Abstract
Background
Troponin is the preferred biomarker for risk stratification in non-ST-elevation ACS. The incremental prognostic utility of the initial magnitude of troponin elevation and its value in conjunction with ST segment resolution (STRes) in STEMI is less well-defined.
Methods
Troponin T (TnT) was measured in 1250 patients at presentation undergoing fibrinolysis for STEMI in CLARITY-TIMI 28. STRes was measured at 90 minutes. Multivariable logistic regression was used to examine the independent association between TnT levels, STRes, and 30-day cardiovascular (CV) mortality.
Results
Patients were classified into undetectable TnT at baseline (n=594), detectable but below the median of 0.12 ng/ml (n=330), and above the median (n=326). Rates of 30-day CV death were 1.5%, 4.5%, and 9.5% respectively (P<0.0001). Compared with those with undetectable levels and adjusting for baseline factors, the odds ratios for 30-day CV death were 4.56 (1.72-12.08, P=0.002) and 5.81 (2.29-14.73, P=0.0002) for those below and above the median, respectively. When combined with STRes, there was a significant gradient of risk, and in a multivariable model both baseline TnT (P=0.004) and STRes (P=0.003) were significant predictors of 30-day CV death. The addition of TnT and STRes to clinical risk factors significantly improved the C-statistic (0.86 to 0.90, P=0.02) and the integrated discriminative improvement 7.1% (P=0.0009).
Conclusions
Baseline TnT and 90-minute STRes are independent predictors of 30-day CV death in patients with STEMI. Use of these two simple, readily available tools can aid clinicians in early risk stratification.
Keywords: Risk stratification, STEMI, Troponin, ST-segment resolution
Cardiac troponin is a sensitive and specific marker for myocyte necrosis and has proven prognostic value in non-ST-elevation acute coronary syndromes.1, 2 There has been less investigation of the prognostic value of troponin levels at presentation in ST elevation myocardial infarction (STEMI).1, 3, 4 Although myocyte necrosis and hence troponin elevation is to be expected in all patients with STEMI, quantification of troponin at presentation could offer a simple biochemical assessment of the severity of the initial myocardial insult.
ST segment resolution is also a useful prognostic variable in STEMI patients undergoing fibrinolysis. ST segment resolution measured on a standard 12-lead electrocardiogram 90 minutes after fibrinolysis is correlated with infarct-related artery patency, microvascular reperfusion, and long-term clinical outcomes, and thus is viewed as an integrative, non-invasive marker of the success of pharmacologic reperfusion therapy.5, 6
We therefore hypothesized that, in the setting of fibrinolytic therapy for STEMI, the combination of the quantification of troponin elevation at presentation and the degree of ST segment resolution at 90 minutes would offer additive, dynamic risk stratification, beyond traditional clinical factors. We tested this hypothesis using data from CLARITY-TIMI 28, a clinical trial of pharmacologic reperfusion therapy in STEMI.7
Methods
Study population
In brief, patients 18-75 years presenting ≤12 hours from the onset of ischemic chest pain and found to have a STEMI were to receive aspirin, a fibrinolytic, and heparin (required if they were to receive a fibrin-specific lytic), and were randomized to clopidogrel or placebo.7 Relevant exclusion criteria included evidence of cardiogenic shock. Patients were scheduled to undergo coronary angiography 2-8 days after initiation of therapy to assess late patency of the infarct-related artery, or earlier if clinically indicated. Patients were followed for clinical outcomes and adverse events through 30 days following randomization.
Troponin
A sample of blood was obtained at the time of enrollment and was available for testing in 1250 subjects. There were no clinically meaningful differences in the baseline characteristics of this group and the overall trial cohort (Supplemental Table 1). Cardiac troponin T (TnT) was measured using the Elecsys 2010 (Roche Diagnostics, Indianapolis, IN). The Elecsys TnT Immunoassay has a lower limit of detection of 0.01 ng/ml and a coefficient of variation of 10% at 0.03 ng/ml.
ST segment resolution
Standard 12-lead ECGs before and 90 minutes after pharmacologic reperfusion therapy were analyzed by two physicians at the TIMI ECG Core Laboratory using a handheld electronic caliper. Investigators where blinded to the study drug and clinical outcomes. The percent of ST resolution was categorized using a previously described 3 component definition: complete (>70%), partial (30-70%), and no ST resolution (<30%).8 If the readers' classification disagreed, a third reader was brought in to adjudicate. Of the patients in CLARITY-TIMI 28, 70% had 90-minute ST resolution data available. The reasons for lack of ST resolution data included no 90-minute ECG available (21%), insufficient ST elevation at baseline (8%), and ECGs unintepretable for ST resolution (LBBB, etc. 1%).9 A total of 880 subjects had 90-minute ST resolution data in addition to baseline troponin data. There were no clinically meaningful differences between this cohort and the overall trial cohort (Supplemental Table 1).
Outcomes
Clinical outcomes for this analysis included cardiovascular (CV) death, congestive heart failure (CHF), recurrent MI, and stroke through 30 days of follow-up. Outcomes were defined according to previously reported criteria.7 All ischemic events were adjudicated by a Clinical Events Committee and all angiographic outcomes by the TIMI Angiographic Core Laboratory, both of which were blinded to the assigned treatment arm.
Statistical analyses
Patients were grouped according to troponin values as having undetectable levels, ≤median detectable level, or >median detectable level. Rates of angiographic and clinical outcomes were compared across troponin categories using chi-squared tests for trend. Analyses were then repeated with subjects stratified by categories of ST segment resolution (complete, partial, or none) and then with subjects stratified by both. Troponin was also treated as a continuous variable, for which it was log transformed, with undetectable values coded as an intermediate value (0.005 ng/ml) between 0 and the limit of detection of the assay. Similarly, ST segment resolution was also treated as a continuous variable by adding 400% to all values which then underwent log transformation.
Multivariable logistic regression was used to adjust for all the elements of the TIMI Risk Score for STEMI10 including the following baseline characteristics: time from reported symptom onset to start of reperfusion therapy, age, hypertension, diabetes, prior MI, prior CHF, anterior MI, Killip class, heart rate, systolic blood pressure, and weight. We created receiver operating characteristic curves incorporating clinical variables as well as troponin and ST segment resolution to predict the 30-day CV death risk. C-statistics were calculated and compared between models. We determined the effect on reclassification by calculating the integrated discrimination improvement (IDI), a metric of the net improvement in sensitivity and specificity.11 SAS 8.02 for Windows statistical software (SAS Inc. Cary, NC) was used for all the analyses presented. A P value < .05 was considered statistically significant.
Funding and authorship
CLARITY-TIMI 28 was supported by the pharmaceutical partnership of Sanofi-Aventis and Bristol-Myers Squibb. Reagents for troponin testing were supplied by Roche Diagnostics. Drs. Morrow, Gerszten, and Sabatine were supported in part by grant U01 HL081341 from the NHLBI. The authors are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the paper.
Results
Baseline Characteristics
Of the 1250 patients with baseline troponin data, 594 patients (47.5%) had undetectable levels, 330 (26.4%) patients had low-level elevation (less than or equal to the median detectable troponin level of 0.12 ng/ml), and 326 patients (26.1%) had high-level elevation (greater than the median detectable troponin level). The baseline characteristics across these three groups are shown in Table 1. Patients with higher baseline troponin levels were older, more likely to have a history of hypertension, present with an anterior MI, be categorized as Killip Class II-IV on presentation, and had longer times from reported symptom onset to start of reperfusion therapy.
Table 1.
Baseline Characteristics
| Characteristic | Troponin Undetectable | Troponin ≤ Median (0.01-0.12) | Troponin > Median (0.12-11.08) | P-value for trend |
|---|---|---|---|---|
| Number | 594 | 330 | 326 | … |
| Age (Mean±SD) | 56.3±10.2 | 59.1±9.9 | 59.9±10.4 | <0.0001 |
| Female | 19.0% | 22.4% | 21.5% | 0.42 |
| Hypertension | 35.7% | 38.7% | 46.9% | 0.004 |
| Hyperlipidemia | 45.0% | 36.9% | 36.6% | 0.02 |
| Current smoker | 50.4% | 44.1% | 44.9% | 0.11 |
| Diabetes mellitus | 15.6% | 16.4% | 21.5% | 0.07 |
| Prior MI | 10.0% | 6.7% | 7.4% | 0.17 |
| Prior PCI | 5.9% | 3.6% | 3.1% | 0.09 |
| Prior CHF | 0.8% | 1.2% | 2.2% | 0.24 |
| Anterior MI | 27.4% | 43.0% | 50.3% | <0.0001 |
| Killip Class II-IV | 5.5% | 5.7% | 10.9% | 0.008 |
| Time from symptom onset to fibrinolytic, hrs (IQR) | 2.00 (1.42-2.75) | 2.67 (1.83-3.87) | 3.77 (2.42-5.42) | <0.0001 |
MI=Myocardial Infarction, PCI=Percutaneous Coronary Intervention, CHF=Congestive Heart Failure
Angiographic Findings
The rates of TIMI Flow Grade in the infarct-related artery, TIMI Myocardial Perfusion Grade, degree of stenosis of the infarct-related artery, and extent of coronary disease in patients stratified across troponin categories are shown in Table 2. There were no statistically significant differences in any of these parameters. However, the rate of a closed infarct-related artery or death before angiography could be performed (a reverse surrogate for a closed-infarct related artery) was higher in those patients with higher baseline troponin levels (P=0.0038).
Table 2.
Baseline Troponin and Angiographic Outcomes
| Parameter | Troponin Undetectable | Troponin ≤ Median (0.01-0.12) | Troponin > Median (0.12-11.08) | P-value for trend |
|---|---|---|---|---|
| TFG 0/1 | 13.5% | 12.7% | 17.4% | 0.18 |
| TFG 0/1 or death before angiography | 13.9% | 14.1% | 21.9% | 0.0038 |
| TMPG 0/1 | 48.4% | 43.4% | 45.7% | 0.35 |
| Thrombus | 47.7% | 45.2% | 51.9% | 0.25 |
| Stenosis (Mean±SD) | 69.6±19.6 | 69.3±18.9 | 69.0±21.4 | 0.68 |
| Multivessel CAD or LM ≥ 50% | 30.7% | 34.3% | 36.3% | 0.22 |
TFG=TIMI Flow Grade, TMPG=TIMI Myocardial Perfusion Grade, CAD=Coronary Artery Disease, LM=Left Main
Clinical Outcomes
Rates of cardiovascular death were 3-fold higher in patients with low-level troponin elevation and more than 6-fold higher in patients with high-level troponin elevation, as compared with patients with undetectable troponin (P<0.0001, Table 3). When troponin data were log transformed and then evaluated as a continuous variable, the risk of 30-day CV death was ∼2.5-fold higher per 1-SD increase (OR 2.44, CI 1.88-3.16, P<0.0001). In sensitivity analyses, the association between troponin categories and cardiovascular death was seen both in the 652 patients who received reperfusion therapy within 2.5 hours of symptom onset (0.7% vs. 3.9% vs. 11.2%, P<0.001) and in the 593 patients who received reperfusion therapy >2.5 hours after symptom onset (3.3% vs. 5.1% vs. 9.0%, P=0.013). Of note, we did not find a significant association between baseline CK-MB levels and 30-day mortality, either in terms of the risk per 1-SD of log-transformed CK-MB (OR 0.88, 95% CI 0.63-1.17; P=0.38) or across CK-MB quartiles (3.9%, 2.7%, 2.3%, and 6.4%, P=0.20).
Table 3.
Baseline Troponin and Clinical Outcomes
| Outcome | Troponin Undetectable | Troponin ≤ Median (0.01-0.12) | Troponin > Median (0.12-11.08) | P-value for trend |
|---|---|---|---|---|
| 30-day CV Death | 1.5% | 4.5% | 9.5% | <0.0001 |
| CHF | 1.9% | 3.0% | 5.8% | 0.005 |
| CV Death or CHF | 3.2% | 7.3% | 14.4% | <0.0001 |
| Recurrent MI | 8.6% | 5.5% | 3.7% | 0.01 |
CHF=Congestive Heart Failure, CV=Cardiovascular death, MI=Myocardial Infarction
Similarly, the rates of heart failure and the composite of cardiovascular death or heart failure increased significantly with increasing baseline troponin levels (P=0.005 and P<0.0001, respectively). Conversely, rates of recurrent MI decreased with increasing baseline troponin levels (P=0.01) (Table 3). There was no significant interaction between the benefit of clopidogrel and the degree of baseline troponin elevation (P=NS, data not shown).
ST segment resolution
ST segment resolution data at 90 minutes after presentation were available in 880 patients who also had troponin data. A total of 366 patients (41.6%) had complete ST segment resolution, 276 patients (31.4%) had partial resolution, and 238 patients (27.0%) had no resolution. The rates of poor TIMI Flow Grade in the infarct-related artery and poor TIMI Myocardial Perfusion Grade increased with the lack of ST segment resolution (P<0.0001 and P=0.059 respectively, Table 4). The degree of stenosis and rates of intracoronary thrombus also increased with the lack of ST segment resolution (P=0.0048 and P<0.0001) and are shown in (Table 4) Rates of cardiovascular death were 1.4% in patients with complete ST segment resolution, 4.3% in those with partial resolution, and 7.1% in those with no resolution (P=0.0003, Table 5). When evaluated as a continuous variable, the risk of 30-day CV death was 1.32 (95% CI 1.08-1.63, P=0.0068) per 1-SD decrease in log transformed ST segment resolution. Rates of CHF and the composite rates of heart failure and 30-day CV death also increased significantly with the lack of ST segment resolution (P=0.003 and P<0.0001). Rates of recurrent MI were not significantly related to ST segment resolution. Of note, baseline ST deviation was also associated with 30-day mortality. Dividing patients into those with <8 mm (n=282), 8-14 mm (n=281), and >14 mm deviation (n=283), which approximates tertiles, there was a gradient of 30-day mortality (2.4%, 3.4%, and 5.7%, respectively, P=0.04). However, this gradient was less significant than that across ST resolution categories and in a model with ST resolution, ST deviation was no longer statistically significant (P=0.08).
Table 4.
90-Minute ST Resolution and Angiographic Outcomes
| Parameter | STRes Complete | STRes Partial | STRes None | P-value for trend |
|---|---|---|---|---|
| Median time to angiography, hrs (IQR) | 81.6 (52.7-125.5) | 76.1 (50.9-123.7) | 70.8 (4.6-125.5) | 0.02 |
| TFG 0/1 | 8.9% | 13.6% | 24.2% | <0.0001 |
| TFG 0/1 or death before angiography | 9.2% | 14.9% | 27.2% | <0.0001 |
| TMPG 0/1 | 43.6% | 46.0% | 52.1% | 0.059 |
| Thrombus | 42.1% | 48.7% | 61.2% | <0.0001 |
| Stenosis (Mean±SD) | 67.9±18.6 | 69.8±18.3 | 72.7±21.6 | 0.0048 |
| PCI | 66.1% | 59.1% | 65.1% | 0.16 |
PCI=percutaneous coronary intervention, TFG=TIMI Flow Grade, TMPG=TIMI Myocardial Perfusion Grade
Table 5.
90-Minute ST Resolution and Clinical Outcomes
| Outcome | STRes Complete | STRes Partial | STRes None | P-value for trend |
|---|---|---|---|---|
| 30-day CV Death | 1.4% | 4.3% | 7.1% | 0.0003 |
| CHF | 1.9% | 2.2% | 6.7% | 0.003 |
| CV Death or CHF | 3.3% | 6.5% | 12.6% | <0.0001 |
| Recurrent MI | 9.0% | 3.3% | 9.7% | 0.78 |
CHF=Congestive Heart Failure, CV=Cardiovascular death, MI=Myocardial Infarction
Combined Risk Stratification with Troponin and ST Segment Resolution
Patients with higher baseline troponin values were less likely to achieve complete ST segment resolution at 90 minutes (P=0.002) (Supplemental Table 2). When patients were stratified by baseline troponin level and then by ST segment resolution at 90 minutes (Figure 1), there was a steep and highly significant association with cardiovascular death (P=0.001), with both the level of baseline troponin and the degree of ST segment resolution contributing significantly to the risk prediction (P<0.0001 and P=0.0005, respectively). Cardiovascular death ranged from 0.5% in patients without detectable troponin and complete ST segment resolution to 14.9% in patients with high-level troponin elevation and no ST segment resolution. There was no significant interaction between the degree of troponin elevation and ST resolution and the risk of 30-day cardiovascular mortality (Pinteraction=0.82).
Figure 1. Rates of 30 day cardiovascular death stratified by Troponin and ST resolution.
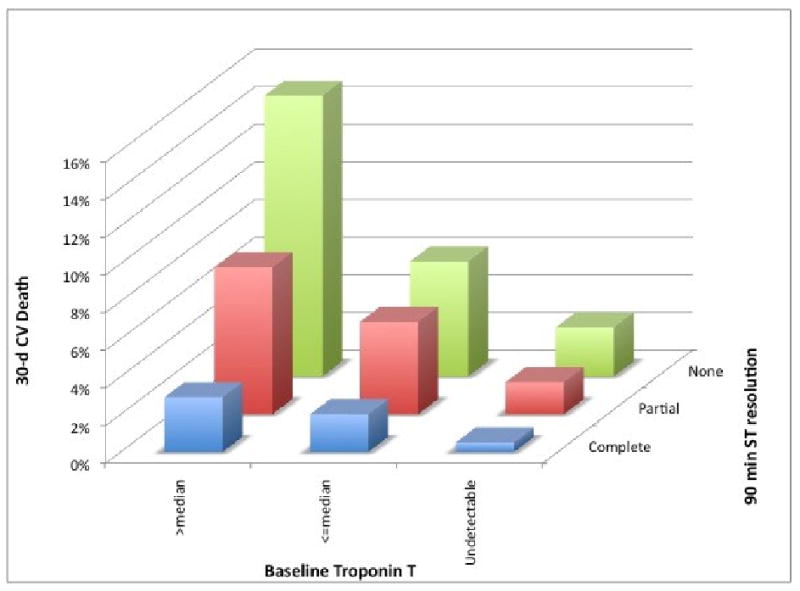
Among patients without detectable troponin elevation and complete ST resolution (n=198), the rate of 30-day cardiovascular mortality were low regardless of whether the patient underwent PCI or did not (0% vs. 1.5%, P=0.16). Among patients with either detectable troponin or incomplete ST resolution (n=401), there was a non-significant lower rate of 30-day cardiovascular mortality among those who underwent PCI compared with those who did not (1.5% vs. 3.8%, P=0.13). In contrast, for those patients with both troponin elevation and incomplete ST resolution (n=281), those who underwent PCI had a significantly lower rate of 30-day cardiovascular mortality compared with those who did not (4.5% vs. 13.7%, OR 0.29, 95% CI 0.12-0.72, P=0.0059).
Multivariable adjusted analyses
After adjustment for time from reported symptom onset to start of reperfusion therapy, age, hypertension, diabetes, prior MI, prior CHF, anterior MI, Killip class, heart rate, systolic blood pressure, and weight, low-level baseline troponin elevation (adjusted OR 4.56, 95% CI 1.72-12.08) and high-level troponin elevation (adjusted OR 5.81, 95% CI 2.29-14.73) remained significant predictors of cardiovascular death (P for trend = 0.0002). Similarly, after adjustment for the clinical factors listed above, ST segment resolution remained a significant predictor of 30-day CV death (P for trend = 0.0005), with partial ST segment resolution having an adjusted OR of 3.96 (95% CI 1.18-13.25) and no ST segment resolution having an adjusted OR of 6.29 (95% CI 1.91-20.72). In a multivariable model containing the aforementioned covariates and both baseline troponin elevation and 90 minute ST segment resolution, both remained significant independent predictors of cardiovascular death (P=0.004 and P=0.003, respectively; Figure 2).
Figure 2. Odds Ratios for 30 day cardiovascular death.
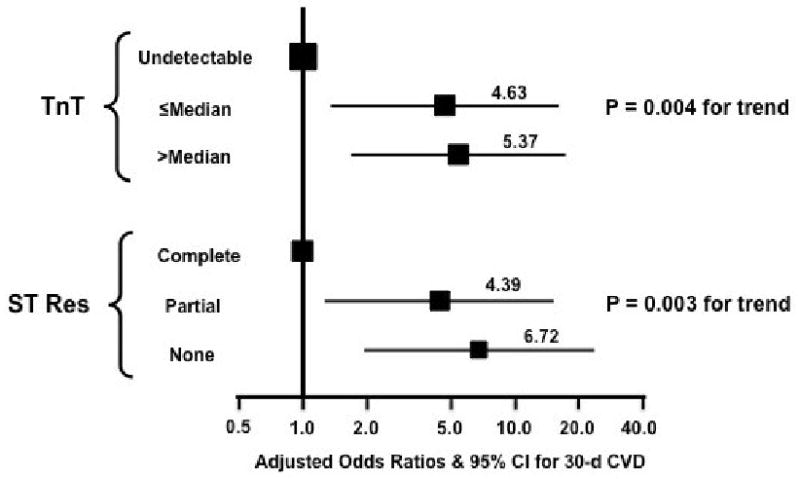
Odds ratios (squares) and 95% confidence intervals (horizontal lines) for the risk of cardiovascular death through 30 days for the magnitude of troponin elevation (undetectable is reference) and the degree of ST segment resolution (complete is reference), adjusted for clinical variables (see Methods).
Discrimination and Reclassification
To evaluate the discriminative ability of baseline troponin and ST segment resolution, we created receiver operating characteristic (ROC) curves for two models to predict the 30-day CV death risk in this population of patients. The first model included the aforementioned clinical variables and had a c-statistic (AUC) of 0.86. The addition of troponin and ST segment resolution significantly improved the c-statistic to 0.90 (P=0.02, Figure 3). In terms of reclassification, addition of troponin and ST segment resolution to the clinical model improved the IDI by 7.1% (P=0.0009). The model was well-calibrated with the Hosmer-Lemeshow test showing no significant deviation of observed from predicted risk (P=0.20).
Figure 3. Receiver Operating Characteristic Curves for 30 day cardiovascular death.
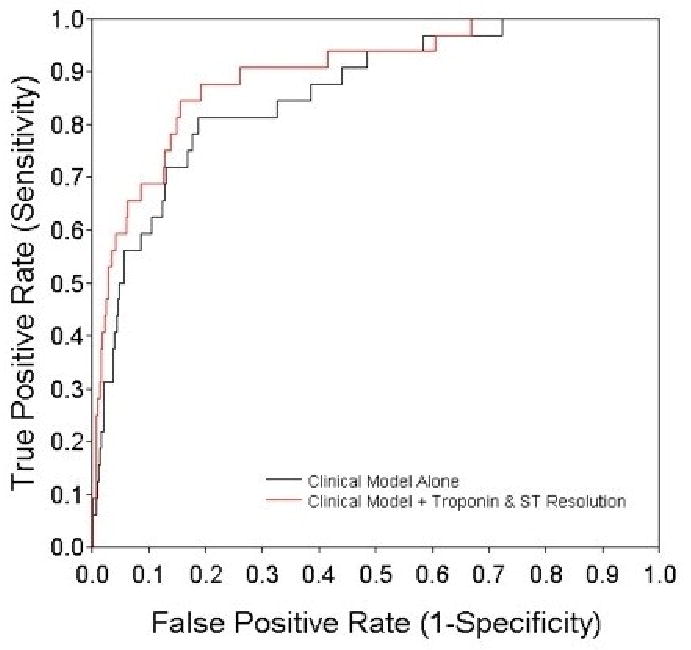
Receiver operating characteristic curves plotting sensitivity by 1-specificity for cardiovascular death through 30 days for a clinical model alone (see Methods) in black (c-statistic 0.86) and the same model plus troponin and ST resolution in red (c-statistic 0.90, P=0.02 for comparison with clinical model alone).
Discussion
In a cohort of patients with STEMI receiving pharmacologic reperfusion therapy, we show that the level of troponin at presentation is a significant, independent predictor of cardiovascular death over the ensuing 30 days. Furthermore, early dynamic risk stratification using baseline troponin and 90-minute ST segment resolution offered significant, complementary risk stratification, superior discrimination, and improved classification.
Our findings for the prognostic significance of baseline troponin in STEMI expand on observations from other studies. Ohman and colleagues showed that an elevated baseline troponin was associated with higher rates of mortality in GUSTO IIA and GUSTO III.1, 3 Some,1, 3, 12 but not all studies,13, 14 demonstrated that baseline troponin was a significant predictor of outcomes independent of baseline clinical characteristics. The latter studies may have been limited by their small sample size; in fact, most of the prior studies were less than half the size of our study. Similar findings have been observed in the setting of primary PCI,4, 15 although again the studies have been on the order of one or two hundred subjects.
Of note, most of the prior studies have treated troponin as a simple dichotomous variable, being either positive or negative. Building on our group's prior experience demonstrating the prognostic value of the magnitude of troponin elevation in the setting of non-ST-elevation acute coronary syndromes,2, 16 we now show that the risk of cardiovascular death in STEMI is related not just to the presence but the degree of troponin elevation at presentation.
We and others have demonstrated the prognostic significance of ST-segment resolution in patients with STEMI.5, 6, 9, 17 We now take the next logical step and demonstrate the value of dynamic risk utilizing both the magnitude of troponin elevation at baseline and the degree of ST segment resolution at 90 minutes. This approach builds on the prior work of Frostfeld et al.13 and Bjorklund et al.,14 both of whom examined troponin elevation and ST segment analysis in patients with STEMI receiving fibrinolytic therapy. Although their results qualitatively support our findings, in neither study did both factors remain significant predictors of mortality after multivariable adjustment. With a larger sample size and finer categorization of troponin elevation and ST-segment resolution, we were now able to demonstrate definitively the prognostic value of both factors. We also used receiver operating characteristic curves to demonstrate that the addition of troponin and ST segment resolution to traditional clinical risk factors significantly increases discriminative ability and classification for 30-day CV death. We believe that the 30-fold mortality gradient identified using these two variables and the significant additional value demonstrated using both established and novel statistical tools justifies their inclusion among the traditional markers of risk in STEMI patients.
This study was not designed to define the mechanisms underlying the prognostic significance of troponin elevation and ST segment resolution. Nonetheless, based on prior data and our findings in this study with regard to which baseline characteristic were associated with troponin levels, we speculate that troponin elevation represents a biochemical, quantifiable integrated assessment of both the duration of ischemia and extent of myocardium at risk. With respect to the former, we suspect that troponin level remains a significant predictor of cardiovascular death even after adjusting for time from symptom onset to initiation of reperfusion therapy because symptom onset is highly subjective. ST segment resolution then complements troponin elevation by reflecting the response to fibrinolytic therapy, both in epicardial flow and myocardial perfusion.5, 17 In terms of re-infarction, rates were inversely associated with increasing troponin levels. We speculate that those patients with the highest troponin levels on admission had already sustained a large amount of myocardial damage and thus were less likely to experience a recurrent MI from the same infarct artery. Surprisingly, there was no association detected between ST resolution and recurrent MI.
In terms of clinical applicability, troponin assays are readily available, recommended to be measured on presentation in all patients presenting with STEMI, and results can be available within 60 minutes. Similarly, ST resolution is easily calculated from the standard 12-lead ECGs recommended to be obtained in all patients presenting with STEMI. Thus, within 90 minutes both of these variables are routinely available to be added to baseline risk factors to allow early dynamic risk stratification. Although our study was observational and does not address altering therapy in response to these factors, we think it reasonable to consider tailoring management based on these data. Specifically, patients with both an undetectable troponin level at presentation and complete ST segment resolution at 90 minutes are at low risk for cardiovascular death (0.5%). In contrast, those with some degree of troponin elevation and incomplete ST resolution are at high risk for cardiovascular death (5 to 15%). Although not randomly allocated in this study, the patients in this subgroup who underwent PCI had a markedly lower risk of 30-day cardiovascular mortality than those who did not. Thus we hypothesize that these patients might benefit from early transfer to a tertiary care center where mechanical reperfusion and mechanical left ventricular support could be initiated promptly.
There are several potential limitations to our study. First, the study population excluded patients older than 75 years of age, those presenting >12 hours after symptom onset and those with shock; therefore, we cannot comment on the generalizability of our findings to such individuals. Also, all patients received fibrinolytic therapy; our findings may not be applicable to patients undergoing primary PCI or receiving no reperfusion therapy. Patients in whom ST segment resolution cannot be assessed (e.g., those with left bundle branch block or ventricularly paced rhythms) would not be able to be risk stratified using this approach. Alternative ECG metrics of successful reperfusion including single lead ST elevation resolution, single lead ST elevation residual, summed ST elevation resolution, and summed ST deviation (elevation or depression) residual have been studied.18-20 All appear to be roughly comparable to summed ST deviation resolution, with no alternative metric prospectively validated to be clearly superior. We did not have single lead ST data available, but future analyses combining such metrics with baseline troponin hold the promise of further facilitating risk stratification by clinicians. Other investigators have demonstrated the significant impact of in-hospital complications over the first week on 30-day mortality.21, 22 We did not include in-hospital complications over the first week in our model. Rather, our aim was to achieve early risk stratification using easily available biochemical data and electrocardiographic information within the first 90 minutes as this is a the time period in which decisions for transfer to a tertiary care center are typically made.
Conclusions
In patients with STEMI receiving fibrinolytic therapy, two readily available parameters, the magnitude of baseline troponin elevation and the degree of ST-segment resolution at 90 minutes, can be combined with baseline risk factors to provide early dynamic risk stratification. These two factors allow patients to be classified across a 30-fold gradation of 30-day cardiovascular mortality risk.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ohman EM, Armstrong PW, Christenson RH, Granger CB, Katus HA, Hamm CW, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med. 1996;335(18):1333–41. doi: 10.1056/NEJM199610313351801. [DOI] [PubMed] [Google Scholar]
- 2.Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. New England Journal of Medicine. 1996;335(18):1342–9. doi: 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 3.Ohman EM, Armstrong PW, White HD, Granger CB, Wilcox RG, Weaver WD, et al. Risk stratification with a point-of-care cardiac troponin T test in acute myocardial infarction. GUSTOIII Investigators. Global Use of Strategies To Open Occluded Coronary Arteries. Am J Cardiol. 1999;84(11):1281–6. doi: 10.1016/s0002-9149(99)00558-5. [DOI] [PubMed] [Google Scholar]
- 4.Matetzky S, Sharir T, Domingo M, Noc M, Chyu KY, Kaul S, et al. Elevated troponin I level on admission is associated with adverse outcome of primary angioplasty in acute myocardial infarction. Circulation. 2000;102(14):1611–6. doi: 10.1161/01.cir.102.14.1611. [DOI] [PubMed] [Google Scholar]
- 5.de Lemos JA, Braunwald E. ST segment resolution as a tool for assessing the efficacy of reperfusion therapy. J Am Coll Cardiol. 2001;38(5):1283–94. doi: 10.1016/s0735-1097(01)01550-9. [DOI] [PubMed] [Google Scholar]
- 6.Anderson RD, White HD, Ohman EM, Wagner GS, Krucoff MW, Armstrong PW, et al. Predicting outcome after thrombolysis in acute myocardial infarction according to ST-segment resolution at 90 minutes: a substudy of the GUSTO-III trial. Global Use of Strategies To Open occluded coronary arteries. Am Heart J. 2002;144(1):81–8. doi: 10.1067/mhj.2002.123319. [DOI] [PubMed] [Google Scholar]
- 7.Sabatine MS, Cannon CP, Gibson CM, Lopez-Sendon JL, Montalescot G, Theroux P, et al. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med. 2005;352(12):1179–89. doi: 10.1056/NEJMoa050522. [DOI] [PubMed] [Google Scholar]
- 8.Schroder R, Wegscheider K, Schroder K, Dissmann R, Meyer-Sabellek W. Extent of early ST segment elevation resolution: a strong predictor of outcome in patients with acute myocardial infarction and a sensitive measure to compare thrombolytic regimens. A substudy of the International Joint Efficacy Comparison of Thrombolytics (INJECT) trial. J Am Coll Cardiol. 1995;26(7):1657–64. doi: 10.1016/0735-1097(95)00372-x. [DOI] [PubMed] [Google Scholar]
- 9.Scirica BM, Sabatine MS, Morrow DA, Gibson CM, Murphy SA, Wiviott SD, et al. The role of clopidogrel in early and sustained arterial patency after fibrinolysis for ST-segment elevation myocardial infarction: the ECG CLARITY-TIMI 28 Study. J Am Coll Cardiol. 2006;48(1):37–42. doi: 10.1016/j.jacc.2006.02.052. [DOI] [PubMed] [Google Scholar]
- 10.Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102(17):2031–7. doi: 10.1161/01.cir.102.17.2031. [DOI] [PubMed] [Google Scholar]
- 11.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. doi: 10.1002/sim.2929. discussion 207-12. [DOI] [PubMed] [Google Scholar]
- 12.Stubbs P, Collinson P, Moseley D, Greenwood T, Noble M. Prognostic significance of admission troponin T concentrations in patients with myocardial infarction. Circulation. 1996;94(6):1291–7. doi: 10.1161/01.cir.94.6.1291. [DOI] [PubMed] [Google Scholar]
- 13.Frostfeldt G, Gustafsson G, Lindahl B, Nygren A, Venge P, Wallentin L. Possible reasons for the prognostic value of troponin-T on admission in patients with ST-elevation myocardial infarction. Coron Artery Dis. 2001;12(3):227–37. doi: 10.1097/00019501-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Bjorklund E, Lindahl B, Johanson P, Jernberg T, Svensson AM, Venge P, et al. Admission Troponin T and measurement of ST-segment resolution at 60 min improve early risk stratification in ST-elevation myocardial infarction. Eur Heart J. 2004;25(2):113–20. doi: 10.1016/j.ehj.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 15.Giannitsis E, Muller-Bardorff M, Lehrke S, Wiegand U, Tolg R, Weidtmann B, et al. Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction. Circulation. 2001;104(6):630–5. doi: 10.1161/hc3101.093863. [DOI] [PubMed] [Google Scholar]
- 16.Morrow DA, Cannon CP, Rifai N, Frey MJ, Vicari R, Lakkis N, et al. Ability of minor elevations of troponins I and T to predict benefit from an early invasive strategy in patients with unstable angina and non-ST elevation myocardial infarction. JAMA. 2001;286:2405–2412. doi: 10.1001/jama.286.19.2405. [DOI] [PubMed] [Google Scholar]
- 17.Schroder R, Wegscheider K, Schroder K, Dissmann R, Meyer-Sabellek W. Extent of early ST segment elevation resolution: a strong predictor of outcome in patients with acute myocardial infarction and a sensitive measure to compare thrombolytic regimens. A substudy of the International Joint Efficacy Comparison of Thrombolytics (INJECT) trial. J Am Coll Cardiol. 1995;26(7):1657–64. doi: 10.1016/0735-1097(95)00372-x. [DOI] [PubMed] [Google Scholar]
- 18.Zeymer U, Schroder K, Wegscheider K, Senges J, Neuhaus KL, Schroder R. ST resolution in a single electrocardiographic lead: a simple and accurate predictor of cardiac mortality in patients with fibrinolytic therapy for acute ST-elevation myocardial infarction. Am Heart J. 2005;149(1):91–7. doi: 10.1016/j.ahj.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 19.De Luca G, Maas AC, Suryapranata H, Ottervanger JP, Hoorntje JC, Gosselink AT, et al. Prognostic significance of residual cumulative ST-segment deviation after mechanical reperfusion in patients with ST-segment elevation myocardial infarction. Am Heart J. 2005;150(6):1248–54. doi: 10.1016/j.ahj.2005.01.056. [DOI] [PubMed] [Google Scholar]
- 20.Buller CE, Fu Y, Mahaffey KW, Todaro TG, Adams P, Westerhout CM, et al. ST-segment recovery and outcome after primary percutaneous coronary intervention for ST-elevation myocardial infarction: insights from the Assessment of Pexelizumab in Acute Myocardial Infarction (APEX-AMI) trial. Circulation. 2008;118(13):1335–46. doi: 10.1161/CIRCULATIONAHA.108.767772. [DOI] [PubMed] [Google Scholar]
- 21.Chang WC, Boersma E, Granger CB, Harrington RA, Califf RM, Simoons ML, et al. Dynamic prognostication in non-ST-elevation acute coronary syndromes: insights from GUSTO-IIb and PURSUIT. Am Heart J. 2004;148(1):62–71. doi: 10.1016/j.ahj.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Chang WC, Kaul P, Fu Y, Westerhout CM, Granger CB, Mahaffey KW, et al. Forecasting mortality: dynamic assessment of risk in ST-segment elevation acute myocardial infarction. Eur Heart J. 2006;27(4):419–26. doi: 10.1093/eurheartj/ehi700. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


