Abstract
Humans differ in their initial response to, and subsequent abuse of, addictive drugs like cocaine. Rodents also exhibit marked individual differences in responsiveness to cocaine. Previously, we classified male Sprague-Dawley rats as either low or high cocaine responders (LCRs or HCRs, respectively), based on their acute low-dose cocaine-induced locomotor activity, and found that with repeated drug exposure LCRs exhibit greater cocaine locomotor sensitization, reward and reinforcement than HCRs. Differential cocaine-induced increases in striatal dopamine help to explain the LCR/HCR phenotypes. Differential levels of stress and/or anxiety could also contribute but have not been explored. Here we measured open-field activity and plasma corticosterone levels both pre- and post-cocaine treatment in LCRs, HCRs, and saline-treated controls. The three groups did not differ in baseline locomotor activity or corticosterone levels. Importantly, LCR/HCR differences in corticosterone levels were also not observed following acute cocaine (10 mg/kg, i.p.), when cocaine induced approximately 3.5-fold greater locomotor activity in HCRs than LCRs. Additionally, there were no LCR/HCR differences in plasma corticosterone levels following five days of once-daily cocaine, during which time LCRs developed locomotor sensitization such that their cocaine-induced locomotor activity no longer differed from that of HCRs. Likewise, there were no group activity differences in any of four concentric zones within the open-field chamber. In summary, neither plasma corticosterone levels nor thigmotaxis-type anxiety appears to be a factor that contributes to the observed cocaine-induced LCR/HCR behavioral differences.
Keywords: cocaine, locomotor activity, corticosterone, locomotor sensitization, individual differences, HPA-axis
Humans display individual differences in cocaine responsiveness [7, 8, 10]. Only a subset of the population reports lifetime cocaine use, and ~15% of these users will transition to an addiction [33]. Among various contributing factors, stress and/or anxiety may predispose individuals to initiate drug use or renew drug-seeking/relapse behavior [31]. Understanding the bases for individual differences may allow clinicians to focus specific treatments on a subpopulation of drug users.
Dysregulation of both dopamine (DA) neurotransmission and the hypothalamic-pituitary-adrenal (HPA) axis contribute to cocaine abuse [15]. Cocaine increases DA levels by inhibiting DA transporter (DAT)-mediated DA uptake [28]. Cocaine can also increase plasma levels of corticosterone or cortisol, the stress-related hormone released from rat or human adrenal glands, respectively [4, 21]. Conversely, stress, and subsequently corticosterone, can increase DA neuronal firing and levels [27, 32]. In humans, increasing cortisol levels increases subjective feelings of stress, which predict a greater propensity for cocaine relapse [3]. Collectively, these studies motivate investigation of individual differences in drug-responsiveness as they relate to stress-hormone levels.
Animal models of individual differences in stress responsiveness have been developed [6, 12, 24]. An open-field can be used to assess exploratory behavior, novelty responsiveness, and anxiety [5]. The low and high responder model (LR and HR, respectively) classifies drug-naïve animals based on their locomotor response to a novel open-field environment [24]. LR/HR classification predicts cocaine self-administration acquisition [20], but does not as reliably predict psychostimulant-induced activity or conditioned place preference [16, 24]. Higher sustained corticosterone levels in drug-naïve HRs, compared to LRs, have been associated with greater susceptibility to self-administer psychostimulants [25, 26]. Despite higher corticosterone, HRs also exhibit greater activity in anxiogenic environments, compared to LRs [14]. Likewise, outbred rats with more elevated plus maze open-arm explorations exhibit higher cocaine self-administration break points [6]. However, rats with high, compared to low, stress-induced self-grooming levels have greater cocaine self-administration break points and corticosterone levels, but also greater elevated plus maze-measured anxiety [12]. Thus, the varied results using these animal models motivated our investigation of whether individual differences in stress and/or anxiety could help explain individual differences in initial cocaine responsiveness.
Our model for individual differences is focused on initial low-dose cocaine responsiveness. Previously, we have classified male Sprague-Dawley rats as low or high cocaine responders (LCRs or HCRs, respectively), based on the median split of their acute cocaine-induced locomotor activity [17, 22, 29]. LCR/HCR classification predicts cocaine-induced locomotor sensitization, cocaine-conditioned place preference, and motivation to self-administer cocaine [1, 17, 30], and is related to individual differences in striatal DAT number/function and extracellular DA levels [22, 29, 30]. To assess the potential contribution of stress and/or anxiety to the LCR/HCR phenotypes, here we collected intravenous blood samples for plasma corticosterone determinations before and after acute and repeated cocaine, while concurrently measuring central and peripheral zone locomotor activity in open-field chambers.
The male outbred Sprague-Dawley rats (n=24; Charles Rivers Laboratories, Wilmington, MA) weighed 240–260 g on arrival. Rats were housed on a 12-hr light-dark cycle (0700–1900) with ad libitum water and chow. The University of Colorado Denver IACUC approved these studies. This research program operates in accordance with the National Institutes of Health’s guidelines (NIH Publication No. 80-23, revised 1996).
(−)-Cocaine hydrochloride was a gift from the National Institute on Drug Abuse (RTI International, Research Triangle Park, NC). Ketamine, xylazine, heparinized saline, bupivacaine, and Penicillin-G® were obtained from the University of Colorado Hospital Pharmacy or Office of Laboratory Animal Resources (Aurora, CO).
Intravenous catheters were constructed and inserted into the right jugular vein under ketamine (100 mg/kg, i.m.) and xylazine (10 mg/kg, i.m.) anesthesia [17]. Published pre- and post-operative care and handling protocols were used [17]. Catheters were flushed with 200 µL of 0.9% sodium chloride containing 30 USP U/mL heparin.
Locomotor activity and LCR/HCR classification protocols were adapted from published methods [22, 29, 30]. All testing was conducted during the light phase of the circadian cycle (0900–1200), when endogenous corticosterone levels are stable. At least 6 days post-surgery, animals were habituated first to the behavioral testing room (60 min) and then to the open-field activity chamber (90 min; San Diego Instruments, San Diego, CA). After habituation, animals were removed from the chamber, injected with cocaine (10 mg/kg, i.p.) or saline (1 mL/kg, i.p.) and placed back into the chamber for 60 min. Locomotor activity was recorded as horizontal beam breaks, converted to distance traveled, and summed into bins (cm/10 min). The chamber (40×40×30 cm) was divided into four concentric zones: Zone 1 (‘Center’; middle 100 cm2), Zone 2 (‘Inner’; a 10-cm wide rectangle surrounding Zone 1), Zone 3 (‘Outer’; next 10-cm wide rectangle), and Zone 4 (‘Edge’; 10 cm-wide edge). Horizontal beam breaks within each zone were used to calculate ‘Zone Activity.’ Rats received five once-daily injections of cocaine or saline. On Days 1 and 5, locomotor activity was recorded and repeated blood sampling was performed. Animals received their injection in their home cage on Days 2 and 4 and in the activity chambers on Day 3 (data not shown).
Venous blood samples (200 µL) were collected into tubes containing 5 µL each of EDTA (100 mg/mL) and aprotinin (5,000 KIU/mL). Samples were centrifuged (4°C, 13,000 rpm, 8 min) and stored (−80°C). ‘Baseline’ samples were collected on Days 0 and 4 (1000 hr). On Days 1 and 5, samples were collected 30 min before (1000 hr) and 20, 40, and 60 min after injection. Following blood collection, 200 µL of saline was infused for volume replacement. Plasma corticosterone was measured using the ACTIVE® Rat Corticosterone enzyme immunoassay (Diagnostic Systems Laboratories, Webster, TX), per the manufacturer’s instructions. The intra- and inter-assay variations were 5 and 4%, respectively.
Each day’s activity and corticosterone data were analyzed with two-way repeated measures analysis of variance (RMANOVA; SPSS-16.0, Chicago, IL). Significant main effects were analyzed with one-way ANOVA or RMANOVA. When Mauchly’s test of sphericity failed, significance was tested using the Hunyh-Feldt corrected degrees of freedom, indicated by an asterisk (*). Paired or unpaired t-tests were used to compare locomotor activity or corticosterone levels between Days 0 and 4 or 1 and 5. Pearson r values (GraphPad Prism, La Jolla, CA) were used to compare relationships between cocaine-induced activity and corticosterone. Activity counts in each zone, and then each group, were analyzed on Day 1 or 5 using one-way ANOVAs. Data are expressed as mean ± standard error of the mean (SEM). Significance was set at p<0.05.
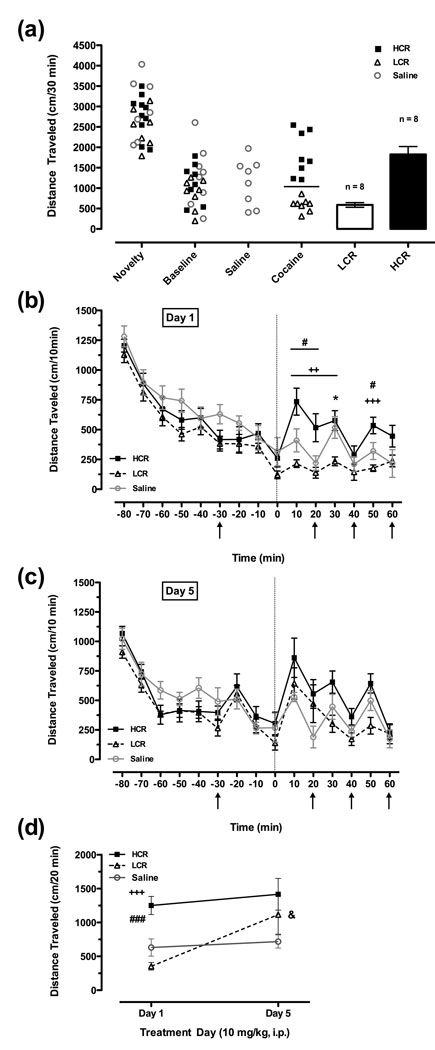
Following the initial cocaine injection, rats exhibited individual variability in cocaine-induced locomotor activity. Rats were readily classified as LCRs or HCRs using the median split of cocaine-induced locomotor activity 20 min post-injection (Fig.1a), prior to the first post-injection blood sample. None of the rats subsequently defined as LCRs or HCRs or the saline-treated controls differed in their locomotor response to the novel environment, after 20 (Fig.1a; HCR = 2089±113 cm/20 min, LCR = 1938±99, Saline = 2179±180) or 60 (HCR = 4361±391 cm/60 min, LCR = 3913±297, Saline = 4914±500) min of chamber exposure. Likewise, there were no group differences in baseline activity 20 min prior to injection (Fig.1a, ‘Baseline’). Conversely, 20 min post-cocaine, HCRs exhibited ~3.5-fold greater cocaine-induced locomotor activity compared to LCRs (Fig.1a; HCR = 1251±133 cm/20 min, LCR = 354±56). Fig.1b shows the locomotor activity time course. Two-way RMANOVA revealed main effects of time [*F(8.36,175.6) = 44.49, p<0.001] and group [*F(2,21) = 4.22, p=0.03], and a time by group interaction [*F(16.73,175.6) = 2.11, p=0.009]. One-way ANOVA revealed significant differences between LCRs and HCRs 30 and 50 min post-injection (p<0.01 and p<0.001, respectively; Fig.1b). HCRs also differed from saline-treated controls 20 min post-injection (p<0.05); LCRs differed significantly from controls only at 30 min post-injection (p<0.05).
Figure 1.
Differential cocaine-induced open-field locomotor activity and sensitization. (a) Summed novelty (first 20 min), baseline (20 min before injection), and post-injection (20 min) locomotor activity on Day 1 in saline-treated control rats (n=8) and cocaine-treated rats (n=16; 10 mg/kg, i.p.), subsequently classified as LCRs (n=8; white bar) or HCRs (n=8; black bar) based on the group median (horizontal line). (b,c) Time courses of locomotor activity on Days 1 (b) and 5 (c). Arrows represent time of blood samples (see Fig.2); dotted line indicates time of cocaine or saline injection. (d) Cocaine- and saline-induced locomotor activity (20 min) on Days 1 and 5 prior to the first post-cocaine blood sample. ++p<0.01, +++p<0.001, LCR vs. HCR; #p<0.05, ###p<0.001, HCR vs. Saline; *p<0.05, LCR vs. Saline; &p<0.05, LCR Day 1 vs. LCR Day 5. Mean ± SEM.
All rats received five once-daily injections of cocaine or saline. Similar to Day 1, there were no group differences in pre-injection activity (Fig.1c). On Day 5 (Fig.1c), two-way RMANOVA revealed a main effect of time [*F(9.99,209.7) = 20.0, p<0.001], but not a group or time by group interaction. Importantly, LCRs developed locomotor sensitization such that their activity on Day 5 was significantly higher than on Day 1 [Fig.1d; t(7) = 2.60, p<0.05] and no longer differed from HCRs. Post-injection locomotor activity did not differ between Days 1 and 5 for either HCRs or saline-treated controls (Fig.1d).
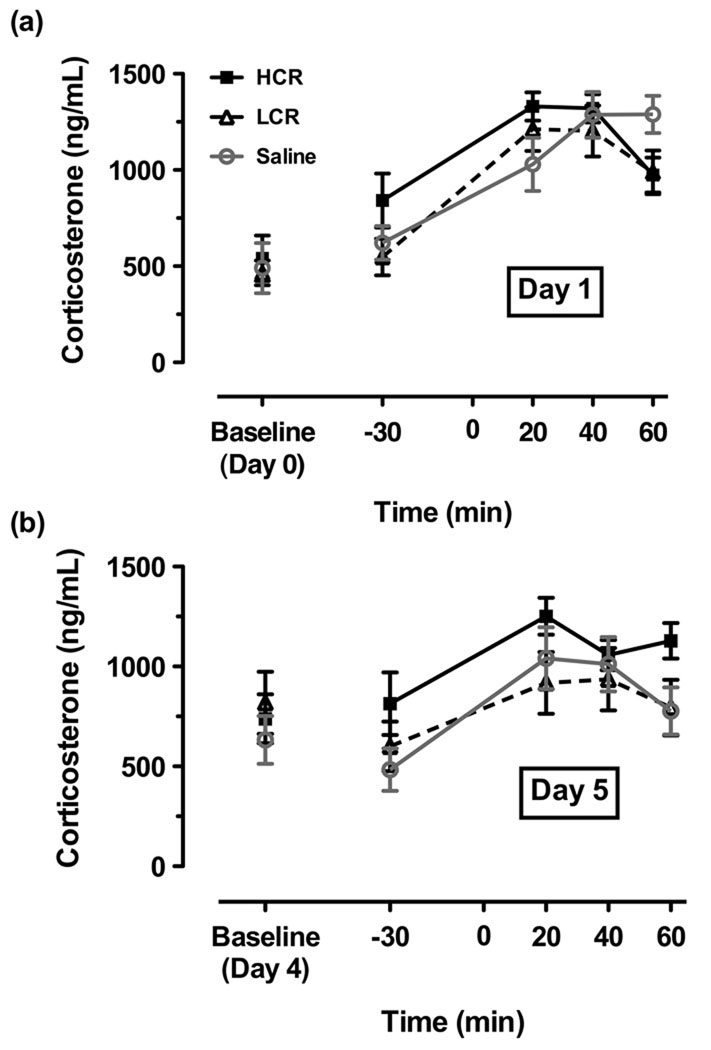
Chronically-implanted catheters allowed for rapid, repeated blood collection over multiple days. Baseline plasma corticosterone levels were measured on Days 0 and 4, one day prior to each locomotor activity/blood sampling experimental day (Days 1 and 5), and no differences were observed between LCRs, HCRs, or saline-treated controls on either day (Fig.2a or 2b, respectively). Means on Days 0 and 4 were ~500 and 730 ng/mL, respectively. On Day 1, 30 min prior to injection, group plasma corticosterone levels also did not differ significantly (Fig.2a). On Day 1, two-way RMANOVA revealed a main effect of time [F(3,60) = 24.08, p<0.001] but not group, and a time by group interaction [F(6,60) = 2.38, p=0.04]. One-way RMANOVA revealed main effects of time for LCRs, HCRs, and saline-treated controls (p≤0.001). However, notably, one-way ANOVAs at all time points revealed no between group differences (Fig.2a), suggesting the corticosterone responses reflect primarily effects of injection stress. Therefore, on Day 1, LCRs and HCRs had similar plasma corticosterone levels at time points when their locomotor activity profiles differed significantly.
Figure 2.
Similar plasma corticosterone levels in LCRs, HCRs, and saline-treated controls. Plasma corticosterone levels were measured (a) on Day 0 (baseline) and then on Day 1 before (−30 min) and after (20, 40, and 60 min) injection of cocaine or saline (see Fig.1b) and (b) similarly on Days 4 and 5 of the repeated cocaine or saline protocol (see Fig.1c). n=8 (HCR), n=8 (LCR), n=8 (Saline), except on Days 1 and 4 when blood samples could not be collected from one Saline animal due to a temporarily clogged catheter. Mean ± SEM.
On Day 5 of repeated cocaine or saline treatment, again no significant group differences were detected in corticosterone levels (Fig.2b). Two-way RMANOVA revealed a main effect of time [*F(2.37,49.8) = 10.5, p<0.001], but not a group or time by group interaction. To further assess post-injection corticosterone levels, group means for all post-injection corticosterone levels (20, 40, and 60 min) were calculated; however, no LCR/HCR differences were revealed on either Day 1 or 5 (data not shown). Further, irrespective of LCR/HCR classification, cocaine-induced locomotor activity and plasma corticosterone levels in individual rats were not correlated on either Day 1 (r = 0.22) or 5 (r = 0.17; data not shown).
Novel environments can induce anxiety in a variety of behavioral paradigms, including an open–field. We measured the activity counts of each rat in four concentric zones. There were no group differences in activity counts in any zone, before or after cocaine or saline injection, on either Day 1 or 5 (Table 1). However, all groups spent more time in the zone closest to the chamber walls (Zone 4) compared to the center (Zone 1), an indication of similar levels of thigmotaxis-type anxiety (Table 1; p<0.001). Despite the limitations of this ‘anxiety’ measure [5], this paradigm was selected because it could be employed concurrently with LCR/HCR classification, sensitization measures, and blood collection.
Table 1.
Activity counts in zones 1 (center), 2 (inner), 3 (outer) and 4 (edge) of the open-field chamber as a percent of total activity counts. Mean ± SEM.
| Treatment Day |
Zone | HCR (n=8) | LCR (n=8) | Saline (n=8) |
|---|---|---|---|---|
| % of Total | % of Total | % of Total | ||
| Day 1 | Zone 1 (Center) |
8 ± 1 | 6 ± 1 | 8 ± 1 |
| Zone 2 (Inner) |
25 ± 2 | 29 ± 2 | 25 ± 2 | |
| Zone 3 (Outer) |
30 ± 1 | 29 ± 2 | 32 ± 1 | |
| Zone 4 (Edge) |
37 ± 3 | 36 ± 3 | 35 ± 1 | |
| Day 5 | Zone 1 (Center) |
8 ± 1 | 8 ± 1 | 7 ± 1 |
| Zone 2 (Inner) |
25 ± 1 | 24 ± 1 | 24 ± 1 | |
| Zone 3 (Outer) |
31 ± 2 | 30 ± 2 | 32 ± 2 | |
| Zone 4 (Edge) |
36 ± 3 | 38 ± 1 | 37 ± 2 | |
Collectively, our results support the conclusion that neither plasma corticosterone nor thigmotaxis-type anxiety is a major contributor to LCR/HCR differences in cocaine responsiveness. First, all drug-naïve animals, including those subsequently classified as LCRs or HCRs, exhibited similar locomotor responses to a novel environment and basal plasma corticosterone levels. Second, following acute low-dose cocaine, when HCRs exhibited ~3.5-fold greater cocaine-induced activity than LCRs, plasma corticosterone levels did not differ. Third, this lack of group differences in hormone levels persisted after five days of repeated cocaine treatment, during which time LCRs developed locomotor sensitization, whereas HCRs and saline-treated controls did not. Paralleling their similar corticosterone levels, LCRs, HCRs, and saline-treated controls also had similar thigmotaxis-type anxiety responses.
It was important to address the possibility that individual differences in stress and/or anxiety could help explain LCR/HCR differences in cocaine responsiveness [17, 22] because results from other animal models support this idea. For example, individual differences in stress responsiveness, measured behaviorally or via corticosterone levels, have been linked to variability in drug responsiveness [6, 12, 24]. Furthermore, individual differences in plasma corticosterone levels of drug-naïve rats, which correlate with their novelty responsiveness (i.e. LR/HR phenotype) and plus maze open-arm explorations, predict psychostimulant self-administration [14, 25, 26]. Additionally, inbred Fischer 344 and Lewis rats, which differ in cocaine responsiveness, exhibit strain differences in behavioral and biochemical measures following corticosterone treatment [23]. In other models, rats with variable levels of anxiety-related behaviors, including stress-induced self-grooming and proclivity for elevated plus maze open-arm explorations, have inter-individual differences in self-administration behavior and corticosterone levels [6, 12].
The literature also suggests, however, that corticosterone levels need not contribute to LCR/HCR behavioral differences because: (1) locomotor activity and corticosterone levels are not always correlated, (2) corticosterone is not the sole mechanism by which stress can induce DA-related neuronal/behavioral changes, and (3) corticosterone-mediated changes in DA can be ‘state-dependent.’ First, despite the overall correlation between novelty-induced activity and corticosterone levels in LRs and HRs, no group differences in hormone levels were observed 30 minutes after novelty exposure when LR/HR activity differences were greatest [26]. Other studies report a lack of cocaine-induced corticosterone sensitization following repeated cocaine [18]. Likewise, our experiments demonstrated no corticosterone sensitization and no correlations between locomotor activity and corticosterone levels. Second, stress can modulate drug self-administration, DA neuronal firing, and extracellular DA levels via corticosteroid receptors on DA neurons [11, 27, 32]. However, corticosterone is not the sole mechanism by which stress can induce increases in extracellular DA, as this effect is not blocked by a glucocorticoid receptor antagonist and extracellular DA and plasma corticosterone levels are not necessarily correlated [13]. Recently, transgenic mice were used to demonstrate that unique populations of glucocorticoid receptors influence anxiety behaviors and cocaine self-administration, suggesting a dissociation of the mechanisms by which corticosterone mediates these behaviors [2]. Third, the phenomenon of corticosterone-mediated changes in DA levels, locomotor activity, and self-administration behavior appears to be ‘state-dependent.’ For example, the corticosterone-induced amplification of the behavioral effects of HRs, compared to LRs, is related to basal LR/HR dopaminergic and corticosterone differences [25]. Specifically, there is a basal corticosterone threshold that is met by HRs, but not LRs, that contributes to their individual differences in self-administration [9]. Additionally, cocaine-induced locomotor activity can depend on baseline corticosterone levels, not cocaine-induced corticosterone levels, and is reduced following adrenalectomy or glucocortocoid antagonist administration [19].
In the case of the LCR/HCR model, we demonstrated here that all of the rats tested had equivalent baseline and post-injection corticosterone levels. It warrants mentioning that blood sampling for the corticosterone measurements may have affected locomotor activity, but its influence did not appear to vary between groups, as their activity profiles were similar to those previously published [1, 22]. Clearly, there is a disconnect between equivalent corticosterone levels and significant variability in cocaine-induced locomotor activity, such that one does not predict the other. Therefore, while corticosterone can have a modulatory effect on the psychomotor and reinforcing effects of cocaine, the results from our LCR/HCR model of individual differences in cocaine responsiveness support the idea that this can be secondary to cocaine’s direct actions at DATs and subsequent differences in DAT-mediated DA clearance and extracellular DA [22, 29, 30].
Significant research has focused on individual differences in drug responsiveness and drug abuse susceptibility in humans [7, 8] and drug reward and reinforcement in rodents [17, 22, 29], as well as the contributions of stress and anxiety through HPA-axis dysregulation [3, 15, 19, 26]. While LCRs exhibit low initial responsiveness to cocaine compared to HCRs, LCRs develop cocaine-induced locomotor sensitization, conditioned place preference, and greater motivation to self-administer cocaine [1, 17, 29]. Here, we determined that LCRs and HCRs do not differ in either basal or post-cocaine levels of plasma corticosterone, suggesting that this stress hormone is not a major contributing factor to the observed LCR/HCR phenotypes. Our present results underscore a unique feature of the LCR/HCR model and, importantly, further differentiate this model from the other rat models previously discussed. Specifically, we observed no LCR/HCR differences in corticosterone levels or thigmotaxis-type anxiety. Without these additional individual differences in stress and/or anxiety, the LCR/HCR model appears to have more specific utility for elucidating the role of individual variability in (1) DAT function and DA levels, and (2) how initial drug-responsiveness relates to subsequent abuse liability, which vary between humans [7, 8, 10].
Acknowledgements
We thank Drs. Richard Allen and Bruce Mandt for their training in catheter surgeries. This research was supported by DA024948 (AMN), DA015050 and DA004216 (NRZ).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Allen RM, Everett CV, Nelson AM, Gulley JM, Zahniser NR. Low and high locomotor responsiveness to cocaine predicts intravenous cocaine conditioned place preference in male Sprague-Dawley rats. Pharmacol Biochem Behav. 2007;86:37–44. doi: 10.1016/j.pbb.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambroggi F, Turiault M, Milet A, Deroche-Gamonet V, Parnaudeau S, Balado E, Barik J, van der Veen R, Maroteaux G, Lemberger T, Schutz G, Lazar M, Marinelli M, Piazza PV, Tronche F. Stress and addiction: glucocorticoid receptor in dopaminoceptive neurons facilitates cocaine seeking. Nat Neurosci. 2009;12:247–249. doi: 10.1038/nn.2282. [DOI] [PubMed] [Google Scholar]
- 3.Back SE, Hartwell K, Desantis SM, Saladin M, McRae-Clark AL, Price KL, Moran-Santa Maria MM, Baker NL, Spratt E, Kreek MJ, Brady KT. Reactivity to laboratory stress provocation predicts relapse to cocaine. Drug Alcohol Depend. 2009 doi: 10.1016/j.drugalcdep.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baumann MH, Gendron TM, Becketts KM, Henningfield JE, Gorelick DA, Rothman RB. Effects of intravenous cocaine on plasma cortisol and prolactin in human cocaine abusers. Biol Psychiatry. 1995;38:751–755. doi: 10.1016/0006-3223(95)00083-6. [DOI] [PubMed] [Google Scholar]
- 5.Bourin M, Petit-Demouliere B, Dhonnchadha BN, Hascoet M. Animal models of anxiety in mice. Fundam Clin Pharmacol. 2007;21:567–574. doi: 10.1111/j.1472-8206.2007.00526.x. [DOI] [PubMed] [Google Scholar]
- 6.Bush DE, Vaccarino FJ. Individual differences in elevated plus-maze exploration predicted progressive-ratio cocaine self-administration break points in Wistar rats. Psychopharmacology (Berl) 2007;194:211–219. doi: 10.1007/s00213-007-0835-7. [DOI] [PubMed] [Google Scholar]
- 7.Cox SM, Benkelfat C, Dagher A, Delaney JS, Durand F, McKenzie SA, Kolivakis T, Casey KF, Leyton M. Striatal dopamine responses to intranasal cocaine self-administration in humans. Biol Psychiatry. 2009;65:846–850. doi: 10.1016/j.biopsych.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 8.de Wit H. Individual differences in acute effects of drugs in humans: Their relevance to risk for abuse. NIDA Res Monogr. 1998;169:176–187. [PubMed] [Google Scholar]
- 9.Goeders NE, Guerin GF. Role of corticosterone in intravenous cocaine self-administration in rats. Neuroendocrinology. 1996;64:337–348. doi: 10.1159/000127137. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein R, Woicik P, Moeller S, Telang F, Jayne M, Wong C, Wang G, Fowler J, Volkow N. Liking and wanting of drug and non-drug rewards in active cocaine users: the STRAP-R questionnaire. J Psychopharmacol. 2008 Nov 21; doi: 10.1177/0269881108096982. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harfstrand A, Fuxe K, Cintra A, Agnati LF, Zini I, Wikstrom AC, Okret S, Yu ZY, Goldstein M, Steinbusch H, et al. Glucocorticoid receptor immunoreactivity in monoaminergic neurons of rat brain. Proc Natl Acad Sci U S A. 1986;83:9779–9783. doi: 10.1073/pnas.83.24.9779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Homberg JR, van den Akker M, Raaso HS, Wardeh G, Binnekade R, Schoffelmeer AN, de Vries TJ. Enhanced motivation to self-administer cocaine is predicted by self-grooming behaviour and relates to dopamine release in the rat medial prefrontal cortex and amygdala. Eur J Neurosci. 2002;15:1542–1550. doi: 10.1046/j.1460-9568.2002.01976.x. [DOI] [PubMed] [Google Scholar]
- 13.Imperato A, Puglisi-Allegra S, Casolini P, Angelucci L. Changes in brain dopamine and acetylcholine release during and following stress are independent of the pituitary-adrenocortical axis. Brain Res. 1991;538:111–117. doi: 10.1016/0006-8993(91)90384-8. [DOI] [PubMed] [Google Scholar]
- 14.Kabbaj M, Devine DP, Savage VR, Akil H. Neurobiological correlates of individual differences in novelty-seeking behavior in the rat: differential expression of stress-related molecules. J Neurosci. 2000;20:6983–6988. doi: 10.1523/JNEUROSCI.20-18-06983.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164:1149–1159. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kosten TA, Miserendino MJ. Dissociation of novelty- and cocaine-conditioned locomotor activity from cocaine place conditioning. Pharmacol Biochem Behav. 1998;60:785–791. doi: 10.1016/s0091-3057(97)00388-2. [DOI] [PubMed] [Google Scholar]
- 17.Mandt BH, Schenk S, Zahniser NR, Allen RM. Individual differences in cocaine-induced locomotor activity in male Sprague-Dawley rats and their acquisition of and motivation to self-administer cocaine. Psychopharmacology (Berl) 2008;201:195–202. doi: 10.1007/s00213-008-1265-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mantsch JR, Goeders NE. Effects of cocaine self-administration on plasma corticosterone in rats: relationship to hippocampal type II glucocorticoid receptors. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24:633–646. doi: 10.1016/s0278-5846(00)00098-1. [DOI] [PubMed] [Google Scholar]
- 19.Marinelli M, Rouge-Pont F, Deroche V, Barrot M, De Jesus-Oliveira C, Le Moal M, Piazza PV. Glucocorticoids and behavioral effects of psychostimulants. I: locomotor response to cocaine depends on basal levels of glucocorticoids. J Pharmacol Exp Ther. 1997;281:1392–1400. [PubMed] [Google Scholar]
- 20.Marinelli M, White FJ. Enhanced vulnerability to cocaine self-administration is associated with elevated impulse activity of midbrain dopamine neurons. J Neurosci. 2000;20:8876–8885. doi: 10.1523/JNEUROSCI.20-23-08876.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moldow RL, Fischman AJ. Cocaine induced secretion of ACTH, beta-endorphin, and corticosterone. Peptides. 1987;8:819–822. doi: 10.1016/0196-9781(87)90065-9. [DOI] [PubMed] [Google Scholar]
- 22.Nelson AM, Larson GA, Zahniser NR. Low or high cocaine responding rats differ in striatal extracellular dopamine levels and dopamine transporter number. J Pharmacol Exp Ther. 2009 doi: 10.1124/jpet.109.159897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ortiz J, DeCaprio JL, Kosten TA, Nestler EJ. Strain-selective effects of corticosterone on locomotor sensitization to cocaine and on levels of tyrosine hydroxylase and glucocorticoid receptor in the ventral tegmental area. Neuroscience. 1995;67:383–397. doi: 10.1016/0306-4522(95)00018-e. [DOI] [PubMed] [Google Scholar]
- 24.Piazza PV, Deminiere JM, Le Moal M, Simon H. Factors that predict individual vulnerability to amphetamine self-administration. Science. 1989;245:1511–1513. doi: 10.1126/science.2781295. [DOI] [PubMed] [Google Scholar]
- 25.Piazza PV, Deroche V, Deminiere JM, Maccari S, Le Moal M, Simon H. Corticosterone in the range of stress-induced levels possesses reinforcing properties: implications for sensation-seeking behaviors. Proc Natl Acad Sci U S A. 1993;90:11738–11742. doi: 10.1073/pnas.90.24.11738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piazza PV, Maccari S, Deminiere JM, Le Moal M, Mormede P, Simon H. Corticosterone levels determine individual vulnerability to amphetamine self-administration. Proc Natl Acad Sci U S A. 1991;88:2088–2092. doi: 10.1073/pnas.88.6.2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piazza PV, Rouge-Pont F, Deroche V, Maccari S, Simon H, Le Moal M. Glucocorticoids have state-dependent stimulant effects on the mesencephalic dopaminergic transmission. Proc Natl Acad Sci U S A. 1996;93:8716–8720. doi: 10.1073/pnas.93.16.8716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ritz MC, Lamb RJ, Goldberg SR, Kuhar MJ. Cocaine receptors on dopamine transporters are related to self-administration of cocaine. Science. 1987;237:1219–1223. doi: 10.1126/science.2820058. [DOI] [PubMed] [Google Scholar]
- 29.Sabeti J, Gerhardt GA, Zahniser NR. Acute cocaine differentially alters accumbens and striatal dopamine clearance in low and high cocaine locomotor responders: behavioral and electrochemical recordings in freely moving rats. J Pharmacol Exp Ther. 2002;302:1201–1211. doi: 10.1124/jpet.102.035816. [DOI] [PubMed] [Google Scholar]
- 30.Sabeti J, Gerhardt GA, Zahniser NR. Individual differences in cocaine-induced locomotor sensitization in low and high cocaine locomotor-responding rats are associated with differential inhibition of dopamine clearance in nucleus accumbens. J Pharmacol Exp Ther. 2003;305:180–190. doi: 10.1124/jpet.102.047258. [DOI] [PubMed] [Google Scholar]
- 31.Stewart J. Pathways to relapse: the neurobiology of drug- and stress-induced relapse to drug-taking. J Psychiatry Neurosci. 2000;25:125–136. [PMC free article] [PubMed] [Google Scholar]
- 32.Thierry AM, Tassin JP, Blanc G, Glowinski J. Selective activation of mesocortical DA system by stress. Nature. 1976;263:242–244. doi: 10.1038/263242a0. [DOI] [PubMed] [Google Scholar]
- 33.Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26:479–488. doi: 10.1016/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]