Abstract
Bone marrow derived stem cells administered after minimal manipulation represent an important cell source for cellbased therapies. Clinical trial results, have revealed both safety and efficacy of the cell reinfusion procedure in many cardiovascular diseases. Many of these early clinical trials were performed in a period before the entry into force of the US and European regulation on cellbased therapies. As a result, conflicting data have been generated on the effectiveness of those therapies in certain conditions as acute myocardial infarction. As more academic medical centers and private companies move toward exploiting the full potential of cellbased medicinal products, needs arise for the development of the infrastructure necessary to support these investigations. This review describes the regulatory environment surrounding the production of cell based medicinal products and give practical aspects for cell isolation, characterization, production following Good Manufacturing Practice, focusing on the activities associated with the investigational new drug development.
Keywords: “Good Manufacturing Practice”, “Acute Myocardial Infarction”, “Peripheral Vascular Disease”, “Stem Cells”, “Advanced Therapy Medicinal Products”, “Cell Factory”
Introduction
Stem-cell–based therapies, encompassing collection, purification, manipulation, characterization delivery of cells for therapeutic purposes, have existed since the first successful bone marrow transplantations in 1968 [1]. The Food and Drug Administration (FDA) promulgated a regulation on human cells, tissues, and cellular and tissuebased products issuing an appropriate regulatory structure for the wide range of stem-cell–based products that may be developed to regenerate damaged tissues. The publications regulating the use of cell therapy products are codified within the Code of Federal Regulations in the following sections: IND regulations (21 CFR 312), biologics regulations (21 CFR 600) and cGMP (21 CFR 211). In particular, US Federal regulation on cellular therapy is divided into two sections of the Public Health Service Act, referred as“361 products”and “351 products”. Traditional blood and bone marrow progenitor cells as well as other tissues for transplantation fall into 361 products definition. The FDA has established that cells or tissues used for therapeutic purposes, and the regulation that pertain to processing of 361 products are codified under the Good Tissue Practice (GTP).
The European Union (EU) regulation (1394/2007) on advanced therapy medicinal products (ATMP) was entered into force in all European Member States on December 2008. The Regulation makes reference to and is in coherence with the 2004/23/EC directive on donation, procurement and testing of human cells and tissues and with directive 2002/98/ EC on human blood and blood components. This means that any use of human cells has to be in compliance with the quality requirements therein described. Both EU and US regulations are also clear on requiring that cells have to be prepared according to the good manufacturing practice (GMP) for medicinal products.
The concept that adult stem/progenitor cells can differentiate either in haematopoietic or non-haematopoietic tissues is supported by a relevant amount of data[2]: adult stem cells are located in tissues throughout the body and act as a reservoir to replace damaged tissues and senescent cells. This large amount of preclinical data drove the introduction of several stem/progenitor cells into regenerative medicine with different extent of therapeutic benefit. Based on these concepts, progenitor cells have been considered as pharmaceutical products. Adult mononucleated cells (MNC), containing the stem/progenitor cell fraction, can be isolated from mobilized peripheral blood and bone marrow tissue using density gradients [3].
Despite the similar physical properties, bone marrow derived MNC (BM-MNC) represent a heterogeneous group of cells, which include several stem/progenitor cells: the haematopoietic stem cells (HSC), the mesenchymal stromal/stem cell (MSC) precursors, and the endothelial progenitor cells (EPC).
HSC constitute 1:10.000 of cells in myeloid tissue and give rise in vitro and in vivo to all blood progeny [4]. This cell pool is represented by both longterm repopulating HSC, with high selfrenewal capacity, and short term repopulating HSC, which can transiently generate haematopoietic lineages after transplantation [5]. Both these populations are identified by the cellsurface antigen CD34, found in a few percent of BM-MNC, and by other haematopoietic restricted antigens, such as CD38, HLA-DR[6] and CD133[7]. BM-MNC contain also the fraction of MSC precursors [5]. These cells represent less than 0.1% of the density gradient selected cells and are able to generate non-haematopoietic tissues such as adipocytes, chondrocytes and osteocytes [8, 9]. Interestingly, rising amount of data indicate that MSC precursors may also differentiate into skeletal myocytes, cardiomyocytes and endothelial cells [10].
EPC act as major players in marrow angiogenesis due to their relevant clonogenic potential [11]: these cells are also mobilized into the peripheral blood, giving rise to mature endothelial cells in newly formed vessels after either injury (i.e myocardial infarction) or tumors [12]. Based on these findings, a model has been suggested in which marrow EPC may represent a reservoir for the entire body angiogenesis and vasculogenesis [13].
Based on this representation, several authors indicate the revascularization as leading mechanism to improve cardiac function, prompting local BM-MNC deliveries as a strategy to enhance dramatically the contribution of EPC to injured hearts [14]. Hill et al [15] developed a clusterforming assay, by preplating human peripheral blood mononuclear cells for 48 hours on fibronectin coated dishes and then replating the nonadherent cells to quantify the emergence of the EPC colony–forming units several days later. The putative EPCs (that produce the progeny that form the colony) have been referred to as colony forming unit-Hill (CFU-Hill). The CFU-Hill assay has been used to demonstrate a significant inverse correlation between the circulating CFU-Hill concentration and Framingham cardiovascular risk score in human subjects. While functional data are supporting these approaches, there is no consensus on defined surface antigens useful in progenitor isolation within the marrow compartment and in blood. However, because CD34 antigen is expressed in both HSC and endothelial cells, Asahara et al., injecting CD34+ marrow cells in a limb ischemia model, indicate in this subtype a possible phenotypic marker for EPC [16]. Similarly, CD133+ marrow cells have been suggested as subsets of progenitors highly enriched in EPC [17]. When defining an EPC, one should attempt to encompass much of the vast array of data obtained from in vitro and in vivo experiments in animal models and in human subjects. The term as commonly used today, would indicate that a human EPC is a circulating cell that promotes neovascularization at sites of ischemia, hypoxia, injury, or tumor formation. However, in the strictest sense of defining a cell that displays postnatal vasculogenic activity, a human EPC is a circulating cell that displays the ability to produce endothelial progeny that function to form endothelial tubes in vitro and contribute to the functional endothelial lining of injured or de novo emergent vascular structures in vivo. To date, the only cells that display this activity at a clonal level are the so called Endothelial Colony Forming Cells (ECFC) [18, 19].
Apart from myocardial and vascular regeneration as mechanisms of stem cell action, other mechanisms have been proposed. For some authors in many cases the frequency of stem cell engraftment and the number of newly generated cardiomyocytes and vascular cells, either by transdifferentiation or cell fusion, appear too low to explain the significant cardiac improvement described. Accordingly, an alternative hypothesis has been proposed [20-22]: the transplanted stem cells release soluble factors that, acting in a paracrine fashion, contribute to cardiac repair and regeneration. Indeed, cytokines and growth factors can induce cytoprotection and neovascularization. It has also been postulated that paracrine factors may mediate endogenous regeneration via activation of resident cardiac stem cells. Furthermore, cardiac remodeling, contractility, and metabolism may also be influenced in a paracrine fashion.
One of the most relevant aspects for cellbased medicinal products is the scarce availability of classical toxicology studies from the preclinical development. Due to the characteristic of the xenogenic relation, the human cells may be administered only to immunedeficient animals to avoid the host rejection of the donor cells. Homologous models using cells from the same species and strain to simulate the behavior of the cellbased medicinal product are suggested but might be of limited value due to the known and unknown differences in cell physiology between species. In presence of a reduced preclinical section, it is required that the clinical study should be performed with the highest attention to the safety and ethical issue involved. A strong risk analysis should guide the sponsors to perform the best clinical development possible with the lowest risk for the patients involved.
Bone marrow derived mononucleated cells for cardiac regeneration
Despite significant advances in medical practice and interventional strategy, ischemic heart disease (IHD) remain a major cause of mortality and morbidity worldwide [23]. The interest in utilizing adult BM-MNC for cardiac regeneration began after a report that highly purified murine transgenic haematopoietic stem cells contributed to the regeneration of cardiac muscle, following direct injection of the cells into the site of the induced myocardial infarction [24, 25]. Animal models have documented that transplantation of BM-MNC following acute myocardial infarction (AMI) and in ischemic cardiomyopathy (ICM) is associated with a reduction of the scar size and with an improvement of the left ventricular ejection fraction (LVEF) and tissue perfusion [26]. There is now clear evidence that BM-MNC engraft, survive and grow within the infarcted myocardium by forming junctional complexes with resident myocytes expressing at their interface connexin 43 and N-cadherin [27]. Starting from these promising findings, several clinical trials have been conducted analyzing the effects of intracoronary BM-MNC injection in patients with AMI successfully treated by primary percutaneous coronary intervention. Results of the main clinical trials are reported in Table 1. Likewise, in other trials, patients were treated by direct intramyocardial injection during coronary artery bypass graft surgery (CABG) mostly in the border zone of the infarcted myocardium[28].
Table 1.
Randomized clinical trials of intracoronary treatment with bone marrow cells after AMI
| Authors | Trial | N° of patients | Days after AMI | Follow up, months | LVEF Outcome treatment vs control |
|---|---|---|---|---|---|
| Wollert et al. [66], 2004 | BOOST | 60 | 4.8 | 6 | 6.7% vs 0.7% |
| Meyer et al., [67] 2006 | BOOST | 60 | 4.8 | 18 | 5.9% vs 3.1% |
| Schächinger et al., 2006 [68] | REPAIR-AMI | 204 | 3-7 | 6 | 5.5% vs 3.0% |
| Lunde et al., 2006 [72] | ASTAMI | 100 | 4-8 | 6 | 3.1% vs 2.1% |
| Huikuri et al., 2008 [69] | FINCELL | 80 | Morning of stenting | 6 | 7.1% vs 1.2% |
| Nijveldt et al., 2008 [70] | HEBE | 200 | 5-7 | 4; 12 | 2.3% vs 2.3% |
| Tendera et al., 2009 [71] | REGENT | 200 | 3-12 | 6 | 3.0% vs 0% |
Although promising, these preliminary trials reveal the typical heterogeneity of phase one clinical trials driven by academic groups. As a result, it is now difficult to clearly compare outcomes: studies differ for sample size, mean follow-up duration, disease, route of injection (intracoronary, intramyocardial, or via transendocardial delivery using electromechanical mapping system), cell type (unseparated whole BM, BM-MNC, circulating progenitor cells, EPC, mobilized peripheral blood, selected CD34+ or CD133+ cells) [29, 30]. Abdel-Latif et al. published a systematic review and meta-analysis of the literature, evidencing that BMC transplantation is safe and associated with modest improvements in left ventricular function, remodeling and scar size in patients with both AMI and ICM: although the benefit seems modest, the results support the need for further large randomized trials [31]. Actually our own group figures as co-organizer of the randomized, multicenter SWISS-AMI trial[32], that aims to analyze the optimal time point of BM-MNC treatment after AMI. Worldwide, in further 25 registered clinical trials patients with AMI are actively recruited for BM-MNC based therapy. Nine groups are recruiting patients with ICM to be treated with such a therapy (clinicaltrials.gov).
BMC in peripheral vascular disease
Despite recent advances in surgical and interventional techniques, a large percentage (about 40%) of patients with critical limb ischemia (CLI) is not eligible for revascularization procedures due to the anatomical location of the lesions, the extent of the disease or extensive comorbidity [33, 34]. No effective pharmacological therapy is available [35, 36].
Amputation is often the only option but is associated with even worse prognosis: perioperative mortality is 5-20%, a second amputation is required in 30% of cases and full mobility is achieved in only 25-50% of patients. Consequently, EPC have been identified as a potential new therapeutic target.
In animal experiments, injection of ex vivo expanded EPC or BM cells, augmented neovascularization in hind limb or myocardial ischemia [37-42]. In 2002 the TACT Study Investigators showed that intramuscular injection of autologous BM-MNC in ischemic legs (n=45) was safe and significantly improved anklebrachial pressure index, transcutaneous oxygen pressure, rest pain and painfree walking time at 4 and 24 weeks. A preliminary uncontrolled study in 7 patients with CLI showed that intra-arterial infusion of autologous peripheral blood-derived progenitor cells was safe and feasible and improved anklebrachial pressure index, transcutaneous oxygen pressure and endotheliumdependent vasodilatation at 12 weeks [43].
In the uncontrolled trial study of Kawamura et al., [44] intramuscular administration of autologous PB-MNC could prevent limb amputation in 22 out of 30 ischemic limbs. In another trial, intramuscular injection PB-MNC also caused a significant improvement of clinical manifestations in 5 patients with severe arteriosclerosis obliterans of lower extremities [45], and in a randomized open controlled clinical trial on 28 diabetic patients with CLI, cell treatment improved critical limb ischemia [46].
The TAM-PAD trial analyzed combined intra-arterial and intramuscular BMC transplantation in 13 patients with CLI due to peripheral arterial disease. Cells were injected intramuscular and intra-arterial into the ischemic limb. In contrast to the control group, after 2 months the pain-free walking distance of the transplanted patients significantly increased from 147 to 500 meters and the ankle-brachial index was also significantly improved. Similar improvement was documented in capillaryvenous oxygen-saturation and venous occlusion plethysmography; after 13 months the positive effects persisted at their improved level.
More recently, the effect of exclusive intramuscular (IM) versus combined intra-arterial/ intra-muscular (IA+IM) delivery of autologous BMC was evaluated in patients with CLI who were not candidates for surgical or endovascular treatment: 27 patients were treated with either combined IA+IM (n=12) or sole IM (n=15) administration. BMC treatment resulted in a significant and sustained (>12 months) improvement. Authors concluded that both intramuscular and combined intramuscular/intra-arterial delivery of autologous BMC resulted in relevant and sustained improvement in a considerable proportion of patients with severe PAD not amenable for conventional treatment [47]. Cobellis et al., investigated the longterm effects of repeated BM-MNC cell transplantation in 10 patients with severe PAD and CLI [48]. Substantial improvement of blood flow and increasing capillary densities were seen when compared with a concomitant control group. The ankle–brachial index (ABI) and painfree walking distance improved significantly in treated patients. The improvement was sustained 12 months after treatment. At the moment, about 14 clinical studies are registered in clinicaltrials.gov to evaluate the efficiency of the intra-arterial administration of BMC into an ischemic limb.
Bone Marrow Cells in other diseases
The great plasticity of BM-MNC has been clearly reported: beside the generation of cardiomyocytes, there are evidences that BM-MNC can generate skeletal muscle. Muscle regeneration and repair are though to be carried out by muscle-specific stem cells called satellite cells. Derivation of skeletal muscle myocytes from BM -MNC has been studied in human and in mouse models of degenerative muscle disease [13, 49]. Conversion of BMC to hepatocytes has been evidenced in animal models [50] and in humans [51]. A safety study of autologous BM-MNC in liver cirrhosis is in course at the Federal University of Rio de Janeiro (NCT00382278). Patients with moderate liver dysfunction and waiting time expectancy of liver transplantation longer than 12 months are infused with Technetium 99m through the hepatic artery. Scintigraphy is performed 2 and 24 hrs after infusion and evaluated over a period of 12 months.
Has been also evidenced that BMC can differentiate in pancreatic endocrine-cells without cell fusion [52, 53] and BM-derived pancreatic islet cells were shown to be functional in a mouse model of chemically induced diabetes [53]. In a clinical trial promoted by the university of Shan-dong Qilu University Hospital (NCT00465478), patients with Diabetes mellitus type I/II are transplanted with autologous BM mononucleated cells (BM-MNC) through the splenic artery with the distal lumen occlusion by means of an arterial catheter.
Several papers also suggested that BM-MNC can differentiate into central nervous system (CNS) cells, including neurons, oligodendrocytes and astrocytes, both in vivo and in vitro (reviewed in Grove et a [54]). In a clinical trial promoted by the Imperial College of London (NCT00535197), ten patients with ischemic stroke will be transplanted with autologous BM selected CD34+ cells. The immunoselected cells will be directly infused into the area of the stroke intra-arterially using the middle cerebral artery. At the federal University of Rio de Janeiro, 10 patients with ischemic stroke within the middle cerebral artery territory will be transplanted with up to 500x106 autologous BM-MNC injected into the middle cerebral artery through a percutaneous approach. Changes in neurological deficits and improvements in functions will be evaluated at baseline and at regular intervals during 4 months follow-up.
Cell processing
Manufacture of cells as medicinal products, requires compliance with all aspects of GMP regulations. The first step to developing a cell therapy program is the design, construction and validation of the physical infrastructure dedicated to this project [55, 56]. The GMP facility is relied on to control environmental contamination and thereby generates a sterile product. Aseptic techniques are used throughout product manufacture to control contamination. Maintaining aseptic technique drives the construction, design and function of GMP facilities. Aseptic technique (Figure 1) is maintained through environmental controls (including air filtration systems and routine cleaning and maintenance programs), control of critical materials, and personnel training and physical isolation (gowning). The entire manufacturing process of an advanced therapy medicinal product, including the marrow collection and transportation, the cell manipulation including packaging and the final transportation should be validated according to ICH [57] with the aim to demonstrate that each step of the manufacturing process is well controlled. Furthermore, aseptic processing should be validated and critical points of the manufacturing process defined.
Figure 1.
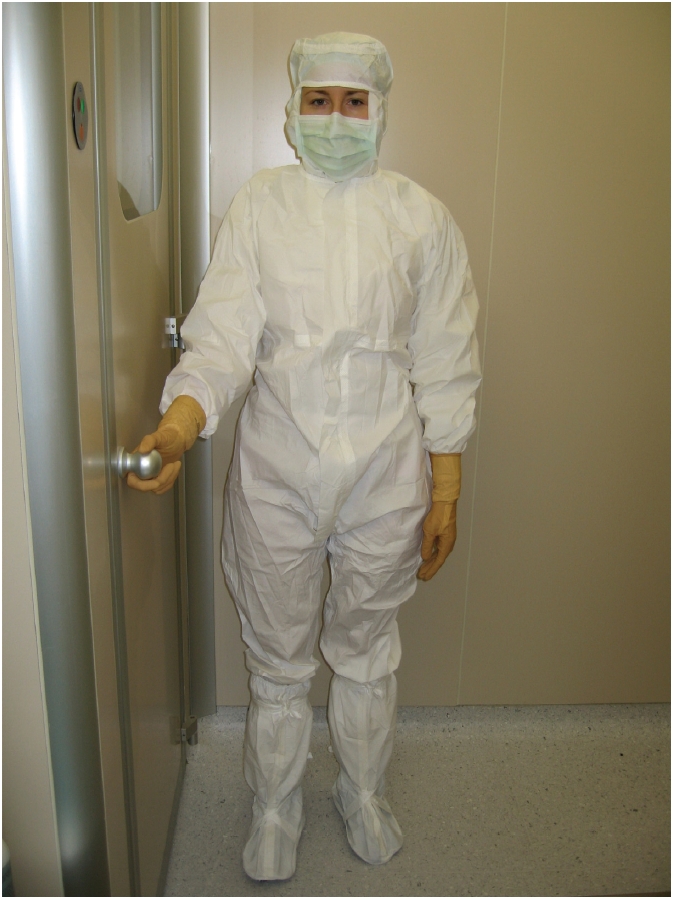
Special gowning for entry in a controlled contamination area
Qualified medical professionals should collect BM-MNC; sample contamination with PB can be minimized and BM collection maximized by limiting the aspiration volume per puncture. Cells should be sent to the production facility under controlled temperature. The limit storage time for the unmanipulated cells should be determined based on stability testing of the final product.
Virological screening must be performed on starting material in accordance with current national regulations [58, 59] before entering the GMP facility. Once received, BM cells could be fractionated or immunoselected for a defined cell population. As a condition, all reagents and buffer used during cell manipulation should be produced under GMP and complete traceability of the lot should be available. MNC cells could be typically separated from other physically different cells such as erythrocytes and granulocytes after density gradient centrifugation (1.073-1.077 g/ml). The BM sample is typically filtered by using a 100 μm cell strainer, diluted in a suitable buffer (e.g. 0.9% saline or D -PBS) and manually layered on the density gradient. Cells are then centrifuged (e.g. 400xg for 30-40 min at room temperature) and the MNC ring collected. Cells are then washed and centrifuged typically at 60-100xg for 10 min at room temperature.
The cellwashing step should be optimized in order to ensure the clearance under the permitted daily exposure (PDE) for the extractable compounds constituting the density gradient medium. Cells are then filtered using a 70 μm cell strainer and resuspended in a defined volume in an injectable media. A sample of the final product must be retained for QC analysis. If the MNC cells are used for cardiac regeneration by intracoronary administration, cells are typically resuspended in 10 ml of an injectable media and aspirated in a luerlock syringe. The syringe is defined as the primary container and should be labeled as indicated by GMP.
Density gradient separation could be performed also automatically in a closed system, reducing the risk of cell contamination by using automated cell separators or elutriators now available on the market.
The use of sedimenting agents able to remove RBC and PLT from the bone marrow sample have been purposed and used in clinical protocols of cardiac regeneration [60]: the BM is filtered by using a 200 μm blood infusion filter and mixed with 50% v/v of a solution of gelatinpolysuccinate or hydroxyethylstarch, two commonly used plasma substitutes; cells are then separated without centrifugation at room temperature, recovered, extensively washed and resuspended in a suitable media.
When a specific cell subpopulation is required, cells should be selected by immunomagnetic labeling and washed in a closed system: the application of a selection procedure is limited to those antigens for which clinical grade anti-bodies are available.
The cell product must be subjected to release testing: should be visually assessed for integrity, correct labeling, and absence of macroaggregates. An acceptance cell viability range should be specified based on preclinical and/or clinical observations [61] and the minimum and maximum cell content should be declared based over safety considerations related to the site and route of implantation. For selected cell populations, the percentage of cell purity should be specified as well as the limit acceptance for undesired populations (RBC, PLT, granulocytes, etc). The quantification of endotoxin content of the cell product by using the methods described in the EU or US pharmacopeia constitutes a release criteria [62].
A shelf life should be assigned to the cell product once released and should be supported by experimental data with regard to the maintenance of cell integrity and product stability during the defined period of validity. Once released, a container able to maintain the declared temperature for the maximum interval of time established should be used and the temperature monitored. The identity the cell therapy product should be defined in terms of its phenotypic profile. Cells should be characterized at least in terms of expression of the following surface antigens: CD45, CD34, CD133. While these markers do not strictly relate to the regenerative actions of BM-MNC, they represent surrogate markers linked to a function already validated by published data.
The cell product should be free from adventitious microbial agents (viruses, mycoplasma, bacteria, and fungi) that could originate from the starting or raw materials or adventitiously introduced during the manufacturing process even if cells are minimally manipulated. In any case, a thorough testing for aerobes and anaerobes bacteria and fungi must be performed at the level of finished product by using the methods described in the pharmacopea.
Cell potency is the quantitative measure of biological activity based on the attribute of the product and on his relevant biological properties. As far as concern the potency testing within the clinical use of BM-MNC in cardiac repair, the importance of characterizing the function of injected cells has been clearly pointed out [31, 63]. To evaluate the potency of BM-MNC obtained after density gradient centrifugation, authors proposed both in vitro and in vivo assays.
In the first case, BM-MNC cells were evaluated by haematopoietic colonyforming unit (CFU), and assessment of CFU-Fibroblast clonogenic potential. Furthermore, based on observation that the migratory capacity of BM-MNC predicts the functional improvement after cell transplantation in tissue ischemia [64, 65] authors assessed the BM-MNC invasion capacity in vitro.
The mouse hind limb ischemia model is currently purposed as an in vivo assay for the evaluation of the neovascularization capacity of BM-MNC.
The tumorigenicity of the cell product differs from the classical pharmaceutics as the transformation can also happen in the cellular component of the product and not only in the treated individual. The transformation risk associated with the cells should be evaluated based on a risk analysis. In the case of cardiac regeneration or hind limb ischemia treatment, cells are typically of autologous origin and the level of cell manipulation is minimal. Furthermore, a number of clinical trials are now available evaluating the safety of the use of selected or unselected BM-MNC for some applications. Considering as above-mentioned, the risk of tumorigenicity associated with the infusion autologous bone marrow cells could be considered low.
Summary
Stem cells from bone marrow, administered after minimal manipulation represent an important cell source for cellbased therapies. The ease of collection, combined with a minimal manipulation that can be an immunological or a density gradient separation, in the past has meant that many clinical trials have been carried out starting from this source of stem cells. The trial results, have revealed both safety and efficacy of the use of stem cells starting from BM-MNC in many cardiovascular diseases. Many of these clinical trials were performed in a period before the entry into force of the regulation on advanced therapies: this meant that in some cases, the quality of infused cells (e.g. cell viability) had not always been considered. As a result, conflicting data have been generated on the effectiveness of cellbased therapies in certain diseases as acute myocardial infarction.
We now have a clear regulatory framework that will allow for better development of the drug, which should be based on clear scientific evidences, on the development of appropriate preclinical models and rely on a production based on GMP standards to ensure maximum safety for people involved in clinical trials. Hospitals, clinics and industry must be able to meet the challenge for the future.
References
- 1.Gatti RA, Meuwissen HJ, Allen HD, Hong R, Good RA. Immunological reconstitution of sexlinked lymphopenic immunological deficiency. Lancet. 1968;2:1366–1369. doi: 10.1016/s0140-6736(68)92673-1. [DOI] [PubMed] [Google Scholar]
- 2.Kuci S, Kuci Z, Latifi-Pupovci H, Niethammer D, Handgretinger R, Schumm M, Bruchelt G, Bader P, Klingebiel T. Adult stem cells as an alternative source of multipotential (pluripotential) cells in regenerative medicine. Curr Stem Cell Res Ther. 2009;4:107–117. doi: 10.2174/157488809788167427. [DOI] [PubMed] [Google Scholar]
- 3.Boyum A. Isolation of mononuclear cells and granulocytes from human blood. Isolation of monuclear cells by one centrifugation, and of granulocytes by combining centrifugation and sedimentation at 1 g. Scand J Clin Lab Invest Suppl. 1968;97:77–89. [PubMed] [Google Scholar]
- 4.Wilmut I, Schnieke AE, McWhir J, Kind AJ, Campbell KH. Viable offspring derived from fetal and adult mammalian cells. Nature. 1997;385:810–813. doi: 10.1038/385810a0. [DOI] [PubMed] [Google Scholar]
- 5.Noort WA, Kruisselbrink AB, in't Anker PS, Kruger M, van Bezooijen RL, de Paus RA, Heemskerk MH, Lowik CW, Falkenburg JH, Willemze R, Fibbe WE. Mesenchymal stem cells promote engraftment of human umbilical cord blood-derived CD34(+) cells in NOD/SCID mice. Exp Hematol. 2002;30:870–878. doi: 10.1016/s0301-472x(02)00820-2. [DOI] [PubMed] [Google Scholar]
- 6.Sutherland DR, Keating A. The CD34 antigen: structure, biology, and potential clinical applications. J Hematother. 1992;1:115–129. doi: 10.1089/scd.1.1992.1.115. [DOI] [PubMed] [Google Scholar]
- 7.Miraglia S, Godfrey W, Yin AH, Atkins K, Warnke R, Holden JT, Bray RA, Waller EK, Buck DW. A novel five-transmembrane hematopoietic stem cell antigen: isolation, characterization, and molecular cloning. Blood. 1997;90:5013–5021. [PubMed] [Google Scholar]
- 8.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 9.Colter DC, Class R, DiGirolamo CM, Prockop DJ. Rapid expansion of recycling stem cells in cultures of plastic-adherent cells from human bone marrow. Proc Natl Acad Sci U S A. 2000;97:3213–3218. doi: 10.1073/pnas.070034097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JH, Kosinski PA, Kemp DM. Contribution of human bone marrow stem cells to individual skeletal myotubes followed by myogenic gene activation. Exp Cell Res. 2005;307:174–182. doi: 10.1016/j.yexcr.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Urbich C, Dimmeler S. Endothelial progenitor cells: characterization and role in vascular biology. Circ Res. 2004;95:343–353. doi: 10.1161/01.RES.0000137877.89448.78. [DOI] [PubMed] [Google Scholar]
- 12.Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endo-thelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 13.Valgimigli M, Rigolin GM, Fucili A, Porta MD, Soukhomovskaia O, Malagutti P, Bugli AM, Bragotti LZ, Francolini G, Mauro E, et al. CD34+ and endothelial progenitor cells in patients with various degrees of congestive heart failure. Circulation. 2004;110:1209–1212. doi: 10.1161/01.CIR.0000136813.89036.21. [DOI] [PubMed] [Google Scholar]
- 14.Kinnaird T, Stabile E, Burnett MS, Epstein SE. Bone-marrow-derived cells for enhancing collateral development: mechanisms, animal data, and initial clinical experiences. Circ Res. 2004;95:354–363. doi: 10.1161/01.RES.0000137878.26174.66. [DOI] [PubMed] [Google Scholar]
- 15.Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600. doi: 10.1056/NEJMoa022287. [DOI] [PubMed] [Google Scholar]
- 16.Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, Kearne M, Magner M, Isner JM. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res. 1999;85:221–228. doi: 10.1161/01.res.85.3.221. [DOI] [PubMed] [Google Scholar]
- 17.Quirici N, Soligo D, Caneva L, Servida F, Bossolasco P, Deliliers GL. Differentiation and expansion of endothelial cells from human bone marrow CD133(+) cells. Br J Haematol. 2001;115:186–194. doi: 10.1046/j.1365-2141.2001.03077.x. [DOI] [PubMed] [Google Scholar]
- 18.Hirschi KK, Ingram DA, Yoder MC. Assessing identity, phenotype, and fate of endothelial progenitor cells. Arterioscler Thromb Vasc Biol. 2008;28:1584–1595. doi: 10.1161/ATVBAHA.107.155960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mund JA, Ingram DA, Yoder MC, Case J. Endothelial progenitor cells and cardiovascular cell-based therapies. Cytotherapy. 2009;11:103–113. doi: 10.1080/14653240802714827. [DOI] [PubMed] [Google Scholar]
- 20.Gnecchi M, Zhang Z, Ni A, Dzau VJ. Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res. 2008;103:1204–1219. doi: 10.1161/CIRCRESAHA.108.176826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gnecchi M, He H, Liang OD, Melo LG, Morello F, Mu H, Noiseux N, Zhang L, Pratt RE, Ingwall JS, Dzau VJ. Paracrine action accounts for marked protection of ischemic heart by Aktmodified mesenchymal stem cells. Nat Med. 2005;11:367–368. doi: 10.1038/nm0405-367. [DOI] [PubMed] [Google Scholar]
- 22.Gnecchi M, He H, Noiseux N, Liang OD, Zhang L, Morello F, Mu H, Melo LG, Pratt RE, Ingwall JS, Dzau VJ. Evidence supporting paracrine hypothesis for Aktmodified mesenchymal stem cellmediated cardiac protection and functional improvement. Faseb J. 2006;20:661–669. doi: 10.1096/fj.05-5211com. [DOI] [PubMed] [Google Scholar]
- 23.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. Jama. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 24.Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM, et al. Bone marrow cells regenerate infarcted myocardium. Nature. 2001;410:701–705. doi: 10.1038/35070587. [DOI] [PubMed] [Google Scholar]
- 25.Jackson KA, Majka SM, Wang H, Pocius J, Hartley CJ, Majesky MW, Entman ML, Michael LH, Hirschi KK, Goodell MA. Regeneration of ischemic cardiac muscle and vascular endothelium by adult stem cells. J Clin Invest. 2001;107:1395–1402. doi: 10.1172/JCI12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dawn B, Bolli R. Adult bone marrow-derived cells: regenerative potential, plasticity, and tissue commitment. Basic Res Cardiol. 2005;100:494–503. doi: 10.1007/s00395-005-0552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rota M, Kajstura J, Hosoda T, Bearzi C, Vitale S, Esposito G, Iaffaldano G, Padin-Iruegas ME, Gonzalez A, Rizzi R, et al. Bone marrow cells adopt the cardiomyogenic fate in vivo. Proc Natl Acad Sci U S A. 2007;104:17783–17788. doi: 10.1073/pnas.0706406104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stamm C, Kleine HD, Choi YH, Dunkelmann S, Lauffs JA, Lorenzen B, David A, Liebold A, Nienaber C, Zurakowski D, et al. Intramyocardial delivery of CD133+ bone marrow cells and coronary artery bypass grafting for chronic ischemic heart disease: safety and efficacy studies. J Thorac Cardiovasc Surg. 2007;133:717–725. doi: 10.1016/j.jtcvs.2006.08.077. [DOI] [PubMed] [Google Scholar]
- 29.Cannon RO, 3rd, Dunbar CE. BM-derived cell therapies for cardiovascular disease. Cytotherapy. 2007;9:305–315. doi: 10.1080/14653240701431176. [DOI] [PubMed] [Google Scholar]
- 30.Yoon YS, Lee N, Scadova H. Myocardial regeneration with bone-marrow-derived stem cells. Biol Cell. 2005;97:253–263. doi: 10.1042/BC20040099. [DOI] [PubMed] [Google Scholar]
- 31.Abdel-Latif A, Bolli R, Tleyjeh IM, Montori VM, Perin EC, Hornung CA, Zuba-Surma EK, Al-Mallah M, Dawn B. Adult bone marrow-derived cells for cardiac repair: a systematic review and meta-analysis. Arch Intern Med. 2007;167:989–997. doi: 10.1001/archinte.167.10.989. [DOI] [PubMed] [Google Scholar]
- 32.Sürder D SJ, Moccetti T, Astori G, Rufibach K, Plein S, Lo Cicero V, Soncin S, Windecker S, Moschovitis A, Erne P, Jamshidi P, Auf der Maur C, Manka R, Soldati G, Landmesser U, Lüscher TF, Corti R. Cell-based therapy for myocardial repair in patients with acute myocardial infarction: Rationale and study design of the SWiss multicenter Intracoronary Stem cells Study in Acute Myocardial Infarction (SWISS-AMI) AHJ. 2010 doi: 10.1016/j.ahj.2010.03.039. accepted for pubblication. [DOI] [PubMed] [Google Scholar]
- 33.Guidelines for percutaneous transluminal angioplasty. Standards of Practice Committee of the Society of Cardiovascular and Interventional Radiology. Radiology. 1990;177:619–626. doi: 10.1148/radiology.177.3.2147067. [DOI] [PubMed] [Google Scholar]
- 34.Valentine RJ, Myers SI, Inman MH, Roberts JR, Clagett GP. Late outcome of amputees with premature atherosclerosis. Surgery. 1996;119:487–493. doi: 10.1016/s0039-6060(96)80255-8. [DOI] [PubMed] [Google Scholar]
- 35.Schainfeld RM, Isner JM. Critical limb ischemia: nothing to give at the office? Ann Intern Med. 1999;130:442–444. doi: 10.7326/0003-4819-130-5-199903020-00017. [DOI] [PubMed] [Google Scholar]
- 36.Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344:1608–1621. doi: 10.1056/NEJM200105243442108. [DOI] [PubMed] [Google Scholar]
- 37.Kocher AA, Schuster MD, Szabolcs MJ, Takuma S, Burkhoff D, Wang J, Homma S, Edwards NM, Itescu S. Neovascularization of ischemic myocardium by human bone-marrow-derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Nat Med. 2001;7:430–436. doi: 10.1038/86498. [DOI] [PubMed] [Google Scholar]
- 38.Kalka C, Masuda H, Takahashi T, Kalka-Moll WM, Silver M, Kearney M, Li T, Isner JM, Asahara T. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc Natl Acad Sci U S A. 2000;97:3422–3427. doi: 10.1073/pnas.070046397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kawamoto A, Gwon HC, Iwaguro H, Yamaguchi JI, Uchida S, Masuda H, Silver M, Ma H, Kearney M, Isner JM, Asahara T. Therapeutic potential of ex vivo expanded endothelial progenitor cells for myocardial ischemia. Circulation. 2001;103:634–637. doi: 10.1161/01.cir.103.5.634. [DOI] [PubMed] [Google Scholar]
- 40.Shintani S, Murohara T, Ikeda H, Ueno T, Sasaki K, Duan J, Imaizumi T. Augmentation of postnatal neovascularization with autologous bone marrow transplantation. Circulation. 2001;103:897–903. doi: 10.1161/01.cir.103.6.897. [DOI] [PubMed] [Google Scholar]
- 41.Kamihata H, Matsubara H, Nishiue T, Fujiyama S, Tsutsumi Y, Ozono R, Masaki H, Mori Y, Iba O, Tateishi E, et al. Implantation of bone marrow mononuclear cells into ischemic myocardium enhances collateral perfusion and regional function via side supply of angioblasts, angiogenic ligands, and cytokines. Circulation. 2001;104:1046–1052. doi: 10.1161/hc3501.093817. [DOI] [PubMed] [Google Scholar]
- 42.Dimmeler S, Zeiher AM, Schneider MD. Unchain my heart: the scientific foundations of cardiac repair. J Clin Invest. 2005;115:572–583. doi: 10.1172/JCI24283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lenk K, Adams V, Lurz P, Erbs S, Linke A, Gielen S, Schmidt A, Scheinert D, Biamino G, Emmrich F, et al. Therapeutical potential of blood-derived progenitor cells in patients with peripheral arterial occlusive disease and critical limb ischaemia. Eur Heart J. 2005;26:1903–1909. doi: 10.1093/eurheartj/ehi285. [DOI] [PubMed] [Google Scholar]
- 44.Kawamura A, Horie T, Tsuda I, Ikeda A, Egawa H, Imamura E, Iida J, Sakata H, Tamaki T, Kukita K, et al. Prevention of limb amputation in patients with limbs ulcers by autologous peripheral blood mononuclear cell implantation. Ther Apher Dial. 2005;9:59–63. doi: 10.1111/j.1774-9987.2005.00218.x. [DOI] [PubMed] [Google Scholar]
- 45.Huang PP, Li SZ, Han MZ, Xiao ZJ, Yang RC, Qiu LG, Han ZC. Autologous transplantation of peripheral blood stem cells as an effective therapeutic approach for severe arteriosclerosis obliterans of lower extremities. Thromb Haemost. 2004;91:606–609. doi: 10.1160/TH03-06-0343. [DOI] [PubMed] [Google Scholar]
- 46.Huang P, Li S, Han M, Xiao Z, Yang R, Han ZC. Autologous transplantation of granulocyte colony stimulating factor-mobilized peripheral blood mononuclear cells improves critical limb ischemia in diabetes. Diabetes Care. 2005;28:2155–2160. doi: 10.2337/diacare.28.9.2155. [DOI] [PubMed] [Google Scholar]
- 47.Van Tongeren RB, Hamming JF, Fibbe WE, Van Weel V, Frerichs SJ, Stiggelbout AM, Van Bockel JH, Lindeman JH. Intramuscular or combined intramuscular/intra-arterial administration of bone marrow mononuclear cells: a clinical trial in patients with advanced limb ischemia. J Cardiovasc Surg (Torino) 2008;49:51–58. [PubMed] [Google Scholar]
- 48.Cobellis G, Silvestroni A, Lillo S, Sica G, Botti C, Maione C, Schiavone V, Rocco S, Brando G, Sica V. Long-term effects of repeated autologous transplantation of bone marrow cells in patients affected by peripheral arterial disease. Bone Marrow Transplant. 2008;42:667–672. doi: 10.1038/bmt.2008.228. [DOI] [PubMed] [Google Scholar]
- 49.Bittner RE, Schofer C, Weipoltshammer K, Ivanova S, Streubel B, Hauser E, Freilinger M, Hoger H, Elbe-Burger A, Wachtler F. Recruitment of bone-marrow-derived cells by skeletal and cardiac muscle in adult dystrophic mdx mice. Anat Embryol (Berl) 1999;199:391–396. doi: 10.1007/s004290050237. [DOI] [PubMed] [Google Scholar]
- 50.Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, Boggs SS, Greenberger JS, Goff JP. Bone marrow as a potential source of hepatic oval cells. Science. 1999;284:1168–1170. doi: 10.1126/science.284.5417.1168. [DOI] [PubMed] [Google Scholar]
- 51.Theise ND, Nimmakayalu M, Gardner R, Illei PB, Morgan G, Teperman L, Henegariu O, Krause DS. Liver from bone marrow in humans. Hepatology. 2000;32:11–16. doi: 10.1053/jhep.2000.9124. [DOI] [PubMed] [Google Scholar]
- 52.Ianus A, Holz GG, Theise ND, Hussain MA. In vivo derivation of glucose-competent pancreatic endocrine cells from bone marrow without evidence of cell fusion. J Clin Invest. 2003;111:843–850. doi: 10.1172/JCI16502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hess D, Li L, Martin M, Sakano S, Hill D, Strutt B, Thyssen S, Gray DA, Bhatia M. Bone marrow-derived stem cells initiate pancreatic regeneration. Nat Biotechnol. 2003;21:763–770. doi: 10.1038/nbt841. [DOI] [PubMed] [Google Scholar]
- 54.Grove JE, Bruscia E, Krause DS. Plasticity of bone marrow-derived stem cells. Stem Cells. 2004;22:487–500. doi: 10.1634/stemcells.22-4-487. [DOI] [PubMed] [Google Scholar]
- 55.Dietz AB, Padley DJ, Gastineau DA. Infrastructure development for human cell therapy translation. Clin Pharmacol Ther. 2007;82:320–324. doi: 10.1038/sj.clpt.6100288. [DOI] [PubMed] [Google Scholar]
- 56.EudraLex, editor. The Rules Governing Medicinal Products in the European Union Volume 4. EU Guidelines toGood Manufacturing Practice. Medicinal Products for Human and Veterinary Use. Annex 1. Manufacture of Sterile Medicinal Products (corrected version). 2008.
- 57. International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use. ICH harmonised tripartite guideline validation of analytical procedures: text and methodology Q2(R1). 1994.
- 58. Directive 2004/23/EC of the European Parliament and of the Council on setting standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells. 2004.
- 59.Food and Drug Administration, editor. Eligibility determination for donors of human cells, tissues, and cellular and tissue-based products (HCT/Ps). 2007. [PubMed]
- 60.Griesel C, Heuft HG, Herrmann D, Franke A, Ladas D, Stiehler N, Stucki A, Braun M, Wollert KC, Meyer GP, et al. Good manufacturing practice-compliant validation and preparation of BM cells for the therapy of acute myocardial infarction. Cytotherapy. 2007;9:35–43. doi: 10.1080/14653240601052734. [DOI] [PubMed] [Google Scholar]
- 61. Research FaDACfBEa: Guidance for FDA Reviewers and Sponsors: content and review of chemistry, manufacturing, and control (CMC) information for human somatic cell therapy investigational new drug applications (IND). (Services UdoHaH ed.; 2008.
- 62.Soncin S, Lo Cicero V, Astori G, Soldati G, Gola M, Surder D, Moccetti T. A practical approach for the validation of sterility, endotoxin and potency testing of bone marrow mononucleated cells used in cardiac regeneration in compliance with good manufacturing practice. J Transl Med. 2009;7:78. doi: 10.1186/1479-5876-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Seeger FH, Tonn T, Krzossok N, Zeiher AM, Dimmeler S. Cell isolation procedures matter: a comparison of different isolation protocols of bone marrow mononuclear cells used for cell therapy in patients with acute myocardial infarction. Eur Heart J. 2007;28:766–772. doi: 10.1093/eurheartj/ehl509. [DOI] [PubMed] [Google Scholar]
- 64.Heeschen C, Lehmann R, Honold J, Assmus B, Aicher A, Walter DH, Martin H, Zeiher AM, Dimmeler S. Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Circulation. 2004;109:1615–1622. doi: 10.1161/01.CIR.0000124476.32871.E3. [DOI] [PubMed] [Google Scholar]
- 65.Britten MB, Abolmaali ND, Assmus B, Lehmann R, Honold J, Schmitt J, Vogl TJ, Martin H, Schachinger V, Dimmeler S, Zeiher AM. Infarct remodeling after intracoronary progenitor cell treatment in patients with acute myocardial infarction (TOPCARE-AMI): mechanistic insights from serial contrast-enhanced magnetic resonance imaging. Circulation. 2003;108:2212–2218. doi: 10.1161/01.CIR.0000095788.78169.AF. [DOI] [PubMed] [Google Scholar]
- 66.Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, Lippolt P, Breidenbach C, Fichtner S, Korte T, Hornig B, Messinger D, et al. Intracoronary autologous bone-marrow cell transfer after myocardial infarction: the BOOST randomised controlled clinical trial. Lancet. 2004;364:141–148. doi: 10.1016/S0140-6736(04)16626-9. [DOI] [PubMed] [Google Scholar]
- 67.Meyer GP, Wollert KC, Lotz J, Steffens J, Lippolt P, Fichtner S, Hecker H, Schaefer A, Arseniev L, Hertenstein B, et al. Intracoronary bone marrow cell transfer after myocardial infarction: eighteen months’follow-up data from the randomized, controlled BOOST (BOne marrOw transfer to enhance ST-elevation infarct regeneration) trial. Circulation. 2006;113:1287–1294. doi: 10.1161/CIRCULATIONAHA.105.575118. [DOI] [PubMed] [Google Scholar]
- 68.Schachinger V, Erbs S, Elsasser A, Haberbosch W, Hambrecht R, Holschermann H, Yu J, Corti R, Mathey DG, Hamm CW, et al. Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med. 2006;355:1210–1221. doi: 10.1056/NEJMoa060186. [DOI] [PubMed] [Google Scholar]
- 69.Huikuri HV, Kervinen K, Niemela M, Ylitalo K, Saily M, Koistinen P, Savolainen ER, Ukkonen H, Pietila M, Airaksinen JK, et al. Effects of intracoronary injection of mononuclear bone marrow cells on left ventricular function, arrhythmia risk profile, and restenosis after thrombolytic therapy of acute myocardial infarction. Eur Heart J. 2008;29:2723–2732. doi: 10.1093/eurheartj/ehn436. [DOI] [PubMed] [Google Scholar]
- 70.Nijveldt Intracoronary Infusion of Mononuclear Cells After PrimaryPercutaneous Coronary Intervention: The HEBE Trial. Circulation. 2008:2309–2317. 118 (2008 Late-Breaking Clinical Trial Abstracts): [Google Scholar]
- 71.Tendera M, Wojakowski W, Ruzyllo W, Chojnowska L, Kepka C, Tracz W, Musialek P, Piwowarska W, Nessler J, Buszman P, et al. Intracoronary infusion of bone marrow-derived selected CD34+CXCR4+ cells and non-selected mononuclear cells in patients with acute STEMI and reduced left ventricular ejection fraction: results of randomized, multicentre Myocardial Regeneration by Intracoronary Infusion of Selected Population of Stem Cells in Acute Myocardial Infarction (REGENT) Trial. Eur Heart J. 2009;30:1313–1321. doi: 10.1093/eurheartj/ehp073. [DOI] [PubMed] [Google Scholar]
- 72.Lunde K, Solheim S, Aakhus S, Arnesen H, Moum T, Abdelnoor M, Egeland T, Endresen K, Ilebekk A, Mangschau A, Forfang K. Exercise capacity and quality of life after intracoronary injection of autologous mononuclear bone marrow cells in acute myocardial infarction: results from the Autologous Stem cell Transplantation in Acute Myocardial Infarction (ASTAMI) randomized controlled trial. Am Heart J. 2007;154(710):e711–718. doi: 10.1016/j.ahj.2007.07.003. [DOI] [PubMed] [Google Scholar]


