Abstract
This study examined the relationships among three risk factors – body investment, depression, and alcohol use – and suicide proneness as measured by the Life Attitudes Schedule – Short Form (LAS-SF) in college students (n = 318). Path analysis was used to construct a causal model of suicide proneness. The Body Investment Scale (BIS) subscales were assumed to be causally prior to depression, which was in turn modeled as occurring prior to alcohol use, which was in turn modeled as prior to suicide proneness. Results revealed that, as expected suicide proneness was positively predicted by alcohol use, alcohol use was positively predicted by depression, and depression was negatively predicted by the body image component of the BIS. Additionally, the body image-suicide proneness link was significantly mediated by depression and its direct effect on suicide proneness as well as by the two-mediator path of body image on depression on drinking on suicide proneness. Implications are offered for the improved identification and treatment of young adults at risk for suicidal and health-diminishing behaviors.
The incidence of suicide among young adults has nearly tripled since the 1950s (Brener, Hassan, & Barrios, 1999). Suicide is now the third leading cause of death among young adults (18–24 years of age), following accidents and homicide (CDC, 2007), and the second leading cause of death among college students in the United States (Suicide Prevention Resource Center, 2004). Although suicide completion rates among college students are approximately one-half the U. S. national rate (Silverman, Meyer, Sloane, Raffel, & Pratt, 1997), a significant number of college students throughout the U. S. report having suicidal thoughts (Brener et al., 1999). Estimates of suicide ideation among college students range from 32% to 70% (Gutierrez, Osman, Kopper, Barrios, & Bagge, 2000). Further, suicidal ideation is often the precursor of later suicide-related behavior (Crosby, Cheltenham, & Sacks, 1999), as 34.7% of life-time suicide ideators eventually make a suicide attempt (Kessler, Borges, & Walters, 1999).
However, one barrier encountered by clinicians and prevention specialists is that the majority of current clinical assessment methods focus on assessing suicide risk directly instead of using indirect methods or measuring characteristics or risk factors that may be associated with suicidality. Nock and Banaji (2007) noted that this approach is problematic because individuals who are experiencing suicidal thoughts often conceal or deny such thoughts in order to avoid unwanted intervention and/or treatment. Thus, although research using direct methods has shown suicide ideation to be prevalent on college campuses, asking students to self-report on their suicidal thoughts may not be the best method to identify the greatest number of at-risk individuals.
Evidence also suggests that suicide prevention centers and traditional mental health resources will miss the majority of individuals at high risk for suicide (Hoffman, 2000). Moreover, only a small percentage of students who have thoughts, attempt, or commit suicide have had prior contact with campus mental health personnel (Kisch, Leino, & Silverman, 2005). Consequently, two recent lines of research have developed which have focused on improving our ability to predict suicide risk. One line has used cognitive priming tasks such as the Implicit Associations Test to assess suicidal intentions indirectly. This method has been shown to add incremental validity to the risk assessment process (Nock & Banaji, 2007). A second method has been the development of self-report measures that are designed to assess a broad domain of suicide prone and potentially life-diminishing behaviors. One such measure, the Life Attitudes Schedule – Short Form (LAS-SF; Rohde, Lewinsohn, Langhinrichsen-Rohling, & Langford, 2004), which measures the broad domain of suicide related behaviors was chosen to be the dependent variable in the current study. The LAS-SF has been shown to be a psychometrically sound instrument that can be successfully used to identify individuals who are at risk for engaging in suicidal and life-threatening behaviors (Rohde, Lewinsohn, Seeley, & Langhinrichsen-Rohling, 1996). The LAS-SF consists of items pertaining to various health-related thoughts, behaviors, and emotions that have been shown to correlate with a variety of health-compromising behaviors, including suicidality (Ellis & Trumpower, 2008; Rohde, Seeley, Langhinrichsen-Rohling, & Rohling, 2003). Use of this measure to assess suicide proneness and its associations with body investment, depression, and alcohol use in college students will thus extend the existing literature on the suicidal behavior of young adults.
Kraemer and colleagues (1997) suggest that the effectiveness of suicide prevention programs on college campuses will depend largely on how well these programs serve to mitigate the key risk factors for suicidal behavior among college students. Although the suicide rates of college student populations are lower than among those not attending college, many of the predictors or risk factors for suicide are the same (Silverman et al., 1997). Alcohol use (Schaffer, Jeglic, & Stanley, 2008) and depression (Konick & Gutierrez, 2005) or depressive symptoms are two of the key risk factors for suicidal behavior in adolescents and young adults. In addition, one’s attitude and investment in one’s body has been posited as having an important role in adolescent suicidality (Orbach, 1996; Orbach et al., 2006) and may also be a relevant risk factor for suicide proneness in young adults attending college. In spite of the considerable literature on the distinct or independent relations that alcohol use, depression, and one’s investment in one’s body have with suicidal behaviors, to our knowledge no published studies to date have simultaneously considered the relationships among these variables and suicide proneness in young adults. This study was designed to fill this gap in the literature.
Body image dissatisfaction has recently been identified as a risk factor for the development of depression in youth and young adults (Crow, Eisenberg, Story, & Neumark-Stainer, 2008; Muehlenkamp, Swanson, & Brausch, 2005; Thompson, Coovert, Richards, Johnson, & Cattarin, 1995). It has also been shown to prospectively predict depressive symptoms among several samples of adolescents (Seiffge-Krenke & Stemmler, 2002; Stice, Hayward, Cameron, Killen, & Taylor, 2000). Holsen, Kraft, and Roysamb (2001) found that body image dissatisfaction was causally related to depression over time with no evidence of a reciprocal causal effect in longitudinal data. Further, Rierdan and Koff (1997) showed that one’s negative body image perceptions were significantly predictive of levels of depressive symptomology. These studies imply that body image dissatisfaction may contribute to the onset of depressive symptoms.
A fairly recent development in the body image literature has been to delineate the components of body investment. For example, Orbach and Mikulincer’s Body Investment Scale (BIS; 1998) delineates four distinct components of body investment: body image, body care, body touch, and body protection. Body image includes attitudes and feelings about one’s body, body care focuses on how one cares for one’s body, body touch inquires about one’s comfort with physical touch, and body protection consists of questions about the extent to which one protects one’s body (Orbach & Mikulincer, 1998). Research indicates that body investment is directly and negatively related to suicidal behaviors (Orbach et al., 2006; Orbach & Mikulincer, 1998; Orbach, Stein, & Mirit-Har, 2001). In studies considering the components of body investment, negative body attitudes/feelings, comfort in touch, a lack of care for the body, and reduced body protection were all significantly associated with suicidal behaviors (Brausch & Muehlenkamp, 2007; Miotto, de Coppi, Frezza, & Preti, 2003; Muehlenkamp et al., 2005; Orbach et al., 2006; Orbach et al., 2001).
Health risk behaviors such as alcohol use have been associated with depressive symptoms and psychological well-being in college students (Ellis & Trumpower, 2008; Wietzman, 2004). Alcohol use disorders and depression have also been found to co-occur in adults (Alonso et al., 2004; Andrande, Walters, Gentil, & Laurenti, 2002). In addition some studies have indicated that there may be a direction to the relationship such that increased risk for negative alcohol outcomes such as heavy episodic drinking and alcohol dependence is more likely among adults who are depressed (Aalto-Setala, Marttunen, Tullio-Henricksson, Poikolainen, & Lonnqvist, 2002; Clark, De Bellis, Lynch, Cornelius, & Martin, 2003). Similarly, college students who suffer from depression are more likely than their mentally healthy counterparts to report alcohol use and abuse (Hussong, Hicks, Levy, & Curran, 2001; Weitzman, 2004). One explanation for this phenomenon is that college students may use alcohol to cope with their depression and negative affect (Kushner, Sher, Wood, & Wood, 1994; Hussong, Galloway, & Feagans, 2005).
Alcohol use has also been associated with increased rates of suicide attempts and completions (e.g., Ilgen, Harris, Moos, & Tiet, 2007; Kessler, Borges, & Walters, 1999; Schaffer, Jeglic, & Stanley, 2008). Brener, Hassan, and Barrios (1999) found that college students who reported higher rates of alcohol use relative to other students were at an increased risk to engage in suicidal behaviors and Powell and colleagues (2001) found that drinking frequency, drinking quantity, binge drinking, alcoholism, and immediate prior drinking were all associated with a greater likelihood of a serious suicide attempt. Additionally, two studies examining case reports of suicide attempts further support the hypothesized relation between alcohol use and later suicidal behavior (Hawton, Haigh, Simkin, & Fagg, 1995; Meilman, Pattis, & Kraus-Zeilmann, 1994). The researchers in both studies found that alcohol use immediately preceded the suicide attempt in many cases. In keeping with these findings, Reifman and Windle (1995) examined longitudinal data to determine that alcohol use was a strong predictor of later suicidal ideation and behavior.
Recent attempts to understand and prevent suicide in young adults have resulted in legislation in the United States (e.g., Garrett Lee Smith Memorial Act, 2004). At the same time, there is increased recognition that college campuses may be ideal settings for the development and implementation of suicide prevention programs (Joffe, 2008). Consequently, the purpose of the current study is to examine three risk factors for suicide proneness simultaneously – body investment, depression, and alcohol use – all which have been hypothesized to be associated with suicidal behavior and suicide proneness in college students. In this study, body investment will be measured as a multidimensional construct that includes the following components: body image, body care, body protection, and body touch. It is expected that a better understanding of the interplay among these variables will have implications for the improved identification and treatment of young adults at risk for suicide. Specifically, it is hypothesized that:
Depressive symptoms will be negatively predicted by the body image component of the Body Investment Scale (BIS; Orbach & Mikulincher, 1998). A priori, we had no basis for any specific hypotheses about the relations of body care, body protection, or body touch subscales of the BIS, to depression so any emerging findings with those subscales will be considered exploratory pending independent replication.
Alcohol use will be positively predicted by depressive symptoms and negatively predicted by all four components of the Body Investment Scale.
Suicide proneness will be positively predicted by alcohol use and depressive symptoms and negatively predicted by all components of the Body Investment Scale.
Effects of the Body Investment Scale on suicide proneness will be partially mediated by depressive symptoms and alcohol use.
Effects of depressive symptoms on suicide proneness will be partially mediated by alcohol use.
Method
Participants
Participants consisted of 318 undergraduate students at a moderate-size mid-Atlantic university who volunteered to participate in the study in return for extra credit in their psychology classes. Demographic characteristics of the sample were as follows: 60% female, 86% European American, age range, 18–50 years. Average age was 20.2 years (Median = 19.0, SD = 4.15). Eighty percent of the sample were freshmen or sophomores.
Measures
The Body Investment Scale (BIS)
The BIS (Orbach & Mikulincher, 1998) is a 24-item scale assessing adolescents’ emotional investment in the body through four subscales: body attitudes/feelings, comfort with physical touch, body care, and body protection. The body attitudes/feelings subscale measures feelings of bodily love and acceptance rather than weight and body shape with items such as “I am satisfied with my appearance” and “I feel anger toward my body” (reversed). The comfort with touch subscale is meant to assess an individual’s level of comfort with physical contact with others as well as being in close physical proximity to others with items such as “I don’t like it when people touch me” (reversed). The body care subscale assesses the extent to which an individual engages in behaviors to care for and/or pamper the body with items such as “I like to pamper my body.” The body protection subscale measures the extent to which an individual is invested in protecting the body from physical harm with items such as “I am not afraid to engage in dangerous activities” (reversed) Items are answered according to a 5-point Likert-type scale ranging from “strongly disagree” to “strongly agree.” Scores for each subscale are obtained by averaging item responses within each subscale, with higher scores indicating more positive feelings about the body, more comfort with touch, and a greater degree of body care and protection. Validation studies (Orbach & Mikulincer, 1998) showed that the BIS was correlated with Jourard and Secord’s (1955) Body Cathexis Scale, with Gray’s (1977) Body Image Scale, and with the Physical Anhedonia Scale (Blachard, Belleck, & Muser, 1994), yielding moderate-to-low but significant correlations from r = .19 to r = .63. The BIS has adequate psychometric characteristics and significantly distinguished between suicidal and non suicidal individuals in several samples (see Orbach & Mikulincer, 1998). In the present study the internal consistencies were .83, .74, .61, and .73, for the body image attitudes and feelings, body care, body protection, and comfort in touch subscales, respectively.
National College Health Risk Behavior Survey (NCHRBS, Centers for Disease Control and Prevention [CDC], 1995)
The NCHRBS is a self-administered, 96-item, multiple-choice questionnaire designed by the CDC to elicit information about a wide range of topics regarding health-related behaviors, including tobacco use, dietary behaviors, physical activity, alcohol and other drug use, safe sex practices, and other risk-related behaviors such as seat belt and helmet usage. Students answered the following question about alcohol use: “During the past 30 days, on how many days did you have at least one drink of alcohol?”
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is the depression module of the Patient Health Questionnaire (PHQ), a self-administered mental health screening instrument developed for use in primary-care settings (Spitzer, Kroenke, & Williams, 1999). The PHQ-9 consists of nine items that parallel each of the DSM-IV-TR defined symptoms of major depressive disorder. To be consistent with the DSM-IV-TR major depressive disorder criteria, each of the nine depression items is rated according to how persistent the symptom has been in the past 2 weeks, from 0 (not at all) to 3 (nearly every day), to yield a total score between 0 and 27, with higher scores indicative of greater depressive symptomology. The PHQ-9 has previously shown good internal consistency (Cronbach’s α = .89) and test-retest reliability (r = .84; Kroenke, Spitzer, & Williams, 2001).
Life Attitudes Schedule-Short Form (LAS-SF)
The LAS-SF (Rohde et al., 2004) was used to assess current suicide proneness. The LAS-SF short form is a 24-item version of the original Life Attitudes Schedule (LAS; Lewinsohn, Langhinrichsen-Rohling, Rohde, & Langford, 2004); both measures are at the 4th-grade reading level and have been shown to relate significantly to a wide variety of unhealthy and risk taking behavior (Rohde et al., 2003). Underlying the LAS measures is a theoretical model in which suicide proneness is defined broadly to consist of: 1) overtly suicidal behavior and death-related behaviors; 2) risk and injury behaviors; 3) lack of health and illness-prevention behaviors; and 4) lack of self-enhancement behaviors. Participants report whether each item was true or mostly true, or false or mostly false, for them during the past seven days. To score the LAS-SF, negative responses to positive items are reversed so that higher scores indicate greater engagement in suicide-prone behavior. The LAS-SF has been shown to have good psychometric properties (α = .78) and correlates significantly with both current suicide ideation and a history of past suicide attempts (Langhinrichsen-Rohling & Lamis, 2008). The coefficient alpha for the 24 LAS-SF items in the current sample was .71.
In addition, participants self-reported whether or not, during childhood, they experienced neglect, emotional abuse, physical abuse, sexual abuse, or had witnessed domestic violence. Standard definitions were provided for each of these terms. These terms were included in the model as possible covariates.
Procedure
Prior approval for the study was obtained from the university’s Institutional Review Board. Data collection was conducted over the course of two semesters with approximately equal numbers of participants completing the study during the spring semester and the following fall semester. Participants voluntarily chose to complete this survey in return for extra credit in their psychology courses. Data were gathered in a group setting to facilitate each participant’s sense of anonymity. Prior to data collection, written informed consent was obtained from participants, who were told that the purpose of the study was to better understand their health-related behaviors. They were advised that some items in the survey were personal in nature but that the study was anonymous and the information gathered would not be traceable to specific individuals. At the same time, participants were advised that they were free to leave any items blank that they were not comfortable answering honestly. No negative reactions were reported by participants or observed by the investigators.
Results
Analysis Strategy
The key hypotheses were evaluated in a single, saturated, path analytic model, using Mplus v5.1 (L. K. Muthén & B. O. Muthén, 2008). We selected path analysis as it could incorporate all of the hypotheses concurrently and allows us to estimate the indirect effects as well as the direct effects in one model. Although a full structural equation model (SEM) with a measurement model would have minimized any bias due to measurement error, the sample size available was not deemed adequate to estimate the measurement model effectively, especially considering that most item responses were measured using ordinal rather than interval response scales.
We tested the significance of indirect effects using the same model. Asymmetric confidence intervals (CIs) for the indirect effects were estimated using the bias-corrected bootstrap with 3,000 bootstrap draws, as recommended by MacKinnon and colleagues (2004).
Missing data were accommodated with the Full Information Maximum Likelihood (FIML) estimation feature in Mplus. This method results in unbiased estimates of the parameters when data are missing at random (MAR), meaning, roughly, that the probability of a response being missing is unrelated to the true value of that response, conditioned on other variables in the model (Little & Rubin, 1987). Given the low proportions of missing data on the modeled variables (33% of the sample variances and covariances were estimated with no more than 1% missing data; see also Table 1), and the incorporation of an array of covariates, we felt it reasonable to assume that a likelihood-based missing data strategy would lead to minimal bias in parameter estimates.
Table 1.
Correlation Matrix, Means, and Standard Deviations of study measures
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. BIS Image | -- | ||||||||
| 2. BIS Touch | .20 | -- | |||||||
| 3. BIS Care | .11 | .17 | -- | ||||||
| 4. BIS Protection | .18 | .09 | .44 | -- | |||||
| 5. Alcohol Use | .10 | .12 | −.03 | −.16 | -- | ||||
| 6. Depression | −.43 | −.14 | −.05 | −.16 | .07 | -- | |||
| 7. Suicide Proneness | −.27 | −.07 | −.34 | −.51 | .32 | .47 | -- | ||
| 8. Gender | .19 | .05 | −.42 | −.35 | .10 | −.03 | .26 | -- | |
| 9. Race | −.01 | −.12 | −.06 | .00 | −.14 | .08 | −.10 | .01 | -- |
| Mean | 3.63 | 3.47 | 3.94 | 3.95 | 1.69 | 5.01 | 5.53 | 0.40 | 0.14 |
| SD | 0.81 | 0.73 | 0.68 | 0.60 | 1.60 | 4.92 | 3.35 | 0.49 | 0.35 |
| Proportion Missing | .003 | .003 | .003 | .003 | .053 | .057 | .003 | .003 | .003 |
Note. N = 318. All correlations of magnitude greater than or equal to .11 are significant at p < .05, correlations of magnitude greater than or equal to .15 are significant at p < .01, and correlations of magnitude greater or equal to .19 are significant at p < .001. Gender and Race are dichotomous variables with male and nonwhite coded high, respectively.
Descriptive Statistics
Descriptive statistics on study variables (excluding background covariates) are presented in Table 1. These statistics are based on the FIML estimation, and thus represent the best estimates of the population parameters, after adjusting for missing data.
Analysis Model and Results
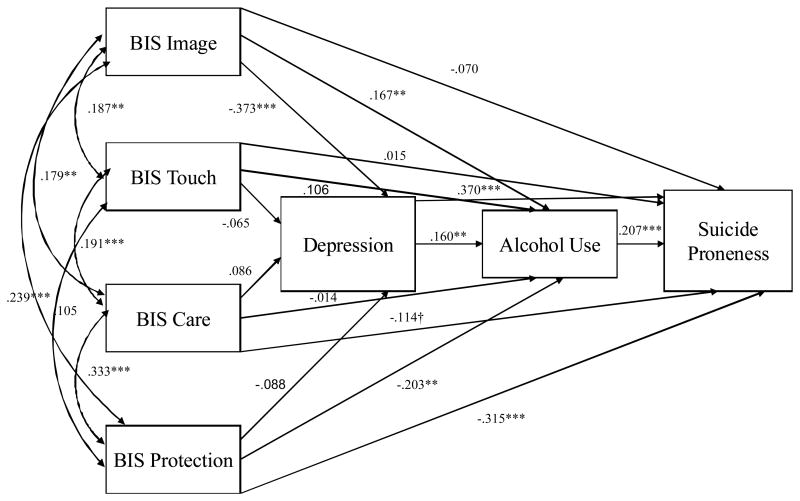
Results were obtained by fitting a saturated path analytic model, as depicted in Figure 1. The BIS subscales were assumed to be causally prior to depression, which was in turn modeled as prior to alcohol use, which was in turn modeled as prior to suicide proneness. Paths were included from each variable to all variables downstream. In addition, an array of eleven measures of potential confounding constructs, along with dichotomous indicators of gender and ethnicity, were modeled as exogenous covariates predicting all study variables.i
Figure 1.
Path model with standardized regression coefficients.
Note:†p < .05; **p < .01; ***p < .001;
The resulting unstandardized path coefficients (with standard errors in parentheses) for the study variables of interest are shown in Table 2; standardized coefficients for significant relations are described herein as they correspond to the hypotheses. Details of the paths from the background covariates are omitted for clarity (full results are available from the first author).
Table 2.
Path Coefficients
| Predictor Variable | ||||||
|---|---|---|---|---|---|---|
| Body Touch | Body Care | Body Protection | Body Image | Depressive Symptoms | 30-Day Alcohol Use | |
| Outcome | ||||||
| Depressive Symptoms | −0.443 (0.366) | 0.618 (0.461) | −0.725 (0.519) | −2.255** (0.395) | -- | -- |
| 30-Day Alcohol Use | 0.234† (0.129) | −0.034 (0.176) | −0.543** (0.165) | 0.331* (0.139) | 0.052* (0.023) | -- |
| Suicide Proneness | 0.070 (.0201) | −0.557* (0.252) | −1.760** (0.268) | −0.289 (0.201) | 0.252** (0.039) | 0.432** (0.098) |
Note: N = 318. Table values are path coefficients regressing the row variable on the column variable.
p < .10;
p < .05;
p < .01.
Hypothesis 1: Depressive symptoms will be negatively predicted by the body image component of the Body Investment Scale
As shown in Table 2 and as expected, positive body image was significantly and negatively related to depressive symptoms, standardized β = −0.373. The other BIS subscales did not contribute significant unique prediction, p’s > .10.
Hypothesis 2: Alcohol use will be positively predicted by depressive symptoms and negatively predicted by all of the components of the Body Investment Scale
As hypothesized, alcohol use within the past 30 days was positively related to depressive symptoms, β = 0.160, and negatively related to body protection, β = −0.203. However, contrary to hypothesis, alcohol use was uniquely positively predicted by positive body image, β = 0.167 (this was consistent in sign with the zero-order correlation, see Table 1). It should be noted that the zero-order correlation was not significant. A positive predictive relation from body touch to alcohol use that approached significance, p < .10, will not be discussed further, save to note that it, too, was consistent in sign with the zero-order correlation. The body care subscale did not significantly predict alcohol use, p > 10.
Hypothesis 3: Suicide proneness will be positively predicted by alcohol use and depressive symptoms and negatively predicted by all of the components of the Body Investment Scale
Consistent with this hypothesis, suicide proneness was predicted positively by alcohol use, β =0.207 and depressive symptoms, β = 0.370, and negatively predicted by body care, β = −0.114 and body protection, β = −0.315. Contrary to expectation, body touch and body image did not contribute significant unique prediction to suicide proneness. Including the confounding variables, the model accounted for .541, SE = .038, percent of the variance in suicide proneness.
Hypothesis 4. Effects of the Body Investment Scale on suicide proneness will be partially mediated by depressive symptoms and alcohol use
As expected from the absence of significant effects on the possible mediators, indirect effects of the body touch and body care scales were not significant, 95% confidence intervals including 1. The negative (beneficial) total effect of body protection on suicide proneness was significantly mediated by body protection’s direct effect on alcohol use, point estimate (product of coefficients) = −0.234, 95% CI: −0.458, −0.094, but not by depression nor the depression to alcohol path, 95% confidence intervals including 1. As noted above, the residual (direct) effect of body protection on suicide proneness was negative and significant.
The beneficial effect of positive body image on suicide proneness was significantly mediated by depression and its direct effect on suicide proneness, estimate = −0.568, 95% CI: −0.830, −0.305, as well as by the two-mediator path of body image on depression on drinking on suicide proneness, estimate = −0.051, 95% CI: −0.119, −0.011. The indirect effect traced through alcohol use but not depression was significant and positive, estimate = 0.143, 95% CI: 0.035, 0.302. The direct effect of body image on suicide proneness was not significant, p = .150. For comparison, the total effect of body image on suicide proneness was significant and negative, estimate = −0.765, 95% CI: −1.178, −0.312.
Hypothesis 5: Effects of depressive symptoms on suicide proneness will be partially mediated by alcohol use
The significant, positive (adverse) effect of depressive symptoms on suicide proneness was significantly mediated by 30-day drinking, estimate = 0.023, 95% CI: 0.005, 0.050. As noted above, the direct effect of depression on suicide proneness was also positive and significant.
Discussion
The present study investigated body investment, depression, and alcohol use as potential risk factors for suicide proneness in undergraduate college students. Past research has suggested that depressive symptoms and alcohol use may be predictors of suicidal behavior, and there has been recent interest in the role of body investment as another possible contributor to suicidality. However, previous studies have not reported findings regarding the relations among these three variables and the nature of their associations with suicide proneness in college students. Consequently, in the present study, we examined these three important variables simultaneously in a single path analytic model (Figure 1) with suicide proneness being the final outcome. Overall, the model accounted for 54% of the variance in college students’ suicide proneness.
The results indicated that measuring body investment, depressive symptoms, and alcohol use is likely to aid in the prediction of suicidal behaviors in college students. As hypothesized, depressive symptoms were positively predicted by body image dissatisfaction. These findings are consistent with previous research suggesting that one’s negative body image perceptions predict depressive symptoms (e.g., Muelenkamp et al., 2005; Stice et al., 2000). Body image dissatisfaction may contribute to depression because there is so much emphasis placed on appearance and it is a critical dimension on which individuals are evaluated in Western culture. Thus, individuals who deviate from the “normal” body image may find themselves being ridiculed by or ostracized from groups, which may further exacerbate their own negative self perceptions, consequently increasing the likelihood of depressed mood. Individuals who are struggling with their body image may also have a more difficult time adjusting to college and the new social environment. It is possible that these students may experience greater amounts of social isolation and/or loneliness, both of which have been positively associated with depression on college campuses (Joiner, 1997; Wei, Russell, & Zakalik, 2005).
Consistent with our hypothesis, alcohol use was positively predicted by depressive symptoms. Specifically, these results indicated that depressed college students are more likely to consume alcohol. This finding is consistent with several other studies that found depression to be a predictor of alcohol use in young adults (Hussong et al., 2004; Weitzman, 2004). Some researchers (e.g., Huchinson, Patock-Peskham, Cheong, & Nagoshi, 1998; Park & Levenson, 2002) suggest that college students who are experiencing depressive symptoms use alcohol as a form of self-medication to cope with existing life issues. Thus, having a better understanding of the precursors to feelings of depression may aid in the development of more efficient alcohol prevention programs at a collegiate level.
As anticipated, alcohol use was negatively predicted by body protection. This finding suggests that individuals who are less inclined to protect their bodies are more likely to engage in high-risk behaviors, such as alcohol consumption, that could potentially cause bodily harm. However, contrary to hypothesis, alcohol use was positively predicted by positive body image. This contradicts previous research in which positive body image was found to be negatively associated with alcohol use in undergraduates (Granner, Black, & Abood, 2002). The unexpected positive direct effect from positive body image to alcohol use in the path model could be interpreted in at least two ways. It may represent a suppressor effect, possibly associated with the positive correlation between the image and protection subscales. A second possibility is that it represents a countervailing indirect effect via an unmeasured mediator. Given the dangers of interpreting either unexpected suppressor effects or unmeasured-variable effects, especially in the absence of any empirical capacity to distinguish between the two, we will leave this as an open question pending replication in an independent sample.
Further, as hypothesized, suicide proneness was positively predicted by alcohol use. This finding provides additional support for the alcohol-suicide link and is consistent with previous research revealing that alcohol use is a strong predictor of suicidal behavior (e.g., Reifman & Windle, 1995; Stephenson, Pena-Shaff, & Quirk, 2006). This result indicates that college students who consume alcohol more frequently are at an increased risk for suicide. Moreover, as expected, suicide proneness was positively predicted by depressive symptoms. This finding is consistent with many other studies that show that depression is a risk factor for suicidal behavior in young adults (Konick & Guttierrez, 2005; Langhinrichsen-Rohling, Arata, Bowers, O’Brien, & Morgan, 2004). Suicide proneness was also found to be negatively predicted by the body care and body protection components of the Body Investment Scale. These findings are consistent with the work of Brausch and Muelenkamp (2007) who found that body care emerged as a significant predictor for suicide ideation. Additionally, the results align with the findings of Orbach and colleagues (2006), who reported that suicidal individuals achieved significantly lower scores on measures of body care and body protection than did a psychiatric group and control group. These findings suggest that the less one protects and cares for one’s body, the more likely one is to engage in suicidal behaviors and vice versa. However, although body protection predicted suicide proneness, it was significantly mediated by body protection’s direct effect on alcohol use. A simple interpretation of this finding suggests that individuals who fail to protect their bodies frequently consume alcohol and thus are at increased risk for suicide.
Contrary to expectation and previous research (e.g., Brausch & Muelenkamp, 2007; Orbach et al., 2001), body image dissatisfaction did not emerge as a significant and unique predictor of suicide proneness. However, consistent with our predictions, the body image-suicide proneness link was significantly mediated by depression and its direct effect on suicide proneness as well as by the two-mediator path of body image on depression on drinking on suicide proneness. These findings replicated and expanded those by Brausch and Gutierrez (2009), providing support for our model and suggesting that body image dissatisfaction may lead to suicide proneness mainly through its impact on depression and alcohol use.
Finally, the last set of analyses revealed that the effects of depressive symptoms on suicide proneness were significantly mediated by alcohol use. This result is consistent with past research indicating a relationship among these variables (Driessen et al., 1998) and further supports our proposed model. Although this finding supports the perspective that depressive symptoms may lead to alcohol use, which in turn contributes to suicide proneness, it is possible that alcohol use may also serve as a precursor to depression in the model. Further longitudinal work is warranted to examine this causal relationship.
It should be noted that there were several limitations to the present study. First, the sample consisted predominantly of young adult European-American college students. Therefore, caution should be exercised in generalizing these findings to other populations, such as older students or minorities. Replication of the study with a larger, more diverse sample will be necessary. Second, the current study was limited to self-report data, which raises the potential problem of method bias. Creating conditions that will enhance the reliability and validity of self-report data is critical for conducting research on these sensitive topics. Future studies should utilize a multi-modal data collection strategy with college students. Third, the use of a single item for alcohol use raises issues of reliability and validity. More research is needed utilizing detailed psychometrically sound alcohol use measures, such as the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Lastly, the study relied exclusively on data collected using a cross-sectional research design, which precludes causal interpretation of associations among variables. Specifically, Kline (2005) points out that significance tests and descriptive fit indices of path models do not prove that hypotheses about causality are necessarily correct, especially when the data are cross-sectional. Future longitudinal research should be conducted before causal inferences can be made regarding the directional pathways connecting these variables in college students.
In spite of these possible limitations, the study findings may help to elucidate risk factors for suicidal behaviors in young adults. These findings may also have prevention implications. Specifically, identified risk factors may be targeted in prevention efforts on college campuses. Moreover, suicide prevention efforts might be enhanced by identifying groups who are at an increased risk for suicide via less direct methods of assessment such as the LAS-SF, prior to these individuals expressing direct suicide intent. These improved intervention and prevention programs could have important implications for reducing the incidence and prevalence of suicidal behaviors on college campuses.
Footnotes
Given the possibility indicated by the literature that processes involving these factors (body investment, depression, suicide proneness) might vary by gender, we used a two-group structural equation model to identify gender interactions. There were significant differences between genders in the model taken as a whole, Wald chi-square (118, N = 318) = 223.6, p < .001. However, when the 15 hypothesis-relevant paths (among body investment, depressive symptoms, alcohol use, and suicide proneness) were constrained to be equal across genders and other estimates were allowed to vary, the constrained model fit adequately, chi-square (15, N = 318) = 18.59, p = .233. We thus concluded that gender non-invariance was not a significant threat to the validity of our findings and used simplified analyses with gender as a covariate for subsequent models.
Contributor Information
Dorian A. Lamis, University of South Carolina
Patrick S. Malone, University of South Carolina
Jennifer Langhinrichsen-Rohling, University of South Alabama
Thomas E. Ellis, Menninger Clinic, Houston, TX
References
- Aalto-Setala T, Marttunen M, Tullio-Henriksson A, Poikolainen K, Lonnqvist J. Depressive symptoms in adolescence as predictors of early adulthood depressive disorders and maladjustment. American Journal of Psychiatry. 2002;159:1235–1237. doi: 10.1176/appi.ajp.159.7.1235. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. 12-month comorbidity patterns and associated factors in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica, Supplementum. 2000;420:28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- Andrade L, Walters EE, Gentil V, Laurenti R. Prevalence of ICD-10 mental disorders in a catchment area in the city of San Paolo, Brazil. Social Psychiatry and Psychiatric Epidemiology. 2002;37:316–325. doi: 10.1007/s00127-002-0551-x. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Bellack AS, Muser T. Affective and social behavioral correlates of the physical and social anhedonia in schizophrenia. Journal of Abnormal Psychology. 1994;103:719–728. doi: 10.1037//0021-843x.103.4.719. [DOI] [PubMed] [Google Scholar]
- Brausch AM, Gutierrez PM. The role of body image and disordered eating as risk factors for depression and suicidal ideation in adolescents. Suicide and Life-Threatening Behavior. 2009;39:58–71. doi: 10.1521/suli.2009.39.1.58. [DOI] [PubMed] [Google Scholar]
- Brausch AM, Muehlenkamp JJ. Body image and suicidal ideation in adolescents. Body Image. 2007;4:207–212. doi: 10.1016/j.bodyim.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Brener DA, Hassan S, Barrios L. Suicidal ideation among collage students in the United Status. Journal of Consulting and Clinical Psychology. 1999;67:1004–1008. doi: 10.1037//0022-006x.67.6.1004. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth risk behavior surveillance: National College Health Risk Behavior Survey. Atlanta, GA: National Center for Chronic Disease and Health Promotion; 1995. [Google Scholar]
- Centers for Disease Control and Prevention. Suicide trends among youths and young adults aged 10–24 years—United States, 1990–2004. Morbidity and Mortality Weekly Report. 2007;56:905–908. [PubMed] [Google Scholar]
- Clark DB, De Bellis MD, Lynch KG, Cornelius JR, Martin CS. Physical and sexual abuse, depression and alcohol use disorders in adolescents: Onsets and outcomes. Drug and Alcohol Dependence. 2003;69:51–60. doi: 10.1016/s0376-8716(02)00254-5. [DOI] [PubMed] [Google Scholar]
- Crosby A, Cheltenham M, Sacks J. Incidence of suicidal ideation and behavior in the United States, 1994. Suicide and Life-Threatening Behavior. 1999;29:131–140. [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, Neumark-Sztainer D. Suicidal behavior in adolescents: Relationship to weight status, weight control behaviors, and body dissatisfaction. International Journal of Eating Disorders. 2008;41:82–87. doi: 10.1002/eat.20466. [DOI] [PubMed] [Google Scholar]
- Driessen M, Veltrup C, Weber J, John U, Wetterling T, Dilling H. Psychiatric co-morbidity, suicidal behaviour and suicidal ideation in alcoholics seeking treatment. Addiction. 1998;93:889–894. doi: 10.1046/j.1360-0443.1998.93688910.x. [DOI] [PubMed] [Google Scholar]
- Ellis TE, Trumpower D. Health risk behaviors and suicidal ideation: A preliminary study of cognitive and developmental factors. Suicide and Life-Threatening Behavior. 2008;38:251–259. doi: 10.1521/suli.2008.38.3.251. [DOI] [PubMed] [Google Scholar]
- Garrett Lee Smith Memorial Act, 2004.
- Granner ML, Black DR, Abood DA. Levels of cigarette and alcohol use related to eating disorder attitudes. American Journal of Health Behavior. 2002;26:43–55. doi: 10.5993/ajhb.26.1.5. [DOI] [PubMed] [Google Scholar]
- Gray SH. Social aspects of the body image perception of normality of weight and affect of college undergraduates. Perceptual and Motor Skills. 1977;45:1035–1044. doi: 10.2466/pms.1977.45.3f.1035. [DOI] [PubMed] [Google Scholar]
- Gutierrez PM, Osman A, Koper BA, Barrios FX, Bagge CL. Suicide risk assessment in a college student population. Journal of Counseling Psychology. 2000;47:403–413. [Google Scholar]
- Hawton K, Haigh R, Simkin S, Fagg J. Attempted suicide in Oxford University students, 1976–1990. Psychological Medicine. 1995;25:179–188. doi: 10.1017/s0033291700028208. [DOI] [PubMed] [Google Scholar]
- Hoffman MA. Suicide and hastened death: A biopsychosocial perspective. The Counseling Psychologist. 2000;28:561–572. [Google Scholar]
- Holsen I, Kraft P, Roysamb E. The relationship between body image and depressed mood in adolescence: A 5-year longitudinal panel study. Journal of Health Psychology. 2001;6:613–627. doi: 10.1177/135910530100600601. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Galloway CA, Feagans LA. Coping motives as a moderator of daily mood-drinking covariation. Journal of Studies on Alcohol. 2005;55:707–718. doi: 10.15288/jsa.2005.66.344. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology. 2001;110:449–461. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- Hutchinson GT, Patock-Peckham JA, Cheong J, Nagoshi CT. Irrational beliefs and behavioral misregulation in the role of alcohol abuse among college students. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 1998;16:61–74. [Google Scholar]
- Ilgen MA, Harris AHS, Moos RH, Tiet QQ. Predictors of a suicide attempt one year after entry into a substance use disorder treatment. Alcoholism: Clinical and Experimental Research. 2007;31:635–642. doi: 10.1111/j.1530-0277.2007.00348.x. [DOI] [PubMed] [Google Scholar]
- Joffe P. An empirically supported program to prevent suicide in a college student population. Suicide and Life-Threatening Behavior. 2008;38:87–103. doi: 10.1521/suli.2008.38.1.87. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Shyness and low social support as interactive diatheses, with loneliness as mediator: Testing an interpersonal-personality view of vulnerability to depressive symptoms. Journal of Abnormal Psychology. 1997;106:386–394. doi: 10.1037//0021-843x.106.3.386. [DOI] [PubMed] [Google Scholar]
- Jourard SM, Secord PF. Body cathexis on the ideal female figure. Journal of Abnormal and Social Psychology. 1955;50:243–246. doi: 10.1037/h0041128. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters MS. Prevalence of and risk factors for lifetime suicide attempts in the national comorbidity survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford; 2005. [Google Scholar]
- Kisch J, Leino EV, Silverman MM. Aspects of suicidal behavior, depression, and treatment in college students: Results from the Spring 2000 National College Health Assessment Survey. Suicide and Life-Threatening Behavior. 2005;35:3–13. doi: 10.1521/suli.35.1.3.59263. [DOI] [PubMed] [Google Scholar]
- Konick LC, Gutierrez PM. Testing a model of suicide ideation in college students. Suicide and Life-Threatening Behavior. 2005;35:181–192. doi: 10.1521/suli.35.2.181.62875. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54:337, 343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Wood MD, Wood PK. Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research. 1994;18:852–860. doi: 10.1111/j.1530-0277.1994.tb00050.x. [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Arata C, Bowers D, O’Brien N, Morgan A. Suicidal behavior, negative affect, gender, and self-reported delinquency in college students. Suicide and Life-Threatening Behavior. 2004;34:255–266. doi: 10.1521/suli.34.3.255.42773. [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Lamis DA. Current suicide proneness and past suicidal behavior in adjudicated adolescents. Suicide and Life-Threatening Behavior. 2008;38:415–426. doi: 10.1521/suli.2008.38.4.415. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Langhinrichsen-Rohling J, Rohde P, Langford RA. Attitudes Schedule (LAS): A risk assessment for suicidal and life-threatening Behaviors. Toronto, ON: Multi-Health Systems; 2004. Technical Manual. [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. J. Wiley & Sons; New York: 1987. [Google Scholar]
- Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meilman PW, Pattis JA, Kraus-Zeilmann D. Suicide attempts and threats on one college campus: Policy and practice. Journal of American College Health. 1994;42:147–154. doi: 10.1080/07448481.1994.9939662. [DOI] [PubMed] [Google Scholar]
- Miotto P, de Coppi M, Frezza M, Preti A. Eating disorders and suicide risk factors in adolescents: An Italian community-based study. The Journal of Nervous and Mental Disease. 2003;191:437–443. doi: 10.1097/01.NMD.0000081590.91326.8B. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Swanson JD, Brausch AM. Self-objectification, risk taking, and self-harm in college women. Psychology of Women Quarterly. 2005;29:24–32. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide, v.4. Los Angeles, CA: Muthen & Muthen; 2007. [Google Scholar]
- Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology. 2007;75:707–715. doi: 10.1037/0022-006X.75.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orbach I. The role of the body experience in self-destruction. Clinical Child Psychology and Psychiatry. 1996;1:607–619. [Google Scholar]
- Orbach I, Gilboa-Schechten E, Sheffer A, Meged S, Har-Even D, Stein D. Negative bodily self in suicide attempters. Suicide and Life-Threatening Behavior. 2006;36:136–153. doi: 10.1521/suli.2006.36.2.136. [DOI] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M. The Body Investment Scale: Construction and validation of a body experience scale. Psychological Assessment. 1998;10:415–425. [Google Scholar]
- Orbach I, Stien DS, Mirit-Har D. Body attitudes and body experience in suicidal adolescents. Suicide and Life-Threatening Behavior. 2001;31:237–249. doi: 10.1521/suli.31.3.237.24250. [DOI] [PubMed] [Google Scholar]
- Park CL, Levenson MR. Drinking to cope among college students: Prevalence, problems, and coping processes. Journal of Studies on Alcohol. 2002;63:486–497. doi: 10.15288/jsa.2002.63.486. [DOI] [PubMed] [Google Scholar]
- Powell K, Kresnow J, Mercy J, Potter L, Swann A, Frankowski R, et al. Alcohol consumption and nearly lethal suicide attempts. Suicide and Life-Threatening Behavior. 2001;32:30–41. doi: 10.1521/suli.32.1.5.30.24208. [DOI] [PubMed] [Google Scholar]
- Reifman A, Windle M. Adolescent suicidal behaviors as a function of depression, hopelessness, alcohol use, and social support: A longitudinal investigation. American Journal of Community Psychology. 1995;23:329–354. doi: 10.1007/BF02506948. [DOI] [PubMed] [Google Scholar]
- Rierdan J, Koff E. Weight, weight-related aspects of body image, and depression in early adolescent girls. Adolescence. 1997;32:615–624. [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Langhinrichsen-Rohling J, Langford R. Life Attitudes Schedule: Short Form (LAS-SF): A risk assessment for suicidal and life-threatening behaviors. Toronto, ON: Multi-Health Systems; 2004. Technical Manual. [Google Scholar]
- Rohde P, Lewinsohn PM, Langhinrichsen-Rohling J, Langford R. The Life Attitudes Schedule Short Form: An abbreviated measure of life-enhancing and life-threatening behaviors in adolescents. Suicide and Life-Threatening Behavior. 1996;26:272–281. [PubMed] [Google Scholar]
- Rohde P, Seeley JR, Langhinrichsen-Rohling J, Rohling ML. The Life Attitudes Schedule-Short Form: Psychometric properties and correlates of adolescent suicide proneness. Suicide and Life-Threatening Behavior. 2003;33:249–260. doi: 10.1521/suli.33.3.249.23216. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schaffer M, Jeglic EL, Stanley B. The relationship between suicidal behavior, ideation and binge drinking among college students. Archives of Suicide Research. 2008;12:124–132. doi: 10.1080/13811110701857111. [DOI] [PubMed] [Google Scholar]
- Schwartz AJ, Whitaker LC. Suicide among college students: Assessment, treatment, and intervention. In: Blumenthal SJ, Kupfer DJ, editors. Suicide over the life cycle: Risk factors, assessment, and treatment of suicidal patients. Washington, DC: American Psychiatric Press; 1990. pp. 303–340. [Google Scholar]
- Seiffe-Krenke I, Stemmler M. Factors contributing to gender differences in depressive symptoms: A test of three developmental models. Journal of Youth and Adolescence. 2002;31:405–417. [Google Scholar]
- Silverman MM, Meyer PM, Sloane F, Raffel M, Pratt D. The big ten suicide study: A 10-year study of suicides on Midwestern university campuses. Suicide and Life-Threatening Behavior. 1997;27:285–303. [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB the Patient Health Questionnnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stephenson H, Pena-Shaff J, Quirk P. Predictors of college student suicidal ideation: Gender differences. College Student Journal. 2006;40:109–117. [Google Scholar]
- Stice E, Hayward C, Cameron RP, Killen JD, Taylor CB. Body-image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology. 2000;109:438–444. [PubMed] [Google Scholar]
- Suicide Prevention Resource Center. Promoting mental health and preventing suicide in college and university settings. Newton, MA: Education Development Center, Inc; 2004. [Google Scholar]
- Wei M, Russell DW, Zakalik RA. Adult attachment, social self-efficacy, self-disclosure, loneliness, and subsequent depression for freshman college students: A longitudinal study. Journal of Counseling Psychology. 2005;52:602–614. [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. The Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]