24, p<.05. Parents of group-mentored children reported significant decreases in internalizing behaviors from pretreatment to posttreatment, t(154)=−2.29, p<.05. Clinically significant changes in reported internalizing problems were found for 5 (12%) mentored children from pretreatment to posttreatment. Families in the intervention and the control group condition did not change differently over time on measures of parent stress, children’s social communication skills, or parent–child relationship quality.
DISCUSSION
The purpose of this study is to examine the effectiveness of a cognitive behavioral group mentoring program on child functioning when administered in a community mental health center setting. Results reveal that group mentoring significantly increased children’s self-reported social problem-solving skills and decreased parent-reported child externalizing and internalizing behavior problems after controlling for other concurrent mental health services (e.g., hours of other mental health services received, psychiatric medication status).
Improving Child Functioning
As expected, children who participated in cognitive behavioral group mentoring reported significant increases in their use of social problemsolving skills. That is, children who participated in mentoring reported a significant increase in their ability to successfully utilize the steps of social problem-solving process when presented with a conflict. Further, mentored children perceived significant increases in their problem-solving self-efficacy and their ability to apply problem-solving strategies automatically. Perhaps one of the largest benefits of increased social problem-solving skills in children is that the skills can be generalized across a number of conditions and domains.
Children who completed the group mentoring program were also viewed as experiencing significant reductions in externalizing and internalizing behavior problems from pre- to posttreatment. Parents of children who completed the mentoring program reported statistically significant decreases in children’s disruptive behavior and internalizing problems following completion of group mentoring, after controlling for other mental health services received. Over one quarter of parents of mentored children viewed their children’s externalizing behaviors as being within normal limits at posttreatment. Overall, the results of the study are consistent with previous mentoring and social problem-solving studies, providing preliminary support for the small to moderate effect of a cognitive behavioral group mentoring approach on reducing children’s behavior problems within a community mental health setting.
Reducing Barriers to Participation
The group mentoring program had a notably low attrition rate for children (7%). The low attrition rate may be the result of reducing a number of identified barriers to service. The limited parent participation required meant that parents did not have to take time from work or other activities to attend. Group mentors provided all transportation and meals for the children, thus reducing transportation and financial barriers. Mentors were compensated for all training, supervision, and time spent with mentored children, likely increasing their commitment to the program. It is promising that this program made significant changes in children’s behavior and that a high proportion of children completed the program, which was implemented in a community mental health setting.
The positive effect on parenting stress and parent–child relationship quality observed in some individual and group mentoring programs did not generalize to the group mentoring program. It may be that the differences between traditional mentoring services and group mentoring explain the variation in parents’ outcomes. The group mentoring program examined in the current study was a 12-week program, whereas traditional mentoring is not time-limited, with many mentoring relationships lasting well over 1 year. It is possible that mentoring takes longer than 12 weeks to demonstrate a significant impact on families’ relationship quality. It is also possible that group mentoring did not impact parent functioning because peer relationships were a more intense focus of the program than adult–child corrective relationships.
In evaluating the results of this study, it should be noted that changes in medication regimen (e.g., changes in dosage or type of medication) during data collection were not tracked. Further, the types of mental health services (e.g., case management, outpatient therapy) and treatment approaches (e.g., cognitive behavioral therapy, psychodynamic therapy) received by children were not controlled. However, children’s status of being prescribed psychiatric medication and the number of hours of mental health services received during data collection were statistically controlled. Measurements in the current study were limited to parent and self-report measures. Third-party ratings of children’s behavior (e.g., objective teacher and mentor ratings, behavior observations) should be included in future studies to further assess actual changes in children’s behaviors and social problem-solving skills. Also, the maintenance of mentoring effects could not be evaluated because follow-up assessments of family functioning were not collected.
Conclusion
The National Research Agenda for Youth Mentoring called for methodologically sound research into the new generation of mentoring programs (Rhodes & DuBois, 2004). This study is the first to examine the effects of group mentoring on families with children being served at a community mental health center. The study provides a foundation for future research on group mentoring in that it utilized a randomized controlled design and a multi-source assessment of child functioning with standardized measures within a community mental health setting.
Given the vast amount of monetary and human resources that are currently allocated to the development and implementation of mentoring programs, further research in this area is warranted. Next steps for group mentoring effectiveness research include: a randomized controlled trial in which children are randomly assigned to either group mentoring, individual mentoring, or a placebo attention control group to examine the relative effectiveness of different mentoring programs over similar periods of time; the exploration of youth-mentor relationship quality as a mechanism of change within group mentoring; a cost-effectiveness evaluation of a group mentoring program that includes paid mentors and funded transportation; and an evaluation of maintenance of mentoring effects over time.
Contributor Information
JASON F. JENT, Miller School of Medicine, University of Miami, Miami, Florida, USA
LARISSA N. NIEC, Department of Psychology, Central Michigan University, Mt. Pleasant, Michigan, USA
References
- Abela JR, Adams P, Hankin BL. Interpersonal vulnerability to depression in children and adolescents: A longitudinal study. Journal of Clinical Child and Adolescent Psychology. 2005;34:182–192. doi: 10.1207/s15374424jccp3401_17. [DOI] [PubMed] [Google Scholar]
- Abidin RR. Parenting stress index: Third edition professional manual. Lutz, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Armsden GC, Greenberg MT. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Children & Adolescence. 1987;16:427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- Blechman EA, Maurice A, Buecker B, Helberg C. Can mentoring or skill training reduce recidivism? Observational study with propensity analysis. Prevention Science. 2000;1:139–155. doi: 10.1023/a:1010073222476. [DOI] [PubMed] [Google Scholar]
- Denham SA, Almeida MC. Children’s social problem-solving skills, behavioral adjustment, and interventions: A meta-analysis evaluating theory and practice. Journal of Applied Developmental Psychology. 1987;8:391–409. [Google Scholar]
- DuBois DL, Holloway BE, Valentine JC, Cooper H. Effectiveness of mentoring programs for children: A meta-analytic review. American Journal of Community Psychology. 2002;30:157–197. doi: 10.1023/A:1014628810714. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Examiner’s manual for the Peabody picture vocabulary test. 3. Circle Pines, MN: American Guidance Service; 1997. [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Filcheck HA, McNeil CB, Greco LA, Bernard RS. Using a whole-class token economy and coaching of teacher skills in a preschool classroom to manage disruptive behavior. Psychology in the Schools. 2004;41:351–361. [Google Scholar]
- Frauenknecht M, Black DR. Social problem-solving inventory for adolescents (SPSI-A): Development and preliminary psychometric evaluation. Journal of Personality Assessment. 1995;64:522–539. doi: 10.1207/s15327752jpa6403_10. [DOI] [PubMed] [Google Scholar]
- Frye AA, Goodman SH. Which social problem-solving components buffer depression in adolescent girls? Cognitive Therapy and Research. 2000;24:637–650. [Google Scholar]
- Gresham FM, Elliott SN. Social skills rating system manual. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- Grossman JB, Tierney JP. Does mentoring work? An impact study of big brothers/big sisters. Evaluation Review. 1998;22:403–426. [Google Scholar]
- Hamilton MA, Hamilton SF. Work and service-learning. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2005. pp. 348–363. [Google Scholar]
- Heppner PP, Petersen CH. The development and implications of a personal problem solving inventory. Journal of Counseling Psychology. 1982;29:66–75. [Google Scholar]
- Hernandez B, Hayes E, Balcazar F, Keys C. Responding to the needs of the underserved: A peer mentor approach. Psychosocial Process. 2001;14:142–149. [Google Scholar]
- Herrera C, Sipe C, McClanahan WS. Mentoring school-age children: Relationship development in community-based and school-based programs. Philadelphia: Public/Private Ventures; 2000. [Google Scholar]
- Herrera C, Vang Z, Gale LY. Group mentoring: A study of mentoring groups in three programs. Philadelphia: Public/Private Ventures; 2002. [Google Scholar]
- Hirsch BJ, Wong V. After-school programs. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2005. pp. 364–375. [Google Scholar]
- Jackson Y. Mentoring for delinquent children: An outcome study with young adolescent children. Journal of Children and Adolescence. 2002;31:111–122. [Google Scholar]
- Jent JF. Unpublished manuscript. 2004. Group mentoring protocol. [Google Scholar]
- Jent JF, Niec LN. The impact of mentoring on family functioning: A mental health sample. Child and Family Behavior Therapy. 2006;28:43–58. [Google Scholar]
- Norusis MJ. SPSS 14.0 advanced statistical procedures companion. Upper Saddle River, NJ: Prentice Hall; 2005. Linear mixed models; pp. 197–239. [Google Scholar]
- Portwood SG, Ayers PM. Schools. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2005. pp. 336–347. [Google Scholar]
- Reitman D, Murphy MA, Hupp SD, O’Callaghan PM. Behavior change and perceptions of change: Evaluating the effectiveness of a token economy. Child & Family Behavior Therapy. 2004;26:17–36. [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior assessment system for children manual. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Rhodes JE, Bogat GA, Roffman J, Edelman P, Galasso L. Children mentoring in perspective: Introduction to the special issue. American Journal of Community Psychology. 2002;30:149–155. doi: 10.1023/A:1014676726644. [DOI] [PubMed] [Google Scholar]
- Rhodes JE, DuBois D. National research agenda for youth mentoring. Alexandria, VA: MENTOR/National Mentoring Partnership; 2004. Retrieved March 13, 2007, from http://www.mentoring.org/program_staff/researchagenda.pdf. [Google Scholar]
- Rhodes JE, Ebert L, Fischer K. Natural mentors: An overlooked resource in the social networks of young, African American mothers. American Journal of Community Psychology. 1992;20:445–461. [Google Scholar]
- Rhodes JE, Grossman JB, Resch NL. Agents of change: Pathways through which mentoring relationships influence adolescents’ academic adjustment. Child Development. 2000;71:1662–1671. doi: 10.1111/1467-8624.00256. [DOI] [PubMed] [Google Scholar]
- Rhodes JE, Haight WL, Briggs EC. The influence of mentoring on the peer relationships of foster youth in relative and nonrelative care. Journal of Research and Adolescence. 1999;9:185–201. [Google Scholar]
- Rhodes JE, Reddy R, Grossman JB. The protective influence on mentoring on adolescents’ substance use: Direct and indirect pathways. Applied Developmental Science. 2005;9:31–47. [Google Scholar]
- Sukhodolsky DG, Kassinove H, Gorman BS. Cognitive-behavioral therapy for anger in children and adolescents: A meta-analysis. Aggression & Violent Behavior. 2004;9:247–269. [Google Scholar]
- Vostanis P, Feehan C, Grattan E, Bickerton W. Treatment for children and adolescents with depression: Lessons from a controlled trial. Clinical Child Psychology & Psychiatry. 1996;1:199–212. [Google Scholar]
- Watkins S, Pittman P, Walden B. The deaf mentor experimental project for young children who are deaf and their families. American Annals of the Deaf. 1998;143:29–34. doi: 10.1353/aad.2012.0098. [DOI] [PubMed] [Google Scholar]