Abstract
This study examined a developmental, cascade model that includes childhood risks of conduct problems and family adversity at age 10 – 12; conduct problems, risk taking, and internalizing during adolescence; and adult outcomes of conduct problems, poor health, health risks, depression, and service use at ages 27 and 30. Analyses showed that childhood conduct problems predicted adolescent conduct problems and risk taking, which, in turn, predicted adult conduct problems, health risks, depression, and service use. Childhood family adversity predicted adolescent internalizing, a predictor itself of poor health, depression, and service use at age 27. There was considerable continuity in the same adult outcomes measured over a 3-year period, as well as some cross-domain prediction from measures at age 27 to measures at age 30. Developmental patterns found in these data offer implications for future research and prevention.
Keywords: conduct problems, family adversity, health risks, poor health, depression, service use
Findings of longitudinal studies have been used to illustrate the ways in which developmental processes unfold in patterns of progressive or cascading effects, characterized by over-time changes in behaviors and experiences from one domain and point of assessment to another (Masten et al., 2005). In one study, Dodge and colleagues (2008) examined a cascade of child predictors related to serious violence in adolescence. They found that social disadvantage was a predictor of harsh and inconsistent parenting of children, itself a predictor of social and cognitive deficits, conduct problems, and social and academic failure in the elementary grades. In turn, early problems experienced by children and families appeared to increase parental withdrawal from supervision and lead to children's involvement with deviant peers, thereby elevating their risk of adolescent violence.
In another study of developmental cascades, Masten and colleagues (2005) examined over-time associations among constructs of externalizing problems, academic competence, and internalizing problems into early adulthood. The study showed developmental continuity in these constructs, as well as cross-domain prediction of childhood externalizing to lower academic competence during adolescence and internalizing in adulthood. Results also showed that adolescent internalizing predicted later externalizing into the adult years, all patterns that are consistent with a developmental cascades perspective.
The current study focuses primarily on childhood conduct problems and family adversity as predictors of later problems in the domains of health, mental health, and service use during adolescence and early adulthood (to age 30). Although prior research has documented associations between childhood risks and outcomes within one or more of these domains, few studies have examined how developmental patterns unfold over time in a manner consistent with a cascades model (Bair-Merritt, Blackstone, & Feudtner, 2006; Batten, Aslan, Maciejewski, & Mazure, 2004; Sachs-Ericsson, Blazer, Plant, & Arnow, 2005; Springer, Sheridan, Kuo, & Carnes, 2003; United States Department of Health and Human Services (USDHHS) 2008). The following review of research summarizes current findings on predictors and outcomes relevant to analyses of this study.
Pathways from Childhood Conduct Problems
Childhood conduct problems are known risk factors for difficulties later in life, including poor academic competence and school failure during adolescence, internalizing problems, depression, substance use, and poor health into early adulthood (Colman et al., 2009; Dodge, Greenberg, & Malone, 2008; Jaffee et al., 2002; Kosterman et al., in press; Mason et al., 2004; Masten et al., 2005; McCarty et al., 2009). Evidence also suggests that early conduct problems can lead to later, more serious forms of antisocial behavior that persists through adolescence (Loeber & Farrington, 2001; Loeber, Wei, Stouthamer-Loeber, Huizinga, & Thornberry, 1999). According to Loeber's model of developmental pathways of delinquency, covert forms of antisocial behavior in children, such as shoplifting, can lead to more moderate and serious forms of delinquency later on. Overt forms of antisocial behavior, such as physical fighting, also follow a pattern of escalation or stable persistence, for some, into the early adult years (Loeber & Stouthamer-Loeber, 1998).
Evidence of a link between conduct problems and internalizing problems is, in several studies, quite strong. In research on participants of the Dunedin Multidisciplinary Health and Development Study (Jaffee et al., 2002), childhood conduct problems were found to be highly comorbid with juvenile depression, and also linked to depression diagnosis in adulthood. Data from earlier analyses of the Seattle Social Development Project (SSDP) dataset also show a significant correlation between childhood conduct problems and later depression (Kosterman et al., in press; Mason et al., 2004; McCarty et al., 2009). For example, Kosterman et al.'s (in press) study showed that self-reported conduct problems in childhood and adolescence consistently predicted depression at age 21. Mason et al. (2004) also found a link between conduct problems and later depression in the SSDP data. Compared to those with lower levels of conduct problems, youth with higher levels of conduct problems at ages 10 and 11 were 4 times more likely to experience a depressive episode in early adulthood. McCarty et al. (2009) found that childhood conduct problems were somewhat more predictive of early adult depression for girls, and for both genders the correlation between conduct problems at age 10 and depression at age 21 was statistically significant.
Additionally, research has shown a link between conduct problems and general social functioning and health (Colman et al., 2009). For example, Colman and colleagues (2009) found that, compared to adolescents without externalizing problems, those with externalizing problems had more depression, alcohol abuse, relationship problems, and more unhappiness with family life in adulthood. In another study, Bardone et al. (1998) showed that conduct problems in adolescent girls predicted more medical problems and poorer self-reported health at age 21. Links to daily smoking; alcohol, marijuana, and tobacco dependence; and sexually transmitted diseases also were documented in that study.
Impact of Family Adversity on Health and Mental Health
High levels of family adversity, including violence and abuse of children, predicts many similar, and some additional, longitudinal outcomes for children (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). In fact, evidence suggests that chronic family adversity can increase general and more specific indicators of poor health and illness; increase mental health problems over the life course; promote risk taking; and, for some, lead to the misuse of alcohol and other substances during adolescence and adulthood (Felitti et al., 1998; Middlebrooks & Audage, 2008; USDHHS 2008).
In a longitudinal cohort study of 354 child participants followed into adulthood, Reinherz et al. (2003) found an association between family environment factors (e.g., family violence by age 15) and major depression diagnosis at ages 18 - 26. Other prospective and retrospective studies provide similar findings on depression, as well as anxiety symptoms and disorders among abused children (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). Yet, even less severe forms of conflict in the home (e.g., frequent arguing and yelling between parents, or between parents and their children) can increase mental health problems in adolescents and young adults (Herrenkohl, Kosterman, Hawkins, & Mason, 2009). For example, Herrenkohl et al. (2009) showed that high initial levels and growth in family conflict during adolescence predicted an increased risk of adult stressful life events, which, in turn, predicted more adult depressive symptoms after accounting for earlier risks of poverty and internalizing problems. In another study, Aseltine et al. (1998) found the co-occurrence of depression and substance use was linked to having had low family support and a negative relationship with parents. A baseline measure of family conflict (e.g., frequent arguments with parents) was, in that study, modestly but significantly correlated with adolescent depression.
Links from various indicators of family adversity to poor health and health impairments have also been studied, although less commonly using prospective, longitudinal data (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). Sachs-Ericsson et al. (2005) investigated the association between retrospectively measured childhood physical and sexual abuse and medical problems among adults ages 15 - 54 in the National Comorbidity Survey (NCS). Analyses found that both types of retrospectively measured abuse before age 15 were independently associated with a higher prevalence of past-year serious health problems, including AIDS, tuberculosis, cancer, high blood pressure, and diabetes (others also noted). Batten et al. (2004) also used data from the NCS to examine a more specific question about the link between child maltreatment (a composite of physical abuse, sexual abuse, and neglect) and cardiovascular health. They found that child maltreatment increased the risk of cardiovascular disease for women only, whereas the risk of lifetime depression increased for both genders. Although it was hypothesized that higher rates of depression might account for the greater risk of cardiovascular disease for individuals with histories of child maltreatment, the data did not show this to be the case; the effect of maltreatment on cardiovascular disease remained after accounting for depression.
Findings from the Adverse Childhood Experiences (ACE) retrospective study of health maintenance organization (HMO) participants also point to an association between family adversity for children reported retrospectively and poor health as adults (Dube et al., 2003; Felitti et al., 1998; Middlebrooks & Audage, 2008). In the ACE study, the more adverse childhood experiences adult participants recalled, the more likely they were to register lower ratings of health, more sexually transmitted diseases, and higher rates of obesity and inactivity. Participants with multiple adversities growing up were also more likely than those with fewer adversities to smoke, abuse drugs and alcohol, and have more sexual partners over their lifetimes, all of which increase morbidity and mortality (Felitti et al., 1998). Moreover, studies find there is a correlation between family adversity and higher medical and mental health service use (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008).
One explanation for the higher rates of both mental health and physical health problems among grown children from high adversity families is the impact of chronic stress on the body. Research has shown that high-level stress experienced over extended periods, and particularly during sensitive periods of development, can damage areas of the brain responsible for learning and memory (Shonkoff, Boyce, & McEwen, 2009). Extreme and prolonged stress can impair the body's immune response, thereby increasing an individual's vulnerability to illness and chronic health problems during and in years following an acute or prolonged stressor (Batten, Aslan, Maciejewski, & Mazure, 2004; Middlebrooks & Audage, 2008). In their recent review of literature, Shonkoff et al., (2009) refer to evidence supporting what they call “cumulative-exposure explanations” of the link between chronic stress and adult disease. Such explanations focus on how conditioned neurobiological responses that typically serve a protective function in dangerous situations (e.g., secretion of stress hormones that increase heart rate and blood flow to the brain to aid in decision-making and response) become “pathogenic” when frequently engaged, leading eventually to irreversible damage to the body, illness, and to a shortened life expectancy.
Other hypotheses focus on the emotional burden of growing up in a threatening and unsafe home environment without positive role models and with fewer primary attachments and less parental warmth (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008; Middlebrooks & Audage, 2008). Here, explanations focus on the foundational influences of secure attachments for children's health and prosocial development and the notion that children who experience family adversity are less likely than are those in stable, nurturing homes to experience and observe healthy relationship patterns, learn skills for problem-solving, and develop the capacity to regulate emotions. Consequently, these children are prone to internalizing problems and depression, as well as externalizing behaviors, such as aggression.
Objectives and Research Question
In that conduct problems and family adversity appear linked to many of the same or similar outcomes in adolescence and adulthood, it is important to examine each with respect to how developmental processes leading to later outcomes emerge. It is also important to account for other known risks or moderator variables, such as family poverty and child gender, so that effects can be understood in a broader developmental context. Of particular interest to us in this study is the degree to which conduct problems and family adversity set in motion one or more progressive patterns of risks and outcomes, or developmental cascades, in which adult health, health behaviors, and service use depend on these vulnerabilities much earlier in life.
Specific goals of this study are to understand the developmental cascade effects of childhood conduct problems and family adversity alongside covariates of family poverty and gender; and to assess proximal and distal outcomes of these risks in relation to chronic conduct problems, health, health behaviors, and service use in early adult life. Analyses include intervening variables of conduct problems, risk taking, and internalizing behaviors at age 14 (adolescence). We seek to answer the following research question: Are conduct problems and family adversity similarly linked to later adult outcomes of conduct problems, health and health risks, mental health, and service use through the same intervening factor(s) in adolescence?
Methods
Sample
The sample consists of all participants in the Seattle Social Development Project (SSDP) (N = 808) who completed one or more surveys across 11 waves of data collected from ages 10 to 30 (1985-2005). The sample, originally recruited from 18 elementary schools in urban Seattle in 1985, contained near equal numbers of males and females (50%) and is ethnically diverse: 47% Caucasian; 26% African American; 22% Asian American; and 5% Native American. Just over 50% of the sample was from childhood poverty, as measured by eligibility for the federal school free and reduced price lunch program. SSDP has maintained a 91% minimum retention of the original sample since the survey assessment of youth respondents at age 14. Detailed summaries of the SSDP sample, methods, and earlier findings can be found in other publications (Battin, Hill, Abbott, Catalano, & Hawkins, 1998; Hawkins, Catalano, Kosterman, Abbott, & Hill, 1999). Data collection procedures were approved by the Human Subjects Review Committee of the University of Washington.
Measures
Measures are a combination of mean scales, variety counts, and summative indexes. Alpha reliabilities are reported for mean scales only. Internal consistency was not expected in the case of counts and summative indexes. Relatively low alphas for some scales are due to the low frequency of certain items, and the small number of items overall used in several composite measures.
Childhood variables include male gender, a dichotomous measure for which males are coded 1 and females 0. Childhood poverty (ages 10 - 13) is a binary measure of family eligibility for the federal school lunch program when children were in fifth, sixth, or seventh grade. Conduct problems (ages 10 - 12) include self-reports of shoplifting, stealing, damaging property, and arrest. Scales at ages 10 and 12 were developed separately and then averaged (range of 0 - 1, mean = .11, sd = .17; α = .52 - .68). Family adversity combines prospective and retrospective reports of low bonding to family, family conflict, harsh discipline, and poor family management at ages 10 - 12. Adult (age 24) retrospective data on childhood abuse/neglect (physical abuse, emotional abuse, sexual abuse, emotional neglect) were combined with these prospective indictors.1 A child was considered having met criteria for family adversity if there was at least one affirmative response to both the prospective and retrospective measures. A total of 97 children (approximately 13% of the analysis sample) were determined to have met criteria for family adversity; of these, 53% are male.
Adolescent measures include conduct problems, risk taking, and internalizing problems at age 14. Past-year conduct problems are comparable to those used in the childhood wave of the study, with some modification in the wording of questions to accommodate the change in ages of participants: past-year arrest, past-year purposely damaged or destroyed property/things, past-year broken into a house, past-year taken something worth $5 or less, past-year taken something worth more than $5 but less than $50 (0 - 1, mean = .08, sd = .18; α = .72). Risk taking includes youth responses to the following questions: How many times have you done the following things: go to a wild, uninhibited party; shock [upset or annoyed adults] people just for the fun of it; do what feels good, regardless of the consequences; do something dangerous because someone dared you to do it; do risky [crazy] things even if they are a little frightening [dangerous]; do crazy things just to see the effect on others (0 - 4, mean = .54, sd = .73; α = .71). Internalizing problems (age 14) were measured with available items from the Achenbach Youth Self-Report Form (YSR) (Achenbach, 1991) for self-reported anxious and withdrawn behaviors (6 items, α = .71). Items include reports of an adolescent's tendency to ‘worry’; be ‘nervous or tense’; ‘too fearful/anxious’; ‘anxious to please’; ‘secretive’; and ‘afraid of mistakes’ (0 - 12, mean = 4.19, sd = 2.51; α = .71).
Adult (ages 24 and 27) measures include conduct problems, health risks, poor health, depression, and service use. Conduct problems in adulthood are a sum of five items similar to those listed for the adolescent wave of the study: past-year arrest, past-year damaged or destroyed property/things, past-year broken into a house, past-year taken something worth less than $50, and past-year taken something worth more than $50. The scale at age 27 has a range of 0 - 1, a mean of .04, and a standard deviation of .11 (α = .61). At age 30, the scale has a range of range of 0 - .6, a mean of .02, and a standard deviation of .08 (α = .40). Poor health at ages 27 and 30 combines perceived general health (1 = excellent to 4 = poor) and chronic physical or mental health problems (1 = yes), which were standardized and then averaged. Scores for the age 27 measure have a range of -.97 - 2.58; a mean of .00 and a standard deviation of .78. The two items that comprise this measure at age 27 are moderately correlated: r = .22. Scores for the age 30 measure have a range of -.96 - 2.48; a mean of .004, and a standard deviation of .77. The two items that comprise this measure at age 30 are moderately correlated: r = .20. Health risks at ages 27 and 30 are sums of multiple items coded to reflect health-averse behaviors. At age 27, the following 10 items were used to derive a composite score: exercise (frequency/week recoded: 1 = no exercise, 0 = 1 or more times exercise); past-year get drunk from alcohol (recoded: yes = 1); smoke tobacco daily (recoded: daily smoking = 1); discuss health concerns (never or rarely = 1); report persistent symptoms to doctor (never or rarely = 1); control stress (never or rarely = 1); keep daily stress low (never or rarely = 1); get adequate sleep (never or rarely = 1); wear a seatbelt (no = 1); and drive under the influence in the past 3 years (yes = 1) (0 - 9, mean 2.54, sd 1.85, α = .56). At age 30, 8 of 10 comparable items were available in the dataset (0 - 8, mean 1.35, sd 1.38, α = .50). Indicators of “discuss health concerns” and “report persistent symptoms to doctor” were not available. Depressive symptoms (age 27) were measured by summing the total number of past-year depressive symptoms from the Diagnostic Interview Schedule (DIS) (Robins, Cottler, Bucholtz, & Compton, 1995), including anhedonia; weight changes; sleep problems; psychomotor agitation or retardation; fatigue; feelings of worthlessness; concentration difficulties; and suicidal ideation (range 0 - 9, mean = 2.55, sd = 1.85, α = .97). A comparable measure of depressive symptoms was included at age 30 (range 0 - 9, mean = 1.26, sd = 2.79, α = .97). Finally, service use (age 27) refers to whether, in the past year, an individual reported having received counseling or used a self-help group (1 = yes); whether she/he received, in that year, outpatient counseling (1 = yes); received counseling from another source (1 = yes); saw a doctor frequently for an illness or symptoms (three or more visits in the past year); or saw a doctor for emotional or psychological problem (one or more visits in the past year). Items were summed (0 - 4, mean = .37, sd .73; α = .46). A similar measure was included in the analysis at age 30 (0 - 5, mean = .4, sd .81; α = .57).
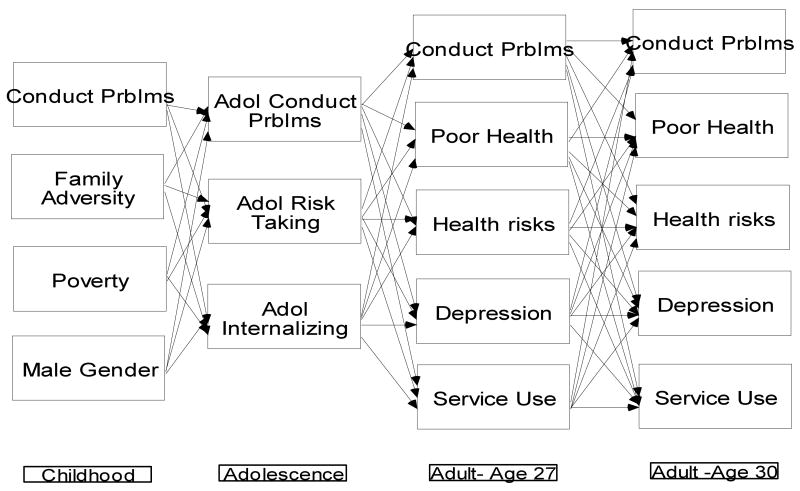
Analysis
Figure 1 shows the analysis model that guided the study. Here, each prior factor was included as a predictor of each subsequent factor longitudinally. In addition to paths shown in Figure 1, analyses accounted for within-time correlations among all variables at each wave of the study. The model was estimated using Mplus 5.0 software (Muthén & Muthén, 2004) with full-information maximum likelihood to accommodate incomplete data. Data were scaled and preliminarily analyzed in SPSS (12.0).
Figure 1.
Analysis model
A test of structural paths shown in Figure 1 was estimated for the full analysis sample after determining that variables of the model operated similarly for males and females. Tests also showed that model covariances did not significantly differ for intervention groups nested within the larger SSDP sample.
Results
Table 1 gives the bivariate correlations for variables included the analysis. Results show significant, moderate associations for most variables tested, with even stronger associations for those measured contemporaneously at each age. There were also significant longitudinal associations between the variables. For example, childhood conduct problems were correlated with adolescent conduct problems (r = .38, p < .001), adolescent risk taking (r = .28, p < .001), conduct problems at age 27 (r = .17, p < .001), health risks at age 27 (r = .15, p < .001), conduct problems at age 30 (r = .20, p < .001), health risks at age 30 (r = .16, p < .001), and depression at age 30 (r = .16, p < .01). Family adversity was significantly correlated with adolescent conduct problems (r = .12, p < .01), adolescent internalizing (r = .13, p < .01), conduct problems at age 27 (r = .10, p < .05), and health risks at age 27 (r = .13, p < .01).
Table 1. Correlations among the variables.
| Gender (male) |
Poverty | Conduct problems (10-12) |
Family adversity (<12) |
Conduct problems (14) |
Adol risk taking (14) |
Adol internalizing (14) |
Conduct problems (27) |
Poor health (27) |
Health risks (27) |
Depression (27) |
Service use (27) |
Conduct problems (30) |
Poor health (30) |
Health risks (30) |
Depression (30) |
Service use (30) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender (male) | -- | -.07* | .18*** | .02 | .18*** | .13*** | -.08* | .18*** | -.10** | .23*** | -.06 | -.09* | .04 | -.09* | .09* | -.09* | -.12** |
| Poverty | -- | .07 | .07 | .02 | .01 | .07 | .03 | .06 | .09* | .12** | .04 | .10* | .06 | .03 | .09* | -.03 | |
| Conduct problems (10-12) | -- | .15*** | .38*** | .28*** | .05 | .17*** | .00 | .15*** | .01 | .04 | .20*** | .05 | .16*** | .12** | .03 | ||
| Family adversity (<12) | -- | .12** | .07 | .13*** | .10* | .07 | .13*** | .07 | .04 | .07 | .07 | .06 | .06 | .02 | |||
| Conduct problems (14) | -- | .52*** | .03 | .26*** | .07 | .15*** | .07 | .10** | .19*** | .05 | .17*** | .08* | .06 | ||||
| Risk taking (14) | -- | .03 | .20*** | .05 | .09* | .10** | .03 | .14*** | .02 | .15*** | .15*** | .04 | |||||
| Internalizing (14) | -- | .04 | .12*** | .03 | .13*** | .04 | .07 | .09* | .07 | .13** | .04 | ||||||
| Conduct problems (27) | -- | .08* | .22*** | .19*** | .16*** | .41*** | .04 | .13*** | .13** | .14*** | |||||||
| Poor health (27) | -- | .20*** | .28*** | .29*** | .08* | .50*** | .23*** | .26*** | .20*** | ||||||||
| Health risks (27) | -- | .19** | .07 | .12** | .16*** | .46*** | .17*** | .02 | |||||||||
| Depression (27) | -- | .34*** | .18*** | .28*** | .18*** | .44*** | .20** | ||||||||||
| Service use (27) | -- | .14*** | .32*** | .07 | .26*** | .42*** | |||||||||||
| Conduct problems (30) | -- | .07 | .19*** | .17*** | .12** | ||||||||||||
| Poor health (30) | -- | .29*** | .34*** | .27*** | |||||||||||||
| Health risks (30) | -- | .28*** | .16*** | ||||||||||||||
| Depression (30) | -- | .42*** | |||||||||||||||
| Service use (30) | -- |
p < .05;
p < .01;
p < .001.
Adolescent conduct problems (age 14) were modestly correlated with conduct problems at ages 27 and 30, health risks at ages 27 and 30, service use at age 27, and depression at age 30 in the range of .08 to .26. Risk taking in adolescence (age 14) was correlated with conduct problems at age 27, health risks at age 27, depression at age 27, conduct problems at age 30, health risks at age 30, and depression at age 30, also within that general range. Adolescent internalizing was correlated with poor health at age 27, depression at age 27, poor health at age 30, and depression at age 30. All correlations for this latter set of variables were below .15. Finally, many of the variables measured at ages 27 and 30 were significantly, and somewhat more strongly, correlated in the range of .10 - .50.
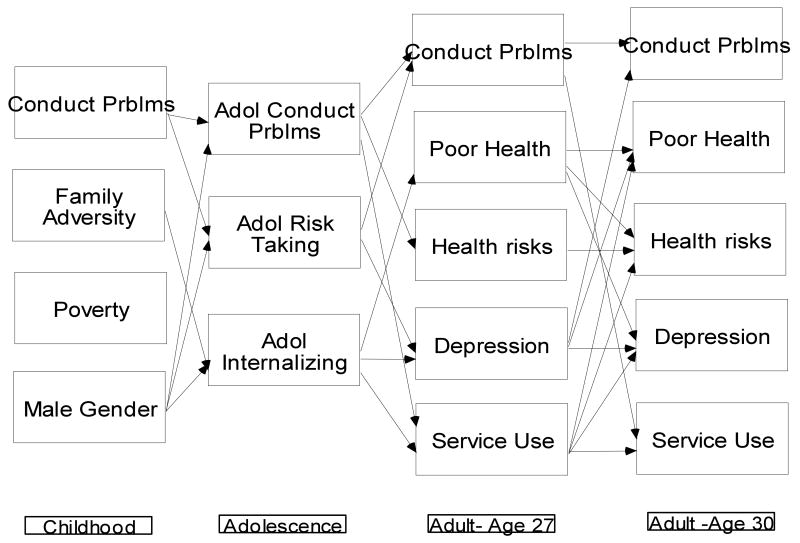
Figure 2 shows the significant paths of the hypothesized model. For clarity, nonsignificant paths were removed, as were correlations among the variables within each wave of the study (all of which were freely estimated). Standardized and unstandardized coefficients for all estimated paths of the model are shown in Table 2.
Figure 2.
Results of the hypothesized model showing statistically significant paths
Table 2. Standardized (unstandardized) path coefficients for the estimated model.
| Independent Variable | Dependent Variable | Standardized (Unstandardized) Coefficient |
|---|---|---|
| Childhood to Adolescence (age 14) | ||
| Childhood conduct problems | Adolescent conduct problems | .36 (.39)*** |
| Family adversity | .05 (.03) | |
| poverty | .00 (.00) | |
| Male gender | .13 (.05)*** | |
| Childhood conduct problems | Adolescent risk taking | .27 (.59)*** |
| Family adversity | .02 (.04) | |
| Poverty | -.03 (-.00) | |
| Male gender | .09 (.12)* | |
| Childhood conduct problems | Adolescent internalizing | .04 (.59) |
| Family adversity | .13 (.93)** | |
| Poverty | .05 (.24) | |
| Male gender | -.09 (-.44)* | |
| Adolescence to Adulthood (age 27) | ||
| Adolescent conduct problems | Conduct problems (age 27) | .20 (.12)*** |
| Adolescent risk taking | .10 (.02)* | |
| Adolescent internalizing | .03 (.00) | |
| Adolescent conduct problems | Poor health (age 27) | .05 (.21) |
| Adolescent risk taking | .02 (.02) | |
| Adolescent internalizing | .11 (.04)** | |
| Adolescent conduct problems | Health risks (age 27) | .14 (1.43)** |
| Adolescent risk taking | .02 (.06) | |
| Adolescent internalizing | .03 (.02) | |
| Adolescent conduct problems | Depression (age 27) | .02 (.32) |
| Adolescent risk taking | .09 (.35)* | |
| Adolescent internalizing | .12 (.15)** | |
| Adolescent conduct problems | Service use (age 27) | .10 (.41)* |
| Adolescent risk taking | -.04 (-.04) | |
| Adolescent internalizing | .08 (.02)* | |
| Adulthood (age 27) to Adulthood (age 30) | ||
| Conduct problems (age 27) | Conduct problems (age 30) | .38 (.25)*** |
| Poor health (age 27) | .00 (.00) | |
| Health risks (age 27) | .02 (.00) | |
| Depression (age 27) | .09 (.00)* | |
| Service use (age 27) | .05 (.01) | |
| Conduct problems (age 27) | Poor health (age 30) | -.05 (-.36) |
| Poor health (age 27) | .41 (.41)*** | |
| Health risks (age 27) | .05 (.02) | |
| Depression (age 27) | .09 (.03)** | |
| Service use (age 27) | .16 (.17)*** | |
| Conduct problems (age 27) | Health risks (age 30) | -.00 (-.01) |
| Poor health (age 27) | .10 (.18)** | |
| Health risks (age 27) | .43 (.32)*** | |
| Depression (age 27) | .03 (.01) | |
| Service use (age 27) | .11 (.21)** | |
| Conduct problems (age 27) | Depression (age 30) | .02 (.46) |
| Poor health (age 27) | .12 (.41)** | |
| Health risks (age 27) | .06 (.09) | |
| Depression (age 27) | .36 (.33)*** | |
| Service use (age 27) | .09 (.36)* | |
| Conduct problems (age 27) | Service use (age 30) | .07 (.53)* |
| Poor health (age 27) | .08 (.08)* | |
| Health risks (age 27) | -.05 (-.02) | |
| Depression (age 27) | .05 (.01) | |
| Service use (age 27) | .37 (.41)*** |
p < .05;
p < .01;
p < .001
In the model, childhood conduct problems predicted adolescent conduct problems (β = .36, p < .001) and risk taking (β = .27, p < .001), after controlling for family adversity, poverty, and male gender. Family adversity predicted adolescent internalizing (β = .13, p < .01), but not adolescent conduct problems or risk taking. Male gender, added to the model as a covariate, predicted adolescent conduct problems, risk taking, and internalizing. Poverty, another covariate in the model, predicted none of the three adolescent measures after accounting for other variables in the analysis.
Adolescent conduct problems predicted, in turn, conduct problems at age 27, health risks at age 27, and service use at age 27. Additionally, adolescent risk taking predicted conduct problems at age 27 and depression at age 27. Adolescent internalizing predicted poor health at age 27, depression at age 27, and service use at age 27.
As expected, there was considerable continuity from age 27 to age 30 in all tested outcomes: conduct problems (β = .38, p < .001), poor health (β = .41, p < .001), health risks (β = .43, p < .001), depression (β = .36, p < .001), and service use (β = .37, p < .001). Additionally, conduct problems at age 27 predicted service use at age 30. Poor health at age 27 predicted health risks at age 30, depression at age 30, and service use at age 30. Depression at age 27 predicted conduct problems at age 30 and poor health at age 30. Finally, service use at age 27 predicted poor health at age 30, health risks at age 30, and depression at age 30.
Consistent with the correlations in Table 1, most model constructs were significantly correlated within time (results not shown), although this was not the case for family adversity and male gender. Conduct problems and family adversity were only marginally correlated in the childhood wave.
In sum, results suggest that childhood risks of conduct problems and family adversity differ somewhat in their prediction of variables in adolescence. From adolescence to adulthood, conduct problems, risk taking, and internalizing were significantly predictive of similar, as well as differing, outcomes at age 27, although all variables from that intervening, second wave of the study were associated with two or more of the health and health behavior variables at that later point in development. From age 27 to age 30, results show consistency in the measured outcomes, as well as prediction across domains.
Discussion
Developmental cascade models of child and adolescent development focus on patterns of mediation and over-time changes in behavior and adverse experiences (Burt, Obradovic, Long, & Masten, 2008; Dodge, Greenberg, & Malone, 2008; Masten et al., 2005). There have been relatively few extended longitudinal studies of mediators and moderators of childhood risk factors, particularly those that account for cross-domain effects (Burt, Obradovic, Long, & Masten, 2008). Analyses of this study sought to test a cascade model of childhood risks in which conduct problems and family adversity were mediated in their prediction of later health, health behaviors, and service use by measures of adolescent conduct problems, risk taking, and internalizing. Childhood family poverty and gender were included in the model as covariates.
Findings of the study show that conduct problems predicted later conduct problems and risk taking, both of which were significant predictors of later health, mental health, conduct problems, health risks, and service use outcomes. Family adversity predicted only adolescent internalizing, although internalizing at age 14 was itself a predictor of poor health, depression, and greater use of services at age 27.
Whether conduct problems and family adversity lead to some of the same or a similar set of outcomes in adulthood through different adolescent behaviors and experiences is possible given findings of this study. One explanation for the observed differences in pathways of these risk factors is that children from abusive and high-conflict, poorly managed families may exhibit, at least initially, more emotional and psychological symptoms than physical or outward manifestations of the trauma they experienced. As children progress through adolescence, this early conflict may leave them vulnerable to other risk factors, which can, in turn, promote additional and a more extensive problems, including conduct problems and poor health. In fact, these results are quite consistent with the retrospective accounts of adults who experienced family adversity years earlier; their early hardship as children linked years later to an array of health impairments and illnesses (Felitti et al., 1998). However, it is important to note that these findings are at the same time somewhat inconsistent with prior research on child abuse and other forms of maltreatment, which shows rather robust associations between those forms of family adversity and adolescent conduct problems, including delinquency (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). With respect to either hypothesis, further testing of pathways similar to those of this study is warranted.
Pathways from adolescent variables through two waves of adult data show that there is considerable stability in health and mental health problems after they are first reported, at least for the 3-year period reflected in the analysis. Conduct problems, poor health, health risks, depression, and service use measured at age 27 all were significantly predictive of those same outcomes at age 30. Additionally, several of these variables showed cross-domain prediction, in which outcomes, like poor health at age 27, led to additional health risks, depression, and greater use of services at age 30. Further, depression at age 27 predicted poor health and conduct problems at age 30. Thus, findings show rather convincingly that, even after controlling for within-time correlations among the tested variables, problems in adult health and mental health persist, and sometimes extend into other areas.
The fact that health risks at age 27 did not predict poor health and service use at age 30 is also interesting, in that one would expect these particular behaviors (e.g., low exercise, misuse of alcohol, tobacco use) to lead to worse health and more extensive problems. However, it may be that the amount of time from the first to second adult assessment is not sufficient to capture the general deterioration in health that one would expect, and that may eventually occur, should the behaviors continue. Further testing of the links between health risks and later health problems, perhaps from early to middle adulthood, may help establish the degree to which certain health behaviors impact wellness among individuals during prime years of life.
Also of note in the current study (although not a primary focus of the analysis) are the conditional effects of male gender on all three variables in adolescence. Being male appeared to increase conduct problems and risk taking at age 14, whereas being female appeared to increase adolescent internalizing, findings that are mostly consistent with earlier research on gender (Moffitt, Caspi, Rutter, & Silva, 2001). Gender differences in risks and outcomes are examined in other studies, some of which focus on specific hypotheses of the ways in which males and females are socialized differently, or predisposed to different outcomes. Findings here, while not addressing any one hypothesis about the ways which childhood risks affect boys and girls differently over the life course, conform to the often mentioned dynamic in which boys engage more frequently and more extensively than girls in physical conduct and risk behaviors like delinquency and aggression. Ongoing analysis and replication of findings should help support/refute and extend these findings on gender.
There are many important practice and policy implications that emerge from these data, including the need for public awareness of the causes, consequences, and financial burden of early conduct problems and family adversity (Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). Prevention programs that seek to intervene early with vulnerable children; to promote child safety and improve parent-child attachments; and to restore functioning within families all appear important—and advisable—given results of this study (Dodge, Greenberg, & Malone, 2008). In some families, it may be particularly important to support and teach children how to understand and seek to positively cope with past experiences of abuse, and to avoid taking the blame for difficulties of others in the household. Findings also underscore the need for focused interventions to help parents reduce conduct problems in children, as these problems are one pathway to adult health and mental health problems. Helping parents understand and act on the needs of adolescents with depression is also warranted and may similarly reduce children's vulnerability to later outcomes investigated in this study. The study also provides useful information for programs targeting young adults. For example, findings suggest the need to assess and intervene with young adults to lessen health risks and to improve health and mental health more generally, possibly by treating depression and promoting wellness initiatives that focus on exercise, less tobacco use, and low or moderate intake of alcohol.
Limitations
Limitations of the study include a reliance on a relative few self-report measures of health and service use, which are intentionally very broad. These measures do less well in the way of isolating specific risks and disorders. However, self-reports of health have been shown to have good reliability and predictive validity (Sachs-Ericsson, Blazer, Plant, & Arnow, 2005). Nonetheless, more refined analyses of behaviors, conditions, and types of services could help establish specific links to subsequent, equally specific, outcomes. Additionally, analyses target just a few of the many possible risks and intervening variables that could predict symptoms of poor health, mental health, and service use among adults, although conduct problems and family adversity are unquestionably among the more widely referenced predictors of these and similar outcomes (Dube et al., 2003; Felitti et al., 1998; Herrenkohl, Sousa, Tajima, Herrenkohl, & Moylan, 2008). Analyses may also be limited by the use of retrospective measures of child maltreatment, which can be influenced by inaccurate recall of distant childhood events (Widom, Raphael, & DuMont, 2004). However, we sought to address this problem to some extent by combining retrospective and prospective indicators of household dysfunction and adversity in a single measure (Middlebrooks & Audage, 2008). Yet, as with other studies, errors in measurement are hard to determine and results require replication. Finally, analyses do not control for adult abuse and later family dysfunction, which can also increase current and later physical and psychological complaints and disorders (Springer, Sheridan, Kuo, & Carnes, 2003).
Acknowledgments
This research was supported by grants #1R01DA09679-11 and #9R01DA021426-08 from the National Institute on Drug Abuse and #21548 from the Robert Wood Johnson Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Respondents were asked about abuse/neglect before age 10 and through to age 18. We used the earlier age cutoff to capture a similar developmental period to that assessed with the prospective family adversity measures.
To examine gender as a potential moderator variable, we conducted a multiple-group test in which coefficients of the structural paths were constrained to be equal across the two groups. A comparison of a fully unconstrained model to one in which all paths except conduct problems at age 27 to conduct problems at age 30 were constrained equal for the two groups showed no significant reduction in overall model fit (Δχ(48) = 45.53, p > .05). The one differing path for conduct problems at ages 27 and 30 reflects the weaker correlation between these two variables for males (r = .38) compared to females (r = .57). Given that only this one difference was found, and these correlations were in the same direction and significant for both groups, a single-group model was tested.
A portion of the sample was exposed to a multicomponent preventive intervention in the elementary grades, consisting of teacher training, parenting classes, and social competence training for children (Hawkins, Catalano, Kosterman, Abbott, & Hill, 1999). While differences in prevalences and means have been observed between the intervention and control groups on variables including school bonding and depression, prior analyses have shown few differences in the covariance structures among the groups (Abbott, Catalano, & Hawkins, 1991; Catalano, Kosterman, Hawkins, Newcomb, & Abbott, 1996; Huang, Kosterman, Catalano, Hawkins, & Abbott, 2001). Analyses for this report are based on the full sample after examining possible differences in the relationships of the predictors and outcomes, comparing the control group with the intervention conditions combined. A comparison of the fully constrained model for these two groups to one in which paths for the two groups were freely estimated showed a significant reduction in overall fit (Δχ(52) = 97.05, p < .05); however, the addition of a single path from male gender to health risks at age 27 resulted in a model that was not significantly different from the fully unconstrained model (Δχ(50) = 63.53, p > .05). Given that only this one difference was found, a single-group model that combined the intervention groups was tested.
References
- Abbott RD, Catalano RF, Hawkins JD. Issues in the analysis of data from the Seattle Social Development Project. Unpublished technical report, Seattle 1991 [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Aseltine RH, Gore S, Colten ME. The co-occurrence of depression and substance abuse in late adolescence. Development and Psychopathology. 1998;10:549–570. doi: 10.1017/s0954579498001746. [DOI] [PubMed] [Google Scholar]
- Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: A systemic review. Pediatrics. 2006;117:e278–e290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Batten SJ, Aslan M, Maciejewski PK, Mazure CM. Childhood maltreatment as a risk factor for adult cardiovascular disease and depression. Journal of Clinical Psychiatry. 2004;65:249–254. doi: 10.4088/jcp.v65n0217. [DOI] [PubMed] [Google Scholar]
- Battin SR, Hill KG, Abbott RD, Catalano RF, Hawkins JD. The contribution of gang membership to delinquency beyond delinquent friends. Criminology. 1998;36:93–115. [Google Scholar]
- Burt KB, Obradovic J, Long JD, Masten AS. The interplay of social competence and psychopathology” Testing transactional and cascade models. Child Development. 2008;79:359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Kosterman R, Hawkins JD, Newcomb MD, Abbott RD. Modeling the etiology of adolescent substance use: A test of the social development model. Journal of Drug Issues. 1996;26:429–455. doi: 10.1177/002204269602600207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Murrary J, Abbott RA, Maughan B, Kuh D, Croudace TJ, et al. Outcomes of conduct problems in adolescence: 40 year follow-up of a national cohort. British Medical Journal. 2009;338:1–8. doi: 10.1136/bmj.a2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Greenberg MT, Malone PS. Testing an idealized dynamic cascade model of the development of serious violence in adolescence. Child Development. 2008;76:1907–1927. doi: 10.1111/j.1467-8624.2008.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles W, et al. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The Adverse Childhood Experiences Study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Archives of Pediatrics and Adolescent Medicine. 1999;153:226–234. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- Herrenkohl TI, Kosterman R, Hawkins JD, Mason WA. Effects of growth in family conflict in adolescence on adult depressive symptoms: Mediating and moderating effects of stress and school bonding. Journal of Adolescent Health. 2009;44:146–152. doi: 10.1016/j.jadohealth.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrenkohl TI, Sousa C, Tajima EA, Herrenkohl RC, Moylan CA. Intersection of child abuse and children's exposure to domestic violence. Trauma, Violence, & Abuse. 2008;9:84–99. doi: 10.1177/1524838008314797. [DOI] [PubMed] [Google Scholar]
- Huang B, Kosterman R, Catalano RF, Hawkins JD, Abbott RD. Modeling mediation in the etiology of violent behavior and adolescence: A test of the social development model. Criminology. 2001;39:75–107. [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;50:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Mason WA, Herrenkohl TI, Lengua LJ, McCauley E. Assessment of behavior problems in childhood and adolescence as predictors of early adult depression. Journal of Psychopathology and Behavioral Assessment. doi: 10.1007/s10862-009-9138-0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Farrington DP. The significance of child delinquency. In: Loeber R, Farrington DP, editors. Child delinquents. Thousand Oaks, CA: Sage; 2001. pp. 1–22. [Google Scholar]
- Loeber R, Stouthamer-Loeber M. Development of juvenile aggression and violence. American Psychologist. 1998;53:242–259. doi: 10.1037//0003-066x.53.2.242. [DOI] [PubMed] [Google Scholar]
- Loeber R, Wei E, Stouthamer-Loeber M, Huizinga D, Thirnberry T. Behavioral antecedents to serious and violent juvenile offending: Joint analyses from the Denver Youth Study, the Pittsburgh Youth Study, and the Rochester Development Study. Studies in Crime and Crime Prevention. 1999;8:245–263. [Google Scholar]
- Mason WA, Kosterman R, Hawkins JD, Herrenkohl TI, Lengua LJ, McCauley E. Predicting depression, social phobia, and violence in early adulthood from childhood behavior problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:307–315. doi: 10.1097/00004583-200403000-00012. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradovic J, Riley JR, et al. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41:733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Kosterman R, Mason WA, McCauley E, Hawkins JD, Herrenkohl TI, et al. Longitudinal associations among depression, obesity, and alcohol use disorders in young adulthood. General Hospital Psychiatry. 2009;31:442–450. doi: 10.1016/j.genhosppsych.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middlebrooks JS, Audage NC. The effects of childhood stress on health across the lifespan. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2008. [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in physical violence and sex similarities in partner abuse. In: Moffitt TE, Caspi A, Rutter M, Silva PA, editors. Sex differences in antisocial behaviour: Conduct disorder, delinquency, and violence in the Dunedin Longitudinal Study. New York: Cambridge University Press; 2001. pp. 53–70. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 3rd. Los Angeles: Muthen & Muthen; 2004. [Google Scholar]
- Reinherz HZ, Paradis AD, Giaconia RM, Stashwick CK, Fitzmaurice G. Childhood and adolescent predictors of major depression in the transition to adulthood. American Journal of Psychiatry. 2003;160:2141–2147. doi: 10.1176/appi.ajp.160.12.2141. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler L, Bucholtz K, Compton W. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University; 1995. [Google Scholar]
- Sachs-Ericsson N, Blazer D, Plant EA, Arnow B. Childhood sexual and physical abuse and 1-year prevalence of medical problems in the National Comorbidity Study. Health Psychology. 2005;24:32–40. doi: 10.1037/0278-6133.24.1.32. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Springer K, Sheridan J, Kuo D, Carnes M. The long-term health outcomes of childhood abuse: An overview and a call to action. Journal of General Internal Medicine. 2003;18:864–870. doi: 10.1046/j.1525-1497.2003.20918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Long-term consequences of child abuse and neglect. 2008 Retrieved March 11, 2009, from http://www.childwelfare.gov/pubs/factsheets/long_term_consequences.cfm.
- Widom CS, Raphael KG, DuMont KA. The case for prospective longitudinal studies in child maltreatment research: Commentary on Dube, Willisamson, Thompson, Felitti, and Anda. Child Abuse and Neglect. 2004;28:715–722. doi: 10.1016/j.chiabu.2004.03.009. [DOI] [PubMed] [Google Scholar]