Abstract
Pyridoxine-dependent epilepsy was recently shown to be due to mutations in the ALDH7A1 gene, which encodes antiquitin, an enzyme that catalyses the nicotinamide adenine dinucleotide-dependent dehydrogenation of l-α-aminoadipic semialdehyde/l-Δ1-piperideine 6-carboxylate. However, whilst this is a highly treatable disorder, there is general uncertainty about when to consider this diagnosis and how to test for it. This study aimed to evaluate the use of measurement of urine l-α-aminoadipic semialdehyde/creatinine ratio and mutation analysis of ALDH7A1 (antiquitin) in investigation of patients with suspected or clinically proven pyridoxine-dependent epilepsy and to characterize further the phenotypic spectrum of antiquitin deficiency. Urinary l-α-aminoadipic semialdehyde concentration was determined by liquid chromatography tandem mass spectrometry. When this was above the normal range, DNA sequencing of the ALDH7A1 gene was performed. Clinicians were asked to complete questionnaires on clinical, biochemical, magnetic resonance imaging and electroencephalography features of patients. The clinical spectrum of antiquitin deficiency extended from ventriculomegaly detected on foetal ultrasound, through abnormal foetal movements and a multisystem neonatal disorder, to the onset of seizures and autistic features after the first year of life. Our relatively large series suggested that clinical diagnosis of pyridoxine dependent epilepsy can be challenging because: (i) there may be some response to antiepileptic drugs; (ii) in infants with multisystem pathology, the response to pyridoxine may not be instant and obvious; and (iii) structural brain abnormalities may co-exist and be considered sufficient cause of epilepsy, whereas the fits may be a consequence of antiquitin deficiency and are then responsive to pyridoxine. These findings support the use of biochemical and DNA tests for antiquitin deficiency and a clinical trial of pyridoxine in infants and children with epilepsy across a broad range of clinical scenarios.
Keywords: antiquitin, pyridoxine, epilepsy, α-AASA, ALDH7A1
Introduction
Pyridoxine-dependent epilepsy (PDE) (MIM 266100) was first described in 1954 (Hunt, 1954). In classical PDE, seizures are observed within the first month of life, often within hours of birth (Baxter, 2001). They are resistant to antiepileptic drugs but are controlled within an hour by 50–100 mg of pyridoxine, usually given intravenously. The epilepsy remains controlled by 5–10 mg/kg/day of oral pyridoxine; fits may restart within days when pyridoxine is stopped but are rapidly controlled again when treatment is restarted. In atypical (late onset) PDE, seizures start later (up to 2 years) (Baxter, 2001). Up to seven days of pyridoxine therapy may be required before seizure response. Seizure freedom may then continue for up to five years following withdrawal. Various additional clinical features have been described in patients with classical PDE including abnormal foetal movements, features suggestive of birth asphyxia or hypoxic ischaemic encephalopathy, irritability, abnormal cry, exaggerated startle response, dystonic movements, respiratory distress, abdominal distension, bilious vomiting, hepatomegaly, hypothermia, shock and acidosis. Seizures may be of almost any type but generalized tonic-clonic seizures predominate. The EEG is usually severely abnormal (Nabbout et al., 1999); possible patterns include burst suppression, hypsarrhythmia and multiple spike-wave discharges. Imaging may be normal or may demonstrate cerebellar dysplasia, hemispheric hypoplasia or atrophy, neuronal dysplasia, periventricular hyperintensity or intracerebral haemorrhage (Baxter, 2001).
Until recently the biochemical basis of PDE was unknown and diagnosis was exclusively clinical. In 2000, elevation of pipecolic acid concentrations in plasma and CSF of patients with PDE was described (Plecko et al., 2005). This however is not specific for PDE with elevation also demonstrated secondary to liver disease and in peroxisomal defects (Peduto et al., 2004). Recently we showed that a group of children with classical PDE had mutations in ALDH7A1 that abolished the activity of antiquitin as an l-α-aminoadipic semialdehyde (α-AASA)/l-Δ1-piperideine 6-carboxylate (P6C) dehydrogenase (Mills et al., 2006). In solution, α-AASA is in equilibrium with P6C, its cyclic Schiff base. These children accumulated α-AASA in their body fluids and P6C was shown to inactivate the active form of pyridoxine (pyridoxal phosphate) by the formation of a Knoevenagel condensation product. Mutations in the ALDH7A1 gene in other children with PDE have been reported subsequently (Kanno et al., 2007; Plecko et al., 2007; Salomons et al., 2007; Kaczorowska et al., 2008; Bennett et al., 2009; Gallagher et al., 2009; Kluger et al., 2009; Striano et al., 2009), including in patients who had been previously diagnosed as having ‘folinic acid responsive seizures’. To characterize further the phenotypic spectrum of this disorder we investigated individuals with clinically proven or suspected PDE by measurement of urinary α-AASA and mutational analysis of the ALDH7A1 gene.
Materials and methods
Patients
This study was approved by the Ethics Committee of the UCL Institute of Child Health and Great Ormond Street Hospital. Urine samples were sent to our laboratories for analysis of urinary α-AASA/creatinine ratio because the primary clinician suspected or wanted to rule out PDE. A preliminary analysis indicated that the ion chromatograms were of inferior quality when very dilute samples were analysed therefore a repeat sample was requested. The results included in this article are all on urine samples with a creatinine >0.5 mM.
Of the 272 urine samples with creatinine >0.5 mM, 269 samples (from 243 patients) were from children with a seizure disorder and three were asymptomatic heterozygote first degree relatives of patients shown to have two ALDH7A1 mutations. When a urine sample was shown to have an elevated α-AASA/creatinine ratio relative to the control range established using urine samples from normal children (Mills et al., 2006), a repeat urine analysis or sequence analysis of the ALDH7A1 gene was offered to the family. Of the 269 samples from symptomatic patients, seven were duplicate urine samples (i.e. seven patients, 14 samples), eight were triplicate samples (i.e. eight patients, 24 samples) and four samples were from one patient in order to determine whether an elevated value could be confirmed. Of the 243 patients (208 urine samples from 208 patients; 10 urine samples from five patients; 24 urine samples from eight patients; four urine samples from one patient), 222 who had no ALDH7A1 mutations or no reported response to pyridoxine and the three asymptomatic heterozygotes were assigned to the control group. Values of urinary α-AASA/creatinine ratio for this group were subsequently used to establish new age-specific control ranges for children investigated for PDE (see Results section for further details).
ALDH7A1 sequencing was undertaken on 21 patients who had elevated urinary α-AASA, in addition to 16 patients with a clinical diagnosis of PDE (Baxter, 2001) in whom urinary α-AASA/creatinine ratio was not measured. For all patients shown to have a mutation or mutations in the ALDH7A1 gene, the referring clinician was asked to fill in a questionnaire regarding clinical, biochemical, MRI and EEG features. Detailed histories of patients who demonstrated a severe phenotype, classical PDE with additional features, cortical malformations and late-onset PDE are included in the online Supplementary material.
Biochemical methods
The chemical synthesis of AASA/P6C was as described previously (Mills et al., 2006). Essentially, allysine ethylene acetal was deblocked by mixing with Amberlyst-15 (dry) ion exchange resin. The resin was subsequently washed twice with 1 ml water prior to elution of AASA/P6C from the resin with 25% ammonia solution. The eluant was dried under nitrogen at room temperature and resuspended in water. Measurement of α-AASA in urine was performed using liquid-chromatography-tandem mass spectrometry (Mills et al., 2006). One nmol of 15N-α-aminoadipic acid was added to 10 µl of urine prior to derivatization with 9-fluorenylmethyl chloroformate. Reaction mixture (15 µl) was analysed on a 5 cm × 2.1 mm, 5 µm Discovery® HS F5 high-pressure liquid chromatography column (Supelco). The fluorenylmethyloxycarbonyl derivatives of α-aminoadipic semialdehyde and 15N-aminoadipic acid were eluted from the column. The mobile phase consisted of A (4 mM ammonium acetate, pH 5.0) and B (100% acetonitrile) and the following gradient was used: 0–1.9 min (95% A and 5% B; 0.5 ml/min), 2–10 min (80% A and 20% B to 20% A and 80% B; 0.25 ml/min), 10–12 min (80% A and 20% B to 100% B; 0.25–0.5 ml/min), 12–16 min (100% B; 0.5 ml/min). The column was then re-equilibrated prior to the next sample injection. All gradient steps were linear. 15N-Aminoadipic acid and α-AASA were analysed in positive ion mode. The multiple reaction monitoring transitions monitored were 366.04 > 144.04 m/z and 383.02 > 161.06 m/z for α-AASA and 15N-aminoadipic acid, respectively.
The concentration of creatinine was determined by liquid-chromatography-tandem mass spectrometry, using a Waters 2795XE high-pressure liquid chromatograph coupled to an electrospray triple quadrupole mass spectrometer (QuattroMicro, Waters, UK). Ten microlitres of 5 mM creatinine-d3 (CDN isotopes) were added to 10 µl of urine and diluted with 200 µl of water. Ten microlitres of the mixture was analysed on a 5 cm × 2.1 mm, 5 µm Discovery® HS F5 high-pressure liquid chromatography column (Supelco). The mobile phase consisted of A (4 mM ammonium acetate, pH 5.0) and B (MeOH) and the following gradient was used: 0–1.9 min (95% A and 5% B; 0.5 ml/min), 1.9–2 min (95% A and 5% B to 100% A; 0.2 ml/min) 2–6 min (100% B; 0.5 ml/min), 6.01–10.00 min (95% A and 5% B; 0.5 ml/min). All gradient steps were linear. The multiple reaction monitoring transitions monitored were 113.70 > 43.90 m/z and 116.70 > 46.90 m/z for creatinine and creatinine-d3, respectively.
All control urine samples featured in this article were measured by the laboratory in London whilst those of patients with clinical PDE were measured either in London or Amsterdam. The concentration of pyridoxal phosphate in CSF was determined using published methods (Ormazabal et al., 2008).
ALDH7A1 gene analysis
Mutation analysis of the ALDH7A1 gene was essentially as described previously (Mills et al., 2006). The 18 exons and intron/exon boundaries of the antiquitin gene were amplified by polymerase chain reaction using intronic primers. A typical polymerase chain reaction reaction using 100 ng of genomic DNA contained 25 pmol of each primer, 1 × NH4 reaction buffer (Bioline), 0.2 mmol/l deoxynucleotide triphosphates and 0.25 µl (1.25 units) BioPro DNA polymerase (Bioline) (added after a ‘hot start’). PCRx Enhancer System (Invitrogen) was used for amplification of exon 6. Mutations were detected by directly sequencing the amplified regions using the BigDye Terminator v. 3.1 Cycle Sequencing Kit (Applied Biosystems) and the MegaBACE capillary DNA sequencer (Amersham Biosciences). All new sequence changes were confirmed by digestion with a restriction enzyme or by amplification created restriction site polymerase chain reaction. Numbering of mutations is based on the Ensembl protein-coding gene, ENSG00000164904 (http://www.ensembl.org) with +1 as the A of the ATG initiation codon and the Ensembl transcript, ENST00000297542. Any mutations that were believed to have an affect on splicing were analysed using a splice site prediction programme (http://fruitfly.org/seq_tools/splice.html).
Results
Urinary α-AASA as a diagnostic test
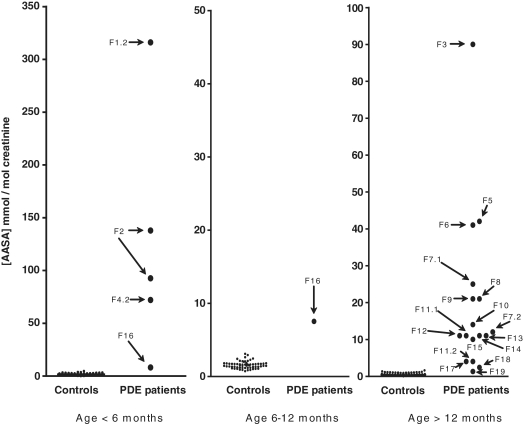
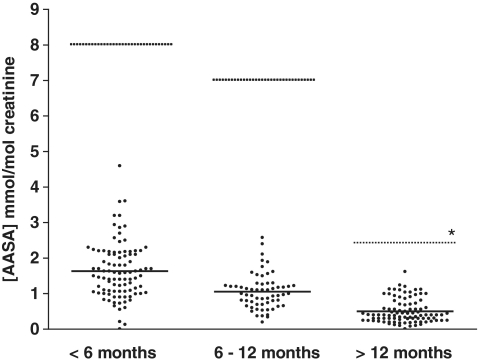
Analysis of urinary α-AASA by liquid-chromatography-tandem mass spectrometry in 272 samples identified 21 new patients with PDE; the urinary α-AASA/creatinine ratio (Fig. 1 and Table 1) was well above the control range (<1 mmol/mol creatinine) (Mills et al., 2006) and sequencing of ALDH7A1 showed mutations. Two of these patients had a second urine sample analysed, therefore two values are included in Fig. 1. The α-AASA/creatinine ratios of the patients with ALDH7A1 mutations were >7 mmol/mol creatinine in children <6-months-old and from 6 months to 1 year (six samples from four patients) and >2 mmol/mol creatinine for children over 1 year of age (16 samples from 16 patients). There was one exception; one symptomatic and pyridoxine responsive child (F19), for whom we only found one heterozygous mutation, had a urinary α-AASA concentration of 1.3 mmol/mol creatinine. This was only just above the upper limit of the control range of the laboratory in Amsterdam where this sample was analysed. Two infants aged <6 months, who did not fit the clinical criteria for definite PDE (P1 and P2), had duplicate samples with urinary α-AASA excretion in the range 2.2–4.6 mmol/mol creatinine; ALDH7A1 was sequenced for these two infants and no mutations were found. A third urine sample from P1 and P2 showed ratios of <1.0 and <1.2, respectively. Hence a new threshold for ALDH7A1 sequencing was established for the laboratory in London (<6 months, <5 mmol α-AASA/mol creatinine; 6–12 months, <2.5 mmol α-AASA/mol creatinine; >12 months, <2 mmol α-AASA/mol creatinine). Subsequently, 12 other urine samples were also found to have a urinary α-AASA concentration >1.0 mmol α-AASA/mol creatinine but below these thresholds. At least one repeat sample from nine of the 12 showed a value <1.0 and all were below the new thresholds and so they were assigned to the control group. Of the 249 urine α-AASA results assigned to the control group [no mutations (two patients, seven samples), no diagnostic response to pyridoxine and/or alternative diagnosis (239 samples, 217 patients) or asymptomatic heterozygotes (three patients)], 95 were aged <6 months, 61 were aged 6–12 months, and 93 were over 1 year (Figs 1 and 2). Analysis of the α-AASA/creatinine ratios in these three groups using the Dunn’s multiple comparison test showed that the three groups were significantly different from one another indicating that the urine α-AASA excretion is age-dependent.
Figure 1.
Analysis of urinary α-AASA for patients with mutations in ALDH7A1 and age-matched controls. Number of controls measured: age <6 months = 95; age 6–12 months = 61; age >12 months = 93. Patient F2 had two measurements of urinary α-AASA while under 6 months of age and Patient F16 had α-AASA measured once when <6 months and once when 6–12 months of age.
Table 1.
Summary of mutations found in ALDH7A1
| Family | Current age | α-AASA concentration mmol/mol creatinine | Mutation | Presumed effect | Age of onset | Published (ref.) |
|---|---|---|---|---|---|---|
| F1.2 | Died at 1 m | 316(Am) | c.[1482-1G>C] (P) + c.[1482-1G>C] (M) | Splice errors + splice errors | 1 h | Novel |
| F2 | 1 y | 93(Lon), 138(Lon) | c. [248G>A] + c. [818A>T] | p. [Gly83Glu] + p. [Asn273Ile] | 7 d | Plecko et al., 2007; Gallagher et al., 2009 |
| F3 | 14 y, 9 m | 90(Am) | c. [712C>T] + c. [712C>T] | p. [Arg238Stop] + p. [Arg238Stop] | 2 d | Bennett et al., 2009 |
| F4.2 | 3 y, 11 m | 72 (Lon) | c. [758delA] (P) + c. [758delA] (M) | p. [Gln253 frameshift] (P) + p. [Gln253 frameshift] (M) | <24 h | Novel |
| F5 | 2 y, 2 m | 42(Lon) | c. [1195G>C] +c.[1343C>T] | p. [Glu399Gln] + p. [Ser448Leu] | 9 weeks | Mills et al., 2006; novel |
| F6 | 4 y, 10 m | 41 (Lon) | c. [1195G>C] (P) + c. [1195G>C] (M) | p. [Glu399Gln] (P) + p. [Glu399Gln] (M) | 2 h | Mills et al., 2006 |
| F7.1 | 13 y, 10 m | 25 (Lon) | c. [750G>A] (M) + c. [233C>T] (P) | Splice errors (M) + p. [Pro78Leu] (P) | 3 d | Salomons et al., 2007; novel |
| F7.2 | 15 y, 5 m | 12(Lon) | c. [750G>A] (M) + c. [233C>T] (P) | Splice errors (M) + p. [Pro78Leu] (P) | 3 d | Salomons et al., 2007; novel |
| F8 | 4 y, 5 m | 21(Lon) | c.[1195G>C] +? | p. [Glu399Gln] +? | 6 d | Mills et al., 2006 |
| F9 | 6 y, 11 m | 21(Am) | c. [1195G>C] (P) + c. [1195G>C] (M) | p. [Glu399Gln] (P) + p. [Glu399Gln] (M) | <24 h | Mills et al., 2006 |
| F10 | 3 y, 6 m | 14(Lon) | c.191_192insA (M) + c.[1195G>C] (P) | p. [Val64 frameshift] (M) + p. [Glu399Gln] (P) | 2 h | Mills et al., 2006; novel |
| F11.1 | 9 y, 4 m | 11(Am) | c.[750G>A] (P) + c.[505C>T] (M) | Splice errors (P) + p. [Pro169Ser] (M) | 8 d | Salomons et al., 2007; novel |
| F11.2 | 6 y, 10 m | 4(Am) | c.[750G>A] (P) + c.[505C>T] (M) | Splice errors (P) + p. [Pro169Ser] (M) | 8 d | Salomons et al., 2007; novel |
| F12 | 16 y, 3 m | 11(Am) | c. [1429G>C] + c. [500A>G] | p. [Gly477Arg] + p. [Asn167Ser] | <24 h | Bennett et al., 2009 |
| F13 | 18 y, 10 m | 11(Am) | c. [1195G>C] + c. [749delT] | p. [Glu399Gln] + p. [Val250 frameshift] | 2 d | Mills et al., 2006; novel |
| F14 | 6 y, 10 m | 11(Am) | c. [1405+2T>C] + c. [1429G>C] | Splice errors + p. [Gly477Arg] | 4 d | Bennett et al., 2009; novel |
| F15 | 6 y, 9 m | 10(Lon) | c. [446C>A] + c. [446C>A] | p. [Ala149Glu] + p. [Ala149Glu] | 14 d | Novel |
| F16 | 3 y, 5 m | 8(Lon), 7(Lon) | c. [866C>T] +? | p. [Ser289Leu] +? | 5 d | Novel |
| F17 | 18 y, 8 m | 4(Am) | c.[1195G>C] (M) + c.[611+5G>A] | p. [Glu399Gln] (M) + Splice errors | 1 d | Mills et al., 2006; novel |
| F18 | 5 y, 6 m | 2.4(Lon) | c.[505C>T] (P) + c.[505C>T] (M) | p. [Pro169Ser] (P) + p. [Pro169Ser] (M) | 7 d | Novel |
| F19 | 17 y, 11 m | 1.3(Am) | c. [523T>G] (not P) +? | p. [Trp175Gly] +? | 14 m | Novel |
| F20 | 30 y, 4 m | n.m. | c. [244C>T] + c. [523T>G] | p. [Arg82Stop] + p. [Trp175Gly] | 8 m | Mills et al., 2006; novel |
| F21 | 3 y, 2 m | n.m. | c. [899A>G] (P) + c. [899A>G] (M) | Q300R (P) + Q300R (M) | 1 d | Novel |
| F22a | 15–26 y | n.m. | c. [385G>C] (P) + c. [1192A>C] (M) | A129P (P) + T398P (M) | 30 min | Novel; novel |
| F23 | 2 y | n.m. | c.[787+3del AAGT] + c.[787+3del AAGT] | p. [Gly263 frameshift] + p. [Gly263 frameshift] | <24 h | Novel |
| F24 | 22 y | n.m. | c. [157C>T] (P) + c. [157C>T] (M) | p. [R53Stop] (P) + p. [R53Stop] (M) | <4 d | Novel |
| F25 | 34 y, 9 m | n.m. | c. [750G>A] + c. [1195G>C] | Splice errors + p. [Glu399Gln] | Unknown | Mills et al., 2006; Salomons et al., 2007 |
| F26a | 17–20 y | n.m. | c.[434-1G>C] + c.[434-1G>C] | Splice errors + splice errors | <4 d | Mills et al., 2006 |
| F27b | 14–16 y | n.m. | c. [1140T>G] + c. [1140T>G] | p. [Y380Stop] + p. [Y380Stop] | <4 d | Mills et al., 2006 |
| F28 | 23 y, 9 m | n.m. | c.[1195G>C] (P) + c.[1195G>C] (M) | p. [Glu399Gln] (P) + p. [Glu399Gln] (M) | <4 d | Mills et al., 2006 |
| F29 | 5 y | n.m. | c.[890C>G] (M) + c.[1405+5G>A] (P) | p. [Thr297Arg] (M)+ Splice errors (P) | <7 d | Gallagher et al., 2009; Striano et al., 2009 |
| F30 | 22 y, 4 m | n.m. | c.419–422delTCTT + c.[1195G>C] | p. [Ile140 frameshift] + p. [Glu399Gln] | Unknown | Mills et al., 2006; Gallagher et al., 2009 |
Where parent DNA available inheritance was investigated and the allele carrying the mutation is indicated as: P (paternal) or M (maternal). n.m. = not measured; ? = no second mutation found; (Am) = sample analysed in Amsterdam (control range = <1 mmol/mol creatinine); (Lon) = sample analysed in London [Control range: <2.5 mmol/mol creatinine (<6 months), <1.5 mmol/mol creatinine (6–12 months), <1.0 mmol/mol creatinine (>12 months)]; y = years; m = months; d = days.
a Three affected siblings.
b Two affected siblings.
Figure 2.
Urinary α-AASA concentrations of controls. All of these controls were measured in the laboratory in London. Number of controls measured: age <6 months = 95; age 6–12 months = 61; age >12 months = 93. Solid line represents the mean. Dotted line indicates the lowest measurement of α-AASA in age-related patients with PDE in whom at least one mutation in ALDH7A1 has been demonstrated. Using the Dunn’s multiple comparison test, the three control groups are found to be significantly different from each other (P < 0.001). The asterisk indicates that Patient F19 had a urine excretion <2 but was measured in the laboratory in Amsterdam and we have found one ALDH7A1 mutation (see Supplementary material).
An additional 16 patients with a clinical phenotype of PDE, in whom α-AASA was not measured, have also been confirmed genetically.
Mutations
Mutations were identified in ALDH7A1 of 37 individuals (Table 1) from 30 families. Seventeen of these were novel mutations and included missense, nonsense and splice site mutations as well as deletions and a single-base insertion. All other mutations have been published previously (Mills et al., 2006; Kanno et al., 2007; Plecko et al., 2007; Salomons et al., 2007; Kaczorowska et al., 2008; Bennett et al., 2009; Gallagher et al., 2009; Kluger et al., 2009; Striano et al., 2009). The novel missense mutations P169S, P78L, W175G, S289L, Q300R and S448L were not found in ethnically matched controls (Caucasian; n = 96). Similarly, the novel missense mutations A129P, A149E and T398P were also not found in ethnically matched controls (Pakistani; n = 96). A splice site prediction tool was used to predict the effect of the novel splice site mutations; c.1482−1G>C and c.1405+2T>C are both predicted to result in the abolition of splice sites. For the novel splice mutation c.611+5G>A, however, the prediction tool suggests that the extremely high probability score of 0.99 for the authentic donor site only drops to 0.92 in the presence of the mutation. However, this mutation was not found in 96 ethnically matched control samples and analysis of urinary α-AASA (Table 1) confirmed the clinical diagnosis of PDE.
Only one mutated allele has been identified for patients F19, F16 and F8. Two of these patients had clearly elevated levels of urinary α-AASA (Table 1). In one (F19) the elevation is equivocal (Supplementary material) but clinically he had late onset PDE, with seizures recommencing within 10 days of pyridoxine withdrawal on three occasions.
Biochemical data
For some patients, data were available for CSF and plasma analyses prior to treatment (Tables 2 and 3). Additionally we had data from two patients described previously (H1 and H2) (Mills et al., 2006). In all of these patients, CSF threonine was elevated. In three patients in whom 3-methoxytyrosine was measured, this was elevated prior to treatment and elevated 38 days after a single intravenous dose of pyridoxine. CSF glycine was only elevated in 3/5, taurine in 1/2 and histidine in 1/4. Alanine, glutamine, phenylalanine and methionine were elevated in 3/4. Arginine was low in 2/4. CSF glutamate and aspartate were low-normal or low. Plasma analyses showed that all patients had elevated plasma glycine; a number of other amino acid abnormalities were seen but inconsistently or with fewer than three results available.
Table 2.
CSF biochemistry of patients with PDE with proven mutations in the ALDH7A1 gene prior to treatment
| CSF concentration (µM) |
|||||||
|---|---|---|---|---|---|---|---|
| Patient identifier | H1a | F4.2 | F29 | Normal range | F1.2 | F1.1 | Normal range |
| Threonine | 78 | 53 | 97 | 10–45 | 107 | 118 | 0–101 |
| Glycine | 8 | 5 | 28 | 4–14 | 18 | 17 | 3.7–7.6 |
| Taurine | 7 | 13 | n.d. | 3–10 | n.d. | n.d. | n.d. |
| Histidine | 40 | 18 | n.d. | 3–18 | 23 | 36 | 8–29 |
| Alanine | 46 | 18 | n.d. | 16–36 | 45 | 70 | 17–37 |
| Aspartate | n.d. | n.d. | n.d. | n.d. | 1 | 1 | 3.1–9.9 |
| Arginine | 15 | 11 | n.d. | 15–40 | 9 | 13 | 10–30 |
| Methionine | 9 | 6 | n.d. | 2–6 | 11 | 15 | 0.7–6.0 |
| Glutamine | 1126 | 549 | n.d. | 420–600 | 1063 | 971 | 363–785 |
| Glutamate | 3 | 2 | n.d. | 5–17 | 2 | 0 | 0–7.8 |
| Phenylalanine | 27 | 16 | n.d. | 5–15 | 37 | 43 | 0.6–23 |
| Serine | 49 | 46 | n.d. | 10–81 | 45 | 57 | 27–77 |
| 3-methoxytyrosine | n.d. | 0.13 (11d)b0.44 (38d)c | 1.2 | <0.3 | n.d. | n.d. | |
| Peaks seen in folinic acid dependent epilepsy | Present | Present | Not seen | ||||
These data were collected from three different laboratories using different methodologies for CSF amino acid analysis. For this reason the reference range for the local laboratory is given to the right of each patient’s results. n.d. = not determined.
Bold values indicate above the normal range for the measuring laboratory.
Underlined values indicates below the normal range for the measuring laboratory.
a Mutation analysis published previously (Mills et al., 2006).
b Pyridoxine 50 mg i/v had been given at 7 d (4 days previously).
c Pyridoxine 50 mg i/v had been given at 7 d (38 days previously).
Table 3.
Plasma biochemistry of patients with PDE with proven mutations in the ALDH7A1 gene prior to treatment
| Plasma concentration (µM) |
|||||||
|---|---|---|---|---|---|---|---|
| Patient identifier | F16 | H2a | H1a | Normal range | F1.2 | F1.1 | Normal range |
| Threonine | 138 | 127 | 92 | 70–220 | 129 | 116 | 70–190 |
| Glycine | 409 | 437 | 349 | 100–330 | 415 | 573 | 140–300 |
| Taurine | 155 | 200 | 221 | 40–140 | 99 | 38 | 35–110 |
| Histidine | 105 | 129 | 100 | 30–150 | 54 | 58 | 60–105 |
| Alanine | 529 | 102 | 336 | 150–450 | 243 | 470 | 190–450 |
| Aspartate | n.d. | n.d. | n.d. | n.d. | 3 | 3 | 5–10 |
| Arginine | 67 | 34 | 26 | 40–120 | 10 | 28 | 40–110 |
| Citrulline | n.d. | n.d. | n.d. | n.d. | 6 | 12 | 10–35 |
| Glutamine | 691 | 858 | 605 | 480–800 | 767 | 681 | 400–700 |
| Glutamate | 156 | 27 | 26 | 25–130 | 92 | 78 | 30–100 |
| Proline | 267 | 510 | 547 | 85–290 | 313 | 241 | 100–280 |
| Serine | 456 | 146 | 124 | 90–290 | 144 | 199 | 65–279 |
n.d. = not determined.
Bold values indicate above the normal range for the measuring laboratory.
Underlined values indicate below the normal range for the measuring laboratory.
a Mutation analysis published previously (Mills et al., 2006).
Clinical phenotypes
The available clinical data confirmed that the spectrum of additional features previously described in PDE (Baxter, 2001), occur in antiquitin deficiency. Our series also identified some new clinical features including profound electrolyte derangement (hypocalcaemia and hypomagnesaemia) and endocrine disturbance (hypothyroidism, diabetes insipidus) that broaden the clinical phenotype (Table 4 and Supplementary material). This series highlights some of the practical difficulties in relying upon clinical response to pyridoxine to make a diagnosis of, or to exclude, PDE. For example, 38% of patients with antiquitin deficiency had seizures that were partially controlled by antiepileptic drugs, and in addition 14% did not show a clear clinical or EEG response to pyridoxine—often when other antiepileptic drugs were being given or in the presence of electrolyte disturbance or infection. Following withdrawal of pyridoxine, fits took up to 51 days to recur (mean = 13.5 days; median = 9 days, range 1–51 days; n = 11).
Table 4.
Clinical features observed in patients with PDE diagnosed by urine α-AASA measurement and ALDH7A1 gene analysis
| Clinical features and demographics | Incidence |
|---|---|
| Gender | Male 12; female 20 |
| Ethnicity | Caucasian 22; Turkish 1; Mauritian 1; Algerian 4; Pakistani 1; Indian 1; Ghanaian 1; Caucasian/Asian 1 |
| Parental consanguinity | 7/28 (25%) |
| Gestational age ≤37/40 | 5/28 (18%) |
| Abnormal intrauterine movements | 8/24 (33%) |
| Foetal distress | 8/27 (29%) |
| Apgar score <7 at 1 min | 3/20 (15%) |
| Acidosis | 6/23 (26%) |
| Respiratory distress | 6/18 (33%) |
| Hypotonia (neonatal) | 13/23 (57%) |
| Abdominal distension/vomiting | 6/22 (27%) |
| Irritability | 14/24 (58%) |
| Seizure onset within first 28 days | 24/27 (89%) |
| Resistance to antiepileptic drugs | Complete: 14/24 (58%); partial: 9/24 (38%) |
| Seizure type: clonic | 21/23 (91%) |
| Seizure type: tonic | 11/25 (44%) |
| Seizure type: myoclonic jerks | 16/26 (62%) |
| Pyridoxine trial at ≤28 days | 22/29a (76%) |
| Age at first pyridoxine trial | Range 1 day–3 years; median 8 days |
| Cardiovascular/respiratory decompensation with pyridoxine trial | 6/22 (27%) |
| Complete cessation of seizures with first trial of pyridoxine | 25/29 (86%) |
| Speech delay | 11/19 (58%) |
| Squint | 6/18 (33%) |
| Motor delay | 18/24 (75%) |
| Breakthrough seizures with fever | 8/23 (35%) |
| Trial of pyridoxine withdrawal (range of days until seizure recurrence) | 14/23 (61%) (1–51 days) |
| Observed in the present series but not previously described in clinically diagnosed classical PDE | |
| Thrombosis | 1 |
| Escherichia coli sepsisa | 2 |
| Hypocalcaemia plus hypomagnesaemia | 2 |
| Hypoglycaemia | 4 |
| Diabetes insipidus | 1 |
| Optic nerve hypoplasia | 2 |
| Hypothyroidism | 1 |
a Reported previously but only in one patient (Adam et al., 1972).
In two late-onset patients (F20 and F19), seizures commenced at 8 and 14 months, respectively. F20 had two mutations in the ALDH7A1 gene and learning difficulties responded to an increased dose of pyridoxine (Supplementary material) (Baxter, 2001). In the case of F19 (Supplementary material) both seizures and autistic features responded to treatment with pyridoxine.
Reported seizure types (Table 4) included clonic (91%), myoclonic jerks (62%) and tonic (44%). The EEG abnormalities (Table 5) included burst suppression (21%) and hypsarrythmia (5%). Normal EEG recordings have been reported in antiquitin deficiency both prior to and following pyridoxine treatment (F20, F13). In two children (F4.2 and F19), abnormal movements were not accompanied by EEG changes and may have been due to dystonia.
Table 5.
Summary of EEG findings for patients with an elevated concentration of urinary α-AASA
| Family | α-AASA (mmol/mol creatinine) | EEG (performed before treatment with pyridoxine except where stated otherwise) | Age of onset |
|---|---|---|---|
| F1.2 | 316(Am) | Burst suppression pattern | 1 h |
| F2 | 93(Lon) (9 days); 138(Lon) (3 m) | Background moderately abnormal with excess of spiky morphology and irregular unvarying fluctuating pattern. Suggests moderately severe diffuse cortical dysfunction. Does not normalize with pyridoxine. Additionally, few very focal left central seizure runs. | 7 d |
| F3 | 90(Am) | Spikes | 2 d |
| F4.2 | 72(Lon) | Day 4 showed frequent, high-voltage bursts of bilateral rhythmic 10–12 Hz activity mixed with very high-voltage irregular slow waves at <1–2 Hz | <24 h |
| F5 | 42(Lon) | Frequent spike wave discharges, high-voltage on right but more prominent on left. | 9 weeks |
| H1a | 28(Am) (2 years); 35(Lon) (6 years) | Neonatal: background showing slow delta wave activity mixed with fast activity with frequent long periods of suppressed cerebral activity. There are epileptic features with frequent intermittent episodes of short runs of theta wave activity in the central region with scattered sharp/spiky waves in the left mid parietal region. | 12 h |
| R3a,b | 28 (Am) | On pyridoxine (6 years; 3 months): widespread 5–9 Hz (20–60 mV). At times sharpened over right central regions and posterior 2–4 Hz activity. Some low amplitude fast. | No seizuresc |
| F7.2 | 12(Lon) | Long runs of sharp waves independently on both sides. | 3 d |
| H2a | 15(Am) (2 years); 11(Lon) (6 years) | Neonatal: slow delta wave activity mixed with beta activity and periods of suppressed cerebral activity. Short runs of rhythmic theta wave activity of sharp configuration in the central region with scattered sharp spiky waves occurring on either side. | 12 h |
| F10 | 14(Lon) | Intermittent burst suppression | 2 h |
| F12 | 11(Am) | No EEG prior to treatment with pyridoxine. Normal whilst on pyridoxine. | <24 h |
| F13 | 11 | First EEG after pyridoxine—‘immature’ | 2 d |
| F14 | 11(Am) | Burst suppression pattern | 4 d |
| F15 | 10(Lon) | Sharp spike waves and waves with right temporal emphasis (<14 weeks). Six months: multi focal spike in association with status epilepticus. Reduction of burst suppression in response to pyridoxine. EEG normalized after 12 days after pyridoxine treatment commenced. | 14 d |
| R2a,b | 7.8(Am) | On pyridoxine (7 years; 4 months): irregular 4–7 Hz (20–70 mV) theta activity dominates the record. 8–11 Hz faster components intermixed. 2–3 Hz delta transients occur intermixed posteriorly. | 4 h |
| R1a,b | 7.4(Am) | On pyridoxine (7 years): some theta waves intermixed with higher frequencies over both right and left temporal areas. Regular spike discharges from right temporosylvian area, increased during sleep. | 4 h |
| F16 | 7(Lon) | Left-sided epileptiform discharges | 5 d |
| F17 | 4(Am) | Hypsarrythmia at 6 weeks | 1 d |
| F19 | 1.3(Am) | 3–4 Hz activity post centrally. Irregular fast and spiking right and left | 14 m |
(Lon)/(Am) = AASA measured in London or Amsterdam, respectively.
a Mutation analyses published previously (Mills et al., 2006).
b Detailed clinical histories (Rankin et al., 2007).
c Treated from in utero; no withdrawal trial ever given.
The MRI findings (Table 6) in antiquitin deficiency were diverse varying from normal to significant cortical dysplasia or hydrocephalus requiring a ventriculoperitoneal shunt. There was no apparent relationship between biochemical (α-AASA) or genetic mutation and MRI or EEG findings.
Table 6.
Summary of MRI findings for patients with an elevated concentration of urinary α-AASA
| Family | α-AASA (mmol/mol creatinine) | MRI/neuropathology | Age of onset |
|---|---|---|---|
| F1.2 | 316(Am) | Neonatal MRI: diffuse signal and density abnormality of the white matter in both cerebral hemispheres | 1 h |
| F2 | 93(Lon) (9 days); 138(Lon) (3 m) | Foetal: mild ventriculomegaly and enlarged posterior ventricles. Neonatal: petechial haemorrhage in periventricular white matter and deep white matter lesions; consistent with periventricular leucomalacia. Four months: long-standing hydrocephalus | 7 d |
| F3 | 90(Am) | Nothing abnormal detected | 2 d |
| F4.2 | 72(Lon) | Neonatal: agenesis of corpus callosum, neuronal heterotopias, cerebellar hypoplasia; subependymal grey matter heterotopia at temperal horn tips. | <24 h |
| F5 | 42(Lon) | Nothing abnormal detected | 9 weeks |
| H1a | 28(Am) (2 years); 35(Lon) (6 years) | Hydrocephalus at 7 months | 12 h |
| R3a,b | 28(Am) | 4 years: borderline normal with a minimal lack of white matter bulk | No seizuresc |
| F8 | 21(Lon) | Neonatal: normal. 10 months: cerebral atrophy of both hemispheres. Poor myelination of cerebral hemispheres. | 6 d |
| H2a | 15(Am) (2 years); 11(Lon) (6 years) | 10 months: nothing abnormal detected | 12 h |
| F10 | 14(Lon) | Nothing abnormal detected | 2 h |
| F11.1 | 11(Am) | Cortical dysplasia (see Supplementary material) | 8 d |
| F13 | 11 | Abnormal: plexus bleeding both posterior ventricle horns, cystic lesions anterior horns | 2 d |
| F14 | 11(Am) | Atrophy especially bifrontal/left temporal regions. Hypoplasia of inferior vermis | 4 d |
| F15 | 10(Lon) | Neonatal: right frontal lobe focal brain abnormality? Cortical dysplasia. Background of diffuse change. Damage to lentiform nucleus | 14 d |
| R2a,b | 7.8(Am) | 5 years; 8 months: white matter hypoplastic to a moderate degree with global lack of bulk. This included the corpus callosum, brainstem, cerebellum and pons. | 4 h |
| R1a,b | 7.4(Am) | 7 years; 3 months: global lack of white matter bulk to a mild degree. Thinning of the posterior region of the corpus callosum. | 4 h |
| F16 | 7(Lon) | Nothing abnormal detected | 5 d |
| F17 | 4(Am) | Agenesis corpus callosum, megacisterna magna, hydrocephalus | 1 d |
| F19 | 1.3(Am) | Nothing abnormal detected | 14 m |
(Lon)/(Am) = AASA measured in London or Amsterdam, respectively.
a Mutation analyses reported previously (Mills et al., 2006).
b Detailed clinical histories (Rankin et al., 2007).
c Treated from in utero; no withdrawal trial ever given.
One patient underwent focal resective epilepsy surgery; neuropathology of the cortex showed Grade II cortical dysplasia (Supplementary material).
Discussion
Urinary α-AASA as a diagnostic test
This study confirms that, in infants and children with a seizure disorder, elevated urinary α-AASA excretion is a good marker for detecting individuals who have PDE due to mutations in the ALDH7A1 gene, provided that age-related control ranges are used. Because the ALDH7A1 gene was not sequenced in all patients with normal α-AASA excretion, we cannot be completely sure that the test does not produce false negative results, but this is unlikely as none of these patients were shown to meet the clinical criteria for PDE.
Mutations
This article takes the number of published disease causing mutations in ALDH7A1 to 64. Whilst many of the mutations were ‘private’ mutations some of the exons appear to be mutation ‘hot spots’. Our analyses further strengthen published findings (Plecko et al., 2007; Salomons et al., 2007; Bennett et al., 2009); that E399Q (exon 14) is a common mutation responsible for ∼30% of mutated alleles. An additional six mutations (nine families) are found in exon 14. Other ‘hot spots’ include exon 6 (five mutations; eight families), exon 11 (six mutations; seven families), exon 9 (5 mutations; 14 families) and exon 4 (three mutations; nine families). The ‘silent’ mutation (c.750G>A; exon 9) (Salomons et al., 2007) has now been detected in 11 patients, all of whom are of Caucasian origin. These data suggest that an initial screen of ALDH7A1 in Caucasian patients should include exons 4, 6, 9, 11 and 14, as ∼60% of the reported mutations to date have been located in these regions of the gene.
The novel missense mutations P169S, P78L, W175G, S289L, Q300R and S448L all occur in regions that are highly conserved in antiquitin across species. P169 is present in the majority of the aldehyde dehydrogenase superfamily (to which antiquitin belongs) and is one of the 12 invariant residues that are found in more than 95% of 145 full-length aldehyde dehydrogenase-related sequences when they were aligned (Perozich et al., 1999). This proline residue lies at a critical turn in the class 3 aldehyde dehydrogenase structures. The homozygous missense mutation Q300R occurs in a region of the antiquitin gene that is not only highly conserved across all species (except soybean) but is indeed one of the 37 residues that have been shown to be conserved in at least 80% of the aldehyde dehydrognase family (Perozich et al., 1999), suggesting that it may have an important structural and/or functional role of the enzyme as an aldehyde dehydrogenase. Conversely, whilst P78, W175 and S289 are conserved in antiquitin across species, they are not conserved across the aldehyde dehydrogenase superfamily, suggesting that these residues are important more specifically for the function/activity of the α-AASA dehydrogenase and not for aldehyde dehydrogenases per se.
The novel missense mutations A129P, A149E and T398P do not occur in such highly conserved regions of antiquitin; A129 and A149 are conserved across mammalian species whilst residue 398 is T in most species but not in plants, rat, mouse and opossum. Because of the conformational rigidity of proline compared to other amino acids it is likely that the substitution of A129 or T398 with this amino acid affects the secondary structure and activity of the protein.
The novel insertion of a single nucleotide c.191_192insA and the single base deletions, c.758delA and c.749delT, are all predicted to result in frameshifts in the nucleotide sequence. The insertion would be predicted to cause a frameshift in the nucleotide sequence resulting in a change of the amino acid sequence creating a premature termination codon (17LGLREENEGVY27 … → 17LGLSRGKNGRV27X). This predicts a highly truncated protein and the coding mRNA is likely to be degraded by nonsense-mediated mRNA decay. c.758delA would alter the next three amino acid residues (250VGKQVGLM257 … → 250VGKRWA255X) prior to introducing an in-frame stop codon, which would result in a highly truncated protein of 255 instead of 511 amino acid residues. c.[749delT] is predicted to result in a frameshift in the nucleotide sequence altering the next six amino acid residues (246GSTQVGKQ253 … → 246GSTQGENRWA255X) prior to introducing an inframe stop codon. This new stop codon is at the same position as that which is introduced by the deletion c.758delA. The deletion c.787+3delAAGT, however, is predicted to affect splicing resulting in ablation of the normal donor site. The novel nonsense mutation, R53X would be expected to result in a severely truncated protein and mRNA that is degraded by nonsense-mediated decay. Unfortunately a source of cDNA was not available to characterize any of these mutations further.
Biochemical phenotype
A comparison of pre-treatment CSF amino acid profiles in patients with antiquitin deficiency (PDE) and pyridoxine-5′-phosphate oxidase deficiency (pyridoxal phosphate-dependent epilepsy) (Table 7) shows that differential diagnosis based on amino acid profiles and amine metabolites is not straightforward (Hoffmann et al., 2007). Biochemical analyses showed evidence of secondary deficiencies of several pyridoxal phosphate-dependent enzymes. Raised levels of CSF threonine, glycine, taurine and 3-methoxytyrosine were evident in >50% of patients with antiquitin deficiency and pyridoxine-5′-phosphate oxidase deficiency, suggesting that biochemical abnormalities in PDE may mimic those of pyridoxine-5′-phosphate oxidase deficiency. Differentiating the two disorders should therefore include α-AASA measurement [for antiquitin deficiency (PDE)], alongside assessment of the response to pyridoxine and/or pyridoxal phosphate. Several previous reports (Kurlemann et al., 1992; Gospe et al., 1994; Goto et al., 2001) have suggested that an imbalance between excitatory (glutamate) and inhibitory (GABA) mechanisms via the pyridoxal phosphate-dependent enzyme glutamate dehydrogenase may play a role in seizure development in PDE. Results reported here (low or normal CSF glutamate) argue against a major role for glutamate excitotoxicity, although as GABA is not routinely measured, we cannot exclude GABA deficiency as a potential seizure mechanism. It remains likely that the clinical features of PDE result from the dysfunction of several pyridoxal phosphate dependent enzymes. A response to pyridoxal phosphate in an infant who failed to respond to pyridoxine is highly suggestive of pyridoxine-5′-phosphate oxidase deficiency. The case histories presented in detail (Supplementary material), however, illustrate that therapeutic trials with pyridoxine may be complicated by concomitant treatment with antiepileptic drugs; with partial response to these drugs and additional biochemical causes of seizures in PDE such as hypocalcaemia and hypomagnesaemia.
Table 7.
Comparison of the pre-treatment CSF amino-acid profiles in our patients with PDE and pyridoxine-5′-phosphate oxidase deficiency (pyridoxal phosphate-dependent epilepsy)
| Biochemical result | PDE | Pyridoxal phosphate- dependent epilepsy |
|---|---|---|
| CSF glycine ↑ | 3/5 | 6/10 |
| CSF threonine ↑ | 5/5 | 6/10 |
| CSF taurine ↑ | 1/2 | 5/10 |
| CSF histidine ↑ | 1/4 | 6/10 |
| CSF 3-methoxytyrosine ↑ | 2/2 | 6/9 |
| Plasma glycine ↑ | 5/5 | 4/5 |
| Plasma threonine ↑ | 0/5 | 3/5 |
| Plasma taurine ↑ | 3/5 | 1/2 |
| Plasma proline ↑ | 3/5 | 0/1 |
↑ = elevated.
Clinical phenotype
Additional presenting features included metabolic acidosis, respiratory distress, hypotonia, irritability, abdominal distension and enteral feed intolerance (requiring parenteral nutrition) in a proportion of early onset, typical cases. Prematurity (<37/40) and foetal distress with low Apgar scores mimicking birth asphyxia were also observed in some cases.
In keeping with previous reports (Baxter, 2001; Basura et al., 2009), neurodevelopmental outcome is impaired in the majority of cases, however, as some of our data were qualitative in nature it is difficult to draw conclusions regarding the relationship of outcome to age at diagnosis and treatment with pyridoxine. Cases of delayed diagnosis and treatment are compatible with normal neurological outcome (Basura et al., 2009); equally, prompt treatment with pyridoxine in screened siblings does not guarantee a normal neurodevelopmental outcome (Rankin et al., 2007).
In siblings F4.1 and F4.2, electrolyte disturbance and endocrine abnormalities were major management problems (and may have contributed to the delay in the diagnosis of pyridoxine dependency). Measurements of plasma parathyroid hormone at times of hypocalcaemia suggested hypoparathyroidism. There is one previous case report of hypocalcaemia occurring in a neonate with PDE (Lauras et al., 1984). Patient F4.2 also had biochemical evidence of hypothyroidism and of diabetes insipidus. These abnormalities resolved with vitamin B6 therapy suggesting that they were secondary to inactivation of pyridoxal phosphate in parathyroid/thyroid/pituitary/hypothalamus cells. It may be that the pathway of lysine degradation in these cells follows the ‘brain pathway’ via P6C and α-AASA, allowing P6C to inactivate pyridoxal phosphate in the same way as is proposed to occur in the brain (Clayton, 2006a, b; Mills et al., 2006).
Two siblings (F1.1 and F1.2) treated with pyridoxine remained neurologically abnormal with persistent hypotonia despite good seizure control. They had persistent vomiting and both developed fatal Escherichia coli sepsis at one month of age for which immunological work-up failed to reveal a cause. There is one previous report of severe neonatal infection with E. coli in a patient with PDE (Adam et al., 1972).
Late onset PDE cases do not usually show major additional features (Baxter, 2001). Previously published findings have shown mutations in ALDH7A1 in children whose seizures started as late as 6 months of age (Bennett et al., 2009). In this study, mutations in ALDH7A1 were found in children whose seizures did not start until 8 and 14 months of age, respectively.
Electroencephalography, magnetic resonance imaging and neuropathology
In this series, no particular EEG abnormality was consistently observed in antiquitin deficiency (Tables 5 and 6). Burst suppression was observed in some cases and hypsarrhythmia in others. The most common MRI finding was an abnormality of white matter often involving reduced bulk e.g. of the corpus callosum and/or cerebellar white matter. There were no pathognomonic EEG and MRI features that could alert the clinician or provide diagnostic clues in advance of biochemical or genetic results. Additionally there was no apparent relationship between biochemical (α-AASA) or genetic mutation and MRI or EEG findings.
The findings of cortical dysplasia (histologically proven in one patient) and antenatal-onset hydrocephalus, support the role of vitamin B6 in the developing brain. Impaired neuronal migration may be an important feature in the pathogenesis of neurodevelopmental dysfunction that persists following control of epilepsy in some patients with PDE. It has recently been established that the pyridoxal phosphate-dependent enzyme serine racemase plays an important role in control of neuronal migration (Kim et al., 2005) and this may provide an explanation for deranged neuronal migration in some patients with PDE. Our results suggest that prior to accepting that an area of cortical dysplasia is the cause of intractable epilepsy, a urine test for α-AASA and a therapeutic trial of pyridoxine should be undertaken.
Genotype–phenotype correlation
Because of the urgency of treatment, data on urinary α-AASA prior to treatment are limited and so it is difficult to ascertain if there is any correlation with genotype. However, there appears to be very little correlation between urinary α-AASA concentration on pyridoxine treatment and genotype. A wide range of concentrations is seen in treated patients that are homozygous for the ‘common’ E399Q missense mutation (Mills et al., 2006; Plecko et al., 2007; Salomons et al., 2007). Indeed E399Q has been reported to cause both neonatal- and late-onset PDE (Bennett et al., 2009). Interestingly in our series, however, the three children (<6 months) with the highest urinary α-AASA concentrations (F1.2, F2 and F4.2) all had a very severe phenotype. Whether this represents some genotype–phenotype correlation is unclear. Only the mutations found in F2 have been described previously. Whilst Asn273Ile was found in a patient with later onset PDE (Bennett et al., 2009), clinical details for the patient carrying Gly83Glu have not been published (Gallagher et al., 2009). It is noteworthy that 2/3 patients in this study with late-onset PDE had the mutation W175G. Molecular modelling of delta(1)-pyrroline-5-carboxylate dehydrogenase (Tang et al., 2008), which accepts the substrate glutamate-γ-semialdehyde (whose aliphatic chain is one CH2 unit shorter than that of α-AASA), indicates that W175 in antiquitin is replaced by glycine—the exact scenario seen in F19 and F20. Indeed the concentration of urinary α-AASA in F19 was only just above the upper limit of the control range of the laboratory in Amsterdam where this sample was analysed. This may be a reflection of the disease severity in this patient, who is seizure free and coping well with mainstream school. Whilst it may be interesting to speculate that W175G is associated with late-onset PDE, mutation analysis of antiquitin in three other patients with late-onset PDE (Bennett et al., 2009) and F5 revealed that one of the patients is homozygous for the ‘common’ E399Q mutation and the other patients are heterozygous for T297R/E399Q, N273I/E399G and S448L/E399Q. Four out of five of these mutations have also been reported in patients with neonatal-onset PDE. The relationship between genotype, over production of α-AASA/P6C, inactivation of pyridoxal phosphate and clinical phenotype is likely to be complex. Determinants of brain pyridoxal phosphate level may include genotype, dietary lysine intake, anabolic/catabolic state, pyridoxine intake, other environmental factors (e.g. infection) and polymorphisms in other genes involved in lysine catabolism and/or pyridoxal phosphate homeostasis.
Conclusion
In conclusion, the clinical diagnosis of PDE may be very challenging because: (i) neonates and infants can have multisystem pathology; (ii) the tendency to regard structural brain abnormalities as a sufficient cause of epilepsy may prevent clinicians considering alternative diagnoses such as PDE; (iii) there may be some response to antiepileptic drugs; and (iv) the response to pyridoxine may not be immediate and total. Our findings support the use of biochemical and DNA tests for antiquitin deficiency in a wide range of infants with epilepsy. We suggest that an adequate trial of pyridoxine (minimum 72 h) with careful clinical and EEG monitoring is necessary and if there is any sign of improvement, then pyridoxine should be continued. A repeat trial should be considered if seizures remain poorly controlled. Measurement of urinary α-AASA should be performed for all neonates with intractable seizures, regardless of the presence of MRI findings of brain structural abnormalities.
Funding
Wellcome Trust (P.B.M. and P.T.C.).
Supplementary material
Supplementary material is available at Brain online.
Supplementary Material
Acknowledgements
We would like to thank the families for participating in the study. We would also like to thank all replying clinicians for their cooperation, in particular the following for kindly providing patient data: Prof. R.A.H. Surtees, Dr P Jardine, Dr M. Champion, Dr D. Lumsden, Dr H. Mundy, Dr A. Fenton, Dr M.A. McShane, Dr J.R. James, Dr O. Maier, Dr M. Kumar, Prof. J. Christodoulou, Dr K. Metcalfe, Dr M. Farrier, Dr G. Kendall, Dr M. O’Driscoll and Dr T. Rootwelt.
Glossary
Abbreviations
- α-AASA
l-α-aminoadipic semialdehyde
- P6C
l-Δ1-piperideine 6-carboxylate
- PDE
pyridoxine-dependent epilepsy
References
- Adam E, Goor M, Delattre B, Farriaux JP, Fontaine G. Les convulsions pyridoxino-dépendantes – a propos d’un noveau cas. Pédiatrie. 1972;27:19–25. [PubMed] [Google Scholar]
- Basura GP, Hagland SP, Wiltse AM, Gospe SM., Jr Clinical features and the management of pyridoxine-dependent and pyridoxine-responsive seizures: review of 63 North American cases submitted to a patient registry. Eur J Pediatr. 2009;168:697–704. doi: 10.1007/s00431-008-0823-x. [DOI] [PubMed] [Google Scholar]
- Baxter P. Pyridoxine dependent/responsive seizures. In: Baxter P, editor. Vitamin responsive conditions in paediatric neurology. London: Mac Keith Press; 2001. pp. 109–165. [Google Scholar]
- Bennett CL, Chen Y, Hahn S, Glass IA, Gospe SM., Jr Prevalence of aldehyde dehydrogenase7A1 mutations in 18 North American pyridoxine-dependent seizure (PDS) patients. Epilepsia. 2009;50:1167–75. doi: 10.1111/j.1528-1167.2008.01816.x. [DOI] [PubMed] [Google Scholar]
- Clayton PT. B6-responsive disorders: a model of vitamin dependency. J Inher Metab Dis. 2006a;29:317–26. doi: 10.1007/s10545-005-0243-2. [DOI] [PubMed] [Google Scholar]
- Clayton PT. Pyridoxine-dependent epilepsy due to α-aminoadipic semialdehyde dehydrogenase (antiquitin) deficiency. In: Valle D, Beaudet AL, Vogelstein B, Kinzler KW, Antonarakis SE, Ballabio A, et al., editors. The on-line metabolic and molecular bases of inherited disease. 2006b. [(May 2010, date last accessed)]. http://www.ommbid.com/OMMBID/the_online_metabolic_and_molecular_bases_of_inherited_disease/b/fulltext/part8/ch86.1/1; Chapter 86.1. [Google Scholar]
- Gallagher RC, Van Hove JLK, Scharer G, Hyland K, Plecko B, Waters PJ, et al. Folinic acid-responsive seizures are identical to pyridoxine-dependent epilepsy. Ann Neurol. 2009;65:550–6. doi: 10.1002/ana.21568. [DOI] [PubMed] [Google Scholar]
- Gospe SM, Olin KL, Keen CL. Reduced GABA synthesis in pyridoxine dependent seizures. Lancet. 1994;343:1133–4. doi: 10.1016/s0140-6736(94)90236-4. [DOI] [PubMed] [Google Scholar]
- Goto T, Matsuo N, Takahashi T. CSF glutamate/GABA concentrations in pyridoxine-dependent seizures: etiology of pyridoxine-dependent seizures and the mechanisms of pyridoxine action in seizure control. Brain Dev. 2001;23:24–9. doi: 10.1016/s0387-7604(00)00193-5. [DOI] [PubMed] [Google Scholar]
- Hoffmann GF, Schmitt B, Windfuhr M, Wagner N, Strehl H, Bagci S, et al. Pyridoxal 5'-phosphate may be curative in early-onset epileptic encephalopathy. J Inherit Metab Dis. 2007;30:96–9. doi: 10.1007/s10545-006-0508-4. [DOI] [PubMed] [Google Scholar]
- Hunt AD, Jr, Stokes J, Jr, McCrory WW, Stroud HH. Pyridoxine dependency: report of a case of intractable convulsions in an infant controlled by pyridoxine. Pediatrics. 1954;13:140–5. [PubMed] [Google Scholar]
- Kaczorowska M, Kmiec T, Jakobs C, Kacinski M, Kroczka S, Salomons GS, et al. Pyridoxine-dependent seizures caused by alpha amino adipic semialdehyde dehydrogenase deficiency: the first polish case with confirmed biochemical and molecular pathology. J Child Neurol. 2008;23:1455–9. doi: 10.1177/0883073808318543. [DOI] [PubMed] [Google Scholar]
- Kanno J, Kure S, Narisawa A, Kamada F, Takayanagi M, Yamamoto K, et al. Allelic and non-allelic heterogeneities in pyridoxine dependent seizures revealed by aldehyde dehydrogenase7A1 mutational analysis. Mol Genet Metab. 2007;91:384–9. doi: 10.1016/j.ymgme.2007.02.010. [DOI] [PubMed] [Google Scholar]
- Kim PM, Aizawa H, Kim PS, Huang AS, Wickramasinghe SR, Kashani AH, et al. Serine racemase: activation by glutamate neurotransmission via glutamate receptor interacting protein and mediation of neuronal migration. Proc Natl Acad Sci USA. 2005;102:2105–10. doi: 10.1073/pnas.0409723102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluger G, Blank R, Paul K, Paschke E, Jansen E, Jakobs C, et al. Pyridoxine-dependent epilepsy: normal outcome in a patient with late diagnosis after prolonged status epilepticus causing cortical blindness. Neuropediatrics. 2009;39:276–9. doi: 10.1055/s-0029-1202833. [DOI] [PubMed] [Google Scholar]
- Kurlemann G, Ziegler R, Grüneberg M, Bömelburg T, Ullrich K, Palm DG. Disturbance of GABA metabolism in pyridoxine-dependent seizures. Neuropediatrics. 1992;23:257–9. doi: 10.1055/s-2008-1071353. [DOI] [PubMed] [Google Scholar]
- Lauras B, Drevon B, Rolland MO, Teyssier G, Bovier-Lapierre M, Freycon F. Convulsions pyridoxino-dépendantes : Observation familiale. Pédiatrie. 1984;39:183–7. [PubMed] [Google Scholar]
- Mills PB, Struys E, Jakobs C, Plecko B, Baxter P, Baumgartner M, et al. Mutations in antiquitin in individuals with pyridoxine-dependent seizures. Nat Med. 2006;12:307–9. doi: 10.1038/nm1366. [DOI] [PubMed] [Google Scholar]
- Nabbout R, Soufflet C, Plouin P, Dulac O. Pyridoxine dependent epilepsy: a suggestive electroclinical pattern. Arch Dis Child Fetal Neonatal Ed. 1999;81:F125–9. doi: 10.1136/fn.81.2.f125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormazabal A, Oppenheim M, Serrano M, García-Cazorla A, Campistol J, Ribes A, et al. Pyridoxal 5′-phosphate values in cerebrospinal fluid: reference values and diagnosis of PNPO deficiency in paediatric patients. Mol Genet Metab. 2008;94:173–7. doi: 10.1016/j.ymgme.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Peduto A, Baumgartner MR, Verhoeven NM, Rabier D, Spada M, Nassogne MC, et al. Hyperpipecolic acidaemia: a diagnostic tool for peroxisomal disorders. Mol Genet Metab. 2004;82:224–30. doi: 10.1016/j.ymgme.2004.04.010. [DOI] [PubMed] [Google Scholar]
- Perozich J, Nicholas H, Wang BC, Lindahl R, Hempel J. Relationships within the aldehyde dehydrogenase extended family. Protein Sci. 1999;8:137–46. doi: 10.1110/ps.8.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plecko B, Hikel C, Korenke GC, Schmitt B, Baumgartner M, Baumeister F, et al. Pipecolic acid as a diagnostic marker of pyridoxine-dependent epilepsy. Neuropediatrics. 2005;36:200–5. doi: 10.1055/s-2005-865727. [DOI] [PubMed] [Google Scholar]
- Plecko B, Paul K, Paschke E, Stoeckler-Ipsiroglu S, Struys E, Jakobs C, et al. Biochemical and molecular characterization of 18 patients with pyridoxine-dependent epilepsy and mutations of the antiquitin (ALDH7A1) gene. Hum Mutat. 2007;28:19–26. doi: 10.1002/humu.20433. [DOI] [PubMed] [Google Scholar]
- Rankin PM, Harrison S, Chong WK, Boyd S, Aylett SE. Pyridoxine-dependent seizures: a family phenotype leads to severe cognitive deficits, regardless of treatment regime. Dev Med Child Neurol. 2007;49:300–5. doi: 10.1111/j.1469-8749.2007.00300.x. [DOI] [PubMed] [Google Scholar]
- Salomons GS, Bok LA, Struys EA, Pope LL, Darmin PS, Mills PB, et al. An intriguing silent mutation and a founder effect in antiquitin (ALDH7A1) Ann Neurol. 2007;62:414–8. doi: 10.1002/ana.21206. [DOI] [PubMed] [Google Scholar]
- Striano P, Battaglia S, Giordano L, Capovilla G, Beccaria F, Struys EA, et al. Two novel ALDH7A1 (antiquitin) splicing mutations associated with pyridoxine-dependent seizures. Epilepsia. 2009;50:933–6. doi: 10.1111/j.1528-1167.2008.01741.x. [DOI] [PubMed] [Google Scholar]
- Tang WK, Wong KB, Lam YM, Cha SS, Cheng CH, Fong WP. The crystal structure of seabream antiquitin reveals the structural basis of its substrate specificity. FEBS Lett. 2008;582:3090–6. doi: 10.1016/j.febslet.2008.07.059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.